- 1Yilong County Hospital of Traditional Chinese Medicine, Nanchong, Sichuan, China
- 2Department of Rehabilitation Medicine, West China Second University Hospital, Sichuan University, Chengdu, China
- 3School of Health Preservation and Rehabilitation, Chengdu University of Traditional Chinese Medicine, Chengdu, China
- 4Integrated Traditional Chinese and Western Medicine Hospital of Panzhihua City, Panzhihua, China
Background: The evidence for the effectiveness of acupuncture for patients with carpal tunnel syndrome (CTS) is insufficient. Therefore, this systematic review and meta-analysis aimed to evaluate the effectiveness of acupuncture on CTS through a comprehensive literature search.
Methods: English and Chinese databases were searched from their inceptions until 27 October 2022 to collect randomized controlled trials (RCTs) that investigated the effect of acupuncture on CTS. Two reviewers independently selected studies that met the eligibility criteria, extracted the required data, assessed the risk of bias using version 2 of the Cochrane risk-of-bias tool for randomized trials (ROB 2), and evaluated the quality of reporting for acupuncture interventions using the Revised Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA). The primary outcomes were symptom severity and functional status, while secondary outcomes included pain intensity, responder rate, and electrophysiological parameters. Review Manager software (version 5.4.1) was used for data analysis. The certainty of the evidence was rated with GRADEpro (version 3.6) software.
Results: We included 16 RCTs with a total of 1,025 subjects. The overall risk of bias was rated as low in one RCT, some concerns in 14, and high in one. Compared with night splints, acupuncture alone was more effective in relieving pain, but there were no differences in symptom severity and functional status. Acupuncture alone had no advantage over medicine in improving symptom severity and electrophysiological parameters. As an adjunctive treatment, acupuncture might benefit CTS in terms of symptom severity, functional status, pain intensity, and electrophysiological parameters, and it was superior to medicine in improving the above outcomes. Few acupuncture-related adverse events were reported. The above evidence had a low or very low degree of certainty.
Conclusion: Acupuncture as an adjunctive treatment may be effective for patients with CTS. Additionally, more rigorous studies with objective outcomes are needed to investigate the effect of acupuncture in contrast with sham acupuncture or other active treatments.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=329925, identifier CRD42022329925.
1. Introduction
Carpal tunnel syndrome (CTS), the common peripheral nerve entrapment syndrome, is caused by compression of the median nerve at the level of the wrist. The prevalence of CTS is 1–5% in the general population (Atroshi et al., 1999) and 7–10% in the working-age population (Spahn et al., 2012b; Feng et al., 2021). CTS can occur in one or both hands and is characterized by pain, numbness, and tingling in the median nerve distribution. In advanced cases, muscle atrophy may develop (Wipperman and Goerl, 2016). Being female, being obese, having to overuse the wrists, those who are pregnant, and those who are in perimenopausal age pose a greater risk of being affected by CTS (Spahn et al., 2012a; Graham et al., 2016). Patients with CTS frequently awaken from sleep due to worsening symptoms and have a lower quality of life. In addition, CTS is associated with reduced work time, decreased productivity, and disability (Daniell et al., 2009). Patients with CTS miss an average of 27 days of work per year, and the costs of CTS are estimated to exceed $2 billion annually in the United States (Palmer and Hanrahan, 1995).
Treatment strategies for CTS include non-surgical and surgical approaches. Given the invasive nature of the surgery, patients with CTS prefer to choose non-surgical management as an initial treatment (Shi and MacDermid, 2011; Calandruccio and Thompson, 2018). According to the American Academy of Orthopaedic Surgeons (AAOS) (Graham et al., 2016), there are various non-surgical treatments for CTS, such as immobilization (brace/splint/orthosis), steroid injections, and oral steroids. However, the evidence for the effectiveness of these non-surgical approaches is insufficient (Page et al., 2012; Padua et al., 2016). Moreover, certain undesirable adverse reactions limit the usage of treatments, such as splints and braces, which may influence sleep when used nightly (Manente et al., 2001), and steroid injections, which can lead to skin thinning, changes in pigmentation, and other adverse reactions (Chesterton et al., 2018). Therefore, it is necessary to explore effective and safe non-surgical interventions for patients with CTS.
Acupuncture is gaining popularity and acceptance worldwide and is widely used in neuro-musculoskeletal disorders (Qiao et al., 2020). Randomized controlled trials (RCTs) have investigated the effect of acupuncture as a monotherapy or adjuvant intervention on CTS, but their findings have been inconsistent. Previous systematic reviews of acupuncture for CTS were conducted by Sim et al. (2011) (6 RCTs), Choi et al. (2018) (12 RCTs), and Wu et al. (2020) (10 RCTs), and these systematic reviews suggested that there was not sufficient and convincing evidence to support the effectiveness of acupuncture on CTS. To further investigate this, we updated the systematic review and meta-analysis to include more objective outcomes and recent RCTs.
2. Methods and analysis
2.1. Study registration
We registered this systematic review and meta-analysis at PROSPERO: https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=329925 (Registration ID: CRD42022329925). This systematic review and meta-analysis was conducted according to A Measurement Tool to Assess Systematic Reviews (AMSTAR 2) (Shea et al., 2017) and reported in light of the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) 2020 statement (Page et al., 2021).
2.2. Inclusion criteria
We included studies that met all of the following criteria:
2.2.1. Type of studies
Our systematic review and meta-analysis included RCTs that evaluated the effectiveness of acupuncture in treating CTS and were published in either English or Chinese.
2.2.2. Type of participants
Our study included adult patients (≥18 years old) with CTS diagnosed using electrophysiological assessment (e.g., nerve conduction studies) and/or a combination of symptoms history and physical examination (as per Erickson et al., 2019). There were no limitations on gender, ethnicity, severity, or duration of CTS among the study participants.
2.2.3. Types of interventions
Experimental group: acupuncture alone or acupuncture plus other treatment(s) (e.g., wrist splinting, drugs, corticosteroid injection, and other non-traditional Chinese medicine). There were no restrictions on the types of acupuncture.
Control group: no treatment, sham acupuncture alone, other treatment, or sham acupuncture combined with other treatment(s).
Presence of cointerventions: cointerventions were required to be equal between the experimental and control groups.
2.2.4. Types of outcomes
2.2.4.1. Primary outcomes
Primary outcomes were symptom severity and functional status. Symptom severity was measured using the Boston Carpal Tunnel Questionnaire’s symptom severity scale (CTQ-SSS) and the global symptoms score (GSS), while functional status was assessed with the CTQ’s functional status scale (CTQ-FSS) and the disabilities of the arm, shoulder, and hand questionnaire (DASH).
2.2.4.2. Secondary outcomes
Secondary outcomes included the following:
(1) Pain intensity: the visual analog scale (VAS) or the numerical rating scale (NRS)
(2) Electrophysiological parameters: compound muscle action potential (CMAP), sensory nerve action potential (SNAP), distal motor latency (DML), distal sensory latency (DSL), motor nerve conduction velocity (MNCV), and sensory nerve conduction velocity (SNCV)
(3) Responder rate: responder (symptom improved or greatly improved) and non-responder (symptom did not change or worsened); and
(4) Adverse events.
2.3. Exclusion criteria
Studies were excluded if they met one of the following conditions:
(1) Studies including patients with CTS from a special population, such as those with diabetes, who were pregnant, and those with rheumatoid arthritis
(2) Patients who had surgery for CTS
(3) Experimental and/or control group included other interventions of traditional Chinese medicine (e.g., Tuina and Chinese herbs)
(4) Studies that provided no details of control intervention
(5) Studies with duplicate data; and
(6) If full texts were unavailable through all practical approaches.
2.4. Search strategy
The following databases were searched from their inceptions until 27 October 2022: PubMed, EMbase, the Cochrane Library, the Chinese Biomedical Literature Database (CBM), the China National Knowledge Infrastructure (CNKI), the Chinese Science and Technology Periodical Database (VIP), and the Wanfang database (Wanfang Data). We utilized Medical Subject Headings (MESH) and free terms related to acupuncture and CTS to build search strategies. The search strategies for the above databases are provided in Supplementary material 1. We manually searched gray literature, reference lists of relevant reviews, and trial registers (ClinicalTrials.gov and the Chinese Clinical Trials Registry). Meanwhile, relevant experts were consulted for potentially eligible studies.
2.5. Study selection
EndNote X9 was used to manage the literature. Two independent reviewers (PY and GC) conducted the study selection. After removing duplicates, irrelevant records which were screened according to titles or abstracts were excluded. Then, the rest records with full text were scrutinized to identify eligible studies. The two reviewers cross-checked their identified studies and discussed any disputes.
2.6. Data extraction
The data on the following aspects were extracted by two reviewers (JL and JD) independently:
(1) Study’s information: first author, year of publication, country, sample size, and information related to the risk of bias (e.g., randomization and blinding)
(2) Participants’ (study level) characteristics: age, gender, diagnostic criteria, duration, and severity of CTS
(3) Experimental group’s details: protocol of acupuncture (type, acupoint selection, frequency, duration, etc.) and/or other cointervention(s) (type, frequency, duration, etc.)
