
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Mol. Neurosci. , 24 November 2022
Sec. Brain Disease Mechanisms
Volume 15 - 2022 | https://doi.org/10.3389/fnmol.2022.1061076
This article is part of the Research Topic Molecular Dynamics of Cognitive-Motor impairment in Neurodegenerative Diseases View all 7 articles
 Alok Raghav1
Alok Raghav1 Manish Singh1,2
Manish Singh1,2 Goo-Bo Jeong3*
Goo-Bo Jeong3* Richa Giri1,4
Richa Giri1,4 Saurabh Agarwal1,4
Saurabh Agarwal1,4 Sanjay Kala5
Sanjay Kala5 Kirti Amresh Gautam6
Kirti Amresh Gautam6Introduction: Extracellular vesicles (EVs) are known to have a significant role in the central nervous system (CNS) and neurodegenerative disease.
Methods: PubMed, Scopus, ISI Web of Science, EMBASE, and Google Scholar were used to identify published articles about EV modifications (2012 to Feb 2022).
Results: In total, 1,435 published papers were identified among the searched articles, with 1,128 non-duplicate publications being identified. Following the screening of titles and abstracts, 214 publications were excluded; following the full-text screening of 93 published articles, another 33 publications were excluded. The remaining 60 studies were considered. The kappa statistic of 0.868 indicated that the raters were highly reliable. Furthermore, the inter-reliability and intra-reliability coefficients were found to be 0.931 and 0.908, respectively, indicating strong reliability and consistency between the eligible studies identified by the raters. A total of 27 relevant studies demonstrated the role of EVs as therapeutic and diagnostic biomarkers in neurodegenerative diseases. Of note, 19 and 14 studies, respectively, found EVs to be pioneering in diagnostic and therapeutic roles.
Discussion: EVs play an important role in the central nervous system (CNS), aiding in cell-to-cell communication and serving as a diagnostic marker and therapeutic target in a variety of neurodegenerative diseases. EVs are the home of several proteins [including-synuclein (-syn) and tau proteins], lipids, and genetic materials such as DNA and RNA. The presence of novel miRNAs in EVs suggests biomarkers for the diagnosis and screening of neurodegenerative disorders. Furthermore, EVs play an important role in the pathogenesis of such disorders. This systematic review discussed the current state of EVs’ role in neurological diseases, as well as some preclinical studies on the therapeutic and diagnostic potential of EVs.
Extracellular vesicles (EVs) are defined as naturally releasing lipid bilayer delimited vesicles from a cell that cannot replicate. It, which is secreted by the cells, mediates conserved intercellular communications through the content present in their lipid bilayer (Doyle and Wang, 2019). The ISEV nomenclature consensus suggestion is to use “extracellular vesicle” as the “generic term for molecules intuitively launched from the cell that is delimited by a lipid bilayer and cannot replicate” and to modify “EV” based on explicit, specific attributes such as the cell of origin, molecular markers, size, density, function (Théry et al., 2018). EVs secreted as exosomes, microvesicles, and apoptotic bodies from cells exhibit diversity in size, function, secretion pathways, and indigenous cargo (Raghav et al., 2021b). For instance, plasma membrane-derived vesicles are termed microvesicles (150–1,000 nm), while endosome (lumen of internal compartments)-derived vesicles are termed exosomes (< 100 nm) (Théry et al., 2018). Most of the cells release EVs in the form of exosomes rich in biological information including microRNAs (miRNAs), proteins (tetraspanin, membrane-bound, and soluble secreted proteins), peptides, growth factors (GFs), nucleic acids along with other coding information such as lipids, small non-coding RNAs, and long non-coding RNAs that can be exploited for therapeutics and diagnosis purposes (Lötvall et al., 2014; Raghav et al., 2021a). Exosomes are secreted EVs with a cup-shaped spherical morphology and electron microscopic sizes ranging from 30 to 100 nm (Raghav et al., 2021a; Figure 1). These are secreted by a variety of cell types, including hematopoietic cells, primary cells, and cancer cells, as well as biological fluids such as saliva, synovial fluid (SF), serum, plasma, bronchoalveolar lavage (BAL) fluid, urine, amniotic fluid (AF), pleural effusions (PE), and menstrual fluid.
The biogenesis of EVs is a continuous mechanism that starts with inward invagination of the plasma membrane giving rise to early and late endosome bodies by the cells into the cytoplasm (Raghav and Jeong, 2021). Later endosomes further undergo invagination, thereby initiating the formation of membrane-bound intraluminal vesicles (ILVs) within the multivesicular bodies (MVBs) (Raghav and Jeong, 2021). These MVBs combine with the plasma membrane of the cell to release EVs within the extracellular space through exocytosis. The cargo inside the EVs exhibits sorting via the endosomal sorting complex required for transport (ESCRT) dependent and independent pathway. The ESCRT-dependent sorting of cargo involves sequential interaction of ESCRT subunits I, II, and III followed by Vps4 protein for initiating the budding and detachment process from the ESCRT III complex (Raghav and Jeong, 2021). Moreover, ESCRT independent sorting mechanism is mediated by tetraspanins, ceramides, and other protein/lipid interplay (Raghav and Jeong, 2021).
Extracellular vesicles were shown to exhibit numerous functions such as deciphering biological pathways involved in inflammation, angiogenesis, programmed cell death, and morphogen transportation (Hill, 2019). This was evident from previously published studies over a decade that a significant amount of research was performed on exploiting EVs for cancer-related studies (Hill, 2019). The EVs have the ability for modification and transportation of desired cargo to desired cells due to their property of flexible lipid bilayer structure, thereby these EVs played important role in the pathogenesis, therapeutics, and diagnosis of several neurological conditions, especially neurodegenerative diseases such as Parkinson’s disease, Alzheimer’s disease, Creutzfeldt–Jakob disease, and amyotrophic lateral sclerosis associated with the misfolded proteins. Besides contributing to the pathogenesis of neurodegenerative diseases, EVs also provide a useful source of biomarkers for such neural complications. A previously published study showed that glioblastoma-derived EVs containing mRNAs/miRNAs at the periphery location can be used as a biomarker for a number of neurological disorders (Redzic et al., 2014).
