
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurosci. , 13 October 2022
Sec. Autonomic Neuroscience
Volume 16 - 2022 | https://doi.org/10.3389/fnins.2022.971958
This article is part of the Research Topic Advances in Understanding the Effects of Stress on the Brain and the Autonomic Nervous System View all 4 articles
Objectives: Mindfulness-based interventions (MBI) can reduce both stress and depressive symptoms. However, the impact of mindfulness on stress level in depressed subjects remains unclear. This study aims to assess electrophysiological correlates of mindfulness in patients with major depressive disorder (MDD) at baseline, under stress exposure, and in relaxation following stress exposure.
Methods: Perceived mindfulness was assessed with the Freiburger Mindfulness Inventory (FMI) in 89 inpatients (mean age 51) with MDD [mean Beck Depression Inventory (BDI) 30]. Electrophysiological parameters [resting heart rate (RHR), heart rate variability (HRV), respiration rate, skin conductance, and skin temperature] were recorded at 5-min baseline, 1-min stress exposure, and 5-min self-induced relaxation.
Results: Freiburger Mindfulness Inventory was strongly inversely correlated with symptom severity measured by BDI (r = –0.53, p < 0.001). No correlations between FM score and electrophysiological parameters in any of the three conditions (baseline, stress exposure, relaxed state) could be found. The factor openness was associated with higher VLF (very low frequency of HRV) in the baseline condition. However, this correlation was no more significant after regression analysis when corrected for respiratory rate, age, and sex.
Conclusion: Autonomous nervous reactivity in depression was not associated with perceived mindfulness as measured by FMI score and presented electrophysiological parameters, despite the strong inverse correlation between state mindfulness and symptom severity.
Mindfulness-based interventions (MBI) integrated the essence of traditional mindfulness practice with contemporary psychological practice and have recently gained much interest in the scientific world and in the therapy of depression (Hofmann et al., 2010; Gu et al., 2015; Segal and Walsh, 2016; Bulzacka et al., 2018; Cladder-Micus et al., 2018; Geurts et al., 2020; Ninomiya et al., 2020).
The mindfulness literature to date shows considerable variance in how mindfulness can be defined. Mindfulness may be conceptualized as a state, a trait, or an outcome of an intervention (Scavone et al., 2020). Additionally, the dimensionality of mindfulness is debated, with some researchers emphasizing one-dimensionality (Brown and Ryan, 2003) and others assuming multidimensionality (Baer et al., 2006). Mindfulness is usually defined by two core dimensions—present-moment attention and non-judgmental acceptance (Kabat-Zinn, 1994; Ludwig and Kabat-Zinn, 2008; Chambers et al., 2009; Davidson, 2010). An often cited definition of mindfulness is “paying attention in a particular way: on purpose, in the present moment, and non-judgmentally (Kabat-Zinn, 1994).
In literature, many possible hypothesized mechanisms underlying the effects of MBI in depression can be found: decrease in repetitive negative thinking (Gu et al., 2015), emotional regulation via exposure and extinction/habituation (Hölzel et al., 2011; Treanor, 2011), decentering (Fresco et al., 2007), self-kindness, and self-compassion (Neff, 2003; Hölzel et al., 2011; Van Dam et al., 2011) as well as a wider range of coping skills (Shapiro et al., 2006; Vago and Silbersweig, 2012).
There is evidence that mindfulness interventions are associated with reduced stress levels (Tang et al., 2009; Arredondo et al., 2017; Pascoe et al., 2017; Lengacher et al., 2019; Krick and Felfe, 2020). The outcomes included cortisol, inflammatory as well as electrophysiological parameters.
The previous studies assessing stress via electrophysiological parameters, use mostly either heart rate variability (HRV) (Watford et al., 2020; Bortolla et al., 2021; Park et al., 2021) or skin conductance (SC) response (Kadziolka et al., 2016). Both parameters dominate the arousal assessment in depression and suicidality: Recent review by McCall et al. (2022) regarding ANS assays and suicidality included 21 studies, 14 of them used HRV, and six studies used skin conductance as a biomarker. In MBI research, HRV has become an increasingly utilized biomarker (Christodoulou et al., 2020).
HRV is a measure of the variability in intervals between consecutive heartbeats is an indirect assessment of cardiac autonomic activity (Sztajzel, 2004; Billman, 2011; Koenig and Thayer, 2016). Similarly, impaired/lower HRV has been repeatedly associated with stress, depression as well as other psychiatric conditions (Lin et al., 2011; Alvares et al., 2016; Hartmann et al., 2018; Huang et al., 2018; Järvelin-Pasanen et al., 2018; Heiss et al., 2021). Most of he research in this field uses time and frequency domains, alternative measures include geometric and non-linear measures (Heart Rate Variability, 1996; Kleiger et al., 2005). It must be emphasized that HRV only provides an indirect assessment of cardiac autonomic activity and does not provide a direct measurement of either cardiac parasympathetic or sympathetic activity (Billman, 2013). Studies with non-clinical samples that included HRV assessment demonstrated mostly positive effects of MBI on HRV immediately after the intervention (Christodoulou et al., 2020; Krick and Felfe, 2020) as well as in follow-up at week 20 (Arredondo et al., 2017). Similarly, an increase in HRV after Zen or Vipassana meditation compared to baseline has been reported (Wu and Lo, 2008; Krygier et al., 2013).
However, there are also contrary findings (Nijjar et al., 2014), partly also due to difficulties comparing different conditions and methods (Voss et al., 2020). A meta-analysis of the effects of standardized MBI by focusing on inflammatory parameters and HRV revealed mixed and inconclusive results (Rådmark et al., 2019). Some authors demonstrated robust effects of MBI on stress when measured via self-report, but less clear for physiological measures (Morton et al., 2020). Despite the rising popularity of HRV measurements in the assessment of stress, there are rising concerns regarding high levels of within-subjects variability in HRV measurements (Uhlig et al., 2020), a variety of HRV measurement protocols (Vila et al., 2019), as well as poorer reliability in real-world recordings (von Rosenberg et al., 2017) and in clinical populations (Sandercock et al., 2005) compared to lab-based scenarios or healthy populations. Some authors suggest the use of broader analyzing tools instead of HRV only (Schumann et al., 2017; Sarlon et al., 2018).
The vast majority of studies addressing the link between mindfulness and physiological changes are based on healthy populations (Watford et al., 2020; Bortolla et al., 2021; Park et al., 2021). If a stress induction task is used, participants are also mostly volunteers (Paul et al., 2013; Feldman et al., 2016; Sun et al., 2019). A widely spread approach is also to compare meditation/mindfulness interventions with the control condition (Magalhaes et al., 2018; Belliveau et al., 2021; Cohen et al., 2021; Saltsman et al., 2021) or comparing experienced meditators with novices (Lutz et al., 2016; Rodriguez-Larios et al., 2021).
In clinical samples (patients with relevant depression), mindfulness-based cognitive therapy reduced depressive symptoms but did not let to significant changes in HRV (Wheeler). A recent study on depressed patients of Belliveau et al. (2021) showed that mindfulness-based cognitive therapy in depressed may not be accompanied by changes in the stress-response and inflammatory pathways.
