
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Neurosci., 15 December 2022
Sec. Translational Neuroscience
Volume 16 - 2022 | https://doi.org/10.3389/fnins.2022.1026759
This article is part of the Research TopicThe Potential Effects and Mechanisms of Traditional Chinese Non-Pharmacological Therapy for Nero-musculoskeletal DisordersView all 26 articles
 HaiXin Yu1†
HaiXin Yu1† CaiYun Liu1†
CaiYun Liu1† Bo Chen1,2*
Bo Chen1,2* JingBo Zhai3
JingBo Zhai3 DongSheng Ba1
DongSheng Ba1 Zheng Zhu1
Zheng Zhu1 NingCen Li1
NingCen Li1 PeiYong Loh1
PeiYong Loh1 AoXiang Chen4
AoXiang Chen4 Bin Wang4
Bin Wang4 Yi Guo1,2*
Yi Guo1,2* YangYang Liu1,2
YangYang Liu1,2 ZeLin Chen1,2
ZeLin Chen1,2Objective: To evaluate the efficacy and safety of acupuncture in treating symptoms for Cancer-related Insomnia(CRI) patients.
Methods: Seven databases were searched from the time of database establishment to 31 March 2022. Randomized Controlled Trials (RCTs) on acupuncture intervention for CRI were collected. Literature screening and data extraction were performed independently by two researchers. Meta-analysis was performed using RevMan 5.4 software.
Results: A total of 13 articles with 1,109 participants were included. Five hundred and seventeen in the treatment group and 592 in the control group. Ten of the RCTs used the PSQI rating scale and four randomized controlled trials used the ISI rating scale, and the PSQI and ISI were analyzed together as continuous data. The results of the meta-analysis were: MD = −1.83, 95%CI = [−2.71, −0.94], P < 0.0001, indicating a significant improvement in PSQI scores in patients with CRI by acupuncture intervention; MD = 0.79, 95%CI = [−0.46, 2.03], P = 0.22. Acupuncture was not statistically significant on ISI scores for patients with CRI compared to controls, which does not yet indicate that acupuncture is effective for symptoms in patients with CRI. The results of the meta-analysis of the other 4 items using sleep disorder logs as efficacy analysis data were as follow, relative risk RR = 0.47, 95%CI = [0.33, 0.66], P < 0.0001. The difference was statistically significant, indicating that acupuncture can improve the symptoms of CRI patients compared to control group.
Conclusion: Acupuncture can improve the symptoms of patients with CRI to some extent, but due to the relatively small number and low quality of the included literature in this study, more high-quality clinical trials are needed as supplement the evidences in future.
Systematic review registration: https://www.crd.york.ac.uk/prospero/.
Cancer-related Insomnia (CRI) is also called tumor-related sleep disorder. It refers to the subjective experience of cancer patients who experience insufficient sleep time and sleep quality to meet normal physiological needs after the onset of cancer, thus affecting their daily life and health (Induru and Walsh, 2014; Zhuang and Fang, 2022). It is a more common clinical symptom, especially in patients with breast cancer, lung cancer and head and neck cancer (Induru and Walsh, 2014). Studies have shown that the incidence of CRI significantly exceeds that of the general insomnia population by a factor of two, accounting for 52.6–67.4% (Reilly et al., 2013), and the incidence of insomnia in cancer patients is 70.1% in China (Schieber et al., 2019). CRI is the second most urgent concomitant symptom of cancers after fatigue (Reilly et al., 2013). CRI affects the quality of life of most patients (Holtdirk et al., 2020) and prolonged insomnia can lead to greater physical and psychological damage, leading to many other serious problems, such as anxiety, depression and impairment of the body's immune function (Fleming et al., 2010; Yao and Tian, 2020), as well as other complications, such as obesity, hypertension, cardiovascular disease, etc. (Knutson et al., 2009). Most clinical studies have shown that most of the drugs are currently commonly used in clinical practice that approving by the Food and Drug Administration (FDA), such as benzodiazepines, anticonvulsants, antihistamines, and melatonin agonists (Asnis et al., 2015), and the treatment effect is often < 80% and many adverse effects (Asnis et al., 2015; Wilt et al., 2016; Lu and Guo, 2021), such as drug resistance, memory loss and dependence, etc. (Zhao, 2013). At the same time, not only does it take a long time to treat, but it also increases the financial burden on patients and their families, which affects the long-term survival of patients (Groenvold et al., 2007). Therefore, finding an effective and inexpensive alternative therapy has become an urgent task.
