
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Hum. Neurosci. , 16 February 2023
Sec. Cognitive Neuroscience
Volume 17 - 2023 | https://doi.org/10.3389/fnhum.2023.990581
This article is part of the Research Topic Frontiers in Psychodynamic Neuroscience View all 18 articles
Introduction: A new line of insomnia research focuses on the developmental trajectories from early live stress to insomnia in adulthood. Adverse childhood experiences (ACE’s) might create a vulnerability for later maladaptive coping with distress, as seen in chronic hyperarousal or insomnia. In an functional magnetic resonance imaging (fMRI) study, failure to dissociate the neurobiological components of shame from autobiographical shameful memories in insomnia was reflected by continued activation of the dorsal anterior cingulate cortex (dACC), which may be a result of maladaptive coping in the wake of ACE’s. Following up on that study, the current pilot study explores the relation between ACE’s, shame coping-styles, adult insomnia, hyperarousal, and neurobiology of autobiographical memory.
Methods: We used existing data (N = 57) from individuals with insomnia (N = 27) and controls (N = 30), and asked these participants to complete the childhood trauma questionnaire (CTQ). Two structural equation models were used to test the hypotheses that shame-coping styles and insomnia symptom severity mediate the association between ACE’s and (1) self-rated hyperarousal symptoms and (2) dACC activation to recall of autobiographical memories.
Results: For the association between ACE’s and hyperarousal, there was a significant mediation of shame-coping style (p < 0.05). This model also indicated worse shame coping with more ACE’s (p < 0.05) and worse insomnia symptoms with more ACES’s (p < 0.05), but no association between shame coping and insomnia symptoms (p = 0.154). In contrast, dACC activation to recall of autobiographical memories could only be explained by its direct association with ACE’s (p < 0.05), albeit that in this model more ACE’s were also associated with worse insomnia symptoms.
Discussion: These findings could have an implication for the approach of treatment for insomnia. It could be focused more on trauma and emotional processing instead of conventional sleep interventions. Future studies are recommended to investigate the relationship mechanism between childhood trauma and insomnia, with additional factors of attachment styles, personality, and temperament.
Adverse childhood experiences (ACEs) have a devastating effect on adult emotional functioning, especially if the ACEs are multiple, leading to higher risks for depressive illness, anxiety, addiction, suicidality, and medical illness (DeBellis, 2010). ACEs are negative experiences, such as emotional abuse or neglect, physical abuse or neglect, sexual abuse, and exposure to parental substance abuse, mental illness, or criminal behavior (Felitti et al., 1998). Other than traumatic situations, such as a car accident, a landslide, or war, ACEs are often inflicted by the caretakers, who in their position were expected to protect and regulate the emotions of the child. In psychoanalytic practice, we see patients with ACEs struggling with a chronic state of hyperarousal (Van der Kolk, 2014) and relationship anxiety (Morrison, 1989; Dorahy et al., 2016, 2017). Their self- and emotion-regulation strategies are limited, as they have internalized dysregulating caretakers that have been a threat to self-cohesion (DeYoung, 2015). Hyperarousal causes a collapse of reflective functioning; emotion and affects are no longer experienced as temporary (conscious and verbal) feeling states but as states reflecting identity (Fonagy et al., 2002). Thus, feelings, such as guilt and shame are experienced as “I am a bad person,” which reflects an equivalent mode of functioning (Allen et al., 2006).
Hyperarousal can be described not only by the above psychological factors but also by the physiological processes involved in arousal, including increased high-frequency electroencephalography (EEG) activity, hormone secretion (e.g., cortisol), limbic brain metabolism, and sympathetic activation (Riemann et al., 2010). Importantly, hyperarousal is considered one of the primary risk factors for the development of mental health problems.
In a series of papers reviewed below, we studied the relationship between hyperarousal and shameful memories from the past in patients suffering from insomnia. Following up on these papers, in the research presented here, we aim to further explain hyperarousal and shame coping by examining more severe negative experiences faced in childhood. We studied the mediating effect of shame coping and insomnia on ACEs and hyperarousal.
A first factor that links ACEs to hyperarousal may be maladaptive shame coping styles. Clinically, a distinction is made between adaptive and maladaptive shame. The former refers to bypassing feelings of shame, which contribute to adaptive self-esteem regulation and social communication (Schalkwijk et al., 2016). The latter is characterized by maladaptive thoughts or behaviors referring to negative self-esteem, and a desire to hide or escape, and is experienced as a negative feeling threatening identity (Luyten et al., 2002). ACEs negatively influence the development of a child’s identity. Often, the sense of self is threatened and the child questions his or her role in these experiences, such as “Who am I, when they can do this to me?” (Lewis, 1971; Tracy et al., 2007; Lichtenberg et al., 2011; Schalkwijk, 2012). Usually, the personality of persons with many ACEs is characterized by feelings of shame, powerlessness, and lack of a sense of agency (Lanius et al., 2020). When circumstances are chronically unfavorable, as in the case of many ACEs, a child’s personality is characterized by maladaptive shame-coping strategies. The shame manifests either as blame for their shortcomings (internalizing) or attributing blame to others (externalizing), which can lead to hyperarousal (Wassing et al., 2016) and mental health disorders (Campbell, 2016).
A second factor linking ACEs to hyperarousal is insomnia (Bader et al., 2007), which is a sleep disorder characterized by hyperarousal (Riemann et al., 2010) and is in itself a primary risk factor for the development of mental health problems (Manber et al., 2008; Baglioni et al., 2011; Christensen et al., 2016; Blom et al., 2017; Hertenstein et al., 2019). Bader et al. (2007) found that 46% of the participants with insomnia reported moderate to severe ACEs, and the number of ACEs has been found to be proportional to the severity of insomnia (Wang et al., 2016). Furthermore, Kajeepeta et al. (2015) found evidence of an association between witnessing family conflict and sexual abuse, and insomnia. Moreover, more ACEs have been linked to disturbed rapid eye movement (REM) sleep in adulthood (Insana et al., 2012), which is a consistent marker not only of insomnia but also of other mental health disorders (Germain et al., 2008; Riemann et al., 2012; Pesonen et al., 2019).