As mentioned above and with regard to the current research of mindfulness and stress/depression, the following main concerns can be expressed, indicating a potential knowledge gap:
• Most of the findings in the literature concern healthy subjects and less depressed patients.
• Findings in clinical samples exploring the effects of mindfulness on HRV are partly contrary to healthy subjects but also in non-clinical samples are the results inconclusive.
• The design of the most studies assessing the influence of mindfulness is comparative/interventional; there is a lack of empirical studies examining state mindfulness.
• Even if popular in German-speaking countries, the Freiburger Mindfulness Inventory (FMI) is usually not a part of the studies assessing mindfulness.
The aim of the present study is, therefore, to assess electrophysiological correlates of perceived mindfulness in patients with major depressive disorder (MDD) using static as well as dynamic measures (indices of the autonomous nervous reactivity) and FMI.
FMI was initially introduced as a 30-item, in the short version a 14-item instrument assessment of present moment attention, non-judgment, and openness (Baer et al., 2006; Walach et al., 2006) and is widely spread in German-speaking clinical settings.
Although our study was primarily explorative, there was one specific hypothesis we aimed to prove. Assuming a potential mediating role of autonomous nervous system activation, we specifically hypothesized that the global mindfulness score (as assessed by FMI) would have an impact on the measured stress level in all three conditions, especially under stress exposure.
In the following section, we report how we selected our sample, all data exclusions, all manipulations, and all measures in the study (Simmons et al., 2011). The data used to derive our statistical inferences are provided as Supplementary material. The study’s design and its analysis were not preregistered.
Over the duration of the study, all new inpatients with MDD were asked to participate. Altogether, 98 inpatients with a diagnosis of unipolar MDD, according to the International Classification of Diseases (ICD-10, 10th edition), based on the clinical examination and interview, entered the study. Exclusion criteria were: bipolar disorder (one subject excluded), other manifest psychiatric disorder as the main diagnosis (three subjects excluded), manifest diabetes mellitus (one subject excluded), manifest neurological disorder (multiple sclerosis, one subject excluded), pathological thyroid-stimulating hormone blood level (two subjects excluded), elevated leukocyte counts (one subject excluded) as well as not compensated arterial hypertonia or heart disease, cancer or other serious medical condition. In case of alcohol use in the history, abstinence from alcohol in the past 4 weeks was required.
The final sample consisted of 89 inpatients (37 women = 42%, mean age 51 years, SD = 11.28, range 23–69). Comorbidity of arterial hypertension was observed in 15 patients, 9 of them on medication. Seven subjects had a history of hypothyroidism, six of them were substituted (levothyroxine). Lumbar syndrome (previous disc prolapse) was reported in three cases, allergy or asthma in six subjects. A total of 31 patients were drug naive, and 58 patients were on psychiatric medication. Antidepressants taken were selective serotonin reuptake inhibitors (SSRI) [escitalopram (12), sertraline (7), citalopram (3)], venlafaxine (13), mirtazapine (13), bupropion (6), vortioxetine (2), and tianeptine (2). Other medications consisted of antihypertensive drugs (nine patients), levothyroxine (six patients), proton pump inhibitors (three patients), asthma spray (in two patients), acetylsalicylic acid, and diclofenac each in one patient. All patients received treatment as usual (TAU) including progressive muscular relaxation or short relaxation 60–90 min per week and have been introduced to the theory of mindfulness in educative group sessions. Specific mindfulness-based therapy (like mindfulness-based stress reduction, MBSR or mindfulness-based cognitive therapy, MBCT) did not take place. Although PMR was a part of the TAU, no slow breathing has been taught. The previous experience with MBI was not systematically assessed.
Overall, we used a repeated measurement design including three time points of measurement: baseline, during stress exposure, and during a relaxation state.
In our study, we decided to use a recall of unpleasant stressful experiences of a medium intensity as a stress exposure. We asked participants to imagine an unpleasant stressful situation from the past of medium intensity and to mark the stress intensity on a visual analog scale (VAS, a horizontal line, 100 mm in length, anchored by word descriptors at each end, and numbered from 0 to 10. The endpoints were “not stressful at all” and “extremely stressful”). The VAS score was determined by measuring in cm from the left end of the line to the patient’s mark. The mean stress intensity measured by VAS was 4.85 (SD = 0.67).
A relaxed state followed the stress exposure: patients should try to relax as much as possible, either with their eyes closed or open, staying in the same position and avoiding all unnecessary movements. They were asked to use their usual strategies to relax as they do in their daily life or in the hospital.
To assess the severity of depressive symptoms, the German version of the BDI (Kühner et al., 2007) was used. Mindfulness was measured using the FMI. Both self-rating tests were administrated prior to the electrophysiological measurements.
Skin conductance (SC) and skin temperature (ST), resting heart rate (RHR), HRV as well as respiration rate (RR) were recorded for 300 s baseline, 60 s stress exposure, and 300 s self-induced relaxation.
Self-reported data (i.e., depression symptoms and mindfulness) were assessed prior to the electrophysiological measurements at baseline. Electrophysiological measurements were recorded as described above.
Beck Depression Inventory II is a revised version of the depression inventory developed by Aaron Beck and consists of 21 items. BDI-II items are rated on a 4-point scale ranging from 0 to 3 based on the severity of each item. The maximum total score is 63. The internal consistency was described as around 0.9 and the retest reliability ranged from 0.73 to 0.96 (Wang and Gorenstein, 2013).
We used the shortened form with 14 items with a Cronbach alpha of 0.86 (the initially 30-item scale with an internal consistency of Cronbach alpha = 0.93) (Walach et al., 2006). Participants should provide an answer for every statement as best they can, choosing one of the following answers: Rarely—occasionally—fairly often—almost always. The score for each item varies from one to four points, given a range of total scores between 14 and 56.
Electrophysiological data were acquired using the NeXus-10 system (NeXus-10 Mark II®, Biotrace +) and were recorded at a sampling rate of 1,024 Hz. For heart rate and HRV recording, a blood volume pulse finger clip sensor was used. To measure SC, Velcro tape with integrated Ag/AgCl electrodes was placed at the middle phalanx of the index finger and the ring finger of the left hand. For the measurement of ST, the NeXus temperature sensor was placed on the middle finger of the left hand and taped to the finger at two positions to ensure stability.
To measure RR, an elastic belt with a breathing sensor was fixed around the lower thorax at the diaphragm, according to the manufacturer’s instructions. The same procedures were used for all study participants to ensure that the data from all individuals were comparable. All measurements were taken in the same room and under the same conditions: sitting, slightly inclined position with eyes open. During the baseline recording, all subjects were asked to breathe normally, not talk, and to avoid all unnecessary movements. Furthermore, to reduce the impact of pre-test activities, they were asked to sit and not move for 5 min prior to placement of the electrodes.