(4) Control group’s details: protocol of comparators and/or other cointervention(s) (type, frequency, duration, etc.); and
(5) Outcomes’ information: primary and secondary outcomes, adverse events.
If there are multiple-arm RCTs, we included only data from the arms with interventions relevant to this study. Two reviewers cross-checked the extracted information. Any discrepancy was resolved through discussion. The authors would be contacted if there was missing information.
2.7. Assessment of risk of bias
Two independent reviewers (QD and XL) assessed the risk of bias in the included studies using version 2 of the Cochrane risk-of-bias tool for randomized trials (ROB 2). According to ROB 2, five domains of bias were evaluated: the randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result. Each domain of individual study and all included studies were rated as “low risk,” “some concerns,” or “high risk.” Any disagreements were resolved with a third reviewer (RJ).
2.8. Assessment of the reporting quality of the intervention
Two independent reviewers (HF and QD) utilized the Revised Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA) to evaluate the reporting quality of interventions for each included study based on the following six items (17 sub-items) (MacPherson et al., 2010): acupuncture rationale, details of needling, treatment regimen, other components of treatment, practitioner background, and control or comparator interventions. The third reviewer (RJ) participated in resolution of discrepancies.
2.9. Certainty of evidence assessment
Two independent reviewers (FW and YY) assessed the certainty of the evidence with the GRADE (Grading of Recommendations Assessment, Development, and Evaluation) system. Each outcome was assessed based on five aspects: limitations, inconsistency, indirectness, imprecision, and publication bias, and categorized as high, moderate, low, or very low evidential certainty. GRADEpro (Version 3.6) software was used to evaluate the evidence and summarize the findings.
2.10. Data analysis
We evaluated acupuncture’s effects as monotherapy and adjunctive treatment, respectively. If feasible, meta-analyses were conducted using post-intervention data when clinical homogeneity existed between studies. We calculated the mean difference (MD) with 95% confidence intervals (CIs) for continuous data measured by uniform standards. Otherwise, standardized mean differences (SMDs) and 95% CIs were evaluated. For dichotomous data (e.g., responder rate), we calculated the risk ratios (RRs) and 95% CIs. The Chi-square test with a significance level of P < 0.10 and I2 statistic were used to detect and quantify heterogeneity, respectively. The random-effects model (REM) was applied in meta-analyses if there was substantial heterogeneity (P < 0.1 or I2 value >50%). Otherwise, the fixed-effects model (FEM) was used. We conducted descriptive analyses when meta-analyses were not appropriate or possible. Review Manager software (version 5.4.1) was used for data synthesis.
3. Results
3.1. Study inclusion and characteristics
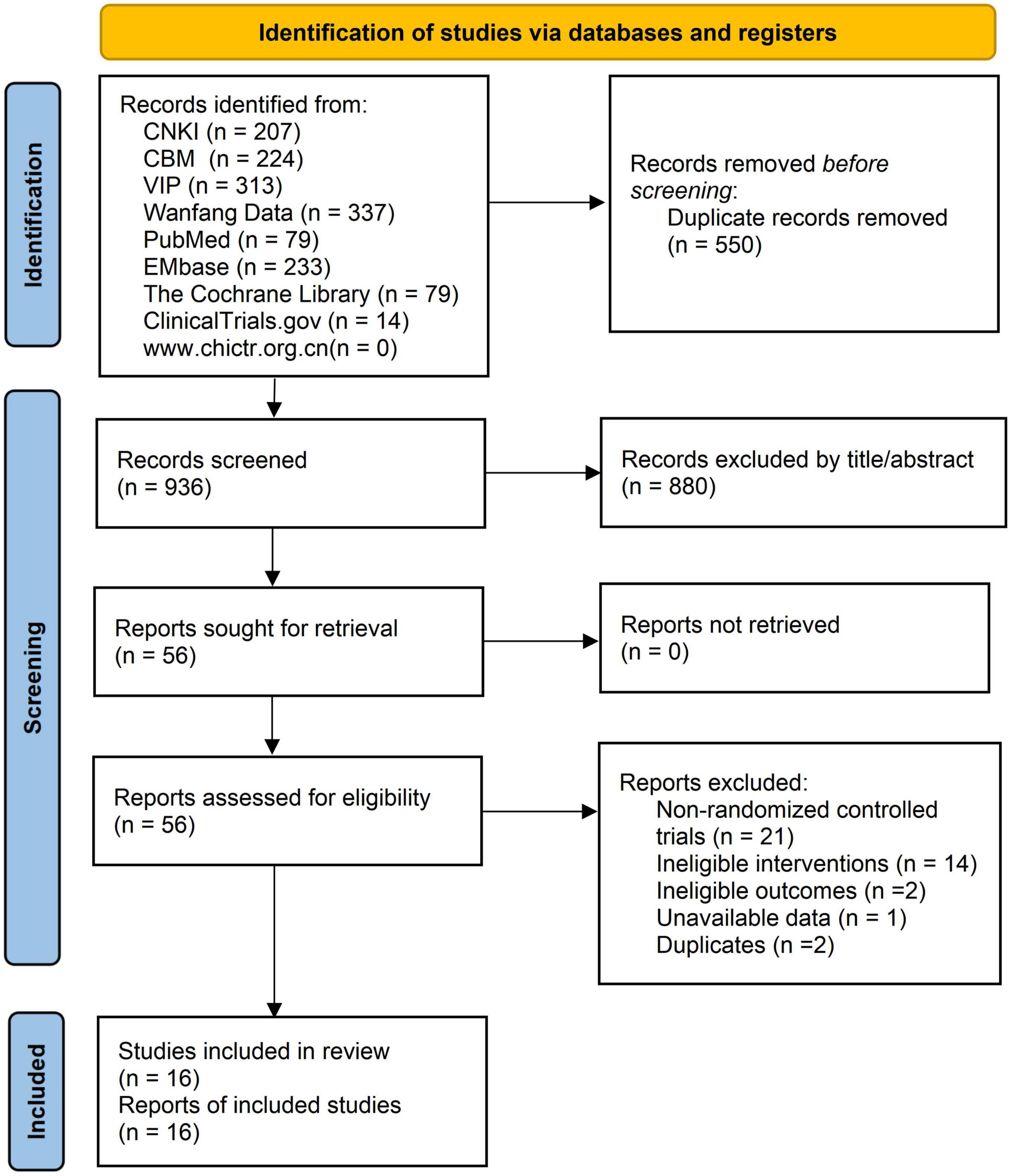
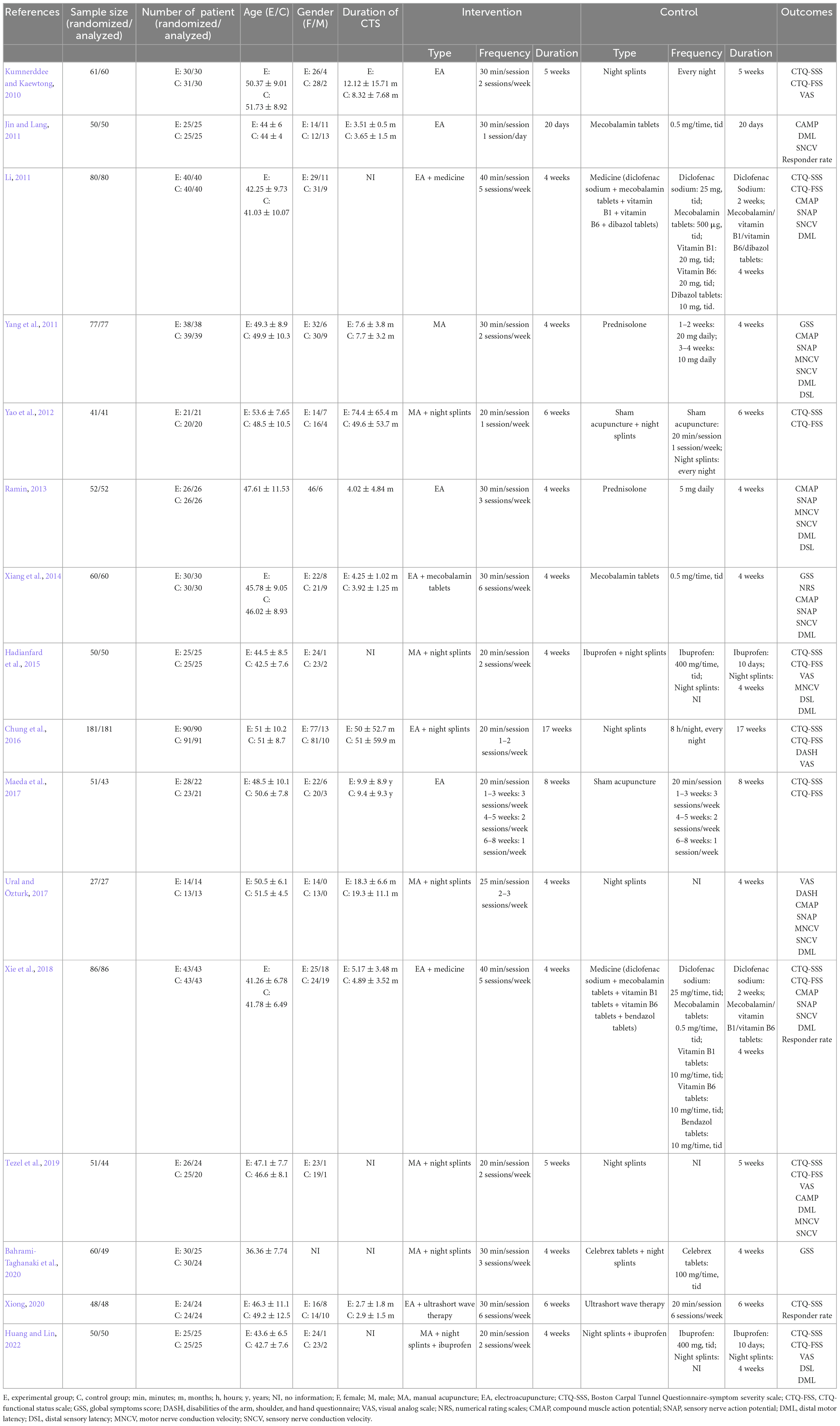
