
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurosci. , 30 April 2018
Sec. Neurodegeneration
Volume 12 - 2018 | https://doi.org/10.3389/fnins.2018.00260
This article is part of the Research Topic Genetics of Neurodegenerative Diseases View all 11 articles
 Karolina Kauppi1,2*
Karolina Kauppi1,2* Chun Chieh Fan1,3
Chun Chieh Fan1,3 Linda K. McEvoy1
Linda K. McEvoy1 Dominic Holland4
Dominic Holland4 Chin Hong Tan5
Chin Hong Tan5 Chi-Hua Chen1
Chi-Hua Chen1 Ole A. Andreassen6,7
Ole A. Andreassen6,7 Rahul S. Desikan5and
Rahul S. Desikan5and  Anders M. Dale1,3,4* for the Alzheimer's Disease Neuroimaging Initiative†
Anders M. Dale1,3,4* for the Alzheimer's Disease Neuroimaging Initiative†Improved prediction of progression to Alzheimer's Disease (AD) among older individuals with mild cognitive impairment (MCI) is of high clinical and societal importance. We recently developed a polygenic hazard score (PHS) that predicted age of AD onset above and beyond APOE. Here, we used data from the Alzheimer's Disease Neuroimaging Initiative (ADNI) to further explore the potential clinical utility of PHS for predicting AD development in older adults with MCI. We examined the predictive value of PHS alone and in combination with baseline structural magnetic resonance imaging (MRI) data on performance on the Mini-Mental State Exam (MMSE). In survival analyses, PHS significantly predicted time to progression from MCI to AD over 120 months (p = 1.07e-5), and PHS was significantly more predictive than APOE alone (p = 0.015). Combining PHS with baseline brain atrophy score and/or MMSE score significantly improved prediction compared to models without PHS (three-factor model p = 4.28e-17). Prediction model accuracies, sensitivities and area under the curve were also improved by including PHS in the model, compared to only using atrophy score and MMSE. Further, using linear mixed-effect modeling, PHS improved the prediction of change in the Clinical Dementia Rating—Sum of Boxes (CDR-SB) score and MMSE over 36 months in patients with MCI at baseline, beyond both APOE and baseline levels of brain atrophy. These results illustrate the potential clinical utility of PHS for assessment of risk for AD progression among individuals with MCI both alone, or in conjunction with clinical measures of prodromal disease including measures of cognitive function and regional brain atrophy.
Late onset Alzheimer's disease (AD) is the most common form of dementia, affecting 24–35 million people world-wide (Querfurth and LaFerla, 2010; Alzheimer's Association, 2015). Novel methods to enable early AD detection based on clinically feasible, economical, and non-invasive measures is of high clinical and societal value. Early identification of high-risk individuals is also of utmost importance for pre-dementia clinical trials (Holland et al., 2012; Ritchie et al., 2016).
A large effort has been made to improve the prediction of progression to AD among older individuals with mild cognitive impairment (MCI), which can be a transition stage from normal age-related cognitive decline to dementia (Roberts and Knopman, 2013). Next to older age, inheritance of the ε4 allele of the Apolipoprotein E (APOE) gene is the strongest individual risk factor for late onset AD (Yu et al., 2014). However, other genetic risk variants of smaller effect also contribute to AD risk (Lambert et al., 2013; Ridge et al., 2013). While most studies examining genetic risk for sporadic AD focus on APOE genotype, some have assessed polygenic risk scores beyond APOE based on case-control data from large-scale genome-wide association studies (GWAS) (Lambert et al., 2013), and found that genetic variants associated with elevated AD risk also influence brain structure (Sabuncu et al., 2012) and cognitive function (Marioni et al., 2017). Given that the incidence of AD increases sharply with age, we recently develop a polygenic hazard score (PHS) for prediction of age-specific AD risk, based on 31 AD-susceptibility variants, including APOE (Desikan et al., 2017). The PHS showed substantial improvement over APOE in predicting age of AD onset and was associated with biomarkers of AD, including MRI-based hippocampal volume loss (Desikan et al., 2017), amyloid, and tau deposition (Tan et al., 2018).
