- 1Beijing Key Laboratory of Mental Disorders, National Clinical Research Center for Mental Disorders & National Center for Mental Disorders, Beijing Anding Hospital, Capital Medical University, Beijing, China
- 2Advanced Innovation Center for Human Brain Protection, Capital Medical University, Beijing, China
Introduction: Many patients with bipolar disorder (BD) need hospitalization, while the number of hospital beds for these patients is limited. Managing the length of stay (LOS) is an effective solution to this issue. Research on LOS and its influencing factors in BD is limited in China. This study aimed to identify the factors relevant to LOS in different polarities in Chinese patients with BD.
Method: This was a real-world, cross-sectional study. Data were obtained from the electronic medical record system. Patients admitted to Beijing Anding Hospital between Jan 2014 and Dec 2017 and diagnosed with BD were included. Demographic information, clinical characteristics, and biochemical variables were collected. Patients were classified into short and long LOS groups based on a cutoff value. A univariate study and a multivariate logistic regression analysis were performed to identify variables related to LOS in various BD polarities. The receiver operating characteristic (ROC) analysis was utilized to evaluate the discrimination accuracy of the regression model.
Result: Four thousand six hundred and seventy-five visits from 4,451 individuals were included in the analysis. For the whole sample, unmarried status, psychotic features, and family history of mental disorders were positively associated with long LOS (all p < 0.05). There was an additive interaction between a family history of mental disorders and polarities (p < 0.05). For manic episodes, unmarried status, psychotic features, and family history of mental disorders were positively associated with long LOS (all p < 0.05). For depressive episodes, psychotic features and high-density lipoprotein cholesterol (HDLC) levels were positively associated with long LOS (all p < 0.05). For mixed states, unmarried status was positively associated with long LOS, while low-density lipoprotein cholesterol (LDLC) levels were negatively associated with LOS (all p < 0.05). The area under the curve (AUC) values for depressive episodes, manic episodes, and mixed states in the combined model were 0.587, 0.553, and 0.619, respectively (all p < 0.05).
Discussion: The findings suggested that LOS correlates differed by polarity, with marital status, psychotic features, a family history of mental disorders, and lipid levels strongly linked with LOS in patients with BD.
Introduction
Bipolar disorder (BD) is a prevalent, chronic, and recurrent mental disorder that has become a leading cause of global disease burden (Alonso et al., 2011; Gore et al., 2011; Webb et al., 2014; Schaffer et al., 2015). A significant proportion of patients with BD may present with psychotic features (e.g., hallucinations, delusions) or hazardous behaviors that may harm themselves or others, which result in hospitalization. Despite the benefits of inpatient treatment, a longer length of stay (LOS) may be counterproductive. Longer LOS is frequently associated with more negative outcomes, such as low patient satisfaction (Bird et al., 2020), mental illness stigma, deterioration of social relationships, and threats to the living situation and career opportunities (Gopalakrishna et al., 2015), which may impact patients’ attitudes toward further psychiatric care (Shi, 2019; Błądziński et al., 2020). China has a significant population of people with BD, but psychiatric ward beds are limited (Que et al., 2019). Longer LOS may rationally and efficiently impact healthcare resource allocation and use. Psychiatric hospitalization accounts for a significant share of mental health expenses, and lengthier psychiatric LOS might incur substantial economic consequences (Habermeyer et al., 2018). Therefore, it is crucial to investigate the variables that may lead to extended LOS for patients with BD in China.
Over the past few decades, several studies conducted in Western countries have reported that the LOS for BD varies across countries, 21.0 days for Sweden (Ragazan et al., 2019), 17.3–20.3 days for Austria (Fellinger et al., 2018), 32.6 days for Ethiopia (Addisu et al., 2015), and 41.2 days for England (Jacobs et al., 2015). Age, gender, marital status, age of onset, course of the disease, and suicidal ideation or attempt were often cited as demographic and clinical correlates of LOS (Jacobs et al., 2015; Deng et al., 2018; Fellinger et al., 2018; Ragazan et al., 2019). However, these studies have some limitations. First, LOS is related to sociocultural factors, while the conclusions obtained from European countries may not be applicable in China. Second, the different polarities of BD (manic episodes/depressive episodes/mixed states) are not distinguished, which may affect the outcome of LOS. Third, most earlier research lacked biochemical variables in patients with BD that have been increasingly shown to be associated with the development and prognosis of the disease.
After reviewing the relevant literature, we selected lipid profiles, immunological components, and hormones for biochemical variables. Previous studies have suggested that aberrant lipid metabolism is prevalent in BD (Chung et al., 2007; Kennedy et al., 2021) and that elevated lipid levels are related to smaller brain structure (Kennedy et al., 2021), more severe mood symptoms (Atmaca et al., 2002; Huang et al., 2018) and cognitive dysfunction (Qiu et al., 2022), lower sleep quality (Soreca et al., 2012), more impulsivity (Tatlidil Yaylaci et al., 2014), and increased drug use (Kumar et al., 2017), all of which may impact LOS. Numerous pieces of evidence continuously have suggested that alterations in the immune system, namely the activation of immune cells and the production of inflammatory compounds, may be associated with changes in the central nervous system (CNS) of BD patients (Pinto et al., 2018). Convincing evidence has shown that altered levels of immune and inflammatory factors are associated with disease risk, symptom profile, cognitive function, treatment response, and prognosis, which affects LOS (Hayes et al., 2017; Park et al., 2017; Bulut et al., 2019; Cuomo et al., 2021). The hypothalamic-pituitary-adrenal (HPA) axis, the hypothalamic-pituitary-thyroid (HPT) axis, and the hypothalamic-pituitary-gonadal (HPG) axis are the three major subsystems of the human neuroendocrine system. Hormonal imbalances in these axes alter the serotonin, dopamine, and glutamate systems in brain areas, which may result in mood, behavior, and cognitive alterations (Niu et al., 2019). Previous studies have shown that indices of hypothalamus-pituitary-adrenal (HPA) axis function is associated with the severity of symptoms of BD (Belvederi Murri et al., 2014). Thyroid hormone levels vary among polarities in BD (Zhao et al., 2021) and are associated with response to medication (Bauer and Whybrow, 2021). Hypothyroidism is associated with rapid transitions to depression or mania in some patients (Buoli et al., 2017). In addition, clinical studies have revealed that gonadal hormones are associated with mood episodes and suicide attempts (Sher et al., 2012). It is concluded that biochemical variables of lipid metabolism, neuroimmune, inflammation, and neuroendocrine may be associated with LOS. According to our knowledge, little research has examined the link between biochemical variables and LOS.
This cross-sectional research aimed to evaluate the demographic, clinical, and biochemical determinants of LOS in various polarities among patients with BD in China. This research provided information for optimizing psychiatric care and allocating mental health resources effectively.