We obtained a total of 1,486 records in the literature search. After removing 550 duplicates, we excluded 880 irrelevant records based on their title and abstract. The full text of 56 remaining records was then evaluated, and 16 eligible studies (Kumnerddee and Kaewtong, 2010; Jin and Lang, 2011; Li, 2011; Yang et al., 2011; Yao et al., 2012; Ramin, 2013; Xiang et al., 2014; Hadianfard et al., 2015; Chung et al., 2016; Maeda et al., 2017; Ural and Özturk, 2017; Xie et al., 2018; Tezel et al., 2019; Bahrami-Taghanaki et al., 2020; Xiong, 2020; Huang and Lin, 2022) were included in the final analysis. A list of excluded records with reasons is provided in Supplementary material 2. The PRISMA flow chart presents the selection procedure (Figure 1). Of the included studies, eight were conducted in China (Jin and Lang, 2011; Li, 2011; Yang et al., 2011; Xiang et al., 2014; Chung et al., 2016; Xie et al., 2018; Xiong, 2020; Huang and Lin, 2022), two in the USA (Yao et al., 2012; Maeda et al., 2017), three in Iran (Ramin, 2013; Hadianfard et al., 2015; Bahrami-Taghanaki et al., 2020), two in Turkey (Ural and Özturk, 2017; Tezel et al., 2019), and one in Thailand (Kumnerddee and Kaewtong, 2010). The sample size of the studies ranged from 27 to 181, with a total of 1,025 participants. The mean age of participants varied between 36.4 and 53.6 years. Fifteen studies included patients with mild to moderate CTS, and one study (Jin and Lang, 2011) did not specify the severity of CTS. Five studies used acupuncture as monotherapy, while 11 studies investigated its adjunctive effect. Table 1 show the characteristics of the included studies.
3.2. Risk of bias
During the randomization process, 11 studies specified the randomization method (Kumnerddee and Kaewtong, 2010; Yang et al., 2011; Yao et al., 2012; Xiang et al., 2014; Hadianfard et al., 2015; Chung et al., 2016; Maeda et al., 2017; Ural and Özturk, 2017; Xie et al., 2018; Tezel et al., 2019; Bahrami-Taghanaki et al., 2020). Two studies (Yang et al., 2011; Chung et al., 2016) implemented appropriate methods to conceal the allocation sequence. All studies reported that there were comparable baselines between groups. Two studies (Yao et al., 2012; Maeda et al., 2017) blinded patients by conducting sham comparisons between the groups. Additionally, several outcomes, including symptom severity, functional status, and pain intensity, were participant-reported outcomes, which meant outcome assessors were blinded in the studies (Yao et al., 2012; Maeda et al., 2017). Seven studies (Kumnerddee and Kaewtong, 2010; Yang et al., 2011; Yao et al., 2012; Chung et al., 2016; Maeda et al., 2017; Tezel et al., 2019; Bahrami-Taghanaki et al., 2020) described dropouts rate with 1.6–18.3%; among these studies, four trials (Chung et al., 2016; Maeda et al., 2017; Tezel et al., 2019; Bahrami-Taghanaki et al., 2020) did not give the detailed reason of dropouts, and three studies (Yang et al., 2011; Yao et al., 2012; Chung et al., 2016) used intent-to-treat analysis. Four trials (Yang et al., 2011; Chung et al., 2016; Maeda et al., 2017; Bahrami-Taghanaki et al., 2020) provided the registration number or published protocol, and all of them reported planned outcomes. Overall, 1 RCT (Yang et al., 2011) was rated as having a low risk of bias, 14 (Kumnerddee and Kaewtong, 2010; Jin and Lang, 2011; Li, 2011; Yao et al., 2012; Ramin, 2013; Xiang et al., 2014; Hadianfard et al., 2015; Chung et al., 2016; Maeda et al., 2017; Ural and Özturk, 2017; Xie et al., 2018; Tezel et al., 2019; Xiong, 2020; Huang and Lin, 2022) had some concerns, and 1 (Bahrami-Taghanaki et al., 2020) was a high risk of bias. The results of the risk of bias in individual studies and the overall risk of bias are shown in Figure 2.
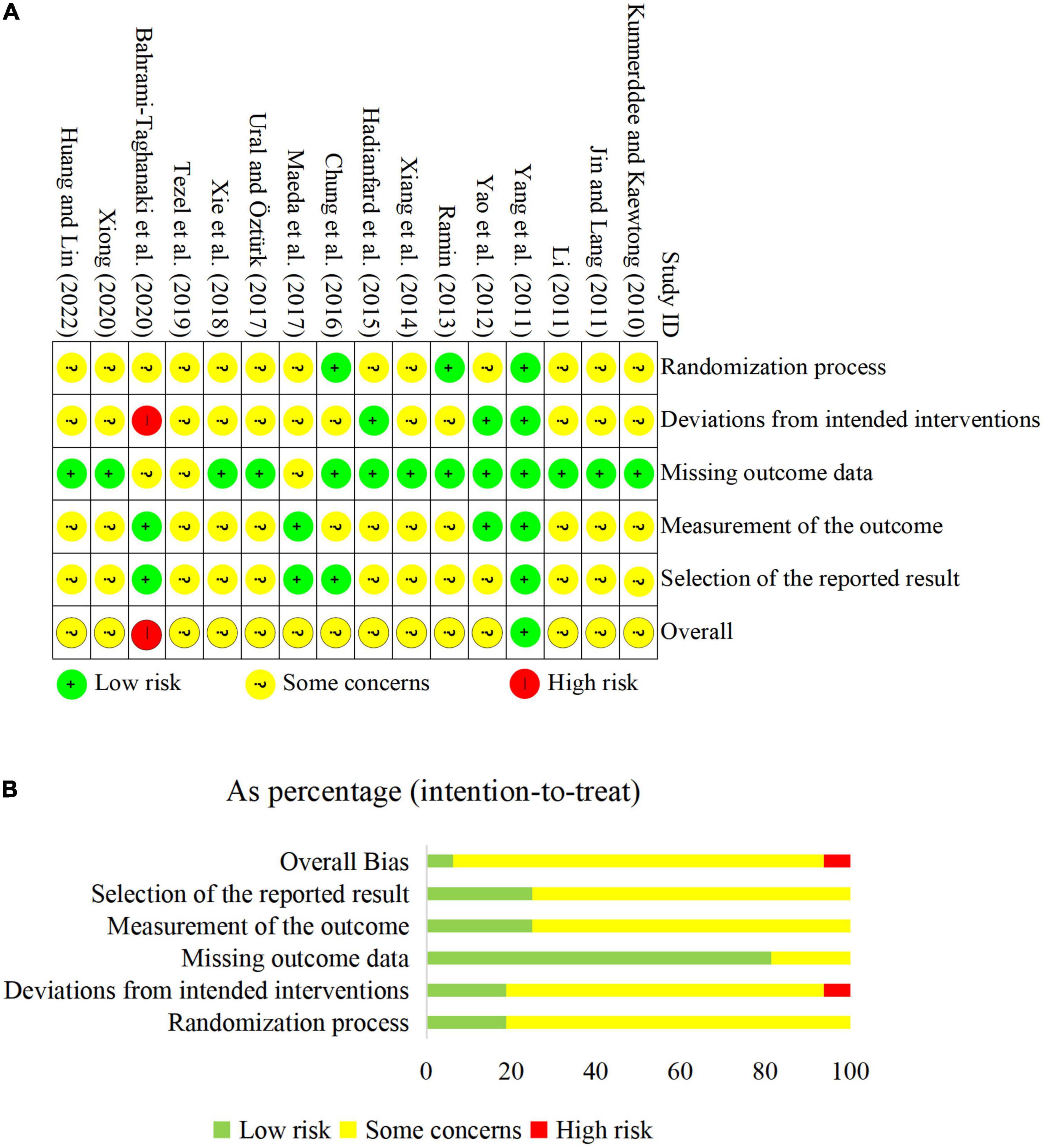
Figure 2. The results of risk of bias assessment. (A) Risk of bias of individual study; (B) overall risk of bias.