Concerning these possible mediation effects between ACEs and hyperarousal, genome-wide association studies followed up by functional annotation analysis suggest strong correlations between the expression of insomnia risk genes, psychiatric traits, and the limbic circuitry (Jansen et al., 2019). Furthermore, a recent systematic review presented consistent findings of altered epigenetic modifications of the glucocorticoid gene NRC31 in adults exposed to ACEs (Lang et al., 2020), which is in line with persistent changes in the function of the hypothalamic-pituitary axis observed in mental health disorders (Griffiths and Hunter, 2014). Importantly, patients with insomnia do not necessarily have increased emotional reactivity to novel experiences, i.e., they do not show stronger initial emotional responses. A recent study with 25,758 participants of the United Kingdom Biobank showed no association between insomnia symptoms and limbic brain activation during an emotional task (Schiel et al., 2022). However, the differences from regular sleepers become evident after sleeping (Wassing and D’Rozario, 2022). Following a night with disturbed REM sleep, patients with insomnia show continued emotional reactivity, which may last for months or even years, and could explain a chronic hyperarousal state (Wassing et al., 2016). It has been proposed that adaptive emotion regulation depends on sound REM sleep (Walker, 2009; Walker and Van der Helm, 2009). During REM sleep, a selective memory consolidation process may support the disengagement of the emotional limbic and salience brain networks. Wassing et al. (2019a) found support for the hypothesis that maladaptive sleep in insomnia perturbs overnight emotion regulation and may contribute to chronic hyperarousal (Wassing et al., 2016). Wassing et al. (2019b) also found support for the hypothesis that chronic hyperarousal in insomnia disorder is associated with the failure to dissociate the limbic circuitry from long-term memory traces. Patients with insomnia who recalled autobiographical shameful memories showed stronger blood-oxygen-level-dependent (BOLD) responses in the dorsal anterior cingulate cortex (dACC), which is part of the limbic and salience circuitry. Recall of adverse emotional memories also activates the dACC in patients with post-traumatic stress disorder (PTSD; Whalley et al., 2013). PTSD can be conceptualized as a disorder of impaired fear-extinction memory, and delayed acquisition of the fear-extinction memory is linked with continued activation of the dACC (Seo et al., 2018). The dACC, otherwise known as the mid-cingulate cortex, has predominant connections with the amygdala, striatum, and dopaminergic and serotonergic systems, and is functionally linked with evaluating prediction errors, updating memory schema, and adapting/persisting behavioral responses (Kolling et al., 2016; van Heukelum et al., 2020). Considering these findings, we aimed to identify the dACC as the neurobiological expression of hyperarousal. Since the dACC is most consistently shown to be involved in emotional memory tasks in insomnia and PTSD populations (Whalley et al., 2013; Seo et al., 2018; Wassing et al., 2019b) we limited our analyses to the dACC and not to other nodes of the salience or limbic network.
Following this line of research, in this exploratory study, we asked ourselves where the vulnerability for hyperarousal and aberrant neurobiology of autobiographical memory in people with insomnia might originate. Could ACEs lead to the vulnerability of insomnia by weakening the stress regulatory processes?
To the best of our knowledge, this is the first exploratory study that investigated the relationship between ACEs, maladaptive shame coping, insomnia, hyperarousal, and dACC activation in the recall of autobiographical memories. In order to evaluate these relationships, we employed structural equation modeling with one direct and two parallel mediation paths so that all covariance between the variables of the hypothesized paths could be fitted to the observed data at once. We used two structural equation models to test the hypotheses that shame-coping styles and insomnia symptom severity mediate the association between ACEs and (1) self-rated hyperarousal symptoms, and (2) dACC activation in recalling autobiographical memories. Furthermore, we expected that more ACEs would result in worse maladaptive shame-coping styles and insomnia severity.
The 57 participants in this study were described by Wassing et al. (2019b). These participants included 27 patients that fulfilled the diagnostic criteria for insomnia disorder [mean, standard deviation (SD) age, 45.5 (13.4) years; 10 men; ISI range 8–26] and regular sleepers [n = 30; mean [SD] age, 42.4 (15.8) years; 17 men, ISI range 0–14]. The participants answered the self-report questionnaires approximately 1 week before the functional magnetic resonance imaging (fMRI) scan.
Since the childhood trauma Questionnaire (CTQ) (Bernstein et al., 2003) was not part of this dataset established in 2015–2016, in February 2021 we asked these participants to complete the CTQ, and 44 participants responded (77%, n = 23 patients with insomnia, n = 21 regular sleepers).
This study was approved by the Ethical Committee of the Department of Education of the University of Amsterdam (approval number 3421). Written informed consent was obtained from the participants prior to enrollment in the study.
Adverse childhood experiences were assessed using the Dutch version of the CTQ (Bernstein et al., 1997; Thombs et al., 2009; Spinhoven et al., 2014). It consists of 25 items rated on a five-point Likert scale (1 = never true, 5 = very often true) and measures five categories of trauma: emotional abuse, physical abuse, sexual abuse, physical neglect, and emotional neglect. An example of a physical neglect item is “During my childhood… I had to wear dirty clothes.” The CTQ demonstrated a Cronbach’s alpha of 0.95 for the total scale. The Cronbach’s alpha for the subscales were 0.91 for physical abuse, 0.89 for emotional abuse, 0.95 for sexual abuse, 0.63 for physical neglect, and 0.91 for emotional neglect.
Coping with shame was assessed using the Compass of Shame Scale (CoSS) (Elison et al., 2006; Schalkwijk et al., 2016). This self-report questionnaire consists of 15 shame-inducing situations and six answer categories. The participants were asked about their reaction to a situation, such as “When an activity makes me feel like my strength or skill is inferior,” and a reaction, such as “I get mad at myself for not being good enough,” on a five-point Likert scale (1 = never, 5 = almost always). This scale measures two maladaptive shame-coping styles: internalizing and externalizing. Internalizing shame coping contains answers in which the person blames himself or herself for being ashamed (“I brood over my flaws”) or the person avoids the shame-provoking situation (“I want to disappear”). Externalizing shame coping includes items in which the person blames others for feeling shame (“I get irritated with other people”) or denies that the situation evokes shame (“I act as if it isn’t so”). Two other categories assess adaptive shame coping (“I think, that was stupid of me, but that’s what happens to everyone”) and proneness to experience shame (“I am ashamed”). The Cronbach’s alpha for the subscales were as follows: avoidance, 0.75; attack other, 0.76; attack self, 0.86; withdrawal, 0.75; adaptive, 0.78; and shame proneness, 0.87.
Insomnia symptom severity was assessed using the Insomnia Severity Index (ISI), a self-report measure used to assess the nature, severity, and impact of insomnia (Bastien et al., 2001). A five-point Likert scale was used (0 = no problem, 4 = severe problem), with a total score ranging from 0 to 28. An example item is “Please rate the current SEVERITY of your insomnia problems: difficulty falling asleep.” The ISI demonstrated a Cronbach’s alpha of 0.76.
Hyperarousal was assessed using the Hyperarousal Scale (HS; Pavlova et al., 2001), a self-report questionnaire consisting of 26 items in the form of statements. Participants judged the statements using four different responses (0 = not at all, 1 = a little, 2 = quite a bit, and 3 = extremely). An example item is “I keep thinking about things long after they happened.” The HS demonstrated a Cronbach’s alpha of 0.81 (Bruno et al., 2020). Note that two out of the 26 items overlap with those in the ISI: “I am slow to awaken in the mornings” (HS) may be anticorrelated with “problems waking up too early” (ISI), and “I have trouble falling asleep” (HS) is likely to be correlated with “difficulty falling asleep” (ISI).