Acupuncture and moxibustion in traditional Chinese medicine has a long history, and its advantages of quit onset, simplicity and low side effects also have an irreplaceable role in modern treatment. As a non-pharmacological interventional technique, acupuncture has been shown to be beneficial for most patients from physical to psycho-spiritual aspects compared to other alternative therapies (Gould and MacPherson, 2001; Choi et al., 2017). Studies have shown that acupuncture can relieve pain, fatigue, hot flashes, anxiety and depression in cancer patients (Choi et al., 2012; Garcia et al., 2013; Posadzki et al., 2013). Therefore, acupuncture has gradually become one of the most popular treatment for patients (Gould and MacPherson, 2001). With the gradual increase of clinical studies using acupuncture for CRI in domestic and abroad, most of the meta-analysis were made for different therapies of acupuncture combined therapies of acupuncture and medicine or moxibustion (Chen, 2021; Yin et al., 2021; Wang et al., 2022; Zhuang and Fang, 2022). The results all showed that the combined therapy were more effective for CRI, but there were fewer studies on acupuncture alone, and no meta-analysis of acupuncture alone for CRI was found in recent years. Recently, some new randomized controlled trials were found to verify the efficacy of acupuncture for CRI (Lee et al., 2022) and meta-analysis was conducted for articles that met the study criteria to evaluate the efficacy and safety of acupuncture for CRI and to provide a medical reference for clinical treatment with acupuncture therapy.
Using computer to search Chinese databases: Chinese National Knowledge Infrastructure (CNKI), WANFANG, VIP. English databases: PubMed, Web of science, Cochrane, Embase. Studies published from the establishment of the databases to 31 March 2022 were searched. The retrieval strategy of “subject words+free words” was adopted, The search terms used are as follows: [“acupuncture” or “electroacupuncture” or “transcutaneous electrical acupoint stimulation (TEAS) ”or “auricular acupuncture” or “needle warming moxibustion”] and [“Cancer-related Insomnia” or “tumor” or “cancer” or “neoplasia” or “CRI”] and [“sleep” or “insomnia” or “sleep disorder”]. The rest of the database is retrieved according to different retrieval methods. The search strategy and search process are detailed in the Supplementary material. PROSPERO registration has been completed in March 2022 with the registration number CRD42022309870.
(1) Research type: Randomized Controlled Trial (RCT). (2) Participants: all adults cancer patients met the diagnostic criteria of insomnia in National Comprehensive Cancer Network and The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), regardless of cancer type, stage or disease duration. (3) Intervention: acupuncture, electroacupuncture, transcutaneous electrical acupoint stimulation, auricular acupuncture, needle warming moxibustion, while western medicine, routine care or sham acupuncture were used in the control group. (4) Outcome index: the curative effect of acupuncture on CRI was measured by any validated tool. The curative effect evaluation index includes one of the following, PSQI, ISI, sleep efficiency, sleep disorder log and subjective self-report sleep questionnaires.
(1) Articles on the combination of acupuncture and medicine or the combination of acupuncture and moxibustion with other therapeutic interventions. (2) Insomnia was not caused by tumor or cancer. (3) The outcome indicators did not meet the inclusion criteria, the data and information are incomplete. (4) Repeated articles. (5) Articles with Jadad scores below 3 scores.
Currently the most commonly outcome indicators are PSQI, ISI and sleep efficiency. PSQI can evaluate sleep quality, sleep dysfunction in clinical and non-clinical samples (Mollayeva et al., 2016). The secondary outcomes included ISI and effective rate. The ISI is used to assess the character and symptoms of the subject's sleep disorder. ISI has beneficial internal consistency, temporal stability and construct validity of instrument for diagnosing CRI patients (Savard et al., 2005). Effective rate included sleep disturbance after treatment, sleep information recorded with sleep diaries, or sleep quality assessed with other validated questionnaires. Security indicators include adverse events.
Two researchers (CaiYun Liu and DongSheng Ba) independently screened articles that met the inclusion criteria and extracted data, and summarized the authors, publication year, subjects (gender-age characteristics, tumor type, sample size), intervention mode, control mode, outcome index and adverse events into an excel table. If the two researchers disagree, they will be reviewed by a third researcher (HaiXin Yu).
The evaluation of the literature was performed using the risk of bias assessment tool in the RevMan 5.4 software provided by the Cochrane Collaboration Network, which focuses on the following components: (1) Random sequence generation; (2) Allocation concealment scheme; (3) Blinding of participants and personnel; (4) Blinding of outcome assessment; (5) Incomplete outcome data; (6) Selective outcome reporting; (7) Other bias (Higgins et al., 2011). The above seven biases were assessed, with red representing high risk, yellow representing unclear risk, and green representing low risk.
Meta-analysis was performed using RevMan 5.4 software, and Relative Risk (RR) was used for efficacy analysis results; Mean Difference (MD) was used for continuous analysis results, and 95% confidence intervals (CI) were given. The I2 statistic (0–100%) was used to assess the heterogeneity between the results of studies expressing different intervention modalities, and when the statistical heterogeneity between studies was small (P>0.1, I2 < 50%), it indicated that the results were not statistically significant and a fixed-effects model was used. When there was a large statistical heterogeneity between studies (P < 0.1, I2 ≥ 50%), it indicated that the results were statistically significant, and the source of heterogeneity was identified and subgroup analysis was performed. When statistical heterogeneity existed between subgroups without significant clinical heterogeneity, a random-effects model was used and the results were analyzed.
