- 1School of Nursing, Guangzhou University of Chinese Medicine, Guangzhou, China
- 2School of Nursing, Southern Medical University, Guangzhou, China
- 3School of Nursing, Guangdong Pharmaceutical University, Guangzhou, China
Background: Disturbances in circadian rhythms are common among night-shift workers and result in poor sleep quality. Nevertheless, the heterogeneity of circadian rhythms and their relationship with sleep quality is less explored in nursing interns. Therefore, we aimed to identify the latent subtypes of circadian rhythm, explore their relationship with sleep quality, and evaluate their moderating role between perceived stress and sleep quality in nursing interns.
Materials and methods: In all, 452 nursing interns were recruited between October 2020 and January 2021 from Be Resilient to Nursing Career (BRNC), which is a multicenter, prospective cohort of a career growth program for nursing students. They were assessed using the 10-item Chinese Perceived Stress Scale, Circadian Type Inventory, and Pittsburgh Sleep Quality Index. Latent profile analysis and moderation analysis were performed.
Results: Overall, 72.3% of the nursing interns reported poor sleep quality. We identified three latent subtypes of circadian rhythms, namely, Vigorousness (40.1%), Inadaptability (18.6%), and Flexibility (41.1%). Females (OR = 1.97, 95% Cl: 1.01–3.83, P = 0.047) with normal body mass index (OR = 1.62, 95% CI: 0.95–2.76, P = 0.078) were prone to Flexibility. Circadian rhythm types significantly moderated the association between perceived stress and sleep quality (P < 0.05).
Conclusion: Nursing interns suffer from poor sleep. There exists heterogeneity of circadian rhythm subtypes in nursing interns, and attention should be paid to those with Inadaptability type. The association between perceived stress and sleep quality is significantly moderated by circadian rhythm subtypes.
Introduction
Circadian rhythms refer to the behavioral and metabolic changes regulated by the circadian clock, which maintains synchronized changes with the natural light–dark cycle (Hastings et al., 2007; Zare et al., 2017). Sleep quality consists of sleep latency, number of awakenings after falling asleep, and sleep efficiency (Facco et al., 2017), which are associated with circadian rhythm (Zare et al., 2017). A recent study indicated that occupational stress might enhance the risk of poor sleep quality by the gene polymorphism of period circadian regulator 3 (PER3) gene (Peng et al., 2022). In a recent study, approximately 43.2% and 63.2% of Chinese night-shift workers had abdominal obesity and poor sleep quality, respectively (Sun et al., 2018). In addition, a large survey indicated that approximately 24.4–32.4% of night-shift workers reported sleep disorders (i.e., insomnia, excessive drowsiness, sleepiness, etc.) (Flo et al., 2012; Chen et al., 2020). Thus, circadian rhythm misalignment and poor sleep quality may be the two most common health-related problems in the night-shift populations (Fido and Ghali, 2008).
The circadian rhythm is defined by three key parameters: the period, the phase, and the amplitude (Zhang and Jain, 2021). The normal rhythm may be disrupted by a change in period, phase, amplitude, or any combination of these through human activities or environmental factors such as night shifts and occupational stressors (Pallesen et al., 2021; Zhang and Jain, 2021). Due to the recognition of individual differences in human biology and their potential role in the adjustment to night work, several self-report measures have been developed that indirectly assess the characteristics of circadian rhythms (Di Milia et al., 2005). Early self-report measures focused on assessing differences in the circadian phase. According to these measures, activity preferences are correlated with circadian rhythm phase differences (Di Milia et al., 2005). Later on, Folkard et al. (1979) developed the Circadian Type Questionnaire (CTQ) based on three characteristics of circadian rhythms. In order to improve the predictive power of the scale for shift tolerance, the Circadian Type Inventory (CTI) was developed, based on the CTQ (Di Milia et al., 2004). The CTI is reported to possess strong psychological properties in shift work studies (Di Milia et al., 2005; Jafari Roodbandi et al., 2015; Chen et al., 2020).
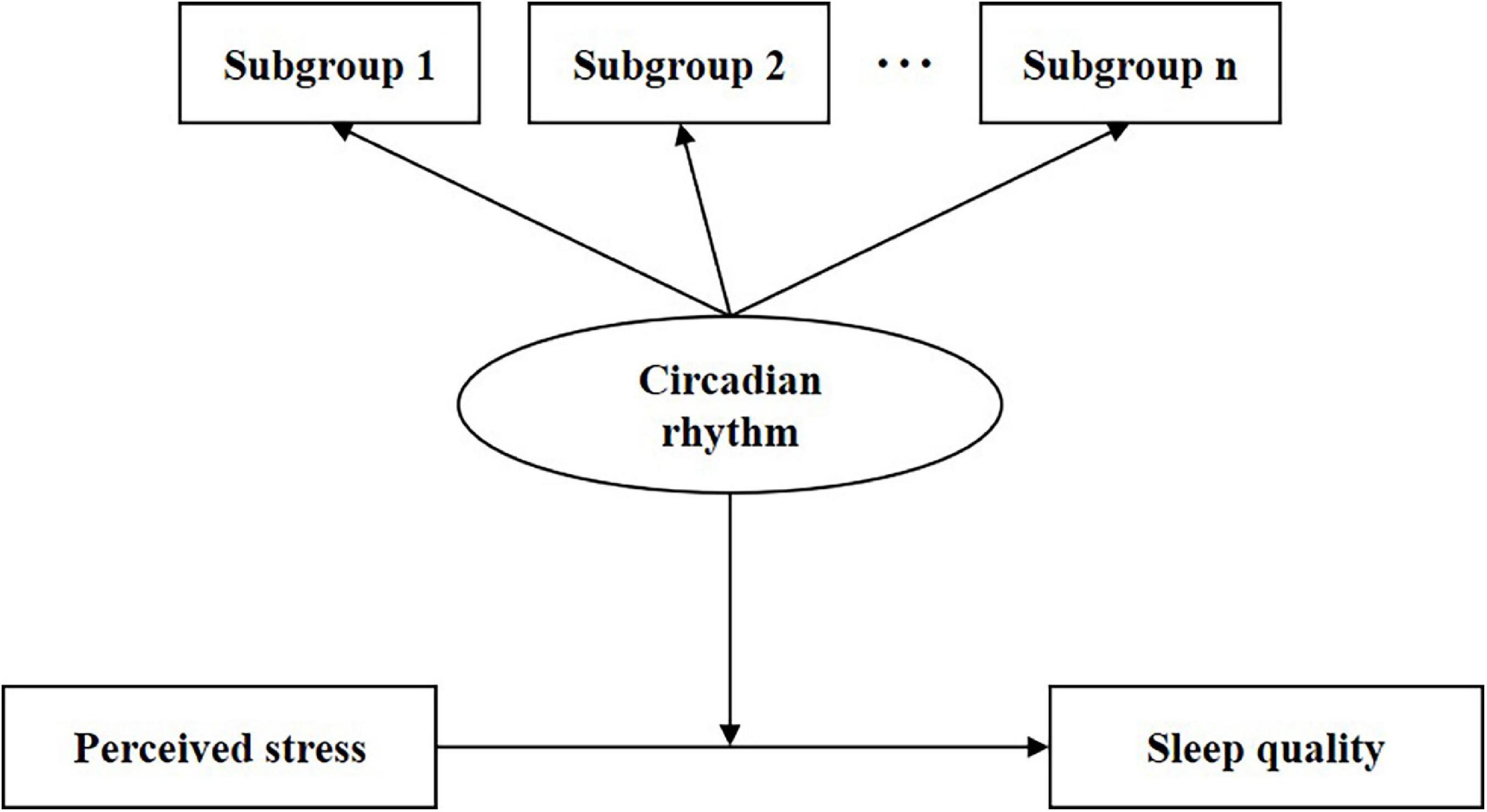
Night-shift work was developed in hospitals to ensure high-quality care; however, it leads to circadian misalignment and poor sleep quality among nurses (Di Muzio et al., 2021). The internship period is the duration for interns to acclimate to night-shift work. Nursing interns are a special subgroup of the nursing team and have received tremendous attention from multidisciplinary researchers (Mei et al., 2022c). Nursing interns experience transition-related stressors as well as non-habitual sleep–wake schedule (Zhang et al., 2019), which leads to night-shift intolerance and poor sleep quality among them (Huang et al., 2021). Previous studies reported that approximately 22.8–38.2% of nursing interns experience sleeping problems (Lai et al., 2020; Gao et al., 2021). Additionally, circadian rhythm disruption affects the levels of ghrelin, leptin, insulin, cortisol, and melatonin among night-shift workers, causing poor sleep quality (Ulhôa et al., 2015; Huang et al., 2021). Poor sleep adversely affects their physical and mental health (e.g., cardiovascular risk, mood disorders, etc.) as well as their work performance (Chang and Li, 2019). Therefore, it is important to pay attention to and address the sleep problems of nursing interns. Nonetheless, the relationship between circadian rhythm and sleep quality is less explored among nursing interns. In addition, there exists heterogeneity in circadian rhythms, and individuals with different latent profiles of circadian rhythms exhibit different responses to night-shift work (Axelsson et al., 2004; Boivin and Boudreau, 2014). However, traditional statistical methods are difficult to explore the psychological complexity of circadian rhythms especially when heterogeneous subgroups exist, and more advanced techniques should be performed in the present study (Choi et al., 2019). The Latent Profile Analysis (LPA) as a person-centered approach could more accurately identify heterogeneity within a population than the variable-centered approach (Kongsted and Nielsen, 2017). Hence, the current study was designed to meet the following objectives: (1) Identify latent subgroups with different circadian rhythm types by Latent Profile Analysis (LPA); (2) Compare sleep quality among subgroups with LPA-based circadian rhythm types; (3) Evaluate the moderating role of LPA-based circadian rhythm types between perceived stress and sleep quality. The hypothesized framework is described in Figure 1.