Recording and primary analysis of all electrophysiological parameters were performed using the BioTrace + software. For the analysis of HRV, time- and frequency-domain parameters and records 5 min in length with a sampling rate of 1,024 Hz were used, according to recognized standards (Heart Rate Variability, 1996). The power frequency spectrum of HRV was subsequently quantified in standard frequency-domain measurements, such as total variance, high-frequency (HF, 0.15–0.4 Hz), low-frequency (LF, 0.04–0.15 Hz), very-low-frequency (VLF, 0–0.04 Hz), and LF/HF ratio. For the time domain, principal parameters such as beat-to-beat interval (RR or NN-interval), the standard deviation of the beat-to-beat interval (SDNN), and the root mean square of successive differences (RMSSD) were used.
Prior to the analyses, all parameters were visually controlled on a 15-s window, and artifacts in the RHR and HRV parameters due to the movement were removed. Artifacts due to device failure in the SC or ST were also removed. Measurements with more than 5% artifacts were excluded; this was the case in four measurements of SC as well as in five measurements of RHR and HRV parameters.
Statistical analyses were performed using R-Studio software (version 1.2). First, a descriptive analysis has been performed to summarize the sample. Median and mean have been used as indicators of central tendency, range, and standard deviation as indicators of variability. Second, a correlation analysis has been conducted. To choose the appropriate statistical tool, the normality of the distribution was assessed using the Shapiro–Wilk test. Variables have been considered as not normally distributed, it the p-value was less than α = 0.05. RR and RHR met the normality assumption. FMI score missed with p = 0.047 the criteria, the single items were not normally distributed either. ST, SC, and HRV parameters were also found not to be normally distributed; moreover, they were extremely skewed. For that reason, we log-transformed all electrophysiological parameters, and the log-transformed HRV values were normally distributed. For normally distributed variables, a Pearson correlation analysis was used; non-normally distributed variables were assessed for correlation using Spearman’s correlation. Third, multistep linear regression controlling for age and sex has been performed, using the command “lm” in R-studio (free version 3.6.3 with R stats and utils, datasets, formal methods, and classes packages as well as dplyr and ggpubr).
The mean FMI score was 32.79 (SD = 6.31), the mean symptom severity measured by the BDI-II score was 29.66 (severe depression). Table 1 is summarizing the study population and all electrophysiological parameters, Figure 1 is visualizing the group differences. Significant between-group differences could be found in RHR, RR, SDNN, LF, and HF. For more details, see also our previous work (Sarlon et al., 2021).
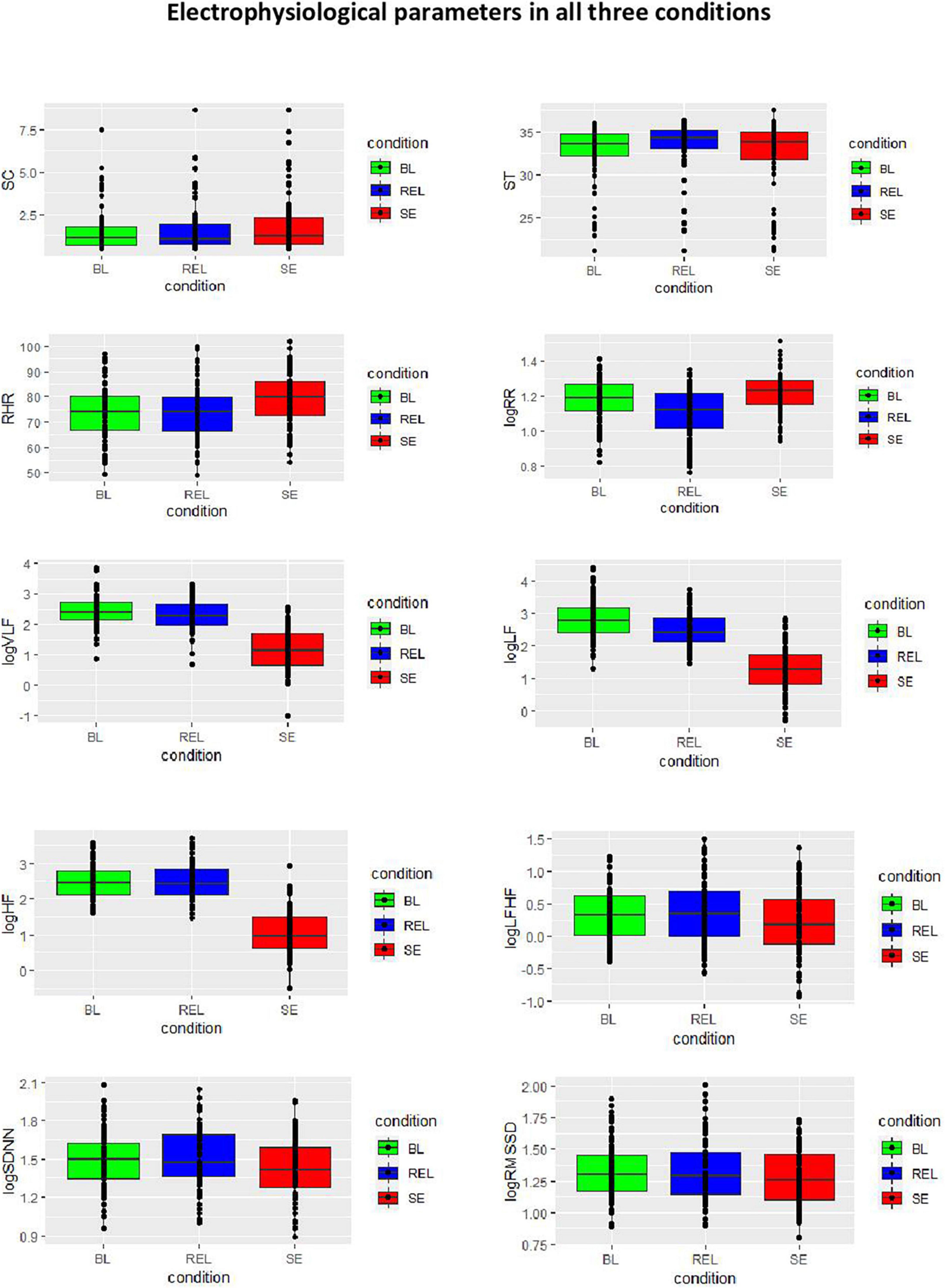
Figure 1. Electrophysiological parameters in all three conditions. SC, skin conductance; ST, skin temperature; RHR, resting heart rate; RR, respiration rate per minute; HRV, heart rate variability; SDDN, standard deviation of beat-to-beat intervals; RMSSD, root mean square of successive differences; VLF, very low frequency; LF, low frequency; HF, high frequency.
The performed correlation analysis (see also section “Materials and methods”) can be characterized by two main steps. At the first step, we correlated the FMI total score with all measured parameters in every condition (baseline, stress exposure, and relaxed state) as well as between the FMI total score and the differences (change scores) of electrophysiological parameters between all three conditions (example: FMI score and the difference between RR at baseline and under stress exposure) (Table 2). A strong, inverse correlation between symptom severity (BDI score) and perceived mindfulness (FMI score) could be observed (Pearson’s r = –0.53, p = 6.7 × 10–8). There was no correlation between FMI score and electrophysiological parameters or other assessed influencing factors.