Through the retrieval of various databases, a total of 1,229 articles were identified from the preliminary searches, including 85 Chinese articles and 1,144 English articles. After eliminating duplicate articles (n = 303), remaining 926 articles, and after reading the titles and abstracts of the articles, the articles were excluded according to the requirements of the inclusion criteria (n = 897), 29 remaining articles were excluded after reading the full text (n = 16), and finally 13 RCTs were included, 3 in Chinese (Song et al., 2015; Peng et al., 2016; Shen et al., 2016) and 10 in English (Feng et al., 2011; Bokmand and Flyger, 2012; Frisk et al., 2012; Mao et al., 2014; Garland et al., 2017, 2019; Bao et al., 2021; Höxtermann et al., 2021; Zhang et al., 2021; Lee et al., 2022). The flow of trials outlined in Figure 1.
The basic information in the articles were collected after reading the full text and plotted in Table 1, which included the author, year of publication, tumor type, gender-age characteristics, sample size, intervention, control modality, outcome indicators and adverse events. As known from the table, a total of 1,109 subjects were included in the 13 RCTs, including 517 in the treatment group and 592 in the control group. The treatment group included 3 treatment: electroacupuncture (Frisk et al., 2012; Mao et al., 2014; Shen et al., 2016; Garland et al., 2017; Bao et al., 2021; Zhang et al., 2021; Lee et al., 2022) (n = 7), manual acupuncture (Feng et al., 2011; Bokmand and Flyger, 2012; Song et al., 2015; Peng et al., 2016; Garland et al., 2019) (n = 5) and auricular acupuncture (Höxtermann et al., 2021) (n = 1). Of the 13 included articles, 11 (Feng et al., 2011; Mao et al., 2014; Song et al., 2015; Peng et al., 2016; Shen et al., 2016; Garland et al., 2017, 2019; Bao et al., 2021; Höxtermann et al., 2021; Zhang et al., 2021; Lee et al., 2022) provided results for PSQI and ISI as continuous data measures, of which 7 (Feng et al., 2011; Mao et al., 2014; Song et al., 2015; Peng et al., 2016; Shen et al., 2016; Garland et al., 2017; Höxtermann et al., 2021) had PSQI as the primary outcome indicator and 3 (Garland et al., 2019; Zhang et al., 2021; Lee et al., 2022) had ISI as the primary outcome indicator; 3 (Garland et al., 2019; Zhang et al., 2021; Lee et al., 2022) had PSQI as the secondary outcome indicator and 1 paper (Bao et al., 2021) had ISI as the secondary outcome indicator. Another four (Bokmand and Flyger, 2012; Frisk et al., 2012; Song et al., 2015; Peng et al., 2016) provided results for efficacy analysis measures.
All included RCTs correctly used the randomization allocation method, with 9 items (Feng et al., 2011; Bokmand and Flyger, 2012; Mao et al., 2014; Song et al., 2015; Peng et al., 2016; Shen et al., 2016; Garland et al., 2017; Höxtermann et al., 2021; Zhang et al., 2021) using random number tables, 2 items (Frisk et al., 2012; Lee et al., 2022) using stratified randomization, and 2 items (Garland et al., 2019; Bao et al., 2021) using random squares. Seven items (Bokmand and Flyger, 2012; Mao et al., 2014; Garland et al., 2017, 2019; Höxtermann et al., 2021; Zhang et al., 2021; Lee et al., 2022) mentioned allocation concealment (six Bokmand and Flyger, 2012; Mao et al., 2014; Garland et al., 2017, 2019; Zhang et al., 2021; Lee et al., 2022 for opaque or closed envelope hiding and one Höxtermann et al., 2021 for central random hiding), and the rest were not mentioned. Three items (Bokmand and Flyger, 2012; Bao et al., 2021; Zhang et al., 2021) were blinded to subjects and researchers. Four items (Garland et al., 2019; Bao et al., 2021; Zhang et al., 2021; Lee et al., 2022) implemented blinding of outcome assessors. Five items (Frisk et al., 2012; Mao et al., 2014; Peng et al., 2016; Bao et al., 2021; Zhang et al., 2021) reported cases missing visits or active withdrawals, of which the number and reasons for missing visits or withdrawals were unbalanced, and the remaining eight (Feng et al., 2011; Bokmand and Flyger, 2012; Song et al., 2015; Shen et al., 2016; Garland et al., 2017, 2019; Höxtermann et al., 2021; Lee et al., 2022) had no personnel withdrawal. Selective reporting bias was low. For the presence of other biases, none of the 13 RCTs mentioned (Figure 2).