The dACC BOLD responses to shameful experiences were obtained during fMRI recordings. For a detailed description of the procedures, functional and structural MRI acquisition, data processing, and statistical analysis see Wassing et al. (2019b). In summary, 1 week prior to the fMRI scan, participants were asked to think of up to ten shameful past experiences, and for each to write down four cue words that, when prompted, allowed them to recall and relive the experience. In addition, for each shameful experience, participants were instructed to also write four cue words for neutral events from the same period (e.g., traveling to work/school). During the fMRI scan, the cue words of each of the experiences were presented on the screen for 16 s. A total of 10 blocks of shameful conditions and 10 blocks of neutral conditions were presented in pseudorandom order. The raw fMRI data were preprocessed using FMRIB Software Library (FSL)1 including corrections for inhomogeneities in the B0-field, motion correction using registration and independent component analysis with automatic removal of motion artifacts (ICA-AROMA) (Pruim et al., 2015), spatial smoothing (5 mm full width at half maximum kernel), grand-mean intensity normalization, nuisance signal regression (from cerebrospinal fluid and white-matter brain masks), and temporal high-pass filtering (1/90 Hz). The mean dACC activation for each participant was obtained using linear regression models in FSL FMRI Expert Analysis Tool (FEAT) (Woolrich et al., 2001) including a contrast on the regressors (shameful vs. neutral) and a mask of the dACC obtained in Wassing et al. (2019b).
The hypotheses were tested using structural equation modeling in R (version 4.1.2, R Foundation, Vienna, Austria) and RStudio (2022.02.3 Build 492) using the lavaan package (R Core Team, 2021). Structural equation modeling is a statistical approach that combines confirmatory factor analysis to extract latent variables from observed variables with regression analysis to estimate and evaluate the statistical significance of hypothesized paths. Instead of performing separate linear models per path, the technique uses the multivariate covariance structure of the observed data to fit the model all at once. We employed two models, one with self-rated hyperarousal as the outcome measure, and one for dACC reactivity to recall autobiographic memories. Path coefficients were obtained using maximum likelihood estimators and considered significant at a two-sided alpha threshold of 0.05. Finally, full mediation was indicated by a significant mediation path estimate in combination with a non-significant direct path estimate between ACES and the outcome variable. A partial mediation was indicated if both the direct path estimate and the mediation path estimate were significant.
The measurement model included four latent variables: (1) “ACES” were measured by the observed scores on the CTQ subscales of emotional neglect, physical neglect, emotional abuse, physical abuse, and sexual abuse; (2) “shame” was measured by the CoSS subscales of shame-proneness, adaptive shame coping, and internalizing and externalizing maladaptive coping; (3) “insomnia” was directly measured by the ISI total score; and (4) “hyperarousal” was directly measured by the hyperarousal-scale total score. The regression model included three equations, all of which included age and sex as confounders. First, shame was predicted by ACEs. Second, insomnia was predicted by ACEs and shame. Third, hyperarousal was predicted by ACES, shame, and insomnia scores. No moderating effects were considered. Mediation path estimates were computed where shame, insomnia, and both shame and insomnia mediated the association between ACEs and hyperarousal.
This structural equation model was similar to the one described in the previous subsection, except that the “hyperarousal” latent variable was replaced with the dACC BOLD responses for relived shameful experiences. Note that the path estimates in the two models between the same variables (e.g., ACEs to insomnia) could be different because the variance explained in ACEs by hyperarousal (model 1) was different from its variance explained by dACC BOLD responses (model 2). This means that the remaining variance in ACEs that was not explained by the outcome variable but was explained by insomnia could be different too.
The mean and SD values of the five CTQ subscales are shown in Table 1. Each subscale contained five question items, and their scores ranged from 5 to 25. Sexual abuse had the lowest mean score (M = 5.27), close to the lowest possible score. Emotional neglect had the highest mean score (M = 12.16), which was half of the highest possible subscale score.
The correlations between observed variables are shown in Figure 1. Concerning the CTQ subscales, the ISI total score was correlated with emotional abuse (r = 0.34, p < 0.03), physical neglect (r = 0.40, p < 0.007), and emotional neglect (r = 0.33, p < 0.03). Emotional abuse was also correlated with shame proneness (r = 0.31, p < 0.04), physical neglect with maladaptive externalizing shame coping (r = 0.34, p < 0.03), and emotional neglect was correlated with both shame proneness (r = 0.34, p < 0.03) and maladaptive externalizing shame coping (r = 0.31, p < 0.05). Most CTQ subscales were not associated with hyperarousal or dACC responses to reliving shameful experiences. Only emotional neglect correlated significantly with hyperarousal (r = 0.30, p < 0.05), and emotional abuse with dACC responses to reliving shameful experiences (r = 0.46, p < 0.002).
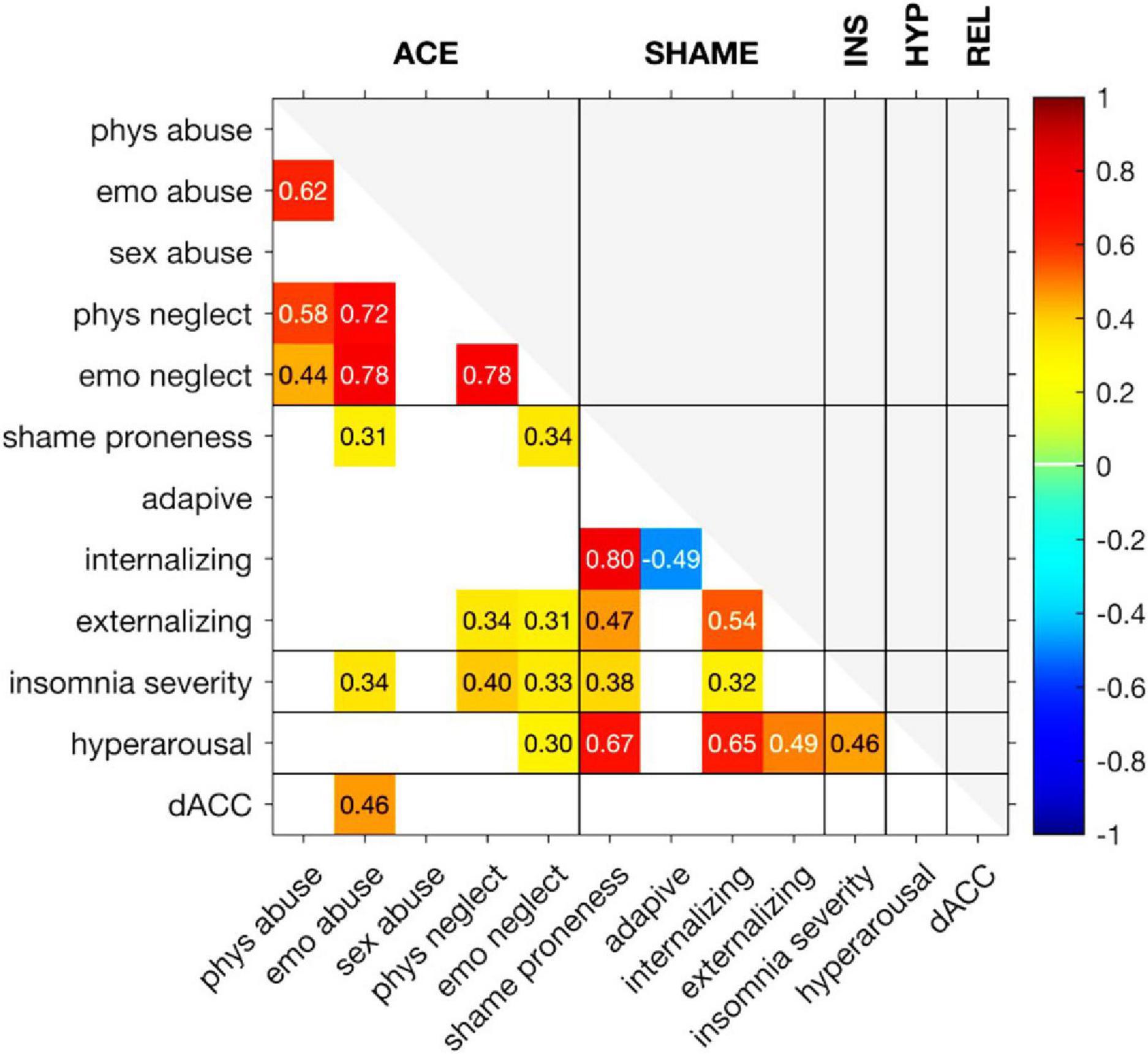
Figure 1. Correlation between observed variables. The color indicates the strength of the correlation. Only correlations with p-value below 0.05 are shown. Abbreviations from left upwards to left downwards: physical abuse, emotional abuse, sexual abuse, physical neglect, emotional neglect, shame proneness, adaptive shame coping, internalizing shame coping, externalizing shame coping, insomnia severity, hyperarousal, and dorsal anterior cingulate cortex. Abbreviations from left upward to right upward: adverse childhood experiences (ACEs), Shame, Insomnia Severity (INS), Hyperarousal (HYP), reliving shameful experiences (REL).
