- Graduate School, Chengdu University of Traditional Chinese Medicine, Chengdu, China
Despite the widespread clinical use of acupuncture in the treatment of pruritus caused by psoriasis, urticaria, uremic, and other diseases, insights into the mechanism of action of acupuncture are still emerging. For the above reasons, a beneficial effect of acupuncture on pruritus was not recommended or reported in recent clinical practice guidelines. Acupuncture is a kind of physical stimulation, which has the characteristics of multi-channel and multi-target effects. The biomechanical stimulation signal of acupuncture needling can be transformed into bioelectric and chemical signals; interfere with kinds of cells and nerve fibers in the skin and muscle; alter signaling pathways and transcriptional activity of cells, mediators, and receptors; and result in inhibition of peripheral and central transmission of pruritus. Available mechanistic data give insights into the biological regulation potency of acupuncture for pruritus and provide a basis for more in-depth and comprehensive mechanism research.
Introduction
Pruritus is a sensation that provokes the desire to scratch (2019European S2k Guideline), which remains one of the most agonizing symptoms for affected patients and a clinical challenge for physicians (Weisshaar et al., 2019). Pruritus may be a result of dermatological diseases or systemic diseases (Satoh et al., 2021). The onset of pruritus with underlying dermatological disease usually coincides with the onset of typical skin lesions (Ständer et al., 2015). Pruritus caused by underlying systemic disorder, such as end-stage renal disease, hemodialysis, or primary biliary cirrhosis, is usually persistent or paroxysmal, and the peak itch sensation mainly occurs at night or in the evening (Millington et al., 2018; Satoh et al., 2021). Region, ethnicity, age, underlying diseases, methods of investigation, and access to the regional healthcare system influence the occurrence of pruritus (Weisshaar and Dalgar, 2009), which may explain the reason for the inconsistency of data reported by various countries or regions (Weisshaar et al., 2006; Weisshaar, 2016). A recent European multi-center study found that the incidence of itching in dermatological diseases was 54.5%, while the incidence in healthy people was 8% (Schut et al., 2019). In China, an epidemiological survey showed that 47.8% of patients with dermatological diseases were accompanied by itching symptoms (Zhang, 2014).
In the clinical practice, although the newly developed drugs for various causes have made great progress, it is also difficult to control the clinical symptoms of itching because the underlying biologic mechanism are not confirmed until now. Antihistamines are the most widely used systemic antipruritic drugs in dermatological diseases. They achieve the purpose of antipruritic by selectively blocking histamine H1 receptors and antagonizing the effects of histamine (Leslie et al., 2015; Thurmond et al., 2015). Long-term use of antihistamines not only cannot fundamentally solve the chronic pruritus (CP) in older Asian adults, but also increases their risk of falling (Moosa et al., 2021). Antihistamines are widely used for the treatment of CP associated with various systemic diseases. However, conventional doses of antihistamines in the treatment of pruritus in internal diseases have not proven to be effective (O’Donoghue and Tharp, 2005). About 30–90% of patients suffering from CP with cholestasis are unresponsive to antihistamines (Langedijk et al., 2021). Regarding non-histaminergic drugs, there are different characteristics in different drugs treating different diseases. Systemic glucocorticoids (GCs) are commonly used as a short-term treatment in severe CP associated with dermatological disease or systemic disease due to its serious side effects (Weisshaar et al., 2019). Cholestyramine, the first-line guideline-recommended treatment for cholestatic pruritus (Hirschfield et al., 2017), has a poor clinical effect on patients with excessive pruritus intensity (Düll and Kremer, 2020). Antidepressants are effective particularly in refractory CP, especially in malignant, cholestatic, and chronic kidney disease. However, side effects of antidepressants are common and include drowsiness, fatigue, and headache (Kouwenhoven et al., 2017).
Chronic pruritus has considerable, severe, and detrimental implications on the quality of life because it is difficult to heal (Whang et al., 2021a,b). Several studies by Gil, Yosipovitch and his colleagues found that pruritus seriously plays a great impact on people’s quality of life, including emotions, attention, eating habits, sexual function, and sleep (Yosipovitch et al., 2001, 2010, 2015). The longer the duration and severity of itching, the greater its substantially negative impact on work productivity and day-to-day activities (Chrostowska-Plak et al., 2012; Yano et al., 2013; Carr et al., 2014). Some patients with CP will lead to psychosocial comorbidities, including anxiety, depression, and even suicidal tendencies (Yosipovitch and Bernhard, 2013; Reszke and Szepietowski, 2018; Brenaut et al., 2019; Whang et al., 2020; Hawro et al., 2021; Umehara et al., 2021).
Acupuncture
The Clinical Effect of Acupuncture
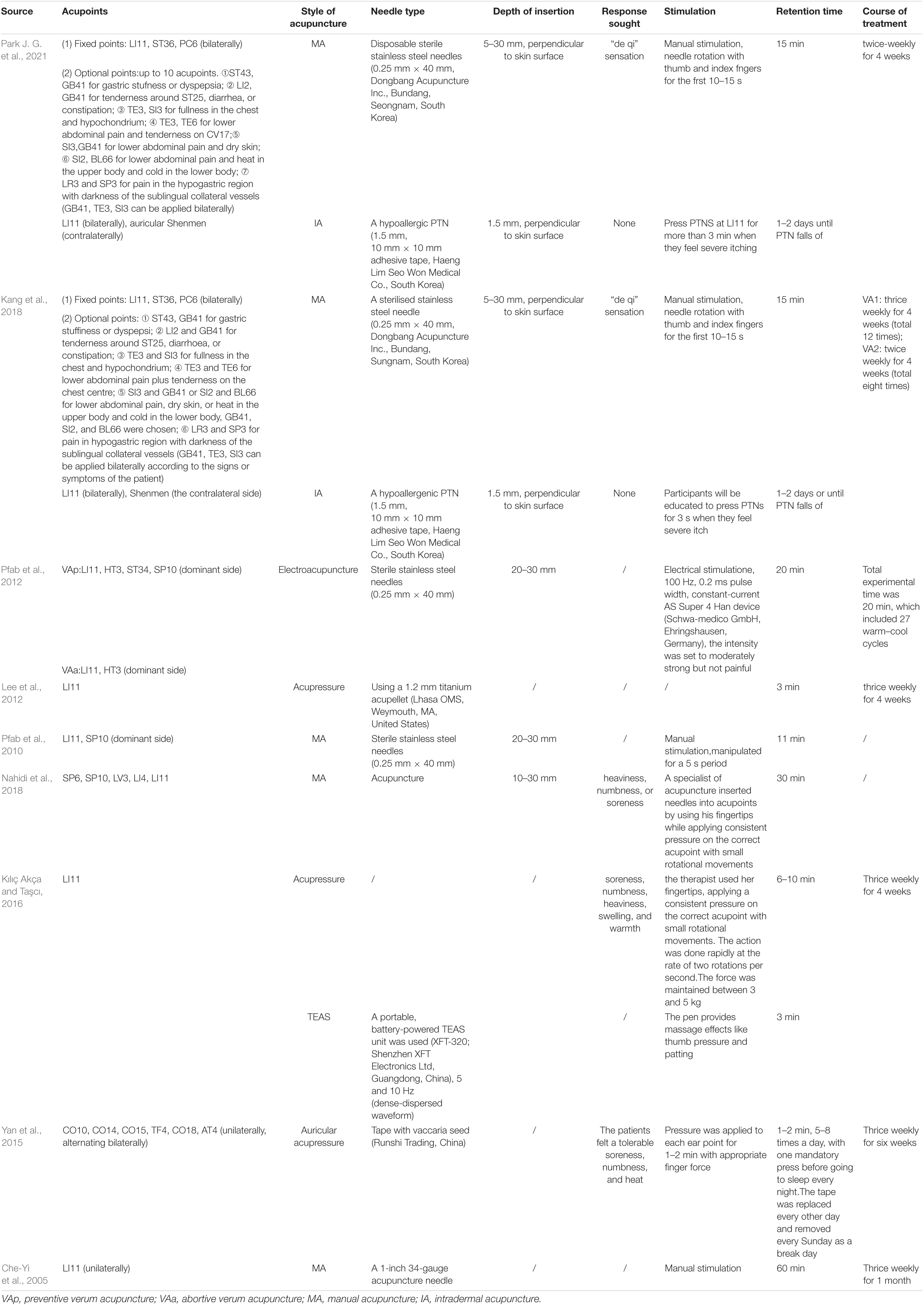
As an important enabling part of Chinese medicine, acupuncture has been used in China for more than 2,500 years in the treatment of itch (van den Berg-Wolf and Burgoon, 2017). Acupuncture is a safe and effective therapy in the treatment of pruritus (Yao et al., 2016). Compared with sham acupuncture, verum acupuncture can significantly reduce the total SCORing Atopic Dermatitis index (SCORAD) (Kang et al., 2018; Park J. G. et al., 2021) and the visual analogue scale (VAS) for itching in patients with atopic dermatitis (Pfab et al., 2012), atopic eczema (Pfab et al., 2010), and hemodialysis (Nahidi et al., 2018). There are three RCTs on uremic pruritus that indicated that acupuncture (Che-Yi et al., 2005), acupressure or transcutaneous electrical acupoint stimulation (TEAS), and auricular acupressure can reduce the VAS for itching in patients with uremic pruritus (Yan et al., 2015; Kılıç Akça and Taşcı, 2016). Che-Yi et al. (2005) have found a significant reduction in pruritus scores of hemodialysis patients with refractory uremic pruritus during the 3-month follow-up after acupuncture. Coincidentally, the relief of pruritus after 4 weeks of acupuncture treatment of patients with mild to moderate atopic dermatitis has been observed (Park J. G. et al., 2021). According to Tables 1, 2, the most commonly used style of acupuncture was manual acupuncture, followed by intradermal acupuncture and acupressure. Electroacupuncture (EA), TEAS, and auricular acupuncture were only used in one study. Antipruritic points included Quchi (LI11), Zusanli (ST36), Xuehai (SP10), and Shaohai (HT3). There are eight RCTs studies that have used Quchi point, which has the functions of dispelling wind to releasing exterior, clearing heat and relieving itching.
