
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurosci., 29 April 2022
Sec. Neural Technology
Volume 16 - 2022 | https://doi.org/10.3389/fnins.2022.804397
This article is part of the Research TopicUse of Computerized Gait Analysis in Neurological Pathologies: Volume IIView all 4 articles
One’s gait can be affected by aging, pathway with turns, task demands, etc., causing changes in gait-related indices and knee flexion (influencing posture). Walking on pathways with turns threatens stability, affecting one’s gait-related indices and posture. The ability to overcome such deficits is compromised with age and neurological disorders, e.g., Parkinson’s Disease (PD) leading to falls. Also, task demands imposed by single and dual-task (e.g., counting backward while walking) conditions affect the gait of individuals using different postural strategies varying with age and neurological disorder. Existing research has investigated either the effect of the pathway with turn or task condition on one’s gait. However, none (to our knowledge) have explored the differentiated implications of the pathway with turn and task conditions on one’s gait-related indices and knee flexion while walking. Our study had two phases with 30 participants. Phase 1 had healthy adults (young and old) and Phase 2 had age and gender-matched healthy elderly and individuals with Parkinson’s disease (PD) who walked on pathways having turns under single and dual-task conditions. We analysed gait in terms of (i) gait-related indices (Phases 1 and 2) and (ii) knee flexion (Phase 2). Also, we analysed one’s counting performance during dual task. One’s gait-related indices and knee flexion were measured using a portable gait quantifier. The aim was to (i)understand whether both pathways with turn and task conditions are equally effective in affecting the gait of (a)individuals of varying ages and (b) gender-matched healthy older adults and individuals with PD, (ii)study variations of knee joint angles while walking on pathways having turns (under different task conditions) in terms of its clinical relevance, and (iii) explore the implication of pathway with turn on counting performance (with relevance to postural strategy) with varying age and PD. Results indicated that for the younger group, the task condition caused statistical variations in gait-related indices. For the older group, both pathways with turn and task conditions had statistical implications on gait-related indices. Additionally, individuals with PD demonstrated a higher variation in knee flexion than their healthy counterparts. Again, pathways with varying turns elicited variations in counting performance indicating different postural strategies being employed by the three groups.
One’s gait (describing the pattern of walking) is an indicator of the quality of life (Paraschiv-Ionescu et al., 2004), with gait being influenced by age (Hodgins, 2008), pathway turn angle (de Morais Faria et al., 2016), task demands (Bayot et al., 2020), etc. Often, the elderly demonstrate slower walking (Hodgins, 2008) than the young, accompanied by reduced cadence (Novak et al., 2016) along with increased step time (Nagano et al., 2013) and variations in knee flexion (Begg and Sparrow, 2006) as mechanisms to achieve dynamic stability and prevent falls. Again, walking on pathways having different trajectories, namely straight or with turns (de Morais Faria et al., 2016) can influence one’s gait (with the influence increasing with the turning angle (de Morais Faria et al., 2016) with variations quantified in terms of changes in gait-related indices, e.g., stride time, step time, cadence, etc. (O’Sullivan et al., 2013), and knee flexion defining one’s posture during walking (Hora et al., 2017). Turning on a curve along a pathway not only threatens stability but also requires a precise balance of each limb (Bhatt et al., 2013) (affecting one’s gait-related indices and posture), and such an ability is often compromised with an increase in age (Shin et al., 2015) and neurological disorders, such as PD (Bhatt et al., 2013). This is because, turning on a curve (a complex and difficult maneuver for elderly individuals) demands changes in both anteroposterior and medo-lateral impulses, while moving one’s centre of mass toward the new direction of travel (Akram et al., 2010) and precise control of medo-lateral balance is important for preventing falls during walking (Bergland et al., 2003; Jansen et al., 2014). Also, adding to anomalies in gait-related indices (Bhatt et al., 2013), the individuals with PD often demonstrate abnormal posture (Yoshii et al., 2016) with knee flexion reported as one of the observations in their stereotypical stooped appearance (Yoshii et al., 2016). Such flexed posture might adversely affect their daily living and can be associated with falls (Yoshii et al., 2016). The impact of these falls can be debilitating not only because of associated injuries, but also the secondary immobilisation caused by a fear of renewed falls (Bloem et al., 2006).
Adding to the pathway turns, the task demands imposed by task conditions, e.g., single task and dual task conditions (Bayot et al., 2020) during walking can have implications on one’s gait. Research has shown that different task conditions, e.g., walking while reciting alternate letters of the alphabet, serial subtraction, counting backward, etc. (Bayot et al., 2020), can have varying implications on one’s gait. Such implications can be at least partially attributed to the cognitive load due to the dual task (Bayot et al., 2020) that can cause individuals to use different postural strategies varying with age and neurological disorder. For example, healthy young adults who enjoy the automaticity of walking (Clark, 2015) often prioritize cognition over walking (Plummer et al., 2015), while performing a dual task. In contrast, cognitively healthy older adults often prioritize gait over cognition (‘posture first strategy’) (Bayot et al., 2020) to maintain stability and prevent falls. Again, individuals with Parkinson’s disease tend to divide their attention between both the components of a dual task (e.g., walking and counting), while employing the ‘posture second’ strategy (Bloem et al., 2006) which might be associated with their risk of falls.
Though there is a rich history of literature in which researchers have investigated either the effect of pathway turns or task demands of healthy individuals and those with gait disorders, none (to our knowledge) have explored the differentiated implications of pathway turn angles and task conditions on gait-related indices and knee flexion during one’s overground walk with relevance to one’s postural control strategy. This gap in literature warrants deeper investigation to explore the differentiated implications of pathways with varying turn angles and task conditions on healthy and unhealthy gait. For this, we carried out a systematic study in two phases, namely phase 1 and phase 2. Phase 1 involved cognitively healthy adults belonging to younger and older age groups who participated in a walking task on pathways having varying turn angles (0, 90, 120, and 180°) under single-task and dual-task (counting backward while walking) conditions. Phase 2 involved age and gender-matched cognitively healthy elderly and individuals with PD who walked on pathways having turned and under single-task and dual-task conditions. We explored their gait in terms of (i) gait-related indices [that can characterize one’s walking (Solanki and Lahiri, 2018); in Phases 1 and 2] and (ii) knee flexion [with knee joint angle being a key component in understanding human posture (Hora et al., 2017) while walking; in Phase 2]. In addition, we analysed one’s counting performance during the dual task. One’s gait-related indices and knee flexion were measured using a portable gait quantifier (SmartWalk henceforth). The purpose of our study was to (i) understand whether both the pathway with varying turn angles and task conditions are equally effective in affecting the gait of (a) individuals belonging to different age groups and (b) age and gender-matched healthy older adults, and individuals with PD, (ii) study the variations of knee joint angles synchronized with gait events, while walking overground on pathways having turned and under different task conditions in terms of its clinical relevance, and (iii) explore the implication of pathway turn angles on one’s counting performance under the dual-task condition with relevance to postural control strategy from the perspective of age and neurological disorder, such as PD.
This paper is organized as follows: The section on materials and methods presents the system design, followed by the methodology used for the study. The section on results provides our findings obtained during the study. Finally, the section on discussion and limitations summarises the research findings and discusses the limitations of the current research, as well as the direction of future research.
Our study was conducted in phases, namely, phase 1 and phase 2. Table 1 shows the participants’ characteristics for phases 1 and 2. In phase 1, twenty healthy participants categorized into two groups, namely Grp1 (Y1–Y10; 20 ≤ Age ≤ 35 years) and Grp2 (O1–O10; Age > 50 years) were recruited. In phase 2, five age and gender-matched healthy elderly [Grp3 henceforth; (E1–E5; Age > 50 years)] and individuals with PD [Grp4 henceforth; (P1–P5; Age > 50 years)] were recruited. The individuals with PD were recruited from a nearby physiotherapy hospital, where they were undergoing treatment. All the individuals with PD were on medication. Enrolment of these participants was through a physiotherapist’s referral. The inclusion/exclusion criteria for the healthy participants were (i) age between 18 and 90 years, (ii) can understand the experimenter’s instructions, and (iii) have no neurological, musculoskeletal, or vestibular impairment. The individuals with PD were checked for their ability to perform the 10 m walk-test (O’Sullivan et al., 2013) while walking over-ground without any external support such as orthosis, canes, etc. Also, Falls Efficacy Scale (FES) scores (Thomas et al., 2010) were collected from the participants. The FES [having thresholds (Meimandi et al., 2021) as FES score < 22; between 22 and 28; and >28 considered as mild, moderate, and severe fear of fall, respectively] is a clinical tool that can be used to identify one’s confidence while an individual does basic tasks of daily living without falling. This is correlated with measures of balance and gait (Yardley and Smith, 2002) and predicts future falls. On average, the FES scores varied across groups with Grp1 having the lowest (who can be considered to be confident) and Grp4 having the highest score (Grp1 < Grp2 < Grp3 < Grp4 in terms of FES scores). All the participants belonging to Grp2 and Grp3 [except a few, i.e., O1, O2, O6, O7, E1, and E5 (Table 1) who demonstrated confident walking] demonstrated mild fear of falling with one, namely E4 (in Grp3) who demonstrated moderate fear of fall. In contrast, for Grp4, three of the participants [P2, P4, and P5 (Table 1)] demonstrated severe fear of falling, while one showed moderate fear of falling and one (P3) had a mild fear of falling. Again, clinical measures, such as the Unified Parkinson’s Disease Rating Scale motor part (UPDRS III) (Pandey et al., 2016) and H&Y stage (Pandey et al., 2016) indicate the severity of the symptom was collected for Grp4. The Mean (SD) of UPDRS III and H&Y stage is 28.60 (±8.29) and 2 (±0.71), respectively, which shows the mild severity of disease for Grp4 (Pandey et al., 2016). The study had institute ethical clearance (Approval No.: IEC/2014-15/2/UL/003).
The experimental setup for both the phases 1 and 2 comprised of (i) a SmartWalk system comprising of a waist-belt (housing the Data Acquisition/Storage Unit), Instrumented Insoles (housed in a pair of shoes), and Knee Angle Recorder Units positioned in a pair of knee caps that were adjustable with Velcro belts (Figure 1A) for each leg (Figure 1A; described earlier) and (ii) 10-m pathway identified by a pathway delineator (having markers every 1 m), along with ‘START’ and ‘STOP’ lines (Figure 1B). Please note that the Knee Angle Recorder Unit of the SmartWalk system was used only in Phase 2. The pathway was of 4 types based on the pathway turn angles, e.g., 0, 90, 120, and 180°, with each pathway having straight segments and a turn segment, except 0° (that had only the straight segment).