In Alzheimer’s disease, neural cell-derived EVs are responsible to transport amyloid-ß protein and tau proteins to other cells (DeLeo and Ikezu, 2018). Asai et al. (2015) proved that microglia-derived exosomes contribute to the spreading of tau. In one of the preclinical studies performed on mice having tau aggregation, it was observed that brain-derived exosomes showed the presence of tau in vivo that can be further transferred to neurons ex vivo through these exosomes (Asai et al., 2015). In another AD-related study, injection of exosome biosynthesis inhibitors showed a significant reduction of Aβ plaque loads in the brain tissues (Dinkins et al., 2014). Several preclinical/clinical studies demonstrated that immunization treatment against EVs containing proteins associated with neurodegenerative diseases could attenuate neurodegenerative pathologies (Valera and Masliah, 2013; van Dyck, 2018; Wang et al., 2019).
The role of EVs from different origins was evaluated in neurodegenerative disease and neurological injury models by several authors in their previously published studies (An et al., 2013; Xin et al., 2013; Zhang et al., 2015). In such models, authors endorsed the neuroprotective behavior of EVs as these lower the episodes of neuropathology and along with also contribute to ameliorating behavioral and cognitive motor deficits (Xin et al., 2013; Doeppner et al., 2015; Zhang et al., 2015). Other animal studies also conferred improvement in cognitive motor outcomes along with showing protective anti-inflammatory phenotype on intravenous (IV) infusion with mesenchymal stem cell (MSC)-derived EVs that are mediated through reduced inflammatory cytokine levels and apoptotic markers (Kim et al., 2016; Ni et al., 2019). Another study also reported that repeated IV doses of endothelial cell-derived EVs showed improved cognitive motor function through the reduction of Aβ deposits (Pan et al., 2020). A similar study also showed that intracerebroventricular administration of EVs derived from neural stem cells enhanced the cognitive-motor function in an animal model of Alzheimer’s disease (Li et al., 2020). The author of a similar study observed that improvement in the cognitive-motor function is mediated through SIRT1 activation and increased synaptic activities that also simultaneously showed decreased inflammatory responses (Li et al., 2020).
Evidence from previously published studies offered new opportunities for exploiting EVs as therapeutic and diagnostic tools. This study conducted a systematic review of EVs as diagnostic and therapeutic agents in neurodegenerative diseases.
The current systematic review was designed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) recommendations (Page et al., 2021).
By searching PubMed, Scopus, ISI Web of Science, EMBASE, and Google Scholar for all articles on EV modifications, published articles were chosen (2012 to Feb 2022). Figure 1 depicts the number of PubMed publications published in the recent 10 years (2012–2022).
Searches were conducted using the following keywords: “extracellular vesicles” [Medical Subject Headings (MeSH)] OR “exosomes” [Medical Subject Headings (MeSH)] OR “Neurodegenerative disease” (MeSH) OR “therapeutics” (MeSH) OR “diagnostic biomarker” (MeSH). Figure 2 demonstrates the number of publications for the last 10 years (2012 to 2022) extracted from PubMed that showed the therapeutic and diagnostic role of EVs in neurodegenerative disease.

Figure 2. Number of publications for the last 10 years (2012 to 2022) extracted from PubMed that showed the therapeutic and diagnostic role of extracellular vesicles (EVs) in neurodegenerative disease.
Two independent investigators reviewed the titles, aims, and abstracts of published articles to determine eligibility. Full-length articles were evaluated by the same investigators, and inclusion and exclusion criteria were applied to each article. Furthermore, the same researchers screened the references of the initial eligible articles to identify all eligible articles for inclusion in the final list. We calculated the overall risk biasness and inter-reliability agreement.
The quality of the systematic reviews implicated in the present systematic review was evaluated using the GRADE system (Table 1).

Table 1. Statistical descriptive analysis showing the assessment of intraclass correlation coefficient, inter-item correlation coefficient, Cohen’s weighted Kappa, and Cronbach’s Alpha assessment between the agreements of the rating experts to analyze reliability statistics.
In brief, the GRADE scoring system has four levels of evidence including very low, low, moderate, and high. All eligible studies included in this systematic review were assessed for the following characteristics: imprecision, inconsistency, risk of bias, indirectness, and biasness of publication. Publication bias referred to the application of EVs in the extracted data of reviewed papers and the highlights drawn from the results of such studies because studies without references and publications are not available. The validity of the eligible studies was independently assessed by the two reviewers using a standard checklist. The index of inter-and intra-rater agreement, calculated using the kappa statistic, was used to evaluate the items relevant to the review.
For this study, research papers screened during the literature search met the following inclusion criteria: this study included the following topics: (1) EVs; (2) neurodegenerative diseases; (3) therapeutic and diagnostic biomarkers; (4) exosomes; and (5) a published original article with all full-text literature and properly cited references. The following studies were excluded: (1) insufficient reported data with uncited references; (2) published conference proceedings; (3) published review articles, letters, or text written in a language other than English; or (4) repetition of previously published articles.
The names of the authors, the year of publication, the country of origin, and the mode of EV application (therapeutic or diagnostic biomarker) were extracted. The majority of articles decipher the role of EVs in neurodegenerative diseases, either as a therapeutic/diagnostic biomarker or both.
A total of 1,435 articles were screened, and 1,128 non-duplicate publications were found. Following the screening of titles and abstracts, 214 publications were excluded; following the full-text screening of 93 published articles, another 33 publications were excluded. As shown in the PRISMA flow diagram, the remaining 60 studies were included in this systematic review (Figure 3).
Study characteristics of the 27 eligible studies showed that most authors demonstrated the role of EVs as therapeutic and diagnostic biomarkers in neurodegenerative diseases as shown in Table 2 (Candelario and Steindler, 2014; Jan et al., 2017; Lee and Kim, 2017; Izadpanah et al., 2018; Hill, 2019; Jiang et al., 2019; You and Ikezu, 2019; Yuan et al., 2019; Zhang et al., 2019, 2021; Abdel-Haq, 2020; Kapogiannis, 2020; Mäger et al., 2020; Shaimardanova et al., 2020; Vassileff et al., 2020; Yin et al., 2020; Anakor et al., 2021; Cui et al., 2021; D’Anca et al., 2021; Gagliardi et al., 2021; He et al., 2021; Jin et al., 2021; Manu et al., 2021; Toshihide, 2021; Upadhya and Shetty, 2021; Zhao et al., 2021; Picca et al., 2022). In total, 19 studies observed the pioneering role of EVs and exosomes as diagnostic biomarkers in neurodegenerative diseases (Table 2; Coleman and Hill, 2015; Thompson et al., 2016; Vella et al., 2016; Barreca et al., 2017; Chen et al., 2017; Li et al., 2018; Pluta et al., 2018; Ramirez et al., 2018; Gámez-Valero et al., 2019; Karnati et al., 2019; Lee et al., 2019; Pluta and Ułamek-Kozioł, 2019; Pulliam et al., 2019; Vinaiphat and Sze, 2019; Banack et al., 2020; Guedes et al., 2020; Hornung et al., 2020; Rani et al., 2020; Leggio et al., 2021). Moreover, 14 studies alone demonstrated the therapeutic role of EVs and exosomes in neurodegenerative diseases (Table 2; Kim et al., 2013; Katsuda et al., 2015; Rufino-Ramos et al., 2017; Sarko and McKinney, 2017; Araldi et al., 2020; Dolcetti et al., 2020; Lakshmi et al., 2020; Upadhya et al., 2020; Fayazi et al., 2021; Haney et al., 2021; Kumar et al., 2021; Reed and Escayg, 2021; Xu et al., 2021; Meldolesi, 2022). The overall risk biasness was visualized as demonstrated in Figures 4A,B (McGuinness and Higgins, 2021).
