- 1Mohamed VI University Hospital, Nuclear Medicine Department, Cadi Ayyad University, Marrakesh, Morocco
- 2TTA University Hospital, Nuclear Medicine Department, Abdelmalek Esaadi University, Tangier, Morocco
Lung scan is an accurate and noninvasive tool for evaluating the distribution of lung perfusion. We present a rare case of total absence of perfusion on lung scan to the right lung with two contralateral defects due to severe occlusion of the right pulmonary artery, as well as segmental arteries in the left lung in a young female woman diagnosed with Takayasu Arteritis. We highlight the similarities of the findings between pulmonary arteritis in Takayasu disease and thromboembolic disease and the importance of careful interpretation of perfusion lung scan in order to avoid misdiagnosis that could endanger the patient's life.
Introduction
Absence of perfusion to an entire lung on perfusion lung scan with a preserved ventilation is an uncommon yet dramatic finding, accounting for 2% of all lung scans (1). Only a minority of these are due to pulmonary embolism (1). Therefore, other possibilities should be strongly considered to avoid a false positive diagnosis. The most common causes of this finding are external compression by a bronchogenic carcinoma and congenital heart disease (2). Occlusion of a pulmonary artery due to arteritis may result in this appearance but is an uncommon cause (2). We present a patient with Takayasu arteritis (TA) subjected to perfusion lung scan who showed a unilateral absence of perfusion to the right lung as well as contralateral perfusion defects, mimicking pulmonary embolism (PE).
Case presentation
A 36 years old female patient, diagnosed with Takayasu Arteritis one year ago based on clinical, biological and imaging features. She was referred to our department for a perfusion lung scan for suspicion of pulmonary embolism after presenting with chest pain and acute exacerbation of her chronic dyspnea. The patient underwent perfusion lung scan after injection of 148 MBq (4 mCi) of 99mTc-MAA in the supine position. Six views were obtained with a gamma camera with a low energy high resolution parallel hole collimator. Pulmonary ventilation scintigraphy was not available in our department. We completed with a single photon emission tomography combined with computed tomography (SPECT/CT). Planar images (Figure 1) showed a total absence of perfusion to the right lung with a contralateral perfusion defect.
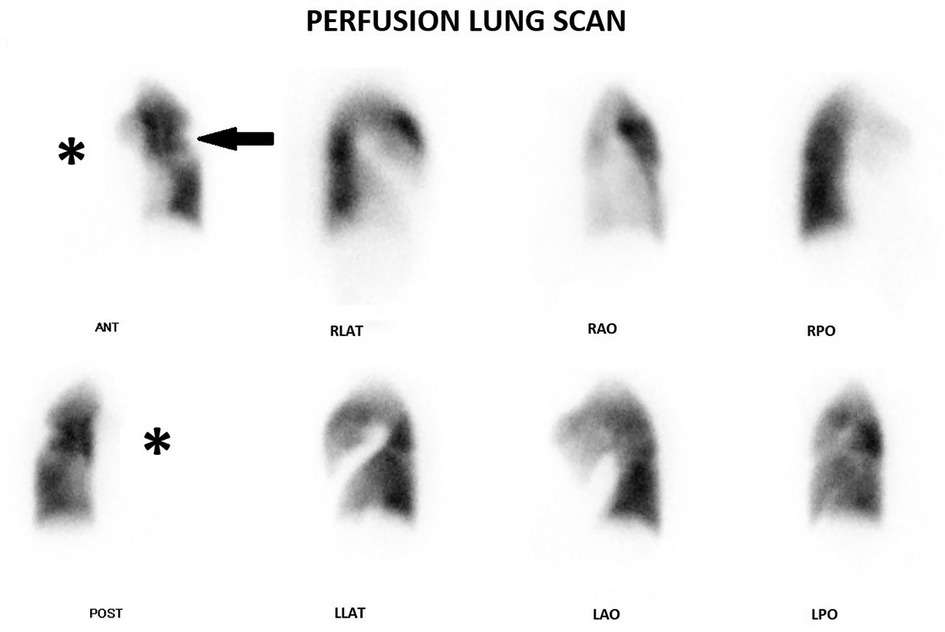
Figure 1. Planar images show a total absence of perfusion to the right lung (star) with a contralateral defect (arrow).