Materials and methods
Participants and procedure
We conducted a multicenter, cross-sectional survey of nursing interns in Guangzhou City, China, between October 2020 and January 2021. In all, 478 nursing interns were recruited from Be Resilient to Nursing Career (BRNC) by cluster sampling (Chen et al., 2022; Mei et al., 2022a,b,c; Wu et al., 2022). Of these, 452 completed the survey resulting in a response rate of 94.6%. The minimum sample for LPA analysis with 80% accuracy is 300 (Swanson et al., 2012). Thus, the sample size of 452 in the current study was efficiently powerful. The inclusion criteria were as follows: (1) nursing interns who had been working on night shifts from the start of their internship until the survey month and (2) clinical internship ≥3 months. Additionally, participants with any mental disorder diagnosed by clinical psychiatrists in the last 6 months were excluded.
Measures
Demographic characteristics
Demographic characteristics including gender and educational level were collected. Also, sleep-related characteristics, such as the habit of consuming caffeinated drinks, regularity of diet, and body mass index (BMI) were collected according to previous research (St-Onge et al., 2016; Sun et al., 2018; Gross et al., 2020; Ono et al., 2020; Ribas-Latre et al., 2021).
Measure of circadian rhythm
The Chinese version of the Circadian Type Inventory (CTI) assesses circadian flexibility and languidity in shift nurses and was validated by Qi et al. (2019). It has two domains including Flexible/Rigid (FR) and Languid/Vigorous (LV). The total score ranges from 11 to 55 with higher scores indicating a greater ability to handle with shift-related sleep problems. The cut-offs for FR and LV are 18.75 and 22.5, respectively (Di Milia et al., 2004; Jafari Roodbandi et al., 2015). In this study, Cronbach’s alpha was 0.879 for FR and 0.764 for LV.
Measure of sleep quality
Pittsburgh Sleep Quality Index (PSQI) assesses sleep quality and can be applied to patients with sleep disorders as well as the general population. It has seven domains including sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medications, and daytime dysfunction (Buysse et al., 1989). The cut-off for PSQI is 5 (Jafari Roodbandi et al., 2015). The Cronbach’s alpha was 0.852 in the current study.
Measure of perceived stress
The 10-item Chinese Perceived Stress Scale (CPSS-10) was developed by Cohen (1988), and the Chinese version is proven to be reliable (Ng, 2013). It assesses the perceived stress level of individuals in the last month. CPSS-10 has two domains including “Perceived Helplessness” and “Perceived Self-efficacy.” The total scores range from 0 to 40, with a higher score indicating a higher stress level. The cut-off for CPSS-10 is 26 (Cohen, 1988). In the present study, the Cronbach’s alpha was 0.877.
Statistical analysis
First, demographic and sleep-related characteristics (categorical variables) were described as frequencies and proportions (%). Second, spearman correlation analysis was performed to assess the associations among perceived stress, circadian rhythm, and sleep quality. Strength of relationship was categorized as follows: weak (|r| < 0.3); moderate (0.3 ≤ | r| < 0.5); strong (|r| ≥ 0.5) (Cohen, 2013). In addition, Generalized Additive Model (GAM) was employed to estimate the non-linear associations (Hastie and Tibshirani, 2017). Third, LPA was performed to identify potential subgroups with different circadian rhythm types. It began with a one-class model, continuing until fit indices could not be significantly improved. Bayesian Information Criteria (BIC), Akaike’s Information Criteria (AIC), Lo-Mendell-Rubin (LMR), and Entropy value were utilized as main fitting indicators (Muthén and Muthén, 2017). Fourth, LPA-based differences in PSQI scores were estimated by Bayesian Factor. The Cauchy prior width was set at 0.7, which indicates a 70% probability of the actual effect size being between –0.5 and 0.5 (Molero Jurado et al., 2021). The Bayes factor value greater than 10 indicates strong relative evidence for a hypothesis (Quintana and Williams, 2018). Fifth, univariate (P < 0.2) and multivariate regressions were used to recognize potential indicators of LPA-based circadian rhythm types. Sixth, stratified analysis was performed to evaluate the difference in sleep quality among subgroups with different circadian rhythm types after controlling for potential covariates. At last, the moderating role of LPA-based circadian rhythm types (category variable) was estimated between perceived stress (continuous variable) and sleep quality (continuous variable). The data were run by Statistical Product and Service Solutions (SPSS, version 22.0), Mplus (version 8.3), Empower Stats (version 3.0), and JASP (version 0.16.0). Significance was set at 0.05.
Results
Demographic characteristics
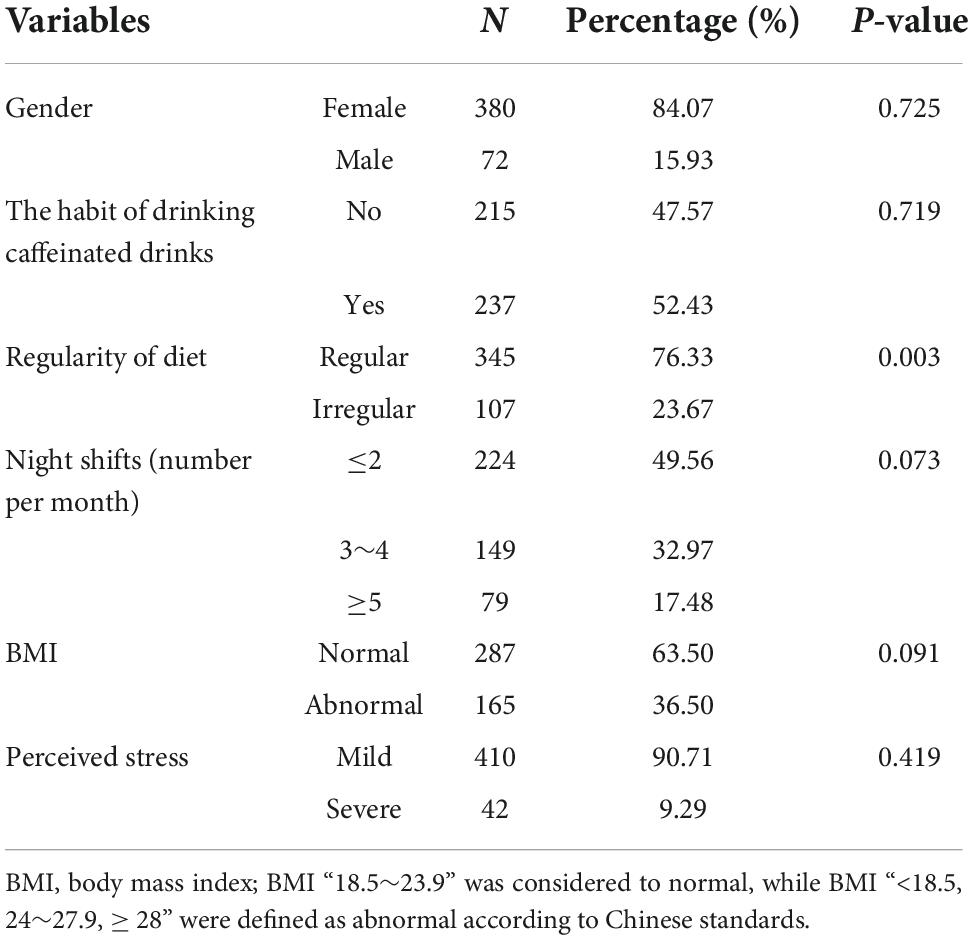
A total of 452 nursing interns completed the survey (female, N = 380); 52.43% were accustomed to caffeinated drinks and 23.67% had irregular meal intake during the internship. The BMI of male and female interns were 20.36 (SD = 3.51) and 20.05 (SD = 3.35), respectively. The median of night shifts per month was three and 17.5% reported more than five per month. Other demographic details are presented in Table 1.
