- Cardiff University Brain Research Imaging Centre (CUBRIC), School of Psychology, College of Biomedical and Life Sciences, Cardiff University, Cardiff, United Kingdom
Gender-affirming hormone replacement therapy (gaHRT) is an important step for many in the gender diverse community, associated with increased quality-of-life and lower self-reported scores of depression and anxiety. However, considering the interactions that the involved sex hormones have on vasculature (with oestrogen and testosterone demonstrating vasodilatory and vasoconstricting properties, respectively), it is important for transgender healthcare research to examine how the manipulation of these hormones interact with cerebrovascular structure and functioning. There is a stark lack of research in this area. This mini-review outlines the research suggesting a vascular impact of these sex hormones using evidence from a range of cohorts (e.g., menopause, polycystic ovary syndrome) and discusses the work that has been done into cerebrovascular changes following gaHRT. Finally, recommendations for future research into cerebrovascular health in transgender cohorts following gaHRT are outlined.
Introduction
Transgender people are individuals whose gender identity does not align with that assigned to them at birth. While exact prevalence rates of gender diverse individuals are difficult to determine due to the variety of criteria and methods used (Collin et al., 2016), the self-reported rate is ∼0.1–2%, depending on geographical location (Goodman et al., 2019; Spizzirri et al., 2021). Despite this, it represents an under-researched population. For example, only 0.08% of clinical trials published between January 2018 and July 2022 reported transgender participation (Round et al., 2023).
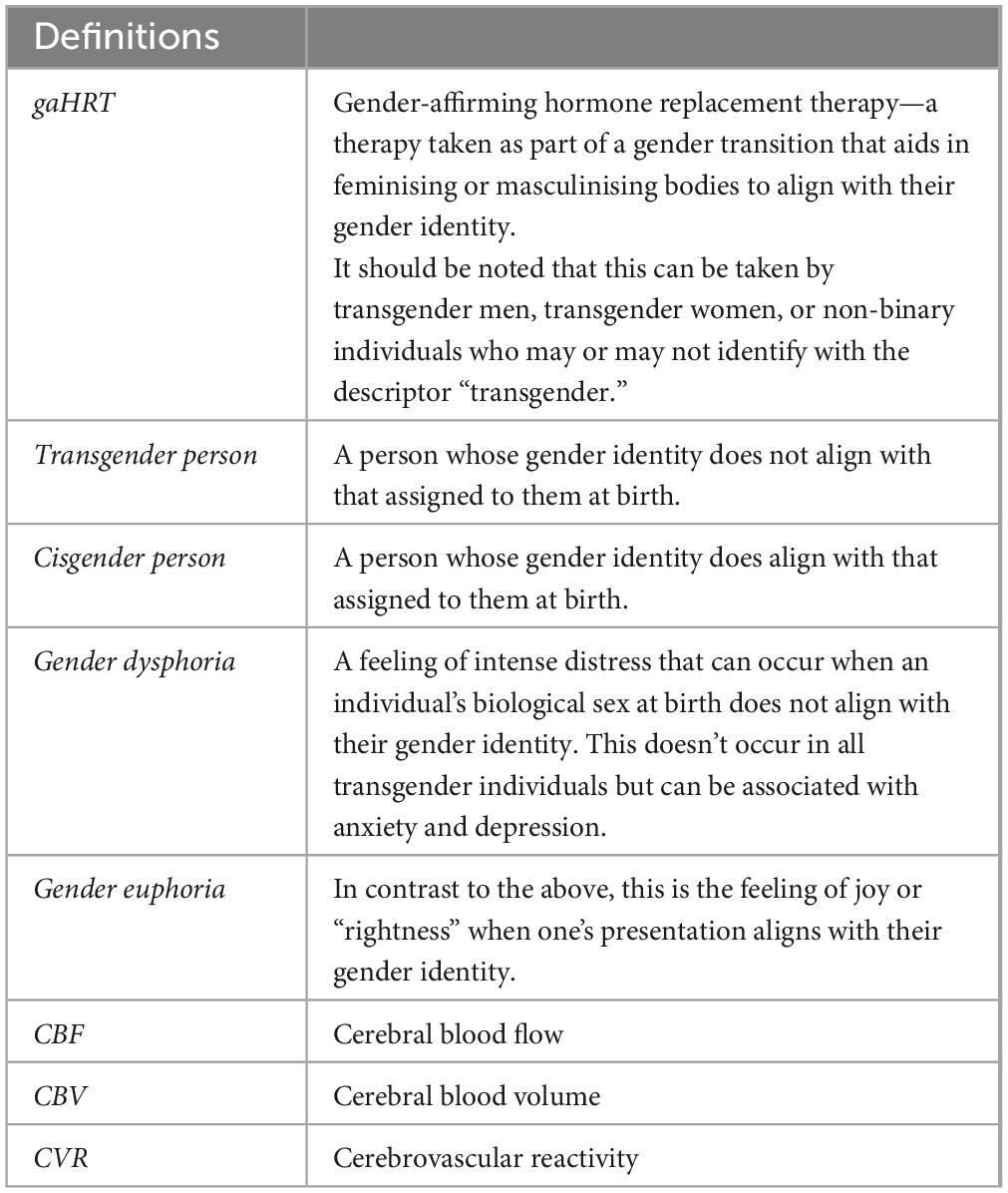
Transgender people may take gender-affirming hormone replacement therapy (gaHRT) to aid in their gender transition. This forms an essential part of people’s transition (Mohamed and Hunter, 2018), improving anxiety and depression and alleviating symptoms of gender dysphoria (see Table 1 for definitions; Colizzi et al., 2013; Baker et al., 2021; Chaovanalikit et al., 2022). To better understand and serve transgender health, it is important to consider the impact of gaHRT treatment.
This review focuses on the influence of gaHRT in transgender individuals on cerebrovascular function and health. Measures of cerebrovascular function include cerebral blood flow (CBF), blood-brain barrier function, cerebral blood volume (CBV), cerebrovascular reactivity (CVR), and cerebral vessel pulsatility. The brain has a high metabolic demand, and the supporting vasculature is essential for maintaining cognitive function and brain health (Iadecola, 2017; Zimmerman et al., 2021). As hormones can have large vascular effects, it is vitally important to investigate how gaHRT influences cerebrovascular health to inform transgender healthcare.
Gender-affirming hormone replacement therapy
There are two broad categories of gaHRT. Masculinising gaHRT introduces exogenous testosterone to maximise virilization (e.g., deepening of the voice, changes in musculature, hair growth) and to suppress female secondary sex characteristics. A range of administration routes are available (oral, subcutaneous, transdermal) to achieve blood concentrations of 300–1,000 ng/dL (after which, the goal becomes maintenance; Unger, 2016). While the early presentation of masculinising effects is dose-dependent, different dosages appear equally effective after six-months (Nakamura et al., 2013).
Feminising gaHRT involves the delivery of exogenous oestrogen which changes fat distribution and reduces male pattern hair growth (Giltay and Gooren, 2000). This suppresses androgen production (Dittrich et al., 2005) and is generally prescribed with additional anti-androgenic therapy. Different administration routes are available (Oral, subcutaneous, transdermal) to achieve the blood oestradiol target level of 100–200 pg/mL (Unger, 2016). The addition of progesterone to gaHRT treatment regimens, to better represent female hormonal profiles, may be beneficial for feminising outcomes, but it’s efficiency remains under-researched (Deutsch, 2016; Prior, 2019; Milionis et al., 2022). In both masculinising and feminising cases, the exact form and dosage of gaHRT can and should be tailored to an individual and their transition goals.
