- Shandong University of Traditional Chinese Medicine, Jinan, Shandong, China
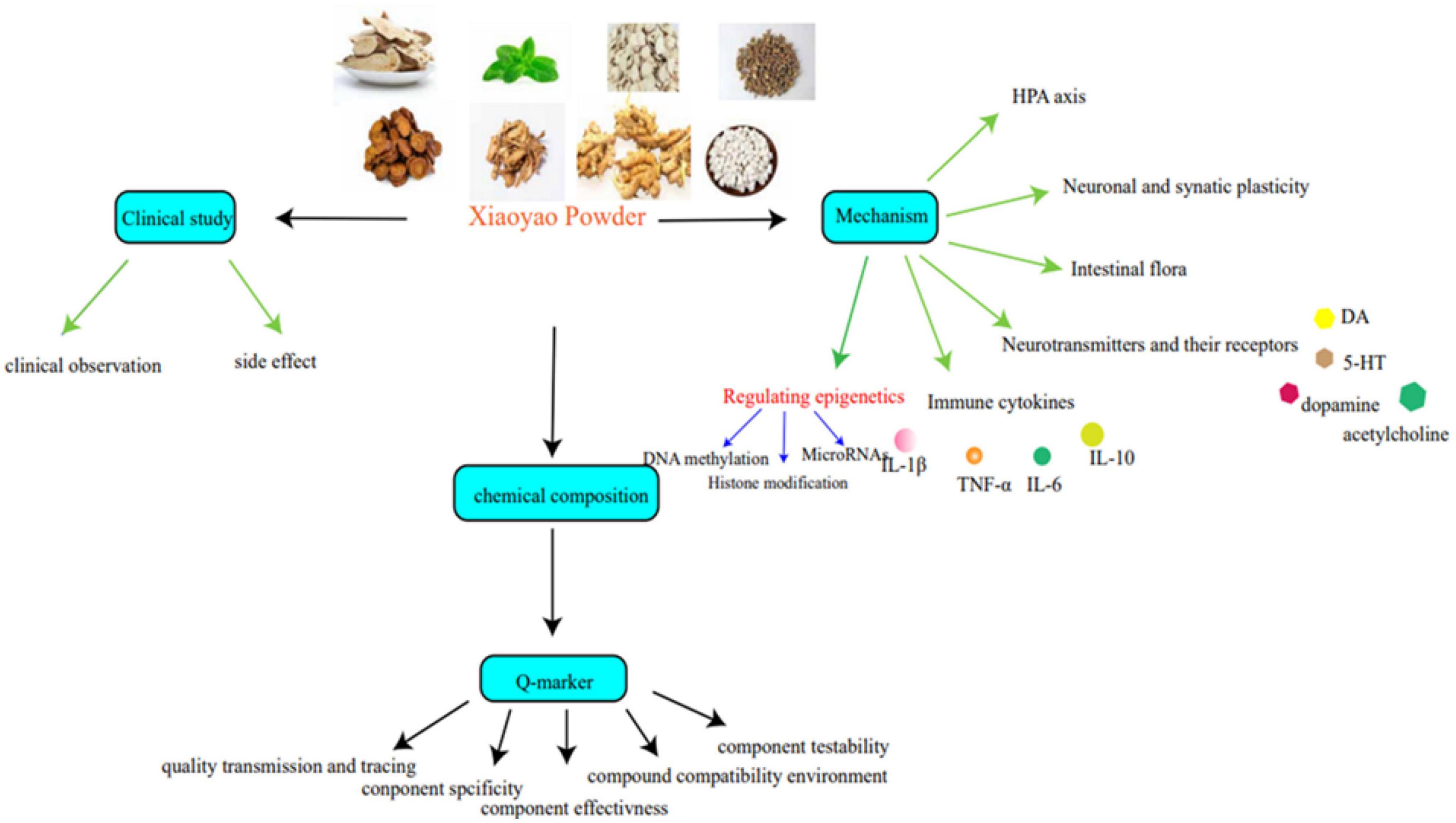
Depression has become one of the most common public health issues around the world, and the incidence has been increasing in recent years. A large amount of clinical investigations have proven that the treatment of depression is difficult. The prognosis is poor, and the fatality rate is high. At present, western medicine is the preferred treatment for depression, but it often causes adverse clinical reactions such as dry mouth, blurred vision, and memory loss, etc. The herbal compound Xiaoyao Powder is a traditional medicine for soothing the liver and relieving depression, strengthening the spleen, and nourishing the blood. It can reduce adverse reactions. It is effective in treating depression. In this study, we elucidate the function of Xiaoyao Powder in anti-depression from the perspective of clinical application and pharmacological mechanisms such as regulating epigenetic and chemical quality markers to provide empirical and experimental theoretical results that contribute to developing future depression therapy with Xiaoyao Powder.
Introduction
Depression is a type of emotional mental disorder that harms human physical and mental health. Studies have shown that morbidity in men is lower than in women (Ivanets et al., 2021). With the increasing pressures of modern society, emotional disorders and cognitive impairments are on the rise in the global burden of disease, and have received widespread attention (Huang et al., 2019; Perini et al., 2019). In clinical medication, 5-hydroxytryptamine (5-HT) reuptake inhibitors and melatonin receptor agonists are often used for treatment, such as Psilocybin, fluoxetine, paroxetine, agomelatine, and so on. However, they have a slow onset, low remission rate, and different degrees of side effects such as dry mouth, blurred vision and memory loss, anxiety, transient headaches, and so on (Carhart-Harris et al., 2016). Traditional Chinese Medicine (TCM), based on the advantages of multiple targets, multiple approaches, and multiple levels, has strengthened depression treatment to a large extent (Chi et al., 2019).
Epigenetics is mostly studied in the case of constant gene nucleotide sequences. The expression of genes is mostly caused by factors such as the environment, emotion, and disease. Therefore, the variation caused by epigenetics is mostly caused by changes in environmental factors and nucleotide interactions. Epigenetic modification, such as histone modification, DNA methylation, and non-coding RNA, affects gene expression. It is generally believed that patients with depression are mostly caused by physiological, psychological, social stress, genetic, and other factors. Similarly, there are differences in epigenetic modification in patients with depression (Nagy et al., 2015), so patients with depression are related to epigenetics.
Xiaoyao Powder comes from the “Formulary of the Bureau of Taiping People’s Welfare Pharmacy.” It consists of Bupleurum Chinese DC. (Radix Bupleuri), Paeonia lactiflora Pall. (Paeonia Lactiflora), Atractylodes macrocephala Koidz. (Atractylodes macrocephala), Angelica sinensis (Oliv.) Diels. (Angelica sinensis), Poria cocos (Schw.) Wolf. (Poria cocos), Glycyrrhiza uralensis Fisch. (Radix Glycyrrhizae), Mentha haplocalyx Briq (Mentha haplocalyx), and Zingiber officinale Rosc. (Ginger) (Table 1). It is generally applied in clinical medication to cure anxiety disorder and multiple diseases complicated with depression (Li et al., 2007; Zhang et al., 2022). Compared with western medicine, it can relieve adverse reactions such as bradycardia, lower limb swelling, headache, dry mouth, blurred vision, and so on. Based on systematically collating relevant domestic and foreign research, this review includes an examination of pharmacological action, clinical applications, and the chemical quality markers of Xiaoyao Powder and how it can be used to treat depression to provide quality control references for the subsequent study (Figure 1).
Clinical application of Xiaoyao Powder in the treatment of depression
Clinical observations of Xiaoyao Powder in the treatment of depression
From the Song Dynasty to the present, Xiaoyao Powder was found to have good efficacy in relieving depression. At the moment, Xiaoyao Powder alone or combined with western medicine such as fluoxetine, paroxetine, and so on has quite a good curative effect on depression. The Xiaoyao Powder has been recognized as an effective medicine for depression, and can relieve depressive symptoms with fewer side effects. A study reported on the use of Xiaoyao Powder in mild depression (liver depression and spleen deficiency type in Chinese medicine). The results made clear that Xiaoyao Powder might enhance the clinical therapeutic effectiveness of the treatment group (96.7%) and reduce the HAMD score of patients in the treatment group (Wang, 2020). A study by Chen included 30 patients with depression and treated them with Jiawei Xiaoyao Powder for 8 weeks, and the Hamilton index indicated that Jiawei Xiaoyao Powder had more significant efficacy compared with fluoxetine treatment (Chen and Wu, 2016). Yuan randomly divided 72 depression patients into an experimental group who took Xiaoyao Powder orally combined with Fluoxetine and a control group (oral Fluoxetine), with 36 cases in each group. After 4 weeks of treatment, they found that the experimental group had a better curative effect according to the Hamilton Depression Scale and TCM syndrome score (Yuan et al., 2022). Chen chose 141 depression patients treated with Jiawei Xiaoyao Powder (Xiaoyao Powder plus Paeonia suffruticosa Andrews, Gardenia jasminoides J. Ellis) and placebo, respectively. The GI symptom score (GIS), Hamilton Depression Scale, and Hamilton Anxiety Scale were observed. The GIS was much higher for those treated with Jiawei Xiaoyao Powder than for those treated with the placebo (Chen et al., 2020). It has also been reported that Xiaoyao Powder combined with other therapies has good curative effects on depression with gynecological diseases, such as breast cancer, perimenopause, and so on (Sun et al., 2016; Tang et al., 2019; Xiao, 2021). Gao (2017) found that 70 patients with postpartum depression were selected and treated with Xiaoyao Powder and paroxetine hydrochloride, respectively. After 12 weeks of treatment, they found that the total effective rates of Xiaoyao Powder and paroxetine hydrochloride were 97.14 and 77.14%, respectively. The incidence of adverse reactions was 2.86 and 25.71%, suggesting that Xiaoyao Powder can significantly improve the symptoms of patients with depression, and high safety. Zheng et al. (2021) randomly divided 150 patients with anxiety and depression into an observation group and a control group who took Xiaoyao Powder, Flupentixol, and Melitracen Tablets, respectively. After 4 weeks of treatment, HAMD (86.3%) and HAMA (79.4%) were higher in the observation group (77.8%) than HAMA (72.2%) in the control group. The anxiety/somatization factor score of the HAMD scale in the observation group (3.5 ± 1.4) was significantly lower than that in the control group (4.6 ± 1.3), and the sleep disorder factor score (2.6 ± 1.3) was significantly lower than that in the control group (3.3 ± 1.4). This shows that Xiaoyao Powder and Flupentixol and Melitracen tablets have obvious effects on improving the symptoms of mixed anxiety and depression, but that Xiaoyao Powder is superior to Flupentixol and Melitracen tablets in improving anxiety, somatization, and sleep disorders and long-term effects. Jiao J. et al. (2019) selected 48 patients with depression syndrome of liver depression and spleen deficiency after chemotherapy for breast cancer, and randomly divided them into a control group (Lifumin tablets) and a traditional Chinese medicine group (Xiaoyao Powder group). After 8 weeks of continuous treatment, the TCM syndrome score of the Xiaoyao Powder group decreased by 12.96 points after treatment, and the total effective rate of treatment was 87.5%. The TCM syndrome score of the control group decreased by 4.96 points, and the total effective rate of treatment was 45.8%. Therefore, Xiaoyao Powder can effectively alleviate the depression syndrome of liver depression and spleen deficiency type in patients with breast cancer undergoing post-operative chemotherapy, and can significantly improve the TCM syndrome score, and the treatment is safer and more effective, with better clinical application value.