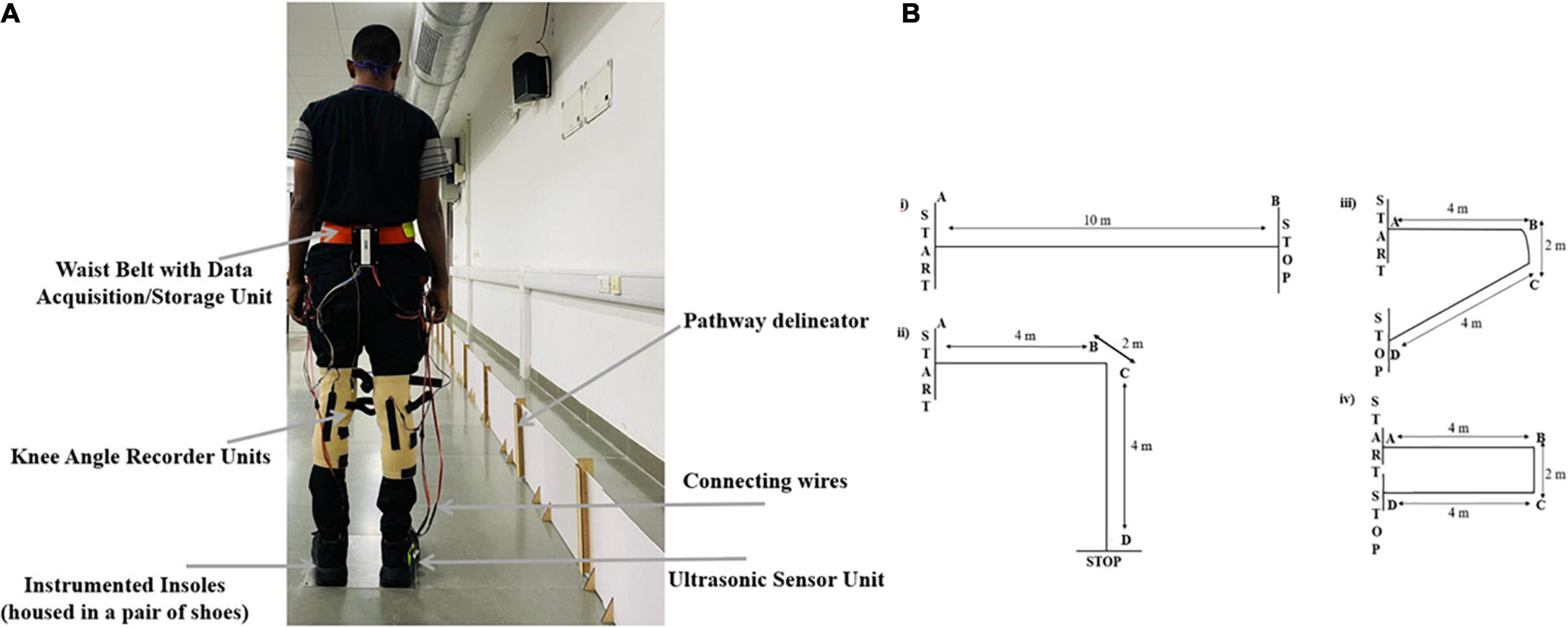
Figure 1. (A) Back view of a person wearing SmartWalk, (B) 10-m pathways (i) 0° (A–B), (ii) 90° (A–D), (iii) 120° (A–D), and (iv) 180° (A–D). AB and CD are straight segments and BC is turn segment. Note: Knee Angle Recorder Units were used in Phase 2 of our study.
Each phase of our study had single task (TaskC1 henceforth) and dual-task (TaskC2 henceforth) conditions. In TaskC1, one was asked to walk (with self-selected speed) on the pathway without speaking. In TaskC2, one was asked to walk (with self-selected speed) on the pathway while counting backward (Bayot et al., 2020) and the counting performance was recorded by the experimenter. One was told not to match his/her steps with backward counting. The order of presentation of TaskC1 and TaskC2 was randomized across participants to eliminate ordering effects (Bayot et al., 2020). Each of TaskC1 and TaskC2 required ∼30 min of commitment from each participant. In each phase, when the participant entered the study room, the experimenter asked him/her to sit on a chair and relax. This was followed by the experimenter showing the experimental setup to the participant and demonstrating what he/she was expected to do in the study while describing the study with a visual schedule (abiding by the ethical considerations). Also, one was told that he/she was free to discontinue the study at any time if uncomfortable. In addition, they were told that they can ask for a break at any point during the tasks. When the participant expressed that he/she understood the task and consented to participate in the study, the consent signing was administered. In the case of Phase 2 for Grp4, the accompanying therapist collected the clinical measures. Also, the therapist confirmed whether the patient was in the OFF-state (for data collection). Then, the experimenter helped the participant to wear the SmartWalk and offered the pathways for walking with components of SmartWalk and pathways varying depending on the Phase of the study. At the end of each phase, the experimenter collected verbal feedback on the overall impression of the participant regarding the use of SmartWalk and his/her participation in the study.
In this phase, the participant was offered pathways with 0, 90, 120, and 180° turns (order of presentation being randomized across participants). The experimenter helped the participant to wear the waist belt (housing the Data Acquisition/Storage Unit), shoes (housing the Insoles), and Ultrasonic Sensor Unit (mounted on the lateral side of the heel location of one of the shoes). Also, before commencing a walk in each of TaskC1 and TaskC2, the participant was asked to stand as straight as possible with both legs touching the ‘START’ line (Figure 1B).
In this phase, the participant was offered the pathway having 0 and 180° turns (Figure 1B). The experimenter helped the participant to wear the waist belt, shoes, Ultrasonic Sensor Unit, and a pair of kneecaps (adjustable with Velcro belts) housing the Knee Angle Recorder Units toward the knee pit. Also, before commencing walk in each of TaskC1 and TaskC2, the participant was asked to stand as straight as possible with both legs touching the ‘START’ line (Figure 1B) when baseline recording of the Knee flexion (AngleBaseline henceforth) was made.
The SmartWalk (Figure 1A) comprised of (A) Instrumented Insoles, (B) Ultrasonic Sensor Unit, (C) Flexion/Extension Recorder Unit (Knee Angle Recorder Unit henceforth), and (D) Data Acquisition/Storage Unit.
In our present research, we used a pair of Instrumented Insoles (Insoles henceforth) that were housed in a pair of shoes. The idea was to use a wearable and portable gait quantifier since the existing state-of-the-art stereophotogrammetric systems and walk mats are used to quantify one’s gait-related indices computed from gait events, namely, heel-strike, toe-off, etc. (O’Sullivan et al., 2013), though powerful, suffer from large setup time, operational complexity, specialized knowledge for operation, high cost, restriction to lab-based settings, line-of-sight issues, etc. Again, within the wearable and portable devices are accelerometers, gyro sensors, goniometers, etc. (Lan and Shih, 2014) that though powerful, often suffer from drift problems (Lan and Shih, 2014) that limit their application in gait monitoring. To overcome such issues, researchers have been exploring the use of portable force sensors (Hanlon and Anderson, 2009) such as Force Sensitive Resistors (FSRs) to detect one’s gait events and measure gait-related indices. For example, different researchers have used multiple FSRs located at different positions under one’s feet (Pinkam and Nilkhamhang, 2013) to characterize one’s gait. Usage of multiple FSRs though lends improved precision of measurements, yet it increases the hardware complexity along with difficulty in troubleshooting making it infeasible for practical applications. On the other hand, too few FSRs can miss picking up certain aspects of gait abnormalities, such as foot inversion/eversion (Forghany et al., 2014) that can be seen in the elderly and those with gait disorders. In our present research, each of the Insoles had FSRs [0–445°N (FlexiForce A201; from Tekscan) with an active diameter of 9.53 mm] [similar to that mentioned in Solanki and Lahiri (2018)] and the data was acquired from sensors placed at the heel locations [lateral and medial border to take care of any possible foot inversion/eversion (Forghany et al., 2014)] to record one’s heel-strike events. The acquired data was processed to compute one’s gait-related indices, namely, Stride time (O’Sullivan et al., 2013), Step time (O’Sullivan et al., 2013), and cadence (O’Sullivan et al., 2013) (details in Section “Data Processing” below). The Insoles were calibrated using the VICON setup (from Vicon Motion Systems Ltd.). The calibration results of a pilot study with healthy participants {n = 5; Mean (SD) = 27 (±3.67) years; Body Mass Index (BMI) [Mean (SD) = 21.98 (±2.33) Kg/m2]} indicated good agreement between gait-related indices measured by the Insoles and the VICON setup with average %Absolute error being 0.71 and 0.8% for Stride time and Step time, respectively.
An Ultrasonic Sensor Unit [HCSR04 (Hanan et al., 2019)] is comprised of an ultrasonic transmitter, receiver, and control circuit. This unit was used to transmit synchronising markers to the Data Acquisition/Storage Unit to keep track of the distance traversed (by a participant) along the pathway laid out using a pathway delineator (please see Section “Experimental Setup” for details).
Again, given that the estimation of joint angle is a key component of the analysis of human gait (Lee et al., 2016), we used a calibrated Knee Angle Recorder Unit [similar to that mentioned in Pallavi et al. (2021)]. One’s joint angles can be measured by using standard camera-based techniques, e.g., VICON (McGrath and Stirling, 2020) which though powerful, suffers from portability issues, high cost, line-of-sight issues, etc. Given the importance of joint angle estimation and the need to have portable, wearable sensing to facilitate human gait analysis in free-living conditions, research had been focused on using Inertial Measurement Units (IMUs), Goniometers, etc. However, the IMU-based systems suffer from drift problems (Lee et al., 2016) and Electro-Goniometers may not be suitable for real-time measurement (Lee et al., 2016). To mitigate such issues, our Knee Angle Recorder Unit was made using a commercially available 4.5” bend sensor (from Spectra Symbol) (Figure 1A) to record the flexion/extension angle at the knee of each leg. The idea was to measure the angle between the line connecting the greater trochanter and knee, and the line connecting the knee and lateral malleolus (Yoshii et al., 2016). The bend sensor was calibrated using a stepper motor-hinge setup with a motor driver for varying bend positions (Pallavi et al., 2021). Given that the knee flexion during one’s gait is less than 90° (Rowe et al., 2000), we mounted the bend sensor in a kneecap, so that the bending location allowed us a range of measurement from 0° to ∼100° with the calibrated sensor output changing linearly (R2 = ∼0.99) with bend angle along with satisfactory repeatability (Pallavi et al., 2021). The analogue signal (0–5 V) from the bend sensor along with time stamping was acquired by the Data Acquisition/Storage Unit.
Finally, a Data Acquisition/Storage Unit housing (i) a Microcontroller (ATMEGA 2560) and (ii) a 64-GB SD card (from SanDisk Ultra), mounted on a waist-belt was used to store the analogue signals (0–5 V) from the FSRs (of the Insoles), Ultrasonic Sensor, and Knee Angle Recorder Unit. The data from the sensors were sampled using a 10-bit Analogue-to-Digital converter of the Microcontroller at ∼200 samples/second (Solanki and Lahiri, 2018) and then stored in the SD card along with time stamping. In addition, for the Insole data, the Insole ID (‘left’ and ‘right’) was stored. The stored data was further processed.
The stored data were processed using the Microcontroller of the Data Acquisition/Storage Unit to extract the (i) gait-related indices and (ii) Coefficient of Variation (%CV henceforth) of the knee flexion during heel-strike.