Gender-affirming hormone replacement therapy (gaHRT) benefits wellbeing and health outcomes (e.g., depression, anxiety, quality-of-life, self-reported and physiological stress) equally across gender identity, age and psychological attachment style (e.g., Colizzi et al., 2013; Baker et al., 2021; Chaovanalikit et al., 2022).
It is important to consider how an altered hormonal profile will influence cerebral vasculature structure and function. Generalising from other populations is inadequate; transgender individuals may present with different healthy reference levels than their cisgender counterparts (e.g., Roberts et al., 2014, found that “normal” levels of certain clinical measurands, important for diagnosis and monitoring, was different following gaHRT compared to cisgender individuals of either sex) and interaction with other factors (e.g., age of onset, length of use, previous hormonal history, environmental stress) may lead to altered patterns of risk.
The influence of sex hormones on cerebrovascular health—evidence from other cohorts
The importance of investigating cerebrovascular health after hormonal changes can be highlighted by examining other cohorts. Although these results may not generalise, they demonstrate that sex hormones influence cerebrovascular health, suggesting that effects may be expected following gaHRT.
Oestrogen and progesterone
Oestrogen receptors are found throughout the brain (Shughrue and Merchenthaler, 2001; Milner et al., 2010; Mitterling et al., 2010) and the hormone is considered to be vascular- and neuro-protective. Cisgender women have a lower risk of cardiovascular and cerebrovascular disease compared to cisgender men up until menopause, at which point their risk significantly increases (Hayward et al., 2000; Aggarwal et al., 2018). Earlier menarche and longer reproductive lifespan are also associated with lower risk of stroke, suggesting a beneficial influence of lifetime exposure to oestrogen on the cerebrovascular system [Chen et al., 2023; relatedly, lifetime oestrogen exposure also shows associations with better memory score and larger medial temporal cortical volumes (Steventon et al., 2023)]. Animal models demonstrate that oestrogen increases vasodilation (Tostes et al., 2003), decreases pathological vasoreactivity (Wassmann et al., 2001), and increases CBF and angiogenesis (Robison et al., 2019). Additionally, it suppresses inflammatory responses and increases perfusion after ischemic injury (Hurn et al., 1995; Santizo et al., 2002). This vascular-protective effect is present in both male and female animal models (Roof and Hall, 2000), though may be age-dependant (Deer and Stallone, 2016).
The influence of progesterone on the cerebrovascular system is less clear, with conflicting results on inflammation. For example, Gibson et al. (2005) reports that administration of progesterone suppressed aspects of the post-injury inflammatory response, while Sunday et al. (2006) found that the administration of progesterone exacerbated the inflammatory response in ovariectomized rats. However, there have been multiple reports of progesterone having a beneficial impact on recovery from brain injury (Chen et al., 2011, 2021; Gibson et al., 2011) and facilitating vascular reactivity (Cunha et al., 2020; da Costa et al., 2021).
Due to relatively predictable lifetime changes in oestrogen and progesterone, there are several informative cohorts for investigating their combined influence on the human cerebrovascular system. By assessing cisgender women multiple times across a menstrual cycle, oestrogen and progesterone were found to have independent, region-specific influences on CBF (Cote et al., 2021). Fluctuations in progesterone and oestrogen/progesterone ratio impact CVR (Debert et al., 2012; Skinner et al., 2023). While some studies report reduced CBF and CVR following menopause, high-quality evidence and consistent menopausal criteria are lacking (Ruediger et al., 2021). A confounding factor is the impact of age and physical fitness at menopause age on cerebrovascular health (Chen et al., 2023; Moir et al., 2023; Ruediger et al., 2023). A recent systematic review of the influence of sex hormones on cerebrovascular function in human subjects suggested that, though there were often differences between high and low hormonal states, the directions were not consistent (Skinner et al., 2021). A meta-analysis indicated that HRT improves pulsatility but not CBF, though notable heterogeneity exists (Skinner et al., 2021). More research is needed to illustrate the influence of oestrogen and progesterone on cerebrovascular function. While a vascular impact is strongly suggested, mainly by animal research, the interactions are complex and may be influenced by factors unique to each cohort (e.g., current age, age of menarche, chronic vs. acute exposure/deprivation and history of HRT use).
Testosterone
Testosterone is a prominent circulating androgen affecting receptors throughout the neural system (Sheridan, 1983; Sarkey et al., 2008), with its potency linked to genetic factors (Chamberlain et al., 1994; Tirabassi et al., 2013). Animal model and isolated cell culture studies suggest that androgen levels improve angiogenesis (Louissaint et al., 2002; Yoshida et al., 2013), though this effect is diminished with age (Lecce et al., 2014). Testosterone appears to influence pathways that mediate CBF, with chronic testosterone deprivation/exposure in male animal models eliciting vasodilation/vasoconstriction of cerebral vessels, respectively (Geary et al., 2000; Gonzales et al., 2004, 2005; Abi-Ghanem et al., 2020). This vasoconstrictive influence may explain cisgender sex differences in CBF, which is higher in women than men (e.g., Rodriguez et al., 1988; Aanerud et al., 2017). However, acute testosterone administration in other vascular beds elicits vasodilation (Yue et al., 1995; Deenadayalu et al., 2001; Tep-areenan et al., 2002). At a cellular level, testosterone facilitates vasodilatory and protective mechanisms (Deenadayalu et al., 2001; Perusquía, 2003; Perusquía et al., 2015). Testosterone’s influence may also be mediated by sex, possibly due to hormonal history or other sex-associated differences in vascular physiology. Sieveking et al. (2010) found that androgen administration increased angiogenesis only in male mice models. Additionally, testosterone levels appear to have opposite actions on ET-1 (a vasoconstrictor) in cisgender vs. transgender men (Polderman et al., 1993; Kumanov et al., 2007; Abi-Ghanem et al., 2020). While testosterone appears to have a vasoconstricting influence on the vascular system, the effect is mediated by multiple other factors (such as sex and age), and it may facilitate vasodilation in certain vessels.
Testosterone’s influence on cerebrovasculature in cisgender women or following gaHRT is less well known. An important cohort for investigating this is patients with polycystic ovary syndrome (PCOS), a condition commonly characterised by hyperandrogenism, irregular/missing menstruation, and ovarian cysts. Excess testosterone increases systemic arterial stiffness in PCOS patients compared to controls (Kilic et al., 2021) but the influence on cerebrovascular function is vastly under-researched. Acar et al. (2005) reported no statistically significant difference in CBV using colour duplex sonography, though blood velocity in the vertebral artery was significantly reduced in PCOS patients. Direct comparisons to testosterone level were not made. The PCOS cohort represents an excellent opportunity to investigate testosterone’s influence on the cerebrovascular system.
It is noteworthy that testosterone can be locally metabolised into oestrogens, making each hormone’s influence difficult to separate. For example, estrone level, a form of oestrogen, is elevated in PCOS patients (DeVane et al., 1975).