Concerning the CoSS subscales, shame proneness was correlated with the ISI total score (r = 0.38, p < 0.02) and hyperarousal (r = 0.67, p < 10–6). In addition, maladaptive internalizing shame coping was correlated with the ISI total score (r = 0.32, p < 0.04) and hyperarousal (r = 0.65, p < 10–5). Finally, maladaptive externalizing shame coping was correlated with hyperarousal (r = 0.49, p < 0.001).
The ISI total score was correlated with hyperarousal (r = 0.46, p < 0.002).
All the model-fit indices combined indicated a satisfactory to a good fit. The Root Mean Square Error of Approximation (RMSEA) was 0.09 (p = 0.14; the null hypothesis that the RMSEA was less than or equal to 0.05, could not be rejected, indicating a good fit). However, the discrepancy between the observed and fitted covariance matrices was barely significant (χ2(56) = 74.7, p = 0.048). The sample-size insensitive metrics also indicated a satisfactory to a good fit, that is, the comparative fit index = 0.92 (good) and the Tucker–Lewis index = 0.89 (satisfactory > 0.90). The factor loadings of the observed variables on the latent variables are shown in Figure 2. Of note, sexual abuse was loaded onto the ACES latent variable with trend-level significance (p = 0.09). The structural equation model for hyperarousal is shown in Figure 2.
Adverse childhood experiences did not directly predict hyperarousal (p = 0.98), but there were significant associations between ACEs and shame [β (SD) = 0.05 (0.02), standardized β = 0.33, Z = 2.08, p < 0.04] and ACEs and insomnia [β (SD) = 0.58 (0.24), standardized β = 0.36, Z = 2.42, p < 0.02]. However, insomnia was not predicted by shame (p = 0.17). Hyperarousal was predicted by shame [β (SD) = 7.30 (1.42), standardized β = 0.65, Z = 5.15, p < 10–6] and insomnia [β (SD) = 0.21 (0.11), standardized β = 0.22, Z = 1.96, p < 0.05]. The combined path estimate from ACEs via insomnia to hyperarousal was not significant [β (SD) = 0.12 (0.08), standardized β = 0.08, Z = 1.50, p = 0.13]. Finally, the combined path estimate from ACEs via shame to hyperarousal was significant [β (SD) = 0.33 (0.17), standardized β = 0.21, Z = 1.98, p < 0.05], indicating that the association between ACEs and hyperarousal was fully mediated by shame.
All model-fit indices combined indicated a good fit. The RMSEA was 0.06 (p = 0.39), and there was no significant discrepancy between the observed and fitted covariance matrices (χ2(56) = 64.9, p = 0.20). The comparative fit index (0.95) and Tucker–Lewis index (0.94) also indicated a good fit.
Adverse childhood experiences directly predicted the dACC responses to relived experiences [β (SD) = 0.07 (0.03), standardized β = 0.39, Z = 2.38, p < 0.02]. Furthermore, while ACEs did not predict shame in this model (p = 0.12), ACES did predict insomnia [β (SD) = 0.62 (0.24), standardized β = 0.38, Z = 2.62, p < 0.01], although insomnia was not predicted by shame (p = 0.15). Finally, there were no associations between dACC responses to relived experiences and shame (p = 0.85) or insomnia (p = 0.82), which also indicated that no mediation paths were significant (p > 0.82). The structural equation model for dACC reactivity to recall autobiographical memories is shown in Figure 3.