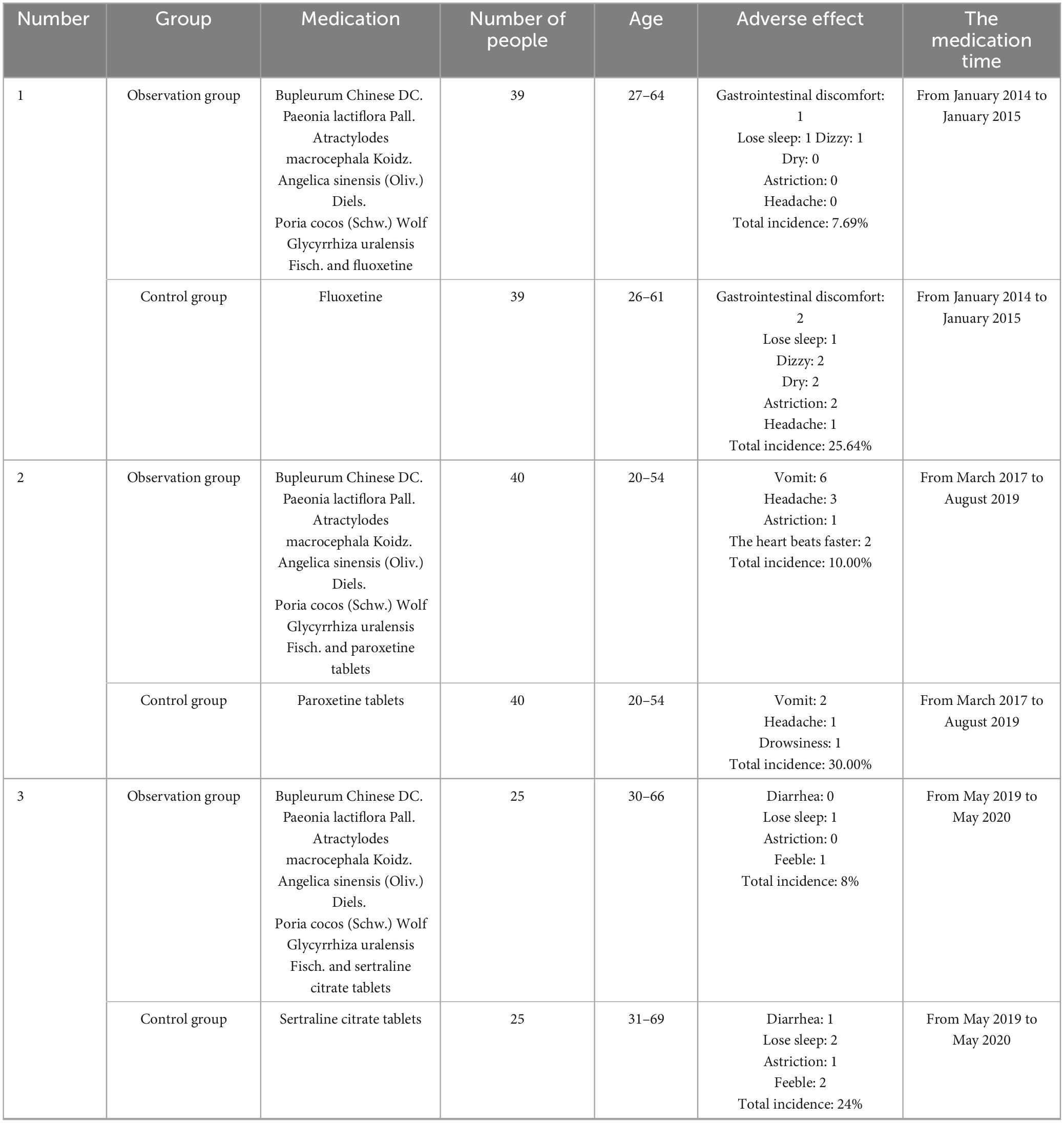
Xiaoyao Powder can improve adverse reactions to depression
The drugs for depression currently include fluoxetine, Paxil, propranolol, venlafaxine, and flecainide. However, through clinical observations, patients often present with bradycardia, lower limb swelling, headache, and other clinical manifestations (Woron et al., 2019). A clinical investigation randomly divided 78 patients into an experimental and control group. The patients in the control group were treated with fluoxetine hydrochloride dispersive tablets and the other group was used to cure fluoxetine hydrochloride dispersive tablets combined with modified Xiaoyao Powder. It was found that the Hamilton Depression Scale was lower in the experimental group (P < 0.05). The experimental group displayed fewer adverse reactions such as dizziness, insomnia, gastrointestinal discomfort, dry mouth, headache, and constipation (Lv, 2015). In another study, 80 patients were assigned to two groups (Xiaoyao Powder and paroxetine separately). Compared with the western medicine group, the effective rate of the TCM group was significantly higher. The occurrence of adverse reactions such as headache, constipation, and rapid heartbeat was reduced for the 2 months of treatment. There were fewer adverse reactions in the TCM group. The effectiveness rate was 95% higher than that of the western drug group (77.5%) (Ma et al., 2020). In addition, Zheng (2021) found that Xiaoyao Powder combined with sertraline on post-stroke depression might enhance the efficacy of sertraline and reduce adverse reactions, which is worth promoting (Table 2).
Pharmacological mechanisms of Xiaoyao Powder in the treatment of depression
Xiaoyao Powder adjusts the HPA axis
Modern research has shown that the incidence of depression has a bearing on the dysfunction of the HPA axis (Cai et al., 2015; Zhou et al., 2022). In addition, the HPA axis of the hypothalamus can promote the expression of corticotropin-releasing factor (CRF), which is transferred from the portal system to the pituitary gland to synthesize ACTH and stimulate the production of cortisol in the adrenocortical cortex (Olloquequi et al., 2018). Wu found that Jiawei Xiaoyao Powder could relieve depression-like behavior and hyperactivity of the HPA axis (Wu et al., 2016). O’Carroll et al. (2003) found that chronic stress reduced the expression of apelin in the PVN and the content of cortisol in plasma, and increased the expression of APJ, meaning it has a negative feedback effect with the HPA axis. Xiaoyao Powder can inhibit the changes in the apelin/APJ system in depressed mice by upgrading the apelin level and downgrading the APJ level (Yan et al., 2018).
Xiaoyao Powder regulates neurotransmitters and their receptors
The neurotransmitter hypothesis is one of the widely accepted mechanisms of gloomy, which consists of the monoamine hypothesis and glutamate-mediated excitatory toxicity hypothesis. The HPA axis is controlled by monoamine neurotransmitters such as 5-HT to relieve emotional stress (Goel et al., 2011). Zhang et al. (2018) found that the addition of the traditional medicine Xiaoyao Powder increased the expression of cortisol and tyrosine hydroxylase, reduced the levels of monoamine neurotransmitters (5-HT and norepinephrine), and alleviated the depressive phenotype and depressive-like behavior of zebrafish. Other scholars have found that Xiaoyao Powder can expand the level of 5-HT in the central nervous system of depression rats and reduce the content of 5-HIAA in depression rats, thus improving depressive symptoms (Bao et al., 2008). Tryptophan metabolism plays a key role in mental diseases. Xiaoyao Powder can up-regulate the IDO1, down-regulate TPH2 to improve tryptophan metabolism, and increase the contents of canine urine, 5-hydroxytryptophan to play an antidepressant role (Jiao H. Y. et al., 2019). Ding found that Xiaoyao Powder could inhibit the release of NE into the blood by LC-NE neurons, resulting in increasing NE in rats, thus playing an antidepressant role (Ding et al., 2014). Wang argued that Xiaoyao Powder shortened the recovery time of post-stroke depressed rats, and regulated the mRNA expression of BDNF. The CB1R and CB2R were upgraded, while the expression of CRF was downgraded (Wang et al., 2019). Glutamic acid is the most abundant amino acid, which is the main excitatory neurotransmitter (Brosnan and Brosnan, 2013). Li (2020) found a strategy that can quicken the effects of antidepressants. For example, Rapid E/I balance is achieved by relieving the inhibition of GABA interneurons on glutamatergic pyramidal neurons and directly activating pyramidal neurons. 5-HT transporters bind to some receptors such as 5-HT1A/1B, and regulate 5-HT neuronal activity and Glu/GABA balance etc (Li, 2020). Luo et al. (2013) found that the biochemical effects of Xiaoyao Powder were characterized by elevated levels of glutamic acid in plasma.
Xiaoyao Powder regulates synaptic plasticity
Synaptic plasticity is the basis for the stability of studying and memory function and plays a regulatory part in sleep, anxiety, and depression (Lovinger and Abrahao, 2018). In the study of depression, many scholars have found that there is a correlation between synaptic plasticity and depression (Alves et al., 2017). Li X. H. et al. (2017) found that Xiaoyao Powder could reduce the damage caused by stress on original synapses, accelerate the connection and formation of new synapses, and thus maintain synaptic plasticity. In most patients with depression, the synaptic structure and synaptic plasticity that are changed are universal. From the perspective of the mechanism, BDNF is essential for the growth, proliferation, survival, and synaptic activity of neurons, playing a decisive part in the survival of neurons and synaptic activity (Machaalani and Chen, 2018; Chen et al., 2022). The BDNF is critically decreased in mood disorders and plays an essential role in most anti-depressant treatments (Caviedes et al., 2017). Ding et al. (2017) found that Xiaoyao Powder could also significantly improve the body weight and depression-like behavior of CUMS mice, significantly increase the BDNF and GDNF in serum, and add the standard of GFAP protein, mRNA as well as immune reactivity in the hippocampus.
Xiaoyao Powder regulates intestinal flora disorders
All kinds of chronic stress can lead to the imbalance of intestinal flora in the body, causing inflammation in the intestinal tract and affecting the absorption of nutrients by intestinal flora. Some surveys have found that severe depression was associated with microbial imbalance. An AI-2 molecule was produced by segmental filamentous bacteria in the intestinal flora. The AI-2 molecule was found to reduce the expression of serum amyloid proteins SAA1 and SAA2, and changed the distribution of inflammatory factors in the brain through the interaction between inflammatory factors and the brain (Medina-Rodriguez et al., 2020). Zhu et al. (2019) believed that Xiaoyao Powder could regulate the balance of intestinal flora, enhance the abundance of Firmicutes, Bacteroidetes, Proteobacteria, and Ruminococcus, reduce the abundance of Prevotellaceae_Ga6A1_group, Prevotellaceae_UCG-001, Desulfovibrio and regulate its metabolites such as short-chain fatty acids so as to play an antidepressant role. Other studies have indicated that Xiaoyao Powder can regulate the excessive abundance of Proteobacteria, Firmicutes, and Cyanobacteria in rats with chronic and unpredictable stress, which restores them to normal levels, thus achieving the effect of treating functional dyspepsia and LSSD after exposure to CUMS (Qiu et al., 2017).
Xiaoyao Powder regulates inflammation cytokines
At present, it is found that cellular inflammatory factors can promote the incidence of depression, and present hypercortisolemia by directly activating the abnormal regulation of the hypothalamus-pituitary-adrenal axis and indirectly changing the sensitivity of glucocorticoid receptors to cortisol, resulting in hypercortisolemia. Cytokines consume central synaptic 5-HT levels by reducing synaptic 5-HT synthesis and increasing its reuptake. They may also deplete neurotrophic factors (Makhija and Karunakaran, 2013). Studies have shown that depressive patients demonstrate increased secretion of pro-inflammatory cytokines including interleukin-1β (IL-1β), interleukin-6 (IL-6), and tumor necrosis factor (TNF-α), cut down the amounts of anti-inflammatory cytokines such as interleukin-4 (IL-4) and interleukin-10 (IL-10). Experimental studies have shown that Xiaoyao Powder can effectively reduce the expression of IL-6 and TNF-α in the hippocampus of rats induced by chronic and unpredictable mild stress (Wan et al., 2020). Jiawei Xiaoyao Powder can elevate the depression-like behavior of LPS-induced rat models with depression, downregulating the overexpression of IL-1β, IL-6, and TNF-α mRNA in the hippocampus (Yu et al., 2017). Xiaoyao Powder can decrease the LPS in the stool, blood, and colon tissue and reduce inflammatory cytokines such as IL-1β, NLRP3, ASC mRNA, and DNA in the colon, thus relieving depression and other symptoms (Hao et al., 2021). It can regulate the hyperfunction of the HPA axis, the immune balance of Th2 and Th17 cells in rats under chronic bondage stress, and reduce the plasma ACTH, serum CORT, IL-13, and IL-17 (Li X. H. et al., 2017).
Chinese medicine in the treatment of depression based on epigenetics
The relationship between epigenetics and depression
DNA methylation is a natural modification. In mammals, DNA methylation is an epigenetic mechanism, that mainly refers to the methyl transfer to the C5 position (Moore et al., 2013). Studies have found that some diseases of external environmental stress like post-traumatic stress disorder are closely related to DNA methylation (Klengel et al., 2014). At present, relevant scholars have found that the abnormal expression of RUFY3 and GBBR2 genes in the brain of patients with depression is increased, and the expression of GRIK2 and BEGAIN is decreased. The abnormal expression of BDNF, SLC6A4, ZBTB20, HDAC2, and HDAC5 genes in the surrounding tissues increased, and the expression of GRIN2A and WDR26 decreased (Saavedra et al., 2016; Penner-Goeke and Binder, 2019). Histone modification is mostly caused by chromatin remodeling, mainly nucleosomes, histones, and corresponding DNA molecules change. The common modification methods mainly include acetylation, methylation, ubiquitination, etc (Li et al., 2008), of which acetylation is the most common modification form. This process is regulated by histone deacetylase (HDAC) and histone acetyltransferase (HAT) to regulate gene activation by regulating the acetylation of histones or transcription factors. Scholars believe that histone acetylation-related genes can be used as potential biomarkers of peripheral blood vessels in patients with depression, which can inhibit HDAC or improve depression-like behavior with antidepressant combination therapy (Schroeder et al., 2007; Hobara et al., 2010). MicroRNAs are endogenous non-coding RNAs with regulatory functions in eukaryotes. They can bind to miRNA response elements (MREs) in the 3′-untranslated regions (3′UTRs) of target genes through sequence complementation to degrade or inhibit the translation of target genes, thereby inhibiting the level of target genes. A variety of studies have shown that miRNAs play a key role in the pathogenesis of neurological diseases such as depression (Lopez et al., 2014; Dwivedi, 2018; Muñoz-Llanos et al., 2018).