However, the underlying mechanism of these consequences remain largely unknown. An important question is that whether these observed effects share a common mode of action or result from a variety of distinct processes. This review summarizes the physiological basis of acupuncture treatment of pruritus, explores the peripheral and central mechanisms of acupuncture to relieve itching, and proposes existing challenges and future research directions.
Physiological Basis of Acupuncture Relieving Itch
Through opography of the cadavers, it was found that most of the acupoints on the meridians are dominated by peripheral nerves (Wick et al., 2007). Acupuncture points in humans may be excitatory muscle/skin–nerve complexes with high-density nerve endings (Li et al., 2004). The acupoint tissues are rich in various forms of receptors, such as free nerve endings and cyst receptors in the dermis, muscle spindles in muscle tissue, and Rufini bodies near the joint capsule. According to the relationship between meridian acupoints and nerves, the commonly used antipruritic acupoints Quchi, Zusanli, Hegu, etc. (Zhang et al., 2019) are located at the muscle movement points, and the nerve endings on the body surface are particularly dense (Guo, 2016). Because of the appropriate stimulation produced by various forms of acupuncture techniques such as hand acupuncture, electroacupuncture, and transcutaneous electrical stimulation, acting on receptor cells, the external stimulation is transformed into transmembrane electrical signals through channel proteins or membrane-specific receptors with specific sensory structures. For chemically sensitive receptors, the transduction process is related to the release of chemical substances. Chemical substances activate different receptors through direct and indirect effects, depolarizing the receptors to produce afferent impulses. The sensory terminals of itch neurons terminate in the epidermis and form branched free nerve terminals, which contain numerous membrane receptors for various mediators (Zylka et al., 2005; Imamachi et al., 2009; Han et al., 2013).
Mechanism of Acupuncture for Acute Itch
Acute itch is defined as the duration of pruritus ≤6 weeks according to a recommendation by the International Forum for the Study of Itch (IFSI). The acute attack of pruritus is a reaction that eliminates the harmful environment of our body, which plays a positive protective effect role in our survival (Wang et al., 2021). As claimed by currently known studies, after allergens, external irritants, or pruritogens interface with the skin, the keratinocytes and local immune cells recruit and release a great deal of chemical mediators (Pasparakis et al., 2014). Mast cells activate and release the elements of cytoplasmic granules. These mediators bind to the membrane receptors of homologous mediators in the itch-sensitive neuron endings (histaminergic neurons and non-histaminergic neurons) (Ikoma et al., 2006) located in the epidermis. Then, the itching signal is generated (Dong and Dong, 2018). The itching signal is transmitted to the dorsal root ganglion (DRG) at the dorsal horn of the spinal cord through the unmyelinated fiber C and a small portion of Aδ nerve fibers for preliminary processing. After that, the processed itching signal is transmitted to multiple brain areas and circuits through the spinothalamic tract for processing (Bourane et al., 2015; Cevikbas and Lerner, 2020). These distinct brain areas are thought to be involved in different aspects of itch signal processing (Chen and Sun, 2020). The primary and secondary somatosensory cortices contribute to the localization, intensity rating, and recognition of and attention to itch (Yosipovitch and Mochizuki, 2015). The midcingulate cortex is activated during itch induction or itch-related behaviors, for it is closely related to the premotor planning and process of affective-motivational in itch (Schneider et al., 2008). The putamen is significantly activated during scratching of itch. The reason is that it is a critical component of the striato-thalamo-cortical circuity related to motivational processing, habitual behavior, and action initiation, which is the basis of scratching (Graybiel, 2008).
An important peripheral target of acupuncture in relieving acute pruritus is 5-HT and receptor, which is an important histamine-independent pruritus mediator (Hachisuka et al., 2010; Bautista et al., 2014). 5-HT can directly activate the 5-HT receptors of sensory neurons (Han and Dong, 2014). After depolarization of the 5-HT receptor, transient voltage receptor cation channel (TRP) family ion channels are activated, resulting in phosphorylation of extracellular regulated protein kinases (ERK). The skin sensory nerve fibers are excited and then itching signal is reduced (Yamaguchi et al., 1999; Zhao et al., 2014). At present, several animal models of acute itch treated by acupuncture have been studied. Electroacupuncture can effectively inhibit the degranulation of mast cells in mice with acute itching induced by compound 48/80 (Wang and Xu, 2014). Zhao et al. (2018) found that acupuncture can reduce the serum content of 5-HT in the mice with histamine-induced acute itching. Park H. J. et al. (2021) found that acupuncture can blockade the expression of 5-HT2 and 5-HT7 receptors in the skin of mice with serotonergic itch. Shao and Chen (2012) found that acupuncture can reduce the serum content of IgE and the concentration of 5-HT2A receptors in the skin of 5-HT-induced itching in rats. The 5-HT neurons in the central nervous system, involved in regulating the itch signal induced by various factors, play an important part of the itch signal transduction pathway (Akiyama et al., 2009, 2017). Related research found that mice lacking 5-HT or serotonergic neurons in the brainstem exhibit remarkably reduced scratching behavior (Zhao et al., 2014). In an animal model, acupuncture downregulated 5-HT neurons in the medulla oblongata, reducing excitability of nerve cells and inhibiting pruritus (Yan, 2017; Zhao et al., 2017). In humans, a recent fMRI result of experimental pruritus induced by histamine showed that the positive functional connectivity of putamen and the pMCC was associated with the antipruritic effects of acupuncture (Min et al., 2019).