Volumetric MRI-based measures of regional brain atrophy, particularly medial temporal volume loss are important biomarkers for assessing risk of progression to AD in patients with MCI (Li et al., 2016). In previous work from our lab, we derived a composite regional “brain atrophy score” from linear discrimination analysis trained on data from healthy controls and AD patients, which was better at predicting 1 year cognitive decline than atrophy in medial temporal structures alone (McEvoy et al., 2009). The atrophy score is based on volume of the hippocampus, and thickness of entorhinal cortex, middle temporal gyrus, bank of the superior temporal sulcus, isthmus cingulate (retrosplenial cortex), superior temporal gyrus, medial and lateral orbitofrontal gyri, with weightings for each ROI determined through a linear discrimination analysis that best distinguished AD patients from healthy controls. In a subsequent study, this brain atrophy score predicted 1-year risk of progression to AD in individual patients (McEvoy et al., 2011). Prediction of 1-year clinical decline was further improved by adding subjects' baseline Mini-Mental State Exam (MMSE) scores and number of APOE ε4 alleles to the model (McEvoy et al., 2009).
In the current study, we investigated the clinical utility of PHS for individual assessment of risk for clinical progression to AD over time among older individuals with MCI, a critical question for most patients admitted to memory clinics. Whereas prior work from our group has shown the value of PHS for predicting AD-associated clinical and cognitive decline among non-demented elderly individuals (Tan et al., 2017), a critical next step in assessing the potential clinical utility of PHS is to examine the extent to which PHS provides independent information beyond other commonly used predictors, such as brain atrophy levels and baseline cognitive function, and to determine whether combinations of these measures improve prediction of clinical decline and progression to dementia. To this end, we used survival analyses (Klein et al., 2013) to compare single-, two-, and three-factor models of PHS, atrophy score, and MMSE for prediction of time to progression from MCI to AD over 120 months of follow-up. As a complementary approach, we used linear mixed-effect modeling to examine prediction of clinical change in MMSE and the Clinical Dementia Rating, sum of boxes (CDR-SB), over 36 months.
We used participants from the ADNI database, available as of November 2011. ADNI 1 is a 5-year multi-site program launched in 2003 as a public-private partnership including the National Institute on Aging, Food and Drug Administration, pharmaceutical companies, and nonprofit organizations (led by Principal Investigator Michael W. Weiner, MD.). The main goal of ADNI is to examine if progression from MCI to AD can be predicted based on neuroimaging, biological biomarkers as well as clinical and neuropsychological assessments.
The baseline data was collected in 2005, including elderly healthy controls (n = 200), Alzheimer's disease patients (n = 200), and individuals with MCI (n = 400), followed by annual follow-ups for 36 months. We included 336 participant with a MCI diagnosis at baseline in ADNI 1 and available genetic, MRI, and cognitive data, including mini-mental state examination (MMSE) (Folstein et al., 1975) and Clinical dementia rating, sum of boxes (CDR-SB) (Hughes et al., 1982). The age range was 55–89 at baseline. Longitudinal data on CDR-SB and MMSE was included from ADNI 1, with 36-month follow-up. Data on progression to AD was also included from ADNI 2 and ADNI GO, providing data on progression to AD for up to 120 months after baseline. The ADNI study was approved by local institutional review boards, and all participants or participant's guardians provided written informed consent. Additional information about ADNI is available at http://www.adni-info.org.
Details of image acquisition and analysis have been described in our previous publications (McEvoy et al., 2009). Briefly, we downloaded the raw baseline DICOM MRI data from the ADNI web site (http://adni.loni.usc.edu/data-samples/mri/) and obtained volumetric assessments on neuroanatomic regions of interest (ROIs) using a modified version of the FreeSurfer image-analysis software (Brewer, 2009; Brewer et al., 2009). We used a previously validated brain atrophy score based on volume of the hippocampus, and thickness of entorhinal cortex, middle temporal gyrus, bank of the superior temporal sulcus, isthmus cingulate (retrosplenial cortex), superior temporal gyrus, medial and lateral orbitofrontal gyri, with weightings for each ROI determined through a linear discrimination analysis that best distinguished AD patients from healthy controls (for additional details, see McEvoy et al., 2009, 2011). In the current paper, we computed an atrophy score as the sum of weighted measures from these brain regions, averaging left, and right hemispheres.
