- Functional Brain Diagnostics and Therapy, Department of Neurology, Medical University of Vienna, Vienna, Austria
Unmatched by other non-invasive brain stimulation techniques, transcranial ultrasound (TUS) offers highly focal stimulation not only on the cortical surface but also in deep brain structures. These unique attributes are invaluable in both basic and clinical research and might open new avenues for treating neurological and psychiatric diseases. Here, we provide a concise overview of the expanding volume of clinical investigations in recent years and upcoming research initiatives concerning focused ultrasound neuromodulation. Currently, clinical TUS research addresses a variety of neuropsychiatric conditions, such as pain, dementia, movement disorders, psychiatric conditions, epilepsy, disorders of consciousness, and developmental disorders. As demonstrated in sham-controlled randomized studies, TUS neuromodulation improved cognitive functions and mood, and alleviated symptoms in schizophrenia and autism. Further, preliminary uncontrolled evidence suggests relieved anxiety, enhanced motor functions in movement disorders, reduced epileptic seizure frequency, improved responsiveness in patients with minimally conscious state, as well as pain reduction after neuromodulatory TUS. While constrained by the relatively modest number of investigations, primarily consisting of uncontrolled feasibility trials with small sample sizes, TUS holds encouraging prospects for treating neuropsychiatric disorders. Larger sham-controlled randomized trials, alongside further basic research into the mechanisms of action and optimal sonication parameters, are inevitably needed to unfold the full potential of TUS neuromodulation.
1 Introduction
With its unique capability to non-invasively reach deep brain areas at unparalleled precision, transcranial ultrasound (TUS) applications have attracted increasing interest in basic and clinical research. Depending on focal energy levels, TUS can be administered to achieve highly focal tissue ablation through high-intensity focused ultrasound or for neuromodulation using low-intensity ultrasound which avoids morphological destructions (Beisteiner and Lozano, 2020). Furthermore, concomitant use of TUS and intravenously administered microbubbles has been evaluated for transiently opening the blood–brain-barrier, for example to deliver therapeutic agents (Meng et al., 2019), to clear amyloid-beta accumulations in Alzheimer’s disease (AD, Rezai et al., 2020; Jeong et al., 2022) or to enhance neuromodulatory effects (Jeong et al., 2021). Non-invasive TUS neuromodulation has been investigated using different techniques, starting with unfocussed diagnostic ultrasound systems (Hameroff et al., 2013; Nicodemus et al., 2019), advancing to unnavigated focal applications (e.g., Lohse-Busch et al., 2014; Wang et al., 2022), and resulting in the current state-of-the-art of neuronavigated focal applications, allowing real-time positioning of the ultrasound beam based on individual brain anatomy.
Two classes of technologies are currently available for navigated focal stimulation, low-intensity transcranial focused ultrasound (e.g., tFUS, LIFUS) and transcranial pulse stimulation (TPS). While tFUS is administered in intermittent trains of ultrasound pulses using sinus tones, TPS applies ultrashort (3 μs) pressure pulses with a range of different frequencies which are repeated at 1 to 8 Hz (for review see Beisteiner et al., 2023). Both techniques result in an elongated elliptical ultrasound beam with an axial resolution of approximately 4 cm and a transversal resolution of approximately 4 mm full width at half maximum for typical carrier frequencies of 500 kHz for tFUS and 250 kHz for TPS (Beisteiner et al., 2019; Truong et al., 2022). This spatial resolution surpasses non-invasive brain stimulation methods based on electromagnetic fields, such as transcranial magnetic stimulation (TMS) or transcranial direct current stimulation (tDCS), by far (Figure 1). TPS and certain tFUS systems are currently approved for research purposes (Investigational Device Exemption by the FDA), and TPS is authorized for the treatment of AD (CE certification).
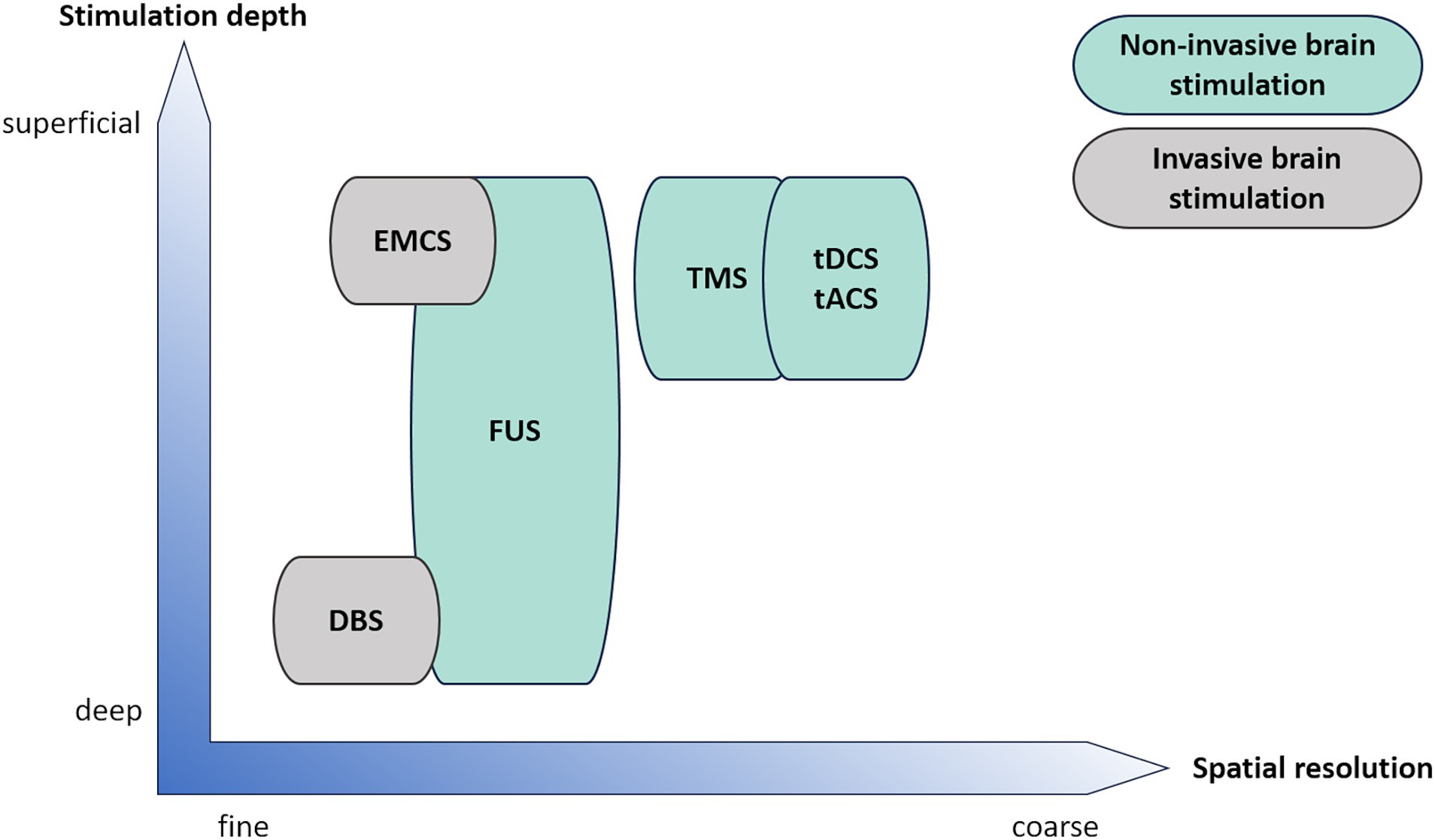
Figure 1. Schematic comparison of invasive (grey) and non-invasive (green) clinical brain stimulation techniques regarding spatial resolution and stimulation depth. DBS, deep brain stimulation; EMCS, extradural motor cortex stimulation; FUS, focused ultrasound; tACS, transcranial alternating current stimulation; tDCS, transcranial direct current stimulation; TMS, transcranial magnetic stimulation.