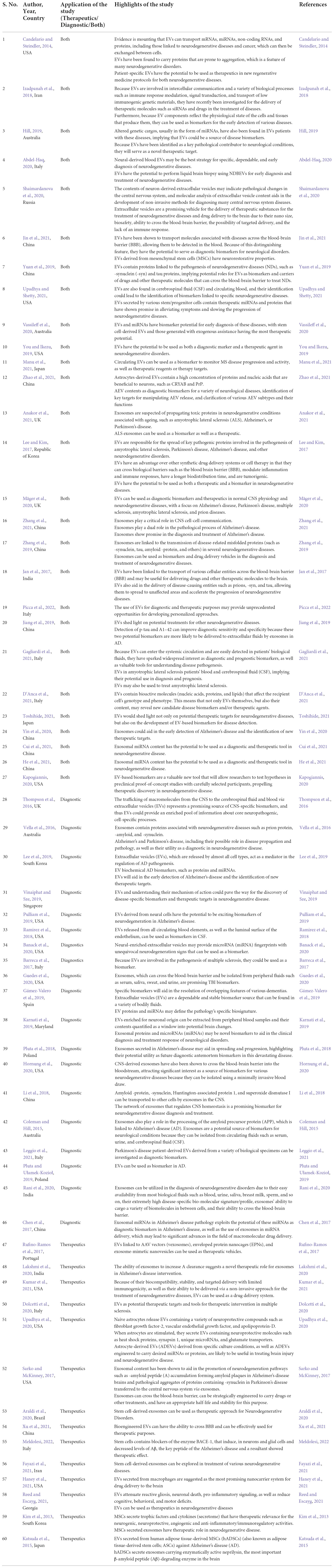
Table 2. Eligible studies included in the systematic review showing the application of extracellular vesicles (EVs) as diagnostic biomarkers and therapeutics or both in neurodegenerative disease.
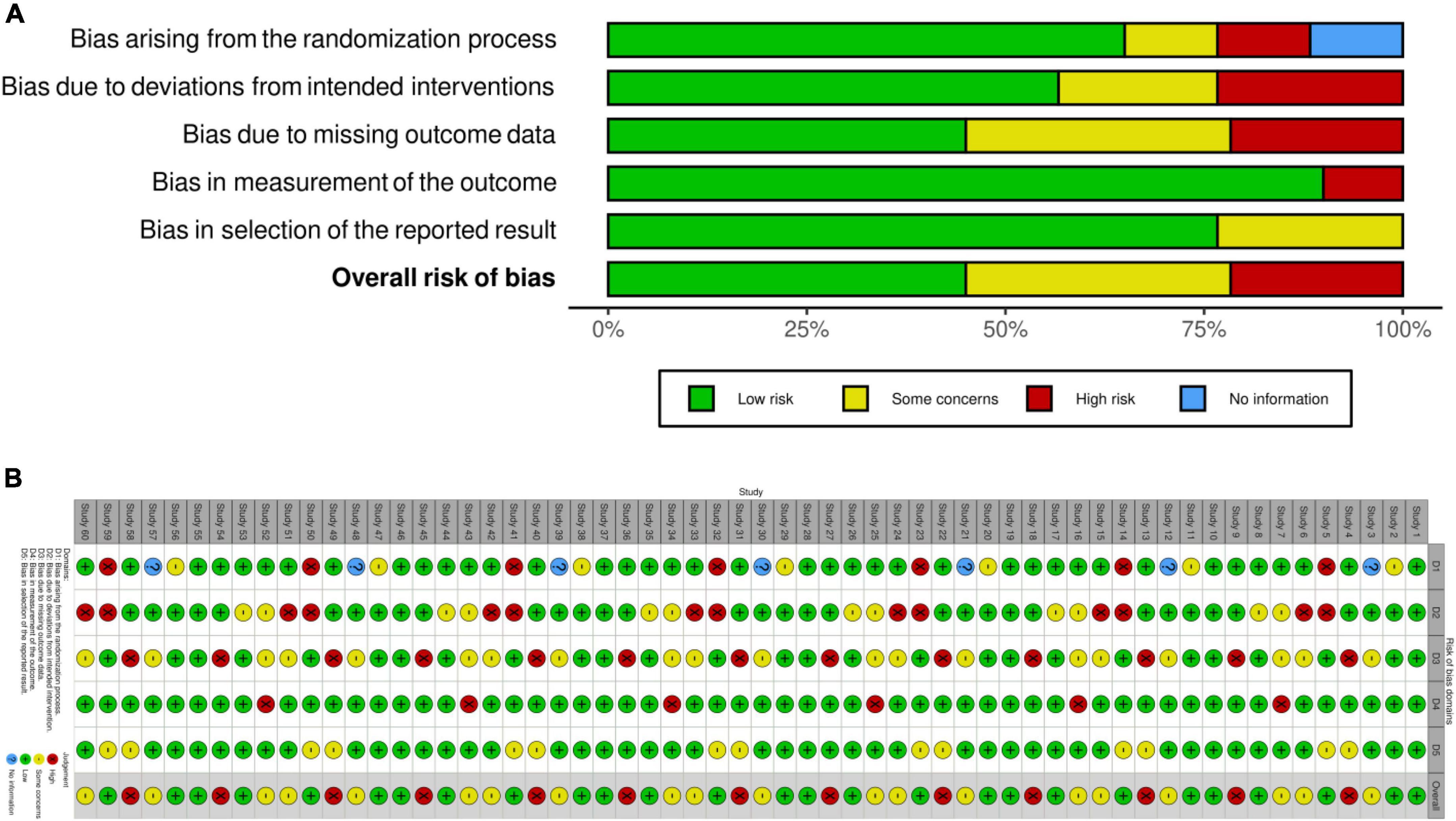
Figure 4. Plot showing risk biasness. (A) Weighted bar plots of the distribution of risk-of-bias judgments within each bias domain; (B) traffic light plots of the domain-level judgments for each individual result.