3.3. Acupuncture protocols included trials
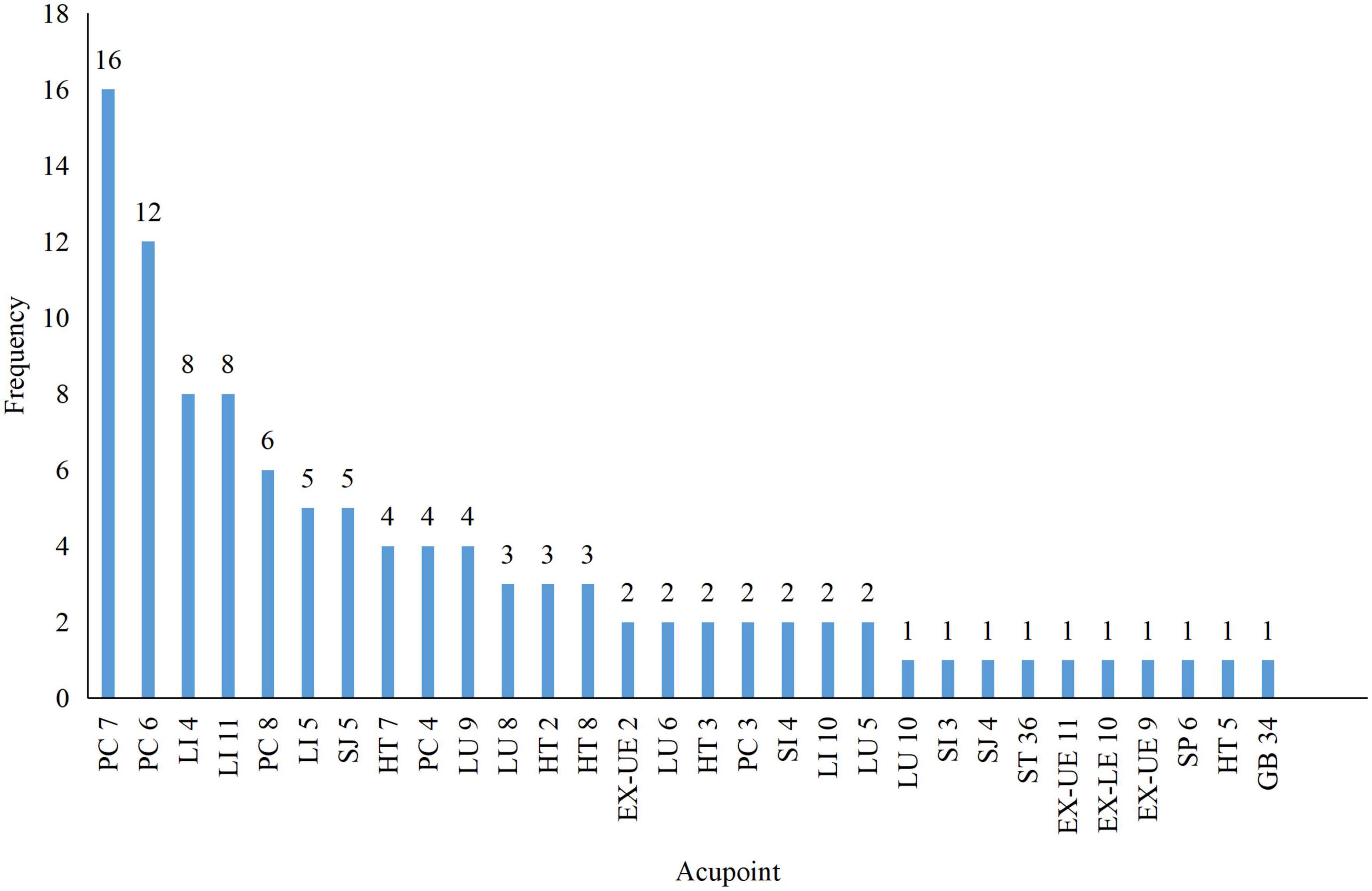
There were different acupuncture techniques, among which manual acupuncture was applied in seven studies (Yang et al., 2011; Yao et al., 2012; Hadianfard et al., 2015; Ural and Özturk, 2017; Tezel et al., 2019; Bahrami-Taghanaki et al., 2020; Huang and Lin, 2022) and electroacupuncture in nine (Kumnerddee and Kaewtong, 2010; Jin and Lang, 2011; Li, 2011; Ramin, 2013; Xiang et al., 2014; Chung et al., 2016; Maeda et al., 2017; Xie et al., 2018; Xiong, 2020), respectively. All studies reported the selected acupoints, and the frequency of all acupoints is shown in Figure 3. The most used acupoints were Daling (PC7, 100%), Neiguan (PC6, 75.0%), Hegu (LI 4, 50.0%), Quchi (LI 11, 50.0%), and Laogong (PC 8, 37.5%). Thirteen included studies (Kumnerddee and Kaewtong, 2010; Jin and Lang, 2011; Yang et al., 2011; Yao et al., 2012; Ramin, 2013; Xiang et al., 2014; Hadianfard et al., 2015; Chung et al., 2016; Ural and Özturk, 2017; Tezel et al., 2019; Bahrami-Taghanaki et al., 2020; Xiong, 2020; Huang and Lin, 2022) applied the fixed acupoint protocol and 3 (Li, 2011; Maeda et al., 2017; Xie et al., 2018) used individualized acupoint protocol (fixed main acupoints plus acupoints based on syndrome differentiation). In addition, the retention time was mainly 20 or 30 min, and the total sessions ranged from 6 to 36 sessions within 20 days to 17 weeks of treatment duration.
3.4. STRICTA checklist for the included studies
According to the STRICTA checklist, the items with more than 70% of reporting rates were item 3a (number of treatment sessions, 100%), item 2e (needle stimulation, 100%), item 3b (frequency and duration of treatment sessions, 93.8%), item 6b (precise description of the control or comparator, 87.5%), item 2d (response sought, 81.3%), item 2f (needle retention time, 81.3%), and item 2g (needle type, 81.3%). Item 4b (setting and context of treatment) and 1c (the extent to which treatment was varied) were not reported in the included studies. Detailed information on the STRICTA checklist is provided in Supplementary material 3.
3.5. Primary outcomes
3.5.1. Acupuncture as monotherapy
3.5.1.1. Acupuncture vs. sham acupuncture
Maeda et al. (2017) found no difference in the improvement of symptom severity (CTQ-SSS) or functional status (CTQ-FSS) between the electroacupuncture and sham electroacupuncture groups.
3.5.1.2. Acupuncture vs. night splints
Kumnerddee and Kaewtong (2010) found no difference in symptom severity (CTQ-SSS) or functional status (CTQ-FSS) between the electroacupuncture and night splints groups.
3.5.1.3. Acupuncture vs. medicine
Yang et al. (2011) observed that manual acupuncture was not superior to prednisolone in reducing symptom severity as measured by CSS.
3.5.2. Acupuncture as an adjunctive treatment
3.5.2.1. Acupuncture plus night splints vs. sham acupuncture plus night splints
Yao et al. (2012) reported that there was no difference between the manual acupuncture plus night splints group and the sham acupuncture plus night splints group in symptom severity (CTQ-SSS) or functional status (CTQ-FSS).
3.5.2.2. Acupuncture plus night splints vs. medicine plus night splints
Compared with medicine plus night splints, manual acupuncture plus night splints showed lower symptom severity (CTQ-SSS/GSS: SMD = −1.51, 95% CI −1.58 to −0.72, I2 = 47%) (Figure 4), but Hadianfard et al. (2015) found there was a greater effect of manual acupuncture plus night splints on functional status (CTQ-FSS).
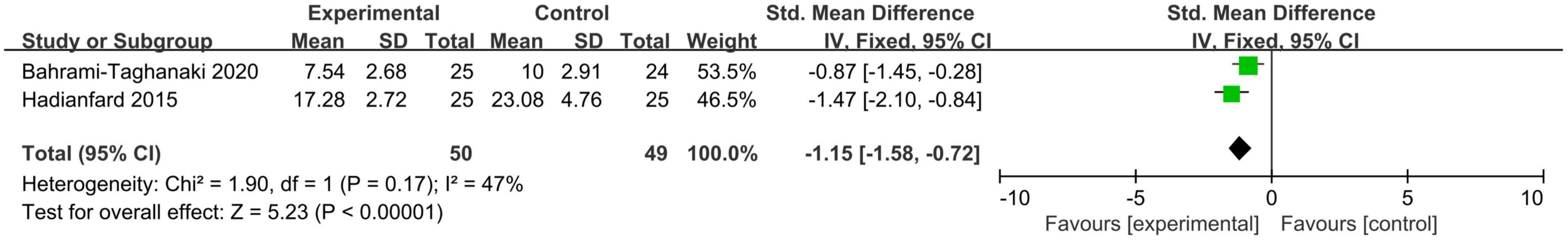
Figure 4. A meta-analysis of symptom severity of acupuncture plus night splints vs. medicine plus night splints.