The FSR data acquired from the Insoles was processed by the Microcontroller [as in Solanki and Lahiri (2018)] of the SmartWalk system to compute (a) Normalised Average Stride time (Stride timeAVG_NORM henceforth), Normalised Average Ste time (SteptimeAVG_NORMhenceforth) and Normalised Cadence (CadenceNORM henceforth).
The Stride time was computed from the time interval between two consecutive heel-strike events of each ipsilateral i.e., same leg (O’Sullivan et al., 2013) followed by normalization using Equation (1) (Angelini et al., 2016). Here, h and g represent one’s body height and gravitational acceleration, respectively.
Again, the Step time was computed from the time interval between two consecutive heel-strike events of contralateral legs (O’Sullivan et al., 2013) followed by normalization using Equation (2). The h and g are the same as before.
Also, one’s cadence was computed from the heel-strike events quantifying the number of steps taken per minute (O’Sullivan et al., 2013) followed by normalization using Equation (3) (Fang et al., 2018).
Here, h and n represent one’s body height and the number of participants, respectively.
The coefficient of variation (of the knee flexion) can be a valuable measure with regard to falls (Moon et al., 2015) during walking. We computed the %CV of the knee flexion during heel-strike events using Equation (4).
Post our studies, we analysed the gait-related indices (computed for each of TaskC1 and TaskC2 during phases 1 and 2) and the counting performance (computed for TaskC2 during Phases 1 and 2) corresponding to pathways with varying turns for the participant groups for statistical significance. Since our sample size was limited and data was not normally distributed [using the Shapiro–Wilk test (Field, 2013)], we implemented a non-parametric dependent sample Wilcoxon Signed Rank test (Field, 2013) and independent sample Mann Whitney test (Field, 2013) for investigating the statistical significance during data analysis. The statistical tests were carried out using the SPSS Statistics 20 software and effect size (r) was computed from the z-value obtained using the statistical tests (Fritz et al., 2012).
While the participants took part in our study, at the end of each phase, the experimenter collected verbal feedback from the participant that indicated that all the participants (including those belonging to Grp4) were comfortable with our SmartWalk. Regarding the participation in the study, Grp1 reported that they were comfortable with taking part in our study while walking on the pathways with varying turns and under different task conditions. For Grp2 and Grp3, we received similar feedback. For Grp4, the participants mentioned that they had a good experience while walking on the pathways under varying task conditions. None of them took any intermediate break during the task though they were free to ask for breaks if needed during the study. The aim of our study was to understand the implications of pathways with turns and task conditions on one’s (i) gait-related indices (measured using SmartWalk), (ii) postural changes, and (iii) dual-task performance (i.e., counting performance) with relevance to postural strategy.
Here we present our observations on the gait-related indices of Grp1 and Grp2 for pathways with varying turns and task conditions. The Grp1 and Grp2 differed statistically (p-value < 0.00001) with a large effect (r = 0.8) in age (using independent sample Mann–Whitney test).
The intra-group analysis for TaskC1 indicated that the group average CadenceNORM (Figure 2A) decreased as the turn angle of pathways increased and Stride timeAVG_NORM (Figure 2B) and Step timeAVG_NORM (Figure 2C) increased as the turn angle of pathways increased (less variation given that the participants were healthy) for each of Grp1 and Grp2. The dependent sample Wilcoxon Signed Rank test indicated that the pathways with varying turns did not cause any statistical variation in any of the gait-related indices for Grp1. In contrast, for Grp2, we could find the statistical difference (with a p-value ranging from 0.01 to 0.04) with a large effect (ranging from r = 0.52 to r = 0.8) in the gait-related indices, while walking on pathways having 120 and 180° turns concerning that with 0 and 90° turns.
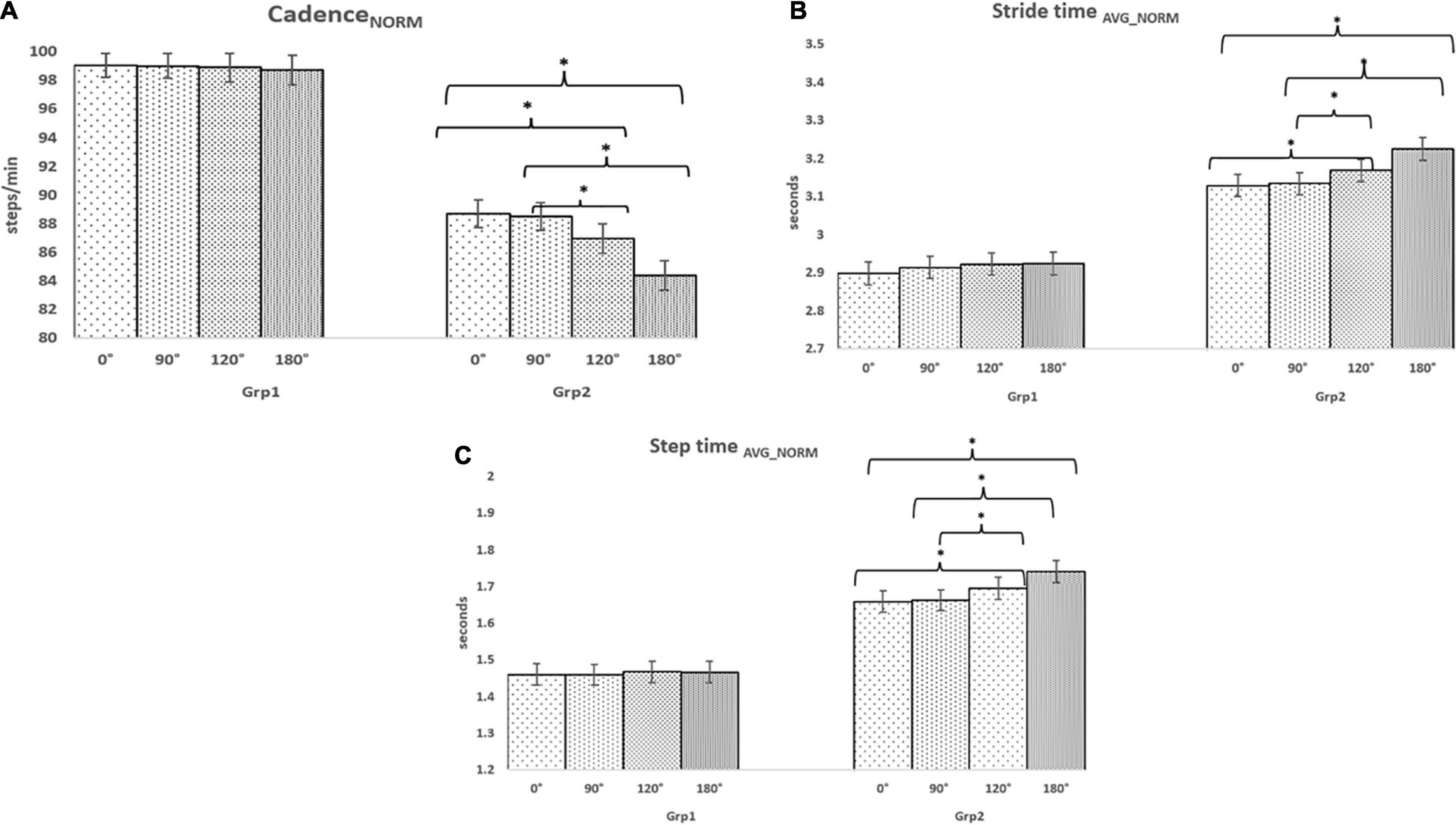
Figure 2. Comparative analysis of Group (Grp1 and Grp2) average (A) CadenceNORM for TaskC1, (B) Stride timeAVG_NORM for TaskC1, and (C) Step timeAVG_NORM for TaskC1. *p < 0.05.
While considering inter-group analysis, we could find that irrespective of the pathways with varying turns, there was a reduction (%Δ = 10.45%, %Δ = 10.58%, %Δ = 12.04%, and %Δ = 14.53% for 0, 90, 120, and 180°, respectively) in group average CadenceNORM from Grp1 to Grp2 and an increase in Stride timeAVG_NORM (%Δ = 7.54%, %Δ = 7.98%, %Δ = 8.39%, and %Δ = 10.28% for 0, 90, 120, and 180°, respectively) and Step timeAVG_NORM (%Δ = 13.60%, %Δ = 13.98%, %Δ = 15.52%, and %Δ = 18.65% for 0, 90, 120, and 180°, respectively) from Grp1 to Grp2. The Independent sample Mann–Whitney test indicated that all the gait-related indices were statistically different (with p-value ranging from 0.01 to 0.03) with a large effect (ranging from r = 0.7 to r = 0.8) between Grp1 and Grp2 irrespective of pathways with varying turn angles.
The intra-group analysis for TaskC2 indicated that the group average CadenceNORM (Figure 3A) decreased as the turn angle of the pathways increased and the Normalised Stride time (Figure 3B) and Step time (Figure 3C) increased as the turn angle of the pathways increased for each of Grp1 and Grp2 (similar to TaskC1). Again, from Figures 2A, 3A, we find that for pathways with varying turns, the CadenceNORM for TaskC1 was higher (%Δ = 0.40, 0.83, 0.80, and 1.08% for 0, 90, 120, and 180°, respectively, for Grp1 and (%Δ = 1.31, 1.82, 1.92, and 2.09% for 0, 90, 120, and 180°, respectively, for Grp2) than that for TaskC2. Similar was the observation in terms of increase in the Normalised Stride and Step times from TaskC1 to TaskC2. A dependent sample Wilcoxon Signed Rank test revealed statistical variation (with a p-value ranging from 0.03 to 0.04) with a large effect (ranging from r = 0.66 to r = 0.69) in all the gait-related indices between 0 and 180° for Grp1 during TaskC2, unlike that in TaskC1. In contrast, for Grp2, all the gait-related indices corresponding to pathways with varying pathway turn angles were statistically different (with p-value ranging from 0.01 to 0.04) with a large effect (ranging from r = 0.7 to r = 0.9).