Mechanism of Acupuncture for Chronic Itch
Chronic itch is defined as pruritus lasting six or more weeks according to a recommendation by the International Forum for the Study of Itch (IFSI) (Ständer et al., 2007; Zhang et al., 2019). In heterogeneous forms of pruritus with dermatological disease accompanied by inflammation of the skin, persistent and continuous immune activation provoke a radical augmentation of histamine and mediators in the affected skin area, resulting in thickening and morphological changes of the epidermis, infiltration of a large number of immune cells, and chronic itching (Dong and Dong, 2018).
Closely related to the mechanism of acupuncture treatment of CP in the periphery is the cytokines released by immune cells, such as interleukin-4 (IL-4), interleukin-2 (IL-2), and interleukin-2 (IL-10). Increased IL-4 signaling was closely related to the development of pruritus with atopic dermatitis (Chan et al., 2001; Bogaczewicz et al., 2016). IL-4 directly promotes itch through the IL-4 receptor on itch-sensing neurons (Chiu et al., 2014; Usoskin et al., 2015). The activation of IL-4 receptor signal elevates the neuronal Ca2+ through the Janus kinase (JAK) pathway as well as both the transient receptor potential vanilloid V1 (TRPV1) and transient receptor potential ankyrin A1 (TRPA1) ion channels, resulting in activating the peripheral sensory nerve fibers and inducing chronic itch (Oetjen et al., 2017; Yosipovitch et al., 2018). By the regulation of cytokines, electroacupuncture reduces the generation of itching signals directly and inhibits the inflammatory response of the skin in the pruritus underlying dermatological disease. In humans, recent research results suggested that electroacupuncture reduced the level of IL-4 and IL-2 in the blood of patients with atopic dermatitis and increased the level of interferon γ (IFN-γ) (Deng, 2018). In patients with CP, electroacupuncture intensified the level of anti-inflammatory cytokine IL-10 in the serum and inhibited the content of inflammatory cytokine TNF-α, bringing about the reduction of inflammatory in the skin (Ni, 2017; Huang et al., 2020). However, serum IL-6 and interferon inducible protein (IP-10) may not be concerned with the antipruritic effect of acupuncture (Wang, 2018). In animals, a study found that electroacupuncture promoted the secretion of IFN-γ in the serum of mice with atopic dermatitis, while there was no sensible change about IL-4 (Jiang et al., 2016a).
Increasing evidence about central mechanism of CP suggested that microglial activity played a momentous role in the pathogenesis of CP evoked by 2,4-dinitrofluorobenzene (DNFB), compound 48/80, and 5′-guanidinonaltrindole (GNTI) (Liu et al., 2015; Ying et al., 2015; Zhang et al., 2015; Xu et al., 2020). Microglia exacerbate itch sensation by facilitating the phosphor-38 (p38) mitogen-activated protein kinase (MAPK) signaling pathway through chemokine CX3C receptor1 (CX3CR1) (Zhang et al., 2015). In addition, the suppression of the microglial-specific protein ionized calcium-binding adapter molecule 1 (lba1) in the spinal cord not only reduced the number of scratches in mice with atopic dermatitis, but repaired the afflicted skin area and improved inflammation of the skin (Torigoe et al., 2016). In Western blot analysis, electroacupuncture repressed the lba1 and phospho-p38 expression increased by s.c. injection of GNTI to the back of the neck in the spinal cord (Lin et al., 2016). A recent study showed a similar result in that manual acupuncture reduces cholestatic pruritus by alleviating spinal microglial activation (Lee et al., 2018).
Moreover, acupuncture in conjunction with the participation of multiple brain regions is one of the central mechanisms to antipruritics. In humans, the fMRI data outcome of patients with AD (Vitaly et al., 2014) showed that the activation of the right anterior insula, nucleus patella, putamen, globus pallidus, caudate nucleus, and nucleus accumbens was inhibited by electroacupuncture during the aggravation of itching. The activation of bilateral primary and right secondary somatosensory/motor cortex, middle frontal gyrus, cuneiform lobe, and left posterior cingulate cortex areas was reduced during the peak period of itching. The reduction of the intensity of itching was consistent with the inhibition of brain activation. Among these brain areas, they found that the reduction in putamen was closely correlated with the itch reduction following acupuncture.
Mechanism of Acupuncture for Itch and Pain
Itch and pain are two different unpleasant somatic sensations with different behavioral manifestations. Pain causes the action of shrinking to avoid harmful stimuli, while itch causes the action of scratching to remove harmful substances invading the skin (McMahon and Koltzenburg, 1992). However, the sensations of itch and pain are also regarded as closely related. Itch can be suppressed by scratching and painful stimuli, whereas suppressed pain can elicit itch (Miyamoto and Patapoutian, 2011). One noteworthy reason for this appearance is that there is a broad crosstalk between pain- and itch-related mediators and/or receptors in the periphery and center, such as opioids and cannabinoids (Ikoma et al., 2006).
There are three opioid peptides, namely, β-endorphin (β-EP), enkephalin, and dynorphin (DYN), that are widely distributed in the periphery and the center. They modulate pain and itch by activating their respective opioid receptors. μ-Opioid system is itch-inducible, whereas the κ-opioid system is itch-suppressive (Kenya et al., 2017; Oeda et al., 2018). β-EP act as the agonist of μ opioid receptors to activate cognate morphine receptor-1D (MOR1D), which heterodimerizes with gastrin-releasing peptide receptor (GRPR, the itch-specific neurons) in the spinal cord to relay itch information (Liu et al., 2011). DYN, an endogenous κ-receptor agonist, is known to activate κ-opioid receptors (KORs) on GRPR-positive neurons and inhibit these neurons, resulting in attenuation of chemical itch (Mishra and Hoon, 2013; Yosipovitch et al., 2018; Chen et al., 2020). Moreover, DYN released by BhIhb5-1 neurons in the spinal dorsal horn is a neuromodulator to inhibit itch (Kardon et al., 2014).