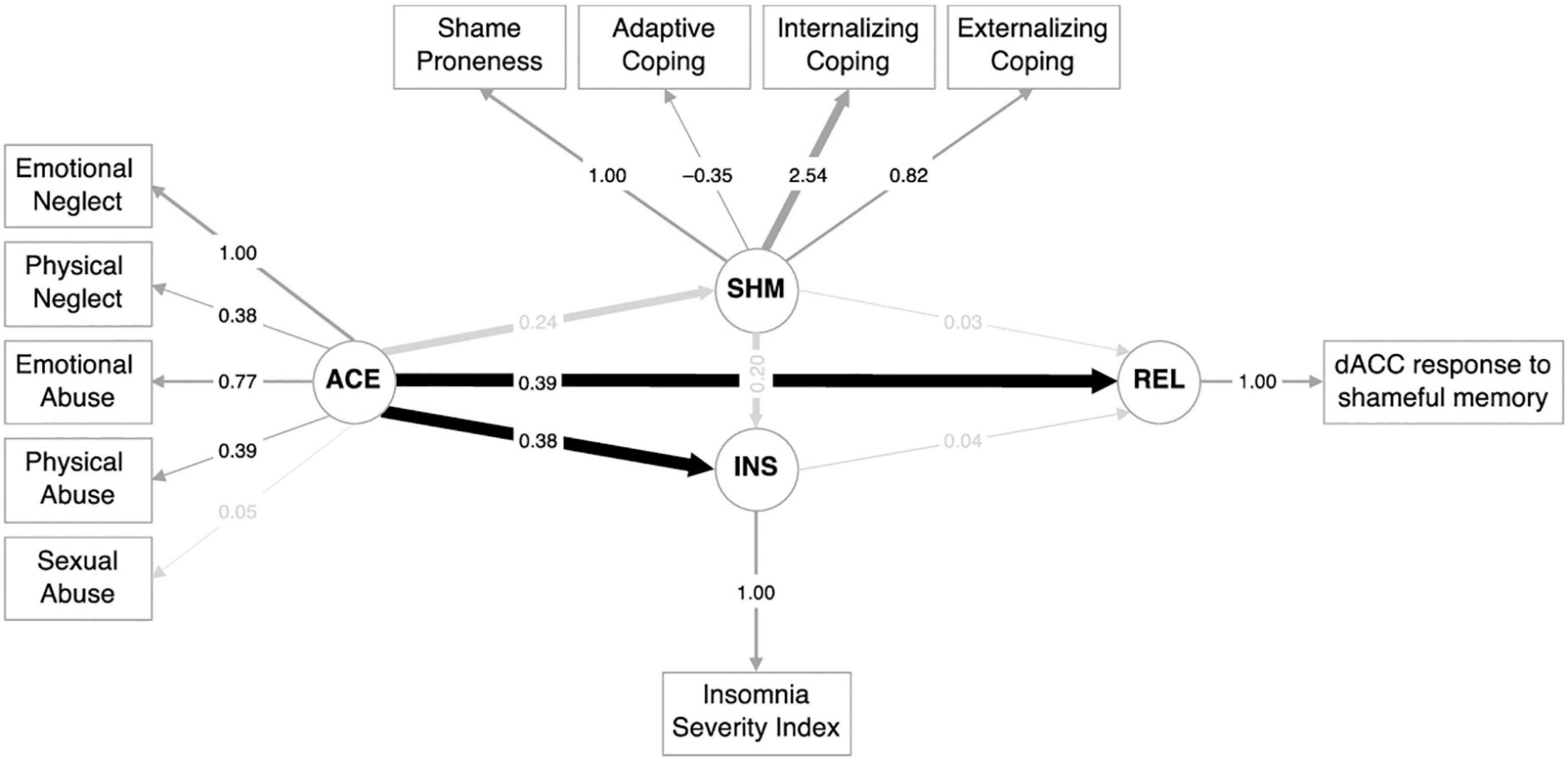
Figure 3. Structural equation model for dorsal anterior cingulate cortex (dACC) reactivity to recall of autobiographical memories.
This exploratory study investigated the mediating effect of dysfunctional shame regulation strategies and insomnia between ACES and emotionally experienced chronic hyperarousal, and its potential neurobiological underpinnings.
Our main interest in this study was the mediating effect of dysfunctional shame regulation strategies and insomnia between ACEs and emotionally experienced chronic hyperarousal and dACC responses to reliving shameful experiences. The bivariate correlation structure showed that, from the five groups of ACEs, emotional neglect seemed to have the most impact on hyperarousal and emotional abuse on dACC responses to reliving shameful experiences. Indeed, emotional abuse and neglect have been linked with the most long-term detrimental effects (Strathearn et al., 2020). Clinically speaking, maladaptive shame regulation strategies have been developed. Note that in this first structural equation model, insomnia did not significantly mediate the association between ACEs and hyperarousal, whereas indeed a significant mediation effect was found for maladaptive shame coping styles.
In the second structural equation model, our interest was the mediating effect of dysfunctional shame regulation strategies and insomnia between ACEs and the dACC response to reliving shameful memories. In contrast to the first model, we found no mediational effects for maladaptive shame regulation, nor for insomnia symptom severity. In a study by Wassing et al. (2019b), the insomnia patients, but not the controls, demonstrated dACC responses to the shame-inducing recall of autobiographical memories. In the current study, we now show that more ACEs relate to more severe insomnia symptoms and that insomnia severity did not mediate the association between ACEs and dACC responses. This may indicate that ACEs independently contribute to dACC responses when recalling shameful experiences. According to Van der Kolk’s (2014) book title, the body does keep score of these events leading to hyperarousal. Our findings support the importance of explicitly addressing the component of shame in ACEs during treatment.
Secondly, we discuss the bivariate correlation structure reported in Figure 1. Here we analyzed the premise that more ACEs lead to increased insomnia (Bader et al., 2007; Wang et al., 2016; Muscatello et al., 2020; Reffi et al., 2022). This was confirmed: having experienced more ACEs was predictive of insomnia severity in adults. However, this was found merely for the ACEs of emotional neglect, emotional abuse, and physical neglect. Differently from what happens with ACEs that include physical intrusions, such as sexual or physical abuse, other types of ACEs, such as emotional neglect, emotional abuse, and physical neglect, may go unnoticed as a child may never address or voice these experiences. In these cases, children tend to react physically and emotionally to these experiences with maladaptive coping strategies. Prior work has shown that emotional abuse and neglect can have the most detrimental effects long term (DeBellis, 2010). These kinds of ACEs are associated with much more adverse outcomes in areas of cognition and education, psychological and mental health, addiction and substance use, and sexual and physical health than the physically intrusive ACEs (Strathearn et al., 2020). In our study, we showed the association between maladaptive shame regulation strategies and experiencing a subjective state of chronic hyperarousal (Schore, 2003; Porges, 2011). Sexual and physical abuse, however, is associated with the violation of body integrity, which is a far more obvious violation for a child to notice and these might lead to other coping strategies. A typical outcome of sexual abuse is lifelong PTSD and depression (Strathearn et al., 2020), dissociation (Draijer and Langeland, 1999; Dorahy et al., 2017; Vonderlin et al., 2018; Nicolai, 2020; Voestermans et al., 2021), and self-destructive behavior. Dissociation protects the individual from experiencing the painful emotions experienced during the abuse, such as physical pain, shame, disgust, and helplessness. Also, there is no sexual abuse without neglect (Draijer, 1990). In other words, ACEs seldom take place alone.
This pilot study has several limitations. The number of participants was small and they were recruited based on insomnia rather than trauma. Therefore, those who were physically and sexually abused probably were underrepresented in our sample and the distribution of male and female participants was uneven. Another limitation was caused by the psychological effect of chronic arousal mentioned in the introduction. We have discussed that chronic hyperarousal hampers reflective functioning and people have limited capacity for recognizing (conscious and verbal) feeling states. Feelings cannot be differentiated or reflected upon, so feelings of shame, guilt, and anxiety end up confirming the cognition of preconceived notions, such as that the individual who suffered ACESs is bad, stupid, and disgusting. The found effect of ACEs on chronic hyperarousal might thus be underreported, as people have difficulties in reflecting on their (conscious and verbal) feeling states.