Traditional Chinese medicine can treat depression through epigenetics
DNMT3L is an important regulator of DNA methylation (Wienholz et al., 2010). The change of the MBP gene may be one of the pathological changes of depression. Li (2011) induced depression rat model by CUMS. Acupuncture at “Baihui” and “Yanglingquan” can increase the mRNA expression level of the DNMT3L gene and decrease the mRNA expression level of the MBP gene in a depression rat model. Studies have shown that the gene expression of BDNF is closely related to the expression of methyl CpG binding protein 2 (MeCP2), a key molecule involved in epigenetic modification (Jiang, 2008), and MeCP2 can inhibit DNA methylation, chromatin remodeling, and transcription (Yu et al., 2006c). Shi et al. (2018) found that proanthocyanidins can increase the level of MeCP2, carry out epigenetic modification, and then increase the protein expression of depression-related molecule BDNF, thereby improving the cognitive function of depression. Yin et al. (2017) found kidney-tonifying and qi-invigorating prescriptions, such as Zuogui Pill and Yiqi Congming Decoction. It can up-regulate the expression of the egr1 gene and reduce the methylation rate of the egr1 region, increasing the learning and memory ability of elderly rats, and improving cognitive emotion. Ren et al. (2012) found that compared with untrained women, the DNA methylation status of 6 CpG sites that should increase with age was significantly lower than normal. Related studies have found that depressed animals can inhibit the role of histone deacetylases (HDACs) in the brain and inhibit HDAC in the nucleus accumbens, hippocampus, and amygdala (Covington et al., 2015). Covington et al. (2011) found that the level of acetylated histone H3 (acH3) in the amygdala and hippocampus of mice with chronic social stress failure continued to decrease. Traditional Chinese Medicine has various forms of antidepressant effects through histone modification. For example, ginsenosides Rg1 and Rb1 in ginseng can increase the phosphorylation of amygdala protein kinase (APKA) and cyclic adenosine monophosphate effect element binding protein, activate the cyclic adenosine monophosphate-cyclic adenosine monophosphate effect element binding protein-brain-derived neurotrophic factor (cAMP-CREB-BDNF) circuit in the prefrontal cortex, improve synaptic structural abnormalities in the prefrontal cortex, and thus improve depression (Liu et al., 2016). Su et al. (2014) found that Xiaochaihu Decoction can increase the expression of 5-hydroxytryptamine, BDNF, nerve growth factor, and TrkB mRNA in the hippocampus of the model. In addition, acupuncture can improve the depression-like behavior of CUMS model rats by increasing the phosphorylation level of ERK1/2 and increasing the expression of neurotrophic factor BDNF protein, thereby alleviating depressive symptoms (Li et al., 2018). Jiang et al. (2018) found that acupuncture could down-regulate the expression of HDAC2 protein in the hippocampus, promote the acetylation of histone H3K9 in the hippocampus, increase the expression of BDNF mRNA, and alleviate depression-like behavior. MiRNA is the most studied and characterized, and has become the main regulator of neural plasticity and advanced brain function. Yang et al. (2015) found that exosomes secreted by mesenchymal stem cells after intervention with Buyang Huanwu decoction can increase the expression of miR-126 and decrease the expression of miR-221 and miR-222, thereby improving cognitive function. Lily Rehmannia decoction can change a series of miRNAs in depression. For example, miR-144-3p down-regulates targeting glutamate decarboxylase 1 (Gad1) and anti-vesicular GABA transporter (VGAT), and down-regulates miR-495-mediated BDNF expression to exert antidepressant effects (Zhang H. et al., 2021). Duan et al. (2016) found that the expression of miR-383-5p and miR-764-5p was down-regulated in CUMS rats after electroacupuncture intervention, suggesting that electroacupuncture may play an antidepressant role by promoting neurotrophic and inhibiting neuronal apoptosis signaling pathways.
Xiaoyao Powder can treat depression through epigenetics
Li (2018) found that Xiaoyao Powder can effectively affect the insulin signaling pathway by up-regulating the candidate target gene Slc2a4 regulated by differential methylation in the hypothalamic arcuate nucleus of depression model rats and down-regulating Nmur2, thereby improving depression. Through Sequenom Mass ARRAY, Sun et al. (2018a,b) found that the methylation of some specific regions in Npas2 and Stk32 increased after chronic stress. After taking Xiaoyao Powder, the expression of Npas2 m RNA and its corresponding protein decreased, and the degree of DNA methylation at the corresponding sites decreased significantly (Sun et al., 2018a,b).
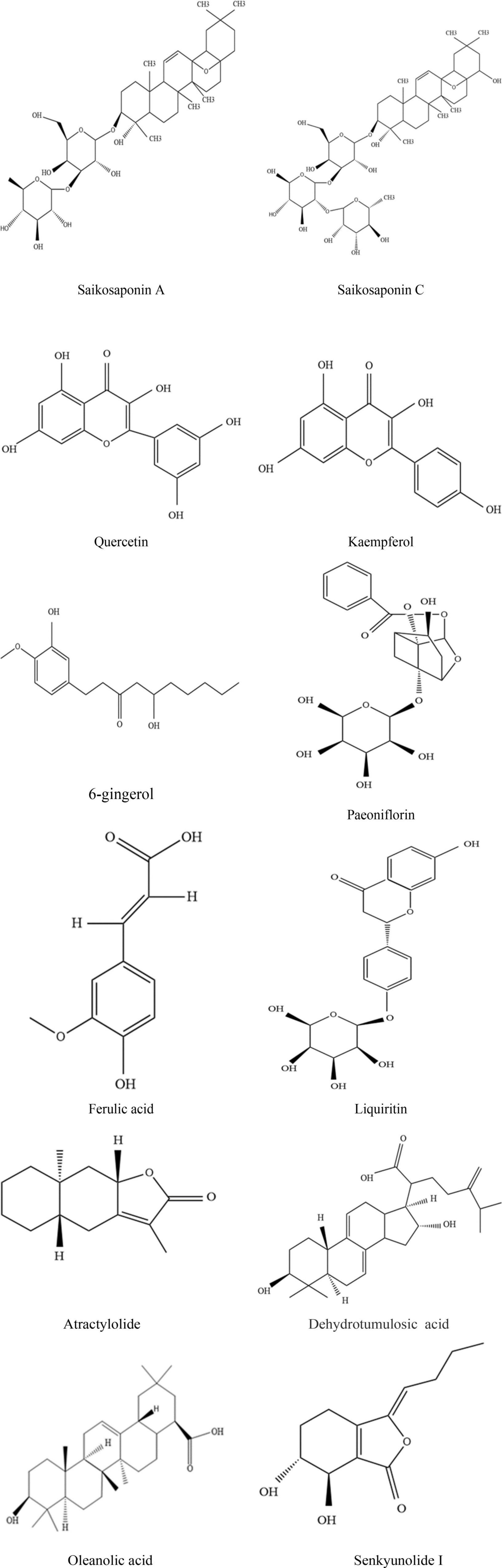
Study on the chemical constituents of Xiaoyao Powder
The chemical constituents of Xiaoyao Powder
The chemical components of Bupleurum Chinese DC. Mainly include saponins, volatile oils, flavonoids, and so on. Studies have found that citric acid, laurene, ethanoic acid, and other components are present in the flowers, leaves, stems, roots, and fruits of Bupleurum Chinese DC., as determined by GC-MS (Meng et al., 2014). Fifty compounds such as saikosaponin A, saikosaponin D, saikosaponin B3, and saikosaponin B1 were detected in Bupleurum Chinese DC. by means of the UHPLC-Q-TOF-MS technique (Lei et al., 2018). Liu et al. (2017) determined saikosaponin B1, saikosaponin F and saikosaponin W etc., in Bupleurum Chinese DC. Root using the spectrometric method. The HPLC method was used to determine the contents of quercetin, isorhamnetin, and kaempferol in Bupleurum Chinese DC. The results showed that the contents were as high as 4.7081, 0.7740, and 0.09515 mg g–1, respectively (Lin et al., 2012).
The chemical components of Angelica sinensis (Oliv.) Diels. mainly include benzene peptides, polysaccharides, and so on. Zhang et al. (2016) discovered a new skeleton of phenyl peptide trimmers and phenyl peptide dimers containing peroxy bridge groups. Later, Two pairs of phthalide trimers such as (−)/(+) triligustilides A (1a/1b) and (−)/(+) triligustilides B (2a/2b) were isolated from Angelica sinensis (Oliv.) Diels. (Zou et al., 2018). Zhao et al. (2023) detected twelve chemical components by high-performance liquid chromatography and triple quadrupole mass spectrometry method. Polysaccharides were found to be one of the main active components in Angelica sinensis (Oliv.) Diels. (Zhao et al., 2016). Additionally, it was found that polysaccharides from Angelica sinensis (Oliv.) Diels. were mainly divided into acid polysaccharides and neutral polysaccharides (Sun et al., 2005).
The chemical components of Atractylodes macrocephala Koidz. mainly include lactones, coumarins, polysaccharides, volatile oils, and so on. Li found two new eudesmane-type sesquiterpenes in the rhizome of Atractylodes macrocephala Koidz., namely eudesma-4(15),7(11)-dien-8α,12-ether (atractylenother, 1),8α-hydroxyeudesma-4(15),7(11)-dien-8β,12-olide (8-epiatractylenolide III, 2), and one new natural product named 4(R),15-epoxy-8 beta hydroxy-atractylenolide II. In addition, it was found that coumarins and phenylpropyl compounds isolated from the rhizomes and aboveground parts of Atractylodes macrocephala Koidz. in recent years were mainly daphne, artemisinin, scopolamine, umbelactone, and so on (Li and Yang, 2014). Wang et al. (2014) detected atractylodes’ polysaccharides, mainly including rhamnose-xylose, mannose, and galactose by high-performance gel permeation chromatography and gas chromatography-mass spectrometry. By using GC-TOF-MS analysis, they found that 26 compounds were reduced in stir-fried bran as compared to raw bran. It indicated that the processing method had a significant influence on the types of volatile components in Atractylodes macrocephala Koidz (Zhang et al., 2014).
The chief chemical constituents of Paeonia lactiflora Pall. are terpenoids, polyphenols, flavonoids, and so on. Studies have found that triterpenoids such as oleanolic acid, ivy saponin, paeoniflorin, betulinic acid, 11α,12α-epoxy-3β, 23-dihydroxy-30-noroleanol-20-ene-28, and 13β-cycloester are the main constituents of Paeonia lactiflora Pall. (Zhou and Wang, 2017). Flavonoids in Paeonia lactiflora Pall. are mainly compounds with a 2-phenylchromogen structure, including catechin, 4′,5-dihydroxy-flavone-7-o-β-D-glucoside, and 5,7-dihydroxy-flavone-4′-o-β-d-glucoside (Shu et al., 2014).
The major chemical components of Poria cocos (Schw.) Wolf are polysaccharides, triterpenoids, sterols, and others. In recent years, scholars have isolated and purified PCSG, PCS3-II, PCM3-II, galactose, glucose, mannose, and other polysaccharide compounds (Shen et al., 2012). Yang et al. (2014) obtained triterpenoids such as oleanolic acid, oleanolic acetate, and alpha-aromatic resin alcohol acetate through their experiments by mass spectrometry and nuclear magnetic resonance. Wang et al. (2015) identified the components in Poria cocos (Schw.) Wolf Skin and White Poria cocos (Schw.) Wolf Skin by UHPLC-DAD-FT/MS. They discovered that dehydrotumulosic acid, trametenolic acid, dehydrotrametenolic acid, and poricoic acid A were the main compounds.