3.5.2.3. Acupuncture plus night splints vs. night splints
The results of the meta-analysis showed that neither symptom severity (CTQ-SSS: SMD = −0.13, 95% CI −0.59 to 0.32, I2 = 52%) nor functional status (CTQ-FSS: SMD = −0.20, 95% CI −0.87 to 0.46, I2 = 76%) was significantly different between the acupuncture plus the night splints group and the night splints group (Figure 5A). However, the improvement of functional status measured by DASH was greater in the acupuncture plus night splints group than in the night splints group (change of DASH: SMD = −0.40, 95% CI −0.68 to −0.13, I2 = 0%) (Figure 5B).
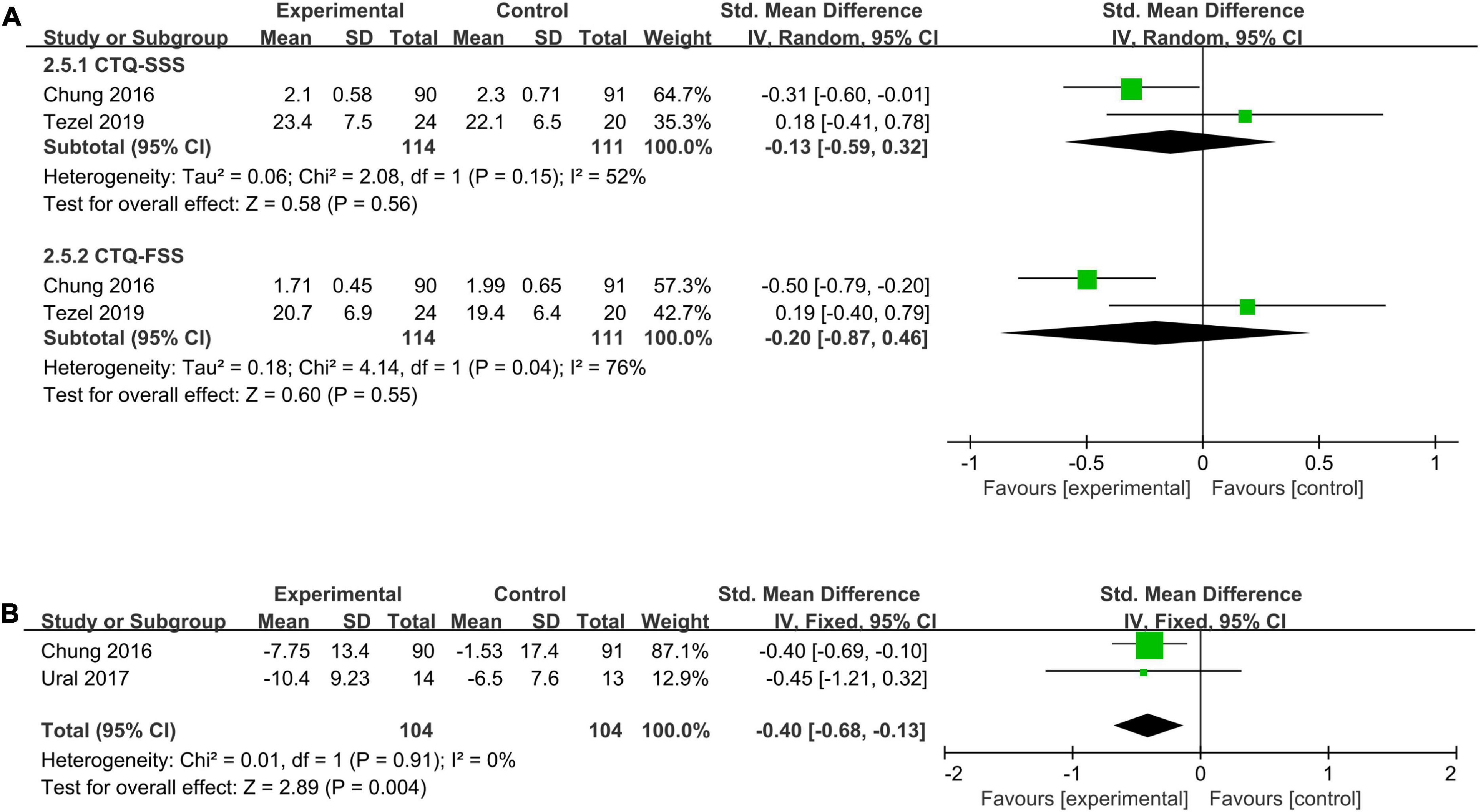
Figure 5. A meta-analysis of symptom severity and functional status of acupuncture plus night splints vs. night splints. (A) CTQ-SSS and CTQ-FSS; (B) change of DASH.
3.5.2.4. Acupuncture plus medicine vs. medicine
According to pooled results, the acupuncture plus medicine group had lower symptom severity (CTQ-SSS/GSS: SMD = −1.17, 95% CI −2.31 to −0.03, I2 = 93%) than the medicine group (Figure 6A), but the functional status (CTQ-FSS: MD = −2.17, 95% CI −6.45 to 2.10, I2 = 98%) was not significantly different between the two groups (Figure 6B).
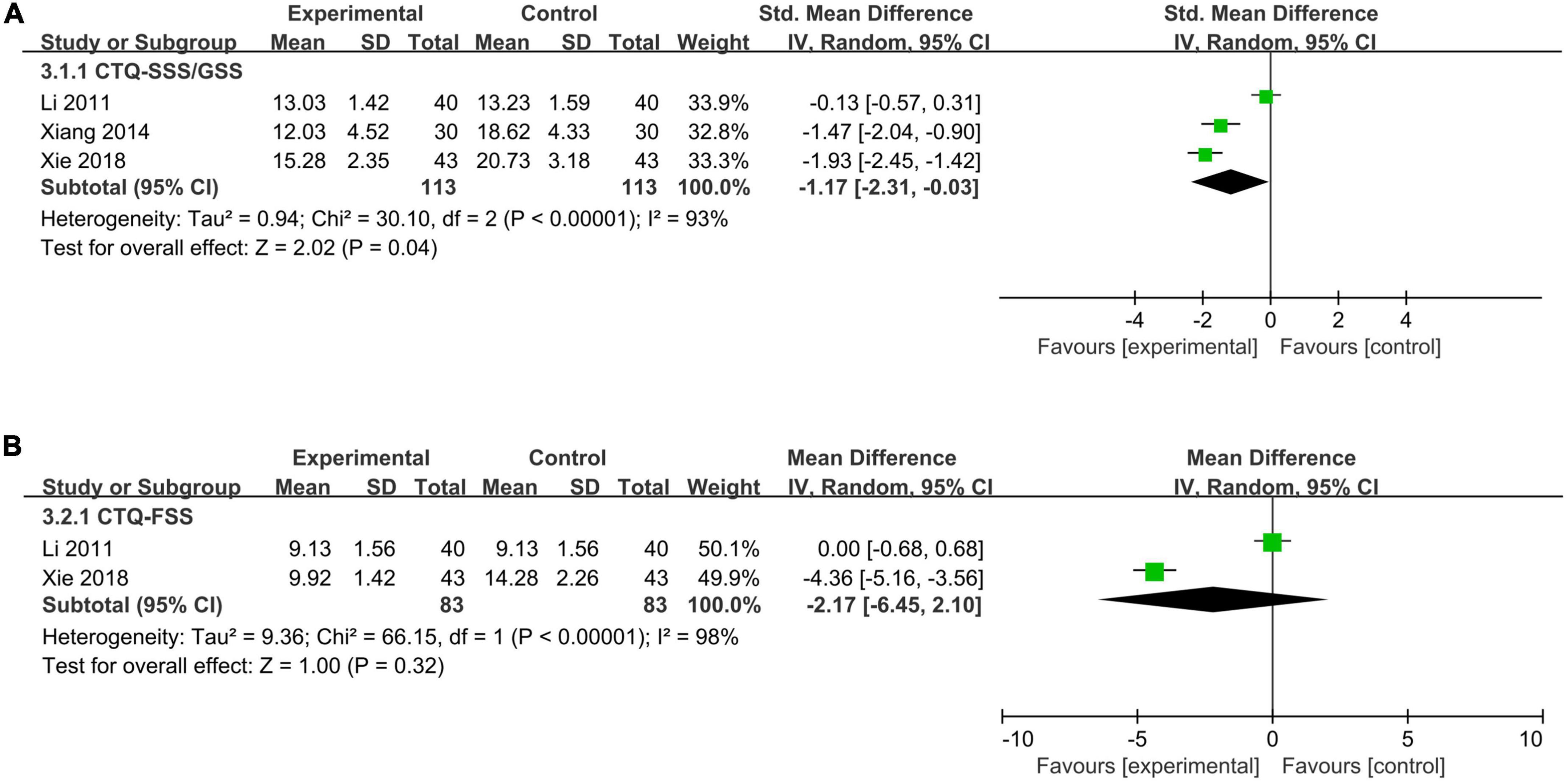
Figure 6. A meta-analysis of symptom severity and functional status of acupuncture plus medicine vs. medicine. (A) CTQ-SSS/GSS; (B) CTQ-FSS.