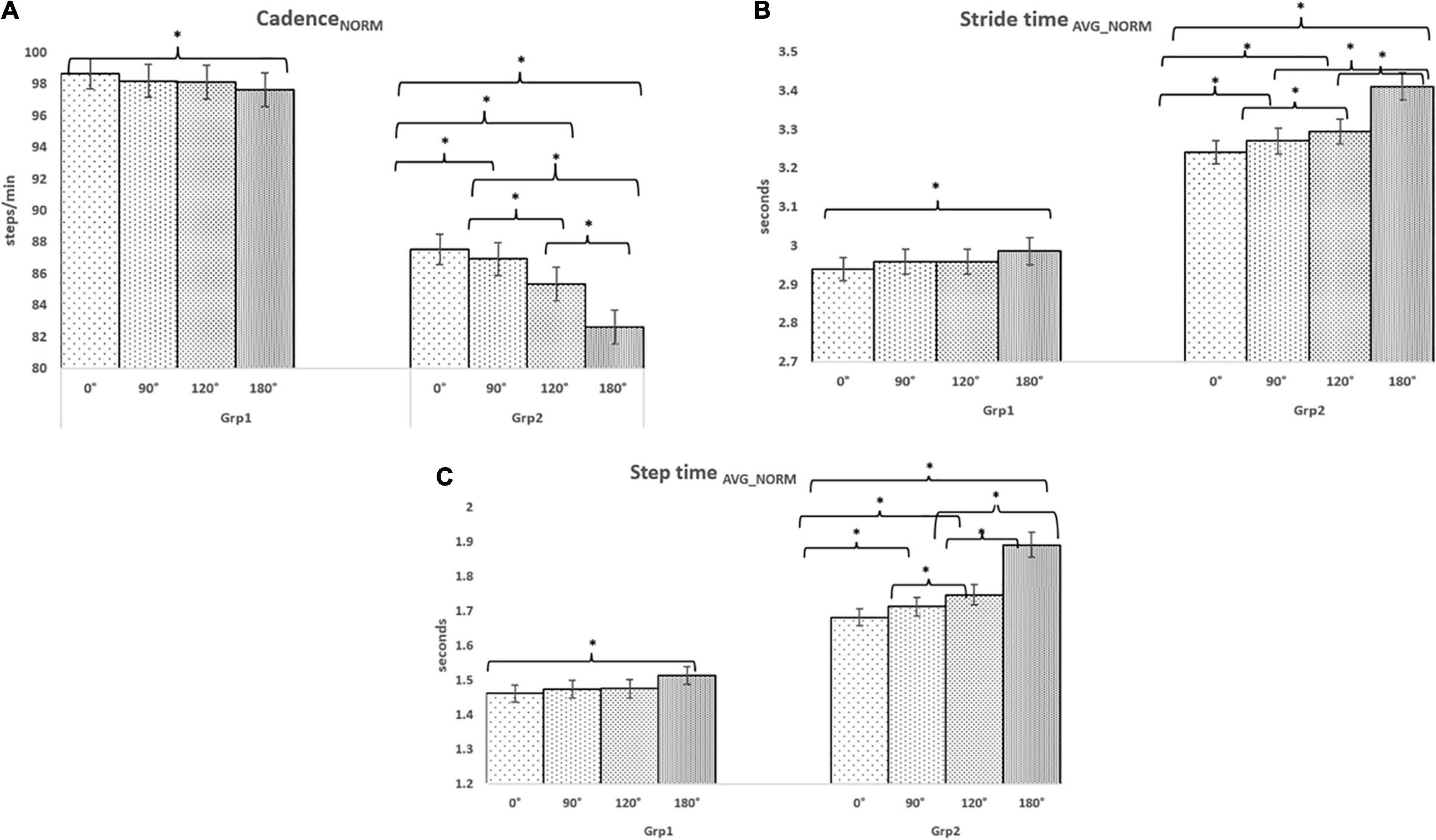
Figure 3. Comparative analysis of Group (Grp1 and Grp2) average (A) CadenceNORM for TaskC2, (B) Stride timeAVG_NORM for TaskC2, and (C) Step timeAVG_NORM for TaskC2. *p < 0.05.
While considering the inter-group analysis, we could find that irrespective of pathway turn, there was a reduction in group average CadenceNORM (%Δ = 11.90 and 12.77%, respectively, for TaskC1 and TaskC2) from Grp1 to Grp2 and an increase in Stride timeAVG_NORM (%Δ = 8.54 and 11.58%, respectively, for TaskC1 and TaskC2) and Step timeAVG_NORM (%Δ = 15.43 and 18.64%, respectively, for TaskC1 and TaskC2) from Grp1 to Grp2. The Independent sample Mann–Whitney test indicated that all the gait-related indices were statistically different (with p-value ranging from 0.01 to 0.04) with a large effect (ranging from r = 0.52 to r = 0.9) between Grp1 and Grp2 corresponding to pathways with varying turn angles. Again, while comparing the observations for TaskC1 and TaskC2, the %Δ in the gait-related indices between Grp1 and Grp2 during TaskC2 was higher than that for TaskC1.
We wanted to understand whether both the pathways having varying turns and task conditions were equally effective in affecting the gait of Grp1 and Grp2. Irrespective of the task condition, pathways having varying turns contributed to statistically significant variation (with p-value ranging from 0.01 to 0.03) with a large effect (ranging from r = 0.7 to r = 0.8) using Dependent sample Wilcoxon Signed Rank test) in the gait-related indices for Grp2 unlike that for Grp1 (with no statistical difference in the indices except that between pathways with 0 and 180° turns for TaskC2).
Again, irrespective of the pathway having varying turns, variation in the task condition contributed to statistically significant variation (with a p-value ranging from 0.01 to 0.048) with a large effect (ranging from r = 0.52 to r = 0.9) using dependent sample Wilcoxon Signed Rank test in the gait-related indices for Grp2 and Grp1. In summary, both the pathways (with turns) and task condition were effective in affecting the gait of the older group (Grp2) unlike that of the younger group (Grp1), whose gait was more affected by the variation in task condition than that due to pathway having varying turn angles. However, given the small sample size, we do not intend to generalize our observations.
Having seen that the increase in pathway turn contributes to variation in one’s gait-related indices and that the 180° pathway turn caused statistical variations in the gait-related indices of even the healthy young adults, concerning that with 0° turn in the case of TaskC2, we wanted to understand the implication of pathways with 0 and 180° turn angles on the gait-related indices of age and gender-matched healthy elderly (Grp3) and individuals with PD (Grp4) through a pilot study (i.e., phase 2). Also, we wanted to carry out a comparative investigation of the effect of task conditions on their gait-related indices. Again, given that knee flexion is associated with a stereotypical stooped appearance in individuals with PD (Yoshii et al., 2016) that might be related to falls (Yoshii et al., 2016), we wanted to understand the implication of pathways with varying turn angles and task condition on the knee flexion measured by the Knee Angle Recorder Unit.
The intra-group analysis for TaskC1 indicated a reduction (%Δ = 2.78%) in the group average CadenceNORM (Figure 4A) with an increase in turn angle of pathways for Grp3 (similar findings as discussed earlier for Grp2) and an increase in Stride timeAVG_NORM (%Δ = 3.06%) (Figure 4B) and Step timeAVG_NORM (%Δ = 2.04%) (Figure 4C) with an increase in turn angle of pathways for Grp3 (similar findings as discussed earlier for Grp2). In contrast, for Grp4, an increment (%Δ = 4.14%) in the group average CadenceNORM (Figure 4A) for pathway with increasing turn angles and a decrease in Stride timeAVG_NORM (%Δ = 5.93%) (Figure 4B) and Step timeAVG_NORM (%Δ = 6.46%) (Figure 4C) for pathway with increasing turn angles were observed. A dependent sample Wilcoxon Signed Rank test revealed statistical variation (p-value = 0.04) with a large effect (r = 0.9) in all the gait-related indices while considering pathways with 0 and 180° turns for both groups during TaskC1. In addition, we wanted to understand the clinical relevance of such statistical variations in the gait-related indices of Grp4 in terms of its relation to FES scores. Pearson’s correlation (Ratner, 2009) between their FES scores and gait-related indices on an average was ∼0.70 for pathway with 00 turns and ∼0.64 for that with 180° turns.
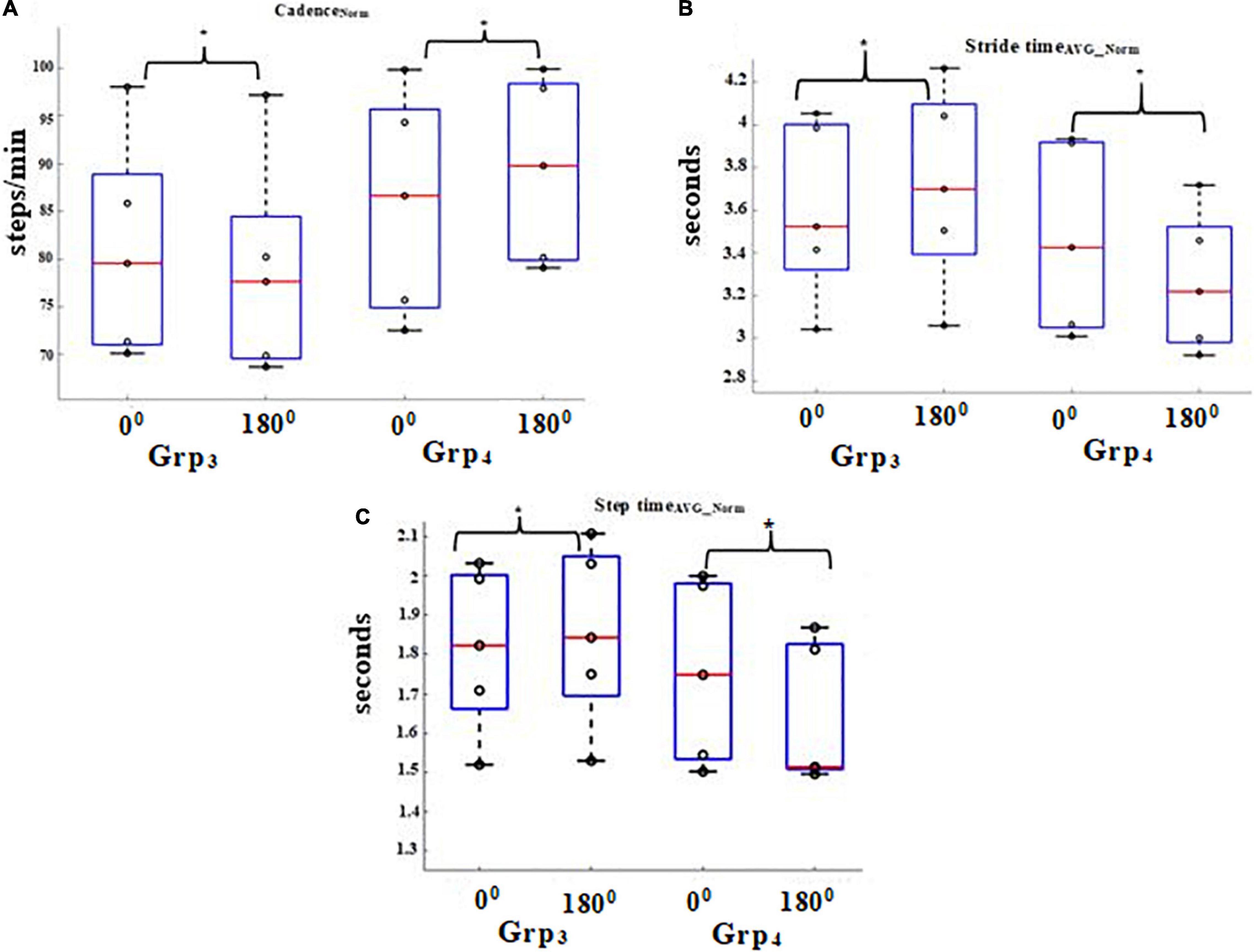
Figure 4. Comparative analysis of Group (Grp3 and Grp4) average (A) CadenceNORM for TaskC1, (B) Stride timeAVG_NORM for TaskC1, and (C) Step timeAVG_NORM for TaskC1. *p < 0.05.