Materials and methods
Participants and study design
This study was a real-world, cross-sectional study. Data were obtained from Beijing Anding Hospital, Capital Medical University, one of China’s national medical centers for psychiatric disorders. Patients admitted to Beijing Anding Hospital between Jan 2014 and Dec 2017 and diagnosed with BD were included. Patients were between 18 and 60 (including 18 and 60 years old) and of either gender. For further analysis, BD sub-diagnoses were categorized according to polarity into manic episodes (F31.0–F31.2), depressive episodes (F31.3–F31.5), and mixed states (F31.6). ICD-10-diagnoses F31.7–9 (F31.7 BD, now in remission, F31.8 other BD, F31.9 BD, undefined) were excluded from the study because they were insufficiently specific to be classified.
Independent variables included demographic information, clinical characteristics, and biochemical variables. The dependent variable, LOS, was encoded as a binary variable with “short LOS” defined as ≤28 days and “long LOS” as >28 days. Twenty-eight days are selected as the cutoff value for two reasons: (1) the median LOS for this sample was 28 days, and (2) previous studies on factors associated with LOS in major depressive disorder and schizophrenia also used 28 days as a cutoff value (Cheng et al., 2022a, b).
Measures
Demographic information
At the index time of admission, demographic information was obtained, including age, gender (male/female), and marital status (married/unmarried status; unmarried status comprised single, divorced, and widowed).
Clinical characteristics
The patients’ clinical characteristics included the age of onset, course of the disease, comorbid psychotic features, family history of mental disorders, and current polarity (manic episodes/depressive episodes/mixed states).
Biochemical variables
Biochemical variables were measured the day after admission using a fully automated biochemical analyzer. Lipid profiles include total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDLC), and low-density lipoprotein cholesterol (LDLC). Immune and inflammatory factors include immunoglobulin G (IgG), immunoglobulin A (IgA), immunoglobulin M (IgM), complement C3 (C3), complement C4 (C4), C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR). Hormones include adrenocorticotropic hormone (ACTH), total triiodothyronine (TT3), total thyroxine (TT4), prolactin (PRL), cortisol (COR), testosterone (TES), estradiol (E2), and progesterone (PGN).
Statistical analysis
SPSS version 26.0 (IBMCorp., New York, United States) was used for data analysis. The Shapiro-Wilk test was employed to determine if the data distribution was normal. All non-normally distributed continuous variables were reported using the median and quartile range. The differences between the two groups were compared using the rank sum test. The Chi-square test was used to compare categorical data expressed as numbers and proportions (%). The screening criterion was set at p < 0.1 to avoid omitting significant variables. The correlations of LOS in the whole sample were investigated using multivariate logistic regression. To determine if the influence of each variable on LOS varied by polarity, an interaction study was conducted between polarity and each variable. Then, multivariate logistic regression analysis was done again to investigate characteristics related to LOS in various BD polarities. A Receiver Operator Characteristic Curve (ROC) study was done to evaluate the LOS prediction accuracy of this regression model. p < 0.05 was used as the statistical threshold.
Results
Description statistics
Four-thousand six-hundred and seventy-five visits from 4,451 unique individuals were included in the analysis (3,531 individuals were hospitalized once, 826 twice, 70 three times, 17 four times, 5 five times, 1 six times, and 1 nine times). The whole sample had the highest percentage of manic episodes (manic episodes: 62.87%, depressive episodes: 23.91%, mixed states: 13.22%).
The median age of the whole sample was relatively young (31 years for manic episodes, 32 years for depressive episodes, and 29 years for mixed states). In manic episodes, the proportions of males and females were roughly equal. In depressive episodes and mixed states, the proportion of women was slightly higher than that of men. The proportion of unmarried status was significantly higher than married status in each polarity.
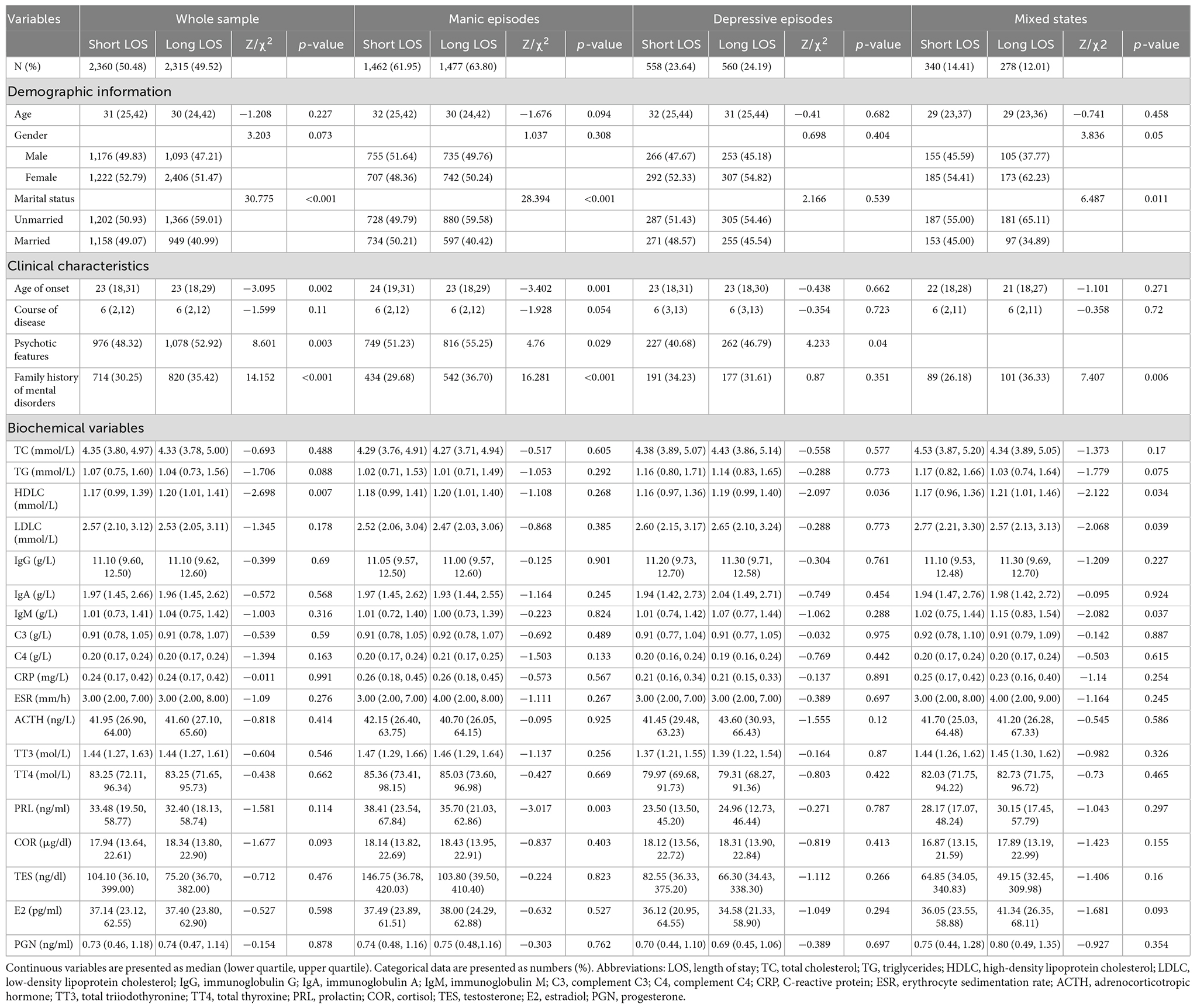
In terms of clinical features, more than half of the patients in each polarity had an onset in their early adulthood (the median was 22/23 years). The median course of the disease was six years. Approximately 50 percent of individuals with manic or depressive episodes had psychotic features. More than one-third of patients have family members who used to suffer from mental illness. The LOS of the whole group varied substantially between 1 day and 344 days (1–344 days for manic episodes, 2–211 days for depressive episodes, and 2–161 days for mixed states). The whole sample’s median LOS was 28 days (28 days for manic episodes, 29 days for depressive episodes, and 27 days for mixed states). The average LOS for the whole sample was 31 days (31 days for manic episodes, 31 days for depressive episodes, and 29 days for mixed states). See Table 1.