The main chemical components of Processed Glycyrrhiza uralensis Fisch. are flavonoids, coumarin, and other components. Processed Glycyrrhiza uralensis Fisch. mainly contains flavonols, isoflavones, chalcone, and other flavonoids (Li et al., 2000). Through UPLC-Q-TOF-MS Cui found that the contents of five flavonoids such as glycyrrhiza flavonol, glycyrrhiza A, isoflavone and so on increased, while the contents of two coumarins such as 7,2′,4′-trihydroxy-5-methoxy-3-aromatic coumarin and Hedysarimcoumestane B astragalus coumarin B decreased significantly after the processing of Glycyrrhiza uralensis Fisch. It indicates that the composition of Glycyrrhiza uralensis Fisch. changes after processing (Cui et al., 2020).
The other type of herbs are Zingiber officinale Rosc. and Mentha haplocalyx Briq. They mainly have contains volatile oil components. The researchers found that by gas chromatography-mass spectrometry, the Zingiber officinale Rosc. associated irritants include zingerone, shogaols, gingerols, paradols, wikstromol, and so on (Idris et al., 2019). And someone has detected that the piperitenone oxide and carvone are rich in content in the Mentha haplocalyx Briq (Kowalczyk et al., 2022).
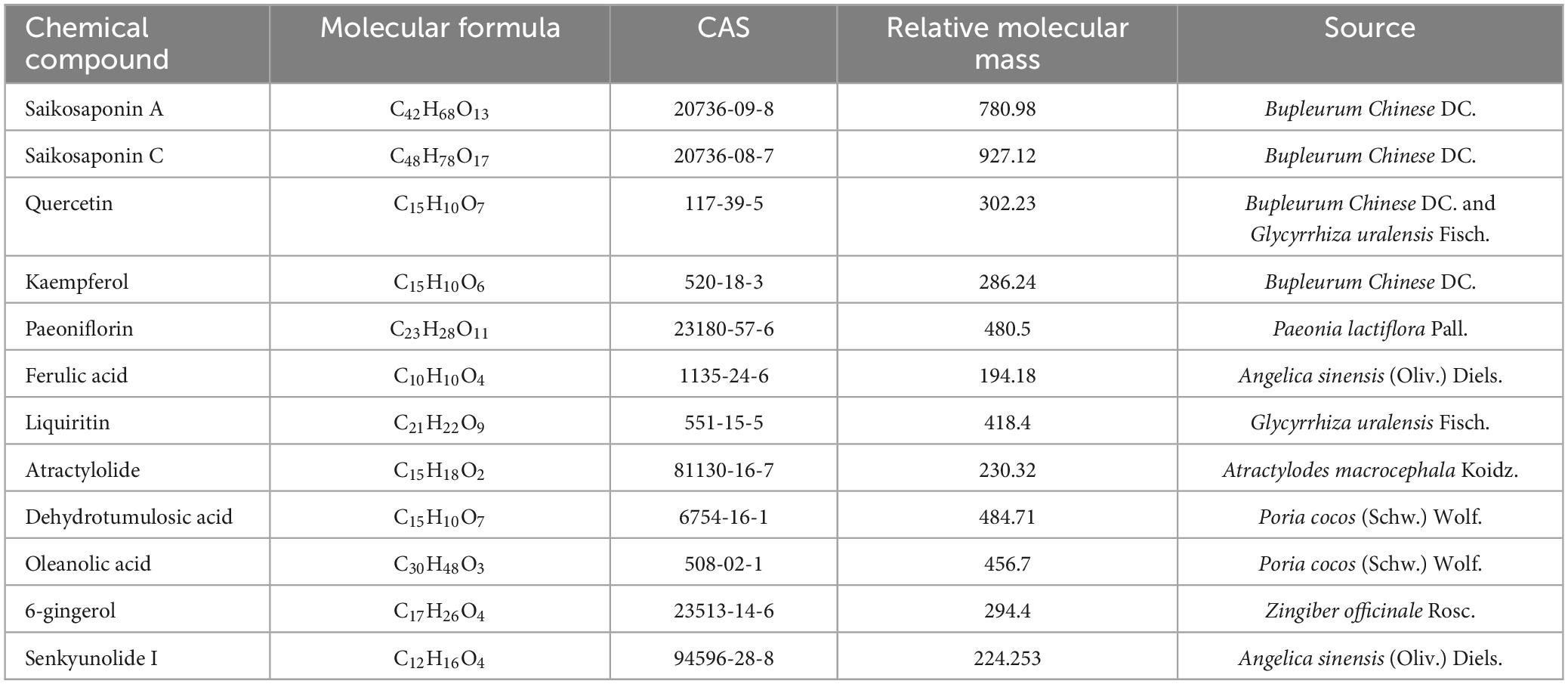
Analysis of quality markers of Xiaoyao Powder in the treatment of depression
Some studies have explored the components of Xiaoyao Powder, but few studies have examined its quality markers. Quality markers are a new concept proposed by Changxiao Liu (Li Y. B. et al., 2019), which mainly include “quality transmission and tracing,” “component specificity,” “component effectiveness,” “compound compatibility environment,” and “component testability.” The components of traditional Chinese medicine and compound are complex and diverse, and there are many targets for the treatment of diseases. The quality of single traditional Chinese medicine will affect the efficacy of the compound, so it is necessary to establish a complete quality evaluation system to control the traditional Chinese medicine compound. Therefore, the article is determined by the quality markers of Xiaoyao Powder in the treatment of depression, which has more clinical application value and the feasibility of establishing a quality control system throughout the whole process.
Q-marker prediction based on mass transfer and traceability
Bupleurum Chinese DC., Angelica sinensis (Oliv.) Diels., Atractylodes macrocephala Koidz., Paeonia lactiflora Pall., Poria cocos (Schw.) Wolf., Processed Glycyrrhiza uralensis Fisch., Zingiber officinale Rosc. and Mentha haplocalyx Briq. are the key ingredients in Xiaoyao Powder, and these were used as keywords in Q-marker prediction. A total of 1,352 chemical components were retrieved from the TCSMP database,1 including 349 came from Bupleurum Chinese DC., 120 for Angelica sinensis (Oliv.) Diels., 55 for Atractylodes macrocephala Koidz., 85 for Paeonia lactiflora Pall., 34 for Poria cocos (Schw.) Wolf, 220 for Processed Glycyrrhiza uralensis Fisch., 164 for Mentha haplocalyx Briq. and 265 for Zingiber officinale Rosc. According to oral drug bioavailability (OB) ≥30% and drug-like (DL) ≥0.12, the following active ingredients were screened out: 14 for Bupleurum Chinese DC. (saikosaponin a, quercetin, kaempferol, etc.), 4 for, Angelica sinensis (Oliv.) Diels. (rohamberyl, β-sitosterol, stigmasterol, etc.), 12 for Atractylodes macrocephala Koidz. (balanol, atractylodes I, atractylodes II, etc.), 13 for Paeonia lactiflora Pall. (methyl trans linoleate, oleanolic acid, paeoniflorin, etc.), 13 for Poria cocos (Schw.) Wolf. (poria acid, dehydroporia acid, trametenolic acid, etc.), 94 for Processed Glycyrrhiza uralensis Fisch. (kaempferol, glycyrrhiza A, urchin etc.), 16 for Zingiber officinale Rosc. (6-gingerol, 6-shogaol, beta-sitosterol, etc.), and 13 for Mentha haplocalyx Briq. (fortunellin, acacetin, linarin, etc.).
The effective components of the compound enter the blood, reach the relevant targets, and exert their activity, which are the main features of the efficacy of the compound prescription. Xu et al. (2018) found that quercetin, ferulic acid, and liquiritigenin in Xiaoyao Powder entered the blood faster, respectively (Tmax = 0.10 ± 0.03,0.21 ± 0.10,0.19 ± 0.07) through UPLC-MS. The absorption of atractylenolide II and atractylenolide III into blood was slow (Tmax = 0.64 ± 0.29,0.67 ± 0.26). Saikosaponin a, saikosaponin c and glycyrrhizic acid were absorbed into the blood due to factors such as enterohepatic recirculation and changes in gastric emptying, and the blood concentration-time curve showed a bimodal type (Xu et al., 2018). Other scholars found that gamma-octalactone, paeoniflorin, and p-hydroxybenzoic acid were the main blood components of Bupleurum Chinese DC. and Paeonia lactiflora Pall. through UPLC-Q-TOF-MS (Zhang et al., 2019). Through UPLC-Q-Orbitrap-HRMS technology, L-tryptophan and atractyloside A were found to be the main blood components of Atractylodes macrocephala Koidz. (Zheng et al., 2022). Lu discovered that Senkyunolide I, senkyunolide H, etc., are considered as an entry component of Angelica sinensis (Oliv.) Diels. (Lu et al., 2017). In addition, through the analysis of UPLC-TOF-MS, Neng found that the main prototype components of Poria cocos (Schw.) Wolf. in the blood were poria C, dehydrosleumoic acid, and oleanolic acid (Neng et al., 2020). Li L. L. et al. (2019) analyzed eight components of Zingiber officinale Rosc. into blood such as 6-gingerol, 6-shogaol, 8-gingerol and so on. Therefore, gamma-octalactone, paeoniflorin, p-hydroxybenzoic acid, L-tryptophan, atractyloside A, polylactic acid C, dehydrostrymoic acid, oleanolic acid, and gingerol may be the direct active components of Xiaoyao Powder.
Prediction of Q-markers based on component specificity
Radix Bupleuri is a plant in the umbrella family Bupleurum Chinese DC. and Bupleurum scorzonerifolium Willd. The dried roots of this plant mainly contain saponins, sterols, volatile oils, polysaccharides, and other components. It is generally believed that saponins and sterols are the material basis of Radix Bupleuri. Therefore, saikosaponin can be used as the unique component of Radix Bupleuri (Sui et al., 2021).
Angelica sinensis is the dried root of Angelica sinensis (Oliv.) Diels. It mainly includes volatile oils, vitamins, organic acids, and other components. It is generally believed that volatile oils and organic acids are the material basis of Angelica sinensis. Therefore, angelic lactone and ferulic acid can be used as the specific components of angelica sinensis (Li et al., 2022).
Atractylodes macrocephala is the dried rhizomes of Atractylodes macrocephala Koidz. The dried rhizomes of this plant mainly contain volatile oils, flavonoids, glycosides, and other components. It is generally believed that volatile oils and flavonoids are the material basis of Atractylodes macrocephala. Therefore, atractylodes ketone, atractylodes lactone can be used as the specific components of Atractylodes macrocephala (Wang et al., 2022).
Paeonia Lactiflora is the dried root of Paeonia lactiflora Pall. It mainly contains volatile oil, glycosides, resins, tannins, and other components. It is generally believed that glycosides and volatile oils are the material basis of Paeonia Lactiflora. Therefore, paeoniflorin and methyl antilinoleate can be used as the specific components of Paeoniae Lactiflora (Tanaka et al., 2013).
Poria cocos is the dried sclerotium of Poria cocos (Schw.) Wolf. It mainly contains polysaccharides, organic acids, amino acids, and other components. It is generally believed that polysaccharide and organic acid are the material basis of Poria cocos. Therefore, the poria polysaccharides, dehydromomoic acid, and oleanolic acid can be used as the specific components of Poria cocos (Lu et al., 2022).
Radix glycyrrhizae is the dried roots and rhizomes of Glycyrrhiza uralensis Fisch, Glycyrrhiza inflata Bat, and Glycyrrhiza glabra L. It mainly contains polysaccharides, flavonoids, organic acids, and other components. It is generally believed that polysaccharides and organic acids are the material basis of Radix glycyrrhizae. Therefore, the glycyrrhiza polysaccharides, glycyrrhiza glycoside, and glycyrrhizic acid can be used as the specific components of Radix glycyrrhizae (Lu et al., 2022).
Ginger is a fresh rhizome of Zingiber officinale Rosc. It mainly includes volatile oils. It is believed that it is the effective material base of Ginger, and gingerol is a specific component of Ginger (Li et al., 2013).
Mentha haplocalyx is the whole grass and leaves of the Mentha haplocalyx Briq. It also mainly has volatile oils. Some think that it is the effective material base of Mentha haplocalyx or menthol (Zhang et al., 2015).
Quality markers of Xiaoyao Powder in the treatment of depression based on the correlation between components and pharmacodynamics
Bupleurum Chinese DC.