The growing number of clinical investigations on focused ultrasound in neurological and psychiatric disorders in recent years underscores the necessity for an update of current evidence and forthcoming research initiatives planned in the field. This includes investigations concerning pain, dementia, psychiatric disorders, movement disorders, epilepsy, disorders of consciousness, and other disorders, as detailed in the subsequent section. A critical synthesis of existing evidence, limitations, and future trajectories for TUS are provided in the Discussion.
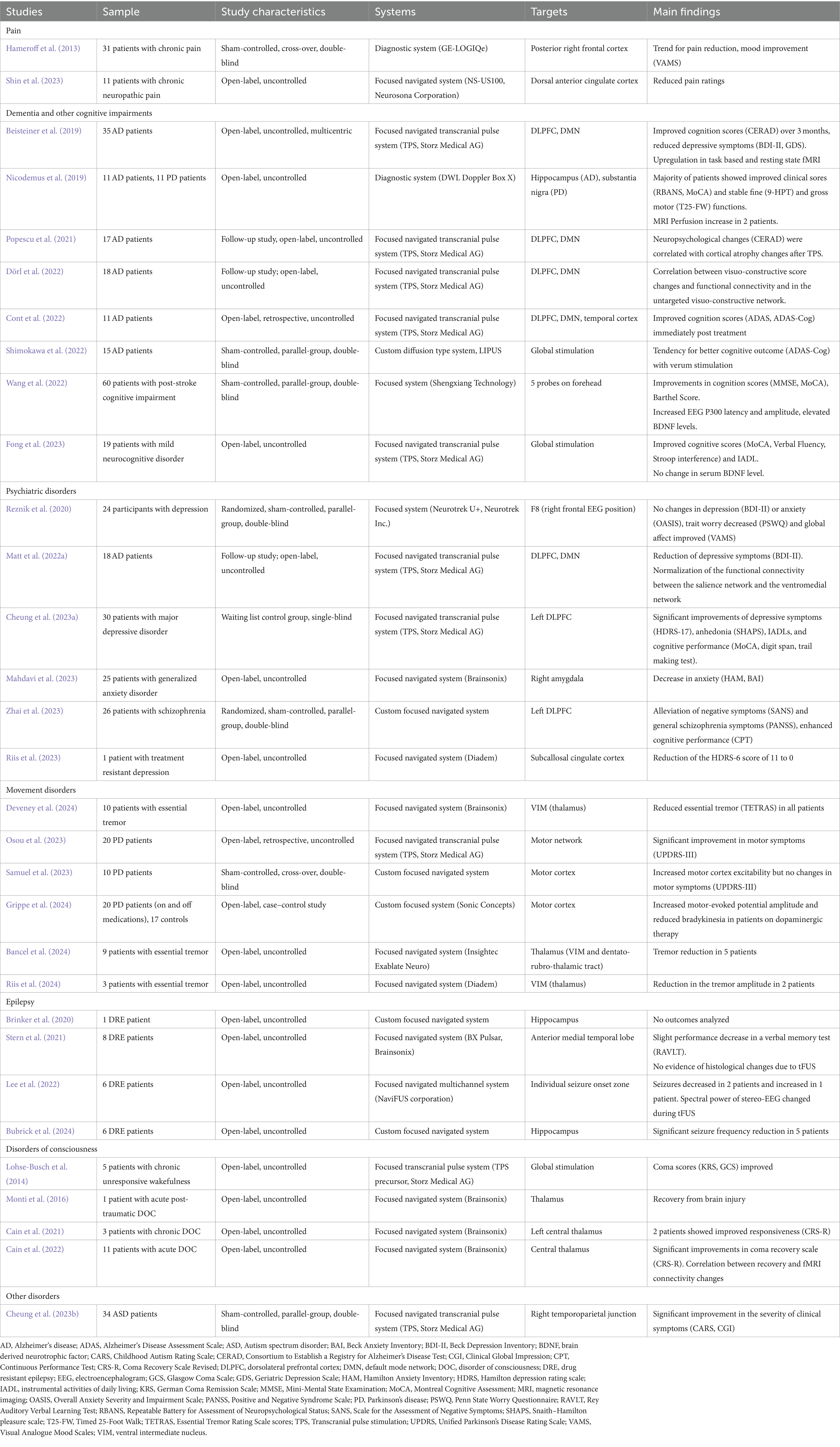
2 Evidence in clinical populations
2.1 Pain
The first report of TUS neuromodulation in humans was provided by Hameroff et al. (2013) who applied an unfocused diagnostic ultrasound device in 31 chronic pain patients in a sham-controlled crossover trial. Compared to sham, verum ultrasound application to the right posterior frontal cortex led to significant improvements in mood and a trend for pain reduction (see Table 1 for details). Focused tFUS directed at the dorsal anterior cingulate cortex reduced pain ratings for up to 4 weeks as found in an open-label study involving 11 patients with chronic neuropathic pain (Shin et al., 2023).
Further, sham-controlled investigations in healthy participants support antinociceptive effects of tFUS. Badran et al. (2020) found decreased sensitization to thermal pain in 19 healthy participants following tFUS targeting the anterior thalamus for active compared to sham stimulation. Relative to sham, verum tFUS of the posterior insula resulted in reduced heat pain ratings and affected early EEG components, whereas stimulation of the anterior insula influenced the heart rate variability and later EEG amplitudes (Legon et al., 2024).
Encouraged by these findings, several clinical trials are planned in neuropathic pain using tFUS only (NCT03111277, NCT04485208, JPRN-jRCTs052230116, Table 2) or in combination with tDCS (diabetic neuropathic pain, NCT03625752). This combination is also used for pain in the context of carpal tunnel syndrome (NCT04206215), osteoarthritis (NCT02723929,) and opiate use disorder with chronic pain (NCT04379115). In addition, tFUS applications are currently investigated in trigeminal neuralgia (NCT04579692) and generalized chronic pain (NCT05674903).