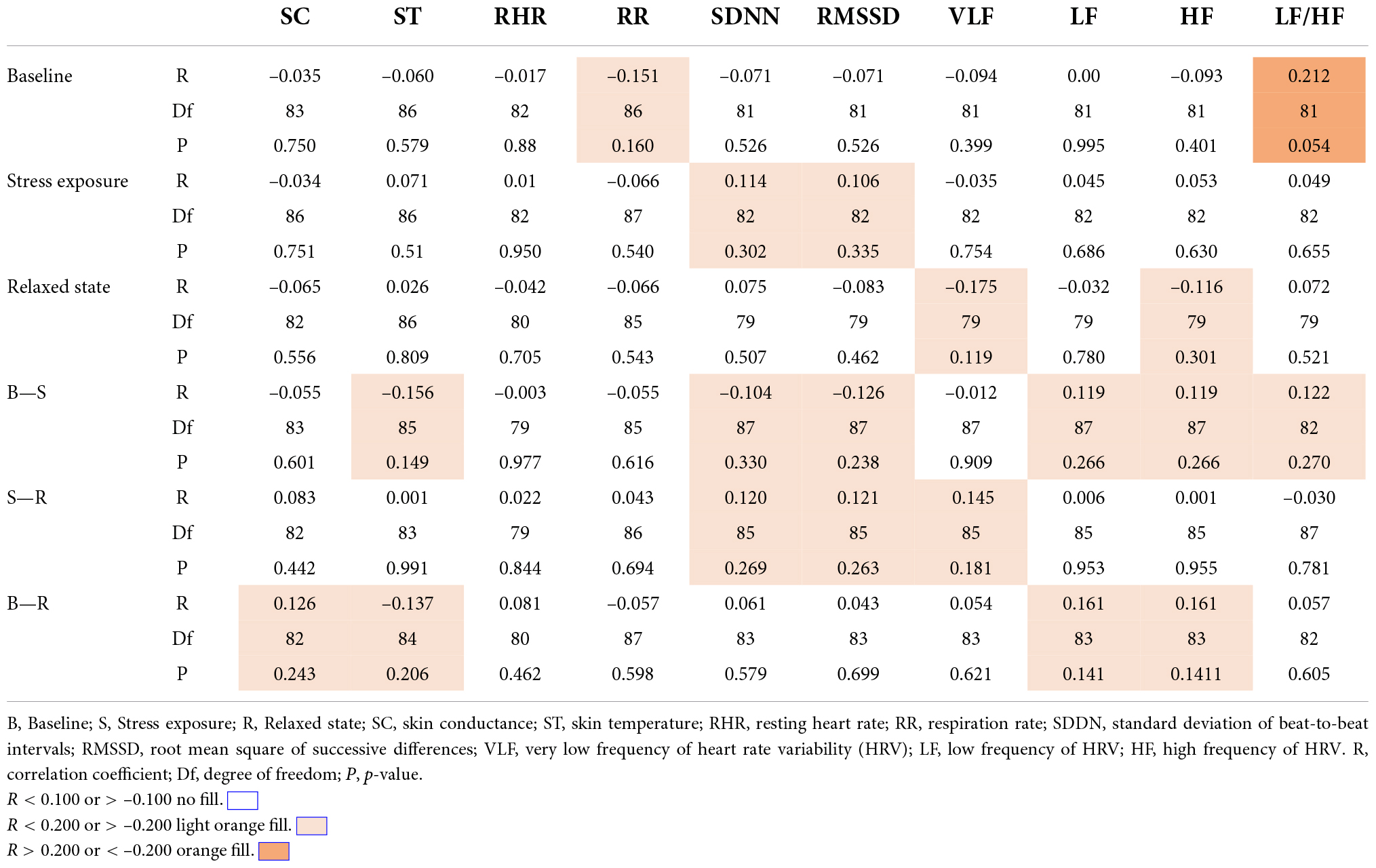
Table 2. Correlation of FMI and electrophysiological parameters across the three different conditions.
In the next step, we compared the three main factors as postulated by the authors of FMI (see Figure 2) with the electrophysiological parameters in different stages. The third factor, “Openness” correlated with VLF at baseline (Spearman’s rho = –0.246, p = 0.025), no other correlation could be observed.
Assessed HRV indicators are described above (see section “Pre-processing and analysis”). In the following, some HRV indicators are briefly summarized. Both parasympathetic and sympathetic systems are believed to contribute to SDNN, which is highly correlated with ULF, VLF, and LF. For short-term recording, ULF will not be assessed. The RMSSD is believed to be more influenced by parasympathetic system than sympathetic system than SDNN. Experimental evidence suggests that VLF is modulated by physical activity and stress responses. The HF band reflects parasympathetic activity and corresponds to the HR variations related to the respiratory cycle (Shaffer and Ginsberg, 2017). The inclusion of LF/HF-ratio in our overview has a historic background (previously suggested as an index of sympatho–vagal balance). At this point it should be clearly stated, that available data challenge this interpretation, showing that LF is determined by both sympathetic and parasympathetic systems as being an index of sympathetic activity (Houle and Billman, 1999; Heathers, 2012; Billman, 2013; Reyes del Paso et al., 2013).”
The role of influencing factors was an object of the previous author’s work (Sarlon et al., 2021).
Briefly summarized, symptom severity measured by BDI score was associated with higher SC under stress exposure and with a lower RR in the relaxed state. Age and higher blood pressure were both associated with lower HRV and higher RHR. Significant gender differences could be demonstrated in the relaxed state only: LF was higher in men compared to women. Higher body mass index was associated with higher ST at baseline, stress exposure, and in a relaxed state. (Tobacco) smokers showed lower HF under stress exposure than non-smokers.
Since age was the most influencing factor for the measures at baseline and in a relaxed state, we conducted multiple linear correlation analyses with correction for age. In addition, we corrected VLF parameters for respiratory rate (RR interferes with a high frequency of HRV) as well as for sex (significant sex differences). The correlation between openness and VLF was no more significant after multiple correlation analyses (p = 0.09).
The main objective of this primary explorative study was to examine electrophysiological correlates of perceived mindfulness as assessed by FMI at baseline, under stress exposure and in a relaxed state. To our knowledge, no study so far has addressed this question.
A deeper understanding of the link between perceived mindfulness and physiological response in MDD might be highly relevant since the physiological reactivity in MDD is altered and MBI aim to improve depressive symptoms.
No correlations between the FMI-total score and the assessed parameters could be observed, contrary to our hypothesis. Interestingly, our finding of a strong inverse correlation between symptom severity and perceived mindfulness (r = –0.53) is in line (even exactly the same value) with a meta-analysis comprising 157 distinct samples and 44,075 participants using the Five Facet Mindfulness Questionnaire (r = –0.53) (Carpenter et al., 2019).