3.5.2.5. Acupuncture plus ultrashort wave therapy vs. ultrashort wave therapy
Xiong (2020) observed that patients who received acupuncture plus ultrashort wave therapy had lower symptom severity (CTQ-SSS) compared with those who received ultrashort wave therapy alone.
3.5.2.6. Acupuncture plus medicine plus night splints vs. medicine plus night splints
One RCT (Huang and Lin, 2022) found that adjunctive manual acupuncture in addition to night splints and ibuprofen treatment could improve symptom severity (CTQ-SSS) and functional status (CTQ-FSS) better than night splints plus ibuprofen treatment.
3.6. Secondary outcomes (pain intensity)
3.6.1. Acupuncture as monotherapy
Kumnerddee and Kaewtong (2010) reported that the electroacupuncture group showed a greater reduction in VAS than the night splints group.
3.6.2. Acupuncture as adjuvant treatment
3.6.2.1. Acupuncture plus night splints vs. medicine plus night splints
Hadianfard et al. (2015) observed that manual acupuncture plus night splints had a better effect than medicine plus night splints in decreasing VAS.
3.6.2.2. Acupuncture plus night splints vs. night splints
Meta-analysis results from three studies (Chung et al., 2016; Ural and Özturk, 2017; Tezel et al., 2019) showed that the acupuncture plus night splints group had lower pain intensity than the night splints group (VAS: MD = −1.65, 95% CI −3.05 to −0.26, I2 = 91%) (Figure 7).
3.6.2.3. Acupuncture plus medicine vs. medicine
Xiang et al. (2014) suggested that electroacupuncture plus medicine treatment was superior to medical treatment in relieving pain as measured by the NRS.
3.6.2.4. Acupuncture plus medicine plus night splints vs. medicine plus night splints
Huang and Lin (2022) found that manual acupuncture plus medicine and night splints were more effective in improving VAS scores than medicine plus night splints.
3.7. Secondary outcomes (electrophysiological parameters)
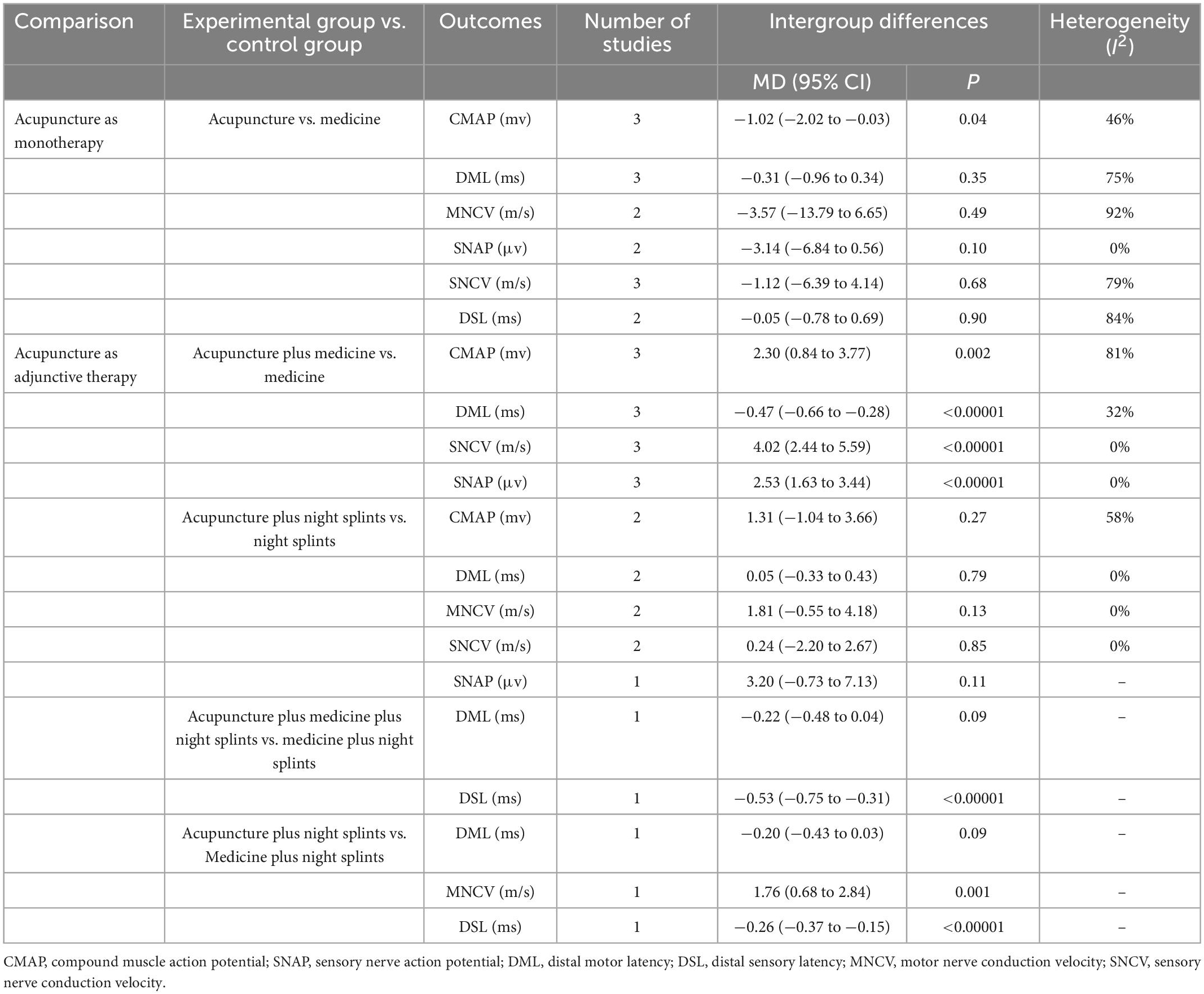
The results for electrophysiological parameters are shown in Table 2.
3.7.1. Acupuncture as monotherapy
Compared with medicine, the acupuncture group had a lower CMAP (MD = −1.02, 95% CI −2.02 to −0.03, I2 = 46%). No differences were found in DML, DSL, MNCV, SNAP, and SNCV between the two groups.
3.7.2. Acupuncture as an adjunctive treatment
3.7.2.1. Acupuncture plus night splints vs. medicine plus night splints
Hadianfard et al. (2015) found a faster MNCV and shorter DSL in the acupuncture plus night splints group than in the medicine plus night splints group. However, no difference in DML existed between the two groups.
3.7.2.2. Acupuncture plus night splints vs. night splints
There were no differences between the acupuncture plus night splints group and the night splints group in CMAP, DML, MNCV, SNCV, and SNAP.
3.7.2.3. Acupuncture plus medicine vs. medicine
Compared with the medicine group, the acupuncture plus medicine group showed higher CMAP (MD = 2.30, 95% CI 0.84 to 3.77, I2 = 81%) and SNAP (MD = 2.53, 95% CI 1.63 to 3.44, I2 = 0%), shorter DML (MD = −0.47, 95% CI −0.66 to −0.28, I2 = 32%), and faster SNCV (MD = 4.02, 95% CI 2.44 to 5.59, I2 = 0%).
3.7.2.4. Acupuncture plus medicine and night splints vs. medicine plus night splints
Huang and Lin (2022) found that the DML showed no significant difference between the acupuncture plus medicine and night splints group and the medicine plus night splints group, but the DSL was shorter in the acupuncture plus medicine and night splints group.
3.8. Responder rate
Three studies (Jin and Lang, 2011; Xie et al., 2018; Xiong, 2020) provided the responder rate. Jin and Lang (2011) reported a comparable responder rate between the acupuncture group and the medicine group. Xie et al. (2018) reported a superior responder rate in the acupuncture plus medicine group than the medicine group. Xiong (2020) observed that acupuncture plus ultrashort wave therapy had no better than ultrashort wave therapy in responder rate.
3.9. Adverse events
Four studies (Jin and Lang, 2011; Yang et al., 2011; Yao et al., 2012; Tezel et al., 2019) found no adverse events or serious adverse events related to acupuncture treatment occured. Kumnerddee and Kaewtong (2010) observed 6 of 30 cases in electroacupuncture group experienced skin bruises but no serious complication took place. Another study (Chung et al., 2016) reported electroacupuncture-related adverse events, including bruises at acupoints (4/90), mild local dermatitis around acupoints (3/90), increased pain (2/90), and numbness and tingling after electroacupuncture treatment (2/90), and the above adverse events disappeared within a week. The rest of the 10 studies provided no information on the adverse events.
3.10. Certainty of evidence
There was low and very low certainty of evidence attributed to some concern risk of bias, imprecision, and strongly suspected publication bias. A summary of the finding table is provided in Supplementary material 4.