Vascular research in transgender populations undergoing gaHRT
Research specifically investigating cerebrovascular health in transgender populations undergoing gaHRT has focused on disease outcomes rather than function (e.g., CBF, CVR). There exists an increased risk of ischemic stroke following feminising gaHRT (Connelly et al., 2019; Pribish and Iwamoto, 2023), though the low event rate present in younger cohorts limits interpretation (e.g., of 966 transgender women, five died from stroke; Asscheman et al., 2011). The use of an outdated oral form of gaHRT (ethinyl oestradiol) in these studies also limits the present-day generalisability of the results (Asscheman et al., 2011; Irwig, 2018; Pribish and Iwamoto, 2023). Current, but not past, ethinyl oestradiol use is linked to cardiovascular events (Asscheman et al., 2011). However, ischemic stroke risk is increased in transgender women, even when excluding ethinyl oestradiol use (Getahun et al., 2018). Notably, the cerebrovascular event risk was unchanged initially and only increased after the 6 year follow-up (Getahun et al., 2018), which highlights the importance of longitudinal comparisons. While Getahun et al. (2018) found elevated cerebrovascular disease risk in transgender women compared to cisgender women (but not cisgender men), others report the opposite pattern (Wierckx et al., 2013) or no difference at all (Meyer et al., 2017), suggesting unappreciated mediating factors. Cerebrovascular disease risk is not elevated with masculinising gaHRT (Wierckx et al., 2013; Getahun et al., 2018; Connelly et al., 2019) and in fact migraine risk (related to vasculature) appears lower (Todd et al., 2023). In terms of broader cardiovascular disease outcomes and risk factors, a similar pattern is seen, with elevated risk in transgender women but not transgender men (Connelly et al., 2019; Kulprachakarn et al., 2020; Pribish and Iwamoto, 2023). However, this is not always observed (Martinez et al., 2023) and an improvement in vascular function following feminising gaHRT has been reported (New et al., 1997, 2000). Importantly, Karalexi et al. (2022) reported that cardiovascular disease incidence in gender diverse populations was similar regardless of gaHRT use. Increased disease incidence may therefore be due to healthcare barriers (Safer et al., 2016) and other environmental factors (e.g., minority stress) rather than gaHRT. Clearly, more work is needed to understand risk following gaHRT, especially following feminising gaHRT, which mirrors the mixed evidence of vascular benefits following post-menopausal HRT despite protective effects of oestrogen (Boardman et al., 2015). More research into specific cerebrovascular functions may help in understanding this complex relationship.
Evidence for changes in cerebral vessels can also be inferred from related work. A recent review describes twenty transgender male patients who had been undergoing gaHRT and presented with intracranial hypertension, a condition characterised by increased intracranial pressure (ICP). They suggest an association with cerebral spinal fluid (CSF) hypoandrogenism (Kamboj et al., 2023). Chronic testosterone treatment in lean rat models led to an increase in ICP, potentially due to increased CSF secretion rate (Wardman et al., 2023). ICP itself is associated with vascular pulsatility, an index of vascular health (Hamzah et al., 2020). Increased vascular pulsatility is associated with damage to cerebrovascular microstructure and cognition due to pulsatile stress reaching the brain (Singer et al., 2014; Palta et al., 2019). If cerebrovascular pulsatility is altered by testosterone-based gaHRT, this may be an important area for monitoring/consideration. Cunha et al. (2023) found that arterial stiffness (measured using carotid–femoral pulse wave velocity) was significantly higher in transgender men compared to cisgender men and women, suggesting increased aortic stiffness and thus increased levels of vascular pulsatility. Within the transgender men group, there was a significant positive correlation between gaHRT duration (which ranged from 4 to 32 years) and pulsatility. Such studies provide important insights into how masculinising gaHRT impact vascular haemodynamics. Future studies will shed light on how this translates to cerebral vasculature and brain health.
A small number of studies have investigated the retina, the layer of neural tissue in the anterior eye that supports vision. The retina is of interest because it can be more directly imaged non-invasively than the cerebrovasculature. Changes in retinal vasculature and structure are associated with many vascular disorders (e.g., Sairenchi et al., 2011; Hanff et al., 2014; Moss, 2015; Wiseman et al., 2023). Measuring blood flow in the ophthalmic artery using Colour Doppler Ultrasonograph, Alpogan et al. (2021) observed no difference between transgender men, cisgender men, and cisgender women. However, the systole/diastole flow ratio significantly correlated with circulating testosterone level. Using Optical Coherence Tomography Angiography (OCT-A), Tüten et al. (2022) found that retinal vessel density (VD) was lower across multiple regions in transgender men compared to cisgender women controls, reaching statistical significance in the inferior region and for radial peripapillary capillary VD. These studies provide important information on the influence of exogenous testosterone on ocular health and may suggest wider vascular changes. However, without transgender women participants as a comparison, conclusions about whether it is the testosterone per se or just hormonal profile changes are difficult to draw. For example, while oestrogen is reported to be protective of vascular health (e.g., Parker et al., 2009; Burns and Korach, 2012; Iorga et al., 2017; Novella et al., 2019; Shin et al., 2022), oestrogen (or combined oestrogen and progesterone) HRT does not conclusively prevent cardiovascular disease in post-menopausal women (Boardman et al., 2015). Overall, the retina provides a unique window into general cerebrovascular health and specifically neural microvasculature.
In conclusion, cerebrovascular function changes in transgender populations taking gaHRT. However, the research into disease outcomes and risk paints a complex picture that is not fully understood. Cerebrovascular function needs to be fully investigated against detailed hormonal profiles.
Recommendations
More research is needed in this area. Cohort-relevant factors such as age of onset, previous hormonal profile, length of use, and environmental stresses must be considered. In particular, longitudinal studies with long-term follow ups would be beneficial as gaHRT may be taken for multiple decades (Mohamed and Hunter, 2018). Though such studies represent a significant investment, they are essential in determining how cerebrovascular health is affected by long-term hormonal use. Additionally, cross-sectional studies should take into account many confounding factors that will vary between transgender and cisgender participants, such as chronic stress, lifestyle, level of dysphoria, external support systems, and traumatic experiences. Transgender cohorts represent a marginalised group and face significant social stressors in their day-to-day life (Harrison et al., 2012; Valentine and Shipherd, 2018; Chodzen et al., 2019; Lin et al., 2021; Wilson et al., 2023), which themselves are associated with cerebrovascular function changes (Endo et al., 1999; Lee et al., 2015; Burrage et al., 2018). Consideration of such factors is also important during longitudinal studies, as reported levels of psychological wellbeing improve over the course of gaHRT (e.g., Chaovanalikit et al., 2022). Well-controlled and considered longitudinal studies are essential in determining the influence of gaHRT on cerebrovascular health.
Older adults undergoing gaHRT are a particularly under-researched subgroup. The cerebrovascular benefits/risks in older people who commenced gaHRT at a young age may present very differently to those who start gaHRT in later life, especially considering age-related comorbidities. Qualitative research into transgender women aged 20–79 years old (96% of which were taking gaHRT) suggest that, although it is an “essential” part of their transition, they have concerns about the long-term effects of gaHRT (Mohamed and Hunter, 2018). Research should consider how to best serve the community and address such concerns (Minalga et al., 2022).