For each participant included in the study, we calculated their individual PHS based on our previous publication (Desikan et al., 2017). In brief, PHS was derived by first identifying common variants associated with AD in the International genetics of Alzheimer's Project (IGAP) GWAS on AD, with a p-value threshold of <10−5 using summary statistics. These SNPs were examined for association with AD in the Alzheimer's Disease Genetic consortia (ADGC) phase 1 genetic data. A stepwise Cox proportional hazard model was applied in which the SNPs that improved the model most were included sequentially until the model was no longer improved by adding more SNPs. This resulted in a list of 31 SNPs, including the two SNPs that constitute the APOE ε genotype, which were used to generate the PHS. Finally, the PHS estimates from ADGC were integrated with established AD-incidence rates from the US population to provide quantitative estimates of the annualized (cumulative) incidence rate. The PHS is the vector product of a person's genotype for the 31 SNPs and the corresponding parameter estimates from the Cox proportional hazard model.
We used Cox proportional Hazard models in Matlab [version 8.5.0.197613 (R2015a)] to model time to progression from MCI to AD with a follow up period of 120 months. Time to event was defined as time from baseline to AD onset (with end of study time or drop out as censoring). We used Kaplan–Meier survival analysis to determine the time to progression for the 10th, 50th, and 90th risk percentile. We first fitted a baseline model containing age, age2, sex, and age*sex as predictors. We then added PHS to the baseline model, and used log likelihood ratio to assess whether PHS significantly improved the prediction. Model comparisons between PHS and number of APOE ε4 alleles were also made (Baseline and APOE vs. Baseline, APOE and PHS). Thereafter, we examined the combined model of PHS and atrophy score at baseline, and performed model comparisons with each factor alone. Finally, we added baseline measure of MMSE to a three-factor model, and performed model comparisons among all two-factor models. Cross-validated prediction accuracy, sensitivity, specificity and area under the curve (AUC) were calculated via the receiver operator characteristics (ROC) analyses using the perfcurve function in Matlab (MathWorks). The assumption of proportional hazards was not violated for any of the included covariates (p's > 0.05, as evaluated by scaled Schoenfeld residuals using the cox.zph function in R).
To predict cognitive decline in patients with MCI, we used linear mixed-effects models to estimate change in MMSE or CDR-SB over 36 months. Mixed effects models were fitted via maximum likelihood by using the lmer function in R (version 3.2.3). Sex, age, education, and five genetic principal components to control for population stratification were included in all analyses as baseline variables. We included PHS, atrophy score and the combination of PHS and atrophy score in three different models each for prediction of change in CDR-SB and MMSE. The models allowed for random subject-specific intercept and slope. Model comparisons of APOE and APOE+PHS were performed, where APOE denotes the number of APOE ε4 alleles. Likelihood ratio test via ANOVA were used for all model comparisons.
Of the 336 participants with MCI at baseline, 182 developed AD within the follow-up period of 120 months. Baseline demographics of stable MCI (MCI-s) and MCI patients that subsequently progressed to AD (MCI-c) are presented in Table 1. The groups did not differ in sex distribution, age, or education. As expected, APOE ε4 alleles, MMSE, atrophy score, and PHS were related to subsequent progression.
Estimated survival functions for the 10th, 50th, and 90th percentile based on one-, two-, and three-factors cox proportional hazard models modeling time to progression from MCI to AD are shown in Figure 1 (Figure 1A, PHS, Figure 1B, PHS and atrophy score, Figure 1C, PHS, atrophy score, and MMSE), and model summaries are shown in Table 2. The PHS significantly predicted progression from MCI to AD over 120 months follow-up (p = 1.07e-5), and PHS was a significantly stronger predictor of progression than APOE ε genotype (p = 0.0152, for model comparison of APOE vs. APOE +PHS). When including atrophy score (McEvoy et al., 2009) in the model, PHS remained significant and the two-factor prediction model was significantly more predictive than either single-factor model (p's = 5.61e-11, and 0.0015 for comparison with single-factor models of PHS and atrophy score, respectively). Finally, we included cognitive functioning at baseline (MMSE) to a three-factor prediction model, which yielded a combined model p-value of 4.28e-17. Model comparisons showed that the three-factor model was significantly more predictive than the two-factor model (p < 0.005).