The main antidepressant active ingredients of Xiaoyao Powder are paeoniflorin, quercetin, saikosaponin D, and so on. Zhang S. et al. (2021) found that Kaempferol can increase the levels of phosphorylated (p) PI3K/PI3K and pAKT/AKT in the hippocampus of CUMS mice, and reduce pGSK3 β/GSK3 β level. Studies have shown that quercetin in bupleurum can significantly reverse anxiety and depression-like behavior induced by corticosterone-releasing factor (CRF) in rats (Bhutada et al., 2010). It was also detected that quercetin could notably inhibit the expression of CRF mRNA, thus achieving the inhibition of hypothalamic–pituitary–adrenal axis hyperfunction (Kawabata et al., 2010). Dimpfel confirmed that quercetin can significantly change the frequency of brain waves and inhibit the activity of monoamine oxidase in rats (Dimpeel, 2009). Saikosaponin D can protect PC12 cells from corticosterone-induced damage by regulating mitochondrial and nuclear corticosteroid receptor transport, partially reversing mitochondrial dysfunction, and inhibiting the mitochondrial apoptosis pathway (Li et al., 2014). Saikosaponin A significantly inhibited MAPK and NF-κβ signaling pathways (Zhu et al., 2013).
Paeonia lactiflora Pall.
Sun found that paeoniflorin in Peony has a significant protective effect on PC12 cells by significantly inhibiting intracellular calcium overload, stabilizing mitochondrial membrane potential, and inhibiting Bax expression, thus promoting Bcl-2 expression and inhibiting cell apoptosis (Sun et al., 2012). Cui found that paeoniflorin in Peony can play an antidepressant role by enhancing the serotonin and monoamine neurotransmitter content (Cui and Jin, 2012). Li et al. thought that paeoniflorin in Paeoniae Radix Alba reduced IFN-α-induced inflammation in serum and brain regions, such as IL-2, IL-4, etc. The depressive-like behavior of mice induced by long-term high-dose IFN-α was also improved (Li J. et al., 2017).
Angelica sinensis (Oliv.) Diels
Angelica ferulic acid can inhibit glutamate uptake to treat mental illness (Yu et al., 2006a). Senkyunolide can protect PC12 cells which can be damaged by glutamic acid and corticosterone. Thus, Senkyunolide may treat psychiatric disorders (Gong, 2019). Zhang et al. (2007) used a forced swimming test, tail suspension test, and drug interaction model in rats and mice to explore the antidepressant mechanism of ferulic acid. They found that sodium ferulate can significantly shorten the swimming time of rats and mice and the immobility time of tail suspension in mice, suggesting that sodium ferulate has an antidepressant effect. By giving excessive Glu or monosodium glutamate to mice, it can cause neuronal deformation in mice and affect the learning and memory ability of mice, while sodium ferulate can improve this situation, suggesting that sodium ferulate exerts antidepressant effects through neuroprotection and neurorestoration pathways (Yu et al., 2006b; Zhang et al., 2008).
Zingiber officinale Rosc.
Curcumin in ginger can significantly increase the number of head twitches in mice caused by 5-HT, antagonize the hypothermia of mice caused by high-dose apomorphine, and increase the amount of 5-HT, NA, dopamine (DA) in the brain, thus playing an antidepressant role (Xu et al., 2005). Kulkarni et al. (2008) further found that Curcumin not only significantly increased the levels of 5-HT and NA in the hippocampus and frontal cortex, but also significantly increased the levels of DA in Striatum and frontal cortex. Chen et al. (2008) also used this model to conduct experiments and found that in the model group, the adrenal/body mass ratio, Adrenal cortex density, serum Corticosterone level, and Glucocorticoid receptor (GR) mRNA expression were increased, and Curcumin could reverse these changes, and also reverse the reduction of Brain-derived neurotrophic factor (BDNF) in rats caused by stress.
Others
Chen et al. (2021) believed that pachymaran in Poria cocos could increase the levels of BDNF, 5-HT, DA, NE, and other Neurotrophins in the hippocampus of rats, significantly reduce the level of Glu, and thus play an antidepressant role. Glycyrrhizin in licorice can significantly reverse the behavioral damage of rats caused by chronic stress and may achieve an antidepressant effect by improving the activity of Superoxide dismutase, eliminating free radicals, preventing lipid peroxidation, and reducing the production of Malondialdehyde (Zhao et al., 2006). Atractylenolide III can inhibit the increase of pro-inflammatory factors such as IL-1, IL-6, and TNF-α, and alleviate CUMS-induced depression and anxiety-like behavior in rats (Zhou et al., 2021). Gao et al. (2018) showed that atractylenolide I reduced the production of IL-1βby inhibiting the activation of NLRP3 inflammasome, and played an antidepressant-like role in a mouse model of depression induced by chronic unpredictable mild stress (CUMS).
In conclusion, quercetin, saikosaponin D, paeonin, and ferulic acid may be the main ingredients of Xiaoyao Powder in the treatment of depression. They can be used as an important reference for the quality markers of it.
Quality markers in the treatment of depression based on network pharmacology combined with the environment
The main clinical application of TCM is in compounds. The same traditional Chinese medicine has different effects and effective material bases in different traditional Chinese medicine compounds. It is necessary to predict the quality markers of the unique characteristics of Xiaoyao Powder in the treatment of depression based on network pharmacology in the compatibility environment of compounds from the specific etiologies, pathogeneses, and treatment methods.
Gao predicted that the main active ingredients in the antidepressant effect such as saikosaponin A, glycyrrhizin, ferulic acid, paeoniflorin, 6-gingerol, and atractylaractone I can play an antidepressant role by regulating Htr2a, Nmdar1, Pkc, CamkII, and Caspase-3 proteins in the glutaminergic synaptic pathway (Gao, 2021). Through TCSMP, PubChem, OMIM, and other databases, researchers found that paeoniflorin, quercetin, catechin, kaempferol, and other components in Xiaoyao Powder played an antidepressant role by acting on SRC, STAT3, JUN, MAPK3, and other targets (Jian et al., 2021). It has also been found that quercetin, kaempferol, and aloe emodin in Xiaoyao Powder can reduce the expression of inflammatory cytokines by acting on targets likes IL-4 and IL-6 to treat depression (Wei et al., 2021).
Quality markers based on component measurability
Xu used UPLC-MS/MS to determine the content of paeoniflorin, ferulic acid, quercetin, isolicorice, atractylolactone III, saikosaponin A, saikosaponin C, and 14 other components in Xiaoyao Powder (Xu et al., 2018). Tian et al. (2015) used UPLC-DA to determine the contents of ligustilide, atractylenolide I, and atractylenolide II in Xiaoyao Powder.
In summary, based on the “five principles” analysis of quality markers, it can be seen that saikosaponin A, saikosaponin C, quercetin, paeoniflorin, ferulic acid, glycyrrhizin, atractylolactone, dehydrolimoic acid, oleanolic acid, kaempferol, senkyunolide, and 6-gingerol are important quality markers in Xiaoyao Powder (Table 3 and Figure 2). They are highly specific, measurable and convenient for quality control, and can be used as quality markers for Xiaoyao Powder in the treatment of depression.
Summary
Depression is a common mental disorder caused by trauma and other factors, which is manifested by clinical manifestations such as low mood and loss of interest (Orsolini et al., 2019). At present, there are many drugs to treat depression, such as fluoxetine, propranolol, paroxetine, and other drugs. But the side effects are serious and many people do not have an effective solution for life and health. The classic famous prescription Xiaoyao Powder is the traditional prescription for treating depression. It can reduce side effects. Pharmacologically, It can adjust the HPA axis, regulate neuronal, and synaptic plasticity, regulate intestinal flora disorders, regulate neurotransmitters, receptors, and inflammation cytokines, and regulate DNA methylation. And twelve quality markers like Saikosaponin A, Quercetin, etc. are summarized. With the development of the times, the pharmacological mechanism has been deepening. More and more scientists have strengthened research on the microscopic molecular mechanism. There are also many clinical studies on the treatment of depression, especially the addition or subtraction of drugs based on the original prescription according to the different clinical manifestations of patients. However, there are few studies on the chemical composition of Xiaoyao Powder, and in particular, there is a lack of information on quality markers. It is hoped that scientists need to strengthen more detailed studies on the aspect in the future.
Author contributions
JW: writing—original draft preparation. QW and CO: writing—review. GL and HY: writing—review and revise. All authors contributed to the present research and reviewed the entire manuscript, read, and agreed to the published version of the manuscript.
Funding
This work was supported by the Shandong Natural Science Foundation of China (ZR2019ZD23).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
Alves, N. D., Correia, J. S., Patrício, P., Mateus-Pinheiro, A., Machado-Santos, A. R., and Loureiro-Campos, E. (2017). Adult hippocampal neuroplasticity triggers susceptibility to recurrent depression. Transl. Psychiatry 7:e1058. doi: 10.1038/tp.2017.29
Bao, L., Chen, Q., Huang, L., Chen, W., Lin, Q., Yao, X. S., et al. (2008). Effect of Xiaoyao powder on behavioral despair and stress depression in mice [J]. Chin. Med. Mater. 09, 1360–1364.
Bhutada, P., Mundhada, Y., Bansod, K., Ubgade, A., Quazi, M., Umathe, S., et al. (2010). Reversal by quercetin of corticotrophin releasing factor induced anxiety- and depression-like effect in mice. Prog. Neuropsychopharmacol. Biol. Psychiatry 34, 955–960. doi: 10.1016/j.pnpbp.2010.04.025
Brosnan, J. T., and Brosnan, M. E. (2013). Glutamate: a truly functional amino acid. Amino Acids 45, 413–418. doi: 10.1007/s00726-012-1280-4
Cai, L., Li, R., Tang, W. J., Meng, G., Hu, X. Y., and Wu, T. N. (2015). Antidepressant-like effect of geniposide on chronic unpredictable mild stress-induced depressive rats by regulating the hypothalamus-pituitary-adrenal axis. Eur. Neuropsychopharmacol. 25, 1332–1341. doi: 10.1016/j.euroneuro.2015.04.009
Carhart-Harris, R. L., Bolstridge, M., Rucker, J., Day, C. M., Erritzoe, D., Kaelen, M., et al. (2016). Psilocybin with psychological support for treatment-resistant depression: An open-label feasibility study. Lancet Psychiatry 3, 619–627. doi: 10.1016/S2215-0366(16)30065-7
Caviedes, A., Lafourcade, C., Soto, C., and Wyneken, U. (2017). BDNF/NF-κB signaling in the neurobiology of depression. Curr. Pharm. Des. 23, 3154–3163. doi: 10.2174/1381612823666170111141915
Chen, G., Feng, P. M., Wang, S. F., Ding, X. P., Xiong, J. Y., Wu, J. H., et al. (2020). An herbal formulation of Jiawei Xiaoyao for the treatment of functional dyspepsia: A multicenter, randomized, placebo-controlled, clinical trial. Clin. Transl. Gastroenterol. 11, e00241. doi: 10.14309/ctg.0000000000000241
Chen, J. B., Lei, C. F., Li, X. J., Wu, Q., Liu, C. Y., Ma, Q. Y., et al. (2022). Research progress on classical traditional Chinese medicine formula Xiaoyaosan in the treatment of depression. Front. Pharmacol. 13:925514. doi: 10.3389/fphar.2022.925514
Chen, K. Z., Chen, S., Ren, J. Y., Lin, S., Xiao, M. J., Ch, L., et al. (2021). Study on the antidepressant effect of acidic polysaccharides from Poria cocos and its mechanism of regulating neurotransmitters and NLRP3 pathway. Chin. J. Trad. Chin. Med. 46, 5088–5095.
Chen, L., Lv, P., Pan, J. C., Yao, H., Jiang, W., Ma, X., et al. (2008). Effects of curcumin on adrenal gland, serum ACTH and immune function in chronic stress rats. J. Wenzhou Med. Coll. 38, 22–24.
Chen, Z. L., and Wu, Z. G. (2016). Clinical observation of Jiawei Xiaoyao Powder in treating depression of liver depression and spleen deficiency. Res. Integr. Trad. Western Med. 8, 298–300.