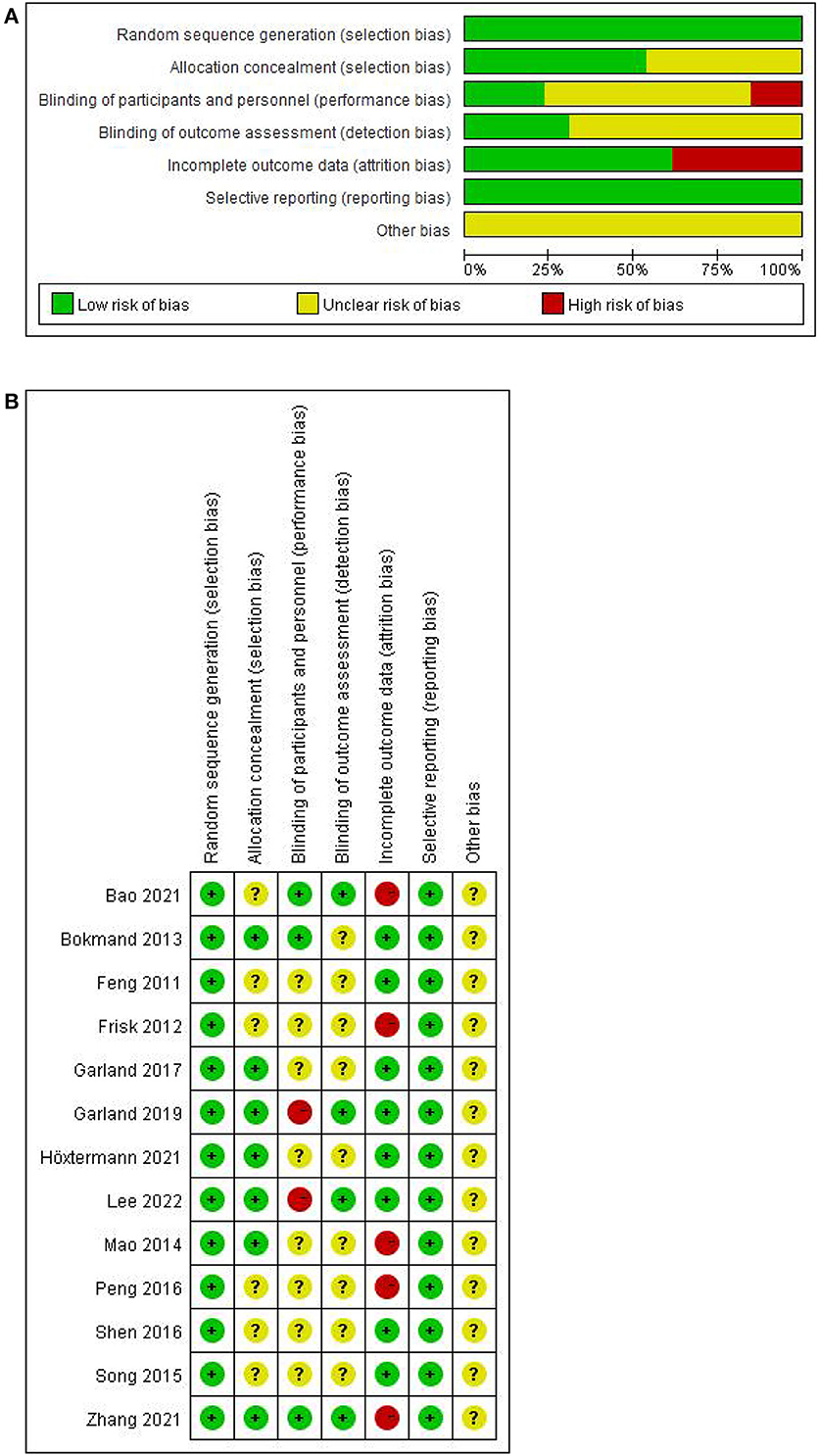
Figure 2. Risk of bias of included trials. (A) Assessment of risk of bias presented as percentages across all included studies. (B) Risk of bias summary for each included study.
PSQI: Ten of the included studies (Feng et al., 2011; Mao et al., 2014; Song et al., 2015; Peng et al., 2016; Shen et al., 2016; Garland et al., 2017, 2019; Höxtermann et al., 2021; Zhang et al., 2021; Lee et al., 2022) addressed changes in PSQI before and after treatment, with a total of 831 participants, of whom 416 were in the experimental group and 415 in the control group. The heterogeneity test was first performed with P = 0.001 and I2 = 67%, showing a large heterogeneity between studies, and a random effects model was adopted for meta-analysis. The results showed that the effect size MD = −1.83, 95% CI = [−2.71, −0.94], P < 0.0001. The difference was statistically significant, indicating acupuncture was effective in treating patients with CRI compared to the control group (Figure 3).
Subgroup analysis was performed according to the different intervention methods, and the results of the subgroup analysis showed that the heterogeneity among the three subgroups was P = 0.84, I2 = 0%, indicating that there was no heterogeneity among the subgroups, and the effect size after the three subgroups were combined was P = 0.001, I2 = 67%, indicating that there was heterogeneity. As we can see from the figure, the literature data on manual acupuncture for patients with CRI may be a source of heterogeneity, so a random effects model was used for analysis, MD = −1.83, 95%CI = [−2.71, −0.94], P < 0.0001. The difference is statistically significant, indicating that acupuncture treated CRI patients with better symptoms than the control group (Figure 4).
ISI: Four of the included studies (Garland et al., 2019; Bao et al., 2021; Zhang et al., 2021; Lee et al., 2022) addressed the changes in ISI before and after treatment in a total of 237 participants, of which 120 were in the experimental group and 117 in the control group. A heterogeneity test was first performed with P = 0.15, I2 = 44%, so a fixed-effects model was adopted for meta-analysis. The results showed that the effect size MD = 0.79, 95%CI = [−0.46, 2.03], P = 0.22. The ISI scores of patients with CRI in the treatment group intervention were not statistically significant compared to the control group (Figure 5).