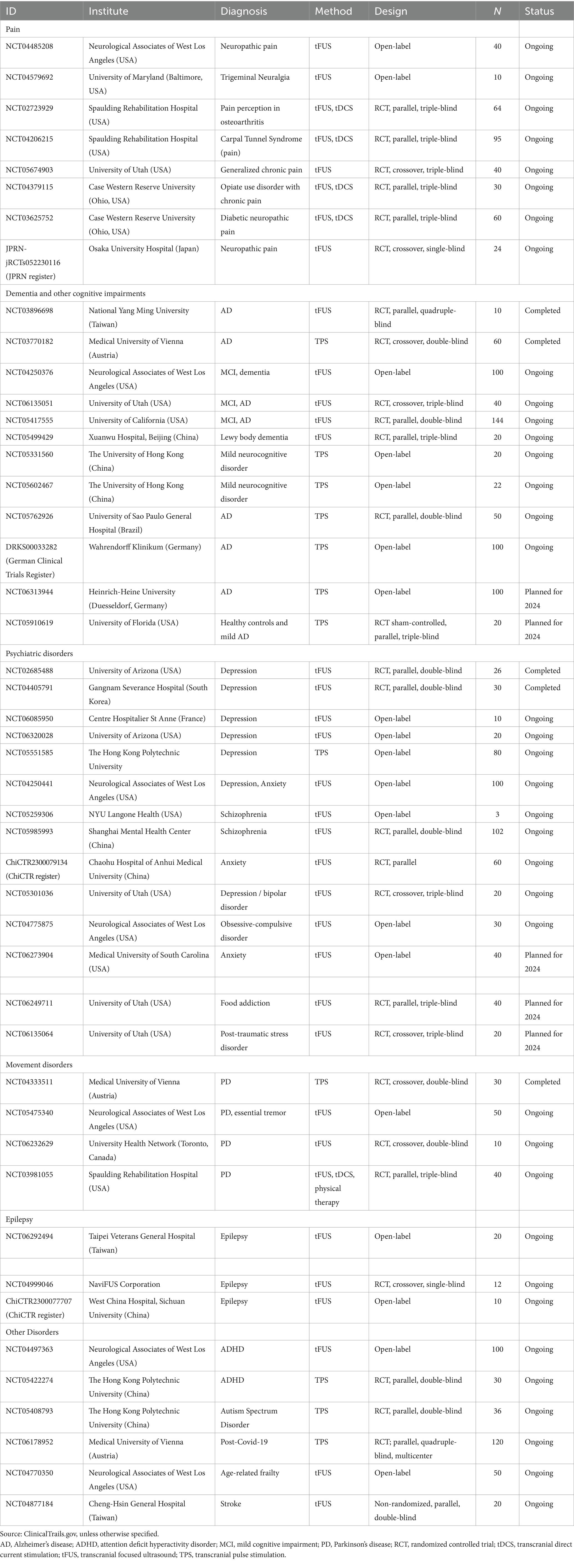
Table 2. Completed (but not yet published), ongoing, and prospective clinical studies on transcranial ultrasound neuromodulation.
2.2 Dementia and other cognitive disorders
Previous findings on TUS regarding reduction of AD-associated amyloid-β depositions and memory improvement in animal models (e.g., Leinenga and Götz, 2015; Eguchi et al., 2018; Bobola et al., 2020), as well as studies on safety and feasibility in healthy participants (e.g., Beisteiner et al., 2019), imply a high potential for therapeutic effects in dementia and other cognitive disorders.
In an open-label study, Nicodemus et al. (2019) directed a diagnostic ultrasound system at the hippocampus in 11 AD patients and at the substantia nigra in 11 patients with Parkinson’s disease (PD) during sleep (see Section 2.3. for motor function evaluation). As reported for the combined AD and PD sample, more than half of the individuals improved in at least one cognitive score (see Table 1 for details). In two patients arterial spin labelling was applied demonstrating increased relative blood flow perfusion after sonication. However, employing identical outcome measures for both AD and PD patients, despite different stimulation targets and the variability of sleep induction—natural or pharmacological—raises questions regarding comparability and interpretation of the findings.
The first clinical investigation with a focused navigated state-of-the-art system was reported by Beisteiner et al. (2019) and this study investigated therapeutic effects in AD. The multicentric open-label study included 35 AD patients who received repeated TPS applications of the dorsolateral prefrontal cortex (DLPFC) and the default mode network. Improved cognitive abilities, particularly in memory and language domains, following TPS interventions persisted up to 3 months and were related to functional upregulation of memory networks. Cognitive enhancements were observed to correlate with cortical atrophy, as evidenced in a subset comprising 17 subjects (Popescu et al., 2021). However, visuo-constructive skills deteriorated after TPS which was associated with a decrease in global efficiency of the visuo-constructive network. As these areas were not targeted by TPS, findings were interpreted as reflecting disease progression within untreated networks, compatible with the high targeting specificity of TUS (Dörl et al., 2022). Using the same technique as Beisteiner et al. (2019), but expanding target regions to the temporal cortex, Cont and colleagues investigated clinical effectiveness of TPS in a retrospective analysis of 11 AD patients and found cognitive enhancements immediately after sonication (Cont et al., 2022). Another open-label TPS study reported a tendency for cognitive improvement in 10 AD patients, along with significantly alleviated neuropsychiatric symptoms 30 days after repeated TPS administration (Shinzato et al., 2024). Further, TPS was reported to improve global cognition, verbal fluency, executive functions, and activities of daily living in an open-label study in 19 older adults with mild neurocognitive disorder (Fong et al., 2023). However, no significant change in the serum level of the brain-derived neurotropic factor (BDNF) was observed here.
Using a diffusion type system adjusted to whole brain low-intensity pulsed sonication, Shimokawa et al. (2022) performed a small sham controlled trial in 22 AD patients, with 10 patients receiving verum sonication and 5 receiving sham stimulation. After more than a year, participants in the treatment group remained cognitively stable while cognitive functions declined in individuals receiving sham. Yet, the difference between groups failed to pass statistical significance, possibly due to the small sample size.
Concerning other cognitive disorders, a randomized sham-controlled trial on post-stroke cognitive impairment included 60 patients who received tFUS treatment of the forehead and cognitive rehabilitation training (Wang et al., 2022). The results depicted significantly higher improvements in cognition, Barthel Score, increased EEG P300 amplitude and latency, and elevated BDNF levels in the verum group.
In conclusion, several open-label studies indicated the potential of TPS and tFUS to improve cognitive deficiencies, as partly supported by functional imaging findings. Larger randomized controlled trials (RCTs) are certainly needed to elucidate the true effect of TUS compared to sham stimulation, as addressed in current and prospective research projects (TPS: NCT03770182, NCT05762926, NCT05910619; tFUS: NCT03896698, NCT06135051, NCT05417555, NCT05499429, see Table 2 for details).