The intra-group analysis for TaskC2 indicated a reduction (%Δ = 3.85%) in the group average CadenceNORM (Figure 5A) with an increase in the turn angle of pathways for Grp3 (similar to that in TaskC1 above) and an increase in the Normalised Stride time (%Δ = 4.89%) (Figure 5B) and Step time (%Δ = 4.12%) (Figure 5C) for pathways with increasing turn angle for Grp3 (similar to that in TaskC1 above). In contrast, for Grp4, we can see that there was an increment (%Δ = 15.92%) in the group average CadenceNORM (Figure 5A) with an increase in the turn angle of pathways (similar to that in TaskC1) and a decrease in Stride timeAVG_NORM (%Δ = 17.94%) (Figure 5B) and Step timeAVG_NORM (%Δ = 17.83%) (Figure 5C) with an increase in turn angle of pathways (similar to that in TaskC1). However, the variation in the group average values of all the gait-related indices for pathways with 0 and 180° turns was much higher in TaskC2 when compared with TaskC1, showing the increased effect of TaskC2 on one’s fall risk than the TaskC1. Given that the number of participants in each group is small, we do not want to generalize our findings. A dependent sample Wilcoxon Signed Rank test revealed statistical variation (p-value = 0.04) with a large effect (r = 0.9) in all the gait-related indices while considering pathways with 0 and 180° turns for both groups during TaskC2 (similar to that in TaskC1). About the clinical relevance of such statistical variations in the gait-related indices of Grp4 in terms of its relation to FES scores, we found that on an average the correlation was ∼0.74 for pathway with 0° turns and ∼0.61 for that with 180° turns.
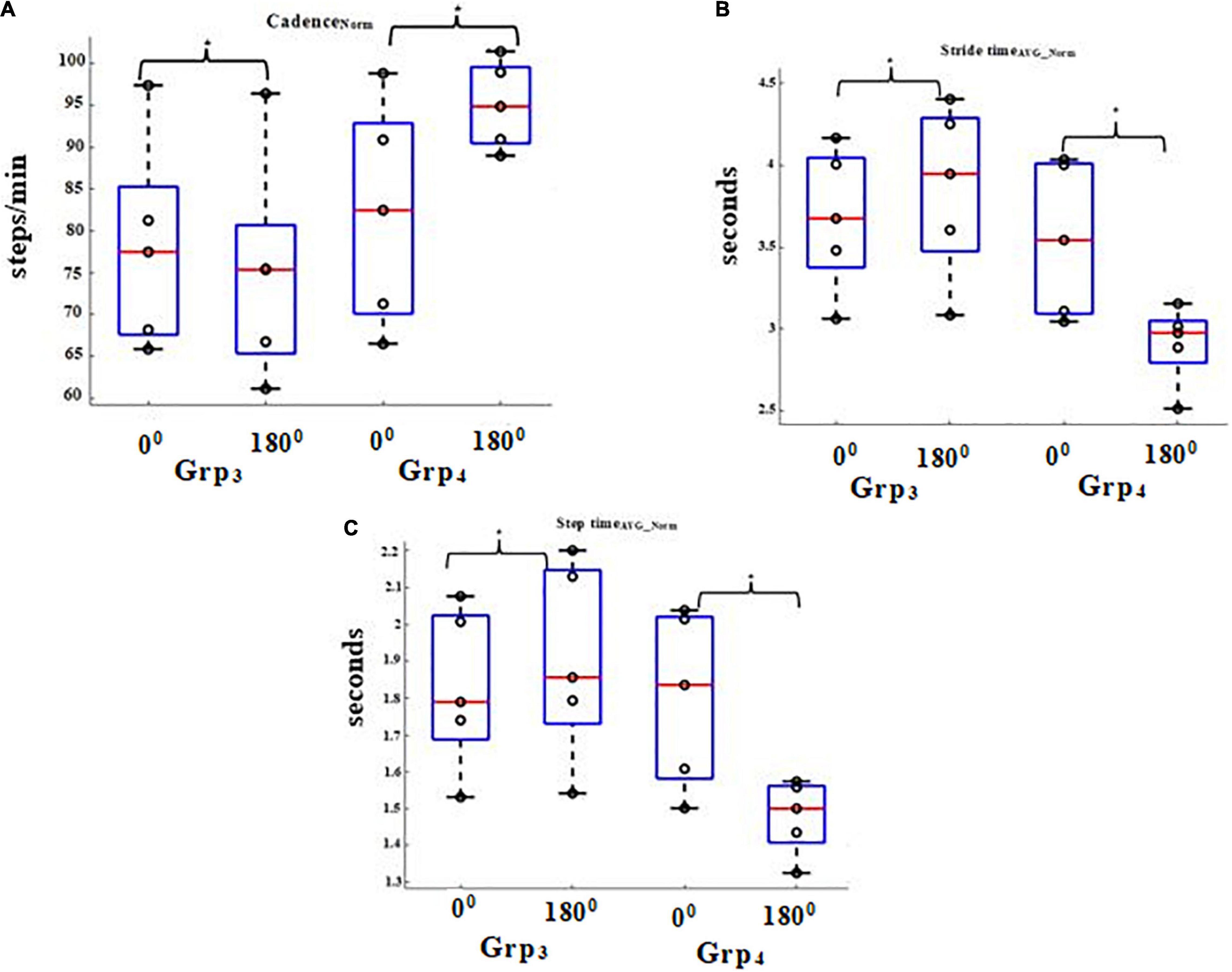
Figure 5. Comparative analysis of Group (Grp3 and Grp4) average (A) CadenceNORM for TaskC2, (B) Stride timeAVG_NORM for TaskC2, and (C) Step timeAVG_NORM for TaskC2. *p < 0.05.
In gait analysis, variability is commonly understood in terms of the fluctuation in the value of a joint angle (Chau et al., 2005). We were interested in further investigating the variability in the knee flexion measured by the Knee Angle Recorder Unit of Grp3 and Grp4 during the heel-strike event while walking on pathways having 0 and 180° turns under both the task conditions since the heel-strike is an important contributor to the bipedal stability (O’Sullivan et al., 2013). Here, we present the group average Coefficient of Variation (%CV; Section Extraction of Gait-related Indices) of the knee flexion of participants during the heel-strike event.
It can be seen from Figure 6 that the %CV of the knee flexion for Grp4 was found to be statistically higher (p-value = 0.04) with a large effect (r = 0.9) for pathway with 180° turns than that with 0° turns for each of TaskC1 and TaskC2 (i.e., %Δ = 41.48 and 66.05% for 0 and 180°, respectively, for TaskC1 and %Δ = 38.13 and 86.18% for 0 and 180°, respectively, for TaskC2) when compared with age and gender-matched healthy elderly irrespective of task conditions. Additionally, the pathway with 180° turn led to increased variation in the knee flexion particularly for Grp4, and these variations were found to be higher for TaskC2 than that for TaskC1 (i.e., %Δ = 30.29 and 62.83% for TaskC1 and TaskC2). About the clinical relevance of such variations in the knee flexion of Grp4 in terms of its relation to FES scores, we found that on average, the correlation was ∼0.68 for pathway with 0° turns and ∼0.62 for that with 180° turns. However, the correlation between the %CV of the knee flexion and FES scores does not necessarily imply that the %CV of the knee flexion (that is considered as a possible proxy measure of bipedal instability of an individual) is a cause behind the bipedal instability. Given that the number of participants in Grp4 was small, we do not want to generalize our findings.
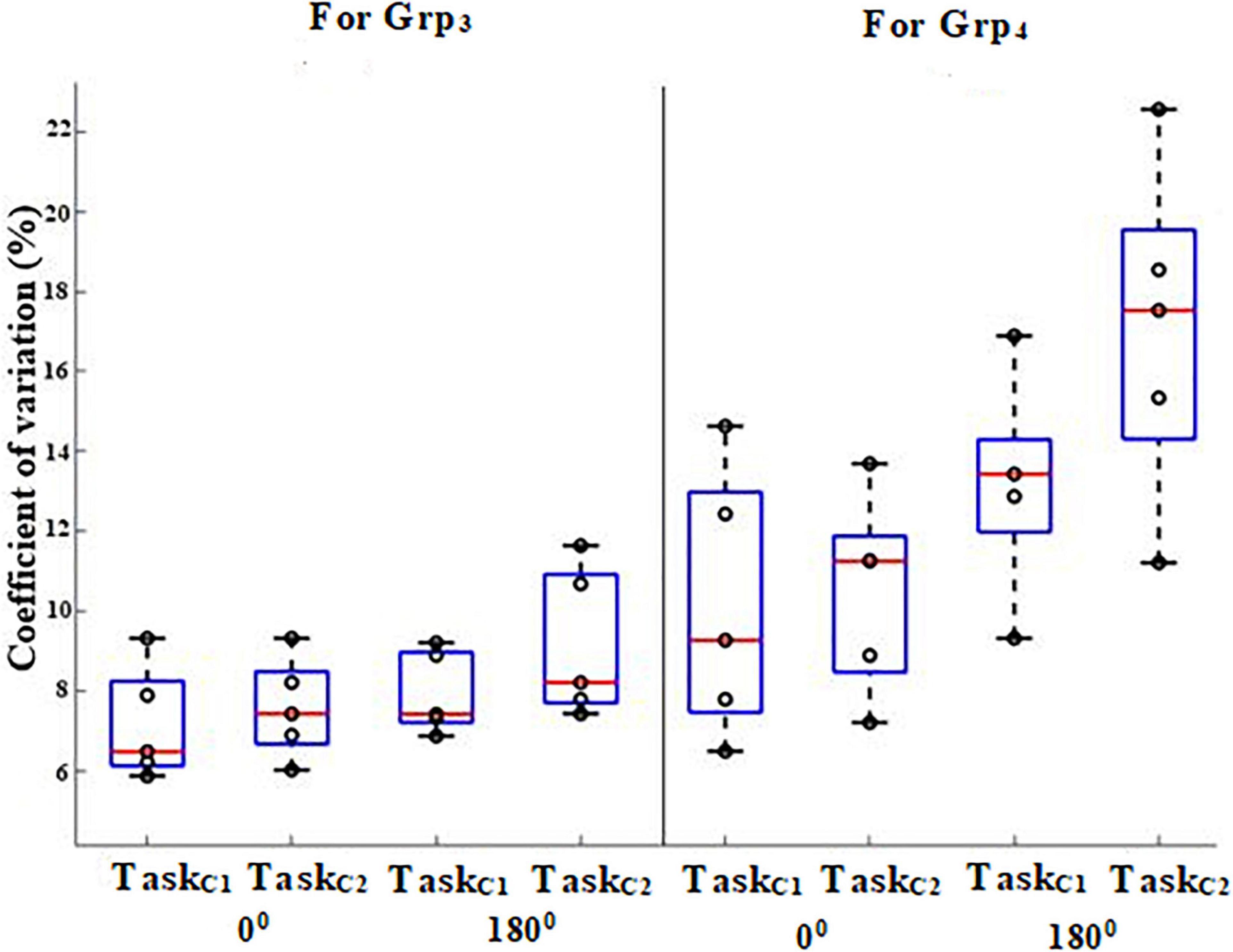
Figure 6. %CV of knee flexion angle while walking on 0 and 180° during heel-strike of Grp3 and Grp4.