Subgroup analysis was performed according to the different intervention methods and the results of the subgroup analysis showed that the heterogeneity between the two subgroups was P = 0.15, MD = 0.16, I2 = 44%, indicating that there was no heterogeneity between the two subgroups, and the effect size after the combination of the two subgroups was P = 0.07, I2 = 70.1%, indicating that there was heterogeneity. As can be seen from the figure, literature data on electroacupuncture for CRI patients may be a source of heterogeneity, so meta-analysis was performed using a random effects model, MD = 0.16, 95%CI = [−1.92, 2.23], P = 0.88 indicating that acupuncture improved ISI decline in CRI patients compared to controls without statistical significance (Figure 6).
Four of the included studies (Bokmand and Flyger, 2012; Frisk et al., 2012; Song et al., 2015; Peng et al., 2016) reported changes before and after sleep disorders in a total of 407 participants, including 203 in the experimental group and 204 in the control group. A heterogeneity test was first performed with P = 0.58, I2 = 0%, and a fixed-effect model was adopted for meta-analysis, which showed that acupuncture improved CRI patients better than controls in terms of sleep disturbances (RR = 0.47, 95%CI = [0.33, 0.66], P < 0.0001) (Figure 7).
The acupuncture treatment sessions varied among studies (Table 2). The most commonly used acupoints were: Baihui (GV20), Shenting (GV24), Neiguan (PC6), Sishencong ((EX-HN1), Yintang (EX-HN3), Zusanli (ST36), all of which were used at least three times, with a possible selection of 2-12 points in each study, and a minimum treatment duration of 1 week and a maximum of 10 weeks, ranging from 20 to 30 minutes. Another study chose auricular acupuncture (Höxtermann et al., 2021) with a duration of 33 days, shorter than manual acupuncture and electroacupuncture. The most common adverse effects of acupuncture in the included studies were pain, pruritus, bruising, and colds. Comparison the relatively low number of adverse events in the experimental group compared to the control group indicates that acupuncture has fewer side effects in the treatment of CRI and has advantages in terms of safety compared to other treatments (e.g., sham acupuncture and cognitive behavioral therapy).
Cancer-related insomnia should belong to the category of “insomnia” from the perspective of Traditional Chinese Medicine, and “insomnia” can be traced back to the “The Yellow Emperor's Canon of Internal Medicine”. CRI is due to the fact that after chemoradiotherapy drugs enter the human body, the struggle between anti-pathogenic qi and pathogenic factors, resulting in disharmony between yin and yang, which leads to insomnia. In addition, the tumor itself belongs to the deficiency of the essence and excess, mostly due to the intertwined phlegm and blood stasis, which affects the function of viscera, the phlegm mists the heart, and the blood stasis stagnates the qi movement (Lu and Guo, 2021). Acupuncture therapy has the effect of regulate and harmonize yin and yang, dredging the meridians, and exerting its effect through related acupoints. Modern research has shown that the pathogenesis of insomnia is complex and closely related to the central nervous system (Bonnet and Arand, 1997), and studies have shown that patients with insomnia often over-active the sympathetic nerves during sleep thus accelerating metabolism in the body (Liu et al., 2022), what's more, acupuncture can affect sleep by activating parasympathetic nerves and inhibiting sympathetic nerves (Li et al., 2003; Liu et al., 2022). In addition, acupuncture can regulate central neurotransmitters, immune cytokines (Li, 2021), a series of chemical factors (Wei et al., 2021) and antioxidant defense systems (Li, 2021) to promote the restoration of balance between yin and yang in the body and achieve improved sleep.
Meta-analysis of 11 RCTs studies of acupuncture for the treatment of symptoms in patients with CRI showed that acupuncture was effective in improving sleep disturbance and reducing PSQI scores, but it could not be stated whether it could reduce ISI scores, due to the small sample size included in this study and the low quality of the articles. In addition, the type of tumor included in the study was not homogeneous, which could have an impact on the results. The control group of RCTs selected for the studies had not only sham acupuncture, but also a variety of interventions such as western medicine and routine care, which may have caused some error in the results. In terms of outcome indicators, the use of sleep logs and questionnaires as evaluation indicators in some RCTs may also have some limitations on the final results. In addition, in terms of adverse events, seven of the included articles (Bokmand and Flyger, 2012; Mao et al., 2014; Garland et al., 2019; Bao et al., 2021; Höxtermann et al., 2021; Zhang et al., 2021; Lee et al., 2022) mentioned mild to moderate reactions with different symptoms, such as acupuncture pain, cough, skin allergy, bruising and so on. In the subgroup analysis results showed that acupuncture or electroacupuncture had more positive efficacy and higher safety compared to drugs such as eszopiclone and gabapentin for the treatment of CRI, while some articles were less good and there were no good solutions mentioned in the text for these adverse reactions, which is something we need to improve in the future when using acupuncture therapy. The study shows that the probability of selecting these acupoints Baihui, Shenting, Neiguan, Sishencong, Yintang, and Zusanli is high, which may indicate that these acupoints have some improvement effect on the treatment of CRI, but the specific acupuncture protocol is not clear, and further investigation on the selection of acupuncture points is needed in the future. Moreover, although acupuncture treatment has fewer side effects, there is no clear solution to these adverse effects, which is what we need to improve in the use of acupuncture in the future, such as pain, itching, bruising, colds, etc. We found the funnel plot was highly biased (Supplementary Figure S1), we think the main reasons are as follows: Firstly, interventions are complex; Secondly, different acupoints selection. Therefore, reducing bias greatly is also an area for us to improve in the future.