It should also be noted that many studies involving transgender individuals use relatively small sample sizes and convenience sampling. They therefore may mostly consist of a narrow range of demographics (e.g., university educated, secure socioeconomic status). To recruit a broader and more representative sample, the transgender community must be actively engaged with. Some of the keys barriers for research participation reported by transgender persons were “lack of trust in research” and “lack of knowledge of opportunities” (Owen-Smith et al., 2016). There are also more cohort-specific worries that should be considered for the safety and comfort of participants, such as the risk of being “outed” (i.e., having their identity shared or obvious to external individuals; Owen-Smith et al., 2016). This particular point could be addressed by, for example, highlighting any relevant signage, being clear about the study location, and outlining anonymisation practises in participant information sheets. Active engagement and public awareness campaigns will be essential for increasing diverse participation and rebuilding trust, as well as gaining input from transgender individuals at the study design stage. Larger and more representative samples will allow for more confident and relevant conclusions to be drawn.
The language of research into the general population can be easily adjusted to be more inclusive to the gender-diverse community and therefore produce more representative results. For example, allowing participants to define their own gender rather than select from a binary response, provides a much richer and more representative dataset (Ghorbanian et al., 2022). Additionally, adjusting the language of calls for participation, surveys and study documents may help in making research more approachable to a wider variety of participants, reducing bias and improving the accessibility/inclusivity of participation pools.
Finally, adequately controlled studies are important. For example, some studies found significant differences when comparing transgender women to cisgender women but not cisgender men (Getahun et al., 2018), while others report the opposite pattern (Wierckx et al., 2013). Studies that only include one cisgender control group may be missing a larger pattern. Additionally, by including both feminising and masculinising gaHRT groups, researchers can make better inferences about whether fluctuations in an outcome metric is due to a particular hormone per se, or just the act of altering hormonal profiles in general.
Conclusion
Significant progress is needed to determine the impact of gaHRT on transgender participants’ cerebrovascular health to uncover mechanisms behind cerebrovascular or neurodegenerative disease risk (Brady et al., 2023). Such studies may highlight subtle risk patterns and will uncover how sex hormones interact with the cerebrovascular system in general populations. It is important to investigate cerebral vessels specifically, as the vasodilatory properties of oestrogen can vary by vascular bed location (Opgaard et al., 2002). In the future, long-term longitudinal research with considered controls and inclusive language will allow for more comprehensive, informative, and representative conclusions to be drawn. As mentioned by Pribish and Iwamoto (2023), work suggesting a vascular risk should not dissuade people from gaHRT use, but instead direct patient education and management to vascular health, highlighting modifiable risk factors before and during gaHRT use.
Author contributions
MW: Conceptualization, Writing – original draft. KM: Conceptualization, Writing – review and editing.
Acknowledgements
We would like to thank Wellcome Trust for their help in publication of this article.
Funding
The authors declare financial support was received for the research, authorship, and/or publication of this article. This research was funded in whole, or in part, by the Wellcome Trust (WT224267). For the purpose of open access, the author has applied a CC BY public copyright license to any Author Accepted Manuscript version arising from this submission.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Aanerud, J., Borghammer, P., Rodell, A., Jónsdottir, K. Y., and Gjedde, A. (2017). Sex differences of human cortical blood flow and energy metabolism. J. Cereb. Blood Flow Metab. 37, 2433–2440. doi: 10.1177/0271678X16668536
Abi-Ghanem, C., Robison, L. S., and Zuloaga, K. L. (2020). Androgens’ effects on cerebrovascular function in health and disease. Biol. Sex Differ. 11:35. doi: 10.1186/s13293-020-00309-4
Acar, M., Cevrioğlu, S., Yücel, A., Değirmenci, B., Albayrak, R., Haktanır, A., et al. (2005). Evaluation of cerebral blood flow volume using color duplex sonography in patients with polycystic ovary syndrome. Electr. J. Gen. Med. 2, 91–95. doi: 10.29333/ejgm/82278
Aggarwal, N. R., Patel, H. N., Mehta, L. S., Sanghani, R. M., Lundberg, G. P., Lewis, S. J., et al. (2018). Sex differences in ischemic heart disease: Advances, obstacles, and next steps. Circ. Cardiovasc. Qual. Outcomes 11:e004437. doi: 10.1161/CIRCOUTCOMES.117.004437
Alpogan, O., Donmez, E. E., Balık, A. Ö, Vural, F., and Kaplan, G. (2021). Effects of testosterone on intraocular pressure, thicknesses of retinal nerve fiber layer, ganglion cell complex, macula and on ocular blood flow in female-to-male transgender persons. Int. Ophthalmol. 41, 3651–3661. doi: 10.1007/s10792-021-01921-y
Asscheman, H., Giltay, E. J., Megens, J. A., de Ronde, W. P., van Trotsenburg, M. A., and Gooren, L. J. (2011). A long-term follow-up study of mortality in transsexuals receiving treatment with cross-sex hormones. Eur. J. Endocrinol. 164, 635–642. doi: 10.1530/EJE-10-1038
Baker, K. E., Wilson, L. M., Sharma, R., Dukhanin, V., McArthur, K., Robinson, K. A., et al. (2021). Hormone therapy, mental health, and quality of life among transgender people: A systematic review. J. Endocr. Soc. 5:bvab011. doi: 10.1210/jendso/bvab011
Boardman, H. M., Hartley, L., Eisinga, A., Main, C., Roqué i Figuls, M., Bonfill Cosp, X., et al. (2015). Hormone therapy for preventing cardiovascular disease in post-menopausal women. Cochr. Datab. Syst. Rev. 2015:CD002229. doi: 10.1002/14651858.CD002229.pub4
Brady, B., Zheng, L., Kootar, S., and Anstey, K. J. (2023). Sex and gender differences in risk scores for dementia and Alzheimer’s disease among cisgender, transgender, and non-binary adults. Alzheimers Dement. 1–11. doi: 10.1002/alz.13317
Burns, K. A., and Korach, K. S. (2012). Estrogen receptors and human disease: An update. Arch Toxicol. 86, 1491–1504. doi: 10.1007/s00204-012-0868-5
Burrage, E., Marshall, K. L., Santanam, N., and Chantler, P. D. (2018). Cerebrovascular dysfunction with stress and depression. Brain Circ. 4, 43–53. doi: 10.4103/bc.bc_6_18
Chamberlain, N. L., Driver, E. D., and Miesfeld, R. L. (1994). The length and location of CAG trinucleotide repeats in the androgen receptor N-terminal domain affect transactivation function. Nucleic Acids Res. 22, 3181–3186. doi: 10.1093/nar/22.15.3181