Chi, X., Wang, S., Baloch, Z., Zhang, H., Li, X., Zhang, Z., et al. (2019). Research progress on classical traditional Chinese medicine formula lily bulb and Rehmannia decoction in the treatment of depression. Biomed. Pharmacother. 112:108616. doi: 10.1016/j.biopha.2019.108616
Covington, H. E., Maze, I., Vialou, V., and Nestler, E. J. (2015). Antidepressant action of HDAC inhibition in the prefrontal cortex. Neuroscience 298, 329–335. doi: 10.1016/j.neuroscience.2015.04.030
Covington, H. E., Vialou, V. F., LaPlant, Q., Ohnishi, Y. N., and Nestler, E. J. (2011). Hippocampal-dependent antidepressant-like activity of histone deacetylase inhibition. Neurosci. Lett. 493, 122–126. doi: 10.1016/j.neulet.2011.02.022
Cui, G. Z., and Jin, S. M. (2012). Effect of paeoniflorin on reserpine-induced depression model. Chin. J. Exp. Prescript. 18, 272–274.
Cui, Y. Y., Zhou, Y. F., Ma, Y. Q., Fang, G. X., Wang, G. Q., Zhang, R. R., et al. (2020). Based on UPLC-Q-TOF-MS, the differences of chemical components in raw and roasted licorice were analyzed. China Pharmacy 31, 1049–1053.
Dimpeel, W. (2009). Rat electropharmacograms of the flavonoids rutin and quercetin in comparison to those of moclobemide and clinically used reference drugs suggest antidepressive and/or neuroprotective action. Phytomedicine 16, 287–294. doi: 10.1016/j.phymed.2009.02.005
Ding, X. F., Liu, Y., Yan, Z. Y., Li, X. J., Ma, Q. Y., Jin, Z. Y., et al. (2017). Involvement of normalized glial fibrillary acidic protein expression in the hippocampi in antidepressant-like effects of Xiaoyao powder on chronically stressed mice. Evid. Based Complement. Alternat. Med. 2017:1960584. doi: 10.1155/2017/1960584
Ding, X. F., Zhao, X. H., Tao, Y., Zhong, W. C., Fan, Q., Diao, J. X., et al. (2014). Xiaoyao powder improves depressive-like behaviors in rats with chronic immobilization stress through modulation of locus coeruleus-norepinephrine system. Evid. Based Complement. Alternat. Med. 2014:605914. doi: 10.1155/2014/605914
Duan, D. M., Dong, X., Tu, Y., and Liu, P. (2016). A microarray study of chronic unpredictable mild stress rat blood serum with electro-acupuncture intervention. Neurosci. Lett. 627, 160–167. doi: 10.1016/j.neulet.2016.05.054
Dwivedi, Y. (2018). MicroRNAs in depression and suicide: Recent insights and future perspectives. J. Affect. Disord. 240, 146–154. doi: 10.1016/j.jad.2018.07.075
Gao, H., Zhu, X., Xi, Y., Li, Q., Shen, Z., and Yang, Y. (2018). Anti-depressant-like effect of atractylenolide I in a mouse model of depression induced by chronic unpredictable mild stress. Exp. Ther. Med. 15, 1574–1579. doi: 10.3892/etm.2017.5517
Gao, L. (2017). Research on the application and effect of Xiaoyao Powder free decoction in the treatment of postpartum depression [J]. Applic. Mod. Chin. Med. 11, 185–186. doi: 10.14164/j.cnki.cn11-5581/r.2017.18.105
Gao, Y. (2021). Integrative study on antidepressant mechanism of Xiaoyao powder based on multi-group and network pharmacology. Shanxi: Shanxi University.
Goel, N., Plylerm, K. S., Daniels, D., and Bale, T. L. (2011). Androgenic influence on serotonergic activation of the HPA stress axis. Endocrinology 152, 2001–2010. doi: 10.1210/en.2010-0964
Gong, W. X. (2019). Study on the antidepressant effect and mechanism of Angelica sinensis and its active constituents. Shanxi: Shanxi University.
Hao, W. Z., Wu, J. J., Yuan, N. J., Gong, L., Huang, J., and Ma, Q. Y. (2021). Xiaoyao powder improves antibiotic-induced depressive-like and anxiety-like behavior in mice through modulating the gut microbiota and regulating the NLRP3 inflammasome in the colon. Front. Pharmacol. 12:619103. doi: 10.3389/fphar.2021.619103
Hobara, T., Uchida, S., Otsuki, K., Matsubara, T., Funato, H., Matsuo, K., et al. (2010). Altered gene expression of histone deacetylases in mood disorder patients. J. Psychiatr Res. 44, 263–270. doi: 10.1016/j.jpsychires.2009.08.015
Huang, Y. Q., Wang, Y., Wang, H., Liu, Z. R., Yu, X., Yan, J., et al. (2019). Prevalence of mental disorders in China: A cross-sectional epidemiological study. Lancet Psychiatry 6, 211–224. doi: 10.1016/S2215-0366(18)30511-X
Idris, N. A., Yasin, H. M., and Usman, A. (2019). Voltammetric and spectroscopic determination of polyphenols and antioxidants in ginger (Zingiber officinale Roscoe). Heliyon 5, e01717. doi: 10.1016/j.heliyon.2019.e01717
Ivanets, N. N., Kinkul’kina, M. A., Tikhonova, Y. G., Makarova, M. A., and Sysoeva, V. P. (2021). Unipolar depression: A gender-based comparative analysis. Zh. Nevrol. Psikhiatr. Im. S S Korsakova 121, 13–18. doi: 10.17116/jnevro202112108113
Jian, C., Li, M. Y., Wei, F. X., Liu, H. L., Qin, X. M., and Liu, X. J. (2021). Study on the network pharmacological mechanism of Xiaoyao powder combined with venlafaxine in anti-depression. Drug Eval. study 44, 2545–2554.
Jiang, H., Zhang, X., Lu, J., Meng, H., Sun, Y., Yang, X., et al. (2018). Antidepressant-like effects of acupuncture-insights from DNA methylation and histone modifications of brain-derived neurotrophic factor. Front. Psychiatry 9:102. doi: 10.3389/fpsyt.2018.00102
Jiang, L. M. (2008). Preliminary study on the expression of MeCP2, BDNF and Atoh1 genes in cochlea and cochlear nucleus of mice with age-related hearing loss. Hunan: Central South University.
Jiao, H. Y., Yan, Z. Y., Ma, Q. Y., Li, X. Q., Jiang, Y. M., Liu, Y. Y., et al. (2019). Influence of Xiaoyaosan on depressive-like behaviors in chronic stress-depressed rats through regulating tryptophan metabolism in hippocampus. Neuropsychiatr. Dis. Treat 15, 21–31. doi: 10.2147/NDT.S185295
Jiao, J., Luo, K. H., and Li, Y. H. (2019). Clinical observation of Xiaoyaosan Decoction in the treatment of depression syndrome of liver depression and spleen deficiency type in patients with breast cancer after postoperative chemotherapy [J]. Tumor Pharmacy 9, 107–111.
Kawabata, K., Kawai, Y., and Terao, J. (2010). Suppressive effect of quercetin on acute stress-induced hypothalamic-pituitary-adrenal axis response in Wistar rats. J. Nutr. Biochem. 21, 374–380. doi: 10.1016/j.jnutbio.2009.01.008
Klengel, T., Pape, J., Binder, E. B., and Mehta, D. (2014). The role of DNA methylation in stress-related psychiatric disorders. Neuropharmacology 80, 115–132. doi: 10.1016/j.neuropharm.2014.01.013
Kowalczyk, A., Kuś, P., Marijanović, Z., Tuberoso, C., Fecka, I., and Jerković, I. (2022). Headspace solid-phase micro-extraction versus hydrodistillation of volatile compounds from leaves of cultivated Mentha Taxa: Markers of safe chemotypes. Molecules 27:6561. doi: 10.3390/molecules27196561
Kulkarni, S. K., Bhutani, M. K., and Bishnol, M. (2008). Antidepressant activity of curcumin: Involvement of serotonin and dopamine system. Psychopharmacology 201, 435–442.
Lei, T. L., Chen, S. F., Wang, K., Zhang, D. D., Dong, L., Lv, C. N., et al. (2018). Characterization and discrimination of raw and vinegar-baked Bupleuri radix based on UHPLC-Q-TOF-MS coupled with multivariate statistical analysis. Biomed. Chromatogr. 32:4044. doi: 10.1002/bmc.4044
Li, B. (2011). Study on the behavioral and epigenetic mechanisms of electroacupuncture and drug antidepressants. Fudan: Fudan University.
Li, J., Huang, S., Huang, W., Wang, W., Wen, G., Gao, L., et al. (2017). Paeoniflorin ameliorates interferon-alpha-induced neuroinflammation and depressive-like behaviors in mice. Oncotarget 8, 8264–8282. doi: 10.18632/oncotarget.14160
Li, L. L., Cui, Y., Guo, X. H., Ma, K., Tian, P., Feng, J., et al. (2019). Pharmacokinetics and tissue distribution of gingerols and shogaols from ginger (Zingiber officinale Rosc.) in Rats by UPLC−Q-Exactive−HRMS. Molecules 24:512. doi: 10.3390/molecules24030512
Li, M. L., Cui, X. W., Jin, L., Li, M. F., and Wei, J. H. (2022). Bolting reduces ferulic acid and flavonoid biosynthesis and induces root lignification in Angelica sinensis. Plant Physiol. Biochem. 170, 171–179. doi: 10.1016/j.plaphy.2021.12.005
Li, Q. H., Shan, X. X., Ye, W. D., Yin, X. Y., Yuan, Y. M., and Fang, X. M. (2013). Research progress and predictive analysis of quality markers of Shegan Mahuang Decoction. Chin. J. Trad. Chin. Med. 2013, 1–11. doi: 10.19540/j.cnki.cjcmm.20230302.201
Li, W., Asada, Y., and Yoshikawa, T. (2000). Flavonoid constituents from Glycyrrhiza glabra hairy root cultures. Phytochemistry 55, 447–456. doi: 10.1016/s0031-9422(00)00337-x
Li, X., Wang, X., He, K., Ma, Y., Su, N., He, H., et al. (2008). High-resolution mapping of epigenetic modifications of the rice genome uncovers interplay between DNA methylation, histone methylation, and gene expression. Plant Cell 20, 259–276. doi: 10.1105/tpc.107.056879
Li, X., Xu, M. M., Jiang, H. L., Lu, J., Zhang, X. H., and Zhao, B. C. (2018). Effect of hand acupuncture intervention on the expression of extracellular regulated protein kinase 1/2 and brain-derived neurotrophic factor in the prefrontal cortex of rats with chronic mild unpredictable stress. Acupunct. Study 43, 705–710.
Li, X. H., Yu, B., Wu, X. J., Xie, M. Y., Zeng, F. C., and Wei, L. T. (2017). Effect of Xiaoyao Powder on HPA Axis, IL-13 and IL-17 in rats with liver depression and spleen deficiency syndrome caused by chronic restraint stress. Shizh. Trad. Chin. Med. 28, 1815–1816.
Li, X. J. (2018). Gen stagnation and spleen deficiency syndrome-Xiaoyao powder (prescription syndrome) whole genome DNA methylation and its regulation of arcuate nucleus. Beijing: Beijing University of Chinese Medicine.
Li, Y., and Yang, X. W. (2014). New eudesmane-type sesquiterpenoids from the processed rhizomes of Atractylodes macrocephala. J. Asian Nat. Prod. Res. 16, 123–128. doi: 10.1080/10286020.2013.840295
Li, Y. B., Zhang, Y. N., Wang, Y. M., Li, Y. M., Yang, F. F., Zhang, P. J., et al. (2019). A strategy for the discovery and validation of toxicity quality marker of Chinese medicine based on network toxicology. Phytomedicine 54, 365–370. doi: 10.1016/j.phymed.2018.01.018
Li, Y. F. (2020). A hypothesis of monoamine (5-HT) - Glutamate/GABA long neural circuit: Aiming for fast-onset antidepressant discovery. Pharmacol. Ther. 208:107494. doi: 10.1016/j.pharmthera.2020.107494
Li, Y. J., Luo, H. C., and Qian, R. Q. (2007). Effect of Danzhi Xiaoyao Powder on neuro-immuno-endocrine system in patients with depression. Zhong. Zhong Xi Yi Jie He Za Zhi 27, 197–200.
Li, Z. Y., Jiang, Y. M., Liu, Y. M., Guo, Z., Shen, S. N., Liu, X. M., et al. (2014). Saikosaponin D acts against corticosterone-induced apoptosis via regulation of mitochondrial GR translocation and a GR-dependent pathway. Prog. Neuropsychopharmacol. Biol. Psychiatry 53, 80–89. doi: 10.1016/j.pnpbp.2014.02.010
Lin, H. X., Wang, S. L., Wang, Y., and Sun, C. P. (2012). Determination of flavonoids in Bupleurum chinense by HPLC. Chin. J. Exp. Prescript. 18, 76–79.