The analysis of the correlations among perceived stress, circadian rhythm, and sleep quality
The mean and standard deviations of variables were perceived stress (16.91 ± 6.62), Flexible/Rigid (12.15 ± 4.68), Languid/Vigorous (17.11 ± 4.85), and PSQI (6.56 ± 3.08). Spearman correlations are described in Figure 2A. PSQI was positively associated with Languid/Vigorous (r = 0.34, P < 0.01) and perceived stress (r = 0.14, P < 0.05). The associations between PSQI, perceived stress, and Flexible/Rigid were non-linear (Figures 2B–D).
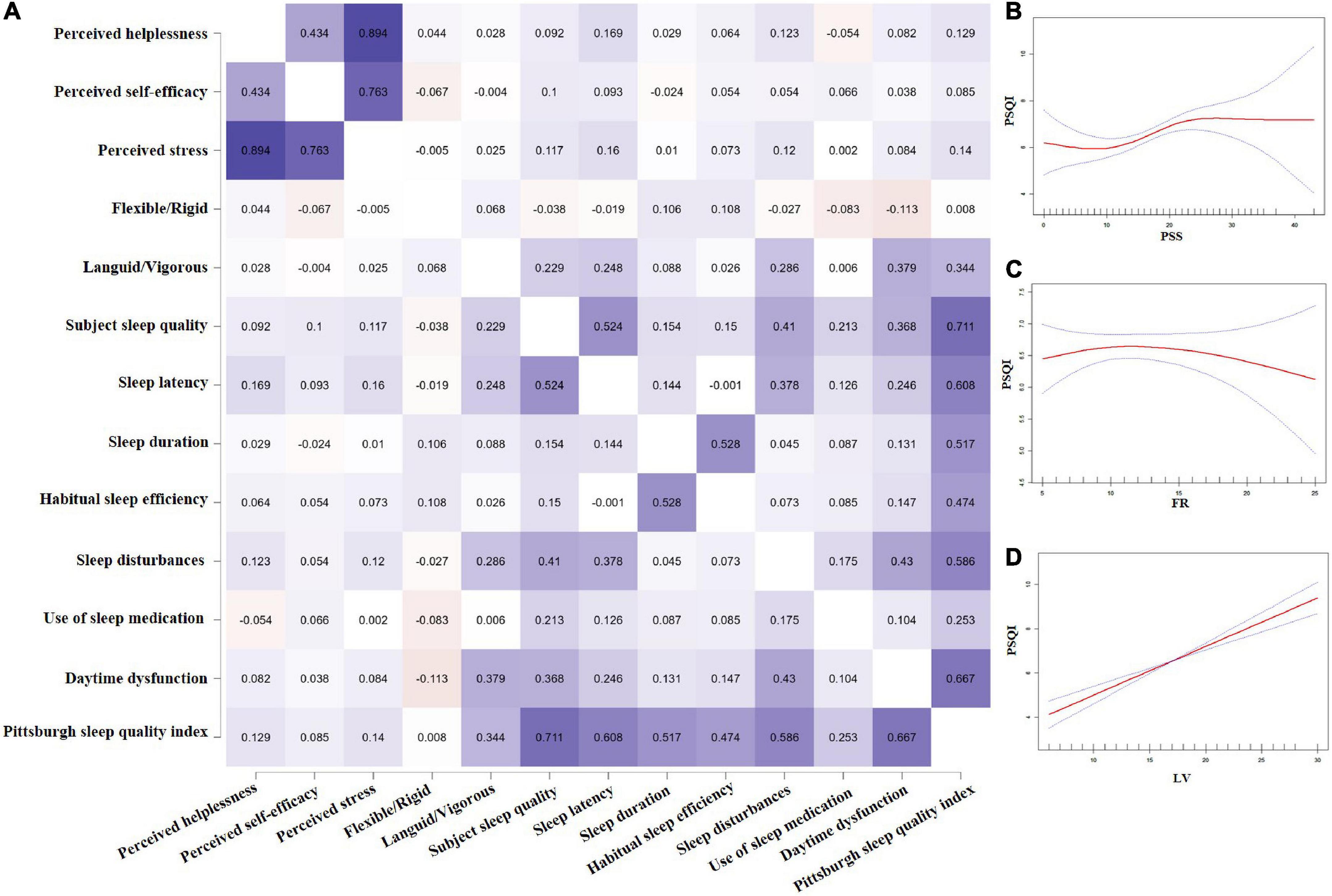
Figure 2. Spearman correlation Heatmap among perceived stress, circadian rhythms, and sleep quality (A), and curve line regression of the above three variables (B–D).
Latent profiles analysis of circadian rhythm
One to five latent subgroups were checked based on fitting indicators and the three-class model was optimal in consideration of (1) relatively small AIC, BIC, and aBIC, (2) the sample size of each class was more than 50, and (3) a significant P-value of Lo-Mendell-Rubin (LMR). Other information is detailed in Figures 3A,B.