Chaovanalikit, T., Wirairat, K., and Sriswadpong, P. (2022). Quality of life, self-esteem, and depression among thai transgender women before and after male-to-female gender confirmation surgery: A prospective cohort observational study. Sex Med. 10:100533. doi: 10.1016/j.esxm.2022.100533
Chen, L., Hu, Z., Wang, X., Zheng, C., Cao, X., Cai, J., et al. (2023). Association of age at menarche and menopause, reproductive lifespan, and stroke among Chinese women: Results from a national cohort study. medRxiv [preprint] doi: 10.1101/2023.05.23.23290429
Chen, Y., Herrold, A. A., Gallagher, V., Martinovich, Z., Bari, S., Vike, N. L., et al. (2021). Preliminary report: Localized cerebral blood flow mediates the relationship between progesterone and perceived stress symptoms among female collegiate club athletes after mild traumatic brain injury. J. Neurotrauma 38, 1809–1820. doi: 10.1089/neu.2020.7217
Chen, Z., Xi, G., Mao, Y., Keep, R. F., and Hua, Y. (2011). Effects of progesterone and testosterone on ICH-induced brain injury in rats. Acta Neurochir Suppl. 111, 289–293. doi: 10.1007/978-3-7091-0693-8_48
Chodzen, G., Hidalgo, M. A., Chen, D., and Garofalo, R. (2019). Minority stress factors associated with depression and anxiety among transgender and gender-nonconforming youth. J. Adolesc. Health 64, 467–471. doi: 10.1016/j.jadohealth.2018.07.006
Colizzi, M., Costa, R., Pace, V., and Todarello, O. (2013). Hormonal treatment reduces psychobiological distress in gender identity disorder, independently of the attachment style. J. Sex Med. 10, 3049–3058. doi: 10.1111/jsm.12155
Collin, L., Reisner, S. L., Tangpricha, V., and Goodman, M. (2016). Prevalence of transgender depends on the case definition: A systematic review. J. Sex Med. 13, 613–626. doi: 10.1016/j.jsxm.2016.02.001
Connelly, P. J., Marie Freel, E., Perry, C., Ewan, J., Touyz, R. M., Currie, G., et al. (2019). Gender-affirming hormone therapy, vascular health and cardiovascular disease in transgender adults. Hypertension 74, 1266–1274. doi: 10.1161/HYPERTENSIONAHA.119.13080
Cote, S., Butler, R., Michaud, V., Lavallee, E., Croteau, E., Mendrek, A., et al. (2021). The regional effect of serum hormone levels on cerebral blood flow in healthy nonpregnant women. Hum. Brain Mapp. 42, 5677–5688. doi: 10.1002/hbm.25646
Cunha, F. S., Bachega, T. A., Costa, E. M., Brito, V. N., Alvares, L. A., Costa-Hong, V. A., et al. (2023). Arterial stiffness in transgender men receiving long-term testosterone therapy. J. Endocr. Soc. 7:bvad040. doi: 10.1210/jendso/bvad040
Cunha, T. R., Giesen, J. A., Rouver, W. N., Costa, E. D., Grando, M. D., Lemos, V. S., et al. (2020). Effects of progesterone treatment on endothelium-dependent coronary relaxation in ovariectomized rats. Life Sci. 247:117391. doi: 10.1016/j.lfs.2020.117391
da Costa, D. T., Gonçalves, L. T., Giesen, J. A., and Dos Santos, R. L. (2021). Progesterone modulates endothelium-dependent coronary vascular reactivity in SHR. J. Mol. Endocrinol. 66, 171–180. doi: 10.1530/JME-20-0187
Debert, C. T., Ide, K., and Poulin, M. J. (2012). Effects of estrogen and progesterone on cerebrovascular responses to euoxic hypercapnia in women. Climacteric 15, 621–631. doi: 10.3109/13697137.2011.631231
Deenadayalu, V. P., White, R. E., Stallone, J. N., Gao, X., and Garcia, A. J. (2001). Testosterone relaxes coronary arteries by opening the large-conductance, calcium-activated potassium channel. Am. J. Physiol. Heart Circ. Physiol. 281, H1720–H1727. doi: 10.1152/ajpheart.2001.281.4.H1720
Deer, R. R., and Stallone, J. N. (2016). Effects of estrogen on cerebrovascular function: Age-dependent shifts from beneficial to detrimental in small cerebral arteries of the rat. Am. J. Physiol. Heart Circ. Physiol. 310, H1285–H1294. doi: 10.1152/ajpheart.00645.2015
Deutsch, M. B. (2016). Overview of feminizing hormone therapy’, UCSF transgender care. Available online at: https://transcare.ucsf.edu/guidelines/feminizing-hormone-therapy (accessed June 17, 2016).
DeVane, G. W., Czekala, N. M., Judd, H. L., and Yen, S. S. (1975). Circulating gonadotropins, estrogens, and androgens in polycystic ovarian disease. Am. J. Obstet. Gynecol. 121, 496–500. doi: 10.1016/0002-9378(75)90081-2
Dittrich, R., Binder, H., Cupisti, S., Hoffmann, I., Beckmann, M. W., and Mueller, A. (2005). Endocrine treatment of male-to-female transsexuals using gonadotropin-releasing hormone agonist. Exp. Clin. Endocrinol. Diabetes 113, 586–592. doi: 10.1055/s-2005-865900
Endo, Y., Nishimura, J. I., Kobayashi, S., and Kimura, F. (1999). Chronic stress exposure influences local cerebral blood flow in the rat hippocampus. Neuroscience 93, 551–555. doi: 10.1016/s0306-4522(99)00176-1
Geary, G. G., Krause, D. N., and Duckles, S. P. (2000). Gonadal hormones affect diameter of male rat cerebral arteries through endothelium-dependent mechanisms. Am. J. Physiol. Heart Circ. Physiol. 279, H610–H618. doi: 10.1152/ajpheart.2000.279.2.H610
Getahun, D., Nash, R., Flanders, W. D., Baird, T. C., Becerra-Culqui, T. A., Cromwell, L., et al. (2018). Cross-sex hormones and acute cardiovascular events in transgender persons: A cohort study. Ann. Intern. Med. 169, 205–213. doi: 10.7326/M17-2785
Ghorbanian, A., Aiello, B., and Staples, J. (2022). Under-representation of transgender identities in research: The limitations of traditional quantitative survey data. Transgend. Health 7, 261–269. doi: 10.1089/trgh.2020.0107
Gibson, C. L., Constantin, D., Prior, M. J., Bath, P. M., and Murphy, S. P. (2005). Progesterone suppresses the inflammatory response and nitric oxide synthase-2 expression following cerebral ischemia. Exp. Neurol. 193, 522–530. doi: 10.1016/j.expneurol.2005.01.009
Gibson, C. L., Coomber, B., and Murphy, S. P. (2011). Progesterone is neuroprotective following cerebral ischaemia in reproductively ageing female mice. Brain 134(Pt. 7), 2125–2133. doi: 10.1093/brain/awr132
Giltay, E. J., and Gooren, L. J. (2000). Effects of sex steroid deprivation/administration on hair growth and skin sebum production in transsexual males and females. J. Clin. Endocrinol. Metab. 85, 2913–2921. doi: 10.1210/jcem.85.8.6710
Gonzales, R. J., Ghaffari, A., Duckles, S., and Krause, D. (2005). Testosterone treatment increases thromboxane function in rat cerebral arteries. Am. J. Physiol. Heart Circ. Physiol. 289, H578–H585. doi: 10.1152/ajpheart.00958.2004
Gonzales, R., Krause, D., and Duckles, S. (2004). Testosterone suppresses endothelium-dependent dilation of rat middle cerebral arteries. Am. J. Physiol. Heart Circ. Physiol. 286, H552–H560. doi: 10.1152/ajpheart.00663.2003
Goodman, M., Adams, N., Corneil, T., Kreukels, B., Motmans, J., and Coleman, E. (2019). Size and distribution of transgender and gender nonconforming populations: A narrative review. Endocrinol. Metab. Clin. North Am. 48, 303–321. doi: 10.1016/j.ecl.2019.01.001
Hamzah Utariani, A., Semedi, B. P., Avidar, Y. P., and Nurofik, N. (2020). Correlation between middle cerebral artery pulsatility index and optic nerve sheath diameter with intracranial pressure in traumatic and non-traumatic brain injury patients of Dr. Soetomo General Hospital Surabaya. Critical Care Shock 23, 35–42.