An important target for acupuncture treatment of CP is β-EP, DYN, and μ and κ receptor systems. A paradoxical result was noteworthy in that acupuncture reduced the β-EP in the plasma of mice with CP, while it increased the expression of β-EP in the medulla oblongata (Yan, 2017). In the analgesic mechanism, β-EP plays a pivotal role in the central nervous system (Zhao, 2008). Therefore, it is inferred that when acupuncture stimulates mice with CP, the pain of acupuncture itself is also prominent, resulting in irritable upregulation of β-EP in central antinociception for analgesia. In addition, it had been found that electroacupuncture relieved pruritus in mice with atopic dermatitis via enhancing the synthesis and release of DYN at the spinal cord pruritus in rats to activate a large number of κ-receptors (Jung et al., 2014; Jiang et al., 2016b). Interestingly, different frequencies of electroacupuncture stimulated different opioid receptors. High frequency electroacupuncture (120 Hz) achieved the purpose of antipruritics by activating κ receptors. Nor-BNI-hydrochloride (k receptor antagonist) can effectively inhibit the antipruritic effect of 120-Hz electroacupuncture (Han et al., 2008). A stimulating finding showed that naloxone (the peripherally acting μ opioid receptor antagonist) partially reversed the antipruritic effect of low-frequency electroacupuncture (2 Hz), while the Nor-BNI-hydrochloride did not eliminate the antipruritic effect in mice with GNTI-induced pruritus (Chen et al., 2013).
Endogenous cannabinoids regulate pain and itch through specific membrane receptors, the cannabinoid receptors (Di Marzo and Petrocellis, 2006). It may be related to the physical increase of cannabinergic neurotransmitters after the activation of cannabinoid receptor 1 (CB1), which increases the pruritus threshold (Gingold and Bergasa, 2003). In animal models of chronic dry skin pruritus (Li, 2019), the expression of the CB1 in the midbrain tissue of mice was increased. Electroacupuncture reduced the scratching behavior through significantly downregulating the expression level of the cannabinoid receptor CB1. Intraperitoneal injection of CB1 receptor antagonist significantly reversed the effect of electroacupuncture. Li believed that the reason was that the antagonist antagonizes the CB1 receptors on both gamma aminobutyric acid (GABA) neurons and glutamatergic neurons, which may result in the domination of glutamatergic neurons to promote 5-HT release. Therefore, he implied that electroacupuncture participated in the central mechanism of acupuncture to relieve pruritus by regulating the CB1 receptor to inhibit the release of 5-HT. On the contrary, it has been suggested that antipruritic effects of cannabinoids are independent of descending inhibitory serotonergic pathways (Todurga et al., 2016).
Challenges and Future Directions
The development of acupuncture represents a prime example of non-pharmacologic treatment. The currently available acupuncture therapy has shown high response rates and long-term remissions in patients with acute or chronic itch with minimal side effect. In this review, the authors provide an overview of the effect in acupuncture recipients and of the method and acupoint in acupuncture management (Figure 1). Furthermore, relieving itching of acute and chronic mechanisms by acupuncture is discussed.

Figure 1. The neurobiological mechanism of acupuncture to relieve itching. The biomechanical stimulation signal of acupuncture can inhibit pruritus via acting on different levels of targets. In the periphery, manual acupuncture downregulates 5-HT (acute pruritus) and blocks its receptor expression. Electroacupuncture regulates cytokines and endocannabinoid receptor CB1 (chronic itch), and opioid peptide receptor is also one of the targets involved in acupuncture to relieve itching. In the center, acupuncture can regulate microglia and DNY in the spinal cord to treat chronic pruritus in animals. 5-HT neurons and β-EP in the medulla oblongata, and CB1 in the midbrain are also its targets. Putamen is a common target of acupuncture treatment for acute and chronic pruritus in humans. As shown in the figure, the red arrow represents the downregulation effect of acupuncture, while the blue arrow represents the upregulation effect of acupuncture. Among them, the purple font represents targets in humans, the yellow font represents both targets in humans and animals, and the rest represent animal research. The gray ellipses represent targets related to acute itch, the green ellipses represent targets related to chronic itch, and the others are both. SII, secondary somatosensory cortex; SI, primary somatosensory cortex; PF, prefrontal area.
The neurobiological mechanism of acupuncture to antipruritics that has made some progress is less in-depth, compared with the already clear mechanism of pruritus. There is a phenomenon of circadian variation of pruritus, and pruritus is usually much severe at night (Millington et al., 2018; Weisshaar et al., 2019). There are many research evidence on the adjustment effect of acupuncture on the circadian rhythm (Kim et al., 2012). For instance, electroacupuncture at different hours produced different effects on leucine-enkephalin contents in rat medulla oblongata regions (Wang and Wang, 1989). It is worthy to explore the mechanism in this area. Chronic pruritus is also often associated with psychopathology, such as anxiety and depression (Gupta and Gupta, 1999). Acupuncture may improve itching by treating related mental illnesses. Unfortunately, research has not yet been conducted.
In conclusion, further application of acupuncture therapy for pruritus will require a better understanding of the peripheral and central, molecular, and cellular mechanisms. Using in vivo calcium imaging, modern genetics, and imaging tools and other technologies, we can expand our understanding of the related circuits in the spinal cord and brain for acupuncture to relieve itching. In addition, cytokines, endocannabinoids and the CB1 receptor, and opioids and their receptors are important targets of acupuncture antipruritic mechanisms worth paying attention to.
Author Contributions
YT and SC performed document retrieval and manuscript writing. XW designed the protocols. JW and YJ performed the literature screening. JW contributed to making Tables 1, 2. QL, HY, and SX performed the data extraction and data analysis. YY and QY performed charts. QY has contributed to the data and make of figure for the work. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Akiyama, T., Merrill, A. W., Carstens, M. I., and Carstens, E. (2009). Activation of superficial dorsal horn neurons in the mouse by a PAR-2 agonist and 5-HT: potential role in itch. J. Neurosci. 29, 6691–6699. doi: 10.1523/jneurosci.6103-08.2009
Akiyama, T., Nagamine, M., Davoodi, A., Ivanov, M., Carstens, M. I., and Carstens, E. (2017). Innocuous warming enhances peripheral serotonergic itch signaling and evokes enhanced responses in serotonin-responsive dorsal horn neurons in the mouse. J. Neurophysiol. 117, 251–259. doi: 10.1152/jn.00703.2016
Bautista, D. M., Wilson, S. R., and Hoon, M. A. (2014). Why we scratch an itch: the molecules, cells and circuits of itch. Nat. Neurosci. 17, 178–182. doi: 10.1038/nn.3619
Bogaczewicz, J., Malinowska, K., Sysa-Jedrzejowska, A., and Wozniacka, A. (2016). Medium-dose ultraviolet A1 phototherapy improves SCORAD index and increases mRNA expression of interleukin-4 without direct effect on human β defensin-1, interleukin-10, and interleukin-31. Int. J. Dermatol. 55, E380–E385. doi: 10.1111/ijd.13213
Bourane, S., Duan, B., Koch, S. C., Dalet, A., Britz, O., Garcia-Campmany, L., et al. (2015). Gate control of mechanical itch by a subpopulation of spinal cord interneurons. Science 350, 550–554. doi: 10.1126/science.aac8653
Brenaut, E., Halvorsen, J. A., Dalgard, F. J., Lien, L., Balieva, F., Sampogna, F., et al. (2019). The self-assessed psychological comorbidities of prurigo in European patients: a multicentre study in 13 countries. J. Eur. Acad. Dermatol. Venereol. 33, 157–162. doi: 10.1111/jdv.14570
Carr, C. W., Emir, V., and Chen, S. C. (2014). Factors Mediating the Impact of Chronic Pruritus on Quality of Life. JAMA Dermatol. 150, 613–620.