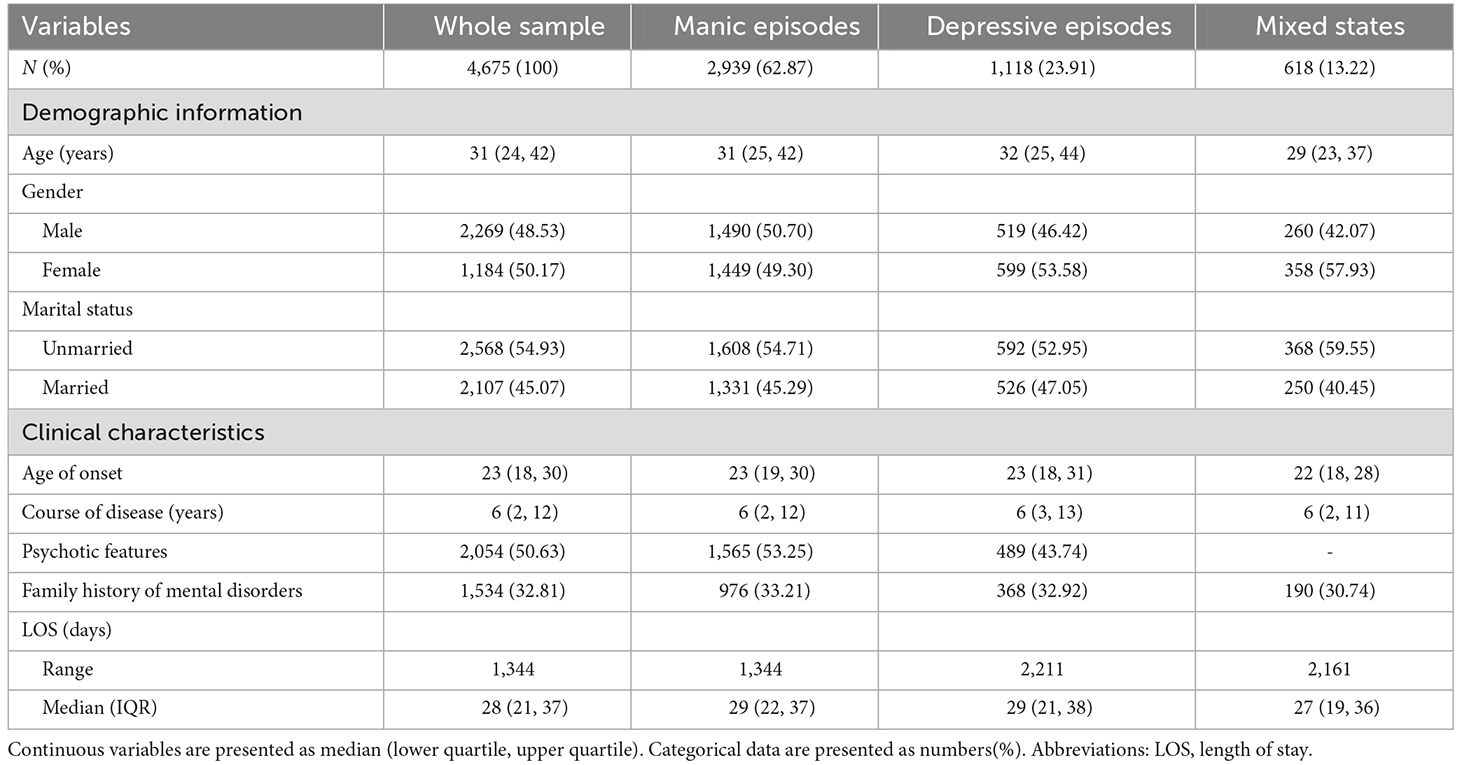
Table 1. Demographic information and clinical characteristics of the whole sample and the three polarities.
Univariate analysis of LOS in the whole sample and different polarities
The long LOS group had larger proportions of females, unmarried status, an earlier age of onset, psychotic characteristics and a family history of mental disorders, a lower TG level, and higher levels of HDLC and COR than the short LOS group for the whole sample (all p < 0.1).
In patients with manic episodes, the long LOS group was younger, had an earlier start and a longer duration of the disease, had a larger percentage of unmarried status, psychotic features, and a family history of mental disorders, and had a lower PRL level than the short LOS group (all p < 0.1).
Compared to the short LOS group, individuals with depressive episodes in the long LOS group exhibited a larger percentage of psychotic characteristics and a higher HDLC level (all p < 0.1).
Compared to the short LOS group, the long LOS group of patients with mixed states had greater proportions of females, unmarried status, and family history of mental disorders, lower levels of TG and LDLC, and higher levels of HDLC, IgM, and E2 (all p < 0.1). See Table 2.