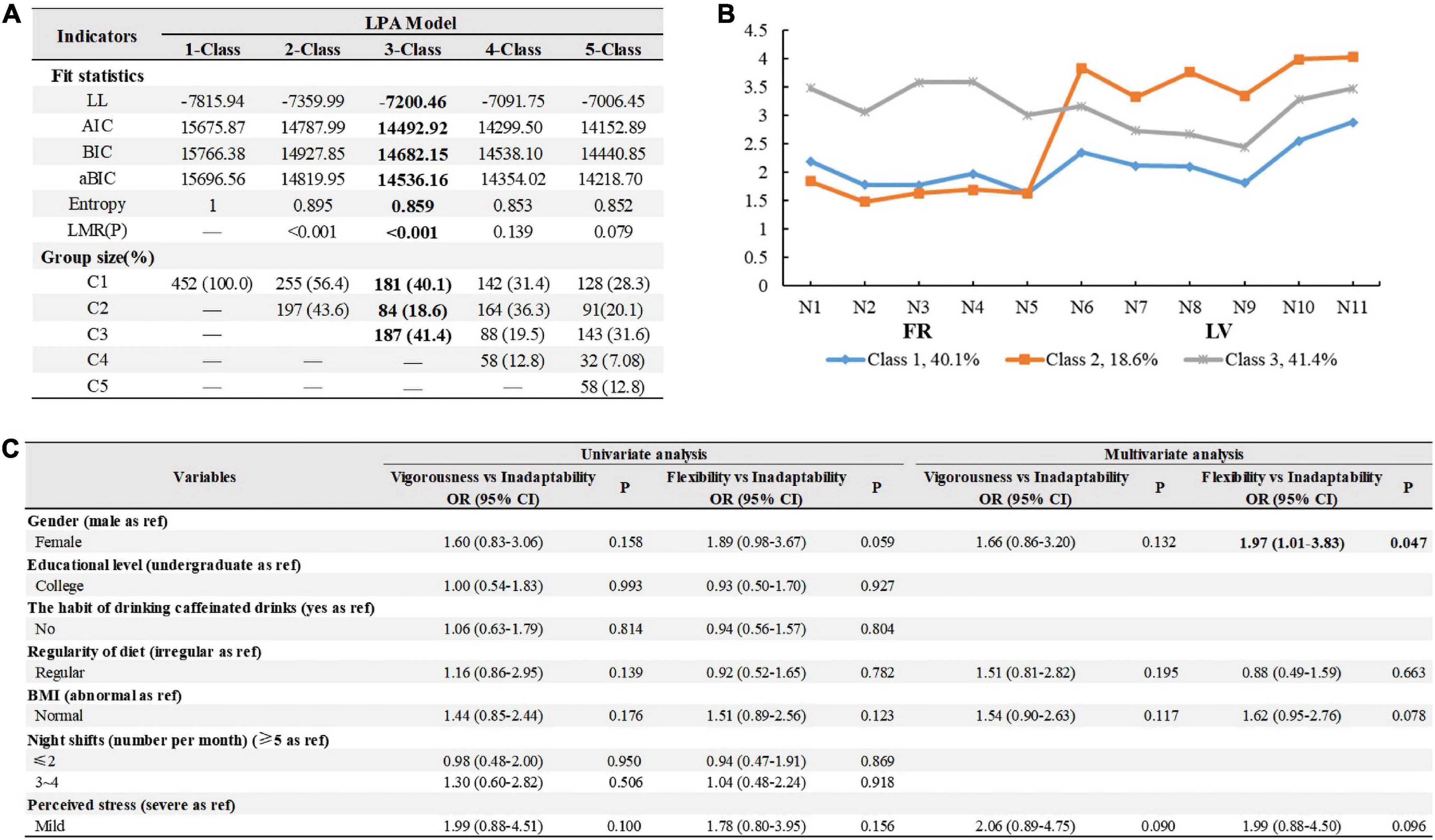
Figure 3. Fitting index and group size of latent profile analysis models and logistic regression results for predicting external features on the 3-class pattern. (A) Fitting index and group size of latent profile analysis models. Bold figures highlight the selected class solution. LL, Log-likelihood; AIC, Akaibe information criterion; BIC, Bayesian information criterion; aBIC, adjusted BIC; LMR, Lo, Mendell, and Rubin likelihood ratio test; C1, vigorous; C2, inadaptability; C3, flexibility. (B) Parameters for the final three-class patterns. FR, flexible/rigid; LV, languid/vigorous. (C) Univariate and multivariate logistic regression results for predicting external features on the 3-class pattern. BMI, body mass index; OR, Odds ratio; CI, confidence interval. Bold figures highlight statistically significant in the multivariate logistic regression.
We named the latent profiles based on the overall distribution of the observed variables to distinguish heterogeneity in the circadian rhythms of interns. Three circadian rhythm types were identified: Vigorousness (40.1%, middle Flexible/Rigid-low Languid/Vigorous), Inadaptability (18.6%, low Flexible/Rigid-high Languid/Vigorous), and Flexibility (41.1%, high Flexible/Rigid-middle Languid/Vigorous). Logistic regression analysis showed that gender was the only indicator of circadian rhythm types (OR = 1.97, 95% CI: 1.01–3.83, P = 0.047), after controlling for the covariates (Figure 3C).
Latent profile analysis-based differences in Pittsburgh sleep quality index scores
The PSQI scores were significantly different between Vigorousness and Inadaptability (BF10 = 986.29, d = –0.56) and between Flexibility and Inadaptability (BF10 = 8.14, d = –0.39), but not between Vigorousness and Flexibility (BF10 = 0.35, d = –0.16). These findings were confirmed by Bayesian Factor Robustness analysis (Figure 4).
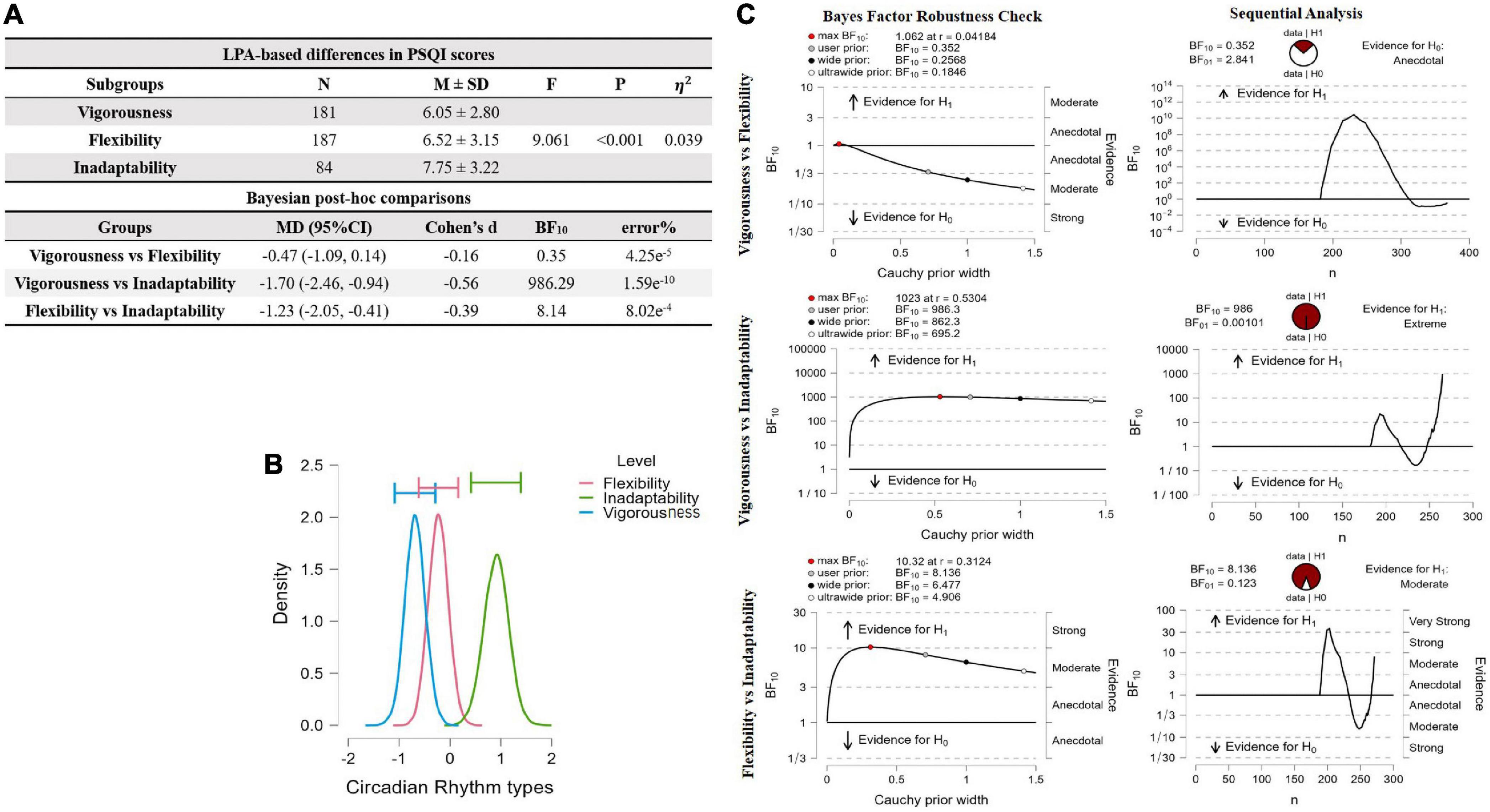
Figure 4. ANOVA comparison of PQSI scores across LPA-based groups and post hoc comparison by Bayesian factor analysis. (A) LPA-based differences on PSQI scores were estimated by Bayesian Factor. V, Vigorous group; F, flexibility group; I, inadaptability group; SD, standard deviation; MD, mean difference; BF, Bayes Factor; η2, eta squared represents the explained unique variance of a dependent variable by three homogenous subgroups. (B) ANOVA model averaged psterior distribution. (C) Inferential plots for Bayesian factor analysis.