The systematic review of the published articles was found consistent in validity appraisal among the two raters, as assessed using a kappa statistic of 0.868. Inter-reliability coefficient and intra-reliability coefficient showed strong agreement between the reviewer’s decisions as shown in Table 1. Table 1 also shows that Cronbach’s alpha (α) coefficient measures reliability and internal consistency and demonstrates excellent reliability levels.
In the present systematic review, the role of EVs in neurodegenerative diseases was evaluated. Altogether, the findings suggested that EVs can be used both as diagnostic biomarkers and therapeutics in neurodegenerative diseases. EVs are nano-sized lipid bilayer vesicles sized between 30 and 1,000 nm that are released by several cell types including healthy and diseased cells. These secreted EVs play an important role in intercellular communication mediated through their biological content (protein, nucleic acids, and lipids). Previous ample evidence suggested that EVs are the carrier of mRNAs, miRNAs, long non-coding RNAs, and proteins that are associated with the neurodegenerative changes in the body, which may be exchanged between cells of the target. Bestowing this reason, EVs attract special space for acting both as diagnostic markers and therapeutics in neurodegenerative diseases. The majority of studies observed the role of EVs in both diagnostics and therapeutics (Candelario and Steindler, 2014; Jan et al., 2017; Lee and Kim, 2017; Izadpanah et al., 2018; Hill, 2019; Jiang et al., 2019; You and Ikezu, 2019; Yuan et al., 2019; Zhang et al., 2019, 2021; Abdel-Haq, 2020; Kapogiannis, 2020; Mäger et al., 2020; Shaimardanova et al., 2020; Vassileff et al., 2020; Yin et al., 2020; Anakor et al., 2021; Cui et al., 2021; D’Anca et al., 2021; Gagliardi et al., 2021; He et al., 2021; Jin et al., 2021; Manu et al., 2021; Toshihide, 2021; Upadhya and Shetty, 2021; Zhao et al., 2021; Picca et al., 2022). Notably, 19 studies observed the pioneering role of EVs as a diagnostic biomarker in neurodegenerative diseases (Table 2; Coleman and Hill, 2015; Thompson et al., 2016; Vella et al., 2016; Barreca et al., 2017; Chen et al., 2017; Li et al., 2018; Pluta et al., 2018; Ramirez et al., 2018; Gámez-Valero et al., 2019; Karnati et al., 2019; Lee et al., 2019; Pluta and Ułamek-Kozioł, 2019; Pulliam et al., 2019; Vinaiphat and Sze, 2019; Banack et al., 2020; Guedes et al., 2020; Hornung et al., 2020; Rani et al., 2020; Leggio et al., 2021). Moreover, 14 studies alone demonstrated the therapeutic role of EVs in neurodegenerative diseases (Table 2; Kim et al., 2013; Katsuda et al., 2015; Rufino-Ramos et al., 2017; Sarko and McKinney, 2017; Araldi et al., 2020; Dolcetti et al., 2020; Lakshmi et al., 2020; Upadhya et al., 2020; Fayazi et al., 2021; Haney et al., 2021; Kumar et al., 2021; Reed and Escayg, 2021; Xu et al., 2021; Meldolesi, 2022).
One of the previously published studies performed on cell culture showed the presence of proteins susceptible to aggregation, which was proven a classical hallmark in neurodegenerative diseases (Funk and Kuret, 2012). A diseased or affected cell transport protein to a healthy cell may further lead to its accumulation and aggregation, thereby causing the pathogenesis of neurodegenerative diseases (Funk and Kuret, 2012). Cerebrospinal fluid (CSF) and blood specimens from patients often implicate the screening and identification of biomarkers. Due to some limitations of other interacting factors and non-specificity, these might not be suitable candidates for the diagnosis of neurodegenerative disease as EVs do. Similarly, the low concentration of nucleic acids in such fluids also limits the use of such biomarkers in the screening of neurodegenerative changes.
Nonetheless, EVs are considered to be an ideal reservoir for specific biomarkers of neurodegenerative changes. EVs are released by all cells including the CSF, blood, and urine, which will be a beneficial approach for the detection of the brain and neural cell-related changes. EVs are resistant to enzymatic degradation and thereby provide stability during the processing and isolation of EV biomarkers. Therefore, EVs explore the potential of liquid biopsy for the investigation of neurodegenerative diseases.
A previously published study observed that EVs of neurodegenerative diseases exhibit the presence of pathogenic proteins including α-synuclein (α-syn) and tau proteins, which serve as diagnostic biomarkers and therapeutic targets in such diseases (Yuan et al., 2019). Over the past few decades, it was observed that neuronal cell-derived EVs possess Aβ42, T-tau, and P-T181-tau exploited as diagnostic biomarkers.
Extracellular vesicles possess the ability to cross the blood-brain barrier (BBB) and have the potential to efficiently deliver therapeutic molecules into the cells providing an attractive opportunity for delivering mRNAs, miRNAs, and drugs to show a protective effect in neurodegenerative diseases. A previously published study showed that astrocyte-derived EVs (AEVs) exhibit neuroprotection in ischemic stroke conditions (Zhao et al., 2021). AEVs showed neuroprotection in ischemic stroke conditions by controlling autophagy, the release of miR-92b-3p, assuaging oxygen-glucose deprivation-induced neuron apoptosis, and inhibiting the expression of TNFα, IL-6, and IL-1β that will further lead to the reduction of infarct volumes (Zhao et al., 2021). Exploring the new area of EV biology seems crucial for scientific and break-throwing discoveries in a variety of diseases including neurodegenerative diseases. EVs from every cellular origin should be exploited for diagnostic and therapeutic in neurodegenerative diseases.
Extracellular vesicles are known to play a dual role in diagnostics as well as therapeutics in neurodegenerative diseases. In one of the previously published studies, it was demonstrated that intraperitoneal injection of EVs derived from umbilical cord MSCs showed improved cognitive outcomes through the decrease in neurological severity scores and improved reflex and sensation mediated by an HDAC1-Dependent EGR2/Bcl2 Axis (Han et al., 2021). Similarly in the rodent model, treatment with EVs showed a decrease in 180° rotation time compared to untreated animals in behavioral negative geotaxis tests (Sisa et al., 2019). Xin and his coworkers demonstrated that EVs derived from MSCs attenuate hindlimb impairment along with improvement in perception and visual impairment by modulating microglia/macrophage polarization and targeting the delivery of miR-21a-5p (Xin et al., 2020).
