
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
MINI REVIEW article
Front. Hum. Neurosci. , 29 November 2022
Sec. Cognitive Neuroscience
Volume 16 - 2022 | https://doi.org/10.3389/fnhum.2022.932820
This article is part of the Research Topic Visual Impairments and Fitness to Drive View all 8 articles
 Eleni Papageorgiou1†
Eleni Papageorgiou1† Daniil Tsirelis2†
Daniil Tsirelis2† Katerina Lazari1
Katerina Lazari1 Vasileios Siokas2
Vasileios Siokas2 Efthimios Dardiotis2
Efthimios Dardiotis2 Evangelia E. Tsironi1,3*
Evangelia E. Tsironi1,3*Background: Impaired driving ability in patients with Alzheimer’s disease (AD) is associated with a decline in cognitive processes and a deterioration of their basic sensory visual functions. Although a variety of ocular abnormalities have been described in patients with AD, little is known about the impact of those visual disorders on their driving performance.
Aim: Aim of this mini-review is to provide an update on the driving ability of patients with dementia and summarize the primary visual disorders affecting their driving behavior.
Methods: Databases were screened for studies investigating dementia, associated visual abnormalities and driving ability.
Results: There is consistent evidence that dementia affects driving ability. Patients with dementia present with a variety of visual disorders, such as visual acuity reduction, visual field defects, impaired contrast sensitivity, decline in color vision and age-related pathological changes, that may have a negative impact on their driving ability. However, there is a paucity in studies describing the impact of oculovisual decline on the driving ability of AD subjects. A bidirectional association between cognitive and visual impairment (VI) has been described.
Conclusion: Given the bidirectional association between VI and dementia, vision screening and cognitive assessment of the older driver should aim to identify at-risk individuals and employ timely strategies for treatment of both cognitive and ocular problems. Future studies should characterize the basic visual sensory status of AD patients participating in driving studies, and investigate the impact of vision abnormalities on their driving performance.
Dementia is characterized by deterioration in cognitive function beyond what might be expected from the usual consequences of biological aging (World Health Organization [WHO], 2021). Currently more than 55 million people worldwide have been diagnosed with dementia, with Alzheimer’s disease (AD) being the most common form of dementia (World Health Organization [WHO], 2021). Driving is a highly complicated task that requires multiple cognitive functions, such as attention, visuoperceptual and visuospatial abilities, which may be considerably compromised in individuals with dementia (Reger et al., 2004; Hird et al., 2016).
Intact vision is one of the essential requirements for safe driving, as more than 90% of the sensory information during driving is considered to be visual. Recent evidence has suggested increased motor vehicle crash risk with binocular visual field impairment (Kasneci et al., 2014; Wood et al., 2022). Visual acuity (VA) has been weakly related to crash involvement (Owsley and McGwin, 1999) and there is no evidence of increased crash risk in drivers with mild VA impairment (Wood et al., 2022). As the retina is a developmental outgrowth of the diencephalon, it is also affected by neurodegeneration, and dementia has been associated with a variety of visual disorders from the retina to the visual cortex. Those alterations could have a negative impact on driving ability (Katz and Rimmer, 1989; Sadun and Bassi, 1990) and visual impairment (VI) has been considered one of the early symptoms of dementia (Kusne et al., 2017). Visual abnormalities, such as reduced contrast sensitivity, visual field defects and loss of color vision have been often described in AD patients (Katz and Rimmer, 1989). Additionally, recent advances of in vivo ocular imaging have also revealed retinal and optic nerve alterations in AD patients, such as retinal ganglion cell (RGC) loss, nerve fiber layer atrophy, retinal thinning, amyloid β-protein (Aβ) accumulation, and amyloid-related neurodegeneration in the retina (Curcio and Drucker, 1993; Berisha et al., 2007; Perrin et al., 2009; Guo et al., 2010; Jindahra et al., 2010).
As the world population is aging quickly and one in three dementia patients still drives (Foley et al., 2000; Silverstein, 2008), it is crucial to understand the primary visual disorders affecting the driving ability of AD patients, in order to ensure on-road safety without violating individual autonomy for fit-to-drive individuals. Although there are several reports on driving with dementia, studies assessing the driving ability of persons with dementia in regard to their VI are scarce. The objective of this mini-review is to provide an update on the driving ability of individuals with AD and summarize the visual disorders affecting their driving behavior.