There are mainly two possible explanations for the presented results according to the literature. First, individuals who score higher in FMI might be better “protected” against emotional dysregulation, ruminations, mind-wandering, self-accusations, and other typical symptoms of MDD (Fountain-Zaragoza et al., 2016; Hsieh et al., 2019; Parmentier et al., 2019; Marion-Jetten et al., 2021; Royuela-Colomer et al., 2021). The other explanation might be that in severe depression, the ability to act mindful is reduced, either because of the impairment of the attentional facet of mindfulness (Teasdale et al., 2000; Elices et al., 2019) or because of the lack of acceptance-related capacities (Eisenlohr-Moul et al., 2016; Kotsou et al., 2018). Nayda and Takarangi (2021) pointed out potential harmful effects of mind-wandering through people’s reduced propensity to be mindful. We assume a combination of both aspects.
In literature, there are first attempts to distinguish the effects of different mindfulness components on the stress level. Lindsay et al. (2018) showed that monitoring plus acceptance training reduced cortisol and systolic blood pressure reactivity compared to monitoring only and control training. In our study, the only correlation between FMI factor “openness” and VLF was no more significant after correction for age, sex, and respiratory rate.
The study has a number of strengths. Participants represent a seriously ill population with a mean BDI score of 30. To our knowledge, findings of the relation between state mindfulness and stress level measured by electrophysiological parameters in different conditions in patients with relevant MDD have not been previously published. Furthermore, we analyzed different possible components of mindfulness, given a solid base for further comparisons with another mindfulness scale, different conditions or other clinical populations.
The following limitations should be mentioned. First, possible confounding effects of respiration (Beda et al., 2014) could not be excluded, since no correction for respiratory rate has been performed in the HRV analysis. However, the respiratory rate was widely within the range of 9–24 breath/min, with exception of some measures mostly in the relaxed state. We conclude that in a relaxed state only, the HRV analysis might be affected by the respiratory bias. Second, the limited power (sample size) can be a potential reason for negative findings. Third, there was no systematic assessment of the individual relaxation strategies.
In summary, despite the heterogeneity of mindfulness definitions, the strong inverse correlation with the symptom severity in depressed patients using FMI in our study was identical with the one in a meta-analysis using different questionnaires (Carpenter et al., 2019), which suggests a robust common conceptual background. The presented study indicates that this inverse correlation between mindfulness and depression severity might not be mediated by stress level, using static as well as dynamic measures (indices of the autonomous nervous reactivity) and self-reported mindfulness.
Our results are in line with previous findings regarding similarities and differences between mindfulness and relaxation responses. Some authors point out, that the effects of mindfulness are to discriminate from stress reduction through relaxation response and do not depend on individuals being in a relaxed state either (citation).
Furthermore, this study underlines the important role of influencing factors in the analysis and interpretation of electrophysiological parameters.
Although MBI can reduce both stress level and depressive symptoms, the presented results do not support the hypothesis that the bidirectional associated between mindfulness and depressive symptoms in patients with MDD is mediated by ANS reactivity as measured by electrophysiological parameters.
For a better understanding of the physiological effects of mindfulness in MDD, the assessment of autonomous nervous reactivity before and after MBI would be of interest.
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Ethikkomission Landesärztekammer Baden-Württemberg, Nr. 2018-046. The patients/participants provided their written informed consent to participate in this study.
JS and AK contributed to conception, study design, and implementation of the study in the clinical setting. JS collected the data, performed the statistical analysis, and wrote the first draft of the manuscript, supervised by AB and UL. AB contributed to the data analysis. UL contributed to the data interpretation. All authors contributed to the manuscript revision, read and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnins.2022.971958/full#supplementary-material
Alvares, G. A., Quintana, D. S., Hickie, I. B., and Guastella, A. J. (2016). Autonomic nervous system dysfunction in psychiatric disorders and the impact of psychotropic medications: A systematic review and meta-analysis. J. Psychiatry Neurosci. 41, 89–104. doi: 10.1503/jpn.140217
Arredondo, M., Sabaté, M., Valveny, N., Langa, M., Dosantos, R., Moreno, J., et al. (2017). A mindfulness training program based on brief practices (M-PBI) to reduce stress in the workplace: A randomised controlled pilot study. Int. J. Occup. Environ. Health 23, 40–51. doi: 10.1080/10773525.2017.1386607
Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J., and Toney, L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment 13, 27–45. doi: 10.1177/1073191105283504
Beda, A., Simpson, D. M., Carvalho, N. C., and Carvalho, A. R. S. (2014). Low-frequency heart rate variability is related to the breath-to-breath variability in the respiratory pattern. Psychophysiology 51, 197–205. doi: 10.1111/psyp.12163
Belliveau, C., Nagy, C., Escobar, S., Mechawar, N., Turecki, G., Rej, S., et al. (2021). Effects of mindfulness-based cognitive therapy on peripheral markers of stress and inflammation in older-adults with depression and anxiety: A parallel analysis of a randomized controlled trial. Front. Psychiatry 12:804269. doi: 10.3389/fpsyt.2021.804269
Billman, G. E. (2011). Heart rate variability—A historical perspective. Front. Physiol. 2:86. doi: 10.3389/fphys.2011.00086