Extracellular vesicles exhibit promising therapeutic and diagnostic uses in biomaterials. These tailored nano-vesicles can be loaded with desired biomolecules, such as proteins, lipids, nucleic acids, and drugs, using different modification approaches to obtain functionalized EVs. These functionalized EVs can be exploited in the treatment of various diseases, including neurodegenerative diseases. In the recent decade, there has been an increasing trend of research into exosomes, which has expanded into neurodegenerative diseases. The body of evidence demonstrates that exosomes play an important part in communication in the brain. On understanding the physical nature of exosomes, it may be possible to manipulate their contents to deliver therapeutic factors to delay the onset of neurodegeneration. Bringing the field of immunology, neurology, and oncology along with infectious diseases could help in exploiting all the aspects of EVs for giving an understanding pathogenesis and management of human diseases. Combining immunology, neurology, oncology, and infectious diseases could aid in the exploitation of all aspects of EVs for understanding the pathogenesis and management of human diseases.
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
AR, G-BJ, MS, RG, and SA: conceptualization. AR and G-BJ: methodology. AR: software, investigation, and writing—original draft preparation. G-BJ, KG, SA, MS, RG, and SK: validation. G-BJ, SA, MS, RG, and SK: formal analysis. SK: resources and project administration. AR and KG: data curation. KG, RG, SA, MS, and G-BJ: writing—review and editing. SA, MS, RG, and SK: visualization. SA, MS, RG, G-BJ, and SK: supervision. All authors contributed to the article and approved the submitted version.
We would like to thank the Multidisciplinary Research Unit, Department of Health Research, Ministry of Health and Family Welfare, New Delhi for providing financial assistance in the form of salary to AR.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
SF, synovial fluid; BAL, bronchoalveolar lavage; AF, amniotic fluid; PE, pleural effusions; EVs, extracellular vesicles; CNS, central nervous system; ILVs, intraluminal vesicles; MVBs, multivesicular bodies; ESCRT, endosomal sorting complex required for transport; AD, Alzheimer’s disease; PRISMA, preferred reporting items for systematic reviews and meta-analysis; CSF, cerebrospinal fluid; BBB, blood brain barrier; AEVs, astrocyte EVs.
Abdel-Haq, H. (2020). The potential of liquid biopsy of the brain using blood extracellular vesicles: The first step toward effective neuroprotection against neurodegenerative diseases. Mol. Diagn. Ther. 24, 703–713. doi: 10.1007/s40291-020-00493-4
An, K., Klyubin, I., Kim, Y., Jung, J. H., Mably, A. J., O’Dowd, S. T., et al. (2013). Exosomes neutralize synaptic-plasticity-disrupting activity of Aβ assemblies in vivo. Mol. Brain 6:47. doi: 10.1186/1756-6606-6-47
Anakor, E., Le Gall, L., Dumonceaux, J., Duddy, W. J., and Duguez, S. (2021). Exosomes in ageing and motor neurone disease: Biogenesis, uptake mechanisms, modifications in disease and uses in the development of biomarkers and therapeutics. Cells 10:2930. doi: 10.3390/cells10112930
Araldi, R. P., D’Amelio, F., Vigerelli, H., de Melo, T. C., and Kerkis, I. (2020). Stem cell-derived exosomes as therapeutic approach for neurodegenerative disorders: From biology to biotechnology. Cells 9:2663. doi: 10.3390/cells9122663
Asai, H., Ikezu, S., Tsunoda, S., Medalla, M., Luebke, J., Haydar, T., et al. (2015). Depletion of microglia and inhibition of exosome synthesis halt tau propagation. Nat. Neurosci. 18, 1584–1593. doi: 10.1038/nn.4132
Banack, S. A., Dunlop, R. A., and Cox, P. A. (2020). An miRNA fingerprint using neural-enriched extracellular vesicles from blood plasma: Towards a biomarker for amyotrophic lateral sclerosis/motor neuron disease. Open Biol. 10:200116. doi: 10.1098/rsob.200116
Barreca, M. M., Aliotta, E., and Geraci, F. (2017). Extracellular vesicles in multiple sclerosis as possible biomarkers: Dream or reality? Adv. Exp. Med. Biol. 958, 1–9.
Candelario, K. M., and Steindler, D. A. (2014). The role of extracellular vesicles in the progression of neurodegenerative disease and cancer. Trends Mol. Med. 20, 368–374.
Chen, J. J., Zhao, B., Zhao, J., and Li, S. (2017). Potential roles of exosomal microRNAs as diagnostic biomarkers and therapeutic application in Alzheimer’s disease. Neural Plast. 2017:7027380.
Coleman, B. M., and Hill, A. F. (2015). Extracellular vesicles – their role in the packaging and spread of misfolded proteins associated with neurodegenerative diseases. Semin. Cell Dev. Biol. 40, 89–96.
Cui, G. H., Zhu, J., Wang, Y. C., Wu, J., Liu, J. R., and Guo, H. D. (2021). Effects of exosomal miRNAs in the diagnosis and treatment of Alzheimer’s disease. Mech. Aging Dev. 200:111593.
D’Anca, M., Fenoglio, C., Buccellato, F. R., Visconte, C., Galimberti, D., and Scarpini, E. (2021). Extracellular vesicles in multiple sclerosis: Role in the pathogenesis and potential usefulness as biomarkers and therapeutic tools. Cells 10:1733. doi: 10.3390/cells10071733
DeLeo, A. M., and Ikezu, T. (2018). Extracellular vesicle biology in Alzheimer’s disease and related tauopathy. J. Neuroimmune Pharmacol. 13, 292–308.
Dinkins, M. B., Dasgupta, S., Wang, G., Zhu, G., and Bieberich, E. (2014). Exosome reduction in vivo isassociated with lower amyloid plaque load in the 5XFAD mouse model of Alzheimer’s disease. Neurobiol. Aging 35, 1792–1800. doi: 10.1016/j.neurobiolaging.2014.02.012
Doeppner, T. R., Herz, J., Görgens, A., Schlechter, J., Ludwig, A. K., Radtke, S., et al. (2015). Extracellular vesicles improve post-stroke neuroregeneration and prevent postischemic immunosuppression. Stem Cells Transl. Med. 4, 1131–1143. doi: 10.5966/sctm.2015-0078
Dolcetti, E., Bruno, A., Guadalupi, L., Rizzo, F. R., Musella, A., Gentile, A., et al. (2020). Emerging role of extracellular vesicles in the pathophysiology of multiple sclerosis. Int. J. Mol. Sci. 21:7336.