Cevikbas, F., and Lerner, E. A. (2020). Physiology and Pathophysiology of Itch. Physiol. Rev. 100, 945–982. doi: 10.1152/physrev.00017.2019
Chan, L. S., Robinson, N., and Xu, L. (2001). Expression of interleukin-4 in the epidermis of transgenic mice results in a pruritic inflammatory skin disease: an experimental animal model to study atopic dermatitis. J. Invest. Dermatol. 117, 977–983. doi: 10.1046/j.0022-202x.2001.01484.x
Chen, S., Gao, X. F., Zhou, Y., Liu, B. L., Liu, X. Y., Zhang, Y., et al. (2020). A spinal neural circuitry for converting touch to itch sensation. Nat. Commun. 11:5074. doi: 10.1038/s41467-020-18895-7
Chen, X. J., and Sun, Y. G. (2020). Central circuit mechanisms of itch. Nat. Commun. 11:3052. doi: 10.1038/s41467-020-16859-5
Chen, Y. H., Yang, H. Y., Lin, C. H., Dun, N. J., and Lin, J. G. (2013). Electroacupuncture Attenuates 5’-Guanidinonaltrindole-Evoked Scratching and Spinal c-Fos Expression in the Mouse. Evid. Based Complement. Alter. Med. 2013:319124. doi: 10.1155/2013/319124
Che-Yi, C., Wen, C. Y., Min-Tsung, K., and Chiu-Ching, H. (2005). Acupuncture in haemodialysis patients at the Quchi (LI11) acupoint for refractory uraemic pruritus. Nephrol. Dial. Transplant. 20, 1912–1915. doi: 10.1093/ndt/gfh955
Chiu, I. M., Barrett, L. B., Williams, E. K., Strochlic, D. E., and Weyer, A. D. (2014). Transcriptional profiling at whole population and single cell levels reveals somatosensory neuron molecular diversity. Elife 3:e04660. doi: 10.7554/eLife.04660
Chrostowska-Plak, D., Reich, A., and Szepietowski, J. C. (2012). Relationship between itch and psychological status of patients with atopic dermatitis. J. Eur. Acad. Dermatol. Venereol. 27, e239–e242. doi: 10.1111/j.1468-3083.2012.04578.x
Deng, C. (2018). Clinical observation on chronic pruritus treated by electroacupuncture with different frequencies and its on IL-4 and IFN-γ levels. China: Hubei University of traditional Chinese Medicine.
Di Marzo, V., and Petrocellis, L. D. (2006). Plant, synthetic, and endogenous cannabinoids in medicine. Annu. Rev. Med. 57, 553–574. doi: 10.1146/annurev.med.57.011205.135648
Dong, X., and Dong, X. (2018). Peripheral and Central Mechanisms of Itch. Neuron 98, 482–494. doi: 10.1016/j.neuron.2018.03.023
Düll, M. M., and Kremer, A. E. (2020). Newer Approaches to the Management of Pruritus in Cholestatic Liver Disease. Curr. Hepatol. Rep. 19, 86–95. doi: 10.1007/s11901-020-00517-x
Gingold, A. R., and Bergasa, N. V. (2003). The cannabinoid agonist WIN 55, 212-2 increases nociception threshold in cholestatic rats: implications for the treatment of the pruritus of cholestasis. Life Sci. 73, 2741–2747. doi: 10.1016/s0024-3205(03)00668-4
Graybiel, A. M. (2008). Habits, rituals, and the evaluative brain. Annu. Rev. Neurosci. 31, 359–387. doi: 10.1146/annurev.neuro.29.051605.112851
Gupta, M. A., and Gupta, A. K. (1999). Depression modulates pruritus perception. A study of pruritus in psoriasis, atopic dermatitis and chronic idiopathic urticaria. Ann. N. Y. Acad. Sci. 885, 394–395. doi: 10.1111/j.1749-6632.1999.tb08697.x
Hachisuka, J., Furue, H., Furue, M., and Yoshimura, M. (2010). Responsiveness of C Neurons in Rat Dorsal Root Ganglion to 5-Hydroxytryptamine-Induced Pruritic Stimuli In Vivo. J. Neurophysiol. 104, 271–279. doi: 10.1152/jn.00938.2009
Han, J. B., Kim, C. W., Sun, B., Kim, S. K., Lee, M. G., Park, D. S., et al. (2008). The antipruritic effect of acupuncture on serotonin-evoked itch in rats. Acupunct. Electrother. Res. 33, 145–156. doi: 10.3727/036012908803861168
Han, L., and Dong, X. (2014). Itch mechanisms and circuits. Annu. Rev. Biophys. 43, 331–355. doi: 10.1146/annurev-biophys-051013-022826
Han, L., Ma, C., Liu, Q., Weng, H. J., Cui, Y., Tang, Z., et al. (2013). A subpopulation of nociceptors specifically linked to itch. Nat. Neurosci. 16, 174–182. doi: 10.1038/nn.3289
Hawro, T., Przybyłowicz, K., Spindler, M., Hawro, M., Steć, M., Altrichter, S., et al. (2021). The characteristics and impact of pruritus in adult dermatology patients: a prospective, cross-sectional study. J. Am. Acad. Dermatol. 84, 691–700. doi: 10.1016/j.jaad.2020.08.035
Hirschfield, G. M., Beuers, U., Corpechot, C., Invernizzi, P., and Jones, D. (2017). EASL Clinical Practice Guidelines: the diagnosis and management of patients with primary biliary cholangitis. J. Hepatol. 67, 145–172. doi: 10.1016/j.jhep.2017.03.022
Huang, L. L., Yin, Y., Fu, L. H., Wu, S. Y., and Li, M. (2020). Clinical effect of Electroacupuncture on chronic pruritus and its influence on IL-2 and IL-10. Lishizhen Med. Mater. Med. Res. 31, 1656–1658.
Ikoma, A., Steinhoff, M., Ständer, S., Yosipovitch, G., and Schmelz, M. (2006). The neurobiology of itch. Nat. Rev. Neurosci. 7, 535–547. doi: 10.1038/nrn1950
Imamachi, N., Park, G. H., Lee, H., Anderson, D. J., Simon, M. I., Basbaum, A. I., et al. (2009). TRPV1-expressing primary afferents generate behavioral responses to pruritogens via multiple mechanisms. Proc. Natl. Acad. Sci. U. S. A. 106, 11330–11335. doi: 10.1073/pnas.0905605106
Jiang, L., Liu, J. H., Huang, J. P., Xie, C. C., and Fu, W. B. (2016a). Antipruritic effect and immunoregulation mechanism of Electroacupuncture on allergic contact dermatitis in mice. Chin. J. Gerontol. 36, 3615–3618. doi: 10.3969/j.issn.1005-9202.2016.16.003
Jiang, L., Xie, C. C., Huang, J. P., and Fu, W. B. (2016b). Antipruritic effect of Electroacupuncture on mice with atopic dermatitis and pruritus and its effect on dynorphin and substance P. Chin. J. Gerontol. 36, 3874–3877.