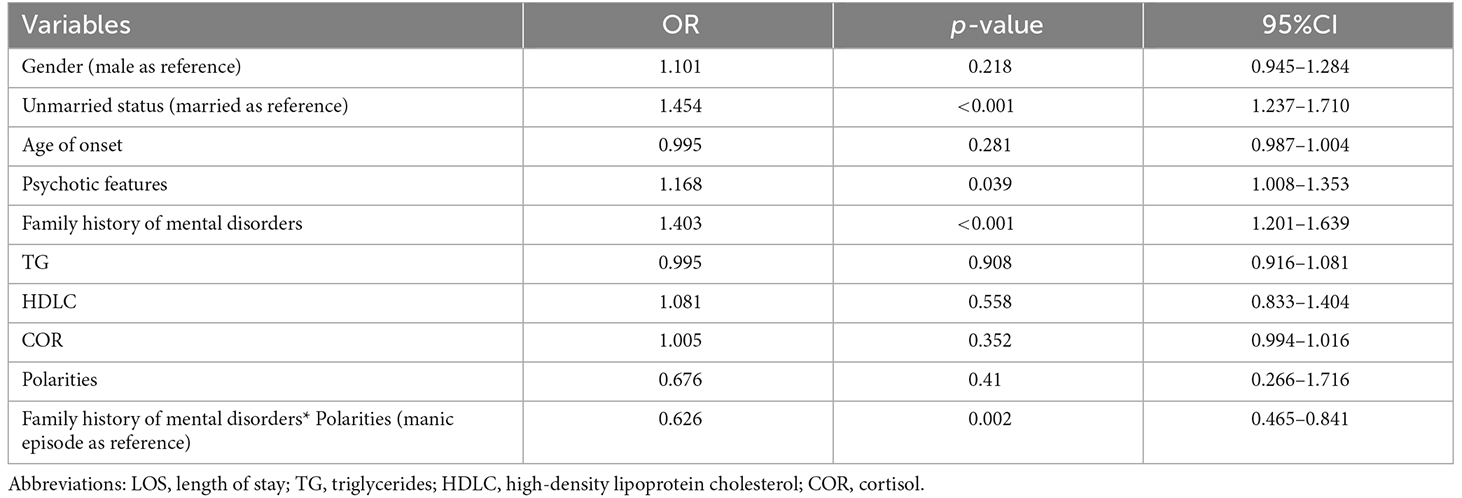
Multivariate analysis of the whole sample
Multiple logistic regression analysis revealed that unmarried status (OR = 1.454, 95%CI = 1.237–1.710, p < 0.001), psychotic features (OR = 1.168, 95%CI = 1.008–1.353, p = 0.039) and family history of mental disorders (OR = 1.403, 95%CI = 1.201–1.639, p < 0.001) were positively associated with long LOS for the whole sample. There was an additive interaction between a family history of mental disorders and polarity with respect to the probability of a long LOS (OR = 0.626, 95%CI = 0.465–0.841, p = 0.002). See Table 3.
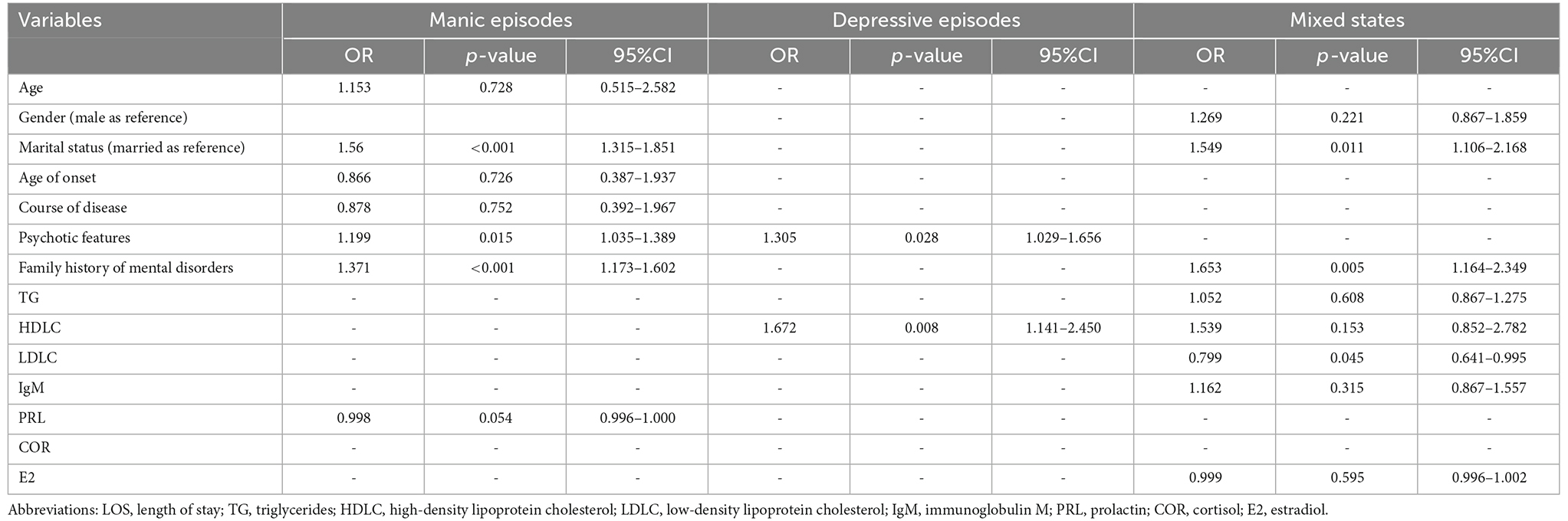
Multivariate analysis of various polarities
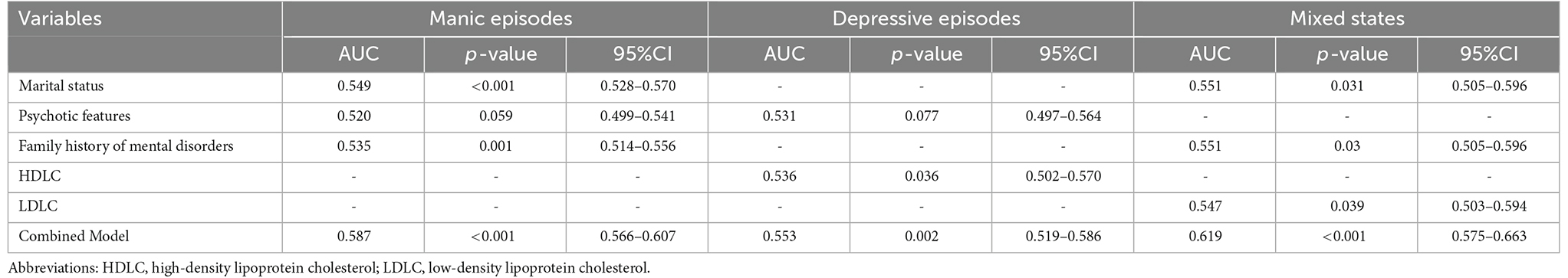
The results showed that unmarried status (OR = 1.560, 95%CI = 1.315–1.851, p < 0.001), psychotic features (OR = 1.199, 95%CI = 1.035–1.389, p = 0.015), and family history of mental disorders (OR = 1.371, 95%CI = 1.173–1.602, p < 0.001) were positively correlated with protracted LOS in patients with manic episodes. See Table 4 and Figure 1. The AUC of each variable varied between 0.520 and 0.549. The combination model increased diagnostic accuracy with an AUC value of 0.587 (95% CI = 0.566–0.607, p < 0.001). See Table 5.