After understanding the implication of variation in knee flexion during heel-strike events on one’s gait, we wanted to do a deeper investigation of the contribution of the pathway segments [e.g., straight and turn segments (Figure 1B)] on the knee flexion of Grp3 and Grp4, while walking overground on pathways having 0 and 180° turns for both the task conditions. For this, we computed the average %change in knee flexion from the respective AngleBaseline measure (see Section “Procedure”) of Grp3 and Grp4 while utilizing the synchronising markers issued by the Ultrasonic Sensor Unit (Figure 1A) tracking the distance (d say) traversed (by a participant) along the pathway laid out using the pathway delineator for (i) 0 m ≤ d ≤ 1 m, (ii) 1 m < d ≤ 4 m, (iii) 4 m < d ≤ 6 m, and (iv) 6 m < d ≤ 10 m.
It can be seen from Figures 7A,B that the %change in knee flexion from the respective AngleBaseline measure (irrespective of the task condition and pathways with 0 and 180° turns) was higher for Grp4 than that of Grp3 corresponding to each pathway segment. Again, for Grp4, while considering the pathway with 180° turn, the %change in knee flexion from the respective AngleBaseline was maximum for the turn segment (i.e., 4 m < d ≤ 6 m) for each of TaskC1 and TaskC2 (Figure 7B). However, the %change in knee flexion from respective AngleBaseline was found to be higher in TaskC2 (irrespective of the pathway segment) than that in TaskC1 (average %Δ = 13.45 and 22.60%, respectively, for pathways with 0 and 180° turns). In contrast, for Grp3 (Figure 7A), in TaskC2, we saw relatively less %change in knee flexion from the respective AngleBaseline (irrespective of the pathway segments) than that in TaskC1 (average %Δ = −2.83 and −2.39%, respectively, for pathways with 0 and 180° turns). Given that the number of participants in both groups was small, we do not want to generalize our findings.
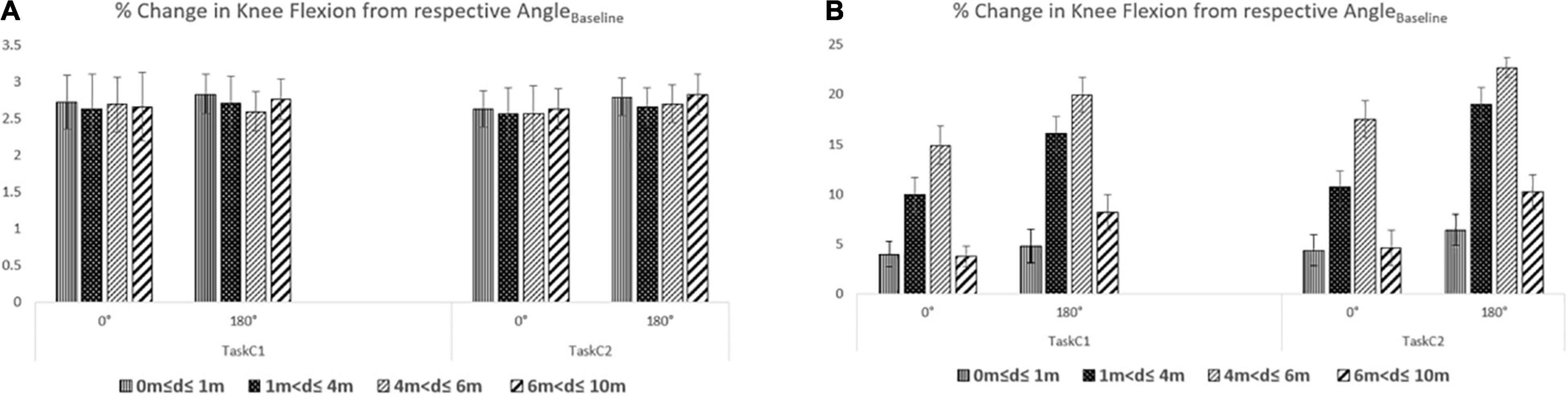
Figure 7. %Change of knee flexion from respective AngleBaseline while walking overground on 0 and 180° (A) for Grp3 and (B) for Grp4.
During TaskC2, the participants counted backward while walking on pathways having varying turn angles. Their counting performance (in terms of the number of errors made in counting) was analysed and is shown in Figure 8. While in phase 1 of the study, Grp1 and Grp2 walked on pathways having 0, 90, 120, and 180° turns, in phase 2, Grp3 and Grp4 walked on the pathways having 0 and 180° turns. We can see that Grp4 made the maximum number of counting errors corresponding to the pathways traversed by them with Grp3, making more counting errors than Grp2, who, in turn, made more errors than Grp1 with an inter-group statistical difference (with p-value ranging from 0.040 to 0.048) with large effect (ranging from r = 0.65 to r = 0.69) based on an independent sample Mann–Whitney test (except for pathway with 0° turn between Grp1 and Grp2, between Grp1 and Grp3, and between Grp2 and Grp3).
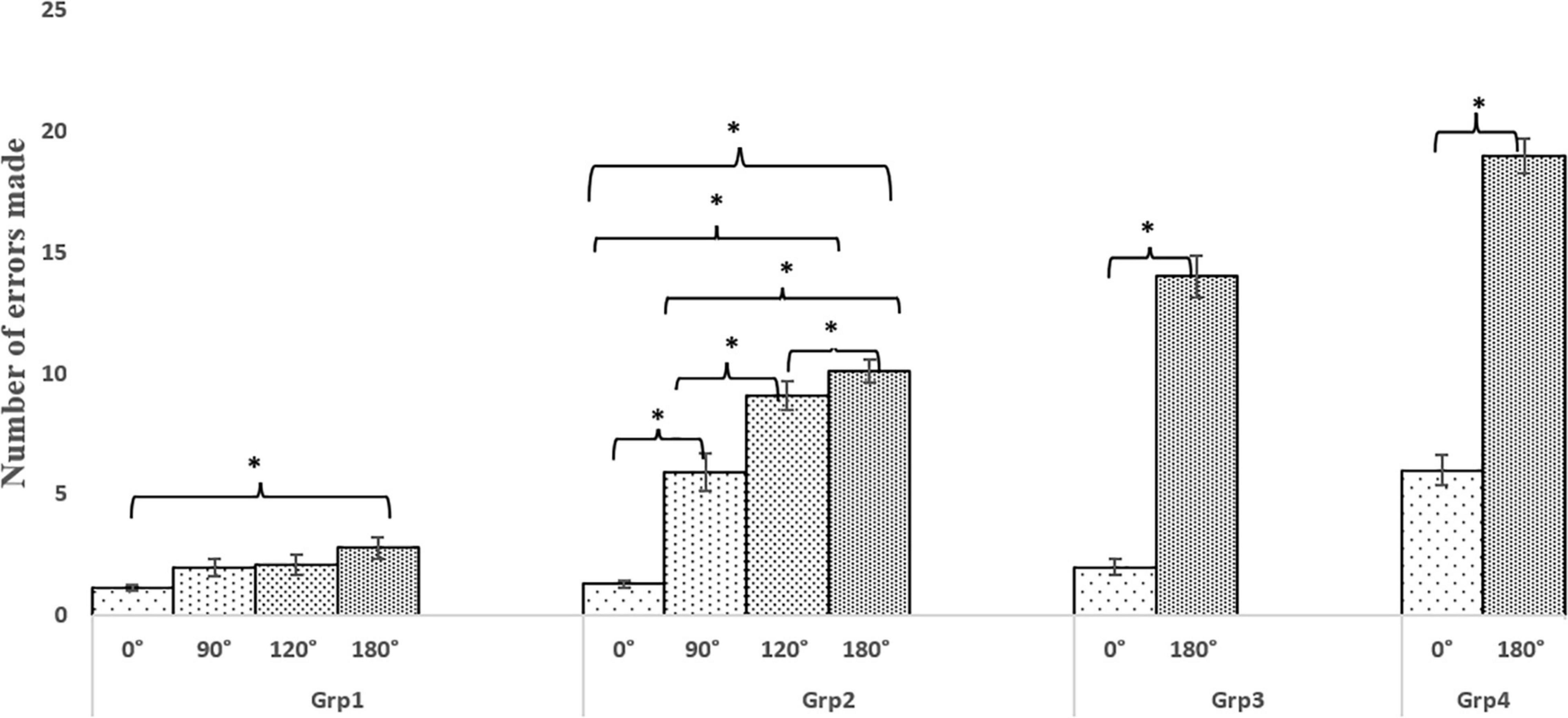
Figure 8. Comparative group analysis of implications of task conditions on the errors made by Grp1, Grp2, Grp3, and Grp4. *p-value < 0.05.
Again, considering the intra-group analysis (with dependent sample Wilcoxon Signed Rank test), for Grp1, we found that the counting performance was statistically different (p-value = 0.048) and large effect (r = 0.8) only between pathways with 0 and 180° turns. For Grp2, the counting performance was statistically different (p-value = 0.048) with a large effect (r = 0.7) across all the pathways with 0, 90, 120, and 180° turns. Finally, for each of Grp3 and Grp4, the difference in the counting performance between pathways with 0 and 180° turns was statistical (p-value = 0.048) with a large effect (r = 0.8).
In summary, a higher number of counting errors made by the elderly groups (Grp2, Grp3, and Grp4) can be an indicator of reduced cognitive performance (Maclean et al., 2017) under dual-task conditions (TaskC2), particularly for the pathway with 180° turn which was accompanied with a deterioration in their gait performance (Figures 4–7). Again, the decrease in the cognitive and gait performance was the most prominent for individuals with PD (i.e., Grp4) among all the participants, specifically for the pathway with 180° turn under dual-task conditions. Given that the number of participants in Grp4 was small, we do not want to generalize our findings.
The main contribution of this study was to examine the implication of pathways with varying turn angles and task conditions on the gait of healthy young (Grp1), healthy elderly (Grp2 and Grp3) and individuals with PD (Grp4) by using a wearable system, namely SmartWalk that can quantify gait in terms of (gait-related indices using Instrumented Insoles and knee flexion using Knee Angle Recorder Unit). Even though there are different factors that can contribute to one’s risk of falls, our wearable system can be used to measure at least a few of these factors, namely variation in one’s gait-related indices and postural changes (in terms of knee flexion) while walking that can have relevance to one’s falls. Again, unlike previous studies that explored the implication of either walking on pathways having various turns (de Morais Faria et al., 2016) or walking under various task conditions (Bayot et al., 2020), here we have investigated the differentiated implication of walking on pathways with varying turn angles (0, 90, 120, and 180°) and task conditions [single (TaskC1) and dual-task (TaskC2) conditions] on one’s gait-related indices and knee flexion by carrying out a systematic study involving cognitively healthy adults belonging to younger and older age groups. In addition, we have investigated the implication of walking on pathways with turns on counting performance along with its dependence on age and also among those with PD.