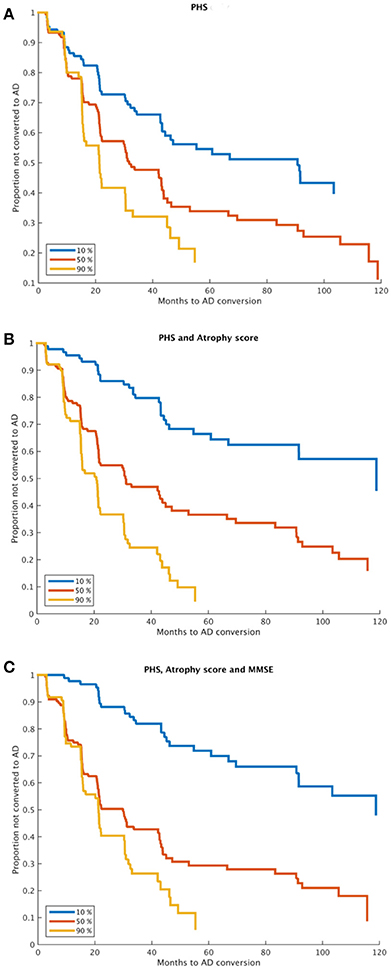
Figure 1. Time to MCI to AD progression. Kaplan-Meier survival curves for 10, 50, and 90th percentiles of (A) PHS, (B) PHS and atrophy score, and (C) PHS, atrophy score and MMSE (at baseline). Model comparisons using log likelihood of the two-factor model (B) vs. any one-factor model, and the three-factor model (C) vs. any combination of two-factor models; all p < 0.005. PHS, Polygenic Hazard Score; AD, Alzheimer's Disease.
ROC analyses were performed to assess performance accuracies for one-, two- and three-factor models for prediction of progression over a 36 months follow-up period based on combinations of atrophy score, MMSE, and PHS (Table 3). In brief, the atrophy score had an accuracy of 74.6, sensitivity of 77.8, and a specificity of 70.8. Adding PHS to the atrophy score increased specificity, at the cost of sensitivity; with increased overall accuracy and AUC (although confidence intervals overlapped). Similar results were seen for comparisons of MMSE alone and in combination with PHS. The full three-factor model had the highest AUC (.84), accuracy (78.9), sensitivity (79.9), and a specificity of 77.8.
Results from the linear mixed-effect models for prediction of change in MMSE and CDR-SB over 36 months are presented in Table 4. Model comparisons showed that PHS significantly improved prediction of both MMSE (χ2 = 26.7, df = 1, p = 2.34e-07) and CDR-SB (χ2 = 21.57, df = 1, p = 3.41e-06) compared to the baseline variables. Further, the PHS performed significantly better than APOE ε4 status in prediction of both MMSE (χ2 = 8.61, df = 1, p = 0.0033) and CDR-SB (χ2 = 6.12, df = 1, p = 0.013). Again, PHS remained significant after adding atrophy score to the model (Table 4). Compared to atrophy score alone, the combined model of PHS and atrophy score was significantly more predictive of change in both MMSE (χ2 = 19.04, df = 1, p = 1.281e-05, [controlling for APOE ε4 alleles: χ2 = 6.97, df = 1, p = 0.008]) as well as CDR_SB (χ2 = 13.43, df = 1, p = 0.00025 [controlling for APOE ε4 alleles: χ2 = 4.57, df = 1, p = 0.033]).