Figure 1. Forest plots depicting logistic regression results of LOS in the three polarities. Abbreviations: HDLC, high-density lipoprotein cholesterol; LDLC, low-density lipoprotein cholesterol; LOC, length of stay.
Long LOS was strongly associated with psychotic features (OR = 1.305, 95%CI = 1.029–1.656, p = 0.028) and HDLC levels (OR = 1.672, 95%CI = 1.141–2.450, p = 0.008) in patients with depressive episodes. See Table 4 and Figure 1. Every variable’s AUC varied between 0.531 and 0.536. The combination model increased diagnostic accuracy with an AUC value of 0.553 (95% CI = 0.519–0.586, p = 0.002). See Table 5.
Unmarried status (OR = 1.549, 95%CI = 1.106–2.168, p = 0.011) and family history of mental illnesses (OR = 1.653, 95%CI = 1.164–2.349, p = 0.005) were strongly linked with protracted LOS in patients with mixed states. A negative correlation was seen between LDLC levels and LOS (OR = 0.799, 95%CI = 0.641–0.995, p = 0.045). See Table 4 and Figure 1. Every variable’s AUC ranged between 0.547 and 0.551. The combination model enhanced diagnosis accuracy with an AUC value of 0.619 (95% CI = 0.575–0.663, p < 0.001). See Table 5.
Discussion
According to our knowledge, this is the first study to investigate the demographic, clinical, and biochemical associations with LOS in various polarities among Chinese patients with BD. Our findings indicated that, for the whole sample, unmarried status, psychotic features, and a family history of mental disorders were positively associated with long LOS; however, the interaction between a family history of mental disorders and the polarity was adversely associated with long LOS. Long LOS was positively correlated with unmarried status, psychotic features, and a family history of mental disorders for manic episodes. Long LOS was positively associated with psychotic features and HDLC values for depressed episodes. Long LOS was positively correlated with unmarried status and a family history of mental disorders, whereas LDLC levels were adversely correlated.
The average LOS of Chinese BD patients in this study was 31 days, longer than that of Sweden (Ragazan et al., 2019) and Austria (Fellinger et al., 2018), shorter than that of Ethiopia (Addisu et al., 2015) and England (Jacobs et al., 2015). Possible explanations for the shorter LOS in Sweden and Austria include variations in help-seeking behavior. A greater percentage of identification of emotional and behavioral issues, for instance, might lead to early treatment seeking and encourage quicker recovery (Gaine et al., 2021). This may also be a result of the community-based rehabilitation treatment system for mental illnesses, which allows patients to return to their families and society before all symptoms have disappeared (Kar Ray et al., 2019; Florentin et al., 2021). However, this conclusion may also be affected by a deficiency in medical resources since fewer accessible beds, and higher inpatient demand may result in earlier discharge.
In this study, unmarried status was a risk factor for long LOS for manic episodes and mixed states. Although the results of earlier research on the influence of marriage on LOS are contradictory, more studies have revealed that married patients had a reduced chance of having extended hospital stays than unmarried patients (Masters et al., 2014; Cheng et al., 2022a), which is consistent with our findings. A possible explanation is that marital relationships enhance social networks, providing emotional and financial support. Studies have found that married patients with psychiatric disorders are more resilient than unmarried patients and that resilience is crucial to their recovery (Wingo et al., 2010).
This study showed that psychotic features were a risk factor for long LOS for manic and depressive episodes, which is consistent with previous studies (Tulloch et al., 2011; Dimitri et al., 2018; Ragazan et al., 2019). Ragazan et al. analyzed all inpatients with a first diagnosis of BD in the Swedish population register from 2005 to 2014 and found that psychotic features were a strong predictor of long LOS for manic and depressive episodes (Ragazan et al., 2019). A prospective cohort study across five countries found that psychotic disorder was the strongest predictor of long LOS (Dimitri et al., 2018). A meta-analysis also showed that psychotic features were associated with increased LOS (Tulloch et al., 2011). One possible explanation is that psychotic features may lead to more severe illness and less self-awareness, which results in longer hospital stays. Another explanation is that BD with psychotic features is more likely to be misdiagnosed as schizophrenia-spectrum disorders, and inappropriate treatment may prolong LOS.
This study indicated that a family history of mental disorders was a risk factor for prolonged LOS in manic episodes and mixed states. Similar results were observed in pediatric and adolescent psychiatric disorder inpatients (Zanato et al., 2021). The significant correlation between a family history of mental disorders and hospitalization duration demonstrates genetic susceptibility’s impact. Literature reveals a high relationship between a family history of mental disorders, especially with afflicted parents, and the likelihood of mental disorders and hospitalization in offspring (Reupert et al., 2013; Tossone et al., 2014; Glahn et al., 2019). The presence of mental disorders in more than one family member may lead to poor communication and low family system cohesion, resulting in more intra-family conflict, making it more challenging to stabilize patients in the acute phase and leading to longer LOS (Glahn et al., 2019). Interestingly, our investigation revealed an interaction between a family history of mental disorders and the polarity of BD, such that the impact of a family history of mental disorders on LOS is dependent on polarity.
To our knowledge, this is the first study to evaluate the association between lipid levels and LOS in patients with BD. High HDLC levels were shown to be a contributing factor for prolonged LOS in depressive episodes, whereas high LDLC levels were protective in mixed states. This might be because lipid levels influence the intensity of symptoms and other prognostic variables in BD. Cholesterol is critical for membrane stability and neurotransmission, while disordered cholesterol metabolism may trigger serious central neuroinflammation, leading to abnormal monoaminergic neurotransmission (De Melo et al., 2017; Reponen et al., 2020). Few studies have examined the association between clinical symptoms and lipid levels in BD. Shapiro et al. discovered that among the BD-mixed/hypomanic subgroup, greater mania ratings were related to a higher TG level, a higher TG/HDLC ratio, and a lower HDLC level (Shapiro et al., 2022). Bartoli et al. performed a meta-analysis to investigate variations in lipid profiles between suicide attempters and non-attempters with BD, but they did not find any significant differences (Bartoli et al., 2017). It should be noted that many factors can affect lipid levels and that psychotropic drug use, poor lifestyle, and other factors often exacerbate dyslipidemia in patients with BD. In conclusion, the study of the association between lipid levels, LOS, and clinical characteristics in BD is still preliminary, and further long-term follow-up studies are needed.