In an endeavour to investigate the differentiated implication of walking on pathways with varying turn angles and task conditions on one’s gait-related indices, we first studied the effect of pathways with varying turn angles while keeping the task condition the same. For each of TaskC1 and TaskC2, we observed a reducing trend in the normalised cadence along with an increasing trend in normalised stride and step times due to walking on pathways with increasing turning angles for each of Grp1, Grp2, and Grp3. A reduction in cadence might infer an increased tendency of the healthy adults to stabilize themselves to prevent falls triggered by pathways having turns (Cao et al., 1997), with the implication being more prominent for pathways having 120 and 180° turns. The turn segments are 120 and 180°, comprising of one 90° turn [often considered to be a rapid change in direction of walk that might trigger unstable walk (Dotov et al., 2016)] along with an additional 30° turn and two 90° turns, respectively, might trigger unstable walk, thereby making these pathways leading to increasing the risk of fall (de Morais Faria et al., 2016), particularly true for Grp2 and Grp3. In-depth data analysis on stride and step times of our participants under different task conditions and pathways with turns show that for Grp1, the variability in the group average normalised stride time was nearly double the group average normalised step time, particularly for pathway with turning angle of 180° irrespective of the task condition. Such observation can be possibly attributed to the spin turn (Gavriliuc et al., 2019) being demonstrated by the majority (∼70%) of Grp1, while traversing the turn segment [i.e., 4 m < d ≤ 6 m; Figure 1B] of the pathway in which one altered direction by spinning his/her body about the pivot foot (Gavriliuc et al., 2019) [with the rest (∼30%) of the Grp1 showing step turn (Gavriliuc et al., 2019)], thereby affecting the stride made by the individual (specifically at the turn segment of the pathway). However, for Grp2, Grp3, and Grp4, the variability in the group average normalised stride time was nearly similar to that of step time, which can be possibly attributed to the majority of our elderly healthy participants, i.e., Grp2 and Grp3 (∼63% showing step turn; rest showing spin turn), and individuals with PD, i.e., Grp4 (∼100%), showed step turn [marked by a weight shift from one leg to the other, while changing the direction of walking (Gavriliuc et al., 2019)], while traversing the turn segment of the pathway to ensure greater stability (Taylor et al., 2005) and prevent possible fall. While considering all the gait-related indices specifically for Grp4, we saw a decrease in normalised stride and step times along with an increase in the normalised cadence due to walking on pathways with increasing turning angles. Such observation for individuals with PD can be indicative of the risk of falls (Hoskovcová et al., 2015) due to pathways with turns, which not only threatens their dynamic stability (Bhatt et al., 2013), but also can be a major contributor to triggering of the freezing (Bhatt et al., 2013) that, in turn, might lead to falls (Bhatt et al., 2013). Again, while exploring the effect of task conditions while keeping the pathways with varying turn angles the same, the variation in the group average values of all the gait-related indices was much higher in TaskC2 than that in TaskC1, attributed to greater cognitive load (Bayot et al., 2020) in TaskC2 as compared to TaskC1.
Again, to investigate the differentiated implication of walking on pathways with varying turn angles and task conditions on one’s postural changes (in terms of knee flexion), we investigated the variation in one’s knee flexion for Grp3 and Grp4. While exploring the effect of pathways having varying turn angles (0 and 180°) while keeping the task condition the same, we found that the pathway with 180° turn elicited greater variability in the knee flexion at heel-strike than that for 0° for each of Grp3 and Grp4 with the variability being higher for Grp4 than that of Grp3. Similar observations about Grp3 and Grp4 while exploring the effect of task conditions while keeping the pathways the same (i.e., pathways having either 0 or 180° turn). Such an observation might infer that Grp4 experienced greater turning difficulties (Bhatt et al., 2013) and also the dual-task condition (contributing to the cognitive load) might have led to increased postural instability in them (Bloem et al., 2006) compared to the age and gender-matched healthy elderly. Our findings are also in line with literature reporting that individuals with PD show more postural instabilities (Yoshii et al., 2016) than their healthy counterparts, and this might be due to greater difficulty in coordination and timing faced by them (Bloem et al., 2006) making them more prone to falls.
While we have been investigating the implications of walking on pathways having varying turn angles on one’s postural changes (in terms of knee flexion), we have been looking at the contribution of the pathway in its entirety rather than exploring the contribution of individual segments (e.g., straight and turn segments) of the pathway on one’s postural changes in Grp3 and Grp4. Our results showed that the %change in knee flexion (irrespective of the pathway segments and the task condition) was higher for Grp4 than that of Grp3 for both pathways with 0 and 180° turns. Such observations are in line with the literature (Yoshii et al., 2016) indicating that a flexed posture is often demonstrated by individuals with PD while walking. Again, the effect of the turn segment (i.e., 4 m < d ≤ 6 m) on the knee flexion was higher than that of the other pathway segments and this was true for each of TaskC1 and TaskC2 with the effect being more prominent for TaskC2 than that for TaskC1. This might be due to the dual task (TaskC2), causing the individuals with PD to divide their attention between both the components (i.e., walking and counting), while employing posture second strategy (Bloem et al., 2006) associated with the risk of falls.
Added to exploring the implication of pathways with varying turn angles and task conditions on one’s gait and posture, we also explored the counting performance of all our participants. Our results show that the elderly (Grp2, Grp3, and Grp4) made more counting errors than that the younger group (Grp1) corresponding to pathways having varying turn angles with Grp4 making the maximum number of counting errors for pathways with 180° turns. Based on the gait-related indices [i.e., reduction in normalised cadence and increase in normalised stride and step times (Figure 3) and the counting performance (Figure 8) of Grp2 and Grp3], we can say that both of these groups prioritized gait over cognition while employing ‘posture first strategy’ (Bayot et al., 2020) to ensure stability (Novak et al., 2016), unlike Grp1 who enjoyed automaticity of walk (Clark, 2015) and prioritized cognition over gait (Plummer et al., 2015). In contrast, for Grp4, an increase in the number of counting errors irrespective of the pathways having varying turns (Figure 8) coupled with an increment in normalised cadence, along with a reduction in the normalised stride and step times (Figures 4, 5), along with increased variation in the knee flexion (Figures 6, 7) compared to Grp3 might infer that Grp4 used a “posture second” strategy and treating all elements of a complex task with equal priority, while compromising with balance, leading to falls (Yoshii et al., 2016).
In summary, in our present study, we investigated the implications of pathways with varying turns and task conditions on one’s gait-related indices, knee flexion, and counting performance in healthy young, healthy old, and age and gender-matched individuals with PD. Our results indicated that for the older group, both the pathway with varying turns and the task conditions affected the gait-related indices and the knee flexion, though the implication was greater for the individuals with PD than the healthy old. Our results indicated that the gait-related indices of individuals with PD showed a lack of dynamic balance [as evident from the correlation of gait-related indices with the FES score (see Section “Implication of Pathway With Varying Turns on Gait-Related Indices: For TaskC1” and Section “Implication of Pathway With Varying Turns on Gait-Related Indices: For TaskC2”)] when compared with age and gender-matched healthy old. A comparatively higher variation in knee flexion of individuals with PD than the healthy old was observed that might be indicative of their increased proneness to falls. Again, pathways with varying turn angles elicited variations in the counting performance under dual-task condition that was more prominent in the older group (with the counting performance error being more for the individuals PD than the healthy old and the discrepancy between the two groups being more for pathway with larger turn angle) than the younger group. Such an observation can be attributed to the prioritization of gait over cognition while employing the ‘posture first strategy’ by the healthy old and the ‘posture second strategy’ adopted by the individuals with PD during the dual task (attributed to the individuals dividing their attention between walking and counting while employing posture second strategy increasing their proneness to fall than that in the healthy old). In contrast, for the younger group, the implication of variation in the task condition on their gait-related indices was stronger than that due to pathways with varying turns.
Though the results were promising, our study had certain limitations. The sample size was limited. In the future, we plan to enroll a larger participant pool. Another limitation was the use of a limited variation in the pathway turns in our study. With daily living tasks requiring one to walk on pathways with turns up to 210° (de Morais Faria et al., 2016), we plan to investigate the implications of pathways with a turn angle >180° on one’s gait. Also, the walkway terrain was level ground. The implications might differ with different walkway terrains, such as uphill or downhill terrains. Another limitation of SmartWalk was that it looked to only one’s gait and knee flexion (for postural changes) for understanding one’s possible risk of fall. However, there can be other factors that can contribute to one’s risk of falls. For example, increased neck flexion, flexed posture, etc. (Yoshii et al., 2016) are also important elements contributing to postural changes that can have a role in one’s risk of falls. In the future, we plan to add these aspects to get a comprehensive view of one’s postural changes. Again, about the clinical measure for falls, we considered collecting FES scores from our participants. In the future, we plan to extend our study while incorporating other clinical measures, e.g., the Dynamic Gait Index (Badke et al., 2004) for quantifying one’s dynamic balance and fear of falls.
Notwithstanding the above limitations, our present study provided us with an understanding of the differentiated implications of pathways with varying turn angles and task conditions on at least some of the important aspects of one’s gait. Also, SmartWalk can offer valuable information to the clinicians regarding specific turn angles and task conditions that can be detrimental to individuals with PD about their falls, thereby offering pre-clinical inputs to the design of intervention studies.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Institutional Ethics Committee (IEC), IIT Gandhinagar. The patients/participants provided their written informed consent to participate in this study.
PP and UL drafted the manuscript and contributed to the experiment design, experimental data collection with healthy and individuals with Parkinson’s disease, data analysis, and statistical analysis. NJ and SD contributed to the enrolment of individuals with Parkinson’s disease and accessing their clinical measures. NP and MK contributed to the design of SmartWalk from the perspective of ergonomics and the pathway delineator. All authors read, corrected/commented on, and approved the final manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors would like to thank the SBB College of Physiotherapy, Centre for Biomedical Engineering of Indian Institute of Technology (IIT) Gandhinagar for providing the resources and space to carry out this study. In addition, the authors would like to thank BIRAC, DST, SERB-POWER, and Tata Innovation Fellowship for partially funding this research. They would also like to thank all the participants for their cooperation and for giving us their valuable time.
Akram, S. B., Frank, J. S., and Chenouri, S. (2010). Turning behavior in healthy older adults: is there a preference for step versus spin turns? Gait Posture 31, 23–26. doi: 10.1016/j.gaitpost.2009.08.238
Angelini, L., Di Puccio, F., Zander, T., and Schmidt, H. (2016). Influence of arm motion on spatio-temporal gait parameters and force data. J. Sports Phys. Educ. 3, 12–16.