4. Discussion
4.1. Summary of main results
We included 16 RCTs with 1,025 subjects and explored the effect of acupuncture as monotherapy and adjunctive therapy on CTS. Compared with night splints, acupuncture alone was more effective in relieving pain, but there were no differences in symptom severity and functional status. Acupuncture had no advantage over medicine in improving symptom severity or electrophysiological parameters. As an adjunctive treatment, acupuncture might effectively alleviate symptom severity, functional status, pain intensity, and electrophysiological parameters.
Meanwhile, acupuncture as adjunctive therapy was more effective than medicine to ameliorate symptom severity, functional status, pain intensity, and electrophysiological parameters. According to narrative analysis, acupuncture as monotherapy or adjunctive therapy, showed no superiority to sham acupuncture. Few acupuncture-related adverse events were reported. The above evidence had low or very low certainty.
4.2. Compared with previous reviews
Sim et al. (2011) included six RCTs and published the first systematic review of acupuncture for CTS, but three of the RCTs they identified were excluded from our study because the participants received other traditional Chinese medicine in one RCT (Shi et al., 2006) and cointerventions between groups were not comparable in the other two RCTs (Hu et al., 2000; Cai, 2007). Limited by insufficient RCTs, Sim et al. (2011) summarized the evidence of acupuncture for CTS as encouraging but not convincing. Choi et al. (2018) also found insufficient evidence to assess the effect of acupuncture and related interventions on CTS with 12 identified RCTs. Wu et al. (2020) conducted the latest systematic review involving 10 RCTs. Except for manual and electroacupuncture, they included laser acupuncture, moxibustion, and transcutaneous electrical nerve stimulation treatment. They drew the conclusion that acupuncture and related therapies appeared to be effective in improving symptoms, function, and pain in CTS, and emphasized that the validity of such a conclusion was limited. We included 16 RCTs to update the evidence and investigate the effect of acupuncture as monotherapy or adjunctive therapy for CTS.
4.3. The effect of acupuncture on CTS
The narrative analysis showed that neither acupuncture alone nor acupuncture as a adjunctive treatment had superiority over sham acupuncture. However, these results were derived from two independent studies, respectively (Yao et al., 2012; Maeda et al., 2017). Given the limited studies and risk of the underrated effect of acupuncture in sham-control trials with a small sample size (Lundeberg et al., 2008; Birch et al., 2022a,b), we failed to identify the advantage of acupuncture over sham acupuncture for CTS, which should continue to be explored in future studies.
One included RCT showed that 10-session acupuncture alone might be more effective than night splints in relieving pain intensity but not symptom severity or functional status. Night splints are recommended for CTS to improve short-term symptoms and function (Erickson et al., 2019). Whether there is a different long-term effect between acupuncture and night splints is unknown. No clear advantages of acupuncture as a monotherapy were observed compared with medicine. Among comparative medicines used in included studies, such as prednisolone (Yang et al., 2011; Ramin, 2013) and oral vitamin B12 (Jin and Lang, 2011), only prednisolone was recommended by the AAOS. Yang et al. (2011) found that patients with CTS who received acupuncture had a lower recurrence rate than those who received prednisolone in the 1-year follow-up period, which indicated acupuncture might have a better long-term effect than prednisolone. Due to insufficient studies, we were unable to compare the effect of acupuncture with other active treatments. More relevant head-to-head trials should be conducted in the future to focus on clinical and cost effects.
Patients with CTS who received acupuncture plus other treatment(s) showed more improvement in symptoms, function, or pain. However, these positive findings of acupuncture as adjunctive therapy came from open-label RCTs, which could be influenced by the patients’ subjective intentions. Based on the results of electrophysiological parameters, we found acupuncture combined with medicine could improve median nerve function better than medicine alone, which provided objective evidence for the adjunctive effect of acupuncture. However, the adjunctive effect of acupuncture should be further investigated in clinical trials with objective outcomes.
4.4. Implications for future research
The outcomes that were measured by subjective tools, such as CTQ, GSS, DASH, and VAS, relied on participants’ self-reports, which might induce measurement bias favoring acupuncture in open-label studies. Therefore, studies using objective outcomes are vital to build convincing evidence of acupuncture for CTS. According to the ROB 2 assessment, allocation concealment and advanced registration, or protocol, should be improved to enhance the credibility of the evidence. Meanwhile, in compliance with the STRICTA, authors should take care to report the details of the intervention, especially in items of acupuncture rationale, cointerventions, practitioner background and control or comparator interventions.
4.5. Limitations
Our systematic review and meta-analysis included the latest RCTs and assessed the effect of acupuncture on CTS. However, several limitations exist and should be considered. In the present review, the small sample size, substantial heterogeneity, and potential risk of bias of the included studies reduced the certainty of the evidence. Thus, the findings should be treated with caution. Owing to limited RCTs and data, we failed to investigate the advantages of different acupuncture techniques, identify the optimal parameters of the acupuncture protocol, or explore the follow-up effect of acupuncture.
5. Conclusion
Acupuncture as an adjunctive treatment may be effective for patients with CTS. In addition, more rigorous studies with objective outcomes are needed to investigate the effect of acupuncture in contrast with sham acupuncture or other active treatments.
Data availability statement
The original contributions presented in this study are included in this article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
RJ and HF conceptualized the study and provided methodological support. PY and GC selected the studies. JL and JD extracted the data. QD and XL assessed the risk of bias and wrote and edited the manuscript. HF and QD assessed the reporting quality of the intervention. FW and YY evaluated the grade. All authors contributed to the article and approved the submitted version.
Funding
This study was financially funded by the Science and Technology Project of Sichuan Province (number: 2019YFS0019).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnins.2023.1097455/full#supplementary-material
References
Atroshi, I., Gummesson, C., Johnsson, R., Ornstein, E., Ranstam, J., and Rosén, I. (1999). Prevalence of carpal tunnel syndrome in a general population. JAMA 282, 153–158. doi: 10.1001/jama.282.2.153
Bahrami-Taghanaki, H., Azizi, H., Hasanabadi, H., Jokar, M. H., Iranmanesh, A., Khorsand-Vakilzadeh, A., et al. (2020). Acupuncture for carpal tunnel syndrome: A randomized controlled trial studying changes in clinical symptoms and electrodiagnostic tests. Altern. Ther. Health Med. 26, 10–16.
Birch, S., Lee, M. S., Kim, T. H., and Alraek, T. (2022a). Historical perspectives on using sham acupuncture in acupuncture clinical trials. Integr. Med. Res. 11:100725. doi: 10.1016/j.imr.2021.100725
Birch, S., Lee, M. S., Kim, T. H., and Alraek, T. (2022b). On defining acupuncture and its techniques: A commentary on the problem of sham. Integr. Med. Res. 11:100834. doi: 10.1016/j.imr.2022.100834
Cai, D. F. (2007). Effect of warming acupuncture and manual release on carpal tunnel syndrome. Inf. Trad. Chin. Med. 5, 56–57.
Calandruccio, J. H., and Thompson, N. B. (2018). Carpal tunnel syndrome: Making evidence-based treatment decisions. Orthop. Clin. North Am. 49, 223–229. doi: 10.1016/j.ocl.2017.11.009
Chesterton, L. S., Blagojevic-Bucknall, M., Burton, C., Dziedzic, K. S., Davenport, G., Jowett, S. M., et al. (2018). The clinical and cost-effectiveness of corticosteroid injection versus night splints for carpal tunnel syndrome (INSTINCTS trial): An open-label, parallel group, randomised controlled trial. Lancet 392, 1423–1433.
Choi, G. H., Wieland, L. S., Lee, H., Sim, H., Lee, M. S., and Shin, B. C. (2018). Acupuncture and related interventions for the treatment of symptoms associated with carpal tunnel syndrome. Cochrane Database Syst. Rev. 12:Cd011215. doi: 10.1002/14651858.CD011215.pub2
Chung, V. C. H., Ho, R. S. T., Liu, S., Chong, M. K. C., Leung, A. W. N., Yip, B. H. K., et al. (2016). Electroacupuncture and splinting versus splinting alone to treat carpal tunnel syndrome: A randomized controlled trial. CMAJ Can. Med. Assoc. J. 188, 867–875. doi: 10.1503/cmaj.151003
Daniell, W. E., Fulton-Kehoe, D., and Franklin, G. M. (2009). Work-related carpal tunnel syndrome in Washington State workers’ compensation: Utilization of surgery and the duration of lost work. Am. J. Ind. Med. 52, 931–942. doi: 10.1002/ajim.20765
Erickson, M., Lawrence, M., Jansen, C. W. S., Coker, D., Amadio, P., and Cleary, C. (2019). Hand pain and sensory deficits: Carpal tunnel syndrome. J. Orthop. Sports Phys. Ther. 49, CG1–CG85. doi: 10.2519/jospt.2019.0301
Feng, B., Chen, K., Zhu, X., Ip, W. Y., Andersen, L. L., Page, P., et al. (2021). Prevalence and risk factors of self-reported wrist and hand symptoms and clinically confirmed carpal tunnel syndrome among office workers in China: A cross-sectional study. BMC Public Health 21:57. doi: 10.1186/s12889-020-10137-1
Graham, B., Peljovich, A. E., Afra, R., Cho, M. S., Gray, R., Stephenson, J., et al. (2016). The American academy of orthopaedic surgeons evidence-based clinical practice guideline on: Management of carpal tunnel syndrome. J. Bone Joint Surg. Am. 98, 1750–1754. doi: 10.2106/JBJS.16.00719
Hadianfard, M., Bazrafshan, E., Momeninejad, H., and Jahani, N. (2015). Efficacies of acupuncture and anti-inflammatory treatment for carpal tunnel syndrome. J. Acupunct. Meridian Stud. 8, 229–235. doi: 10.1016/j.jams.2014.11.005
Hu, N. W., Liu, J. Y., and Wang, F. M. (2000). Clinical observation of combination of acupuncture and medicine in treating carpal tunnel syndrome. Acta Chin. Med. Pharmacol. 3, 57–58.