Limitation
Some limitations must still be indicated. Before doing longitudinal investigations, it is difficult to determine causation and directionality from cross-sectional data. Second, lipid levels are affected by several variables, including age, gender, body mass index (BMI), and current psychotropic medication usage, and we cannot rule out the effect of confounding variables. Third, this study did not distinguish between patients with first and recurrent hospitalizations, which could lead to confounding bias. Finally, the AUC of the model in this study ranged from 0.553 to 0.619, which is close to the random model. This may be due to insufficient variables covered in the study, such as quantitative measures of symptom severity, electroconvulsive therapy (Patel et al., 2019), psychotropic medication type and dosage (Deng et al., 2018; Fornaro et al., 2018; Lee et al., 2020), and health insurance (Masciale et al., 2021).
Conclusion
In conclusion, this study investigated the factors associated with LOS in BD in China. The findings revealed that correlates of LOS varied by polarity, with marital status, psychotic features, family history of mental disorders, and lipid levels significantly associated with LOS. These results emphasize that in the context of inadequate healthcare resources, it is advisable to consider the impact of these critical factors on LOS during the initial patient assessment in order to more appropriately allocate healthcare resources.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the institutional review board of the Beijing Anding Hospital, Capital Medical University. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
YR: study design. WW, JX, and YR: data collection, analysis, and interpretation. WW and JX: drafting of the manuscript. YR, JD, SL, and GX: critical manuscript revision. All co-authors: approval of the final version for publication. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the National Natural Science Foundation of China (81760651), Beijing Municipal Administration of Hospitals Incubating Program (PX2021070), and the Scientific Research Fund of Beijing Anding Hospital (YJ2022-06).
Acknowledgments
We would like to acknowledge all participants involved in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
BD, Bipolar disorder; LOS, Length of stay; ROC, Receiver operating characteristic; AUC, Area under the curve; HPA, Hypothalamus-pituitary-adrenal; TC, Total cholesterol; TG, Triglycerides; HDLC, High-density lipoprotein cholesterol; LDLC, Low-density lipoprotein cholesterol; IgG, Immunoglobulin G; IgA, Immunoglobulin A; IgM, Immunoglobulin M; C3, Complement C3; C4, Complement C4; CRP, C-reactive protein; ESR, Erythrocyte sedimentation rate; ACTH, Hormones: adrenocorticotropic hormone; TT3, Total triiodothyronine; TT4, Total thyroxine; PRL, Prolactin; COR, Cortisol; TES, Testosterone; E2, Estradiol; PGN, Progesterone; BMI, Body mass index.
References
Addisu, F., Wondafrash, M., Chemali, Z., Dejene, T., and Tesfaye, M. (2015). Length of stay of psychiatric admissions in a general hospital in Ethiopia: a retrospective study. Int. J. Ment. Health Syst. 9:13. doi: 10.1186/s13033-015-0006-x
Alonso, J., Petukhova, M., Vilagut, G., Chatterji, S., Heeringa, S., Üsün, T. B., et al. (2011). Days out of role due to common physical and mental conditions: results from the WHO world mental health surveys. Mol. Psychiatry 16, 1234–1246. doi: 10.1038/mp.2010.101
Atmaca, M., Kuloglu, M., Tezcan, E., Ustundag, B., and Bayik, Y. (2002). Serum leptin and cholesterol levels in patients with bipolar disorder. Neuropsychobiology 46, 176–179. doi: 10.1159/000067809
Bartoli, F., Di Brita, C., Crocamo, C., Clerici, M., and Carrà, G. (2017). Lipid profile and suicide attempt in bipolar disorder: a meta-analysis of published and unpublished data. Prog. Neuropsychopharmacol. Biol. Psychiatry 79, 90–95. doi: 10.1016/j.pnpbp.2017.06.008
Bauer, M., and Whybrow, P. C. (2021). Role of thyroid hormone therapy in depressive disorders. J. Endocrinol. Invest. 44, 2341–2347. doi: 10.1007/s40618-021-01600-w
Belvederi Murri, M., Pariante, C., Mondelli, V., Masotti, M., Atti, A. R., Mellacqua, Z., et al. (2014). HPA axis and aging in depression: systematic review and meta-analysis. Psychoneuroendocrinology 41, 46–62. doi: 10.1016/j.psyneuen.2013.12.004
Bird, V., Miglietta, E., Giacco, D., Bauer, M., Greenberg, L., Lorant, V., et al. (2020). Factors associated with satisfaction of inpatient psychiatric care: a cross country comparison. Psychol. Med. 50, 284–292. doi: 10.1017/S0033291719000011
Błądziński, P., Hat, M., Daren, A., Kruk, D., Depukat, A., Cichocki, Ł., et al. (2020). Subjective evaluation of admission and first days of hospitalization at a psychiatric ward from the perspective of patients. Adv. Psychiatry Neurol. 29, 39–53. doi: 10.5114/ppn.2020.94694
Bulut, M., Çatı, S., Güneş, M., Kaya, M. C., Kaplan, İ., and Özkan, M. (2019). Evaluation of serum inflammatory markers in treatment-resistant manic patients and adequate responder manic patients. Psychiatry Res. 272, 73–79. doi: 10.1016/j.psychres.2018.12.073
Buoli, M., Serati, M., and Altamura, A. C. (2017). Biological aspects and candidate biomarkers for rapid-cycling in bipolar disorder: a systematic review. Psychiatry Res. 258, 565–575. doi: 10.1016/j.psychres.2017.08.059
Cheng, P., Wang, L., Xu, L., Zhou, Y., Zhang, L., and Li, W. (2022a). Factors related to the length of stay for patients with schizophrenia: a retrospective study. Front. Psychiatry 12:818254. doi: 10.3389/fpsyt.2021.818254
Cheng, P., Wang, L., Xu, L., Zhou, Y., Zhao, G., Zhang, L., et al. (2022b). Factors related to the length of stay for major depressive disorder patients in China: a real-world retrospective study. Front. Public Health 10:892133. doi: 10.3389/fpubh.2022.892133