A PubMed search of articles published from January 2000 to April 2022 on the driving ability and oculo-visual disorders of persons with AD was performed (human and English language only). Selected key articles published before 2000 were also included. Searches included a combination of the following terms: cognitive impairment, dementia, Alzheimer’s disease, driving, on-road test, driving simulator, neuropsychological tests, traffic accidents, visual acuity, visual search, retinal imaging, and visual field. The references were then reviewed for pertinent articles, resulting in 20 eligible studies (Table 1).
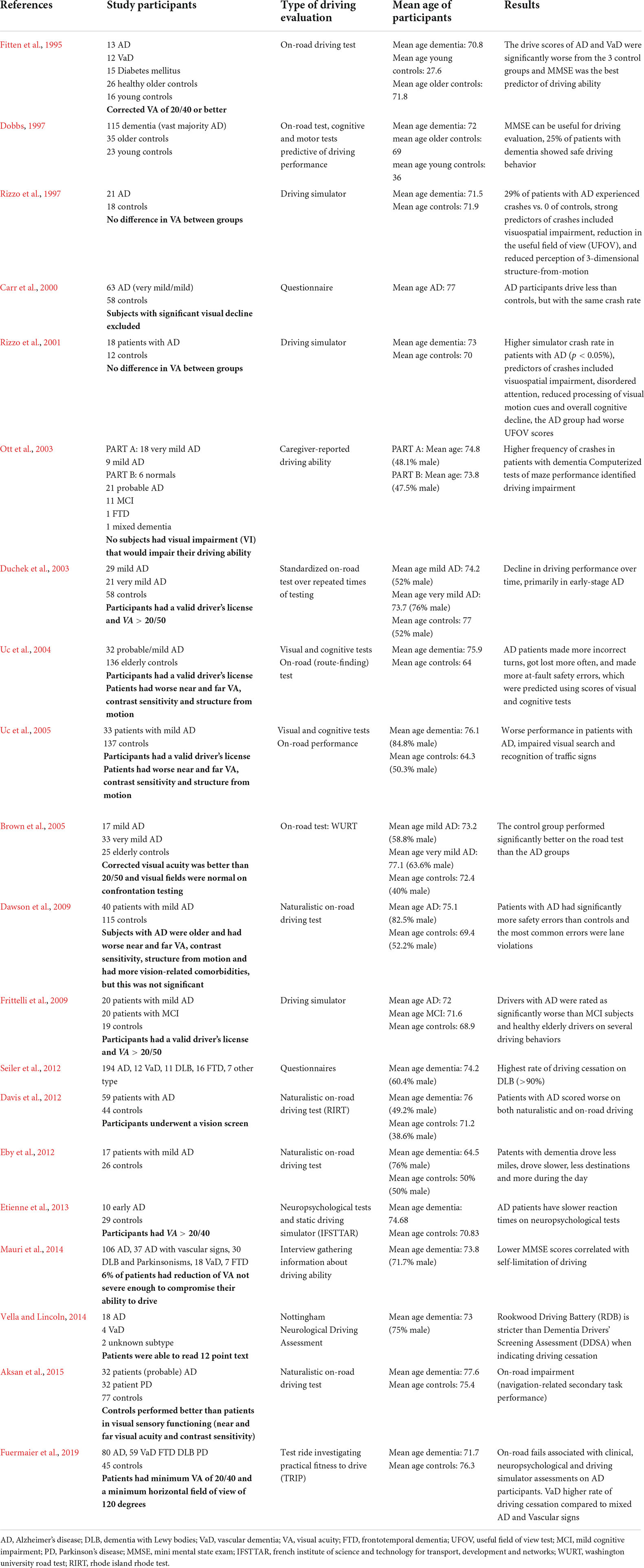
Table 1. Baseline characteristics of studies examining driving aspects in patients with cognitive decline and dementia.