Hanff, T. C., Sharrett, A. R., Mosley, T. H., Shibata, D., Knopman, D. S., Klein, R., et al. (2014). Retinal microvascular abnormalities predict progression of brain microvascular disease: An atherosclerosis risk in communities magnetic resonance imaging study. Stroke 45, 1012–1017. doi: 10.1161/STROKEAHA.113.004166
Harrison, J., Grant, J., and Heramn, J. L. (2012). A gender not listed here: Genderqueers, gender rebels, and otherwise in the national transgender discrimination survey. LGBTQ Public Policy J. Harvard Kennedy Schl 2:13.
Hayward, C. S., Kelly, R. P., and Collins, P. (2000). The roles of gender, the menopause and hormone replacement on cardiovascular function. Cardiovasc. Res. 46, 28–49. doi: 10.1016/s0008-6363(00)00005-5
Hurn, P. D., Littleton-Kearney, M. T., Kirsch, J. R., Dharmarajan, A. M., and Traystman, R. J. (1995). Postischemic cerebral blood flow recovery in the female: Effect of 17 beta-estradiol. J. Cereb. Blood Flow Metab. 15, 666–672. doi: 10.1038/jcbfm.1995.82
Iadecola, C. (2017). The neurovascular unit coming of age: A journey through neurovascular coupling in health and disease. Neuron 96, 17–42. doi: 10.1016/j.neuron.2017.07.030
Iorga, A., Cunningham, C. M., Moazeni, S., Ruffenach, G., Umar, S., and Eghbali, M. (2017). The protective role of estrogen and estrogen receptors in cardiovascular disease and the controversial use of estrogen therapy. Biol. Sex Differ. 8:33. doi: 10.1186/s13293-017-0152-8
Irwig, M. S. (2018). Cardiovascular health in transgender people. Rev. Endocr. Metab. Disord. 19, 243–251. doi: 10.1007/s11154-018-9454-3
Kamboj, A., Brown, M. M., and Abel, A. S. (2023). Intracranial hypertension associated with testosterone therapy in female-to-male transgender patients: A case report and literature review. Semin. Ophthalmol. 38, 559–564. doi: 10.1080/08820538.2023.2169578
Karalexi, M. A., Frisell, T., Cnattingius, S., Holmberg, D., Holmberg, M., Kollia, N., et al. (2022). Cardiovascular outcomes in transgender individuals in Sweden after initiation of gender-affirming hormone therapy. Eur. J. Prev. Cardiol. 29, 2017–2026. doi: 10.1093/eurjpc/zwac133
Kilic, D., Kilic, I. D., Sevgican, C. I., Kilic, O., Alatas, E., Arslan, M., et al. (2021). Arterial stiffness measured by cardio-ankle vascular index is greater in non-obese young women with polycystic ovarian syndrome. J. Obstet. Gynaecol. Res. 47, 521–528. doi: 10.1111/jog.14543
Kulprachakarn, K., Ounjaijean, S., Rerkasem, K., Molinsky, R. L., and Demmer, R. T. (2020). Cardiovascular disease risk factors among transgender women in Chiang Mai, Thailand. Am. J. Cardiovasc. Dis. 10, 124–130.
Kumanov, P., Tomova, A., and Kirilov, G. (2007). Testosterone replacement therapy in male hypogonadism is not associated with increase of endothelin-1 levels. Int. J. Androl. 30, 41–47. doi: 10.1111/j.1365-2605.2006.00706.x
Lecce, L., Lam, Y. T., Lindsay, L. A., Yuen, S. C., Simpson, P. J., Handelsman, D. J., et al. (2014). Aging impairs VEGF-mediated, androgen-dependent regulation of angiogenesis. Mol. Endocrinol. 28, 1487–1501. doi: 10.1210/me.2013-1405
Lee, S., Kang, B. M., Shin, M. K., Min, J., Heo, C., Lee, Y., et al. (2015). Chronic stress decreases cerebrovascular responses during rat hindlimb electrical stimulation. Front. Neurosci. 9:462. doi: 10.3389/fnins.2015.00462
Lin, Y., Xie, H., Huang, Z., Zhang, Q., Wilson, A., Hou, J., et al. (2021). The mental health of transgender and gender non-conforming people in China: A systematic review. Lancet Public Health 6, e954–e969. doi: 10.1016/S2468-2667(21)00236-X
Louissaint, A., Rao, S., Leventhal, C., and Goldman, S. A. (2002). Coordinated interaction of neurogenesis and angiogenesis in the adult songbird brain. Neuron 34, 945–960. doi: 10.1016/s0896-6273(02)00722-5
Martinez, C. A., Rikhi, R., Fonseca Nogueira, N., Pester, M. S., Salazar, A. S., Ashinne, B., et al. (2023). Estrogen-based gender-affirming hormone therapy and subclinical cardiovascular disease in transgender women with HIV. LGBT Health doi: 10.1089/lgbt.2023.0010 [Epub ahead of print].
Meyer, I. H., Brown, T., Herman, J., Reisner, S., and Bockting, W. (2017). Demographic characteristics and health status of transgender adults in select US regions: Behavioral risk factor surveillance system, 2014. Am. J. Public Health 107, 582–589. doi: 10.2105/AJPH.2016.303648
Milionis, C., Ilias, I., and Koukkou, E. (2022). Progesterone in gender-affirming therapy of trans women. World J. Biol. Chem. 13, 66–71. doi: 10.4331/wjbc.v13.i3.66
Milner, T. A., Thompson, L. I., Wang, G., Kievits, J. A., Martin, E., Zhou, P., et al. (2010). Distribution of estrogen receptor β containing cells in the brains of bacterial artificial chromosome transgenic mice. Brain Res. 1351, 74–96. doi: 10.1016/j.brainres.2010.06.038
Minalga, B., Chung, C., Davids, J. D., Martin, A., Perry, N. L., and Shook, A. (2022). Research on transgender people must benefit transgender people. Lancet 399:628. doi: 10.1016/S0140-6736(21)02806-3
Mitterling, K. L., Spencer, J. L., Dziedzic, N., Shenoy, S., McCarthy, K., Waters, E. M., et al. (2010). Cellular and subcellular localization of estrogen and progestin receptor immunoreactivities in the mouse hippocampus. J. Comp. Neurol. 518, 2729–2743. doi: 10.1002/cne.22361
Mohamed, S., and Hunter, M. S. (2018). Transgender women’s experiences and beliefs about hormone therapy through and beyond mid-age: An exploratory UK study. Int. J. Transgend. 20, 98–107. doi: 10.1080/15532739.2018.1493626
Moir, M. E., Corkery, A. T., Senese, K. A., Miller, K. B., Pearson, A. G., Loggie, N. A., et al. (2023). Age at natural menopause impacts cerebrovascular reactivity and brain structure. Am. J. Physiol. Regul. Integr. Comp. Physiol. 324, R207–R215. doi: 10.1152/ajpregu.00228.2022
Moss, H. E. (2015). Retinal vascular changes are a marker for cerebral vascular diseases. Curr. Neurol. Neurosci. Rep. 15:40. doi: 10.1007/s11910-015-0561-1
Nakamura, A., Watanabe, M., Sugimoto, M., Sako, T., Mahmood, S., Kaku, H., et al. (2013). Dose-response analysis of testosterone replacement therapy in patients with female to male gender identity disorder. Endocr. J. 60, 275–281. doi: 10.1507/endocrj.ej12-0319
