- 1Department of Ophthalmology, Peking University Third Hospital, Beijing, China
- 2Beijing Key Laboratory of Restoration of Damaged Ocular Nerve, Beijing, China
A corrigendum on
The impact of patient-reported visual disturbance on dynamic visual acuity in myopic patients after corneal refractive surgery
by Wang, Y., Zhang, Y., Wu, T., Ren, X., Yuan, Y., Li, X., and Chen, Y. (2023). Front. Neurosci. 17:1278626. doi: 10.3389/fnins.2023.1278626
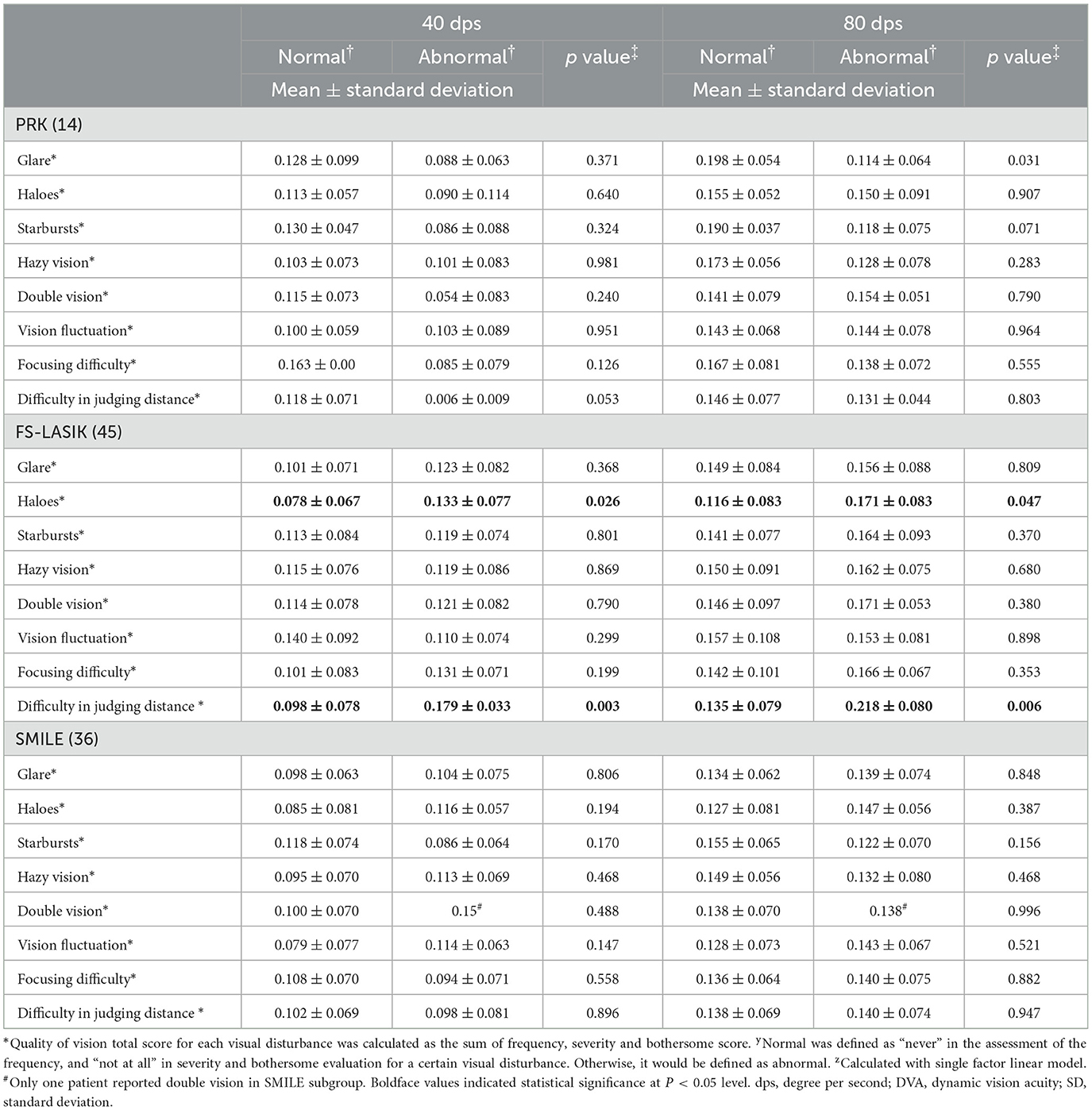
In the published article, there was an error in Table 4 as published. The scientific surgical name should be “photorefractive keratectomy (PRK)” instead of “laser-assisted subepithelial keratectomy (LASEK).” The corrected Table 4 appears below.
In the published article, there was also an error in the text. The scientific surgical name should be “photorefractive keratectomy (PRK)” instead of “laser-assisted subepithelial keratectomy (LASEK)”.