Association between circadian rhythm types and sleep quality
Compared with Inadaptability, Vigorousness and Flexibility generally had better sleep quality, especially in interns with no habit of drinking caffeinated drinks, regular diet, ≤2 night-shifts, normal BMI, and mild perceived stress although the P-values for interaction were all not significant (Figure 5).
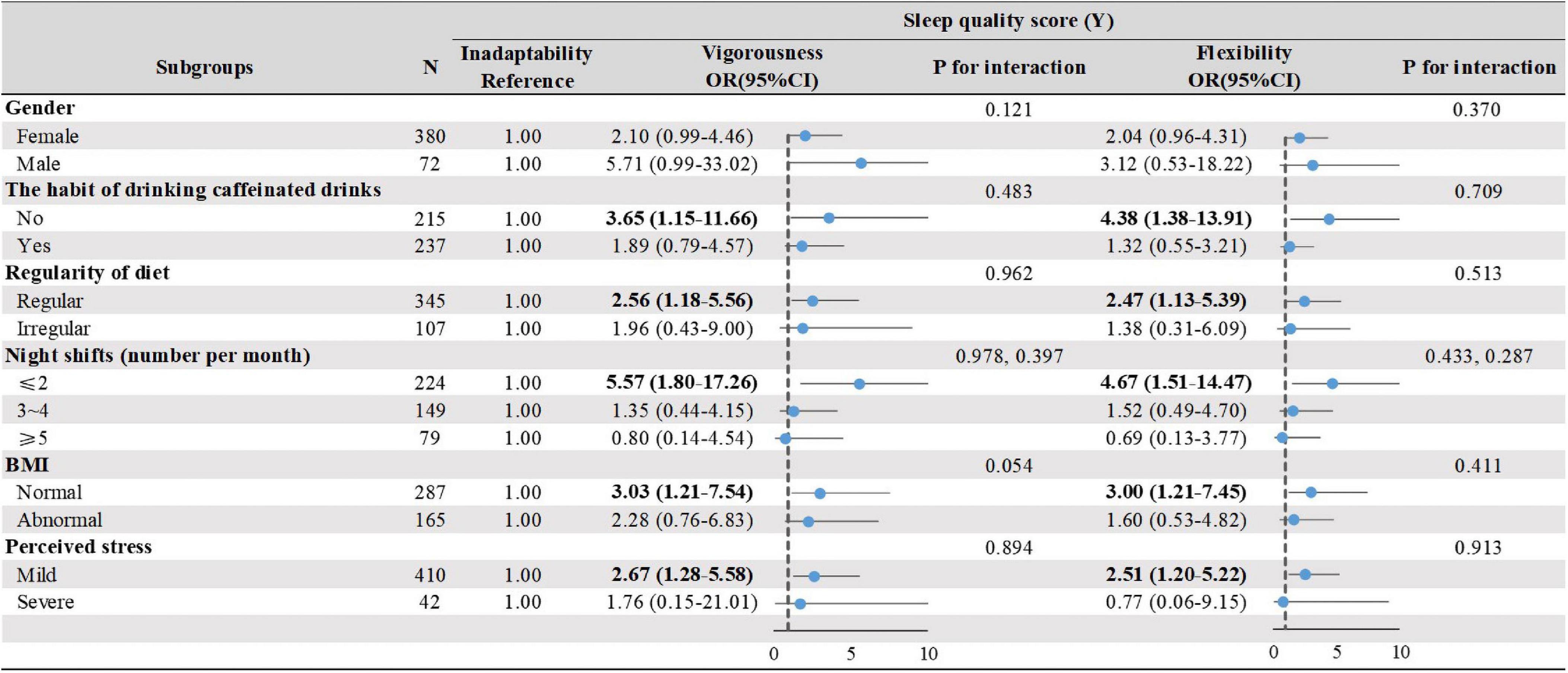
Figure 5. The effect of circadian rhythm subtypes on sleep quality by stratified analysis. Stratified associations between circadian rhythm types and sleep quality by physiological and environmental factors. Analyses were adjusted for covariates gander, the habit of drinking coffee, regularity of diet, night shifts, BMI, PSS when they were not the strata variables. OR, odds ratio; CI, confidence interval. Bold figures highlight statistically significant in the strata variables.
The moderating role of circadian rhythm types between perceived stress and sleep quality
The moderation analyses (Figure 6A) showed that the interactions of perceived stress and circadian rhythm types (Vigorousness vs. Inadaptability, Flexibility vs. Inadaptability) were associated with sleep quality (B = 0.20, SE = 0.07, P = 0.003, and B = 0.20, SE = 0.07, P = 0.004, respectively). However, no significant moderation effect was identified between Vigorousness and Flexibility groups at different levels of stress (B = 0.00, SE = 0.05, P = 0.939). Other information is listed in Figures 6A,B.
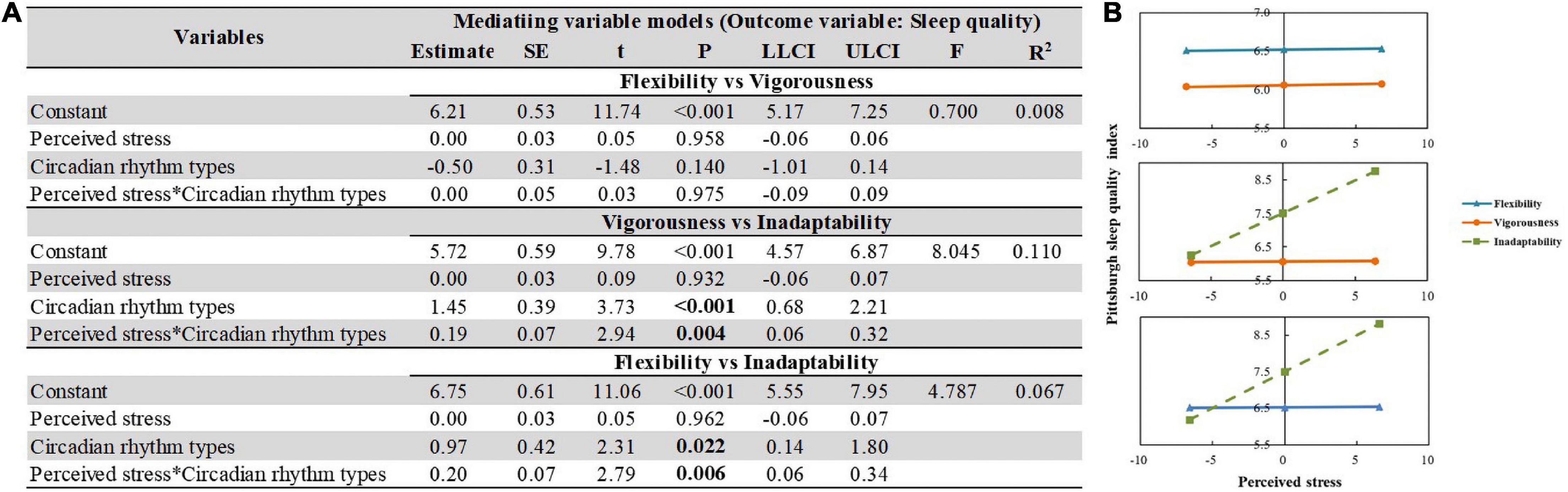
Figure 6. The moderating effect of circadian rhythm types between perceived stress and sleep quality. (A) Moderating role of circadian rhythm types in the association between perceived stress and sleep quantity. Regularity of diet was adjusted for each model. Independent variables were centered before analysis. (B) Simple slope plot of the interaction between circadian rhythm types and perceived stress on sleep quality.