2.3 Psychiatric disorders
Earlier research indicated the potential of non-invasive ultrasound applications to ameliorate behaviors related to depression, fear, and anxiety in animal models (Zhang et al., 2021; Yi et al., 2022; Lee et al., 2024), as well as the capacity to enhance global affect and modulate resting state functional connectivity in healthy subjects (Sanguinetti et al., 2020).
In an RCT, 24 participants with mild to moderate depression were treated with tFUS directed at right fronto-temporal areas (Reznik et al., 2020). Despite the absence of significant reductions in depression and anxiety scores, notable improvements were observed in worrying and global affect after the stimulation. Sonication of the left DLPFC using TPS induced a significant symptom reduction in 30 individuals with depression when compared to a waitlist-control group (Cheung et al., 2023a). Additional improvements were noted in daily functioning as well as anhedonia, and effects remained stable even three months after the treatment conclusion. A durable remission was also reported for a case with severe treatment-resistant depression following sonication of the subcallosal cingulate cortex (Riis et al., 2023).
Additionally, depression scores were assessed within the context of other medical conditions (see corresponding sections for details). Regarding AD cohorts, investigations utilizing TPS showed a reduction of depressive symptoms post-treatment (Cont et al., 2022) and up to 3 months (Beisteiner et al., 2019). A follow-up investigation in a subsample of Beisteiner et al. (2019) revealed that depressive alleviation was associated with normalization of functional connectivity between the salience network and the ventromedial network in AD (Matt et al., 2022a). Conversely, in individuals with mild neurocognitive disorders, there was no mitigation of depressive symptoms after TPS (Fong et al., 2023). Nevertheless, patients suffering from chronic pain showed subjective mood improvements after sonication using an unfocused diagnostic device (Hameroff et al., 2013).
Recently, an open-label pilot study was conducted to investigate the efficacy of tFUS in treating treatment-refractory generalized anxiety disorder (Mahdavi et al., 2023). Anxiety symptoms were significantly reduced following tFUS directed towards the right amygdala in a cohort of 25 patients. In schizophrenia, repetitive tFUS was applied to the left DLPFC in a pilot study including 26 patients resulting in significant improvements of negative and general schizophrenia symptoms in the verum tFUS group only (Zhai et al., 2023).
Consistently, TUS neuromodulation has been found to alleviate depressive symptoms and improve mood, even in non-psychiatric samples and with considerably different stimulation sites. However, sham-controlled evidence is still scarce, stressing the need for more randomized sham-controlled TUS trials in psychiatric disorders, as planned for depression (NCT02685488, NCT04405791, NCT05301036), schizophrenia (NCT05985993), anxiety (ChiCTR2300079134), food addiction (NCT06249711), and post-traumatic stress disorder (NCT06135064).
2.4 Movement disorders
Studies on cortical excitability of the motor cortex and increase in dopamine release in animals (e.g., Zhou et al., 2019; Wang et al., 2020; Xu et al., 2020) and healthy subjects (e.g., Gibson et al., 2018; Legon et al., 2018; Matt et al., 2022b; Bao et al., 2024) suggest a potential benefit of TUS in movement disorders.
In the aforementioned study by Nicodemus et al. (2019, see Section 2.1), no significant alterations after unfocused sonication were found in AD and PD patients regarding fine and gross motor functions (Nicodemus et al., 2019). Potentially, stimulation using a diagnostic US device was not target-specific enough to elicit measurable changes. Personalized focal TPS treatment of cortical motor areas led to a significant improvement in motor symptoms in a retrospective clinical data analysis including 20 PD patients (Osou et al., 2023). Theta-burst TUS stimulation of the motor cortex increased the amplitude of motor evoked potentials (MEP) and improved bradykinesia in 20 PD patients on but not off medication, stressing the impact of dopaminergic therapy for treatment responses (Grippe et al., 2024). In a randomized controlled crossover study applying accelerated theta-burst tFUS to the primary motor cortex in 10 PD patients, reduced pathological motor scores were reported as well, but changes after the treatment were not different between verum and sham stimulation (Samuel et al., 2023). Yet, a significantly increased MEP amplitude was observed for verum vs. sham sonication.
In essential tremor, three open-label studies using tFUS to target the ventral intermediate nucleus of the thalamus showed tremor reductions in the majority of the patients (Bancel et al., 2024; Deveney et al., 2024; Riis et al., 2024).
Evidence for clinical benefits of TUS in movement disorders is currently limited to a few, mostly uncontrolled, studies. The only sham-controlled study so far failed to find a significant clinical difference between verum and sham tFUS, possibly due to the small sample size. Particularly in movement disorders such as PD, which is linked to a dopaminergic deficiency, placebo effects are prominent due to activation of dopaminergic reward system triggered by anticipated symptom relief (Osou et al., 2023). Larger, sham-controlled trials with comprehensive assessments of clinical, behavioral, electrophysiological and imaging outcomes are desirable, as planned in current clinical trials (NCT04333511, NCT06232629, NCT03981055).
2.5 Epilepsy
Motivated by findings in animal epilepsy models (Min et al., 2011; Hakimova et al., 2015; Fomenko et al., 2020) and reports of decreased EEG potentials in humans (e.g., Legon et al., 2014), tFUS has been discussed as a non-invasive technique to suppress epileptiform activity.
Stern et al. investigated the effects of tFUS in eight patients with medication-resistant temporal lobe epilepsy (Stern et al., 2021). Excitatory and inhibitory tFUS was directed towards the anterior mesiotemporal lobe, a region that was subsequently resected in a prescheduled surgery. No histopathological changes were found causally related to tFUS, but neuropsychological tests indicated a reduction in verbal memory functions in a subgroup of four patients.
In another open-label study, tFUS was administered at the individual seizure onset zone in six patients suffering from drug-resistant epilepsy (Lee et al., 2022). Stereo-EEG revealed significant alterations in the spectral power at the targeted electrodes during the stimulation. The frequency of seizures in the subsequent days decreased in two patients, but another patient experienced more frequent subclinical seizures. One patient exhibited impaired memory and naming capabilities that normalized after 3 weeks.
Bubrick et al. (2024) reported a pilot safety trial administering a custom tFUS device, as introduced by Brinker et al. (2020), targeted to the hippocampus in six patients with drug-resistant epilepsy. After six tFUS sessions with scaled intensity, five patients experienced a significantly reduced seizure frequency which persisted for several months thereafter. Resting state fMRI showed a functional connectivity enhancement in the default mode network after stimulation in patients with prominent seizure reduction only, suggesting fMRI as a potential prognostic marker for tFUS effectiveness.