Subsequent SPECT/CT (Figure 2) revealed segmental defects in the lingula and the anterior and posterior segments of the culmen with no lung parenchymal changes in the corresponding CT. We suspected severe occlusion of pulmonary arteries as well as pulmonary embolism. Because a total absence of perfusion to an entire lung is hardly due to pulmonary embolism, we recommended that the patient undergoes a chest angiographic CT (Figure 3) which confirmed a severe stenosis of the right pulmonary artery and the left upper lobar artery as well as inferior segmental ones. This finding in our patient was consistent with a severe involvement of pulmonary arteries in Takayasu disease rather than pulmonary embolism. The patient was initially on prednisolone 5 mg per day, treatment with high-dose prednisolone (120 mg per day) and azathioprine was started right away and symptoms gradually improved within one month. The patient was then lost to further follow up, all attempts to locate her via phone were unsuccessful.
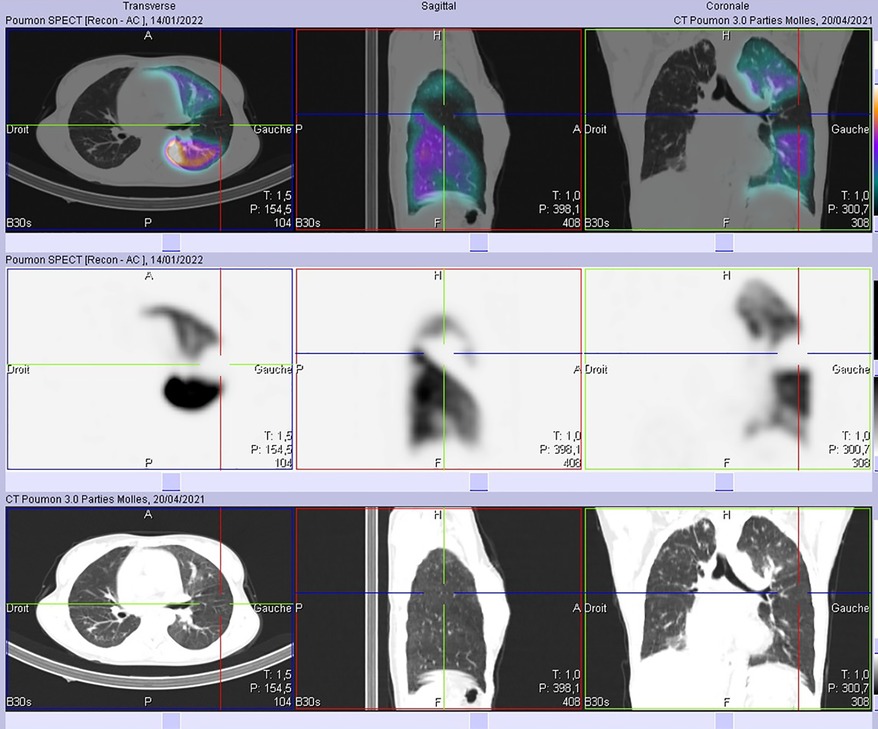
Figure 2. No abnormal parenchymal findings were seen in both lung fields adjacent to the defects on SPECT-CT images.
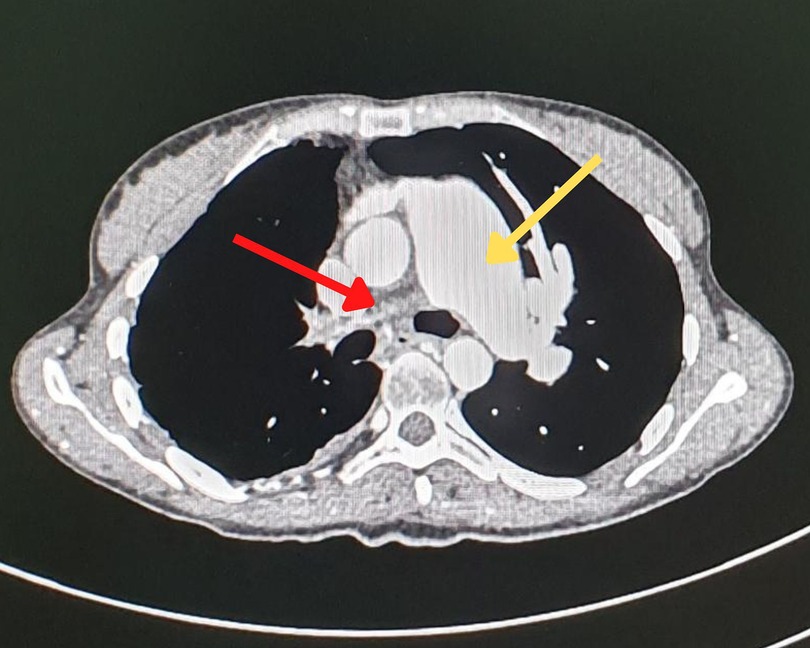
Figure 3. Chest angiographic CT showing a dilatation of the main pulmonary artery (yellow arrow) and a lack of the opacification of the right pulmonary artery (red arrow), consistent with a severe stenosis of the latter.