Using the ADNI dataset, we assessed the potential clinical utility of the recently established age-specific AD PHS (Desikan et al., 2017) to more accurately predict the progression to AD among patients diagnosed with MCI. Examining both time to AD diagnosis and decline in clinical scores (CDR-SB and MMSE), we found that PHS significantly predicted clinical progression to AD beyond APOE genotype. Critically, PHS remained a significant predictor even when regional brain atrophy levels and cognitive functioning was known, and the prediction models were significantly improved by adding PHS to models containing atrophy score and/or MMSE. These results show that the predictive value of PHS is, at least partly, independent of brain atrophy and cognitive functioning at the MCI stage. In a typical memory clinic setting, PHS may be used to assess AD risk before other diagnostics have been performed, and may also be valuable for further improvement of prediction after an individual has underwent an MRI examination.
We used two complementary approaches to assess clinical progression among MCI patients. First, we used survival analyses to assess time to progression from MCI to AD over a long period of 120 months, using combinations of PHS, MRI, and cognitive functioning (Figure 1). The PHS was a significant predictor both alone and when controlling for atrophy level and cognitive function at study start, and model comparisons showed significant model improvements when adding PHS to models consisting of atrophy score and/or MMSE. ROC analyses showed that adding PHS to atrophy score or MMSE improved prediction accuracy, which was primarily driven by increased specificity, but at the cost of lower sensitivity (Table 3). These results suggest that different combinations of biomarkers may be used in different clinical situations where higher sensitivity or specificity is prioritized. As expected, the best model performance was derived from the full three- factor model with PHS, MRI, and cognitive assessment.
Secondly, we used linear mixed-effect models to examine the influence of PHS on change in CDR-SB and MMSE over a shorter time period, 3 years, in the same individuals with MCI at baseline. In line with the results from survival analyses, PHS significantly predicted clinical decline of both CDR-SB and MMSE among elderly diagnosed with MCI beyond APOE status, both individually and when atrophy levels were included in the model (Table 4). Taken together, these results show the utility of the PHS to assess individual risk for clinical decline in patients diagnosed with MCI also when their current levels of brain atrophy and cognitive functioning is known.
Previous studies using both survival analyses and linear mixed effect models showed improved prediction of AD progression by combining MRI data with CSF biomarkers (Vemuri et al., 2009; Westman et al., 2012), APOE genotype (McEvoy et al., 2009; Dukart et al., 2015), and different cognitive test batteries (Callahan et al., 2015; Eckerström et al., 2015; Li et al., 2016). Investigators from our group have shown that the combination of cognitive performance and medial temporal atrophy substantially improves prediction of MCI to AD progression in comparison to prediction based on individual risk factors (Heister et al., 2011), and also that the combination of APOE genotype and brain atrophy outperforms models based on either variable alone (McEvoy et al., 2009). Here, we extend previous models based on APOE to our recently developed PHS based on whole-genome data. It is still not fully known through which mechanisms APOE and other genes with smaller effect impact AD risk, but brain atrophy level and cognitive function are considered intermediate phenotypes that may mediate genetic effects on AD risk. In our previous paper, we found a correlation between PHS and larger volume loss in AD-related brain areas (Desikan et al., 2017). The current findings that PHS is predictive of AD progression when levels of brain atrophy are included in the model, shows that MRI biomarkers are not fully mediating the effect of PHS. Prediction based on genetic testing has the advantages of being relatively cheap, non-invasive, and not time-sensitive (since genetic assessment only has to be carried out once, is valid for a whole life time and can be used for multiple clinical purposes). In contrast to polygenic risk scores developed in a case/control framework, PHS is focused on predicting age of onset, which more accurately captures the increase in population incidence with increased age, where older age is the strongest risk factor for AD development.
ADNI is one of the largest longitudinal dataset for studying progression from MCI to AD, but has limitations. First, participants were recruited from memory clinics and advertisements, and MCI inclusion criteria were highly selective, thus the study group is not representative of the general population. Further, AD diagnosis has not been confirmed with histopathology. Also, study dropouts are biased toward high-risk individuals, which might lead to a bias in the estimates of progression rates. As high-risk individuals are more likely to have a higher PHS, the predictive value of the PHS might be underestimated in this study.
The present study shows that the prediction of clinical progression to AD among MCI patients can be improved by combining the age-sensitive PHS with structural neuroimaging and baseline cognitive ability. Improved individual assessment of AD risk among elderly patients presenting with subjective memory complaints could be helpful in clinical practice to determine treatment plans, and is also of high importance for intervention studies where recruitment of high-risk individuals at an early stage of the disease process is crucial for testing effectiveness of new disease-altering interventions.