Discussion
This study illustrated the significant impact of night-shift on the sleep quality of nursing interns. We found that 72.3% of the nursing interns did not receive adequate sleep, which is greater than that of nursing students in school (66.0%) (Marta et al., 2020) and the general Chinese population (25.0%) (Sun et al., 2015). According to Bjorvatn and Waage (2013), nurses who work in shifts are more likely to experience confusional arousal and nightmares than nurses who work only during the day. This phenomenon was hypothesized to be related to circadian misalignment and sleep deprivation (D’Ettorre et al., 2020), especially for fresh nurses (Ebrahimi et al., 2016).
This study was the first to examine latent profiles of circadian rhythm by LPA in a sample of nursing interns. Using the LPA, individuals could be categorized into groups share similarity but differ from individuals in other groups (Kongsted and Nielsen, 2017). According to the scoring patterns of the Circadian Type Inventory, they were named as Vigorousness (resilient to decreased sleep time), Inadaptability (vulnerable to sleep problems), and Flexibility (can well regulate unusual working hours). These results confirm the heterogeneity of circadian rhythms. Since the sleep–wake cycle of nursing interns with inadaptability (18.6%) was prone to disorders in the night-shift environment, they need more attention (Zare et al., 2017). In addition, the symptoms of sleepiness may be exacerbated by work fatigue, a reduction in alertness, and inability to recover from sleep (Boivin and Boudreau, 2014). Consistent with previous studies, we found that females were more prone to Flexibility and more resilient to disruptions in circadian rhythms compared with males (Fischer et al., 2017; Anderson and FitzGerald, 2020). The rhythms of estrogen and androgen receptors that act on the suprachiasmatic nucleus (SCN) are ascribed to sexual dimorphism, with females showing higher oscillation amplitudes and peaks for gene expression than males (Anderson and FitzGerald, 2020; Joye and Evans, 2021). The amplitude of the rhythm (i.e., the magnitude of the highest and lowest values of the periodic variation in the physiological system) is related to the adaptive adjustment of shift workers (Rajaratnam et al., 2013). In rodent experiments, female mice were more resilient to the destruction of genes and environment on circadian rhythm (Bixler et al., 2009).
We observed a significant difference in PSQI among three LPA-based circadian subgroups. Vigorousness and Flexibility groups, generally, had better sleep quality, especially in interns with no habit of drinking caffeinated drinks, a regular diet, ≤2 night shifts, normal BMI, and a mild level of perceived stress when compared with Inadaptability. These findings are in line with previous research (Muehlbach and Walsh, 1995; St-Onge et al., 2016; Ono et al., 2020; Ribas-Latre et al., 2021). A cross-sectional study involving 4,856 emergency nurses found that nurses who worked more than four night shifts per month suffered from poorer sleep compared with those who never worked in night shifts (Dong et al., 2020). This discrepancy in findings may be attributed to the age, as the mean age of the participants in this study was 21.19 years (SD = 0.85) compared to 35.30 years (SD = 6.80) in Dong et al. (2020). A study reported that sleep–wake circadian rhythms become disrupted with aging, resulting in more awakenings and night terrors, and less slow-wave sleep (Reilly et al., 1997). Nursing staff with higher age and length of service have lower sleep phase stability and rhythmic amplitudes, indicating a greater tolerance for night shifts than interns (Li et al., 2017; Jacobson and Hoyer, 2022). It should be noted that Vigorousness and Flexibility groups were not able to recover well from night shifts and had no better sleep quality than the Inadaptability group when the night shifts exceeded 2. This phenomenon could also be recognized in interns with severe stress levels.
This study confirmed that circadian rhythm types play significant moderating roles between perceived stress and sleep quality. When exposed to increasing stress, the Flexibility and Vigorousness groups exhibited stable sleep quality, while the Inadaptability group was prone to poor sleep quality. An observational and longitudinal study revealed that medical internship (like stress and night shifts) plays an important role in the worsening of sleep quality and mental health (Tafoya et al., 2019), which is consistent with this study. A random sample of 1,163 participants from Australia showed that both vigorous and flexible rhythms (low amplitude and non-rigid) were significantly more resilient, coped better, and required less daily sleep (Di Milia and Folkard, 2021). The importance of these findings lies in showing that Inadaptability group exhibits low levels of resilience and circadian adaptation, which is reflected in poor sleep quality. Additionally, individuals with high resilience tend to well regulate their emotions in response to stress and exhibit regular circadian cortisol rhythms (Chi et al., 2015). However, these confounders need further validation.
Some preventive interventions should be developed for the Inadaptability group. First, timely identification of interns with Inadaptability especially among those with severe stress and >2 night shifts per month. Second, a 60–90 min nap before a night shift is recommended, which is helpful for the body to complete a sleep cycle (Mednick et al., 2003). Third, moderate and timely intake of caffeinated beverages, such as coffee, tea, and functional drinks, can effectively enhance work alertness and efficiency. Studies have shown that 4 mg/kg is the appropriate intake ratio, but it should not be consumed at least 3 h before bedtime to avoid affecting subsequent rest (Muehlbach and Walsh, 1995). Lastly, Cognitive Behavioral Therapy for Insomnia (CBT-I) could also be recommended if necessary (Newsom, 2022).
Limitations
Inevitably, the study has certain limitations. (1) The sample was collected from three universities in southeast China, which might not be representative resulting in selective bias. Thus, the findings of this study require further validation in a new sample with different backgrounds. (2) This study was cross-sectional in nature; hence, a causal relationship could not be determined, and a longitudinal study should be performed to replicate these findings. An ongoing 2-year follow-up assessment of this cohort (BRNC) will provide additional insights in the future. (3) The study included only questionnaire data for sleep, which does not match the objective observations. Hence, objective sleep data are required to validate these findings in future studies. Biological indicators, such as menstrual cycle, body temperature, melatonin, and cortisol, could be incorporated as objective calibrations of circadian rhythms, which will provide more insights into future research. (4) Several important confounders, including resilience (Liang et al., 2022; Mei et al., 2022a,c; Wu et al., 2022), and social support, could be considered in the mediation analysis resulting in improved fitting indicators.
Conclusion
There is a high prevalence of poor sleep quality among nursing interns. The circadian rhythms of nursing interns are heterogeneous and attention should be paid to those with the Inadaptability type. Additionally, the circadian rhythm subtypes moderate the association between perceived stress and sleep quality. Reasonable shift schedules and decreasing occupational stress should be considered when exploring preventive measures for poor sleep among nursing interns.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of The First Affiliated Hospital of Guangzhou University of Chinese Medicine [No: ZYYEC-ERK (2020) 132]. The patients/participants provided their written informed consent to participate in this study.
Author contributions
XW: conceptualization, data curation, methodology, software, and writing—original draft. YL: investigation, resources, and validation. XX, RC, NZ, and CZ: investigation and resources. ZY: supervision and writing—review and editing. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Natural Science Foundation of China (No. 72274043), the Administration of Traditional Chinese Medicine of Guangdong Province, China (No. 20231106), the Humanity and Social Science Foundation of Guangzhou (No. 2021GZGJ57), and the Special Projects of Humanities and Social Sciences at Guangzhou University of Chinese Medicine (No. 2020SKXK01).