A correction has been made to Abstract, Method, This paragraph previously stated:
“This is a prospective nonrandomized study. Adult myopic patients receiving bilateral laser-assisted sub-epithelial keratomileusis (LASEK), femtosecond laser-assisted in situ keratomileusis (FS-LASIK), or small incision lenticule extraction (SMILE) with Plano target were included. Eight types of patient-reported visual disturbance were evaluated regarding frequency, severity and bothersome and dynamic visual acuity (DVA) of 40 and 80 degrees per second (dps) was measured postoperatively at 3 months.”
The corrected paragraph appears below:
“This is a prospective nonrandomized study. Adult myopic patients receiving bilateral photorefractive keratectomy (PRK), femtosecond laser-assisted in situ keratomileusis (FS-LASIK), or small incision lenticule extraction (SMILE) with Plano target were included. Eight types of patient-reported visual disturbance were evaluated regarding frequency, severity and bothersome and dynamic visual acuity (DVA) of 40 and 80 degrees per second (dps) was measured postoperatively at 3 months.”
A correction has been made to Materials and methods, Participants, Paragraph 2. This sentence previously stated:
“Consecutive patients undergoing bilateral laser-assisted sub-epithelial keratomileusis (LASEK), femtosecond laser-assisted in situ keratomileusis (FS-LASIK) or small incision lenticule extraction (SMILE) were prospectively enrolled. The inclusion criteria were as follow: (Lou et al., 2016) age 18–40 years of age (Kim et al., 2019), correction of myopia or myopic astigmatism for Plano target; (Wen et al., 2017) pre-operative and three-month postoperative corrected distance visual acuity (CDVA) 0 (LogMAR) or better. The exclusion criteria were: (Lou et al., 2016) history of severe ocular diseases, including glaucoma, retinal disease, or severe ocular surface disease; (Kim et al., 2019) vestibular dysfunction or cognitive disorder that affects the DVA test.”
The corrected paragraph appears below:
“Consecutive patients undergoing bilateral photorefractive keratectomy (PRK), femtosecond laser-assisted in situ keratomileusis (FS-LASIK) or small incision lenticule extraction (SMILE) were prospectively enrolled. The inclusion criteria were as follow: (Lou et al., 2016) age 18–40 years of age (Kim et al., 2019), correction of myopia or myopic astigmatism for Plano target; (Wen et al., 2017) pre-operative and three-month postoperative corrected distance visual acuity (CDVA) 0 (LogMAR) or better. The exclusion criteria were: (Lou et al., 2016) history of severe ocular diseases, including glaucoma, retinal disease, or severe ocular surface disease; (Kim et al., 2019) vestibular dysfunction or cognitive disorder that affects the DVA test.”
A correction has been made to Materials and methods, Surgical procedures, Paragraph 2. This paragraph previously stated:
“LASEK: The epithelial was removed after soaking in 20% ethanol for 20 s. The ablation was conducted with a Custom Q profile by WaveLight EX500 excimer laser (Alcon Laboratories Inc., Fort Worth, United States). After ablation, a 0.02% mitomycin C pad was covered on the residual stroma. Then the stroma was rinsed with normal saline. A bandage contact lens (Acuvue, Johnson Vision Care. Inc., United States) was placed on the cornea for protection.”
The corrected paragraph appears below:
“PRK: The epithelial was removed after soaking in 20% ethanol for 20 s. The ablation was conducted with a Custom Q profile by WaveLight EX500 excimer laser (Alcon Laboratories Inc., Fort Worth, United States). After ablation, a 0.02% mitomycin C pad was covered on the residual stroma. Then the stroma was rinsed with normal saline. A bandage contact lens (Acuvue, Johnson Vision Care. Inc., United States) was placed on the cornea for protection.”
4. A correction has been made to Results, Paragraph 1. This paragraph previously stated:
“Ninety-five patients were included in the study. The characteristic of the patients are summarized in Table 1. The average age of the included patients was 27.6 ± 6.4 years. Preoperatively, the mean spherical equivalent (SE) was −5.33 ± 1.70 D. The number of eyes enrolled undergone LASEK, FS-LASIK, and SMILE was 28, 88 and 74, respectively. The preoperative characteristics of participants for different surgical procedures are summarized in Supplementary Table 1.”
The corrected paragraph appears below:
“Ninety-five patients were included in the study. The characteristic of the patients are summarized in Table 1. The average age of the included patients was 27.6 ± 6.4 years. Preoperatively, the mean spherical equivalent (SE) was −5.33 ± 1.70 D. The number of eyes enrolled undergone PRK, FS-LASIK, and SMILE was 28, 88 and 74, respectively. The preoperative characteristics of participants for different surgical procedures are summarized in Supplementary Table 1.”