New, G., Duffy, S. J., Harper, R. W., and Meredith, I. T. (2000). Long-term oestrogen therapy is associated with improved endothelium-dependent vasodilation in the forearm resistance circulation of biological males. Clin. Exp. Pharmacol. Physiol. 27, 25–33. doi: 10.1046/j.1440-1681.2000.03195.x
New, G., Timmins, K. L., Duffy, S. J., Tran, B. T., O’Brien, R. C., Harper, R. W., et al. (1997). Long-term estrogen therapy improves vascular function in male to female transsexuals. J. Am. Coll. Cardiol. 29, 1437–1444. doi: 10.1016/s0735-1097(97)00080-6
Novella, S., Pérez-Cremades, D., Mompeón, A., and Hermenegildo, C. (2019). Mechanisms underlying the influence of oestrogen on cardiovascular physiology in women. J. Physiol. 597, 4873–4886. doi: 10.1113/JP278063
Owen-Smith, A. A., Woodyatt, C., Sineath, R. C., Hunkeler, E. M., Barnwell, T., Graham, A., et al. (2016). Perceptions of barriers to and facilitators of participation in health research among transgender people. Transgend. Health. 1, 187–196. doi: 10.1089/trgh.2016.0023
Palta, P., Sharrett, A. R., Wei, J., Meyer, M. L., Kucharska-Newton, A., Power, M. C., et al. (2019). Central arterial stiffness is associated with structural brain damage and poorer cognitive performance: The ARIC study. J. Am. Heart Assoc. 8:e011045. doi: 10.1161/JAHA.118.011045
Parker, W. H., Jacoby, V., Shoupe, D., and Rocca, W. (2009). Effect of bilateral oophorectomy on Women’s long-term health. Womens Health 5, 565–576. doi: 10.2217/WHE.09.42
Perusquía, M. (2003). Androgen-induced vasorelaxation: A potential vascular protective effect. Exp. Clin. Endocrinol. Diabetes 111, 55–59. doi: 10.1055/s-2003-39229
Perusquía, M., Flores-Soto, E., Sommer, B., Campuzano-González, E., Martínez-Villa, I., Martínez-Banderas, A. I., et al. (2015). Testosterone-induced relaxation involves L-type and store-operated Ca2+ channels blockade, and PGE 2 in guinea pig airway smooth muscle. Pflugers Arch. 467, 767–777. doi: 10.1007/s00424-014-1534-y
Polderman, K. H., Stehouwer, C. D., van Kamp, G. J., Dekker, G. A., Verheugt, F. W., and Gooren, L. J. (1993). Influence of sex hormones on plasma endothelin levels. Ann. Intern. Med. 118, 429–432. doi: 10.7326/0003-4819-118-6-199303150-00006
Pribish, A. M., and Iwamoto, S. J. (2023). Cardiovascular disease and feminizing gender-affirming hormone therapy: Implications for the provision of safe and lifesaving care. Curr. Opin. Physiol. 33:100650. doi: 10.1016/j.cophys.2023.100650
Prior, J. C. (2019). Progesterone is important for transgender women’s therapy-applying evidence for the benefits of progesterone in Ciswomen. J. Clin. Endocrinol. Metab. 104, 1181–1186. doi: 10.1210/jc.2018-01777
Roberts, T. K., Kraft, C. S., French, D., Ji, W., Wu, A. H., Tangpricha, V., et al. (2014). Interpreting laboratory results in transgender patients on hormone therapy. Am. J. Med. 127, 159–162. doi: 10.1016/j.amjmed.2013.10.009
Robison, L. S., Gannon, O. J., Salinero, A. E., and Zuloaga, K. L. (2019). Contributions of sex to cerebrovascular function and pathology. Brain Res. 1710, 43–60. doi: 10.1016/j.brainres.2018.12.030
Rodriguez, G., Warkentin, S., Risberg, J., and Rosadini, G. (1988). Sex differences in regional cerebral blood flow. J. Cereb. Blood Flow Metab. 8, 783–789. doi: 10.1038/jcbfm.1988.133
Roof, R. L., and Hall, E. D. (2000). Estrogen-related gender difference in survival rate and cortical blood flow after impact-acceleration head injury in rats. J. Neurotrauma 17, 1155–1169. doi: 10.1089/neu.2000.17.1155
Round, R., Gokool, N., Manica, G., Paschall, L., and Foulcer, S. (2023). Improving access for and experience of transgender and non-binary patients in clinical research: Insights from a transgender patient focus group and targeted literature reviews. Contemp. Clin. Trials 131:107243. doi: 10.1016/j.cct.2023.107243
Ruediger, S. L., Koep, J. L., Keating, S. E., Pizzey, F. K., Coombes, J. S., and Bailey, T. G. (2021). Effect of menopause on cerebral artery blood flow velocity and cerebrovascular reactivity: Systematic review and meta-analysis. Maturitas 148, 24–32. doi: 10.1016/j.maturitas.2021.04.004
Ruediger, S. L., Pizzey, F. K., Koep, J. L., Coombes, J. S., Askew, C. D., and Bailey, T. G. (2023). Comparison of peripheral and cerebral vascular function between premenopausal, early and late postmenopausal females. Exp. Physiol. 108, 518–530. doi: 10.1113/EP090813
Opgaard, O. S, Duckles, S. P., and Krause, D. N. (2002). Regional differences in the effect of oestrogen on vascular tone in isolated rabbit arteries. Pharmacol. Toxicol. 91, 77–82. doi: 10.1034/j.1600-0773.2002.910206.x
Safer, J. D., Coleman, E., Feldman, J., Garofalo, R., Hembree, W., Radix, A., et al. (2016). Barriers to healthcare for transgender individuals. Curr. Opin. Endocrinol. Diabetes Obes. 23, 168–171. doi: 10.1097/MED.0000000000000227
Sairenchi, T., Iso, H., Yamagishi, K., Irie, F., Okubo, Y., Gunji, J., et al. (2011). Mild retinopathy is a risk factor for cardiovascular mortality in Japanese with and without hypertension: The ibaraki prefectural health study. Circulation 124, 2502–2511. doi: 10.1161/CIRCULATIONAHA.111.049965
Santizo, R. A., Xu, H. L., Galea, E., Muyskens, S., Baughman, V. L., and Pelligrino, D. A. (2002). Combined endothelial nitric oxide synthase upregulation and caveolin-1 downregulation decrease leukocyte adhesion in pial venules of ovariectomized female rats. Stroke 33, 613–616. doi: 10.1161/hs0202.102363
Sarkey, S., Azcoitia, I., Garcia-Segura, L. M., Garcia-Ovejero, D., and DonCarlos, L. L. (2008). Classical androgen receptors in non-classical sites in the brain. Horm. Behav. 53, 753–764. doi: 10.1016/j.yhbeh.2008.02.015
Sheridan, P. J. (1983). Androgen receptors in the brain: What are we measuring? Endocr. Rev. 4, 171–178. doi: 10.1210/edrv-4-2-171
Shin, J., Han, K., Jung, J. H., Park, H. J., Kim, W., Huh, Y., et al. (2022). Age at menopause and risk of heart failure and atrial fibrillation: A nationwide cohort study. Eur. Heart J. 43, 4148–4157. doi: 10.1093/eurheartj/ehac364
Shughrue, P. J., and Merchenthaler, I. (2001). Distribution of estrogen receptor beta immunoreactivity in the rat central nervous system. J. Comp. Neurol. 436, 64–81.