A few recommendations are suggested from this study. A larger sample from a variety of clinical institutions would better represent a population with insomnia. In addition, future research should consider that adult survivors of childhood abuse have different trajectories leading to insomnia (Steine et al., 2019). For example, another interesting mediating variable might be attachment style, as research has shown that shame and hyperarousal are associated implicitly with attachment styles, the way people engage in close and intimate relationships (Van der Kolk, 2014). Sedighimornani et al. (2021) found that shame was positively and significantly associated with insecure, fearful, and anxious attachment styles, whereas individuals with a secure attachment style had lower levels of shame (Gross and Hansen, 2000). A clinical example of the relationship between shame and unresolved and entangled attachment is found in borderline personality disorder (BPD). BPD is characterized by higher levels of baseline emotional intensity for guilt, shame, and fear, and higher levels of shame reactivity (Di Bartolomeo et al., 2022; Estric and Lopez-Castroman, 2022). A “chicken-and-egg” discussion is still ongoing concerning the relationship between attachment and temperament, another possible mediating variable (Hong and Park, 2012). Concerning the Big Five personality traits, e.g., high levels of neuroticism are associated with high levels of experiencing shame, whereas high levels of extraversion are associated with less shame (Erden and Akbag, 2015). Palagini et al. (2018) found that, in turn, insecure attachment in patients with insomnia has been associated with hyperarousal, pre-sleep hyperarousal, and emotion dysregulation. Therefore, clinically, we would expect shame and insomnia of having a mediating role between ACES and insecure attachment.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Universiteit van Amsterdam. The patients/participants provided their written informed consent to participate in this study.
FS, EV, and RW contributed equally to this research. JU participated as a graduate student. NN as a clinical expert. All authors contributed to the article and approved the submitted version.
This work was supported by the ZONMW Neuropsychoanalysis Fund Grant 16.561.0001 (to FS and EV), and VICI Grant 453.07.001 (to EV), all part of the Netherlands Organization of Scientific Research (NWO); by the Grant 253/2012 of the Bial Foundation (to EV); by the European Research Council Grants ERC-ADG-2014–671084 INSOMNIA and ERC-2016-PoC-737634 INSOMNIA BEAT IT (to EV), and the Australian National Health and Medical Research Council Investigator Grants GNT1196636 (to RW).
We thank Dr. A. Lam for providing helpful comments on the description of the statistical methodology.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Allen, J. G., Fonagy, P., and Bateman, A. W. (2006). Handbook of mentalization-based treatment. Chichester: Wiley. doi: 10.1002/9780470712986
Bader, K., Schäfer, V., Schenkel, M., Nissen, L., and Schwander, J. (2007). Adverse childhood experiences associated with sleep in primary insomnia. J. Sleep Res. 16, 285–296. doi: 10.1111/j.1365-2869.2007.00608.x
Baglioni, C., Battagliese, G., Feige, B., Spiegelhalder, K., Nissen, C., Voderholzer, U., et al. (2011). Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J. Affect. Disord. 135, 10–19. doi: 10.1016/j.jad.2011.01.011
Bastien, C. H., Vallières, A., and Morin, C. M. (2001). Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2, 297–307. doi: 10.1016/s1389-9457(00)00065-4
Bernstein, D. P., Ahluvalia, T., Pogge, D., and Handelsman, L. (1997). Validity of the childhood trauma questionnaire in an adolescent psychiatric population. J. Am. Acad. Child Adolesc. Psychiatry 36, 340–348. doi: 10.1097/00004583-199703000-00012
Bernstein, D. P., Stein, J. A., Newcomb, M. D., Walker, E., Pogge, D., Ahluvalia, T., et al. (2003). Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 27, 169–190. doi: 10.1016/s0145-2134(02)00541-0
Blom, K., Jernelöv, S., Rück, C., Lindefors, N., and Kaldo, V. (2017). Three-year follow-up comparing cognitive behavioral therapy for depression to cognitive behavioral therapy for insomnia, for patients with both diagnoses. Sleep 40:zsx108. doi: 10.1093/sleep/zsx108
Bruno, A., Rizzo, A., Muscatello, M., Celebre, L., Silvestri, M., Zoccali, R., et al. (2020). Hyperarousal scale: Italian cultural validation, age and gender differences in a nonclinical population. Int. J. Environ. Res. Public Health 17:1176. doi: 10.3390/ijerph17041176
Campbell, J. S. (2016). Development of the military compass of shame scale. Milit. Behav. Health 4, 159–167. doi: 10.1080/21635781.2015.1133346
Christensen, H., Batterham, P. J., Gosling, J. A., Ritterband, L. M., Griffiths, K. M., Thorndike, F. P., et al. (2016). Effectiveness of an online insomnia program (SHUTi) for prevention of depressive episodes (the GoodNight Study): a randomised controlled trial. Lancet Psychiatry 3, 333–341. doi: 10.1016/S2215-0366(15)00536-2
DeBellis, M. D. (2010). “The neurobiology of child neglect,” in The impact of early life trauma on health and disease, eds R. A. Lanius, E. Vermetten, and C. Pain (Cambridge: Cambridge University Press), 123–133.
DeYoung, P. (2015). Understanding and treating chronic shame. A relational/neurobiological approach. London: Routledge. doi: 10.4324/9781315734415
Di Bartolomeo, A. A., Varma, S., Fulham, L., and Fitzpatrick, S. (2022). The moderating role of interpersonal problems on baseline emotional intensity and emotional reactivity in individuals with borderline personality disorder and healthy controls. J. Exp. Psychopathol. 13:20438087221142481. doi: 10.1177/20438087221142481
Dorahy, M. J., Corry, M., Black, R., Matheson, L., Coles, H., Curran, D., et al. (2017). Shame, dissociation, and complex PTSD symptoms in traumatized psychiatric and control groups: direct and indirect associations with relationship distress. J. Clin. Psychol. 73, 439–448. doi: 10.1002/jclp.22339
Dorahy, M. J., Middleton, W., Seager, L., Williams, M., and Chambers, R. (2016). Child abuse and neglect in complex dissociative disorder, abuse-related chronic PTSD, and mixed psychiatric samples. J. Trauma Dissociation 17, 223–236. doi: 10.1080/15299732.2015.1077916
Draijer, N. (1990). Seksuele traumatisering in de jeugd. Gevolgen op lange termijn van seksueel misbruik van meisjes door verwanten. (Sexual traumatization in childhood. Consequences and long term effects). Ph D Thesis. Amsterdam: Universiteit van Amsterdam.
Draijer, N., and Langeland, W. (1999). Childhood trauma and perceived parental dysfunction in the etiology of dissociative symptoms in psychiatric patients. Am. J. Psychiatry 156, 379–385. doi: 10.1176/ajp.156.3.379
Elison, J., Lennon, R., and Pulos, S. (2006). Investigating the compass of shame: the development of the compass of shame scale. Soc. Behav. Pers. Int. J. 34, 221–238. doi: 10.2224/sbp.2006.34.3.221
Estric, C. R., and Lopez-Castroman, J. (2022). Adverse childhood experiences and neurocognition in borderline personality disorder: a call-to-action perspective review. Harvard Rev. Psychiatry 30, 248–260. doi: 10.1097/HRP.0000000000000344
Erden, S., and Akbag, M. (2015). How do personality traits effect shame and Guilt? An evaluation of the Turkish culture. Euras. J. Educ. Res. 58, 113–132. doi: 10.14689/ejer.2015.58.4
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., et al. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The adverse childhood experiences (ACES) Study. Am. J. Prev. Med. 14, 245–258. doi: 10.1016/s0749-3797(98)00017-8
Fonagy, P., Gergely, G., Jurist, E. L., and Target, M. (2002). Affectregulation, mentalization and the development of the self. New York, NY: Orther Press.