Though limited by the small sample size and the lack of a sham-control, reported seizure frequency reductions are promising. A transient decrement in memory functions was found in two of the studies and was discussed as a result of fatigue (Stern et al., 2021) or as a forced normalization phenomenon (Lee et al., 2022). Nonetheless, memory impairment due to medial temporal lobe sonication is conceivable and warrants careful consideration in prospective investigations. The three currently registered ongoing studies demonstrate a slight increase in scheduled patient number, yet only one RCT is listed (see Table 2 for details).
2.6 Disorders of consciousness
In a longitudinal open-label study, Lohse-Busch et al. (2014) examined the effect of global stimulation with a non-navigated TPS precursor in five patients that have been suffering from stable unresponsive wakefulness syndrome for 7–18 years. Patients received several treatment cycles, comprising of 12 sessions over 4 weeks, over a period of 2–4 years. After the treatment, clinically significant improvements in coma scales were noted. In four patients, non-verbal communication became feasible and in three patients the necessity for a feeding tube was eliminated.
In the framework of the first-in-man open-label clinical trial of thalamic tFUS, Monti and colleagues report several cases of patients with disorders of consciousness who were treated with 10 sonications targeted at the central thalamus. In the first case report, a patient with acute disorder of consciousness recovered from minimally conscious state 3 days after one stimulation session (Monti et al., 2016). A subsequent investigation in three patients with chronic minimal conscious state demonstrated improved responsiveness in two patients after two tFUS sessions (Cain et al., 2021). Finally, 11 patients with acute disorder of consciousness received one (n = 8) or two (n = 3) tFUS sessions with concurrent fMRI (Cain et al., 2022). Compared to the baseline, fMRI activation decreased in prefrontal areas, the anterior cingulate cortex, and the striatum during tFUS stimulation. While no benefit was found immediately after sonication, behavioral responsiveness was significantly enhanced the week following tFUS and was correlated with decreased functional connectivity of the targeted thalamus to frontal and subcortical areas.
The small, open-label studies report benefits in the patient’s responsiveness; however, spontaneous recovery particularly in acute stages of disorders of consciousness must be considered. By now, no ongoing or prospective study was found to be registered.
2.7 Other disorders
So far, only one clinical ultrasound neuromodulation study has been published in developmental disorders. Cheung et al. (2023b) investigated the effect of TPS in a randomized sham-controlled clinical trial in 32 participants between 12 and 17 years of age with autism spectrum disorder who received sonication directed towards the right temporoparietal junction. Autism symptoms and global clinical impression significantly improved in the verum group compared to sham, and changes sustained for at least 3 months. Besides this investigation in autism (NCT05408793, Table 2), attention deficit hyperactivation disorder is being investigated using TPS in an RCT (NCT05422274) and applying tFUS in an open-label study (NCT04497363).
Currently, the effectiveness of TPS in treating neurological Post-Covid-19 symptoms is under investigation in a sham-controlled RCT involving 120 individuals. Meanwhile, tFUS is being studied in a double-blind, non-randomized trial for stroke and an open-label study for age-related frailty.
3 Discussion
Despite the increasing volume of clinical research initiatives, non-invasive brain stimulation using ultrasound in neuropsychiatric conditions is still in its nascent stage. The majority of available literature consists of uncontrolled pilot trials or feasibility studies with limited sample size, and in some controlled trials an appropriate sham condition is missing. So far, randomized sham-controlled studies provide evidence of positive effects of ultrasound neuromodulation regarding cognitive enhancement in stroke, mood improvement in depression, increased motor cortex excitability in PD, as well as relief of schizophrenic and autistic symptoms. Although addressed in open-label studies only, findings regarding tremor attenuation, reduction in epileptic seizure frequency and emergence from chronic minimally conscious state after sonication are promising.
Several studies include objective markers of brain physiology change, such as functional imaging or EEG, providing insight about potential mechanisms of action of ultrasound neuromodulation. Depending on stimulation parameters, tFUS is supposed to act both excitatory and inhibitory. Zadeh et al. (2024) compared three different pulse repetition frequencies (PRF) with a constant duty cycle (DC) of 10% regarding their effect on corticospinal excitability and found attenuated MEP for 10 and 100 Hz but no change for 1,000 Hz compared to a sham condition. Zhang et al. (2023) investigated excitatory (PRF = 2000 Hz, DC = 40%) and inhibitory (PRF = 50 Hz, DC = 2%) TUS protocols using MEP and MR spectroscopy and found increased motor cortex excitability, decreased GABA concentration and increased Glx (glutamine + glutamate) concentration for the excitatory parameters. In the inhibitory stimulation protocol decreased MEP were found, along with substantially increased GABA concentration (19%) and significantly altered GABA/Glx ratio. These findings regarding differential inhibitory and excitatory TUS effects encourage applications to several neurological conditions needing (focal) upregulation, for example in neurodegenerative diseases like AD or PD, or suppression of neuronal activation as mandatory in epilepsy, for example. TPS was reported to induce long-term upregulation of functional activation and connectivity in AD (Beisteiner et al., 2019) and in healthy participants (Matt et al., 2022b), suggesting excitatory neuronal modulation with the potential to sustainably change brain networks and associated symptoms. However, TPS sonication parameters were only marginally varied up to now, leaving room for exploring inhibitory applications as well.
So far, both tFUS and TPS has proven to be well tolerated, without any notion of serious adverse events or morphological brain changes (Pasquinelli et al., 2019; Radjenovic et al., 2022). Rarely occurring side effects such as headache, mood changes, or fatigue were mild and transient.
Certainly, neurophysiological and clinical effects are highly dependent on specific sonication parameters. Regrettably, their consistent reporting is lacking in the existing literature, raising questions about which parameters should be prioritized and how they should be presented. In this rapidly changing field, it is mandatory to agree on common standards regarding reporting of methodological aspects, findings, adverse events, as well as recommendations for established and forthcoming clinical applications of TUS, which is currently under debate (Beisteiner et al., 2024; Martin et al., 2024). More randomized sham-controlled trials are needed to solidify the current evidence, preferentially with large cohorts (> 100 participants), comprehensive assessments of clinical, behavioral and neurophysiological changes, as well as longer follow-up periods to determine persistence of clinical changes.
Author contributions
EM: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing. SR: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. MM: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing. RB: Conceptualization, Formal analysis, Funding acquisition, Methodology, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Herzfelder Foundation (AP01014OFF), Austria.