Jung, D. L., Lee, S. D., Choi, I. H., Na, H. S., and Hong, S. U. (2014). Effects of electroacupuncture on capsaicin-induced model of atopic dermatitis in rats. J. Dermatol. Sci. 74, 23–30. doi: 10.1016/j.jdermsci.2013.11.015
Kang, S. H., Kim, Y. K., Yeom, M., Lee, H., Jang, H., Park, H. J., et al. (2018). Acupuncture Improves Symptoms in Patients with Mild to Moderate Atopic Dermatitis: a Randomized, Sham-Controlled Preliminary Trial. J. Acupunct. Meridian Stud. 11, 90–98. doi: 10.1016/j.ctim.2018.08.013
Kardon, A. P., Polgár, E., Hachisuka, J., Snyder, L. M., Cameron, D., Savage, S., et al. (2014). Dynorphin Acts as a Neuromodulator to Inhibit Itch in the Dorsal Horn of the Spinal Cord. Neuron 82, 573–586. doi: 10.1016/j.neuron.2014.02.046
Kenya, K., Takeshi, Y., Hiroteru, K., Akira, S., Satoshi, A., Atsunori, T., et al. (2017). Long-term efficacy and safety of nalfurafine hydrochloride on pruritus in chronic liver disease patients: patient-reported outcome based analyses. PLoS One 12:e0178991. doi: 10.1371/journal.pone.0178991
Kılıç Akça, N., and Taşcı, S. (2016). Acupressure and Transcutaneous Electrical Acupoint Stimulation for Improving Uremic Pruritus: a Randomized, Controlled Trial. Altern. Ther. Health Med. 22, 18–24.
Kim, H. M., Cho, S. Y., Park, S. U., Sohn, I. S., Jung, W. S., Moon, S. K., et al. (2012). Can acupuncture affect the circadian rhythm of blood pressure? A randomized, double-blind, controlled trial. J. Altern. Complement. Med. 18, 918–923. doi: 10.1089/acm.2011.0508
Kouwenhoven, T. A., van de Kerkhof, P. C. M., and Kamsteeg, M. (2017). Use of oral antidepressants in patients with chronic pruritus: a systematic review. J. Am. Acad. Dermatol. 77, 1068–1073.e7. doi: 10.1016/j.jaad.2017.08.025
Langedijk, J., Beuers, U. H., and Elferink, R. (2021). Cholestasis-Associated Pruritus and Its Pruritogens. Front. Med. 8:639674. doi: 10.3389/fmed.2021.639674
Lee, K. C., Keyes, A., Hensley, J. R., Gordon, J. R., Kwasny, M. J., West, D. P., et al. (2012). Effectiveness of acupressure on pruritus and lichenification associated with atopic dermatitis: a pilot trial. Acupunct. Med. 30, 8–11. doi: 10.1136/acupmed-2011-010088
Lee, Y. C., Lin, C. H., Hung, S. Y., Chung, H. Y., Luo, S. T., MacDonald, I., et al. (2018). Manual acupuncture relieves bile acid-induced itch in mice: the role of microglia and TNF-α. Int. J. Med. Sci. 15, 953–960. doi: 10.7150/ijms.24146
Leslie, T. A., Greaves, M. W., and Yosipovitch, G. (2015). Current topical and systemic therapies for itch. Handb. Exp. Pharmacol. 226, 337–356. doi: 10.1007/978-3-662-44605-8_18
Li, A. H., Zhang, J. M., and Xie, Y. K. (2004). Human acupuncture points mapped in rats are associated with excitable muscle/skin-nerve complexes with enriched nerve endings. Brain Res. 1012, 154–159. doi: 10.1016/j.brainres.2004.04.009
Li, H. P. (2019). Neurobiological mechanisms of electroacupuncture inhibiting chronic itch and GRPR receptor expression by endocannabinoid system. Wuhan: Huazhong University of Science & Technology.
Lin, J. G., Lee, Y. C., Tseng, C. H., Chen, D. Y., Shih, C. Y., Macdonald, I., et al. (2016). Electroacupuncture inhibits pruritogen-induced spinal microglial activation in mice. Brain Res. 1649, 23–29. doi: 10.1016/j.brainres.2016.07.007
Liu, X. Y., Liu, Z. C., Sun, Y. G., Ross, M., Kim, S., Tsai, F. F., et al. (2011). Unidirectional Cross-Activation of GRPR by MOR1D Uncouples Itch and Analgesia Induced by Opioids. Cell 147, 447–458. doi: 10.1016/j.cell.2011.08.043
Liu, Y., Wu, X. M., Luo, Q. Q., Huang, S., Yang, Q., Wang, F. X., et al. (2015). CX3CL1/CX3CR1-mediated microglia activation plays a detrimental role in ischemic mice brain via p38MAPK/PKC pathway. J. Cereb. Blood Flow Metab. 35, 1623–1631. doi: 10.1038/jcbfm.2015.97
McMahon, S. B., and Koltzenburg, M. (1992). Itching for an explanation. Trends Neurosci. 15, 497–501. doi: 10.1016/0166-2236(92)90102-e
Millington, G. W. M., Collins, A., Lovell, C. R., Leslie, T. A., Yong, A. S. W., and Morgan, J. D. (2018). British Association of Dermatologists’ guidelines for the investigation and management of generalized pruritus in adults without an underlying dermatosis, 2018. Br. J. Dermatol. 178, 34–60. doi: 10.1111/bjd.16117
Min, S., Kim, K. W., Jung, W. M., Lee, M. J., Kim, Y. K., Chae, Y., et al. (2019). Acupuncture for Histamine-Induced Itch: association With Increased Parasympathetic Tone and Connectivity of Putamen-Midcingulate Cortex. Front. Neurosci. 13:215. doi: 10.3389/fnins.2019.00215
Mishra, S. K., and Hoon, M. A. (2013). The cells and circuitry for itch responses in mice. Science 340, 968–971. doi: 10.1126/science.1233765
Miyamoto, T., and Patapoutian, A. (2011). Why does morphine make you itch? Cell 147, 261–262. doi: 10.1016/j.cell.2011.09.026
Moosa, A. S., Leng, N. S. Y., Kum, C. L., and Tan, N. C. (2021). A qualitative research study on the illness perception of chronic pruritus in older Asian adults based on the Common-Sense Model of self-regulation. Health Expect. 24, 1801–1811. doi: 10.1111/hex.13320
Nahidi, Y., Badiee, S., Torabi, S., Abbasi, S. Z., Nazemeh, N., and Saki, A. (2018). Acupuncture Effect on Pruritus in Hemodialysis Patients: a Randomized Clinical Trial. Iran. Red Crescent Med. J. 20:e65521. doi: 10.5812/ircmj.65521
Ni, G. B. (2017). The clinical observation about the efficacy of electroacupuncture in the treatment of chronic pruriyus and its effect on the levels of IL-10 and TNF-α in serum. master. Wuhan: Hubei University of Traditional Chinese Medicine.
O’Donoghue, M., and Tharp, M. D. (2005). Antihistamines and their role as antipruritics. Dermatol. Ther. 18, 333–340. doi: 10.1111/j.1529-8019.2005.00034.x
Oeda, S., Takahashi, H., Yoshida, H., Ogawa, Y., Imajo, K., Yoneda, M., et al. (2018). Prevalence of pruritus in patients with chronic liver disease: a multicenter study. Hepatol. Res. 48, E252–E262.
Oetjen, L. K., Mack, M. R., Feng, J., Whelan, T. M., Niu, H., Guo, C. J., et al. (2017). Sensory Neurons Co-opt Classical Immune Signaling Pathways to Mediate Chronic Itch. Cell 171, 217–228.e13. doi: 10.1016/j.cell.2017.08.006
Park, H. J., Sora, A., Lee, H., Hahm, D., Kinm, K., and Yeom, M. (2021). Acupuncture ameliorates not only atopic dermatitis-like skin inflammation but also acute and chronic serotonergic itch possibly through blockade of 5-HT2 and 5-HT7 receptors in mice. Brain Behav. Immun. 93, 399–408.