Germain, A., Buysse, D. J., and Nofzinger, E. (2008). Sleep-specific mechanisms underlying posttraumatic stress disorder: Integrative review and neurobiological hypotheses. Sleep Med. Rev. 12, 185–195. doi: 10.1016/j.smrv.2007.09.003
Griffiths, B. B., and Hunter, R. G. (2014). Neuroepigenetics of stress. Neuroscience 275, 420–435. doi: 10.1016/j.neuroscience.2014.06.041
Gross, C. A., and Hansen, N. E. (2000). Clarifying the experience of shame: the role of attachment style, gender, and investment in relatedness. Pers. Individ. Dif. 28, 897–907. doi: 10.1016/S0191-8869(99)00148-8
Hertenstein, E., Feige, B., Gmeiner, T., Kienzler, C., Spiegelhalder, K., Johann, A., et al. (2019). Insomnia as a predictor of mental disorders: a systematic review and meta-analysis. Sleep Med Rev. 43, 96–105. doi: 10.1016/j.smrv.2018.10.006
Hong, Y. R., and Park, J. S. (2012). Impact of attachment, temperament and parenting on human development. Korean J. Pediatr. 55, 449–454. doi: 10.3345/kjp.2012.55.12.449
Insana, S. P., Kolko, D. J., and Germain, A. (2012). Early-life trauma is associated with rapid eye movement sleep fragmentation among military veterans. Biol. Psychol. 89, 570–579. doi: 10.1016/j.biopsycho.2012.01.001
Jansen, P. R., Watanabe, K., Stringer, S., Skene, N., Bryois, J., Hammerschlag, A. R., et al. (2019). Genome-wide analysis of insomnia (N=1,331,010) identifies novel loci and functional pathways. Nat. Genet. 51, 394–403. doi: 10.1038/s41588-018-0333-3
Kajeepeta, S., Gelaye, B., Jackson, C. L., and Williams, M. A. (2015). Adverse childhood experiences are associated with adult sleep disorders: a systematic review. Sleep Med. 16, 320–330. doi: 10.1016/j.sleep.2014.12.013
Kolling, N., Wittmann, M. K., Behrens, T. E., Boorman, E. D., Mars, R. B., and Rushworth, M. F. (2016). Value, search, persistence and model updating in anterior cingulate cortex. Nat. Neurosci. 19, 1280–1285. doi: 10.1038/nn.4382
Lang, J., McKie, J., Smith, H., McLaughlin, A., Gillberg, C., Shiels, P., et al. (2020). Adverse childhood experiences, epigenetics and telomere length variation in childhood and beyond: a systematic review of the literature. Eur. Child Adolesc. Psychiatry 29, 1329–1338. doi: 10.1007/s00787-019-01329-1
Lanius, R. A., Terpou, B. A., and McKinnon, M. C. (2020). The sense of self in the aftermath of trauma: lessons from the default mode network in posttraumatic stress disorder. Eur. J. Psychotraumatol. 11:1807703. doi: 10.1080/20008198.2020.1807703
Lichtenberg, J. D., Lachmann, F. M., and Fosshage, J. L. (2011). Psychoanalysis and motivational systems. New York, NY: Routledge. doi: 10.4324/9780203844748
Luyten, P., Envelope, J., and Fontaine, R. J. (2002). Does the Test of Self-Conscious Affect (TOSCA) measure maladaptive aspects of guilt and adaptive aspects of shame? An empirical investigation. Person. Individ. Differ. 33, 1373–1387. doi: 10.1016/S0191-8869(02)00197-6
Manber, R., Edinger, J. D., Gress, J. L., San Pedro-Salcedo, M. G. S., Kuo, T. F., and Kalista, T. (2008). Cognitive behavioral therapy for insomnia enhances depression outcome in patients with comorbid major depressive disorder and insomnia. Sleep. 31, 489–495. doi: 10.1093/sleep/31.4.489
Muscatello, M. R. A., Rizzo, A., Celebre, L., Mento, C., Pandolfo, G., Cedro, C., et al. (2020). The wounds of childhood: early trauma subtypes, salience and hyperarousal in a sample of adult psychiatric patients. Int. J. Soc. Psychiatry 66, 3–9. doi: 10.1177/0020764019872227
Nicolai, N. (2020). In levende lijve: het lichaam in de psychotherapie (Dutch ed.), 1st Edn. Houten: Bohn Stafleu van Loghum.
Palagini, L., Petri, E., Novi, M., Caruso, D., Moretto, U., and Riemann, D. (2018). Adult insecure attachment plays a role in hyperarousal and emotion dysregulation in Insomnia Disorder. Psychiatry Res. 262, 162–167. doi: 10.1016/j.psychres.2018.01.017
Pavlova, M., Berg, O., Gleason, R., Walker, F., Roberts, S., and Regestein, Q. (2001). Self-reported hyperarousal traits among insomnia patients. J. Psychosom. Res. 51, 435–441. doi: 10.1016/s0022-3999(01)00189-1
Pesonen, A.-K., Gradisar, M., Kuula, L., Short, M., Merikanto, M., Tark, R., et al. (2019). REM sleep fragmentation associated with depressive symptoms and genetic risk for depression in a community-based sample of adolescents. J. Affect. Disord. 245, 757–763. doi: 10.1016/j.jad.2018.11.077
Porges, S. W. (2011). The polyvagal theory. Neurophysiological foundations of emotions, attachment, communication and self-regulation. New York, NY: Norton.
Pruim, R. H. R., Mennes, M., van Rooij, D., Llera, A., Buitelaar, J. K., and Beckmann, C. F. (2015). ICA-AROMA: a robust ICA-based strategy for removing motion artifacts from fMRI data. Neuroimage 112, 267–277. doi: 10.1016/j.neuroimage.2015.02.064
R Core Team. (2021). R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing.