Limitations of the study: (1) The reason of large heterogeneity in meta-analysis may be due to the diversity of intervention methods, as well as differences in the types of drugs, doses, acupuncture times, and acupuncture point selection in the control group. (2) The different types of cancer in studies, included types of breast cancer, thyroid cancer, colon cancer, and lung cancer, may also lead to different analysis results. In order to obtain better efficacy of acupuncture for CRI, future clinical trials can be conducted on different acupuncture interventions, compatibility of acupuncture point selection, needle retention time, and different cancer types and periods of onset to determine the clinical benefits of acupuncture for this disease.
This study shows that acupuncture can improve the symptoms of CRI patients to some extent, sleep quality evaluated by PSQI improved, which is clinically useful and safe, and provides a basis for clinical treatment. Empirically, if combined with acupuncture and pharmacotherapy or alternative therapies, there may be a greater improvement in improving sleep quality. In terms of the safety of acupuncture efficacy, there is a need to further improve and ameliorate the adverse effects associated with acupuncture. However, because of the small amount and low quality of data included in this study, more large samples and high-quality clinical trials are needed to supplement the literature.
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary material.
Thesis guidance: BC, JZ, AC, BW, YG, YL, and ZC. Essay writing: HY, CL, and ZZ. Data analysis and collation: HY, CL, and DB. Illustration of the paper: HY and NL. Table design: HY and ZZ. Thesis translation: PL and HY. All authors contributed to the article and approved the submitted version.
This work was supported by the National Key R&D Program of China (2019YFC1712200-2019YFC1712204); Young Elite Scientists Sponsorship Program by CAST (2019-2021ZGZJXH-QNRC001) and the National Natural Science Foundation of China (NSFC) (82004467).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnins.2022.1026759/full#supplementary-material
Asnis, G. M., Thomas, M., and Henderson, M. A. (2015). Pharmacotherapy treatment options for insomnia: a primer for clinicians. Int. J. Mol. Sci. 17. doi: 10.3390/ijms17010050
Bao, T., Baser, R., Chen, C., Weitzman, M., Zhang, Y. L., Seluzicki, C., et al. (2021). Health-related quality of life in cancer survivors with chemotherapy-induced peripheral neuropathy: a randomized clinical trial. Oncologist 26, e2070–e2078. doi: 10.1002/onco.13933
Bokmand, S., and Flyger, H. (2012). Acupuncture relieves menopausal discomfort in breast cancer patients: a prospective, double blinded, randomized study. Breast 22, 320–323. doi: 10.1016/j.breast.2012.07.015
Bonnet, M. H., and Arand, D. L. (1997). Hyperarousal and insomnia. Sleep. Med. Rev. 1, 97–108. doi: 10.1016/S1087-0792 (97) 90012-5
Chen, S. Y. (2021). Analysis of the effect of acupuncture combined with auricular plaster on improving sleep of patients with advanced lung cancer. Smart Health. 7, 167–169. doi: 10.19335/j.cnki.2096-1219.2021.04.057
Choi, T. Y., Kim, J. I., Lim, H. J., and Lee, M. S. (2017). Acupuncture for managing cancer-related insomnia: a systematic review of randomized clinical trials. Integr. Cancer. Ther. 16, 135–146. doi: 10.1177/1534735416664172
Choi, T. Y., Lee, M. S., Kim, T. H., Zaslawski, C., and Ernst, E. (2012). Acupuncture for the treatment of cancer pain: a systematic review of randomised clinical trials. Support Care Cancer.20, 1147–1158. doi: 10.1007/s00520-012-1432-9
Feng, Y., Wang, X. Y., Li, S. D., Zhang, Y., Wang, H. M., Li, M., et al. (2011). Clinical research of acupuncture on malignant tumor patients for improving depression and sleep quality. J. Tradit. Chin. Med. 31, 199–202. doi: 10.1016/S0254-6272 (11) 60042-3
Fleming, L., Gillespie, S., and Espie, C. A. (2010). The development and impact of insomnia on cancer survivors: a qualitative analysis. Psychooncology 19, 991–996. doi: 10.1002/pon.1652
Frisk, J., Källström, A. C., Wall, N., Fredrikson, M., and Hammar, M. (2012). Acupuncture improves health-related quality-of-life (HRQoL) and sleep in women with breast cancer and hot flushes. Support Care Cancer 20, 715–24. doi: 10.1007/s00520-011-1134-8