Liu, X., Latkolik, S., Atanasov, A. G., Kunert, O., Pferschy-Wenzig, E. M., Heiss, E. H., et al. (2017). Bupleurum chinense Roots: A Bioactivity-Guided Approach toward Saponin-Type NF-κB Inhibitors. Planta Med. 83, 1242–1250. doi: 10.1055/s-0043-118226
Liu, Z., Qi, Y., Cheng, Z., Zhu, X., Fan, C., and Yu, S. Y. (2016). The effects of ginsenoside Rg1 on chronic stress induced depression-like behaviors, BDNF expression and the phosphorylation of PKA and CREB in rats. Neuroscience 322, 358–369.
Lopez, J. P., Lim, R., Cruceanu, C., Crapper, L., Fasano, C., Labonte, B., et al. (2014). miR-1202 is a primate-specific and brain-enriched microRNA involved in major depression and antidepressant treatment. Nat. Med. 20, 764–768. doi: 10.1038/nm.3582
Lovinger, D. M., and Abrahao, K. P. (2018). Synaptic plasticity mechanisms common to learning and alcohol use disorder. Learn Mem. 25, 425–434. doi: 10.1101/lm.046722.117
Lu, G. Y., Xing, X. Y., Wang, J. Y., Wang, Y., Ma, K., and Wang, S. J. (2022). Research progress and predictive analysis of quality markers of the classic famous prescription Shenling Baizhu Powder. Chinese J. Trad. Chin. Med. 47, 5171–5181. doi: 10.19540/j.cnki.cjcmm.20220421.201
Lu, L. N., Wang, J. J., Wang, X. L., Liu, Y., Rong, L. X., Guo, Y. Z., et al. (2017). Study on quality control components selection of Angelica sinensis. Western Chin. Med. 30, 22–26.
Luo, H. G., Chen, J. X., Zhang, Q., Yue, G. X., Ding, J., Zhang, H. T., et al. (2013). Comparative study on effects of Xiaoyao Powder and its modified prescription on plasma metabolomics of rats with chronic immobilization stress. Chin. J. Integr. Med. 19, 610–615. doi: 10.1007/s11655-012-1092-0
Lv, Z. W. (2015). Clinical observation on 39 cases of coronary heart disease with depression treated with modified Xiaoyao powder and fluoxetine. Chin. Folk Med. 24, 107–109.
Ma, H. Q., Li, X. H., and Xing, Y. N. (2020). Evaluation of the effect and adverse reaction rate of modified Xiaoyao powder combined with paroxetine in the treatment of depression. Med. Dietother. Health 18, 14–17.
Machaalani, R., and Chen, H. (2018). Brain derived neurotrophic factor (BDNF), its tyrosine kinase receptor B (TrkB) and nicotine. Neurotoxicology 2018, 186–195. doi: 10.1016/j.neuro.2018.02.014
Makhija, K., and Karunakaran, S. (2013). The role of inflammatory cytokines on the aetiopathogenesis of depression. Aust. N. Z. J. Psychiatry 47, 828–839. doi: 10.1177/0004867413488220
Medina-Rodriguez, E. M., Madorma, D., O’Connor, G., Mason, B. L., Han, D., Deo, S. K., et al. (2020). Identification of a signaling mechanism by which the microbiome regulates Th17 cell-mediated depressive-Like behaviors in mice. Am. J. Psychiatry 177, 974–990. doi: 10.1176/appi.ajp.2020.19090960
Meng, J., Chen, X. F., Yang, W. Y., Song, J. H., Zhang, Y., Li, Z. F., et al. (2014). Gaschromatography-mass spectrometry analysis of essential oils from five parts of Chaihu (Radix Bupleuri Chinensis). J. Tradit. Chin. Med. 34, 741–748. doi: 10.1016/s0254-6272(15)30090-x
Moore, L. D., Le, T., and Fan, G. (2013). DNA methylation and its basic function. Neuropsychopharmacology 38, 23–38. doi: 10.1038/npp.2012.112
Muñoz-Llanos, M., García-Pérez, M. A., Xu, X., Tejos-Bravo, M., Vidal, E. A., Moyano, T. C., et al. (2018). MicroRNA profiling and bioinformatics target analysis in dorsal hippocampus of chronically stressed rats: Relevance to depression pathophysiology. Front. Mol. Neurosci. 11:251. doi: 10.3389/fnmol.2018.00251
Nagy, C., Suderman, M., Yang, J., Szyf, M., Mechawar, N., Ernst, C., et al. (2015). Astrocytic abnormalities and global DNA methylation patterns in depression and suicide. Mol. Psychiatry 20, 320–328. doi: 10.1038/mp.2014.21
Neng, J. J., Wang, S. H., Zhang, Y. Y., and Sheng, H. G. (2020). Analysis of blood ingredient of Guizhi fuling formula based on UPLC-TOF-MS. Shandong J. Trad. Chin. Med. 39, 1233–1239.
O’Carroll, A. M., Don, A. L., and Lolait, S. J. (2003). APJ receptor mRNA expression in the rat hypothalamic paraventricular nucleus: Regulation by stress and glucocorticoids. J. Neuroendocrinol. 15, 1095–1101. doi: 10.1046/j.1365-2826.2003.01102.x
Olloquequi, J., Cornejo-Córdova, E., Verdaguer, E., Soriano, F. X., Binvignat, O., and Auladell, C. (2018). Excitotoxicity in the pathogenesis of neurological and psychiatric disorders: Therapeutic implications. J. Psychopharmacol. 32, 265–275. doi: 10.1177/0269881118754680
Orsolini, L., Chiappini, S., Volpe, U., Berardis, D., Latini, R., Papanti, G. D., et al. (2019). Use of medicinal cannabis and synthetic cannabinoids in Post-Traumatic Stress Disorder (PTSD): A systematic review. Medicina 55:525. doi: 10.3390/medicina55090525
Penner-Goeke, S., and Binder, E. B. (2019). Epigenetics and depression. Dialogues Clin. Neurosci. 21, 397–405. doi: 10.31887/DCNS.2019.21.4/ebinder
Perini, G., Ramusino, M., Sinforiani, E., Bernini, S., Petrachi, R., and Costa, A. (2019). Cognitive impairment in depression: Recent advances and novel treatments. Neuropsychiatr. Dis. Treat. 15, 1249–1258. doi: 10.2147/NDT.S199746
Qiu, J. J., Liu, Z., Zhao, P., Wang, X. J., Li, Y. C., Sui, H., et al. (2017). Gut microbial diversity analysis using Illumina sequencing for functional dyspepsia with liver depression-spleen deficiency syndrome and the interventional Xiaoyao powder in a rat model. World J. Gastroenterol. 23, 810–816. doi: 10.3748/wjg.v23.i5.810
Ren, H., Collins, V., Clarke, S. J., Han, J. S., Lam, P., Clay, F., et al. (2012). Epigenetic changes in response to tai chi practice: A pilot investigation of DNA methylation marks. Evid. Based Complement. Alternat. Med. 2012:841810. doi: 10.1155/2012/841810
Saavedra, K., Molina-Márquez, A. M., Saavedra, N., Zambrano, T., and Salazar, L. A. (2016). Epigenetic modifications of major depressive disorder. Int. J. Mol. Sci. 17:1279. doi: 10.3390/ijms17081279
Schroeder, F. A., Lin, C. L., Crusio, W. E., and Akbarian, S. (2007). Antidepressant-like effects of the histone deacetylase inhibitor, sodium butyrate, in the mouse. Biol. Psychiatry. 62, 55–64. doi: 10.1016/j.biopsych.2006.06.036
Shen, Y. P., Li, J., and Jia, X. B. (2012). Research progress on chemical constituents of Poria cocos. J. Nanjing Univ. Trad. Chin. Med. 28, 297–300.
Shi, C. F., Zhang, M., Li, Y., Jin, Q. Y., and Zhan, L. (2018). Epigenetic mechanism of proanthocyanidins on the improvement of cognitive function in depressed mice. J. Logist. Coll. Chin. Peoples Armed Police Force 27, 889–893.
Shu, X. K., Duan, W. J., Liu, F., Shi, X. G., Geng, Y. L., Wang, X., et al. (2014). Preparative separation of polyphenols from the flowers of Paeonia lactiflora Pall by high-speed counter-current chromatography. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 94, 62–67. doi: 10.1016/j.jchromb.2013.12.004
Su, G. Y., Yang, J. Y., Wang, F., Ma, J., Zhang, K., Dong, Y. X., et al. (2014). Antidepressant-like effects of Xiaochaihutang in a rat model of chronic unpredictable mild stress. J. Ethnopharmacol. 152, 217–226.
Sui, C., Han, W. J., Zhu, C. R., and Wei, J. H. (2021). Recent progress in saikosaponin biosynthesis in bupleurum. Curr. Pharm. Biotechnol. 22, 329–340. doi: 10.2174/1389201021999200918101248
Sun, Q., Guo, W., Jian, D., Ma, H. M., Ma, R., and Chen, H. (2018a). Effect of Xiaoyao powder on the expression of Npas2 gene in hippocampus of chronic stress rats and its mechanism of DNA methylation modification. N. Chin. Med. Clin. Pharmacol. 29, 421–427.
Sun, Q., Guo, W., Jiang, D., Ma, H. M., Ma, R., and Chen, H. (2018b). Preliminary study on the expression of Stk32c gene in hippocampus of chronic stress rats and the epigenetic mechanism of Xiaoyao Powder intervention. Shizhen Trad. Chin. Med. 29, 776–780.
Sun, R., Wang, K., Wu, D., Li, X. Y., and Ou, Y. B. (2012). Protective effect of paeoniflorin against glutamate-induced neurotoxicity in PC12 cells via Bcl-2/Bax signal pathway. Folia Neuropathol. 50, 270–276. doi: 10.5114/fn.2012.30527
Sun, S. L., Yang, L. P., Zhang, H. R., and Wu, Y. S. (2016). Effect of Xiaoyao powder on depression in breast cancer patients undergoing postoperative chemotherapy. Chin. J. Trad. Chin. Med. 31, 1499–1502.
Sun, Y. L., Shen, R. L., Cai, B. Y., and Tang, J. (2005). Classification preparation and composition analysis of angelica polysaccharide. J. Henan Univ. Technol. 2, 40–47. doi: 10.16433/j.cnki.issn1673-2383.2005.02.011
Tanaka, R., Yamazaki, M., Hasada, K., and Nagatsu, A. (2013). Application of quantitative 1H-NMR method to determination of paeoniflorin in Paeoniae radix. J. Nat. Med. 67, 657–661. doi: 10.1007/s11418-012-0711-6
Tang, N. L., Shi, J., and Huang, D. M. (2019). Effect of electroacupuncture combined with Xiaoyao Powder on serum ACTH and CORT in Perimenopausal patients with mild and moderate depression. J. Guangxi Univ. 44, 587–592.
Tian, J. S., Zuo, Y. M., Zhou, Y. Z., Gao, X. X., and Qin, X. M. (2015). UPLC-PDA fingerprint of supercritical CO2 extract of Xiaoyao powder and content determination of characteristic components. Chin. J. Pharm. Ind. 46, 473–476.
Wan, X. M., Zhou, R., Huang, X. T., Kou, M. J., and Zou, X. J. (2020). Effects of Xiaoyao Powder on IL-6 and TNF-α in hippocampus of chronic and unpredictable mild stress induced by liver depression and spleen deficiency in rats. J. Liaoning Univ. Trad. Chin. Med. 22, 47–51.
Wang, C. D., Wu, C. L., Yan, Z. G., and Cheng, X. (2019). Ameliorative effect of Xiaoyao-jieyu-powder on post-stroke depression and its potential mechanisms. J. Nat. Med. 73, 76–84. doi: 10.1007/s11418-018-1243-5
Wang, N. (2020). Clinical observation on the treatment of 30 cases of mild to moderate depression due to liver depression and spleen deficiency with Xiaoyao Powder and Banxia Houpu Decoction combined with droperidol and melitracin tablets. J. Gansu Univ. Trad. Chin. Med. 37, 57–60.