Park, J. G., Lee, H., Yeom, M., Chae, Y., Park, H. J., and Kim, K. (2021). Effect of acupuncture treatment in patients with mild to moderate atopic dermatitis: a randomized, participant- and assessor-blind sham-controlled trial. BMC Complement. Med. Ther. 21:132. doi: 10.1186/s12906-021-03306-1
Pasparakis, M., Haase, I., and Nestle, F. O. (2014). Mechanisms regulating skin immunity and inflammation. Nat. Rev. Immunol. 14, 289–301. doi: 10.1038/nri3646
Pfab, F., Huss-Marp, J., Gatti, A., Fuqin, J., and Darsow, U. (2010). Influence of acupuncture on type I hypersensitivity itch and the wheal and flare response in adults with atopic eczema – a blinded, randomized, placebo-controlled, crossover trial. Allergy 65, 903–910. doi: 10.1111/j.1398-9995.2009.02284.x
Pfab, F., Kirchner, M. T., Huss-Marp, J., Schuster, T., Schalock, P. C., Fuqin, J., et al. (2012). Acupuncture compared with oral antihistamine for type I hypersensitivity itch and skin response in adults with atopic dermatitis: a patient- and examiner-blinded, randomized, placebo-controlled, crossover trial. Allergy 67, 566–573. doi: 10.1111/j.1398-9995.2012.02789.x
Reszke, R., and Szepietowski, J. C. (2018). End-Stage Renal Disease Chronic Itch and Its Management. Dermatol. Clin. 36, 277–292. doi: 10.1016/j.det.2018.02.007
Satoh, T., Yokozeki, H., Murota, H., Tokura, Y., Kabashima, K., Takamori, K., et al. (2021). 2020 guidelines for the diagnosis and treatment of cutaneous pruritus. J. Dermatol. 48, e399–e413. doi: 10.1111/1346-8138.16066
Schneider, G., Ständer, S., Burgmer, M., Driesch, G., Heuft, G., and Weckesser, M. (2008). Significant differences in central imaging of histamine-induced itch between atopic dermatitis and healthy subjects. Eur. J. Pain 12, 834–841. doi: 10.1016/j.ejpain.2007.12.003
Schut, C., Dalgard, F. J., Halvorsen, J. A., Gieler, U., Lien, L., Aragones, L. T., et al. (2019). Occurrence, Chronicity and Intensity of Itch in a Clinical Consecutive Sample of Patients with Skin Diseases: a Multi-centre Study in 13 European Countries. Acta Derm. Venereol. 99, 146–151. doi: 10.2340/00015555-3040
Shao, P., and Chen, Y. G. (2012). Study on The Effect of Acupuncture on Serum IgE and Skin 5-HT2A Receptor in Rat. J. Pract. Trad. Chin. Intern. Med. 26:2.
Ständer, S., Weisshaar, E., Mettang, T., Szepietowski, J. C., Carstens, E., Ikoma, A., et al. (2007). Clinical classification of itch: a position paper of the international forum for the study of itch. Acta Derm. Venereol. 87, 291–294. doi: 10.2340/00015555-0305
Ständer, S., Zeidler, C., Magnolo, N., Raap, U., Mettang, T., Kremer, A. E., et al. (2015). Clinical management of pruritus. J. Dtsch. Dermatol. Ges. 13, 101–116. doi: 10.1111/ddg.12522
Thurmond, R. L., Kazerouni, K., Chaplan, S. R., and Greenspan, A. J. (2015). Antihistamines and itch. Handb. Exp. Pharmacol. 226, 257–290. doi: 10.1007/978-3-662-44605-8_15
Todurga, Z. G., Gunduz, O., Karadag, C. H., and Ulugol, A. (2016). Descending serotonergic and noradrenergic systems do not regulate the antipruritic effects of cannabinoids. Acta Neuropsychiatr. 28, 321–326. doi: 10.1017/neu.2016.16
Torigoe, K., Tominaga, M., Ko, K. C., Takahashi, N., Matsuda, H., Hayashi, R., et al. (2016). Intrathecal minocycline suppresses itch-related behavior and improves dermatitis in a mouse model of atopic dermatitis. J. Invest. Dermatol. 136, 879–881. doi: 10.1016/j.jid.2015.12.037
Umehara, Y., Kiatsurayanon, C., Trujillo-Paez, J. V., Chieosilapatham, P., and Niyonsaba, F. (2021). Intractable Itch in Atopic Dermatitis: causes and Treatments. Biomedicines 9:229. doi: 10.3390/biomedicines9030229
Usoskin, D., Furlan, A., Islam, S., Abdo, H., Lönnerberg, P., Lou, D., et al. (2015). Unbiased classification of sensory neuron types by large-scale single-cell RNA sequencing. Nat. Neurosci. 18, 145–153. doi: 10.1038/nn.3881
van den Berg-Wolf, M., and Burgoon, T. (2017). Acupuncture and Cutaneous Medicine: is It Effective? Med. Acupunct. 29, 269–275. doi: 10.1089/acu.2017.1227
Vitaly, N., Li, A., Loggia, M. L., Jieun, K., Schalock, P. C., Ethan, L., et al. (2014). The Brain Circuitry Mediating Antipruritic Effects of Acupuncture. Cereb. Cortex 24, 873–882. doi: 10.1093/cercor/bhs363
Wang, F., Trier, A. M., Li, F., Kim, S., Chen, Z., Chai, J. N., et al. (2021). A basophil-neuronal axis promotes itch. Cell 184, 422–440.e17. doi: 10.1016/j.cell.2020.12.033
Wang, Q. (2018). The cinical curative effect of electroacupuncturein the treatment of chronic itching and its effects on plasma IL-6 and IP-10 content. Wuhan: Hubei University of traditional Chinese Medicine.
Wang, Y. J., and Wang, S. K. (1989). [Effects of electroacupuncture at different hours on leucine-enkephalin contents in rat brain regions]. Zhen Ci Yan Jiu 14, 420–423.
Wang, Y., and Xu, B. (2014). Research progress on treatment of pruritus with acupuncture and moxibustion. Chin. J. Basic Med. Tradit. Chin. Med. 20, 419–420.
Weisshaar, E., and Dalgar, D. F. (2009). Epidemiology of itch: adding to the burden of skin morbidity. Acta Derm. Venereol. 89, 339–350. doi: 10.2340/00015555-0662
Weisshaar, E., Apfelbacher, C., Jger, G., Zimmermann, E., Bruckner, T., Diepgen, T. L., et al. (2006). Pruritus as a leading symptom: clinical characteristics and quality of life in German and Ugandan patients. Br. J. Dermatol. 155, 957–964. doi: 10.1111/j.1365-2133.2006.07430.x
Weisshaar, E., Szepietowski, J. C., Dalgard, F. J., Garcovich, S., Gieler, U., Giménez-Arnau, A. M., et al. (2019). European S2k Guideline on Chronic Pruritus. Acta Derm. Venereol. 99, 469–506. doi: 10.2340/00015555-3164
Whang, K. A., Khanna, R., Williams, K. A., Mahadevan, V., and Kwatra, S. G. (2020). Health-related quality of life and economic burden of chronic pruritus. J. Invest. Dermatol. 141, 754–760.e1.