Doyle, L. M., and Wang, M. Z. (2019). Overview of extracellular vesicles. Their origin, composition, purpose, and methods for exosome isolation and analysis. Cells 8:727.
Fayazi, N., Sheykhhasan, M., Soleimani Asl, S., and Najafi, R. (2021). Stem cell-derived exosomes: A new strategy of neurodegenerative disease treatment. Mol. Neurobiol. 58, 3494–3514.
Funk, K. E., and Kuret, J. (2012). Lysosomal fusion dysfunction as aunifying hypothesis for Alzheimer’s disease pathology. Int. J. Alzheimers Dis. 2012:752894. doi: 10.1155/2012/752894
Gagliardi, D., Bresolin, N., Comi, G. P., and Corti, S. (2021). Extracellular vesicles and amyotrophic lateral sclerosis: From misfolded protein vehicles to promising clinical biomarkers. Cell. Mol. Life Sci. 78, 561–572. doi: 10.1007/s00018-020-03619-3
Gámez-Valero, A., Beyer, K., and Borràs, F. E. (2019). Extracellular vesicles, new actorsin the search for biomarkers for dementias. Neurobiol. Aging 74, 15–20. doi: 10.1016/j.neurobiolaging.2018.10.006
Guedes, V. A., Devoto, C., Leete, J., Sass, D., Acott, J. D., Mithani, S., et al. (2020). Extracellular vesicle proteins and MicroRNAs as biomarkers for traumatic brain injury. Front. Neurol. 11:663. doi: 10.3389/fneur.2020.00663
Han, J., Yang, S., Hao, X., Zhang, B., Zhang, H., Xin, C., et al. (2021). Extracellular vesicle-derived microRNA-410 from mesenchymal stem cells protects against neonatal hypoxia-ischemia brain damage through an HDAC1-dependent EGR2/Bcl2 axis. Front. Cell Dev. Biol. 8:579236. doi: 10.3389/fcell.2020.579236
Haney, M. J., Zhao, Y., Fallon, J. K., Yue, W., Li, S. M., Lentz, E. E., et al. (2021). Extracellular vesicles as drug delivery system for the treatment of neurodegenerative disorders: Optimization of the cell source. Adv. Nanobiomed Res. 1:2100064. doi: 10.1002/anbr.202100064
He, M., Zhang, H. N., Tang, Z. C., and Gao, S. G. (2021). Diagnostic and therapeutic potential of exosomal MicroRNAs for neurodegenerative diseases. Neural Plast. 2021:8884642.
Hill, A. F. (2019). Extracellular vesicles and neurodegenerative diseases. J. Neurosci. 39, 9269–9273.
Hornung, S., Dutta, S., and Bitan, G. (2020). CNS-derived blood exosomes as a promising source of biomarkers: Opportunities and challenges. Front. Mol. Neurosci. 13:38. doi: 10.3389/fnmol.2020.00038
Izadpanah, M., Seddigh, A., Ebrahimi Barough, S., Fazeli, S. A. S., Ai, J., et al. (2018). Potential of extracellular vesicles in neurodegenerative diseases: Diagnostic and therapeutic indications. J. Mol. Neurosci. 66, 172–179. doi: 10.1007/s12031-018-1135-x
Jan, A. T., Malik, M. A., Rahman, S., Yeo, H. R., Lee, E. J., Abdullah, T. S., et al. (2017). Perspective insights of exosomes in neurodegenerative diseases: A critical appraisal. Front. Aging Neurosci. 9:317. doi: 10.3389/fnagi.2017.00317
Jiang, L., Dong, H., Cao, H., Ji, X., Luan, S., and Liu, J. (2019). Exosomes in pathogenesis, diagnosis, and treatment of Alzheimer’s disease. Med. Sci. Monit. 25, 3329–3335.
Jin, Q., Wu, P., Zhou, X., Qian, H., and Xu, W. (2021). Extracellular vesicles: Novel roles in neurological disorders. Stem Cells Int. 2021:6640836.
Kapogiannis, D. (2020). Exosome biomarkers revolutionize preclinical diagnosis of neurodegenerative diseases and assessment of treatment responses in clinical trials. Adv. Exp. Med. Biol. 1195:149. doi: 10.1007/978-3-030-32633-3_19
Karnati, H. K., Garcia, J. H., Tweedie, D., Becker, R. E., Kapogiannis, D., Greig, N. H., et al. (2019). Neuronal enriched extracellular vesicle proteins as biomarkers for traumatic brain injury. J. Neurotrauma 36, 975–987.
Katsuda, T., Oki, K., and Ochiya, T. (2015). Potential application of extracellular vesicles of human adipose tissue-derived mesenchymal stem cells in Alzheimer’s disease therapeutics. Methods Mol. Biol. 1212, 171–181.
Kim, D. K., Nishida, H., An, S. Y., Shetty, A. K., Bartosh, T. J., and Prockop, D. J. (2016). Chromatographically isolated CD63+CD81+ extracellular vesicles from mesenchymal stromal cells rescue cognitive impairments after TBI. Proc. Natl. Acad. Sci. U.S.A. 113, 170–175. doi: 10.1073/pnas.1522297113
Kim, H. O., Choi, S. M., and Kim, H. S. (2013). Mesenchymal stem cell-derived secretome and microvesicles as a cell-free therapeutics for neurodegenerative disorders. Tissue Eng. Regen. Med. 10, 93–101. doi: 10.3390/ijms21155241
Kumar, A., Zhou, L., Zhi, K., Raji, B., Pernell, S., Tadrous, E., et al. (2021). Challenges in biomaterial-based drug delivery approach for the treatment of neurodegenerative diseases: Opportunities for extracellular vesicles. Int. J. Mol. Sci. 22:138. doi: 10.3390/ijms22010138
Lakshmi, S., Essa, M. M., Hartman, R. E., Guillemin, G. J., Sivan, S., Elumalai, P., et al. (2020). Exosomes in Alzheimer’s disease: Potential role as pathological mediators, biomarkers and therapeutic targets. Neurochem. Res. 45, 2553–2559.
Lee, J. Y., and Kim, H. S. (2017). Extracellular vesicles in neurodegenerative diseases: A double-edged sword. Tissue Eng. Regen. Med. 14, 667–678.
Lee, S., Mankhong, S., and Kang, J. H. (2019). Extracellular vesicle as a source of Alzheimer’s biomarkers: Opportunities and challenges. Int. J. Mol. Sci. 20:1728.