Sieveking, D. P., Lim, P., Chow, R. W., Dunn, L., Bao, S., McGrath, K. C., et al. (2010). A sex-specific role for androgens in angiogenesis. J. Exp. Med. 207, 345–352. doi: 10.1084/jem.20091924
Singer, J., Trollor, J. N., Baune, B. T., Sachdev, P. S., and Smith, E. (2014). Arterial stiffness, the brain and cognition: A systematic review. Ageing Res. Rev. 15, 16–27. doi: 10.1016/j.arr.2014.02.002
Skinner, B. D., Davies, R. J., Weaver, S. R., Cable, N. T., Lucas, S. J., and Lucas, R. A. (2021). A systematic review and meta-analysis examining whether changing ovarian sex steroid hormone levels influence cerebrovascular function. Front. Physiol. 12:687591. doi: 10.3389/fphys.2021.687591
Skinner, B. D., Weaver, S. R., Lucas, S. J., and Lucas, R. A. (2023). Menstrual phase influences cerebrovascular responsiveness in females but may not affect sex differences. Front. Physiol. 13:1035452. doi: 10.3389/fphys.2022.1035452
Spizzirri, G., Eufrásio, R., Lima, M. C., de Carvalho Nunes, H. R., Kreukels, B. P., Steensma, T. D., et al. (2021). Proportion of people identified as transgender and non-binary gender in Brazil. Sci. Rep. 11:2240. doi: 10.1038/s41598-021-81411-4
Steventon, J. J., Lancaster, T. M., Baker, E. S., Bracher-Smith, M., Escott-Price, V., Ruth, K. S., et al. (2023). Menopause age, reproductive span and hormone therapy duration predict the volume of medial temporal lobe brain structures in postmenopausal women. Psychoneuroendocrinology 158:106393. doi: 10.1016/j.psyneuen.2023.106393
Sunday, L., Tran, M. M., Krause, D. N., and Duckles, S. P. (2006). Estrogen and progestagens differentially modulate vascular proinflammatory factors. Am. J. Physiol. Endocrinol. Metab. 291, E261–E267. doi: 10.1152/ajpendo.00550.2005
Tep-areenan, P., Kendall, D. A., and Randall, M. D. (2002). Testosterone-induced vasorelaxation in the rat mesenteric arterial bed is mediated predominantly via potassium channels. Br. J. Pharmacol. 135, 735–740. doi: 10.1038/sj.bjp.0704522
Tirabassi, G., Delli Muti, N., Corona, G., Maggi, M., and Balercia, G. (2013). Androgen receptor gene CAG repeat polymorphism regulates the metabolic effects of testosterone replacement therapy in male postsurgical hypogonadotropic hypogonadism. Int. J. Endocrinol. 2013:816740. doi: 10.1155/2013/816740
Todd, C. M., Yu, A., Lay, C., and Lagman-Bartolome, A. M. (2023). Effect of testosterone therapy on migraine frequency and disability in two transgender patients: A case report. BMJ Case Rep. 16:e251895. doi: 10.1136/bcr-2022-251895
Tostes, R. C., Nigro, D., Fortes, Z. B., and Carvalho, M. H. (2003). Effects of estrogen on the vascular system. Braz J Med Biol Res. 36, 1143–1158. doi: 10.1590/s0100-879x2003000900002
Tüten, A., Hamzaoğlu, K., Gönen, B., Tüten, N., and Uçar, D. (2022). Does exogenous androgen use affect the retinal blood flow: An OCTA study in transgender men. Eur. J. Ophthalmol. 32, 1570–1576. doi: 10.1177/11206721211020639
Unger, C. A. (2016). Hormone therapy for transgender patients. Transl. Androl. Urol. 5, 877–884. doi: 10.21037/tau.2016.09.04
Valentine, S. E., and Shipherd, J. C. (2018). A systematic review of social stress and mental health among transgender and gender non-conforming people in the United States. Clin. Psychol. Rev. 66, 24–38. doi: 10.1016/j.cpr.2018.03.003
Wardman, J. H., Jensen, M. N., Andreassen, S. N., Styrishave, B., Wilhjelm, J. E., Sinclair, A. J., et al. (2023). Modelling idiopathic intracranial hypertension in rats: Contributions of high fat diet and testosterone to intracranial pressure and cerebrospinal fluid production. Fluids Barriers CNS 20:44. doi: 10.1186/s12987-023-00436-1
Wassmann, S., Bäumer, A. T., Strehlow, K., van Eickels, M., Grohé, C., Ahlbory, K., et al. (2001). Endothelial dysfunction and oxidative stress during estrogen deficiency in spontaneously hypertensive rats. Circulation 103, 435–441. doi: 10.1161/01.cir.103.3.435
Wierckx, K., Elaut, E., Declercq, E., Heylens, G., De Cuypere, G., Taes, Y., et al. (2013). Prevalence of cardiovascular disease and cancer during cross-sex hormone therapy in a large cohort of trans persons: A case-control study. Eur. J. Endocrinol. 169, 471–478. doi: 10.1530/EJE-13-0493
Wilson, B. D., Bouton, L. J. A., Badgett, M. V. L., and Macklin, M. L. (2023). LGBT Poverty in the United States.’, UCLA: The Williams Institute. [Preprint]. Available online at: https://escholarship.org/uc/item/0660h520 (accessed September 5, 2023).
Wiseman, S. J., Zhang, J. F., Gray, C., Hamid, C., Valdés Hernández, M. D., Ballerini, L., et al. (2023). Retinal capillary microvessel morphology changes are associated with vascular damage and dysfunction in cerebral small vessel disease. J. Cereb. Blood Flow Metab. 43, 231–240. doi: 10.1177/0271678X221135658
Yoshida, S., Aihara, K., Ikeda, Y., Sumitomo-Ueda, Y., Uemoto, R., Ishikawa, K., et al. (2013). Androgen receptor promotes sex-independent angiogenesis in response to ischemia and is required for activation of vascular endothelial growth factor receptor signaling. Circulation 128, 60–71. doi: 10.1161/CIRCULATIONAHA.113.001533
Yue, P., Chatterjee, K., Beale, C., Poole-Wilson, P. A., and Collins, P. (1995). Testosterone relaxes rabbit coronary arteries and aorta. Circulation 91, 1154–1160. doi: 10.1161/01.cir.91.4.1154
Keywords: hormone, cerebrovascular, transgender, hormone replacement therapy (HRT), LGBT, vascular health
Citation: Wright ME and Murphy K (2023) A mini-review of the evidence for cerebrovascular changes following gender-affirming hormone replacement therapy and a call for increased focus on cerebrovascular transgender health. Front. Hum. Neurosci. 17:1303871. doi: 10.3389/fnhum.2023.1303871
Received: 28 September 2023; Accepted: 31 October 2023;
Published: 22 November 2023.
Edited by:
Riccardo Manca, Brunel University London, United KingdomReviewed by:
Giancarlo Spizzirri, University of São Paulo, BrazilCopyright © 2023 Wright and Murphy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Melissa Emily Wright, d3JpZ2h0bWVAY2FyZGlmZi5hYy51aw==
 Melissa Emily Wright
Melissa Emily Wright Kevin Murphy
Kevin Murphy