Wang, P., Zhao, Y. N., Xu, R. Z., Zhang, X. W., Sun, Y. R., Feng, Q. M., et al. (2022). Sesquiterpene lactams and lactones with antioxidant potentials From Atractylodes macrocephala discovered by molecular networking strategy. Front. Nutr. 9:865257. doi: 10.3389/fnut.2022.865257
Wang, R. J., Zhou, G. S., Wang, M. Y., Peng, Y., and Li, X. B. (2014). The metabolism of polysaccharide from Atractylodes macrocephala koidz and its effect on intestinal microflora. Evid. Based Complement. Alternat. Med. 2014:926381. doi: 10.1155/2014/926381
Wang, W. H., Dong, H. J., Yan, R. Y., Li, H., Li, P. Y., Chen, P., et al. (2015). Comparative study of lanostane-type triterpene acids in different parts of Poria cocos (Schw.) Wolf by UHPLC-Fourier transform MS and UHPLC-triple quadruple MS. J. Pharm. Biomed. Anal. 102, 203–214. doi: 10.1016/j.jpba.2014.09.014
Wei, F. X., Liu, H. L., Fan, Y. H., Li, X. Q., Zhao, S. J., Qin, X. M., et al. (2021). Based on network pharmacology, the mechanism of Xiaoyao Powder’s “treating different diseases together” depression, mammary hyperplasia and functional dyspepsia. Chin. J. Trad. Chin. Med. 46, 4230–4237.
Wienholz, B. L., Kareta, M. S., Moarefi, A. H., Gordon, C. A., Ginno, P. A., and Chédin, F. (2010). DNMT3L modulates significant and distinct flanking sequence preference for DNA methylation by DNMT3A and DNMT3B in vivo. PLoS Genet. 6:e1001106. doi: 10.1371/journal.pgen.1001106
Woron, J., Siwek, M., and Gorostpwicz, A. (2019). Adverse effects of interactions between antidepressants and medications used in treatment of cardiovascular disorders. Psychiatr. Pol. 53, 977–995. doi: 10.12740/PP/OnlineFirst/96286
Wu, L. L., Liu, Y., Yan, C., Pan, Y., Su, J. F., and Wu, W. K. (2016). Antidepressant-like effects of fractions prepared from Danzhi-Xiaoyao powder decoction in rats with chronic unpredictable mild stress: Effects on hypothalamic-pituitary-adrenal axis, arginine vasopressin, and neurotransmitters. Evid. Based Complement. Alternat. Med. 2016:6784689. doi: 10.1155/2016/6784689
Xiao, F. (2021). Clinical effect of Xiaoyao Powder combined with paroxetine in adjuvant treatment of depression after breast cancer surgery. J. Clin. Rational Drug Use 14, 78–80.
Xu, M., Xu, Z., Xu, Q., Zhang, H., Liu, M., Geng, F., et al. (2018). UPLC-MS/MS method for the determination of 14 compounds in rat plasma and its application in a pharmacokinetic study of orally administered Xiaoyao powder. Molecules 23:2514. doi: 10.3390/molecules23102514
Xu, Y., Ku, B. S., Yao, H. Y., Lin, Y. H., Ma, X., Zhang, Y. H., et al. (2005). Antidepressant effects of curcumin. Clin. Rehabil. China 44, 162–164.
Yan, Z., Jiao, H., Ding, X., Ma, Q., Li, X., and Pan, Q. (2018). Xiaoyao powder improves depressive-like behaviors in mice through regulating apelin-APJ system in hypothalamus. Molecules 23:1073. doi: 10.3390/molecules23051073
Yang, J., Gao, F., Zhang, Y., Liu, Y., and Zhang, D. (2015). Buyang Huanwu Decoction (BYHWD) enhances angiogenic effect of mesenchymal stem cell by upregulating VEGF expression after focal cerebral ischemia. J. Mol. Neurosci. 56, 898–906. doi: 10.1007/s12031-015-0539-0
Yang, P. F., Liu, C., Wang, H. Q., Li, J. C., Wang, Z. Z., Xiao, W., et al. (2014). Studies on the chemical constituents of Poria cocos. Chin. J. Trad. Chin. Med. 39, 1030–1033.
Yin, F., Zheng, J., Kang, X. P., Zhang, L. N., and Jin, G. Q. (2017). The mechanism of changes in the expression of learning and memory-related gene egr1 in aged rats and the adjustment effect of Bushen Yiqi Recipe. Chin. J. Geriatr. 37, 4689–4691.
Yu, L., Xuan, Z. Z., Wu, S. W., Wu, Y. F., Wu, B. F., Xu, Y., et al. (2017). Effects of Jiawei Xiaoyao Powder on behavior and expression of inflammatory cytokines in hippocampus of depressed rats. N. Chin. Med. 49, 9–13.
Yu, X. P., Zhang, Y., and Ling, W. H. (2006c). The role of methylated CpG-binding protein families (MeCPs) in epigenetics. Int. J. Genet. 3, 196–200.
Yu, L. J., Zhang, Y. P., Ma, R., Bao, L., Fang, J. Z., and Yu, T. X. (2006a). Potent protection of ferulic acid against excitotoxic effects of maternal intragastric administration of monosodium glutamate at a late stage of pregnancy on developing mouse fetal brain. Eur. Neuropsychopharmacol. 16, 170–177. doi: 10.1016/j.euroneuro.2005.08.006
Yu, L. J., Zhang, Y. P., and Ma, R. D. (2006b). Potent protection of fernlic acid against excitotoxic effects of maternal intragastrie administration of monosodium glutamate at a late stage of pregnancy on developing mouse fetal brain. Eur. Neuropsychopharmacol. 16, 170–177.
Yuan, J. M., Pei, Q. H., Qu, M., and Zheng, Q. (2022). Clinical effect of Xiaoyao powder modified formula on depression of liver depression and spleen deficiency. China Med. Herald 19, 7–22.
Zhang, B., Li, Y., Xin, T., Wang, H., Li, H., and Wang, S. X. (2022). Research progress in the treatment of depression with Xiaoyao Powder. Chin. J. Exp. Prescript. 28, 273–282. doi: 10.13422/j.cnki.syfjx.20221229
Zhang, H., Xue, X., Pan, J., Song, X., Chang, X., Mao, Q., et al. (2021). Integrated analysis of the chemical-material basis and molecular mechanisms for the classic herbal formula of Lily Bulb and Rehmannia Decoction in alleviating depression. Chin. Med. 16:107. doi: 10.1186/s13020-021-00519-x
Zhang, J. D., Cao, G., Xia, Y. H., Wen, C. P., and Fan, Y. S. (2014). Fast analysis of principal volatile compounds in crude and processed Atractylodes macrocephala by an automated static headspace gas chromatography-mass spectrometry. Pharmacogn. Mag. 10, 249–253. doi: 10.4103/0973-1296.137364
Zhang, L. B., Lv, J. L., and Liu, J. W. (2016). Phthalide derivatives with anticoagulation activities from Angelica sinensis. J. Nat. Prod. 79, 1857–1861. doi: 10.1021/acs.jnatprod.6b00080
Zhang, S., Lu, Y. J., Chen, W., Shi, W., Zhao, Q., Zhao, J. J., et al. (2021). Network pharmacology and experimental evidence: PI3K/AKT signaling pathway is involved in the antidepressive roles of Chaihu Shugan San. Drug Des. Devel. Ther. 15, 3425–3441. doi: 10.2147/DDDT.S315060
Zhang, S. H., Liu, X. D., Sun, M. Z., Zhang, Q., Li, T., Li, X., et al. (2018). Reversal of reserpine-induced depression and cognitive disorder in zebrafish by sertraline and Traditional Chinese Medicine (TCM). Behav. Brain Funct 14:13. doi: 10.1186/s12993-018-0145-8
Zhang, W. J., Yang, K., You, C. X., Wang, C. F., Geng, Z. F., Su, Y., et al. (2015). Contact toxicity and repellency of the essential oil from mentha haplocalyx briq. against Lasioderma serricorne. Chem. Biodivers. 12, 832–839. doi: 10.1002/cbdv.201400245
Zhang, X., Liao, M. N., Zhang, Y. P., Bao, H., Nie, J., Zhang, G. Y., et al. (2007). Study on the antidepressant effect of sodium ferulate. Chin. Behav. Med. Sci. 16, 595–596.
Zhang, Y. F., Gao, X. S., Wang, A. N., Du, Y., Wang, Y. Z., Li, L., et al. (2019). Preliminary study on the ingredient of Chaihu Shugan powder. J. Mod. Integr. Trad. Chin. Western Med. 28, 3193–3206.
Zhang, Y. P., Yu, L. J., and Ma, R. D. (2008). Potent protective effects of ferulic acid on glutamate-induced neurotoxicity in adult mice. Chin. Neural Med. 7, 596–599.
Zhao, S. L., Fu, F., Yu, B. Y., and Li, R. S. (2023). Analysis of 12 chemical compounds and pattern recognition of different parts of Angelicae sinensis radix by liquid chromatography-tandem mass spectrometry and chemometrics methods. J. Chromatogr. Sci. 61, 103–109. doi: 10.1093/chromsci/bmac098
Zhao, Y., Shi, Y. Y., Yang, H. X., and Mao, L. J. (2016). Extraction of Angelica sinensis polysaccharides using ultrasound-assisted way and its bioactivity. Int. J. Biol. Macromol. 88, 44–50. doi: 10.1016/j.ijbiomac.2016.01.113
Zhao, Z. Y., Wang, W. X., and Guo, H. Z. (2006). Antidepressant effect of liquiritin on chronic stress depression model rats. China Clin. Rehabil. 27, 69–72.
Zheng, Q., Kong, X. W., and Sun, W. J. (2021). The clinical efficacy of Xiaoyaosan in the treatment of mixed anxiety and depression disorder of liver depression and spleen deficiency type [J]. Clin. Drug Ther. J. 19, 60–64.
Zheng, Q. J. (2021). Clinical effect of Xiaoyao powder combined with sertraline on post-stroke depression. J. Clin. Rat. Drug Use 14, 65–67.
Zheng, W., Shi, H. Y., Wang, P., Wang, S. L., Cai, M. C., and Xu, N. (2022). Analysis of chemical components and blood components of banxia baizhu tianma decoction based on UPLC-Q-Orbitrap-HRMS. Chin. Hosp. Pharm. J. 42, 2331–2339.
Zhou, C. Q., and Wang, X. K. (2017). Rapid determination of isomeric benzoylpaeoniflorin and benzoylalbiflorin in rat plasma by LC-MS/MS method. Int. J. Anal. Chem. 2017:1693464. doi: 10.1155/2017/1693464
Zhou, L., Wang, T., Yu, Y. W., Li, M. A., Sun, X. H., Song, W. H., et al. (2022). The etiology of poststroke-depression: A hypothesis involving HPA axis. Biomed. Pharmacother. 151:113146. doi: 10.1016/j.biopha.2022.113146
Zhou, Y., Huang, S., Wu, F., Zheng, Q., Zhang, F., Luo, Y., et al. (2021). Atractylenolide III reduces depressive- and anxiogenic-like behaviors in rat depression models. Neurosci. Lett. 759:136050. doi: 10.1016/j.neulet.2021.136050
Zhu, H. Z., Liang, Y. D., Ma, Q. Y., Hao, W. Z., Li, X. J., Wu, M. S., et al. (2019). Xiaoyao powder improves depressive-like behavior in rats with chronic immobilization stress through modulation of the gut microbiota. Biomed. Pharmacother. 112:108621.
Zhu, J., Luo, C., Wang, P., He, Q., Zhou, J., and Peng, H. (2013). Saikosaponin A mediates the inflammatory response by inhibiting the MAPK and NF-κB pathways in LPS-stimulated RAW 264.7 cells. Exp. Ther. Med. 5, 1345–1350.
Keywords: Xiaoyao Powder, depression, clinical application, pharmacological mechanisms, epigenetics, quality markers
Citation: Wang J, Wu Q, Ou C, Lu G and Yu H (2023) Research on Xiaoyao Powder in the treatment of depression based on epigenetics and quality markers. Front. Neurosci. 17:1223451. doi: 10.3389/fnins.2023.1223451
Received: 16 May 2023; Accepted: 26 July 2023;
Published: 24 August 2023.
Edited by:
Zulqarnain Baloch, Kunming University of Science and Technology, ChinaReviewed by:
Vivek Puri, Chitkara University, Himachal Pradesh, IndiaBechan Sharma, University of Allahabad, India
Copyright © 2023 Wang, Wu, Ou, Lu and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Guangying Lu, NjAwMjAyMTFAc2R1dGNtLmVkdS5jbg==; Huayun Yu, MDEwMDAwMjlAc2R1dGNtLmVkdS5jbg==
 Jiayun Wang
Jiayun Wang Qiaolan Wu
Qiaolan Wu Guangying Lu
Guangying Lu Huayun Yu
Huayun Yu