Billman, G. E. (2013). The LF/HF ratio does not accurately measure cardiac sympatho-vagal balance. Front. Physiol. 4:26. doi: 10.3389/fphys.2013.00026
Bortolla, R., Galli, M., Spada, G. E., and Maffei, C. (2021). Mindfulness Effects on Mind Wandering and Autonomic Balance. Appl. Psychophysiol. Biofeedback 47, 53–64. doi: 10.1007/s10484-021-09527-x
Brown, K. W., and Ryan, R. M. (2003). The benefits of being present: Mindfulness and its role in psychological well-being. J. Personal. Soc. Psychol. 84, 822–848. doi: 10.1037/0022-3514.84.4.822
Bulzacka, E., Lavault, S., Pelissolo, A., and Bagnis Isnard, C. (2018). [Mindful neuropsychology: Mindfulness-based cognitive remediation]. L Encephale 44, 75–82. doi: 10.1016/j.encep.2017.03.006
Carpenter, J. K., Conroy, K., Gomez, A. F., Curren, L. C., and Hofmann, S. G. (2019). The relationship between trait mindfulness and affective symptoms: A meta-analysis of the Five Facet Mindfulness Questionnaire (FFMQ). Clin. Psychol. Rev. 74:101785. doi: 10.1016/j.cpr.2019.101785
Chambers, R., Gullone, E., and Allen, N. B. (2009). Mindful emotion regulation: An integrative review. Clin. Psychol. Rev. 29, 560–572. doi: 10.1016/j.cpr.2009.06.005
Christodoulou, G., Salami, N., and Black, D. (2020). The Utility of Heart Rate Variability in Mindfulness Research. Mindfulness 11, 554–570. doi: 10.1007/s12671-019-01296-3
Cladder-Micus, M. B., Speckens, A. E. M., Vrijsen, J. N., Donders, A. R., Becker, E. S., and Spijker, J. (2018). Mindfulness-based cognitive therapy for patients with chronic, treatment-resistant depression: A pragmatic randomized controlled trial. Depress. Anxiety 35, 914–924. doi: 10.1002/da.22788
Cohen, Z. P., Cosgrove, K. T., Akeman, E., Coffey, S., Teague, K., Hays-Grudo, J., et al. (2021). The effect of a mindfulness-based stress intervention on neurobiological and symptom measures in adolescents with early life stress: A randomized feasibility study. BMC Complement. Med. Ther. 21:123. doi: 10.1186/s12906-021-03295-1
Davidson, R. J. (2010). Empirical explorations of mindfulness: Conceptual and methodological conundrums. Emotion 10, 8–11. doi: 10.1037/a0018480
Eisenlohr-Moul, T., Peters, J. R., Chamberlain, K. D., and Rodriguez, M. (2016). Weekly fluctuations in nonjudging predict borderline personality disorder feature expression in women. J. Psychopathol. Behav. Assess. 38, 149–157. doi: 10.1007/s10862-015-9505-y
Elices, M., Tejedor, R., Pascual, J. C., Carmona, C., Soriano, J., and Soler, J. (2019). Acceptance and present-moment awareness in psychiatric disorders: Is mindfulness mood dependent? Psychiatry Res. 273, 363–368. doi: 10.1016/j.psychres.2019.01.041
Feldman, G., Lavalle, J., Gildawie, K., and Greeson, J. M. (2016). Dispositional Mindfulness Uncouples Physiological and Emotional Reactivity to a Laboratory Stressor and Emotional Reactivity to Executive Functioning Lapses in Daily Life. Mindfulness 7, 527–541. doi: 10.1007/s12671-015-0487-3
Fountain-Zaragoza, S., Londerée, A., Whitmoyer, P., and Prakash, R. S. (2016). Dispositional mindfulness and the wandering mind: Implications for attentional control in older adults. Conscious. Cogn. 44, 193–204. doi: 10.1016/j.concog.2016.08.003
Fresco, D. M., Segal, Z. V., Buis, T., and Kennedy, S. (2007). Relationship of posttreatment decentering and cognitive reactivity to relapse in major depression. J. Consult. Clin. Psychol. 75, 447–455. doi: 10.1037/0022-006X.75.3.447
Geurts, D. E. M., Compen, F. R., Van Beek, M. H. C. T., and Speckens, A. E. M. (2020). The effectiveness of mindfulness-based cognitive therapy for major depressive disorder: Evidence from routine outcome monitoring data. BJPsych Open 6:e144. doi: 10.1192/bjo.2020.118
Gu, J., Strauss, C., Bond, R., and Cavanagh, K. (2015). How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clin. Psychol. Rev. 37, 1–12. doi: 10.1016/j.cpr.2015.01.006
Hartmann, R., Schmidt, F. M., Sander, C., and Hegerl, U. (2018). Heart Rate Variability as Indicator of Clinical State in Depression. Front. Psychiatry 9:735. doi: 10.3389/fpsyt.2018.00735
Heart Rate Variability (1996). Standards of measurement, physiological interpretation, and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur. Heart J. 17, 354–381.
Heathers, J. A. J. (2012). Sympathovagal balance from heart rate variability: An obituary. Exp. Physiol. 97:556. doi: 10.1113/expphysiol.2011.063867
Heiss, S., Vaschillo, B., Vaschillo, E. G., Timko, C. A., and Hormes, J. M. (2021). Heart rate variability as a biobehavioral marker of diverse psychopathologies: A review and argument for an “ideal range.”. Neurosci. Biobehav. Rev. 121, 144–155. doi: 10.1016/j.neubiorev.2020.12.004
Hofmann, S. G., Sawyer, A. T., Witt, A. A., and Oh, D. (2010). The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. J. Consult. Clin. Psychol. 78, 169–183. doi: 10.1037/a0018555
Hölzel, B. K., Lazar, S. W., Gard, T., Schuman-Olivier, Z., Vago, D. R., and Ott, U. (2011). How Does Mindfulness Meditation Work? Proposing Mechanisms of Action From a Conceptual and Neural Perspective. Perspect. Psychol. Sci. 6, 537–559. doi: 10.1177/1745691611419671
Houle, M. S., and Billman, G. E. (1999). Low-frequency component of the heart rate variability spectrum: A poor marker of sympathetic activity. Am. J. Physiol. 276, H215–H223. doi: 10.1152/ajpheart.1999.276.1.H215
Hsieh, C.-C., Yu, C.-J., Chen, H.-J., Chen, Y.-W., Chang, N.-T., and Hsiao, F.-H. (2019). Dispositional mindfulness, self-compassion, and compassion from others as moderators between stress and depression in caregivers of patients with lung cancer. Psycho Oncol. 28, 1498–1505. doi: 10.1002/pon.5106
Huang, M., Shah, A., Su, S., Goldberg, J., Lampert, R. J., Levantsevych, O. M., et al. (2018). Association of Depressive Symptoms and Heart Rate Variability in Vietnam War-Era Twins: A Longitudinal Twin Difference Study. JAMA Psychiatry 75, 705–712. doi: 10.1001/jamapsychiatry.2018.0747
Järvelin-Pasanen, S., Sinikallio, S., and Tarvainen, M. P. (2018). Heart rate variability and occupational stress-systematic review. Ind. Health 56, 500–511. doi: 10.2486/indhealth.2017-0190
Kabat-Zinn, J. (1994). Wherever You Go, There You are: Mindfulness Meditation in Everyday Life. New York, NY: Hachette Books.