Acknowledgments
We thank Sarah Osou for her support in literature research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Badran, B. W., Caulfield, K. A., Stomberg-Firestein, S., Summers, P. M., Dowdle, L. T., Savoca, M., et al. (2020). Sonication of the anterior thalamus with MRI-guided transcranial focused ultrasound (tFUS) alters pain thresholds in healthy adults: a double-blind, sham-controlled study. Brain Stimul. 13, 1805–1812. doi: 10.1016/j.brs.2020.10.007
Bancel, T., Béranger, B., Daniel, M., Didier, M., Santin, M., Rachmilevitch, I., et al. (2024). Sustained reduction of essential tremor with low-power non-thermal transcranial focused ultrasound stimulations in humans. Brain Stimul. 17, 636–647. doi: 10.1016/j.brs.2024.05.003
Bao, S., Kim, H., Shettigar, N. B., Li, Y., and Lei, Y. (2024). Personalized depth-specific neuromodulation of the human primary motor cortex via ultrasound. J. Physiol. 602, 933–948. doi: 10.1113/JP285613
Beisteiner, R., Hallett, M., and Lozano, A. M. (2023). Ultrasound neuromodulation as a new brain therapy. Adv. Sci. (Weinh) 10:e2205634. doi: 10.1002/advs.202205634
Beisteiner, R., and Lozano, A. M. (2020). Transcranial ultrasound innovations ready for broad clinical application. Adv. Sci. 7:2002026. doi: 10.1002/advs.202002026
Beisteiner, R., Lozano, A., Di Lazzaro, V., George, M. S., and Hallett, M. (2024). Clinical recommendations for non-invasive ultrasound neuromodulation. SSRN Electron. J. doi: 10.2139/ssrn.4744451
Beisteiner, R., Matt, E., Fan, C., Baldysiak, H., Schönfeld, M., Philippi Novak, T., et al. (2019). Transcranial pulse stimulation with ultrasound in Alzheimer’s disease—a new navigated focal brain therapy. Adv. Sci. 7:1902583. doi: 10.1002/advs.201902583
Bobola, M. S., Chen, L., Ezeokeke, C. K., Olmstead, T. A., Nguyen, C., Sahota, A., et al. (2020). Transcranial focused ultrasound, pulsed at 40 Hz, activates microglia acutely and reduces Aβ load chronically, as demonstrated in vivo. Brain Stimul. 13, 1014–1023. doi: 10.1016/j.brs.2020.03.016
Brinker, S. T., Preiswerk, F., White, P. J., Mariano, T. Y., McDannold, N. J., and Bubrick, E. J. (2020). Focused ultrasound platform for investigating therapeutic neuromodulation across the human Hippocampus. Ultrasound Med. Biol. 46, 1270–1274. doi: 10.1016/j.ultrasmedbio.2020.01.007
Bubrick, E. J., McDannold, N. J., Orozco, J., Mariano, T. Y., Rigolo, L., Golby, A. J., et al. (2024). Transcranial ultrasound neuromodulation for epilepsy: a pilot safety trial. Brain Stimul. 17, 7–9. doi: 10.1016/j.brs.2023.11.013
Cain, J. A., Spivak, N. M., Coetzee, J. P., Crone, J. S., Johnson, M. A., Lutkenhoff, E. S., et al. (2022). Ultrasonic deep brain neuromodulation in acute disorders of consciousness: a proof-of-concept. Brain Sci. 12:428. doi: 10.3390/brainsci12040428
Cain, J. A., Visagan, S., Johnson, M. A., Crone, J., Blades, R., Spivak, N. M., et al. (2021). Real time and delayed effects of subcortical low intensity focused ultrasound. Sci. Rep. 11:6100. doi: 10.1038/s41598-021-85504-y
Cheung, T., Li, T. M. H., Ho, Y. S., Kranz, G., Fong, K. N. K., Leung, S. F., et al. (2023a). Effects of transcranial pulse stimulation (TPS) on adults with symptoms of depression-a pilot randomized controlled trial. Int. J. Environ. Res. Public Health 20:2333. doi: 10.3390/ijerph20032333
Cheung, T., Li, T. M. H., Lam, J. Y. T., Fong, K. H., Chiu, L. Y., Ho, Y. S., et al. (2023b). Effects of transcranial pulse stimulation on autism spectrum disorder: a double-blind, randomized, sham-controlled trial. Brain Commun. 5:fcad226. doi: 10.1093/braincomms/fcad226
Cont, C., Stute, N., Galli, A., Schulte, C., Logmin, K., Trenado, C., et al. (2022). Retrospective real-world pilot data on transcranial pulse stimulation in mild to severe Alzheimer’s patients. Front. Neurol. 13:948204. doi: 10.3389/fneur.2022.948204
Deveney, C. M., Surya, J. R., Haroon, J. M., Mahdavi, K. D., Hoffman, K. R., Enemuo, K. C., et al. (2024). Transcranial focused ultrasound for the treatment of tremor: a preliminary case series. Brain Stimul. 17, 35–38. doi: 10.1016/j.brs.2023.12.007
Dörl, G., Matt, E., and Beisteiner, R. (2022). Functional specificity of TPS brain stimulation effects in patients with Alzheimer’s disease: A follow-up fMRI analysis. Neurol. Ther. 11, 1391–1398. doi: 10.1007/s40120-022-00362-8
Eguchi, K., Shindo, T., Ito, K., Ogata, T., Kurosawa, R., Kagaya, Y., et al. (2018). Whole-brain low-intensity pulsed ultrasound therapy markedly improves cognitive dysfunctions in mouse models of dementia – crucial roles of endothelial nitric oxide synthase. Brain Stimul. 11, 959–973. doi: 10.1016/j.brs.2018.05.012
Fomenko, A., Chen, K.-H. S., Nankoo, J.-F., Saravanamuttu, J., Wang, Y., El-Baba, M., et al. (2020). Systematic examination of low-intensity ultrasound parameters on human motor cortex excitability and behavior. eLife 9:e54497. doi: 10.7554/eLife.54497
Fong, T. K. H., Cheung, T., Ngan, S. T. J., Tong, K., Lui, W. Y. V., Chan, W. C., et al. (2023). Transcranial pulse stimulation in the treatment of mild neurocognitive disorders. Ann. Clin. Transl. Neurol. 10, 1885–1890. doi: 10.1002/acn3.51882
Gibson, B. C., Sanguinetti, J. L., Badran, B. W., Yu, A. B., Klein, E. P., Abbott, C. C., et al. (2018). Increased excitability induced in the primary motor cortex by transcranial ultrasound stimulation. Front. Neurol. 9:1007. doi: 10.3389/fneur.2018.01007
Grippe, T., Shamli-Oghli, Y., Darmani, G., Nankoo, J.-F., Raies, N., Sarica, C., et al. (2024). Plasticity-induced effects of Theta burst transcranial ultrasound stimulation in Parkinson’s disease. Mov. Disord. doi: 10.1002/mds.29836