Huang, X. X., and Lin, C. J. (2022). Preliminary analysis of the effect of conventional treatment combined with acupuncture on mild to moderate carpal tunnel syndrome. Fujian Med. J. 44, 63–66.
Jin, L. Q., and Lang, B. X. (2011). Effect of electroacupuncture plus acupoint injection in treating carpal tunnel syndrome of early stage. Shanghai J. Acupunct. Moxibust. 30, 464–466.
Kumnerddee, W., and Kaewtong, A. (2010). Efficacy of acupuncture versus night splinting for carpal tunnel syndrome: A randomized clinical trial. J. Med. Assoc. Thai. 93, 1463–1469.
Li, M. (2011). Study on the Electrophysiological Assessment of the Efficacyof Electric Acupuncture in Treatment of Mild and Moderate Carpal Tunnel Syndromes. Master’s thesis. Guangzhou: Guangzhou University of Chinese Medicine.
Lundeberg, T., Lund, I., Näslund, J., and Thomas, M. (2008). The emperors sham – wrong assumption that sham needling is sham. Acupunct. Med. 26, 239–242. doi: 10.1136/aim.26.4.239
MacPherson, H., Altman, D. G., Hammerschlag, R., Youping, L., Taixiang, W., White, A., et al. (2010). Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): Extending the CONSORT statement. J. Altern. Complement. Med. 16, St1–St14. doi: 10.1089/acm.2010.1610
Maeda, Y., Kim, H., Kettner, N., Kim, J., Cina, S., Malatesta, C., et al. (2017). Rewiring the primary somatosensory cortex in carpal tunnel syndrome with acupuncture. Brain 140, 914–927. doi: 10.1093/brain/awx015
Manente, G., Torrieri, F., Di Blasio, F., Staniscia, T., Romano, F., and Uncini, A. (2001). An innovative hand brace for carpal tunnel syndrome: A randomized controlled trial. Muscle Nerve 24, 1020–1025. doi: 10.1002/mus.1105
Padua, L., Coraci, D., Erra, C., Pazzaglia, C., Paolasso, I., Loreti, C., et al. (2016). Carpal tunnel syndrome: Clinical features, diagnosis, and management. Lancet Neurol. 15, 1273–1284. doi: 10.1016/S1474-4422(16)30231-9
Page, M. J., Massy-Westropp, N., O’Connor, D., and Pitt, V. (2012). Splinting for carpal tunnel syndrome. Cochrane Database Syst. Rev. 2012:Cd010003. doi: 10.1002/14651858.CD010003
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 372, n71. doi: 10.1136/bmj.n71
Palmer, D. H., and Hanrahan, L. P. (1995). Social and economic costs of carpal tunnel surgery. Instr. Course Lect. 44, 167–172.
Qiao, L., Guo, M., Qian, J., Xu, B., Gu, C., and Yang, Y. (2020). Research advances on acupuncture analgesia. Am. J. Chin. Med. 48, 245–258. doi: 10.1142/S0192415X20500135
Ramin, M. (2013). Comparison of Acupuncture and Corticosteroid in lmprovement of Carpal Tunnel Syndrome and its mechanism. Ph.D. thesis. Nanjing: Nanjing University of Chinese medicine.
Shea, B. J., Reeves, B. C., Wells, G., Thuku, M., Hamel, C., Moran, J., et al. (2017). AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 358, j4008. doi: 10.1136/bmj.j4008
Shi, Q., and MacDermid, J. C. (2011). Is surgical intervention more effective than non-surgical treatment for carpal tunnel syndrome? A systematic review. J. Orthop. Surg. Res. 6:17. doi: 10.1186/1749-799X-6-17
Shi, Y. S., Fang, W., Zhao, X. Y., Li, H. X., and Liu, S. (2006). Control study on effect of pricking collateral blood therapy combined with massage on mild carpal tunnel syndrome. Chin. J. Integr. Trad. West. Med. 6, 497–499.
Sim, H., Shin, B. C., Lee, M. S., Jung, A., Lee, H., and Ernst, E. (2011). Acupuncture for carpal tunnel syndrome: a systematic review of randomized controlled trials. J. Pain. 12, 307–314. doi: 10.1016/j.jpain.2010.08.006
Spahn, G., Wollny, J., Hartmann, B., Schiele, R., and Hofmann, G. O. (2012b). Meta-analysis for the evaluation of risk factors for carpal tunnel syndrome (CTS) Part II. Occupational risk factors. Z. Orthop. Unfall 150, 516–524. doi: 10.1055/s-0032-1315346
Spahn, G., Wollny, J., Hartmann, B., Schiele, R., and Hofmann, G. O. (2012a). Meta-analysis for the evaluation of risk factors for carpal tunnel syndrome (CTS) Part I. General factors. Z. Orthop. Unfall 150, 503–515. doi: 10.1055/s-0032-1315345
Tezel, N., Umay, E., Yilmaz, V., and Cakci, A. (2019). Acupuncture plus night splint for quality of life and disability in patients with carpal tunnel syndrome: a randomized controlled trial. Integr. Med. Res. 8, 284–288. doi: 10.1016/j.imr.2019.11.003
Ural, F. G., and Özturk, G. T. (2017). The acupuncture effect on median nerve morphology in patients with carpal tunnel syndrome: an ultrasonographic study. Evid. Based Complement. Altern. Med. 2017:7420648. doi: 10.1155/2017/7420648
Wipperman, J., and Goerl, K. (2016). Carpal tunnel syndrome: diagnosis and management. Am. Fam. Physic. 94, 993–999.
Wu, I. X., Lam, V. C., Ho, R. S., Cheung, W. K., Sit, R. W., Chou, L. W., et al. (2020). Acupuncture and related interventions for carpal tunnel syndrome: systematic review. Clin. Rehabil. 34, 34–44. doi: 10.1177/0269215519877511
Xiang, Y., Jiang, H., and Li, J. H. (2014). Effect of electroacupuncture on mild to moderate carpal tunnel syndrome. Clin. Educ. Gen. Pract. 12, 684–686.
Xie, Q. E., Pan, J., Zhang, X., Xu, Y. G., and Wang, L. H. (2018). Effect of electroacupuncture on patients with mild to moderate carpal tunnel syndrome and electrophysiological parameters. Prog. Mod. Biomed. 18, 343–347.
Xiong, P. (2020). Effect of electroacupuncture combined with local acupoint selection on carpal tunnel syndrome. Hubei J. Trad. Chin. Med. 42, 52–54.
Yang, C. P., Wang, N. H., Li, T. C., Hsieh, C. L., Chang, H. H., Hwang, K. L., et al. (2011). A randomized clinical trial of acupuncture versus oral steroids for carpal tunnel syndrome: a long-term follow-up. J. Pain 12, 272–279. doi: 10.1016/j.jpain.2010.09.001
Keywords: acupuncture, carpal tunnel syndrome, systematic review, meta-analysis, randomized controlled trial
Citation: Dong Q, Li X, Yuan P, Chen G, Li J, Deng J, Wu F, Yang Y, Fu H and Jin R (2023) Acupuncture for carpal tunnel syndrome: A systematic review and meta-analysis of randomized controlled trials. Front. Neurosci. 17:1097455. doi: 10.3389/fnins.2023.1097455
Received: 13 November 2022; Accepted: 12 January 2023;
Published: 23 February 2023.
Edited by:
Min Fang, Shanghai University of Traditional Chinese Medicine, ChinaReviewed by:
Stephen Cina, Massachusetts College of Pharmacy and Health Sciences, United StatesJeungchan Lee, Spaulding Rehabilitation Hospital, United States
Copyright © 2023 Dong, Li, Yuan, Chen, Li, Deng, Wu, Yang, Fu and Jin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rongjiang Jin,  Y2R6eXlkeGpyakAxMjYuY29t; Hui Fu,
Y2R6eXlkeGpyakAxMjYuY29t; Hui Fu,  NTE0NTY0Nzk2QHFxLmNvbQ==
NTE0NTY0Nzk2QHFxLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Qinjian Dong1†
Qinjian Dong1† Rongjiang Jin
Rongjiang Jin