Chung, K.-H., Tsai, S. Y., and Lee, H. C. (2007). Mood symptoms and serum lipids in acute phase of bipolar disorder in Taiwan. Psychiatry Clin. Neurosci. 61, 428–433. doi: 10.1111/j.1440-1819.2007.01689.x
Cuomo, A., Koukouna, D., Spiti, A., Barillà, G., Goracci, A., Bolognesi, S., et al. (2021). Biomarkers, inflammation and bipolar disorder: association between the improvement of bipolar disorder severity and the improvement in c-reactive protein levels after 7 days of inpatient treatment. Front. Psychiatry 12:803034. doi: 10.3389/fpsyt.2021.803034
De Melo, L. G. P., Nunes, S. O. V., Anderson, G., Vargas, H. O., Barbosa, D. S., Galecki, P., et al. (2017). Shared metabolic and immune-inflammatory, oxidative and nitrosative stress pathways in the metabolic syndrome and mood disorders. Prog. Neuropsychopharmacol. Biol. Psychiatry 78, 34–50. doi: 10.1016/j.pnpbp.2017.04.027
Deng, H., Mohite, S., Suchting, R., Nielsen, D. A., and Okusaga, O. O. (2018). Impact of synthetic cannabinoid use on hospital stay in patients with bipolar disorder versus schizophrenia, or other psychotic disorders. Psychiatry Res. 261, 248–252. doi: 10.1016/j.psychres.2017.12.089
Dimitri, G., Giacco, D., Bauer, M., Bird, V. J., Greenberg, L., Lasalvia, A., et al. (2018). Predictors of length of stay in psychiatric inpatient units: does their effect vary across countries? Eur. Psychiatry 48, 6–12. doi: 10.1016/j.eurpsy.2017.11.001
Fellinger, M., Waldhör, T., Blüml, V., Williams, N., and Vyssoki, B. (2018). Influence of gender on inpatient treatment for bipolar disorder: an analysis of 60,607 hospitalisations. J. Affect. Disord. 225, 104–107. doi: 10.1016/j.jad.2017.08.007
Florentin, S., Neumark, Y., Raskin, S., Bdolah-Abram, T., and Rosca, P. (2021). Differential effect of community rehabilitation reform on hospitalizations of patients with chronic psychotic disorders with and without substance use disorder, Israel, 1991–2016. Adm. Policy Ment. Health 48, 354–362. doi: 10.1007/s10488-020-01077-4
Fornaro, M., Iasevoli, F., Novello, S., Fusco, A., Anastasia, A., De Berardis, D., et al. (2018). Predictors of hospitalization length of stay among re-admitted treatment-resistant bipolar disorder inpatients. J. Affect. Disord. 228, 118–124. doi: 10.1016/j.jad.2017.12.009
Gaine, G. S., Nealis, L. J., Zhou, H., Purdon, S. E., and Abba-Aji, A. (2021). Identification of psychiatric inpatient recovery trajectories using routine outcome monitoring with emerging adults. Psychiatry Res. 302:114000. doi: 10.1016/j.psychres.2021.114000
Glahn, D. C., Nimgaonkar, V. L., RaventóS, H., Contreras, J., Mcintosh, A. M., Thomson, P. A., et al. (2019). Rediscovering the value of families for psychiatric genetics research. Mol. Psychiatry 24, 523–535. doi: 10.1038/s41380-018-0073-x
Gopalakrishna, G., Ithman, M., and Malwitz, K. (2015). Predictors of length of stay in a psychiatric hospital. Int. J. Psychiatry Clin. Pract. 19, 238–244. doi: 10.3109/13651501.2015.1062522
Gore, F. M., Bloem, P. J., Patton, G. C., Ferguson, J., Joseph, V., Coffey, C., et al. (2011). Global burden of disease in young people aged 10–24 years: a systematic analysis. Lancet 377, 2093–2102. doi: 10.1016/S0140-6736(11)60512-6
Habermeyer, B., De Gennaro, H., Frizi, R. C., Roser, P., and Stulz, N. (2018). Factors associated with length of stay in a swiss mental hospital. Psychiatr. Q. 89, 667–674. doi: 10.1007/s11126-018-9569-4
Hayes, J. F., Khandaker, G. M., Anderson, J., Mackay, D., Zammit, S., Lewis, G., et al. (2017). Childhood interleukin-6, C-reactive protein and atopic disorders as risk factors for hypomanic symptoms in young adulthood: a longitudinal birth cohort study. Psychol. Med. 47, 23–33. doi: 10.1017/S0033291716001574
Huang, Y.-J., Tsai, S.-Y., Chung, K.-H., Chen, P.-H., Huang, S.-H., and Kuo, C.-J. (2018). State-dependent alterations of lipid profiles in patients with bipolar disorder. Int. J. Psychiatry Med. 53, 273–281. doi: 10.1177/0091217417749786
Jacobs, R., Gutacker, N., Mason, A., Goddard, M., Gravelle, H., Kendrick, T., et al. (2015). Determinants of hospital length of stay for people with serious mental illness in England and implications for payment systems: a regression analysis. BMC Health Serv. Res. 15:439. doi: 10.1186/s12913-015-1107-6
Kar Ray, M., Lombardo, C., Syed, Z., Patel, N., Denman, C., and Jones, P. B. (2019). Embedding recovery to transform inpatient mental health care: the 333 model. Psychiatr. Serv. 70, 465–473. doi: 10.1176/appi.ps.201800284
Kennedy, K. G., Islam, A. H., Grigorian, A., Fiksenbaum, L., Mitchell, R. H. B., Mccrindle, B. W., et al. (2021). Elevated lipids are associated with reduced regional brain structure in youth with bipolar disorder. Acta Psychiatr. Scand. 143, 513–525. doi: 10.1111/acps.13278
Kumar, A., Narayanaswamy, J. C., Venkatasubramanian, G., Raguram, R., Grover, S., and Aswath, M. (2017). Prevalence of metabolic syndrome and its clinical correlates among patients with bipolar disorder. Asian J. Psychiatr. 26, 109–114. doi: 10.1016/j.ajp.2017.01.020
Lee, H. K., Prabhudesai, S., Vadukapuram, R., Eskander, N., and Patel, R. S. (2020). Combination regimen with lithium and antipsychotic in bipolar manic episodes: impact on adult hospitalization length of stay. Cureus 12:e8568. doi: 10.7759/cureus.8568
Masciale, M., Dongarwar, D., and Salihu, H. M. (2021). Predictors of prolonged length of stay in suicidal children transferred to psychiatric facilities. Hosp. Pediatr. 11, 366–373. doi: 10.1542/hpeds.2020-001230
Masters, G. A., Baldessarini, R. J., Öngür, D., and Centorrino, F. (2014). Factors associated with length of psychiatric hospitalization. Compr. Psychiatry 55, 681–687. doi: 10.1016/j.comppsych.2013.11.004