Reffi, A. N., Kalmbach, D. A., Cheng, P., Jovanovic, T., Norrholm, S. D., Sexton, M. B., et al. (2022). Sleep reactivity as a potential pathway from childhood abuse to adult insomnia. Sleep Med. 94, 70–75. doi: 10.1016/j.sleep.2022.03.026
Riemann, D., Spiegelhalder, K., Feige, B., Voderholzer, U., Berger, M., Perlis, M., et al. (2010). The hyperarousal model of insomnia: a review of the concept and its evidence. Sleep Med Rev. 14, 19–31. doi: 10.1016/j.smrv.2009.04.002
Riemann, D., Spiegelhalder, K., Nissen, C., Hirscher, V., Baglioni, C., and Feige, B. (2012). REM sleep instability – A new pathway for insomnia? Pharmacopsychiatry 45, 167–176. doi: 10.1055/s-0031-1299721
Schalkwijk, F. (2012). Schaamte in psychotherapie. Tijdschrift Psychother. 38, 368–380. doi: 10.1007/s12485-012-0042-9
Schalkwijk, F., Stams, G. J., Dekker, J., Peen, J., and Elison, J. (2016). Measuring shame regulation: validation of the compass of shame scale. Soc. Behav. Pers. Int. J. 44, 1775–1791. doi: 10.2224/sbp.2016.44.11.1775
Schiel, J. E., Tamm, S., Holub, F., Petri, R., Dashti, H. S., Domschke, L., et al. (2022). Associations between sleep health and amygdala reactivity to negative facial expressions in the UK Biobank cohort. Biol. Psychiatry 92, 693–700. doi: 10.1016/j.biopsych.2022.05.023
Sedighimornani, N., Rimes, K., and Verplanken, B. (2021). Factors contributing to the experience of shame and shame management: adverse childhood experiences, peer acceptance, and attachment styles. J. Soc. Psychol. 161, 129–145. doi: 10.1080/00224545.2020.1778616
Seo, J., Moore, K. N., Gazecki, S., Bottary, R. M., Milad, M. R., Song, H., et al. (2018). Delayed fear extinction in individuals with insomnia disorder. Sleep 41:zsy095. doi: 10.1093/sleep/zsy095
Spinhoven, P., Penninx, B. W., Hickendorff, M., Van Hemert, A. M., Bernstein, D. P., and Elzinga, B. M. (2014). Childhood trauma questionnaire: factor structure, measurement invariance, and validity across emotional disorders. Psychol. Assess. 26, 717–729. doi: 10.1037/pas0000002
Steine, I. M., Skogen, J. C., Krystal, J. H., Winje, D., Milde, A. M., Grønli, J., et al. (2019). Insomnia symptom trajectories among adult survivors of childhood sexual abuse: a longitudinal study. Child Abuse Negl. 93, 263–276. doi: 10.1016/j.chiabu.2019.05.009
Strathearn, L., Giannotti, M., Mills, R., Kisely, S., Najman, J., and Abajobir, A. (2020). Long-term cognitive, psychological, and health outcomes associated with child abuse and neglect. Pediatrics 146:e20200438. doi: 10.1542/peds.2020-0438
Thombs, B. D., Bernstein, D. P., Lobbestael, J., and Arntz, A. (2009). A validation study of the dutch childhood trauma questionnaire-short form: factor structure, reliability, and known-groups validity. Child Abuse Negl. 33, 518–523. doi: 10.1016/j.chiabu.2009.03.001
Tracy, J. L., Robins, R. W., and Tangney, J. P. (2007). The self-conscious emotions: theory and research. New York, NY: Guilford Press.
Van der Kolk, B. (2014). The body keeps the score: mind, brain, and body in the transformation of trauma. London: Penguin.
van Heukelum, S., Mars, R. B., Guthrie, M., Buitelaar, J. K., Beckmann, C. F., Tiesinga, P. H. E., et al. (2020). Where is cingulate cortex? A cross-species view. Trends Neurosci. 43, 285–299. doi: 10.1016/j.tins.2020.03.007
Voestermans, D., Eikelenboom, M., Rullmann, J., Wolters-Geerdink, M., Draijer, N., Smit, J. H., et al. (2021). The association between childhood trauma and attachment functioning in patients with personality disorders. J. Pers. Disord. 35, 554–572. doi: 10.1521/pedi_2020_34_474
Vonderlin, R., Kleindienst, N., Alpers, G., Bohus, M., Lyssenko, L., and Schmal, C. (2018). Dissociation in victims of childhood abuse or neglect: a meta-analytic review. Psychologtical Med. 48, 2467–2476. doi: 10.1017/S00332911718000740
Walker, M. P. (2009). The role of sleep in cognition and emotion. Ann. N. Y. Acad. Sci. 1156, 168–197. doi: 10.1111/j.1749-6632.2009.04416.x
Walker, M. P., and Van der Helm, E. (2009). Overnight therapy? The role of sleep in emotional brain processing. Psychol. Bull. 135, 731–748. doi: 10.1037/a0016570
Wang, Y., Raffeld, M. R., Slopen, N., Hale, L., and Dunn, E. C. (2016). Childhood adversity and insomnia in adolescence. Sleep Med. 21, 12–18. doi: 10.1016/j.sleep.2016.01.011
Wassing, R., and D’Rozario, A. (2022). Getting all emotional over sleep. Health Biol. Psychiatry 92, 684–686. doi: 10.1016/j.biopsych.2022.08.003
Wassing, R., Benjamins, J. S., Dekker, K., Moens, S., Spiegelhalder, K., Feige, B., et al. (2016). Slow dissolving of emotional distress contributes to hyperarousal. Proc. Natl Acad. Sci. U.S.A. 113, 2538–2543. doi: 10.1073/pnas.1522520113
Wassing, R., Benjamins, J. S., Talamini, L. M., Schalkwijk, F., and Van Someren, E. J. W. (2019a). Overnight worsening of emotional distress indicates maladaptive sleep in insomnia. Sleep 42:zsy268. doi: 10.1093/sleep/zsy268
Wassing, R., Schalkwijk, F., Lakbila-Kamal, O., Ramautar, J. R., Stoffers, D., Mutsaerts, H. J. M. M., et al. (2019b). Haunted by the past: old emotions remain salient in insomnia disorder. Brain. 142, 1783–1796. doi: 10.1093/brain/awz089
Whalley, M. G., Kroes, M. C., Huntley, Z., Rugg, M. D., Davis, S. W., and Brewin, C. R. (2013). An fMRI investigation of posttraumatic flashbacks. Brain Cogn. 81, 151–159. doi: 10.1016/j.bandc.2012.10.002
Keywords: insomnia, adverse childhood experiences (ACEs), childhood trauma, hyperarousal, dorsal anterior cingulate cortex (dACC), shame
Citation: Schalkwijk F, Van Someren EJW, Nicolai NJ, Uijttewaal JL and Wassing R (2023) From childhood trauma to hyperarousal in adults: The mediating effect of maladaptive shame coping and insomnia. Front. Hum. Neurosci. 17:990581. doi: 10.3389/fnhum.2023.990581
Received: 26 July 2022; Accepted: 26 January 2023;
Published: 16 February 2023.
Edited by:
Filippo Cieri, Cleveland Clinic, United StatesReviewed by:
Roee Admon, University of Haifa, IsraelCopyright © 2023 Schalkwijk, Van Someren, Nicolai, Uijttewaal and Wassing. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Frans Schalkwijk,  Zi5zY2hhbGt3aWprQGdtYWlsLmNvbQ==
Zi5zY2hhbGt3aWprQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.