Garcia, M. K., McQuade, J., Haddad, R., Patel, S., Lee, R., Yang, P., et al. (2013). Systematic review of acupuncture in cancer care: a synthesis of the evidence. J. Clin. Oncol. 31, 952–960. doi: 10.1200/JCO.2012.43.5818
Garland, S. N., Xie, S. X., DuHamel, K., Bao, T., Li, Q., Barg, F. K., et al. (2019). Acupuncture Versus Cognitive Behavioral Therapy for Insomnia in Cancer Survivors: A Randomized Clinical Trial. J. Natl. Cancer Inst. 111, 1323–1331. doi: 10.1093/jnci/djz050
Garland, S. N., Xie, S. X., Li, Q., Seluzicki, C., Basal, C., Mao, J. J., et al. (2017). Comparative effectiveness of electro-acupuncture versus gabapentin for sleep disturbances in breast cancer survivors with hot flashes: a randomized trial. Menopause 24, 517–523. doi: 10.1097/GME.0000000000000779
Gould, A., and MacPherson, H. (2001). Patient perspectives on outcomes after treatment with acupuncture. J. Altern. Complement. Med. 7, 261–268. doi: 10.1089/107555301300328133
Groenvold, M., Petersen, M. A., Idler, E., Bjorner, J. B., and Fayers, P. M. (2007). Psychological distress and fatigue predicted recurrence and survival in primary breast cancer patients. Breast. Cancer. Res. Treat. 105, 209–19. doi: 10.1007/s10549-006-9447-x
Higgins, J. P., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D., et al. (2011). Cochrane bias methods group and cochrane statistical methods group. The Cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ. 343, d5928. doi: 10.1136/bmj.d5928
Holtdirk, F., Mehnert, A., Weiss, M., Meyer, B., and Watzl, C. (2020). Protocol for the Optimune trial: a randomized controlled trial evaluating a novel Internet intervention for breast cancer survivors. Trials. 21, 117. doi: 10.1186/s13063-019-3987-y
Höxtermann, M. D., Buner, K., Haller, H., Kohl, W., Dobos, G., Reinisch, M., et al. (2021). Efficacy and safety of auricular acupuncture for the treatment of insomnia in breast cancer survivors: a randomized controlled trial. Cancers (Basel). 13, 2021. doi: 10.3390/cancers13164082
Induru, R. R., and Walsh, D. (2014). Cancer-related insomnia. Am. J. Hosp. Palliat. Care. 31, 777–785. doi: 10.1177/1049909113508302
Knutson, K. L., Van Cauter, E., Rathouz, P. J., Yan, L. L., Hulley, S. B., Liu, K., et al. (2009). Association between sleep and blood pressure in midlife: the CARDIA sleep study. Arch. Intern. Med. 169, 1055–1061. doi: 10.1001/archinternmed.2009.119
Lee, B., Kim, B. K., Kim, M., Kim, A. R., Park, H. J., Kwon, O. J., et al. (2022). Electroacupuncture for treating cancer-related insomnia: a multicenter, assessor-blinded, randomized controlled, pilot clinical trial. BMC. Complement. Med. Ther.22, 77. doi: 10.1186/s12906-022-03561-w
Li, X. M. (2021). Mechanism and clinical research progress of acupuncture and moxibustion in the treatment of insomnia. Inner. Mongolia Trad. Chin. Med. 40, 163–165. doi: 10.16040/j.cnki.cn15-1101.2021.05.093
Li, Z., Jiao, K., Chen, M., and Wang, C. (2003). Effect of magnitopuncture on sympathetic and parasympathetic nerve activities in healthy drivers–assessment by power spectrum analysis of heart rate variability. Eur. J. Appl. Physiol. 88, 404–410. doi: 10.1007/s00421-002-0747-5
Liu, S. R., Yu, B. X., Liu, L. S., and Ni, H. R. (2022). Discussion on the mechanism of acupuncture and moxibustion in treating insomnia. J. Liaoning Univ. Trad. Chin. Med. 24, 194–200.
Lu, Y. Y., and Guo, Y. (2021). Research progress in traditional Chinese medicine treatment of tumor related insomnia. Famous Doctor. 3, 102–104. doi: 10.13194/j.issn.1673-842x.2022.06.041
Mao, J. J., Farrar, J. T., Bruner, D., Zee, J., Bowman, M., Seluzicki, C., et al. (2014). Electroacupuncture for fatigue, sleep, and psychological distress in breast cancer patients with aromatase inhibitor-related arthralgia: a randomized trial. Cancer. 120, 3744–51. doi: 10.1002/cncr.28917
Mollayeva, T., Thurairajah, P., Burton, K., Mollayeva, S., Shapiro, C. M., Colantonio, A., et al. (2016). The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: a systematic review and meta-analysis. Sleep. Med. Rev. 25, 52–73. doi: 10.1016/j.smrv.2015.01.009
Peng, X. H., Zhang, J. L., Song, J. R., Liu, D. Y., Zhao, Y. L., Dan, Z. J., et al. (2016). Observation on the clinical effect of acupuncture and moxibustion on insomnia in tumor patients. Chin. J. Trad. Chin. Med. 31, 2409–2411.