Driving is inevitably a complex visuoperceptual and motor task, which is largely dependent on intact acquisition and processing of visual information. Numerous studies have attempted to define the impact of vision disorders on driving ability by assessing visual measures, such as visual field, VA, contrast sensitivity, glare sensitivity, and useful field of view (UFOV). However, the minimum requirements for the visual function of drivers are highly variable across countries and research is still ongoing. Most studies have identified a weak or no relationship between VA and increased crash risk, however, VA is included as a general measure of vision in the licensing standards of most countries (Owsley and McGwin, 1999; Wood, 2019). A recent systematic review reported no evidence of increased crash risk with mild VA impairment, but increased crash risk with binocular visual field impairment (Wood et al., 2022). The minimum binocular field in Europe should be at least 120° in the horizontal meridian and approximately evenly divided to the left and right of fixation (EU Working Group, 2009). Additionally, no significant defects should be within 20° above and below fixation (EU Working Group, 2009). The UFOV test additionally assesses visual attention and visual processing speed and has been related to crash involvement in older adults (Sekuler and Ball, 1986; Owsley and McGwin, 1999). Impairment of contrast sensitivity has been also linked to deterioration of driving performance in some studies (Owsley and McGwin, 1999). Specific eye conditions of the elderly, who may suffer from dementia as well, have a negative impact on driving performance and safety. Cataract compromises VA, visual field, contrast sensitivity, increases glare, and higher crash risk has been reported in older adults with cataracts (Owsley and McGwin, 1999; Wood and Carberry, 2004; Swan et al., 2019; Wood, 2019). Age-related macular degeneration (AMD) causes deterioration of VA and central field loss and may be associated with impaired driving ability (Wood, 2019). Drivers with visual field loss from glaucoma also report several driving difficulties and display higher collision risk (Wood, 2019). Finally, individuals with homonymous hemianopia are prohibited from driving in many countries, however, some of them may exhibit safe driving skills by means of compensatory eye and head movements (Owsley and McGwin, 1999; Papageorgiou et al., 2012; Kasneci et al., 2014; Bowers, 2016). Although a systematic review showed mixed evidence regarding the impact of cataract, glaucoma, age-related macular degeneration, and homonymous field loss on motor vehicle collision risk, it is clear that the presence of those conditions in older, at-risk for dementia adults deserves careful consideration regarding their fitness to drive (Wood et al., 2022).
A summary of the studies assessing the driving ability of patients with AD is presented in chronological order in Table 1. Eleven studies used on-road driving tests, four studies used a driving simulator and five studies used questionnaires and interviews for assessment of driving ability.
Alzheimer’s disease (AD) is the most common type of dementia (Nichols et al., 2022). It is a major socio-economic issue, and it is expected that that the total number of people suffering from AD in 2050 will be 13.8 million (Hebert et al., 2013). Several risk factors seem to influence the incidence of AD, with age being the most important (Guerreiro and Bras, 2015). Clinically, AD is mainly characterized by deficits in memory, language, executive, and visuospatial domains (Dubois et al., 2021; Graff-Radford et al., 2021). The impairment of those cognitive and visuospatial functions affects the driving ability of people with dementia and it has been reported that drivers with AD are 2.5–4.7 times more likely than age-matched controls to be involved in vehicle collisions (Friedland et al., 1988; Tuokko et al., 1995). Additionally, the majority of patients with AD voluntarily cease or limit driving (Carr and Ott, 2010) and some of them adjust their driving habits, i.e., they drive fewer miles per year, avoid driving in unfamiliar situations, and drive with another person (Davis et al., 2012; Feng et al., 2020; Davis and Owens, 2021). On the other hand, many drivers with mild dementia are able to pass an on-road driving test (Duchek et al., 2003; Brown et al., 2005; Ott et al., 2008; Iverson et al., 2010).
Studies on the driving ability of persons with AD are heterogenous in terms of the tools used for driving assessment and do not always have consistent results. Most authors have concluded that neuropsychological batteries, such as the Mini-Mental State Examination (MMSE), the Rookwood Driving Battery (RDB), and the Dementia Drivers’ Screening Assessment (DDSA), can be used as indicators for driving ability in conjunction with simulator and on-road tests (Dobbs, 1997; Mauri et al., 2014; Vella and Lincoln, 2014).