Discussion
Lung scan is an accurate and noninvasive tool for evaluating the distribution of lung perfusion. The main indication is evaluation of suspected pulmonary embolism with a fairly high accuracy especially with the introduction of single photon emission tomography (SPECT) combined with low dose CT (3). However, the rate of false positive scans is not negligible (4).
Unilateral absence of perfusion to an entire lung on a radionuclide scan is a very rare occurrence. According to a series of 607 lung scans, it accounts for 2% of cases (1). This appearance classically suggests an external compression of the pulmonary arteries by a tumor, mostly bronchogenic carcinoma. Less common entities include congenital heart disease, pneumonectomy and pulmonary embolism (2). The latter being very unlikely particularly with a normal contralateral lung perfusion (5).
Takayasu arteritis is a chronic vasculitis of unknown origin that involves the aorta and its main branches and leads to vascular thickening, stenosis and occlusion (6). Besides the aorta and its branches, pulmonary arteries can also be involved. Their involvement in TA is of late diagnosis because of non-specific symptoms, but it's not infrequent even in the absence of symptoms. Its prevalence varies widely among series and it could be as high as 80% (7).
Radionuclide lung scanning is a simple and safe way to evaluate pulmonary arteries involvement in Takayasu disease (8). The abnormalities in lung scan in Takayasu arteritis can be quite similar to those in pulmonary embolism, showing decreased or absent perfusion corresponding to specific blood vessels. Despite the difficulty to differentiate Takayasu arteritis from pulmonary embolism without clinical findings, there are some differences in the lung scans between these two diseases. In pulmonary embolism, perfusion defects often resolve, particularly in younger patients. On the other hand, perfusion defects in Takayasu arteritis do not change for a long time. These findings might be useful in ruling out pulmonary embolism (8). In contrast, it is generally uncomplicated to differentiate between stenotic lesions and emboli on an angiographic CT. stenotic lesions may appear as areas of narrowing or obstruction within the blood vessel, while emboli may appear as denser, round or oval-shaped areas within the vessel.
Classically, pulmonary arteritis in TA results in multiple perfusion mismatch defects on Ventilation/perfusion lung scan. Although TA can cause unilateral absence of perfusion, in rare cases it can mimic acute pulmonary embolism. As far as we are aware, our case is the third report of unilateral absence of perfusion occurring in a Takayasu arteritis patient. Two prior reports have been described where the diagnosis of TA was not yet known at the time of lung scan which made the interpretation quite tricky and led to misdiagnosis as pulmonary embolism (PE) (9, 10).
In our case, although the diagnosis of TA was established before perfusion lung scan, PE was included in the differential diagnosis because of the clinical presentation, the contralateral systematized defects and the high risk of association of thromboembolism with vasculitis (11). This finding in our patient suggests a long evolution of the disease and thus TA is at the chronic stage, as it was demonstrated in a Japanese study (12).