Whang, K. A., Khanna, R., Williams, K. A., Mahadevan, V., Semenov, Y., and Kwatra, S. G. (2021a). Health-Related QOL and Economic Burden of Chronic Pruritus. J. Invest. Dermatol. 141, 754–760.e1. doi: 10.1016/j.jid.2020.08.020
Whang, K. A., Le, T. K., Khanna, R., Williams, K. A., Roh, Y. S., Sutaria, N., et al. (2021b). Health-related quality of life and economic burden of prurigo nodularis. J. Am. Acad. Dermatol. doi: 10.1016/j.jaad.2021.05.036 [Epub Online ahead of print].
Wick, F., Wick, N., and Wick, M. C. (2007). Morphological Analysis of Human Acupuncture Points Through Immunohistochemistry. Am. J. Phys. Med. Rehabil. 86, 7–11. doi: 10.1097/01.phm.0000250564.88013.89
Xu, Z., Qin, Z., Zhang, J., and Wang, Y. (2020). Microglia-mediated chronic psoriatic itch induced by imiquimod. Mol. Pain 16:1744806920934998. doi: 10.1177/1744806920934998
Yamaguchi, T., Nagasawa, T., Satoh, M., and Kuraishi, Y. (1999). Itch-associated response induced by intradermal serotonin through 5-HT2 receptors in mice. Neurosci. Res. 35, 77–83. doi: 10.1016/s0168-0102(99)00070-x
Yan, C. (2017). Effect of acupuncture on 5-HT and endorphins in chronic pruritus mice model and its clinical observation. Taiyuan: Shanxi University of Chinese Medicine.
Yan, C. N., Yao, W. G., Bao, Y. J., Shi, X. J., Yu, H., Yin, P. H., et al. (2015). Effect of Auricular Acupressure on Uremic Pruritus in Patients Receiving Hemodialysis Treatment: a Randomized Controlled Trial. Evid. Based Complement. Alternat. Med. 2015:593196. doi: 10.1155/2015/593196
Yano, C., Saeki, H., Ishiji, T., Ishiuji, Y., Sato, J., Tofuku, Y., et al. (2013). Impact of disease severity on work productivity and activity impairment in Japanese patients with atopic dermatitis. J. Dermatol. 40, 736–739. doi: 10.1111/1346-8138.12220
Yao, Q., Li, S., Liu, X., Qin, Z., and Liu, Z. (2016). The Effectiveness and Safety of Acupuncture for Patients with Chronic Urticaria: a Systematic Review. Biomed Res. Int. 2016:5191729. doi: 10.1155/2016/5191729
Ying, Z., Dun, S. L., Chen, Y., Luo, J. J., Cowan, A., and Dun, N. J. (2015). Scratching activates microglia in the mouse spinal cord. J. Neurosci. Res. 93, 466–474. doi: 10.1002/jnr.23501
Yosipovitch, G., and Bernhard, J. D. (2013). Clinical practice. Chronic pruritus. N. Engl. J. Med. 368, 1625–1634. doi: 10.1056/NEJMcp1208814
Yosipovitch, G., and Mochizuki, H. (2015). Neuroimaging of itch as a tool of assessment of chronic itch and its management. Handb. Exp. Pharmacol. 226, 57–70. doi: 10.1007/978-3-662-44605-8_4
Yosipovitch, G., Goon, A., Wee, J., Chan, Y. H., and Goh, C. L. (2010). Itch characteristics in Chinese patients with atopic dermatitis using a new questionnaire for the assessment of pruritus. Int. J. Dermatol. 41, 212–216. doi: 10.1046/j.1365-4362.2002.01460.x
Yosipovitch, G., Goon, A., Wee, J., Chan, Y. H., and Goh, C. L. (2015). The prevalence and clinical characteristics of pruritus among patients with extensive psoriasis. Br. J. Dermatol. 143, 969–973.
Yosipovitch, G., Rosen, J. D., and Hashimoto, T. (2018). Itch: from mechanism to (novel) therapeutic approaches. J. Allergy Clin. Immunol. 142, 1375–1390. doi: 10.1016/j.jaci.2018.09.005
Yosipovitch, G., Zucker, I., Boner, G., Gafter, U., Shapira, Y., David, M., et al. (2001). A questionnaire for the assessment of pruritus: validation in uremic patients. Acta Derm. Venereol. 81, 108–111.
Zhang, Y., Yan, J., Hu, R., Sun, Y., Ma, Y., Chen, Z., et al. (2015). Microglia are involved in pruritus induced by DNFB via the CX3CR1/p38 MAPK pathway. Cell. Physiol. Biochem. 35, 1023–1033. doi: 10.1159/000373929
Zhang, Z. N., Yao, Z. Y., Cai, X. W., and Huang, Y. (2019). Itching Symptom: pathology and Commonly used Acupoints. Clin. J. Tradit. Chin. Med. 31, 476–479. doi: 10.16448/j.cjtcm.2019.0141
Zhao, Y. D., Yan, C. D., and Yan, X. N. (2018). Effect of acupuncture on expression of 5- HT and its receptors in mice with histamine- induced pruritus. Mod. J. Integr. Tradit. Chin. Western Med. 27, 2983–2985.
Zhao, Y. D., Yan, C. J., Sun, D., Li, W. B., and Yan, X. N. (2017). Effects of Acupuncture on Expression of 5-HT Neurons in Medulla Oblongata and 5-HTR2B on Mice Models with Chloroquine-induced Pruritus. Chin. J. Inf. TCM 24, 56–59. doi: 10.3969/j.issn.1005-5304.2017.12.014
Zhao, Z. Q. (2008). Neural mechanism underlying acupuncture analgesia. Prog. Neurobiol. 85, 355–375. doi: 10.1016/j.pneurobio.2008.05.004
Zhao, Z.-Q., Liu, X.-Y., Jeffry, J., Karunarathne, W. K., Li, J. L., Munanairi, A., et al. (2014). Descending control of itch transmission by the serotonergic system via 5-HT1A-facilitated GRP-GRPR signaling. Neuron 84, 821–834. doi: 10.1016/j.neuron.2014.10.003
Keywords: itch (pruritus), neurobiologic mechanisms, review, periphery and center, acupuncture-therapy
Citation: Tang Y, Cheng S, Wang J, Jin Y, Yang H, Lin Q, Xu S, Hui L, Yin Q, Yang Y and Wu X (2022) Acupuncture for the Treatment of Itch: Peripheral and Central Mechanisms. Front. Neurosci. 15:786892. doi: 10.3389/fnins.2021.786892
Received: 30 September 2021; Accepted: 13 December 2021;
Published: 30 March 2022.
Edited by:
Man Li, Huazhong University of Science and Technology, ChinaReviewed by:
Miriam Margareta Düll, University Hospital Erlangen, GermanyPeijing Rong, China Academy of Chinese Medical Sciences, China
Yi-Hung Chen, China Medical University, Taiwan
Copyright © 2022 Tang, Cheng, Wang, Jin, Yang, Lin, Xu, Hui, Yin, Yang and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xi Wu, d3V4aUBjZHV0Y20uZWR1LmNu
†These authors have contributed equally to this work and share first authorship
 Yi Tang
Yi Tang Shirui Cheng
Shirui Cheng Jin Wang†
Jin Wang† Qihui Lin
Qihui Lin Sanmei Xu
Sanmei Xu Lin Hui
Lin Hui