Most naturalistic and standardized on-road tests suggest that AD patients perform more driving safety errors and their driving ability is inferior to that of healthy elderly individuals (Zuin et al., 2002; Uc et al., 2004; Lincoln et al., 2006; Dawson et al., 2009; Aksan et al., 2015; Barco et al., 2015). Recently, Davis et al. (2020) showed that drivers with dementia undergoing a license review were far more likely to have their license denied than those without dementia (69.2% vs. 10.3%). Fuermaier et al. (2019) found that individuals with AD, who failed the on-road test, had worse results on operational, tactical and visual aspects of driving compared to individuals with AD who passed the on-road test. In a study by Uc et al. (2005), AD patients reported a significantly lower number of both landmarks and traffic signs, and visual and cognitive screening tests were able to predict the impairment of visual search and identification of roadside landmarks.
Driving simulators have been an effective alternative to the on-road tests for assessing fitness to drive in patients with neurological conditions, due to their safety profile, use of standardized interfaces, and availability of various repeatable scenarios (Etienne et al., 2013). A preliminary study in the Iowa driving stimulator found that 29% of AD patients experienced a crash versus none in the control group (Rizzo et al., 1997). Static spatial contrast sensitivity and UFOV were compromised in AD patients and visual and cognitive evaluations were able to predict patients who would have a crash (Rizzo et al., 1997). Interestingly, some patients of the AD group who experienced a crash, were looking directly at the road but did not avoid the crash. A possible explanation was the “looking without seeing” attitude, which has been described in patients with dorsolateral lesions of the visual cortex due to stroke or AD (Rizzo and Hurtig, 1987; Hof et al., 1990; Mendez et al., 1990; Rizzo, 1993; Davis et al., 2020).
Most studies agree that persons with dementia are more likely to fail a road test than healthy controls and that even mild dementia is associated with impaired driving abilities and a substantially higher risk of failing road tests (Chee et al., 2017). In order to ensure traffic safety, a large body of literature has focused on the understanding of factors associated with impaired driving ability of AD patients and the development of appropriate test batteries to identify unsafe AD drivers. Cognitive processes related to driving errors in AD include attention, memory, decision making, processing speed, executive functioning, and visuospatial orientation (Estevez-Gonzalez et al., 2003; Uc et al., 2005; Ott and Daiello, 2010). However, a variety of sensory system disorders, such as VI and auditory dysfunction, may also negatively affect the driving performance of AD patients. Although the visual manifestations of AD have been extensively described, little is known about the visual deficits associated with impaired driving performance of AD patients.
The cited studies have focused on the decline of cognitive skills and the investigation of neuropsychological tests assessing primarily visuoperceptual, attentional, and executive functions. Seventeen of 20 studies have included age-matched control subjects. Interestingly, there is a paucity in publications assessing the effect of oculovisual decline on the driving ability of AD subjects. Most authors have matched the visual status of patients and controls, but no detailed information is given regarding the ophthalmological tests used. Seventeen of 20 studies have included vision testing in their eligibility criteria for AD patients and controls. Seven studies required a minimum VA of 20/40 or 20/50 sufficient for driving according to current legislations, two studies have included AD patients and controls with equal VA (Rizzo et al., 1997, 2001), and one study reported that participants underwent a vision screen. Four studies did not report on the VA of participants, but included a statement that subjects with significant visual decline were excluded or they had a valid driver’s license (Carr et al., 2000; Ott et al., 2003; Uc et al., 2004, 2005). In the study by Brown et al. (2005) normal confrontation visual fields were required for study participants and Fuermaier et al. (2019) required a minimum horizontal field of view of 120 degrees. However, in almost all studies no additional basic visual sensory function tests were reported and no specific information about the co-existence of age-related eye conditions in the study population, such as cataracts or AMD, was given. Although the above studies included participants with no VI that would impair their driving ability, further data analysis by some authors showed that patients had worse near and far VA, contrast sensitivity and structure from motion (Rizzo et al., 1997, 2001; Uc et al., 2004, 2005; Dawson et al., 2009; Aksan et al., 2015). Dawson et al. (2009) found that patients had more vision-related comorbidities, but this was not significant. Patients with significant motor impairment have been excluded from the cited studies.
In conclusion, although intact vision plays an important role in driving and AD patients may have ocular pathologies related to dementia and age, basic visual sensory function in driving studies with AD patients has received little attention.