Acknowledgments
We would like to thank nurse directors from participating universities for supporting data collection and all the participants for completing surveys. We thank Bullet Edits Limited for the linguistic editing and proofreading of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Anderson, S. T., and FitzGerald, G. A. (2020). Sexual dimorphism in body clocks. Science 369, 1164–1165. doi: 10.1126/science.abd4964
Axelsson, J., Akerstedt, T., Kecklund, G., and Lowden, A. (2004). Tolerance to shift work-how does it relate to sleep and wakefulness? Int. Arch. Occup. Environ. Health 77, 121–129. doi: 10.1007/s00420-003-0482-1
Bixler, E. O., Papaliaga, M. N., Vgontzas, A. N., Lin, H. M., Pejovic, S., Karataraki, M., et al. (2009). Women sleep objectively better than men and the sleep of young women is more resilient to external stressors: Effects of age and menopause. J. Sleep Res. 18, 221–228. doi: 10.1111/j.1365-2869.2008.00713.x
Bjorvatn, B., and Waage, S. (2013). Bright light improves sleep and psychological health in shift working nurses. J. Clin. Sleep Med. 9, 647–648. doi: 10.5664/jcsm.2826
Boivin, D. B., and Boudreau, P. (2014). Impacts of shift work on sleep and circadian rhythms. Pathol. Biol. (Paris) 62, 292–301. doi: 10.1016/j.patbio.2014.08.001
Buysse, D. J., Reynolds, C. F. III, Monk, T. H., Berman, S. R., and Kupfer, D. J. (1989). The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 28, 193–213. doi: 10.1016/0165-1781(89)90047-4
Chang, W. P., and Li, H. B. (2019). Differences in workday sleep fragmentation, rest-activity cycle, sleep quality, and activity level among nurses working different shifts. Chronobiol. Int. 36, 1761–1771. doi: 10.1080/07420528.2019.1681441
Chen, D., Jiang, M., Shi, X., Geng, F., Qi, H., Zhang, Y., et al. (2020). Predictors of the initiation of shift work disorder among Chinese intern nurses: A prospective study. Sleep Med. 68, 199–206. doi: 10.1016/j.sleep.2019.11.1263
Chen, H. L., Wang, H. Y., Lai, S. F., and Ye, Z. J. (2022). The associations between psychological distress and academic burnout: A mediation and moderation analysis. Psychol. Res. Behav. Manag. 15, 1271–1282. doi: 10.2147/prbm.s360363
Chi, P., Slatcher, R. B., Li, X., Zhao, J., Zhao, G., Ren, X., et al. (2015). Perceived stigmatization, resilience, and diurnal cortisol rhythm among children of parents living with HIV. Psychol. Sci. 26, 843–852. doi: 10.1177/0956797615572904
Choi, A. Y., Nylund-Gibson, K., Israel, T., and Mendez, S. E. A. (2019). A latent profile analysis of bisexual identity: Evidence of within-group diversity. Arch. Sex. Behav. 48, 113–130. doi: 10.1007/s10508-018-1325-1
Cohen, J. (2013). Statistical power analysis for the behavioral sciences. New York, NY: Routledge. doi: 10.4324/9780203771587
Cohen, S. (1988). “Perceived stress in a probability sample of the United States,” in The social psychology of health, eds S. Spacapan and S. Oskamp (Thousand Oaks, CA: Sage Publications, Inc).
D’Ettorre, G., Pellicani, V., Caroli, A., and Greco, M. (2020). Shift work sleep disorder and job stress in shift nurses: Implications for preventive interventions. Med. Lav. 111, 195–202. doi: 10.23749/mdl.v111i3.9197
Di Milia, L., and Folkard, S. (2021). More than morningness: The effect of circadian rhythm amplitude and stability on resilience, coping, and sleep duration. Front. Psychol. 12:782349. doi: 10.3389/fpsyg.2021.782349
Di Milia, L., Smith, P. A., and Folkard, S. (2004). Refining the psychometric properties of the circadian type inventory. Pers. Individ. Dif. 36, 1953–1964. doi: 10.1016/j.paid.2003.08.003
Di Milia, L., Smith, P. A., and Folkard, S. (2005). A validation of the revised circadian type inventory in a working sample. Pers. Individ. Dif. 39, 1293–1305.
Di Muzio, M., Diella, G., Di Simone, E., Pazzaglia, M., Alfonsi, V., Novelli, L., et al. (2021). Comparison of sleep and attention metrics among nurses working shifts on a forward- vs backward-rotating schedule. JAMA Netw. Open 4:e2129906. doi: 10.1001/jamanetworkopen.2021.29906
Dong, H., Zhang, Q., Zhu, C., and Lv, Q. (2020). Sleep quality of nurses in the emergency department of public hospitals in China and its influencing factors: A cross-sectional study. Health Qual. Life Outcomes 18:116. doi: 10.1186/s12955-020-01374-4
Ebrahimi, H., Hassankhani, H., Negarandeh, R., Gillespie, M., and Azizi, A. (2016). Emotional support for new graduated nurses in clinical setting: A qualitative study. J. Caring Sci. 5, 11–21. doi: 10.15171/jcs.2016.002
Facco, F. L., Grobman, W. A., Reid, K. J., Parker, C. B., Hunter, S. M., Silver, R. M., et al. (2017). Objectively measured short sleep duration and later sleep midpoint in pregnancy are associated with a higher risk of gestational diabetes. Am. J. Obstet. Gynecol. 217, 447.e1–447.e13. doi: 10.1016/j.ajog.2017.05.066
Fido, A., and Ghali, A. (2008). Detrimental effects of variable work shifts on quality of sleep, general health and work performance. Med. Princ. Pract. 17, 453–457. doi: 10.1159/000151566
Fischer, D., Lombardi, D. A., Marucci-Wellman, H., and Roenneberg, T. (2017). Chronotypes in the US – influence of age and sex. PLoS One 12:e0178782. doi: 10.1371/journal.pone.0178782
Flo, E., Pallesen, S., Magerøy, N., Moen, B. E., Grønli, J., Hilde Nordhus, I., et al. (2012). Shift work disorder in nurses–assessment, prevalence and related health problems. PLoS One 7:e33981. doi: 10.1371/journal.pone.0033981
Folkard, S., Monk, T. H., and Lobban, M. C. (1979). Towards a predictive test of adjustment to shift work. Ergonomics 22, 79–91. doi: 10.1080/00140137908924591
Gao, J., Wang, F., Guo, S., and Hu, F. (2021). Mental health of nursing students amid coronavirus disease 2019 pandemic. Front. Psychol. 12:699558. doi: 10.3389/fpsyg.2021.699558
Gross, G., Maruani, J., Vorspan, F., Benard, V., Benizri, C., Brochard, H., et al. (2020). Association between coffee, tobacco, and alcohol daily consumption and sleep/wake cycle: An actigraphy study in euthymic patients with bipolar disorders. Chronobiol. Int. 37, 712–722. doi: 10.1080/07420528.2020.1725542
Hastings, M., O’Neill, J. S., and Maywood, E. S. (2007). Circadian clocks: Regulators of endocrine and metabolic rhythms. J. Endocrinol. 195, 187–198. doi: 10.1677/joe-07-0378
Huang, Q., Tian, C., and Zeng, X. T. (2021). Poor sleep quality in nurses working or having worked night shifts: A cross-sectional study. Front. Neurosci. 15:638973. doi: 10.3389/fnins.2021.638973
Jacobson, L. H., and Hoyer, D. (2022). Losing sleep with age. Science 375, 816–817. doi: 10.1126/science.abo1822
Jafari Roodbandi, A., Choobineh, A., and Daneshvar, S. (2015). Relationship between circadian rhythm amplitude and stability with sleep quality and sleepiness among shift nurses and health care workers. Int. J. Occup. Saf. Ergon. 21, 312–317. doi: 10.1080/10803548.2015.1081770
Joye, D. A. M., and Evans, J. A. (2021). Sex differences in daily timekeeping and circadian clock circuits. Semin. Cell Dev. Biol. 126, 45–55. doi: 10.1016/j.semcdb.2021.04.026
Kongsted, A., and Nielsen, A. M. (2017). Latent class analysis in health research. J. Physiother. 63, 55–58. doi: 10.1016/j.jphys.2016.05.018
Lai, J., Ma, S., Wang, Y., Cai, Z., Hu, J., Wei, N., et al. (2020). Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
Li, P., Morris, C. J., Patxot, M., Yugay, T., Mistretta, J., Purvis, T. E., et al. (2017). Reduced tolerance to night shift in chronic shift workers: Insight from fractal regulation. Sleep 40:zsx092. doi: 10.1093/sleep/zsx092
Liang, M. Z., Tang, Y., Knobf, M. T., Molassiotis, A., Chen, P., Hu, G. Y., et al. (2022). Resilience index improves prediction of 1-year decreased quality of life in breast cancer. J. Cancer Surviv. 16, 940–947. doi: 10.1007/s11764-022-01239-3
Marta, O. F. D., Kuo, S. Y., Bloomfield, J., Lee, H. C., Ruhyanudin, F., Poynor, M. Y., et al. (2020). Gender differences in the relationships between sleep disturbances and academic performance among nursing students: A cross-sectional study. Nurse Educ. Today 85:104270. doi: 10.1016/j.nedt.2019.104270
Mednick, S., Nakayama, K., and Stickgold, R. (2003). Sleep-dependent learning: A nap is as good as a night. Nat. Neurosci. 6, 697–698. doi: 10.1038/nn1078
Mei, X. X., Wu, X. N., Wang, H. Y., Wu, J. Y., Wang, X. Q., and Ye, Z. J. (2022c). Heterogeneity in psychological resilience and mental health among newly graduated nursing students: A latent profile and generalized additive model analysis. Psychol. Res. Behav. Manag. 15, 597–606. doi: 10.2147/prbm.s348661
Mei, X., Wang, H., Wang, X., Wu, X., Wu, J., and Ye, Z. (2022a). Associations among neuroticism, self-efficacy, resilience and psychological distress in freshman nursing students: A cross-sectional study in China. BMJ Open 12:e059704. doi: 10.1136/bmjopen-2021-059704
Mei, X. X., Wang, H. Y., Wu, X. N., Wu, J. Y., Lu, Y. Z., and Ye, Z. J. (2022b). Self-efficacy and professional identity among freshmen nursing students: A latent profile and moderated mediation analysis. Front. Psychol. 13:779986. doi: 10.3389/fpsyg.2022.779986
Molero Jurado, M. D. M., Pérez-Fuentes, M. D. C., Martos Martínez, Á, Barragán Martín, A. B., Simón Márquez, M. D. M., and Gázquez Linares, J. J. (2021). Emotional intelligence as a mediator in the relationship between academic performance and burnout in high school students. PLoS One 16:e0253552. doi: 10.1371/journal.pone.0253552
Muehlbach, M. J., and Walsh, J. K. (1995). The effects of caffeine on simulated night-shift work and subsequent daytime sleep. Sleep 18, 22–29. doi: 10.1093/sleep/18.1.22
Muthén, L. K., and Muthén, B. (2017). Mplus user’s guide: Statistical analysis with latent variables, user’s guide. Los Angeles, CA: Muthén & Muthén.