Leggio, L., Paternò, G., Vivarelli, S., Falzone, G. G., Giachino, C., Marchetti, B., et al. (2021). Extracellular vesicles as novel diagnostic and prognostic biomarkers for Parkinson’s disease. Aging Dis. 12, 1494–1515. doi: 10.14336/AD.2021.0527
Li, B., Liu, J., Gu, G., Han, X., Zhang, Q., and Zhang, W. (2020). Impact of neural stem cell-derived extracellular vesicles on mitochondrial dysfunction, sirtuin 1 level, and synaptic deficits in Alzheimer’s disease. J. Neurochem. 154, 502–518. doi: 10.1111/jnc.15001
Li, D., Li, Y. P., Li, Y. X., Zhu, X. H., Du, X. G., Zhou, M., et al. (2018). Effect of regulatory network of exosomes and microRNAs on neurodegenerative diseases. Chin. Med. J. (Engl). 131, 2216–2225.
Lötvall, J., Hill, A. F., Hochberg, F., Buzás, E. I., Di, Vizio D, Gardiner, C., et al. (2014). Minimal experimental requirements for definition of extracellular vesicles and their functions: A position statement from the international society for extracellular vesicles. J. Extracell. Vesicles 3:26913. doi: 10.3402/jev.v3.26913
Mä,ger, I., Willms, E., Bonner, S., Hill, A. F., and Wood, M. J. A. (2020). Exosomes: Extracellular vesicles in neurodegenerative disorders. Exosomes 285–305.
Manu, M. S., Hohjoh, H., and Yamamura, T. (2021). Extracellular vesicles as pro- and anti-inflammatory mediators, biomarkers and potential therapeutic agents in multiple sclerosis. Aging Dis. 12, 1451–1461. doi: 10.14336/AD.2021.0513
McGuinness, L. A., and Higgins, J. P. T. (2021). Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Syn. Meth. 12, 55–61. doi: 10.1002/jrsm.1411
Meldolesi, J. (2022). News about therapies of Alzheimer’s disease: Extracellular vesicles from stem cells exhibit advantages compared to other treatments. Biomedicines 10:105. doi: 10.3390/biomedicines10010105
Ni, H., Yang, S., Siaw-Debrah, F., Hu, J., Wu, K., He, Z., et al. (2019). Exosomes derived from bone mesenchymal stem cells ameliorate early inflammatory responses following traumatic brain injury. Front. Neurosci. 13:14. doi: 10.3389/fnins.2019.00014
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 372:n71. doi: 10.1136/bmj.n71
Pan, J., He, R., Huo, Q., Shi, Y., and Zhao, L. (2020). Brain microvascular endothelial cell derived exosomes potently ameliorate cognitive dysfunction by enhancing the clearance of Aβ through Up-regulation of P-gp in mouse model of AD. Neurochem. Res. 45, 2161–2172. doi: 10.1007/s11064-020-03076-1
Picca, A., Guerra, F., Calvani, R., Coelho-Junior, H. J., Bucci, C., and Marzetti, E. (2022). Circulating extracellular vesicles: Friends and foes in neurodegeneration. Neural Regen. Res. 17, 534–542.
Pluta, R., and Ułamek-Kozioł, M. (2019). Lymphocytes, platelets, erythrocytes, and exosomes as possible biomarkers for Alzheimer’s disease clinical diagnosis. Adv. Exp. Med. Biol. 1118, 71–82. doi: 10.1007/978-3-030-05542-4_4
Pluta, R., Ułamek-Kozioł, M., Januszewski, S., and Czuczwar, S. J. (2018). Exosomes as possible spread factor and potential biomarkers in Alzheimer’s disease: Current concepts. Biomark. Med. 12, 1025–1033.
Pulliam, L., Sun, B., Mustapic, M., Chawla, S., and Kapogiannis, D. (2019). Plasma neuronal exosomes serve as biomarkers of cognitive impairment in HIV infection and Alzheimer’s disease. J. Neurovirol. 25, 702–709. doi: 10.1007/s13365-018-0695-4
Raghav, A., and Jeong, G. B. (2021). A systematic review on the modifications of extracellular vesicles: A revolutionized tool of nano-biotechnology. J. Nanobiotechnol. 19:459. doi: 10.1186/s12951-021-01219-2
Raghav, A., Tripathi, P., Mishra, B. K., Jeong, G. B., Banday, S., Gautam, K. A., et al. (2021b). Mesenchymal Stromal cell-derived tailored exosomes treat bacteria-associated diabetes foot ulcers: A customized approach from bench to bed. Front. Microbiol. 12:712588. doi: 10.3389/fmicb.2021.712588
Raghav, A., Khan, Z. A., Upadhayay, V. K., Tripathi, P., Gautam, K. A., Mishra, B. K., et al. (2021a). Mesenchymal stem cell-derived exosomes exhibit promising potential for treating SARS-CoV-2-infected patients. Cells 10:587. doi: 10.3390/cells10030587
Ramirez, S. H., Andrews, A. M., Paul, D., and Pachter, J. S. (2018). Extracellular vesicles: Mediators and biomarkers of pathology along CNS barriers. Fluids Barriers CNS 15, 19–27. doi: 10.1186/s12987-018-0104-7
Rani, P., Karthik, S., and Srisharnitha, A. S. (2020). Molecular signatures in exosomes as diagnostic markers for neurodegenerative disorders. Ann. Alzheimers Dement. Care 4, 012–017.
Redzic, J. S., Ung, T. H., and Graner, M. W. (2014). Glioblastoma extracellular vesicles: Reservoirs of potential biomarkers. Pharmgenomics Pers. Med. 7, 65–77.
Reed, S. L., and Escayg, A. (2021). Extracellular vesicles in the treatment of neurological disorders. Neurobiol. Dis. 157:105445.
Rufino-Ramos, D., Albuquerque, P. R., Carmona, V., Perfeito, R., and Nobre, R. J. (2017). Pereira de Almeida L. Extracellular vesicles: Novel promising delivery systems for therapy of brain diseases. J. Control Release 262, 247–258. doi: 10.1016/j.jconrel.2017.07.001
Sarko, D. K., and McKinney, C. E. (2017). Exosomes: Origins and therapeutic potential for neurodegenerative disease. Front. Neurosci. 11:82. doi: 10.3389/fnins.2017.00082
Shaimardanova, A. A., Solovyeva, V. V., Chulpanova, D. S., James, V., Kitaeva, K. V., and Rizvanov, A. A. (2020). Extracellular vesicles in the diagnosis and treatment of central nervous system diseases. Neural Regen. Res. 15, 586–596.