Kadziolka, M. J., Pierdomenico, E.-A. D., and Miller, C. J. (2016). Trait-Like Mindfulness Promotes Healthy Self-Regulation of Stress. Mindfulness, 7, 236–245 doi: 10.1007/S12671-015-0437-0
Kleiger, R. E., Stein, P. K., and Bigger, J. T. (2005). Heart rate variability: Measurement and clinical utility. Ann. Noninvasive Electrocardiol. 10, 88–101. doi: 10.1111/j.1542-474X.2005.10101.x
Koenig, J., and Thayer, J. F. (2016). Sex differences in healthy human heart rate variability: A meta-analysis. Neurosci. Biobehav. Rev. 64, 288–310. doi: 10.1016/j.neubiorev.2016.03.007
Kotsou, I., Leys, C., and Fossion, P. (2018). Acceptance alone is a better predictor of psychopathology and well-being than emotional competence, emotion regulation and mindfulness. J. Affect. Disord. 226, 142–145. doi: 10.1016/j.jad.2017.09.047
Krick, A., and Felfe, J. (2020). Who benefits from mindfulness? The moderating role of personality and social norms for the effectiveness on psychological and physiological outcomes among police officers. J. Occup. Health Psychol. 25, 99–112. doi: 10.1037/ocp0000159
Krygier, J. R., Heathers, J. A. J., Shahrestani, S., Abbott, M., Gross, J. J., and Kemp, A. H. (2013). Mindfulness meditation, well-being, and heart rate variability: A preliminary investigation into the impact of intensive Vipassana meditation. Int. J. Psychophysiol. 89, 305–313. doi: 10.1016/j.ijpsycho.2013.06.017
Kühner, C., Bürger, C., Keller, F., and Hautzinger, M. (2007). [Reliability and validity of the Revised Beck Depression Inventory (BDI-II). Results from German samples]. Der Nervenarzt 78, 651–656. doi: 10.1007/s00115-006-2098-7
Lengacher, C. A., Reich, R. R., Paterson, C. L., Shelton, M., Shivers, S., Ramesar, S., et al. (2019). A large randomized trial: Effects of mindfulness-based stress reduction (MBSR) for Breast Cancer (BC) survivors on salivary cortisol and IL-6. Biol. Res. Nurs. 21, 39–49. doi: 10.1177/1099800418789777
Lin, H.-P., Lin, H.-Y., Lin, W.-L., and Huang, A. C.-W. (2011). Effects of stress, depression, and their interaction on heart rate, skin conductance, finger temperature, and respiratory rate: Sympathetic-parasympathetic hypothesis of stress and depression. J. Clin. Psychol. 67, 1080–1091. doi: 10.1002/jclp.20833
Lindsay, E. K., Young, S., Smyth, J. M., Brown, K. W., and Creswell, J. D. (2018). Acceptance lowers stress reactivity: Dismantling mindfulness training in a randomized controlled trial. Psychoneuroendocrinology 87, 63–73. doi: 10.1016/j.psyneuen.2017.09.015
Ludwig, D. S., and Kabat-Zinn, J. (2008). Mindfulness in medicine. JAMA 300, 1350–1352. doi: 10.1001/jama.300.11.1350
Lutz, J., Brühl, A. B., Doerig, N., Scheerer, H., Achermann, R., Weibel, A., et al. (2016). Altered processing of self-related emotional stimuli in mindfulness meditators. NeuroImage 124, 958–967. doi: 10.1016/j.neuroimage.2015.09.057
Magalhaes, A. A., Oliveira, L., Pereira, M. G., and Menezes, C. B. (2018). Does Meditation Alter Brain Responses to Negative Stimuli? A Systematic Review. Front. Hum. Neurosci. 12:448. doi: 10.3389/fnhum.2018.00448
Marion-Jetten, A. S., Taylor, G., and Schattke, K. (2021). Mind your goals, mind your emotions: Mechanisms explaining the relation between dispositional mindfulness and action crises. Personal. Soc. Psychol. Bull. doi: 10.1177/0146167220986310
McCall, W. V., Rosenquist, P. B., and Miller, B. J. (2022). Development of autonomic nervous system assays as point-of-care tests to supplement clinical judgment in risk assessment for suicidal behavior: A review. Curr. Psychiatry Rep. 24:11–21. doi: 10.1007/s11920-022-01315-6
Morton, M. L., Helminen, E. C., and Felver, J. C. (2020). A Systematic Review of Mindfulness Interventions on Psychophysiological Responses to Acute Stress. Mindfulness 11, 2039–2054. doi: 10.1007/s12671-020-01386-7
Nayda, D. M., and Takarangi, M. K. T. (2021). The cost of being absent: Is meta-awareness of mind-wandering related to depression symptom severity, rumination tendencies and trauma intrusions? J. Affect. Disord. 292, 131–138. doi: 10.1016/j.jad.2021.05.053
Neff, K. D. (2003). The development and validation of a scale to measure self-compassion. Self Identity 2, 223–250. doi: 10.1080/15298860309027
Nijjar, P. S., Puppala, V. K., Dickinson, O., Duval, S., Duprez, D., Kreitzer, M. J., et al. (2014). Modulation of the autonomic nervous system assessed through heart rate variability by a mindfulness based stress reduction program. Int. J. Cardiol. 177, 557–559. doi: 10.1016/j.ijcard.2014.08.116
Ninomiya, A., Sado, M., Park, S., Fujisawa, D., Kosugi, T., Nakagawa, A., et al. (2020). Effectiveness of mindfulness-based cognitive therapy in patients with anxiety disorders in secondary-care settings: A randomized controlled trial. Psychiatry Clin. Neurosci. 74, 132–139. doi: 10.1111/pcn.12960
Park, G., Kim, H., Mermillod, M., and Thayer, J. F. (2021). The modulation of cardiac vagal tone on attentional orienting of fair-related faces: Low hrv is associated with faster attentional engagement to fair-relevant stimuli. Cogn. Affect. Behav. Neurosci. 22, 229–243. doi: 10.3758/s13415-021-00954-1
Parmentier, F. B. R., García-Toro, M., García-Campayo, J., Yañez, A. M., Andrés, P., and Gili, M. (2019). Mindfulness and symptoms of depression and anxiety in the general population: The mediating roles of worry, rumination, reappraisal and suppression. Front. Psychol. 10:506. doi: 10.3389/fpsyg.2019.00506
Pascoe, M. C., Thompson, D. R., Jenkins, Z. M., and Ski, C. F. (2017). Mindfulness mediates the physiological markers of stress: Systematic review and meta-analysis. J. Psychiatr. Res. 95, 156–178. doi: 10.1016/j.jpsychires.2017.08.004
Paul, N. A., Stanton, S. J., Greeson, J. M., Smoski, M. J., and Wang, L. (2013). Psychological and neural mechanisms of trait mindfulness in reducing depression vulnerability. Soc. Cogn. Affect. Neurosci. 8, 56–64. doi: 10.1093/scan/nss070
Rådmark, L., Sidorchuk, A., Osika, W., and Niemi, M. (2019). A Systematic Review and Meta-Analysis of the Impact of Mindfulness Based Interventions on Heart Rate Variability and Inflammatory Markers. J. Clin. Med. 8:E1638. doi: 10.3390/jcm8101638
Reyes del Paso, G. A., Langewitz, W., Mulder, L. J. M., van Roon, A., and Duschek, S. (2013). The utility of low frequency heart rate variability as an index of sympathetic cardiac tone: A review with emphasis on a reanalysis of previous studies. Psychophysiology 50, 477–487. doi: 10.1111/psyp.12027