Niu, Z., Yang, L., Wu, X., Zhu, Y., Chen, J., and Fang, Y. (2019). The relationship between neuroimmunity and bipolar disorder: mechanism and translational application. Neurosci. Bull. 35, 595–607. doi: 10.1007/s12264-019-00403-7
Park, M., Newman, L. E., Gold, P. W., Luckenbaugh, D. A., Yuan, P., Machado-Vieira, R., et al. (2017). Change in cytokine levels is not associated with rapid antidepressant response to ketamine in treatment-resistant depression. J. Psychiatr. Res. 84, 113–118. doi: 10.1016/j.jpsychires.2016.09.025
Patel, R. S., Jain, S. B., and Youssef, N. A. (2019). Electroconvulsive treatment utilization for the inpatient management of severe manic episodes of bipolar disorder. J. ECT 35, 195–200. doi: 10.1097/YCT.0000000000000587
Pinto, J. V., Passos, I. C., Librenza-Garcia, D., Marcon, G., Schneider, M. A., Conte, J. H., et al. (2018). Neuron-glia interaction as a possible pathophysiological mechanism of bipolar disorder. Curr. Neuropharmacol. 16, 519–532. doi: 10.2174/1570159X15666170828170921
Qiu, Y., Li, S., Teng, Z., Tan, Y., Xu, X., Yang, M., et al. (2022). Association between abnormal glycolipid level and cognitive dysfunction in drug-naïve patients with bipolar disorder. J. Affect. Disord. 297, 477–485. doi: 10.1016/j.jad.2021.10.100
Que, J., Lu, L., and Shi, L. (2019). Development and challenges of mental health in China. Gen. Psychiatry 32:e100053. doi: 10.1136/gpsych-2019-100053
Ragazan, D. C., Eberhard, J., Ösby, U., and Berge, J. (2019). Gender influence on the bipolar disorder inpatient length of stay in Sweden, 2005–2014: a register-based study. J. Affect. Disord. 256, 183–191. doi: 10.1016/j.jad.2019.05.052
Reponen, E. J., Dieset, I., Tesli, M., Mørch, R. H., Aas, M., Vedal, T. S. J., et al. (2020). Atherogenic lipid ratios related to myeloperoxidase and C-reactive protein levels in psychotic disorders. Front. Psychiatry 11:672. doi: 10.3389/fpsyt.2020.00672
Reupert, A. E., Maybery, D. J., and Kowalenko, N. M. (2013). Children whose parents have a mental illness: prevalence, need and treatment. Med. J. Aust. 199, S7–S9. doi: 10.5694/mja11.11200
Schaffer, A., Isometsä, E. T., Tondo, L., Moreno, D. H., Sinyor, M., Kessing, L. V., et al. (2015). Epidemiology, neurobiology and pharmacological interventions related to suicide deaths and suicide attempts in bipolar disorder: part I of a report of the international society for bipolar disorders task force on suicide in bipolar disorder. Aust. N Z J. Psychiatry 49, 785–802. doi: 10.1177/0004867415594427
Shapiro, L. R., Kennedy, K. G., Dimick, M. K., and Goldstein, B. I. (2022). Elevated atherogenic lipid profile in youth with bipolar disorder during euthymia and hypomanic/mixed but not depressive states. J. Psychosom. Res. 156:110763. doi: 10.1016/j.jpsychores.2022.110763
Sher, L., Grunebaum, M. F., Sullivan, G. M., Burke, A. K., Cooper, T. B., Mann, J. J., et al. (2012). Testosterone levels in suicide attempters with bipolar disorder. J. Psychiatr. Res. 46, 1267–1271. doi: 10.1016/j.jpsychires.2012.06.016
Shi, S. (2019). What will the development of psychiatry in China be in 10 years? Gen. Psychiatr. 32:e100025. doi: 10.1136/gpsych-2018-100025
Soreca, I., Wallace, M. L., Frank, E., Hasler, B. P., Levenson, J. C., and Kupfer, D. J. (2012). Sleep duration is associated with dyslipidemia in patients with bipolar disorder in clinical remission. J. Affect. Disord. 141, 484–487. doi: 10.1016/j.jad.2012.01.046
Tatlidil Yaylaci, E., Kesebir, S., and Güngördü, Ö. (2014). The relationship between impulsivity and lipid levels in bipolar patients: does temperament explain it? Compr. Psychiatry 55, 883–886. doi: 10.1016/j.comppsych.2014.02.002
Tossone, K., Jefferis, E., Bhatta, M. P., Bilge-Johnson, S., and Seifert, P. (2014). Risk factors for rehospitalization and inpatient care among pediatric psychiatric intake response center patients. Child Adolesc. Psychiatry Ment. Health 8:27. doi: 10.1186/1753-2000-8-27
Tulloch, A. D., Fearon, P., and David, A. S. (2011). Length of stay of general psychiatric inpatients in the United States: systematic review. Adm. Policy Ment. Health 38, 155–168. doi: 10.1007/s10488-010-0310-3
Webb, R. T., Lichtenstein, P., Larsson, H., Geddes, J. R., and Fazel, S. (2014). Suicide, hospital-presenting suicide attempts and criminality in bipolar disorder: examination of risk for multiple adverse outcomes. J. Clin. Psychiatry 75, e809–e816. doi: 10.4088/JCP.13m08899
Wingo, A. P., Baldessarini, R. J., Holtzheimer, P. E., and Harvey, P. D. (2010). Factors associated with functional recovery in bipolar disorder patients. Bipolar Disord. 12, 319–326. doi: 10.1111/j.1399-5618.2010.00808.x
Zanato, S., Miscioscia, M., Traverso, A., Gatto, M., Poli, M., Raffagnato, A., et al. (2021). A retrospective study on the factors associated with long-stay hospitalization in a child neuropsychiatry unit. Healthcare (Basel) 9:1241. doi: 10.3390/healthcare9091241
Keywords: bipolar disorder, polarity, length of stay, correlates, China, cross-sectional study
Citation: Wang W, Du J, Li S, Xie G, Xu J and Ren Y (2023) Demographic, clinical and biochemical correlates of the length of stay for different polarities in Chinese inpatients with bipolar disorder: A real-world study. Front. Hum. Neurosci. 17:1135403. doi: 10.3389/fnhum.2023.1135403
Received: 31 December 2022; Accepted: 06 February 2023;
Published: 01 March 2023.
Edited by:
Chuanliang Han, Shenzhen Institute of Advanced Technology (CAS), ChinaReviewed by:
Dengyun Ge, Shenzhen Institute of Advanced Technology (CAS), ChinaJinghong Chen, Shanghai Jiao Tong University, China
Copyright © 2023 Wang, Du, Li, Xie, Xu and Ren. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jinjie Xu, c2ptZWRpY2FsX3hqakAxNjMuY29t; Yanping Ren, cmVueWFucGluZ0BjY211LmVkdS5jbg==
 Wei Wang1
Wei Wang1 Jing Du
Jing Du Jinjie Xu
Jinjie Xu Yanping Ren
Yanping Ren