5. A correction has been made to Results, DVA subgroup analysis by surgical procedure, Paragraph 1. This paragraph previously stated:
“The patients were stratified according to the surgical procedure. The postoperative DVA in normal and abnormal patients of each visual disturbance in three surgical subgroups was summarized in Table 4. There was no significant difference in 40 or 80 dps DVA between patients with and without visual distance in LASEK or SMILE subgroup. For patients who had undergone FS-LASIK, significantly worse postoperative DVA at 40 (0.133 ± 0.077) and 80 dps (0.171 ± 0.083) was observed in patients with haloes than those without haloes (40 dps, 0.078 ± 0.067, p = 0.026; 80 dps, 0.116 ± 0.083, p = 0.047). Additionally, the FS-LASIK patients without difficulty in judging distance had significantly better DVA at 40 (0.098 ± 0.078) and 80 dps (0.135 ± 0.079) than those with abnormal symptoms (40 dps, 0.179 ± 0.033, p = 0.003; 80 dps, 0.218 ± 0.080, p = 0.006).”
The corrected paragraph appears below:
“The patients were stratified according to the surgical procedure. The postoperative DVA in normal and abnormal patients of each visual disturbance in three surgical subgroups was summarized in Table 4. There was no significant difference in 40 or 80 dps DVA between patients with and without visual distance in PRK or SMILE subgroup. For patients who had undergone FS-LASIK, significantly worse postoperative DVA at 40 (0.133 ± 0.077) and 80 dps (0.171 ± 0.083) was observed in patients with haloes than those without haloes (40 dps, 0.078 ± 0.067, p = 0.026; 80 dps, 0.116 ± 0.083, p = 0.047). Additionally, the FS-LASIK patients without difficulty in judging distance had significantly better DVA at 40 (0.098 ± 0.078) and 80 dps (0.135 ± 0.079) than those with abnormal symptoms (40 dps, 0.179 ± 0.033, p = 0.003; 80 dps, 0.218 ± 0.080, p = 0.006).”
A correction has been made to Discussion, Paragraph 6. This paragraph previously stated:
“Certain limitations exist in the present research. First, the present study is a nonrandomized cohort research. Due to nonrandomized design, the number of patients receiving different types of procedures is unbalanced. More patients who had undergone FS-LASIK were enrolled than those with LASEK and SMILE. The insignificance of the association between visual disturbance and DVA in the LASEK and SMILE subgroups might be due to the small sample size. Selection bias might exist in choosing the surgery, and the result could not be accurately compared among different procedures. Second, the follow-up period is relatively short. The severity and bothersome of different visual disturbances might change gradually. Long-term observance is required in future studies. Third, only DVA with horizontally moving objects was evaluated in the present research. DVA with other moving patterns, kinetic visual acuity and motion perception might be affected by the visual disturbance in patients after corneal refractive surgery, which remains to be explored in further study. Fourth, following corneal refractive surgery, pupil diameter may affect the severity and bothersome of visual disturbance that impacts the dynamic vision. However, pupil diameter was not measured during the dynamic visual acuity examination.”
The corrected paragraph appears below:
“Certain limitations exist in the present research. First, the present study is a nonrandomized cohort research. Due to nonrandomized design, the number of patients receiving different types of procedures is unbalanced. More patients who had undergone FS-LASIK were enrolled than those with PRK and SMILE. The insignificance of the association between visual disturbance and DVA in the PRK and SMILE subgroups might be due to the small sample size. Selection bias might exist in choosing the surgery, and the result could not be accurately compared among different procedures. Second, the follow-up period is relatively short. The severity and bothersome of different visual disturbances might change gradually. Long-term observance is required in future studies. Third, only DVA with horizontally moving objects was evaluated in the present research. DVA with other moving patterns, kinetic visual acuity and motion perception might be affected by the visual disturbance in patients after corneal refractive surgery, which remains to be explored in further study. Fourth, following corneal refractive surgery, pupil diameter may affect the severity and bothersome of visual disturbance that impacts the dynamic vision. However, pupil diameter was not measured during the dynamic visual acuity examination.”
The authors apologize for these errors and state that this does not change the scientific conclusions of the article in any way. The original article has been updated.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Keywords: visual disturbance, dynamic visual acuity, myopia, corneal refractive surgery, visual function
Citation: Wang Y, Zhang Y, Wu T, Ren X, Yuan Y, Li X and Chen Y (2024) Corrigendum: The impact of patient-reported visual disturbance on dynamic visual acuity in myopic patients after corneal refractive surgery. Front. Neurosci. 18:1444519. doi: 10.3389/fnins.2024.1444519
Received: 05 June 2024; Accepted: 13 June 2024;
Published: 26 June 2024.
Edited and reviewed by: Jiawei Zhou, Wenzhou Medical University, China
Copyright © 2024 Wang, Zhang, Wu, Ren, Yuan, Li and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yueguo Chen, Y2hlbnl1ZWd1b0AyNjMubmV0
 Yuexin Wang
Yuexin Wang Yu Zhang
Yu Zhang Tingyi Wu
Tingyi Wu Xiaotong Ren
Xiaotong Ren Yifei Yuan1,2
Yifei Yuan1,2 Xuemin Li
Xuemin Li Yueguo Chen
Yueguo Chen