Newsom, R. (2022). Cognitive behavioral therapy for insomnia (CBT-I). Arlington, VA: Sleep Foundation.
Ng, S. M. (2013). Validation of the 10-item Chinese perceived stress scale in elderly service workers: One-factor versus two-factor structure. BMC Psychol. 1:9. doi: 10.1186/2050-7283-1-9
Ono, D., Mukai, Y., Hung, C. J., Chowdhury, S., Sugiyama, T., and Yamanaka, A. (2020). The mammalian circadian pacemaker regulates wakefulness via CRF neurons in the paraventricular nucleus of the hypothalamus. Sci. Adv. 6:eabd0384. doi: 10.1126/sciadv.abd0384
Pallesen, S., Thun, E., Waage, S., Vedaa, Ø, Harris, A., Blytt, K. M., et al. (2021). Stability and change of the personality traits languidity and flexibility in a sample of nurses: A 7-8 years follow-up study. Front. Psychol. 12:652569. doi: 10.3389/fpsyg.2021.652569
Peng, X., Li, J., Han, B., Zhu, Y., Cheng, D., Li, Q., et al. (2022). Association of occupational stress, period circadian regulator 3 (PER3) gene polymorphism and their interaction with poor sleep quality. J. Sleep Res. 31:e13390. doi: 10.1111/jsr.13390
Qi, H., Shi, X., Li, L., Yang, L., and Fan, F. (2019). Reliability and validity of the Chinese version of circadian type inventory in nurses on shifts. Chin. J. Clin. Psychol. 27, 258–262. doi: 10.16128/j.cnki.1005-3611.2019.02.009
Quintana, D. S., and Williams, D. R. (2018). Bayesian alternatives for common null-hypothesis significance tests in psychiatry: A non-technical guide using JASP. BMC Psychiatry 18:178. doi: 10.1186/s12888-018-1761-4
Rajaratnam, S. M., Howard, M. E., and Grunstein, R. R. (2013). Sleep loss and circadian disruption in shift work: Health burden and management. Med. J. Aust. 199, S11–S15. doi: 10.5694/mja13.10561
Reilly, T., Waterhouse, J., and Atkinson, G. (1997). Aging, rhythms of physical performance, and adjustment to changes in the sleep-activity cycle. Occup. Environ. Med. 54, 812–816. doi: 10.1136/oem.54.11.812
Ribas-Latre, A., Santos, R. B., Fekry, B., Tamim, Y. M., Shivshankar, S., Mohamed, A. M. T., et al. (2021). Cellular and physiological circadian mechanisms drive diurnal cell proliferation and expansion of white adipose tissue. Nat. Commun. 12:3482. doi: 10.1038/s41467-021-23770-0
St-Onge, M. P., Mikic, A., and Pietrolungo, C. E. (2016). Effects of diet on sleep quality. Adv. Nutr. 7, 938–949. doi: 10.3945/an.116.012336
Sun, M., Feng, W., Wang, F., Zhang, L., Wu, Z., Li, Z., et al. (2018). Night shift work exposure profile and obesity: Baseline results from a Chinese night shift worker cohort. PLoS One 13:e0196989. doi: 10.1371/journal.pone.0196989
Sun, W., Yu, Y., Yuan, J., Li, C., Liu, T., Lin, D., et al. (2015). Sleep duration and quality among different occupations–China national study. PLoS One 10:e0117700. doi: 10.1371/journal.pone.0117700
Swanson, S. A., Lindenberg, K., Bauer, S., and Crosby, R. D. (2012). A Monte Carlo investigation of factors influencing latent class analysis: An application to eating disorder research. Int. J. Eat. Disord. 45, 677–684. doi: 10.1002/eat.20958
Tafoya, S. A., Aldrete-Cortez, V., Ortiz, S., Fouilloux, C., Flores, F., and Monterrosas, A. M. (2019). Resilience, sleep quality and morningness as mediators of vulnerability to depression in medical students with sleep pattern alterations. Chronobiol. Int. 36, 381–391. doi: 10.1080/07420528.2018.1552290
Ulhôa, M. A., Marqueze, E. C., Burgos, L. G., and Moreno, C. R. (2015). Shift work and endocrine disorders. Int. J. Endocrinol. 2015:826249.
Wu, X., Lu, Y., Zhang, Q., Wang, H., Sun, X., Han, H., et al. (2022). Stress/resource complex, sense of coherence and professional identity among nursing students: A latent profile and mediation analysis. Psychol. Res. Behav. Manag. 15, 2409–2420. doi: 10.2147/prbm.s378088
Zare, R., Choobineh, A., and Keshavarzi, S. (2017). Association of amplitude and stability of circadian rhythm, sleep quality, and occupational stress with sickness absence among a gas company employees-a cross sectional study from Iran. Saf. Health Work 8, 276–281. doi: 10.1016/j.shaw.2016.09.007
Zhang, L., and Jain, M. K. (2021). Circadian regulation of cardiac metabolism. J. Clin. Invest. 131:e148276. doi: 10.1172/jci148276
Keywords: perceived stress, circadian rhythm, sleep quality, latent profile analysis, moderation analysis, Be Resilient to Nursing Career (BRNC), nursing interns
Citation: Wu X, Lu Y, Xie X, Chen R, Zhang N, Zhou C and Ye Z (2022) Association between circadian rhythm and sleep quality among nursing interns: A latent profile and moderation analysis. Front. Neurosci. 16:995775. doi: 10.3389/fnins.2022.995775
Received: 20 August 2022; Accepted: 17 October 2022;
Published: 03 November 2022.
Edited by:
Andrew W. McHill, Oregon Health and Science University, United StatesReviewed by:
Anne M. Fink, University of Illinois at Chicago, United StatesTingting Cai, Fudan University, China
Copyright © 2022 Wu, Lu, Xie, Chen, Zhang, Zhou and Ye. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zengjie Ye, emVuZ2ppZXllQHFxLmNvbQ==
 Xiaona Wu
Xiaona Wu Yingzi Lu
Yingzi Lu Xian Xie
Xian Xie Rongjie Chen
Rongjie Chen Ningning Zhang
Ningning Zhang Chen Zhou
Chen Zhou Zengjie Ye
Zengjie Ye