Sisa, C., Kholia, S., Naylor, J., Herrera Sanchez, M. B., Bruno, S., Deregibus, M. C., et al. (2019). Mesenchymal stromal cell derived extracellular vesicles reduce hypoxia-ischaemia induced perinatal brain injury. Front. Physiol. 10:282. doi: 10.3389/fphys.2019.00282
Théry, C., Witwer, K. W., Aikawa, E., Alcaraz, M. J., Anderson, J. D., Andriantsitohaina, R., et al. (2018). Minimal information for studies of extracellular vesicles 2018 (MISEV2018): A position statement of the international society for extracellular vesicles and update of the MISEV2014 guidelines. J. Extracell. Vesicles 7:1535750. doi: 10.1080/20013078.2018.1535750
Thompson, A. G., Gray, E., Heman-Ackah, S. M., Mäger, I., Talbot, K., Andaloussi, S. E., et al. (2016). Extracellular vesicles in neurodegenerative disease — pathogenesis to biomarkers. Nat. Rev. Neurol. 12, 346–357.
Toshihide, T. (2021). Pathogenic and protective roles of extracellular vesicles in neurodegenerative diseases. J. Biochem. 169, 181–186.
Upadhya, R., and Shetty, A. K. (2021). Extracellular vesicles for the diagnosis and treatment of Parkinson’s disease. Aging Dis. 12, 1438–1450.
Upadhya, R., Zingg, W., Shetty, S., and Shetty, A. K. (2020). Astrocyte-derived extracellular vesicles: Neuroreparative properties and role in the pathogenesis of neurodegenerative disorders. J. Control Release 323, 225–239. doi: 10.1016/j.jconrel.2020.04.017
Valera, E., and Masliah, E. (2013). Immunotherapy for neurodegenerative diseases: Focus on alphasynucleinopathies. Pharmacol. Ther. 138, 311–322.
van Dyck, C. H. (2018). Anti-amyloid-beta monoclonal antibodies for Alzheimer’s disease:Pitfalls and promise. Biol. Psychiatry 83, 311–319. doi: 10.1016/j.biopsych.2017.08.010
Vassileff, N., Cheng, L., and Hill, A. F. (2020). Extracellular vesicles - propagators of neuropathology and sources of potential biomarkers and therapeutics for neurodegenerative diseases. J. Cell Sci. 133:jcs243139. doi: 10.1242/jcs.243139
Vella, L. J., Hill, A. F., and Cheng, L. (2016). Focus on extracellular vesicles: Exosomes and their role in protein trafficking and biomarker potential in Alzheimer’s and Parkinson’s disease. Int. J. Mol. Sci. 17:173. doi: 10.3390/ijms17020173
Vinaiphat, A., and Sze, S. K. (2019). Clinical implications of extracellular vesicles in neurodegenerative diseases. Expert Rev. Mol. Diagn. 19, 813–824.
Wang, Z., Gao, G., Duan, C., and Yang, H. (2019). Progress of immunotherapy of anti-alphasynucleinin Parkinson’s disease. Biomed. Pharmacother. 115:108843.
Xin, D., Li, T., Chu, X., Ke, H., Yu, Z., Cao, L., et al. (2020). Mesenchymal stromal cell-derived extracellular vesicles modulate microglia/macrophage polarization and protect the brain against hypoxia-ischemic injury in neonatal mice by targeting delivery of miR-21a-5p. Acta Biomater. 113, 597–613. doi: 10.1016/j.actbio.2020.06.037
Xin, H., Li, Y., Cui, Y., Yang, J. J., Zhang, Z. G., and Chopp, M. (2013). Systemic administration of exosomes released from mesenchymal stromal cells promote functional recovery and neurovascular plasticity after stroke in rats. J. Cereb. Blood Flow Metab. 33, 1711–1715. doi: 10.1038/jcbfm.2013.152
Xu, M., Feng, T., Liu, B., Qiu, F., Xu, Y., Zhao, Y., et al. (2021). Engineered exosomes: Desirable target-tracking characteristics for cerebrovascular and neurodegenerative disease therapies. Theranostics 11, 8926–8944. doi: 10.7150/thno.62330
Yin, Q., Ji, X., Lv, R., Pei, J. J., Du, Y., Shen, C., et al. (2020). Targetting exosomes as a new biomarker and therapeutic approach for Alzheimer’s disease. Clin. Interv. Aging 15, 195–205.
You, Y., and Ikezu, T. (2019). Emerging roles of extracellular vesicles in neurodegenerative disorders. Neurobiol. Dis. 130:104512.
Yuan, Q., Li, X. D., Zhang, S. M., Wang, H. W., and Wang, Y. L. (2019). Extracellular vesicles in neurodegenerative diseases: Insights and new perspectives. Genes Dis. 8, 124–132. doi: 10.1016/j.gendis.2019.12.001
Zhang, L. L., Liu, M. X., Xie, J. X., and Song, N. (2019). Exosomes and their roles in neurodegenerative diseases: From pathogenic, diagnostic and therapeutical perspectives. Sheng Li Xue Bao 71, 439–453.
Zhang, T., Ma, S., Lv, J., Wang, X., Afewerky, H. K., Li, H., et al. (2021). The emerging role of exosomes in Alzheimer’s disease. Aging Res. Rev. 68:101321.
Zhang, Y., Chopp, M., Meng, Y., Katakowski, M., Xin, H., Mahmood, A., et al. (2015). Effect of exosomes derived from multipluripotent mesenchymal stromal cells on functional recovery and neurovascular plasticity in rats after traumatic brain injury. J. Neurosurg. 122, 856–867. doi: 10.3171/2014.11.JNS14770
Keywords: extracellular vesicles, neurodegenerative disease, therapeutics, biomarker, neurological disease
Citation: Raghav A, Singh M, Jeong G-B, Giri R, Agarwal S, Kala S and Gautam KA (2022) Extracellular vesicles in neurodegenerative diseases: A systematic review. Front. Mol. Neurosci. 15:1061076. doi: 10.3389/fnmol.2022.1061076
Received: 04 October 2022; Accepted: 02 November 2022;
Published: 24 November 2022.
Edited by:
Dhiraj Kumar, Jamia Millia Islamia, IndiaReviewed by:
Fohad Mabood Husain, King Saud University, Saudi ArabiaCopyright © 2022 Raghav, Singh, Jeong, Giri, Agarwal, Kala and Gautam. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Goo-Bo Jeong, Z2JqZW9uZ0BnYWNob24uYWMua3I=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.