The ADNI study was approved by the local ethics committee at each center. All subjects gave written informed consent in accordance with the Declaration of Helsinki. For more information see ADNI webpage; http://adni.loni.usc.edu.
KK, CF, RD, and AD: designed the study; CF and KK: performed analyses; KK: wrote the manuscript; CF, LM, DH, CT, C-HC, OA, RD, and AD: read and provided comments on the manuscript.
LM holds equity in CorTechs Labs, Inc. AD is a founder of and holds equity in CorTechs Labs, Inc., and serves on its Scientific Advisory Board. He is also a member of the Scientific Advisory Board of Human Longevity, Inc. (HLI), and receives research funding from General Electric Healthcare (GEHC). The terms of these arrangements have been reviewed and approved by the University of California, San Diego in accordance with its conflict of interest policies. OA has a patent SYSTEMS AND METHODS FOR IDENTIFYING POLYMORPHISMS pending.
The other authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Data collection and sharing for this project was funded by the Alzheimer's Disease Neuroimaging Initiative (ADNI) (National Institutes of Health Grant U01 AG024904) and DOD ADNI (Department of Defense award number W81XWH-12-2-0012). ADNI is funded by the National Institute on Aging, the National Institute of Biomedical Imaging and Bioengineering, and through generous contributions from the following: AbbVie, Alzheimer's Association; Alzheimer's Drug Discovery Foundation; Araclon Biotech; BioClinica, Inc.; Biogen; Bristol-Myers Squibb Company; CereSpir, Inc.; Cogstate; Eisai Inc.; Elan Pharmaceuticals, Inc.; Eli Lilly and Company; EuroImmun; F. Hoffmann-La Roche Ltd and its affiliated company Genentech, Inc.; Fujirebio; GE Healthcare; IXICO Ltd.; Janssen Alzheimer Immunotherapy Research & Development, LLC.; Johnson & Johnson Pharmaceutical Research & Development LLC.; Lumosity; Lundbeck; Merck & Co., Inc.; Meso Scale Diagnostics, LLC.; NeuroRx Research; Neurotrack Technologies; Novartis Pharmaceuticals Corporation; Pfizer Inc.; Piramal Imaging; Servier; Takeda Pharmaceutical Company; and Transition Therapeutics. The Canadian Institutes of Health Research is providing funds to support ADNI clinical sites in Canada. Private sector contributions are facilitated by the Foundation for the National Institutes of Health (www.fnih.org). The grantee organization is the Northern California Institute for Research and Education, and the study is coordinated by the Alzheimer's Therapeutic Research Institute at the University of Southern California. ADNI data are disseminated by the Laboratory for Neuro Imaging at the University of Southern California. This research was also supported by NIH grants P30 AG010129 and K01 AG030514. KK was supported by a grant from the Swedish Research Council, OA by the Research Council of Norway and KG Jebsen Foundation, RD by the National Alzheimer's Coordinating Center Junior Investigator Award, RSNA Resident/Fellow Award Foundation and ASNR Alzheimer's Imaging Grant, and LM by the National Institute on Alcohol Abuse and Alcoholism (R01AA021187).