Rodriguez-Larios, J., Bracho Montes de Oca, E. A., and Alaerts, K. (2021). The EEG spectral properties of meditation and mind wandering differ between experienced meditators and novices. NeuroImage 245:118669. doi: 10.1016/j.neuroimage.2021.118669
Royuela-Colomer, E., Fernández-González, L., and Orue, I. (2021). Longitudinal Associations between Internalizing Symptoms, Dispositional Mindfulness, Rumination and Impulsivity in Adolescents. J. Youth Adolesc.* 50, 2067–2078. doi: 10.1007/s10964-021-01476-2
Saltsman, T. L., Seery, M. D., Ward, D. E., Radsvick, T. M., Panlilio, Z. A., Lamarche, V. M., et al. (2021). Facing the facets: No association between dispositional mindfulness facets and positive momentary stress responses during active stressors. Personal. Soc. Psychol. Bull. 47, 1057–1070. doi: 10.1177/0146167220956898
Sandercock, G. R. H., Bromley, P. D., and Brodie, D. A. (2005). The reliability of short-term measurements of heart rate variability. Int. J. Cardiol. 103, 238–247. doi: 10.1016/j.ijcard.2004.09.013
Sarlon, J., Plaszczyk, S., Engel, S., and Oertel-Knöchel, V. (2018). Electrophysiological parameters as biomarkers for psychiatry: Intra-individual variability and influencing factors. Int. J. Psychophysiol. Organ. Psychophysiol. 123, 42–47. doi: 10.1016/j.ijpsycho.2017.11.011
Sarlon, J., Staniloiu, A., and Kordon, A. (2021). Heart rate variability changes in patients with major depressive disorder: Related to confounding factors, not to symptom severity? Front. Neurosci. 15:675624. doi: 10.3389/fnins.2021.675624
Scavone, A., Kadziolka, M. J., and Miller, C. J. (2020). State and trait mindfulness as predictors of skin conductance response to stress. Appl. Psychophysiol. Biofeedback 45, 221–228. doi: 10.1007/s10484-020-09467-y
Schumann, A., Andrack, C., and Bär, K.-J. (2017). Differences of sympathetic and parasympathetic modulation in major depression. Prog. Neuro Psychopharmacol. Biol. Psychiatry 79, 324–331. doi: 10.1016/j.pnpbp.2017.07.009
Segal, Z. V., and Walsh, K. M. (2016). Mindfulness-based cognitive therapy for residual depressive symptoms and relapse prophylaxis. Curr. Opin. Psychiatry 29, 7–12. doi: 10.1097/YCO.0000000000000216
Shaffer, F., and Ginsberg, J. P. (2017). An Overview of Heart Rate Variability Metrics and Norms. Front. Public Health 5:258. doi: 10.3389/fpubh.2017.00258
Shapiro, S. L., Carlson, L. E., Astin, J. A., and Freedman, B. (2006). Mechanisms of mindfulness. J. Clin. Psychol. 62, 373–386. doi: 10.1002/jclp.20237
Simmons, J. P., Nelson, L. D., and Simonsohn, U. (2011). False-positive psychology: Undisclosed flexibility in data collection and analysis allows presenting anything as significant. Psychol. Sci. 22, 1359–1366. doi: 10.1177/0956797611417632
Sun, S., Hu, C., Pan, J., Liu, C., and Huang, M. (2019). Trait Mindfulness Is Associated With the Self-Similarity of Heart Rate Variability. Front. Psychol. 10:314. doi: 10.3389/fpsyg.2019.00314
Sztajzel, J. (2004). Heart rate variability: A noninvasive electrocardiographic method to measure the autonomic nervous system. Swiss Med. Weekly 134, 514–522.
Tang, Y.-Y., Ma, Y., Fan, Y., Feng, H., Wang, J., Feng, S., et al. (2009). Central and autonomic nervous system interaction is altered by short-term meditation. Proc. Natl. Acad. Sci. U.S.A. 106, 8865–8870. doi: 10.1073/pnas.0904031106
Teasdale, J. D., Segal, Z. V., Williams, J. M., Ridgeway, V. A., Soulsby, J. M., and Lau, M. A. (2000). Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J. Consult. Clin. Psychol. 68, 615–623. doi: 10.1037//0022-006x.68.4.615
Treanor, M. (2011). The potential impact of mindfulness on exposure and extinction learning in anxiety disorders. Clin. Psychol. Rev. 31, 617–625. doi: 10.1016/j.cpr.2011.02.003
Uhlig, S., Meylan, A., and Rudolph, U. (2020). Reliability of short-term measurements of heart rate variability: Findings from a longitudinal study. Biol. Psychol. 154:107905. doi: 10.1016/j.biopsycho.2020.107905
Vago, D. R., and Silbersweig, D. A. (2012). Self-awareness, self-regulation, and self-transcendence (S-ART): A framework for understanding the neurobiological mechanisms of mindfulness. Front. Hum. Neurosci. 6:296. doi: 10.3389/fnhum.2012.00296
Van Dam, N. T., Sheppard, S. C., Forsyth, J. P., and Earleywine, M. (2011). Self-compassion is a better predictor than mindfulness of symptom severity and quality of life in mixed anxiety and depression. J. Anxiety Disord. 25, 123–130. doi: 10.1016/j.janxdis.2010.08.011
Vila, X. A., Lado, M. J., and Cuesta-Morales, P. (2019). Evidence Based Recommendations for Designing Heart Rate Variability Studies. J. Med. Syst. 43:311. doi: 10.1007/s10916-019-1437-8
von Rosenberg, W., Chanwimalueang, T., Adjei, T., Jaffer, U., Goverdovsky, V., and Mandic, D. P. (2017). Resolving ambiguities in the LF/HF Ratio: LF-HF scatter plots for the categorization of mental and physical stress from HRV. Front. Physiol. 8:360. doi: 10.3389/fphys.2017.00360
Voss, A., Bogdanski, M., Langohr, B., Albrecht, R., and Sandbothe, M. (2020). Mindfulness-Based Student Training Leads to a Reduction in Physiological Evaluated Stress. Front. Psychol. 11:645. doi: 10.3389/fpsyg.2020.00645
Walach, H., Buchheld, N., Buttenmüller, V., Kleinknecht, N., and Schmidt, S. (2006). Measuring mindfulness—The Freiburg Mindfulness Inventory (FMI). Personal. Individ. Diff. 40, 1543–1555. doi: 10.1016/j.paid.2005.11.025
Wang, Y.-P., and Gorenstein, C. (2013). Psychometric properties of the Beck Depression Inventory-II: A comprehensive review. Revista Brasileira Psiquiatria 35, 416–431. doi: 10.1590/1516-4446-2012-1048
Watford, T. S., O’Brien, W. H., Koerten, H. R., Bogusch, L. M., Moeller, M. T., Sonia Singh, R., et al. (2020). The mindful attention and awareness scale is associated with lower levels of high-frequency heart rate variability in a laboratory context. Psychophysiology 57:e13506. doi: 10.1111/psyp.13506
Keywords: mindfulness, emotional stress, autonomous reactivity, depressive disorder, electrophysiological parameters
Citation: Sarlon J, Brühl AB, Lang UE and Kordon A (2022) Electrophysiological correlates of mindfulness in patients with major depressive disorder. Front. Neurosci. 16:971958. doi: 10.3389/fnins.2022.971958
Received: 17 June 2022; Accepted: 21 September 2022;
Published: 13 October 2022.
Edited by:
Tijana Bojić, University of Belgrade, SerbiaReviewed by:
Philippe Jawinski, Humboldt University of Berlin, GermanyCopyright © 2022 Sarlon, Brühl, Lang and Kordon. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jan Sarlon, amFuLnNhcmxvbkB1cGsuY2g=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.