Hakimova, H., Kim, S., Chu, K., Lee, S. K., Jeong, B., and Jeon, D. (2015). Ultrasound stimulation inhibits recurrent seizures and improves behavioral outcome in an experimental model of mesial temporal lobe epilepsy. Epilepsy Behav. 49, 26–32. doi: 10.1016/j.yebeh.2015.04.008
Hameroff, S., Trakas, M., Duffield, C., Annabi, E., Gerace, M. B., Boyle, P., et al. (2013). Transcranial ultrasound (TUS) effects on mental states: a pilot study. Brain Stimul. 6, 409–415. doi: 10.1016/j.brs.2012.05.002
Jeong, H., Im, J. J., Park, J.-S., Na, S.-H., Lee, W., Yoo, S.-S., et al. (2021). A pilot clinical study of low-intensity transcranial focused ultrasound in Alzheimer’s disease. Ultrasonography 40, 512–519. doi: 10.14366/usg.20138
Jeong, H., Song, I.-U., Chung, Y.-A., Park, J.-S., Na, S.-H., Im, J. J., et al. (2022). Short-term efficacy of transcranial focused ultrasound to the Hippocampus in Alzheimer’s disease: a preliminary study. J. Pers. Med. 12:250. doi: 10.3390/jpm12020250
Lee, C.-C., Chou, C.-C., Hsiao, F.-J., Chen, Y.-H., Lin, C.-F., Chen, C.-J., et al. (2022). Pilot study of focused ultrasound for drug-resistant epilepsy. Epilepsia 63, 162–175. doi: 10.1111/epi.17105
Lee, J., Kim, Y. E., Lim, J., Jo, Y., Lee, H. J., Jo, Y. S., et al. (2024). Transcranial focused ultrasound stimulation in the infralimbic cortex facilitates extinction of conditioned fear in rats. Brain Stimul. 17, 405–412. doi: 10.1016/j.brs.2024.03.013
Legon, W., Bansal, P., Tyshynsky, R., Ai, L., and Mueller, J. K. (2018). Transcranial focused ultrasound neuromodulation of the human primary motor cortex. Sci. Rep. 8:10007. doi: 10.1038/s41598-018-28320-1
Legon, W., Sato, T. F., Opitz, A., Mueller, J., Barbour, A., Williams, A., et al. (2014). Transcranial focused ultrasound modulates the activity of primary somatosensory cortex in humans. Nat. Neurosci. 17, 322–329. doi: 10.1038/nn.3620
Legon, W., Strohman, A., In, A., and Payne, B. (2024). Noninvasive neuromodulation of subregions of the human insula differentially affect pain processing and heart-rate variability: a within-subjects pseudo-randomized trial. Pain. doi: 10.1097/j.pain.0000000000003171
Leinenga, G., and Götz, J. (2015). Scanning ultrasound removes amyloid-β and restores memory in an Alzheimer’s disease mouse model. Sci. Transl. Med. 7:278ra33. doi: 10.1126/scitranslmed.aaa2512
Lohse-Busch, H., Reime, U., and Falland, R. (2014). Symptomatic treatment of unresponsive wakefulness syndrome with transcranially focused extracorporeal shock waves. NeuroRehabilitation 35, 235–244. doi: 10.3233/NRE-141115
Mahdavi, K. D., Jordan, S. E., Jordan, K. G., Rindner, E. S., Haroon, J. M., Habelhah, B., et al. (2023). A pilot study of low-intensity focused ultrasound for treatment-resistant generalized anxiety disorder. J. Psychiatr. Res. 168, 125–132. doi: 10.1016/j.jpsychires.2023.10.039
Martin, E., Aubry, J.-F., Schafer, M., Verhagen, L., Treeby, B., and Pauly, K. B. (2024). ITRUSST consensus on standardised reporting for transcranial ultrasound stimulation. Brain Stimul. 17, 607–615. doi: 10.1016/j.brs.2024.04.013
Matt, E., Dörl, G., and Beisteiner, R. (2022a). Transcranial pulse stimulation (TPS) improves depression in AD patients on state-of-the-art treatment. Alzheimer’s Dement. (New York) 8:e12245. doi: 10.1002/trc2.12245
Matt, E., Kaindl, L., Tenk, S., Egger, A., Kolarova, T., Karahasanović, N., et al. (2022b). First evidence of long-term effects of transcranial pulse stimulation (TPS) on the human brain. J. Transl. Med. 20:26. doi: 10.1186/s12967-021-03222-5
Meng, Y., Pople, C. B., Lea-Banks, H., Abrahao, A., Davidson, B., Suppiah, S., et al. (2019). Safety and efficacy of focused ultrasound induced blood-brain barrier opening, an integrative review of animal and human studies. J. Control. Release 309, 25–36. doi: 10.1016/j.jconrel.2019.07.023
Min, B. K., Yang, P. S., Bohlke, M., Park, S., Vago, D. R., Maher, T. J., et al. (2011). Focused ultrasound modulates the level of cortical neurotransmitters: potential as a new functional brain mapping technique. Int. J. Imaging Syst. Technol. 21, 232–240. doi: 10.1002/ima.20284
Monti, M. M., Schnakers, C., Korb, A. S., Bystritsky, A., and Vespa, P. M. (2016). Non-invasive ultrasonic thalamic stimulation in disorders of consciousness after severe brain injury: a first-in-man report. Brain Stimul. 9, 940–941. doi: 10.1016/J.BRS.2016.07.008
Nicodemus, N. E., Becerra, S., Kuhn, T. P., Packham, H. R., Duncan, J., Mahdavi, K., et al. (2019). Focused transcranial ultrasound for treatment of neurodegenerative dementia. Alzheimer’s Dement. Transl. Res. Clin. Interv. 5, 374–381. doi: 10.1016/j.trci.2019.06.007
Osou, S., Radjenovic, S., Bender, L., Gaal, M., Zettl, A., Dörl, G., et al. (2023). Novel ultrasound neuromodulation therapy with transcranial pulse stimulation (TPS) in Parkinson’s disease: a first retrospective analysis. J. Neurol. 271, 1462–1468. doi: 10.1007/s00415-023-12114-1
Pasquinelli, C., Hanson, L. G., Siebner, H. R., Lee, H. J., and Thielscher, A. (2019). Safety of transcranial focused ultrasound stimulation: a systematic review of the state of knowledge from both human and animal studies. Brain Stimul. 12, 1367–1380. doi: 10.1016/j.brs.2019.07.024
Popescu, T., Pernet, C., and Beisteiner, R. (2021). Transcranial ultrasound pulse stimulation reduces cortical atrophy in Alzheimer’s patients: a follow-up study. Alzheimer’s Dement. Transl. Res. Clin. Interv. 7, 1–6. doi: 10.1002/trc2.12121
Radjenovic, S., Dörl, G., Gaal, M., and Beisteiner, R. (2022). Safety of clinical ultrasound neuromodulation. Brain Sci. 12:1277. doi: 10.3390/brainsci12101277