Alzheimer's Association, A. (2015). 2015 Alzheimer' s disease facts and figures. Alzheimer's Dement. 11, 332–384. doi: 10.1016/j.jalz.2015.02.003
Brewer, J. B. (2009). Fully-automated volumetric MRI with normative ranges: translation to clinical practice. Behav. Neurol. 21, 21–28. doi: 10.3233/BEN-2009-0226
Brewer, J. B., Magda, S., Airriess, C., and Smith, M. E. (2009). Fully-automated quantification of regional brain volumes for improved detection of focal atrophy in Alzheimer disease. AJNR Am. J. Neuroradiol. 30, 578–580. doi: 10.3174/ajnr.A1402
Callahan, B. L., Ramirez, J., Berezuk, C., Duchesne, S., and Black, S. E. (2015). Predicting Alzheimer's disease development: a comparison of cognitive criteria and associated neuroimaging biomarkers. Alzheimers Res. Ther. 7:68. doi: 10.1186/s13195-015-0152-z
Desikan, R. S., Fan, C. C., Wang, Y., Schork, A. J., Cabral, H. J., Cupples, L. A., et al. (2017). Genetic assessment of age-associated Alzheimer disease risk: development and validation of a polygenic hazard score. PLoS Med. 14:e1002258. doi: 10.1371/journal.pmed.1002258
Dukart, J., Sambataro, F., and Bertolino, A. (2015). Accurate prediction of conversion to Alzheimer's disease using imaging, genetic, and neuropsychological biomarkers. J. Alzheimers Dis. 49, 1143–1159. doi: 10.3233/JAD-150570
Eckerström, C., Olsson, E., Klasson, N., Berge, J., Nordlund, A., Bjerke, M., et al. (2015). Multimodal prediction of dementia with up to 10 years follow up: the gothenburg MCI study. J. Alzheimer's Dis. 44, 205–214. doi: 10.3233/JAD-141053
Folstein, M. F., Folstein, S. E., and McHugh, P. R. (1975). “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 12, 189–198. doi: 10.1016/0022-3956(75)90026-6
Heister, D., Brewer, J. B., Magda, S., Blennow, K., and McEvoy, L. K. (2011). Predicting MCI outcome with clinically available MRI and CSF biomarkers. Neurology 77, 1619–1628. doi: 10.1212/WNL.0b013e3182343314
Holland, D., McEvoy, L. K., Desikan, R. S., and Dale, A. M. (2012). Enrichment and stratification for predementia Alzheimer disease clinical trials. PLoS ONE 7:e47739. doi: 10.1371/journal.pone.0047739
Hughes, C. P., Berg, L., Danziger, W. L., Coben, L. A., and Martin, R. L. (1982). A new clinical scale for the staging of dementia. Br. J. Psychiatry 140, 566–572. doi: 10.1192/bjp.140.6.566
Klein, J. P., Houwelingen, H. C., Ibrahim, J. G., and Scheike, T. H. (eds.). (2013). Handbook of Survival Analysis. London: Chapman and Hall/CRC.
Lambert, J.-C., Ibrahim-Verbaas, C. A., Harold, D., Naj, A. C., Sims, R., Bellenguez, C., et al. (2013). Meta-analysis of 74,046 individuals identifies 11 new susceptibility loci for Alzheimer's disease. Nat. Genet. 45, 1452–1458. doi: 10.1038/ng.2802
Li, J.-Q., Tan, L., Wang, H.-F., Tan, M.-S., Tan, L., Xu, W., et al. (2016). Risk factors for predicting progression from mild cognitive impairment to Alzheimer's disease: a systematic review and meta-analysis of cohort studies. J. Neurol. Neurosurg. Psychiatry 87, 476–484. doi: 10.1136/jnnp-2014-310095
Marioni, R. E., Campbell, A., Hagenaars, S. P., Nagy, R., Amador, C., Hayward, C., et al. (2017). Genetic stratification to identify risk groups for Alzheimer's disease. J. Alzheimer's Dis. 57, 275–283. doi: 10.3233/JAD-161070
McEvoy, L. K., Fennema-Notestine, C., Roddey, J. C., Hagler, D. J., Holland, D., Karow, D. S., et al. (2009). Alzheimer disease: quantitative structural neuroimaging for detection and prediction of clinical and structural changes in mild cognitive impairment. Radiology 251, 195–205. doi: 10.1148/radiol.2511080924