Conclusions
Our case highlights two important points: (I) a rare occurrence of total absence of perfusion to an entire lung due to an uncommon etiology which is TA. (II) interpretation of perfusion lung scan should be careful and clinical features as well as medical history should be taken into account before giving a diagnosis that could endanger the life of the patient.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
The authors confirm contribution to the paper as follows: 1. Concept and design of the article: CS and SH. 2. Data collection: NK. 3. Draft manuscript preparation: CS. 4. Providing critical feedback: SH. 5. Supervision and approval for publication: MAB and AM. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. White RI, James AE, Wagner HN. The significance of unilateral absence of pulmonary artery perfusion by lung scanning. AJR Am J Roentgenol. (1971) 111:501–9. doi: 10.2214/ajr.111.3.501
2. Thomason CB, Rao BR. Lung imaging—unilateral absence or near absence of pulmonary perfusion on lung scanning. Semin Nucl Med. (1983) 13:388–90. doi: 10.1016/s0001-2998(83)80052-x
3. Gutte H, Mortensen J, Jensen CV, Johnbeck CB, von der Recke P, Petersen CL, et al. Detection of pulmonary embolism with combined ventilation–perfusion SPECT and low-dose CT: head-to-head comparison with multidetector CT angiography. J Nucl Med. (2009) 50:1987–92. doi: 10.2967/jnumed.108.061606
4. Rigolon MY, Mesquita CT, Amorim BJ. Guideline for ventilation/perfusion scintigraphy. Int J Cardiovasc Sci. (2018) 32:302–9. doi: 10.5935/2359-4802.20180103
5. Bajc M, Schümichen C, Grüning T, Lindqvist A, Le Roux PY, Alatri A, et al. EANM Guideline for ventilation/perfusion single-photon emission computed tomography (SPECT) for diagnosis of pulmonary embolism and beyond. Eur J Nucl Med Mol Imaging. (2019) 46:2429–51. doi: 10.1007/s00259-019-04450-0
6. Seyahi E. Takayasu arteritis: an update. Curr Opin Rheumatol. (2017) 29:51–6. doi: 10.1097/BOR.0000000000000343
7. Kong X, Ma L, Lv P, Cui X, Chen R, Ji Z, et al. Involvement of the pulmonary arteries in patients with Takayasu arteritis: a prospective study from a single centre in China. Arthritis Res Ther. (2020) 22:131. doi: 10.1186/s13075-020-02203-1
8. Suzuki Y, Konishi K, Hisada K. Radioisotope lung scanning in Takayasu's arteritis. Radiology. (1973) 109:133–6. doi: 10.1148/109.1.133
9. Shlomai A, Hershko AY, Gabbay E, Ben-Chetrit E. Clinical and radiographic features mimicking pulmonary embolism as the first manifestation of Takayasu's arteritis. Clin Rheumatol. (2004) 23:470–2. doi: 10.1007/s10067-004-0929-0
10. Brugiere O, Mal H, Sleiman C, Groussard O, Mellot F, Fournier M. Isolated pulmonary arteries involvement in a patient with Takayasu's arteritis. Eur Respir J. (1998) 11:767–70. doi: 10.1183/09031936.98.11030767
11. Emmi G, Silvestri E, Squatrito D, Amedei A, Niccolai E, D’Elios MM, et al. Thrombosis in vasculitis: from pathogenesis to treatment. Thrombosis J. (2015) 13:15. doi: 10.1186/s12959-015-0047-z
Keywords: perfusion lung scan, takayasu arteritis, pulmonary embolism, pulmonary artery stenosis, unilateral absence of perfusion
Citation: Sebbar C, Hiroual S, Kouassi N, Bsiss MA and Matrane A (2023) Pulmonary artery stenosis in Takayasu disease mimicking pulmonary embolism on perfusion lung scan: A case report. Front. Nucl. Med. 3:1122046. doi: 10.3389/fnume.2023.1122046
Received: 12 December 2022; Accepted: 20 January 2023;
Published: 10 February 2023.
Edited by:
Vikas Prasad, Washington University, United StatesReviewed by:
Roberto Sciagrà, Università di Firenze, ItalyÜmit Özgür Akdemir, Gazi University, Türkiye
© 2023 Sebbar, Hiroual, Kouassi, Bsiss and Matrane. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chaimae Sebbar Y2hhaW1hZXNlYkBnbWFpbC5jb20=
Specialty Section: This article was submitted to PET and SPECT, a section of the journal Frontiers in Nuclear Medicine
 Chaimae Sebbar
Chaimae Sebbar Soufiane Hiroual
Soufiane Hiroual Nathalie Kouassi1
Nathalie Kouassi1