Badke, M. B., Shea, T. A., Miedaner, J. A., and Grove, C. R. (2004). Outcomes after rehabilitation for adults with balance dysfunction. Arch. Phys. Med. Rehabil. 85, 227–233. doi: 10.1016/j.apmr.2003.06.006
Bayot, M., Dujardin, K., Dissaux, L., Tard, C., Defebvre, L., Bonnet, C. T., et al. (2020). Can dual task paradigms predict falls better than single task? – a systematic literature review. Neurophysiol. Clin. 50, 401–440. doi: 10.1016/j.neucli.2020.10.008
Begg, R. K., and Sparrow, W. A. (2006). Ageing effects on knee and ankle joint angles at key events and phases of the gait cycle. J. Med. Eng. Technol. 30, 382–389. doi: 10.1080/03091900500445353
Bergland, A., Jarnlo, G.-B., and Laake, K. (2003). Predictors of falls in the elderly by location. Aging Clin. Exp. Res. 15, 43–50. doi: 10.1007/BF03324479
Bhatt, H., Pieruccini-Faria, F., and Almeida, Q. J. (2013). Dynamics of turning sharpness influences freezing of gait in Parkinson’s disease. Parkinsonism Relat. Disord. 19, 181–185. doi: 10.1016/j.parkreldis.2012.09.006
Bloem, B. R., Grimbergen, Y. A. M., van Dijk, J. G., and Munneke, M. (2006). The “posture second” strategy: a review of wrong priorities in Parkinson’s disease. J. Neurol. Sci. 248, 196–204. doi: 10.1016/j.jns.2006.05.010
Cao, C., Ashton-Miller, J. A., Schultz, A. B., and Alexander, N. B. (1997). Abilities to turn suddenly while walking: effects of age, gender, and available response time. J. Gerontol. A Biol. Sci. Med. Sci. 52, M88–M93. doi: 10.1093/gerona/52a.2.m88
Chau, T., Young, S., and Redekop, S. (2005). Managing variability in the summary and comparison of gait data. J. Neuroengineering Rehabil. 2:22. doi: 10.1186/1743-0003-2-22
Clark, D. J. (2015). Automaticity of walking: functional significance, mechanisms, measurement and rehabilitation strategies. Front. Hum. Neurosci. 9:246. doi: 10.3389/fnhum.2015.00246
de Morais Faria, C. D. C., Paula de Carvalho-Pinto, B., Nadeau, S., and Teixeira-Salmela, L. F. (2016). 180° turn while walking: characterization and comparisons between subjects with and without stroke. J. Phys. Ther. Sci. 28, 2694–2699. doi: 10.1589/jpts.28.2694
Dotov, D. G., Bardy, B. G., and Dalla Bella, S. (2016). The role of environmental constraints in walking: effects of steering and sharp turns on gait dynamics. Sci. Rep. 6:28374. doi: 10.1038/srep28374
Fang, X., Liu, C., and Jiang, Z. (2018). Reference values of gait using APDM movement monitoring inertial sensor system. R. Soc. Open Sci. 5:170818. doi: 10.1098/rsos.170818
Forghany, S., Nester, C. J., Tyson, S. F., Preece, S., and Jones, R. K. (2014). The effect of stroke on foot kinematics and the functional consequences. Gait Posture 39, 1051–1056. doi: 10.1016/j.gaitpost.2014.01.006
Fritz, C. O., Morris, P. E., and Richler, J. J. (2012). Effect size estimates: current use, calculations, and interpretation. J. Exp. Psychol. Gen. 141, 2–18. doi: 10.1037/a0024338
Gavriliuc, O., Paschen, S., Andrusca, A., Berg, D., Schlenstedt, C., and Deuschl, G. (2019). Spin turns in advanced Parkinson’s disease: a new clinical gait sign? Parkinsonism Relat. Disord. 69, 19–22. doi: 10.1016/j.parkreldis.2019.10.011
Hanan, H., Gunawan, A. A. N., and Sumadiyasa, M. (2019). Water level detection system based on ultrasonic sensors HC-SR04 and ESP8266-12 modules with telegram and buzzer communication media. Instrum. Meas. Metrol. 18, 305–309. doi: 10.18280/i2m.180311
Hanlon, M., and Anderson, R. (2009). Real-time gait event detection using wearable sensors. Gait Posture 30, 523–527. doi: 10.1016/j.gaitpost.2009.07.128
Hora, M., Soumar, L., Pontzer, H., and Sládek, V. (2017). Body size and lower limb posture during walking in humans. PLoS One 12:e0172112. doi: 10.1371/journal.pone.0172112
Hoskovcová, M., Dušek, P., Sieger, T., Brožová, H., Zárubová, K., Bezdíèek, O., et al. (2015). Predicting falls in Parkinson disease: what is the value of instrumented testing in off medication state? PLoS One 10:e0139849. doi: 10.1371/journal.pone.0139849
Jansen, K., De Groote, F., Duysens, J., and Jonkers, I. (2014). How gravity and muscle action control mediolateral center of mass excursion during slow walking: a simulation study. Gait Posture 39, 91–97. doi: 10.1016/j.gaitpost.2013.06.004
Lan, K.-C., and Shih, W.-Y. (2014). Using smart-phones and floor plans for indoor location tracking. IEEE Trans. Hum. Mach. Syst. 44, 211–221. doi: 10.3390/s17112678
Lee, S. I., Daneault, J.-F., Weydert, L., and Bonato, P. (2016). “A novel flexible wearable sensor for estimating joint-angles,” in Proceedings of the IEEE 13th International Conference on Wearable and ImplanTable Body Sensor Networks (BSN), San Francisco, CA, 377–382.
Maclean, L. M., Brown, L. J. E., Khadra, H., and Astell, A. J. (2017). Observing prioritization effects on cognition and gait: the effect of increased cognitive load on cognitively healthy older adults’ dual task performance. Gait Posture 53, 139–144. doi: 10.1016/j.gaitpost.2017.01.018
McGrath, T., and Stirling, L. (2020). Body-worn IMU human skeletal pose estimation using a factor graph-based optimization framework. Sensors 20:6887. doi: 10.3390/s20236887
Meimandi, M., Fadavi-Ghaffari, M., Taghizadeh, G., Azad, A., and Lajevardi, L. (2021). Falls efficacy scale and single item question: screening accuracy for older adults residing in nursing homes. Clin. Gerontol. 44, 544–551. doi: 10.1080/07317115.2020.1858467
Moon, Y., Wajda, D. A., Motl, R. W., and Sosnoff, J. J. (2015). Stride-time variability and fall risk in persons with multiple sclerosis. Mult. Scler. Int. 2015:964790. doi: 10.1155/2015/964790
Nagano, H., Begg, R. K., Sparrow, W. A., and Taylor, S. (2013). A comparison of treadmill and overground walking effects on step cycle asymmetry in young and older individuals. J. Appl. Biomech. 29, 188–193. doi: 10.1123/jab.29.2.188
Novak, A. C., Komisar, V., Maki, B. E., and Fernie, G. R. (2016). Age-related differences in dynamic balance control during stair descent and effect of varying step geometry. Appl. Ergon. 52, 275–284. doi: 10.1016/j.apergo.2015.07.027
O’Sullivan, S. B., Schmitz, T. J., and Fulk, G. (2013). Physical Rehabilitation. Philadelphia, PA: FA Davis.
Pallavi, P., Ranjan, S., Patel, N., and Lahiri, U. (2021). “Wearable technology for evaluation of risk of falls,” in Proceedings of the 43rd International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL. doi: 10.1109/EMBC46164.2021.9629940
Pandey, S., Bajaj, B. K., Wadhwa, A., and Anand, K. S. (2016). Impact of sleep quality on the quality of life of patients with Parkinson’s disease: a questionnaire-based study. Clin. Neurol. Neurosurg. 148, 29–34. doi: 10.1016/j.clineuro.2016.06.014
Paraschiv-Ionescu, A., Buchser, E. E., Rutschmann, B., Najafi, B., and Aminian, K. (2004). Ambulatory system for the quantitative and qualitative analysis of gait and posture in chronic pain patients treated with spinal cord stimulation. Gait Posture 20, 113–125. doi: 10.1016/j.gaitpost.2003.07.005
Pinkam, N., and Nilkhamhang, I. (2013). “Wireless smart shoe for gait analysis with automated thresholding using PSO,” in Proceedings of the 10th International Conference on Electrical Engineering/Electronics, Computer, Telecommunications and Information Technology (Krabi: IEEE), 1–6.
Plummer, P., Apple, S., Dowd, C., and Keith, E. (2015). Texting and walking: effect of environmental setting and task prioritization on dual task interference in healthy young adults. Gait Posture 41, 46–51. doi: 10.1016/j.gaitpost.2014.08.007
Ratner, B. (2009). The correlation coefficient: its values range between +1/-1, or do they? J. Target. Meas. Anal. Mark. 17, 139–142. doi: 10.1057/jt.2009.5
Rowe, P. J., Myles, C. M., Walker, C., and Nutton, R. (2000). Knee joint kinematics in gait and other functional activities measured using flexible electrogoniometry: how much knee motion is sufficient for normal daily life? Gait Posture 12, 143–155. doi: 10.1016/s0966-6362(00)00060-6
Shin, S.-S., An, D.-H., and Yoo, W.-G. (2015). Comparison of gait velocity and centre of mass during square and semicircular turning gaits between groups of elderly people with differing visual acuity. J. Phys. Ther. Sci. 27, 387–388. doi: 10.1589/jpts.27.387
Solanki, D., and Lahiri, U. (2018). Design of instrumented shoes for gait characterization: a usability study with healthy and post-stroke hemiplegic individuals. Front. Neurosci. 12:459. doi: 10.3389/fnins.2018.00459
Taylor, M. J. D., Dabnichki, P., and Strike, S. C. (2005). A three-dimensional biomechanical comparison between turning strategies during the stance phase of walking. Hum. Mov. Sci. 24, 558–573. doi: 10.1016/j.humov.2005.07.005
Thomas, A. A., Rogers, J. M., Amick, M. M., and Friedman, J. H. (2010). Falls and the falls efficacy scale in Parkinson’s disease. J. Neurol. 257, 1124–1128. doi: 10.1007/s00415-010-5475-x
Yardley, L., and Smith, H. (2002). A prospective study of the relationship between feared consequences of falling and avoidance of activity in community-living older people. Gerontologist 42, 17–23. doi: 10.1093/geront/42.1.17
Yoshii, F., Moriya, Y., Ohnuki, T., Ryo, M., and Takahashi, W. (2016). Postural deformities in Parkinson’s disease –mutual relationships among neck flexion, fore-bent, knee-bent and lateral-bent angles and correlations with clinical predictors. J. Clin. Mov. Disord. 3:1. doi: 10.1186/s40734-016-0029-8
Keywords: age, Parkinson’s, gait, posture, turnings, errors
Citation: Pallavi P, Jariwala N, Patel N, Kanetkar M, Diwan S and Lahiri U (2022) The Implication of Pathway Turn and Task Condition on Gait Quantified Using SmartWalk: Changes With Age and Parkinson’s Disease With Relevance to Postural Strategy and Risk of Fall. Front. Neurosci. 16:804397. doi: 10.3389/fnins.2022.804397
Received: 29 October 2021; Accepted: 31 March 2022;
Published: 29 April 2022.
Edited by:
Ryan Thomas Roemmich, Kennedy Krieger Institute, United StatesReviewed by:
Federico Villagra, Aberystwyth University, United KingdomCopyright © 2022 Pallavi, Jariwala, Patel, Kanetkar, Diwan and Lahiri. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Priya Pallavi, cHJpeWEucEBpaXRnbi5hYy5pbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.