McEvoy, L. K., Holland, D., Hagler, D. J., Fennema-Notestine, C., Brewer, J. B., and Dale, A. M. (2011). Mild cognitive impairment: baseline and longitudinal structural MR imaging measures improve predictive prognosis. Radiology 259, 834–843. doi: 10.1148/radiol.11101975
Querfurth, H. W., and LaFerla, F. M. (2010). Alzheimer's disease. N. Engl. J. Med. 362, 329–343. doi: 10.1016/B978-0-323-28047-1.00047-0
Ridge, P. G., Mukherjee, S., Crane, P. K., and Kauwe, J. S. K. (2013). Alzheimer's disease: analyzing the missing heritability. PLoS ONE 8:e79771. doi: 10.1371/journal.pone.0079771
Ritchie, C. W., Molinuevo, J. L., Truyen, L., Satlin, A., Van der Geyten, S., and Lovestone, S. (2016). Development of interventions for the secondary prevention of Alzheimer's dementia: the European prevention of Alzheimer's Dementia (EPAD) project. Lancet Psychiatry 3, 179–186. doi: 10.1016/S2215-0366(15)00454-X
Roberts, R., and Knopman, D. S. (2013). Classification and Epidemiology of MCI. Clin. Geriatr. Med. 29, 753–772. doi: 10.1016/j.cger.2013.07.003
Sabuncu, M. R., Buckner, R. L., Smoller, J. W., Lee, P. H., Fischl, B., and Sperling, R. A. (2012). The association between a polygenic Alzheimer score and cortical thickness in clinically normal subjects. Cereb. Cortex 22, 2653–2661. doi: 10.1093/cercor/bhr348
Tan, C. H., Fan, C. C., Mormino, E. C., Sugrue, L. P., Broce, I. J., Hess, C. P., et al. (2018). Polygenic hazard score: an enrichment marker for Alzheimer's associated amyloid and tau deposition. Acta Neuropathol. 135, 85–93. doi: 10.1007/s00401-017-1789-4
Tan, C. H., Hyman, B. T., Tan, J. J. X., Hess, C. P., Dillon, W. P., Schellenberg, G. D., et al. (2017). Polygenic hazard scores in preclinical Alzheimer's disease. Ann. Neurol. 82, 484–488. doi: 10.1002/ana.25029
Vemuri, P., Wiste, H. J., Weigand, S. D., Shaw, L. M., Trojanowski, J. Q., Weiner, M. W., et al. (2009). MRI and CSF Biomarkers in normal, MCL and AD subjects: predicting future clinical change. Neurology 73, 287–293. doi: 10.1212/WNL.0b013e3181af79e5
Westman, E., Muehlboeck, J. S., and Simmons, A. (2012). Combining MRI and CSF measures for classification of Alzheimer's disease and prediction of mild cognitive impairment conversion. Neuroimage 62, 229–238. doi: 10.1016/j.neuroimage.2012.04.056
Keywords: pHs, MCI, AD prediction, MRI, genetics
Citation: Kauppi K, Fan CC, McEvoy LK, Holland D, Tan CH, Chen C-H, Andreassen OA, Desikan RS, Dale AM and for the Alzheimer's Disease Neuroimaging Initiative (2018) Combining Polygenic Hazard Score With Volumetric MRI and Cognitive Measures Improves Prediction of Progression From Mild Cognitive Impairment to Alzheimer's Disease. Front. Neurosci. 12:260. doi: 10.3389/fnins.2018.00260
Received: 09 January 2018; Accepted: 04 April 2018;
Published: 30 April 2018.
Edited by:
Stefano L. Sensi, Università degli Studi G. d'Annunzio Chieti e Pescara, ItalyReviewed by:
Stefano Delli Pizzi, Università degli Studi G. d'Annunzio Chieti e Pescara, ItalyCopyright © 2018 Kauppi, Fan, McEvoy, Holland, Tan, Chen, Andreassen, Desikan, and Dale for the Alzheimer's Disease Neuroimaging Initiative. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Karolina Kauppi, a2Fyb2xpbmEua2F1cHBpQHVtdS5zZQ==
Anders M. Dale, YW1kYWxlQHVjc2QuZWR1
†Data used in preparation of this article were obtained from the Alzheimer's Disease Neuroimaging Initiative (ADNI) database (adni.loni.usc.edu). As such, the investigators within the ADNI contributed to the design and implementation of ADNI and/or provided data but did not participate in analysis or writing of this report. A complete listing of ADNI investigators can be found at: http://adni.loni.usc.edu/wp-content/uploads/how_to_apply/ADNI_Acknowledgement_List.pdf
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.