Rezai, A. R., Ranjan, M., D’Haese, P.-F., Haut, M. W., Carpenter, J., Najib, U., et al. (2020). Noninvasive hippocampal blood-brain barrier opening in Alzheimer’s disease with focused ultrasound. Proc. Natl. Acad. Sci. USA 117, 9180–9182. doi: 10.1073/pnas.2002571117
Reznik, S. J., Sanguinetti, J. L., Tyler, W. J., Daft, C., and Allen, J. J. B. (2020). A double-blind pilot study of transcranial ultrasound (TUS) as a five-day intervention: TUS mitigates worry among depressed participants. Neurol. Psychiatry Brain Res. 37, 60–66. doi: 10.1016/j.npbr.2020.06.004
Riis, T. S., Feldman, D. A., Vonesh, L. C., Brown, J. R., Solzbacher, D., Kubanek, J., et al. (2023). Durable effects of deep brain ultrasonic neuromodulation on major depression: a case report. J. Med. Case Rep. 17:449. doi: 10.1186/s13256-023-04194-4
Riis, T. S., Losser, A. J., Kassavetis, P., Moretti, P., and Kubanek, J. (2024). Noninvasive modulation of essential tremor with focused ultrasonic waves. J. Neural Eng. 21:016033. doi: 10.1088/1741-2552/ad27ef
Samuel, N., Ding, M. Y. R., Sarica, C., Darmani, G., Harmsen, I. E., Grippe, T., et al. (2023). Accelerated transcranial ultrasound neuromodulation in Parkinson’s disease: a pilot study. Mov. Disord. 38, 2209–2216. doi: 10.1002/mds.29622
Sanguinetti, J. L., Hameroff, S., Smith, E. E., Sato, T., Daft, C. M. W., Tyler, W. J., et al. (2020). Transcranial focused ultrasound to the right prefrontal cortex improves mood and alters functional connectivity in humans. Front. Hum. Neurosci. 14, 1–13. doi: 10.3389/fnhum.2020.00052
Shimokawa, H., Shindo, T., Ishiki, A., Tomita, N., Ichijyo, S., Watanabe, T., et al. (2022). A pilot study of whole-brain low-intensity pulsed ultrasound therapy for early stage of Alzheimer’s disease (LIPUS-AD): a randomized, double-blind, placebo-controlled trial. Tohoku J. Exp. Med. 258, 167–175. doi: 10.1620/tjem.2022.J078
Shin, D. H., Son, S., and Kim, E. Y. (2023). Low-energy transcranial navigation-guided focused ultrasound for neuropathic pain: an exploratory study. Brain Sci. 13:1433. doi: 10.3390/brainsci13101433
Shinzato, G. T., Assone, T., Sandler, P. C., Pacheco-Barrios, K., Fregni, F., Radanovic, M., et al. (2024). Non-invasive sound wave brain stimulation with transcranial pulse stimulation (TPS) improves neuropsychiatric symptoms in Alzheimer’s disease. Brain Stimul. 17, 413–415. doi: 10.1016/j.brs.2024.03.007
Stern, J. M., Spivak, N. M., Becerra, S. A., Kuhn, T. P., Korb, A. S., Kronemyer, D., et al. (2021). Safety of focused ultrasound neuromodulation in humans with temporal lobe epilepsy. Brain Stimul. 14, 1022–1031. doi: 10.1016/j.brs.2021.06.003
Truong, D. Q., Thomas, C., Hampstead, B. M., and Datta, A. (2022). Comparison of transcranial focused ultrasound and transcranial pulse stimulation for neuromodulation: a computational study. Neuromodulation 25, 606–613. doi: 10.1016/j.neurom.2021.12.012
Wang, Y., Li, F., He, M.-J., and Chen, S.-J. (2022). The effects and mechanisms of transcranial ultrasound stimulation combined with cognitive rehabilitation on post-stroke cognitive impairment. Neurol. Sci. 43, 4315–4321. doi: 10.1007/s10072-022-05906-2
Wang, Z., Yan, J., Wang, X., Yuan, Y., and Li, X. (2020). Transcranial ultrasound stimulation directly influences the cortical excitability of the motor cortex in parkinsonian mice. Mov. Disord. 35, 693–698. doi: 10.1002/mds.27952
Xu, T., Lu, X., Peng, D., Wang, G., Chen, C., Liu, W., et al. (2020). Ultrasonic stimulation of the brain to enhance the release of dopamine – a potential novel treatment for Parkinson’s disease. Ultrason. Sonochem. 63:104955. doi: 10.1016/j.ultsonch.2019.104955
Yi, S.-S., Zou, J.-J., Meng, L., Chen, H.-M., Hong, Z.-Q., Liu, X.-F., et al. (2022). Ultrasound stimulation of prefrontal cortex improves lipopolysaccharide-induced depressive-like behaviors in mice. Front. Psych. 13:864481. doi: 10.3389/fpsyt.2022.864481
Zadeh, A., Raghuram, H., Shrestha, S., Kibreab, M., Kathol, I., Martino, D., et al. (2024). The effect of transcranial ultrasound pulse repetition frequency on sustained inhibition in the human primary motor cortex: A double-blind, Sham-Controlled Study. Brain Stimul 17, 476–484. doi: 10.1016/j.brs.2024.04.005
Zhai, Z., Ren, L., Song, Z., Xiang, Q., Zhuo, K., Zhang, S., et al. (2023). The efficacy of low-intensity transcranial ultrasound stimulation on negative symptoms in schizophrenia: a double-blind, randomized sham-controlled study. Brain Stimul. 16, 790–792. doi: 10.1016/j.brs.2023.04.021
Zhang, T., Guo, B., Zuo, Z., Long, X., Hu, S., Li, S., et al. (2023). Excitatory-inhibitory modulation of transcranial focus ultrasound stimulation on human motor cortex. CNS Neurosci. Ther. 29, 3829–3841. doi: 10.1111/cns.14303
Zhang, J., Zhou, H., Yang, J., Jia, J., Niu, L., Sun, Z., et al. (2021). Low-intensity pulsed ultrasound ameliorates depression-like behaviors in a rat model of chronic unpredictable stress. CNS Neurosci. Ther. 27, 233–243. doi: 10.1111/cns.13463
Keywords: transcranial ultrasound, neuromodulation, non-invasive brain stimulation, transcranial pulse stimulation, transcranial focused ultrasound
Citation: Matt E, Radjenovic S, Mitterwallner M and Beisteiner R (2024) Current state of clinical ultrasound neuromodulation. Front. Neurosci. 18:1420255. doi: 10.3389/fnins.2024.1420255
Edited by:
Vincent Clark, University of New Mexico, United StatesReviewed by:
Dingjie Suo, Beijing Institute of Technology, ChinaJan Kubanek, The University of Utah, United States
Copyright © 2024 Matt, Radjenovic, Mitterwallner and Beisteiner. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Roland Beisteiner, cm9sYW5kLmJlaXN0ZWluZXJAbWVkdW5pd2llbi5hYy5hdA==
 Eva Matt
Eva Matt Sonja Radjenovic
Sonja Radjenovic Michael Mitterwallner
Michael Mitterwallner Roland Beisteiner
Roland Beisteiner