Posadzki, P., Moon, T. W., Choi, T. Y., Park, T. Y., Lee, M. S., Ernst, E., et al. (2013). Acupuncture for cancer-related fatigue: a systematic review of randomized clinical trials. Support Care Cancer21, 2067–2073. doi: 10.1007/s00520-013-1765-z
Reilly, C. M., Bruner, D. W., Mitchell, S. A., Minasian, L. M., Basch, E., Dueck, A. C., et al. (2013). A literature synthesis of symptom prevalence and severity in persons receiving active cancer treatment. Support Care Cancer. 21, 1525–1550. doi: 10.1007/s00520-012-1688-0
Savard, M. H., Savard, J., Simard, S., and Ivers, H. (2005). Empirical validation of the Insomnia Severity Index in cancer patients. Psychooncology 14, 429–441. doi: 10.1002/pon.860
Schieber, K., Niecke, A., Geiser, F., Erim, Y., Bergelt, C., Büttner-Teleaga, A., et al. (2019). The course of cancer-related insomnia: don't expect it to disappear after cancer treatment. Sleep Med. 58, 107–113. doi: 10.1016/j.sleep.2019.02.018
Shen, L. F., Chen, W. Y., Lv, X. D., Liu, J. L., Yang, X. M., Yao, M., et al. (2016). Effect of Electroacupuncture on improving sleep quality in patients with lung cancer pain. J. Med. Res. 45, 87–90. doi: 10.2016./j.issn.1673-548X.06.022
Song, J. R., Zhao, Y. L., Peng, X. H., and Hu, Y. P. (2015). A randomized controlled clinical study of acupuncture and moxibustion in the treatment of insomnia in cancer patients. Sichuan Trad. Chin. Med. 33, 163–165.
Wang, C. C., Han, E. Y., Jenkins, M., Hong, X., Pang, S., Whitehead, L., et al. (2022). The safety and efficacy of using moxibustion and or acupuncture for cancer-related insomnia: a systematic review and meta-analysis of randomised controlled trials. Palliat. Care. Soc. Pract. 16, 26323524211070569. doi: 10.1177/26323524211070569
Wei, X. K., Wang, H. F., and Wang, Z. H. (2021). Research Progress on the mechanism of acupuncture and moxibustion in treating insomnia. Liaoning J. Trad. Chin. Med. 48, 218–220. doi: 10.13192/j.issn.1000-1719.2021.04.059
Wilt, T. J., MacDonald, R., Brasure, M., Olson, C. M., Carlyle, M., Fuchs, E., et al. (2016). Pharmacologic Treatment of Insomnia Disorder: An Evidence Report for a Clinical Practice Guideline by the American College of Physicians. Ann. Intern. Med.165, 103–112. doi: 10.7326/M15-1781
Yao, J. L., and Tian, J. H. (2020). On the treatment of tumor related insomnia with the combination of form and spirit. Shanxi Trad. Chin. Med. 41, 213–216. doi: 10.3969/j.issn.1000-7369.2020.02.020
Yin, S., Wang, Y., Chen, J. X., Xie, A. W., and Liu, S. (2021). Observation on the efficacy of acupuncture combined with medicine in the treatment of sleep disorders after palliative chemotherapy f or advanced malignant tumors. Shanghai J. Acup. Moxibust. 40, 21–25. doi: 10.13460/j.issn.1005-0957.2020.01.0021
Zhang, J., Qin, Z., So, T. H., Chen, H., Lam, W. L., Yam, L. L., et al. (2021). Electroacupuncture plus auricular acupressure for chemotherapy-associated insomnia in breast cancer patients: a pilot randomized controlled trial. Integr. Cancer. Ther. 20, 15347354211019103. doi: 10.1177/15347354211019103
Zhao, K. (2013). Acupuncture for the treatment of insomnia. Int. Rev. Neurobiol.111, 217–234. doi: 10.1016/B978-0-12-411545-3.00011-0
Keywords: acupuncture, cancer-related insomnia, systematic review, meta-analysis, PSQI, efficacy
Citation: Yu H, Liu C, Chen B, Zhai J, Ba D, Zhu Z, Li N, Loh P, Chen A, Wang B, Guo Y, Liu Y and Chen Z (2022) The clinical efficacy and safety of acupuncture intervention on cancer-related insomnia: A systematic review and meta-analysis. Front. Neurosci. 16:1026759. doi: 10.3389/fnins.2022.1026759
Received: 24 August 2022; Accepted: 09 November 2022;
Published: 15 December 2022.
Edited by:
Yan-Qing Wang, Fudan University, ChinaReviewed by:
Polina Pchelina, I. M. Sechenov First Moscow State Medical University, RussiaCopyright © 2022 Yu, Liu, Chen, Zhai, Ba, Zhu, Li, Loh, Chen, Wang, Guo, Liu and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bo Chen, dGp1dGNtY2hlbmJvQDE2My5jb20=; Yi Guo, Z3VveWlfMTY4QDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.