Current literature suggests that there are several ophthalmological manifestations of AD, which may be relevant for driving performance. Oculovisual alterations in AD patients are due to primary involvement of the visual pathway and higher cortical impairment. Changes in primary vision include reduction of visual acuity, impaired color vision, loss of contrast sensitivity, visual field defects, decreased stereopsis, defective smooth pursuit, and saccadic eye movements (Table 2; Cormack et al., 2000; Pache et al., 2003; Risacher et al., 2013; Nolan et al., 2014; Kim et al., 2022). Higher order visual functions have also been reported to affect visuospatial function, eye-head coordination, motion detection, and identification of objects (Table 2). This review focuses on the disorders of primary vision, which may affect the driving potential of AD patients.
Pathological changes have been described in the crystalline lens, retina, optic nerve, and visual cortex of patients with AD (Table 2). Aβ deposits have been detected in the crystalline lens and aqueous humor, and a specific supranuclear cataract has been described in AD patients (Goldstein et al., 2003). The retina in AD may undergo similar pathological changes to the brain and recent research has focused in detecting retinal biomarkers for AD. Many authors have found Aβ deposits and pTau plaques in AD retinas (Koronyo-Hamaoui et al., 2011; Koronyo et al., 2012; Frost et al., 2014; Williams et al., 2015; La Morgia et al., 2016), although their presence has not been consistent across studies (Schön et al., 2012; Ho et al., 2014).
Recently, optical coherence tomography (OCT) has revealed a reduction in RGCs, retinal nerve fiber layer (RNFL) thickness and macular thickness in AD (Parisi et al., 2001; Paquet et al., 2007; Kesler et al., 2011; Kirbas et al., 2013; Chan et al., 2019). A recent meta-analysis of 11 OCT studies in AD showed that mean RNFL is significantly reduced in all four retinal quadrants around the macula (Coppola et al., 2015). Interestingly, RNFL changes have been demonstrated in early AD patients without VI, suggesting the potential use of RNFL as an early diagnostic marker (Lu et al., 2010; Bambo et al., 2014; Garcia-Martin et al., 2014). As AD progresses, a further decrease in RNFL thickness has been observed, and there was a significant correlation between overall macular volume and severity of cognitive impairment measured by the MMSE (Iseri et al., 2006; Tas et al., 2015). Specific to the optic nerve, imaging studies have demonstrated in vivo evidence of optic nerve head pathology in AD patients, such as larger cup-to-disk ratio and increased pallor of the optic nerve (Tsai et al., 1991; Lu et al., 2010; Bambo et al., 2015), reflecting a significant loss of RGC axons and/or possible retrograde degeneration affecting the retina (Danesh-Meyer et al., 2006). It has been shown that patients with AD have visual dysfunction, such as impairment of color vision and contrast sensitivity, that correlate with structural OCT changes, namely, RNFL thinning and macular thinning (Polo et al., 2017). Moreover, retinal vascular abnormalities, such as reduction in retinal microvasculature, narrowing of retinal veins (Cheung et al., 2014; Williams et al., 2015), reduced retinal blood flow (Feke et al., 2015), increased tortuosity, compromised branching complexity, and reduced choroidal thickness (Gharbiya et al., 2014; Bayhan et al., 2015) have been described.
Visual field defects in patients with AD are of special interest, because a minimum extent of the visual field is currently required from driving license authorities all over the world. In their preliminary study, Trick et al. (1995) showed that visual field loss in AD is most pronounced in the inferonasal and inferotemporal visual field but also involves the central region. Interestingly, the degree of loss correlated with the degree of dementia (Armstrong, 1996), and the predominant inferior field defects were attributed to pathological differences between cuneal and lingual gyri (Armstrong, 1996). Studies with frequency doubling technology (FDT) perimetry have described significantly greater false-negatives, test duration, and abnormal visual fields in AD patients compared with controls, with five-times greater (27.5%) frequency of glaucoma-like alterations in visual fields in AD (Aykan et al., 2013; Cesareo et al., 2015).
Apart from the specific oculo-visual changes associated with dementia, older individuals may also experience age-related visual disorders, such as AMD, glaucoma, and cataracts. Such conditions may further impair the driving ability of affected patients and pose a risk for public safety or lead to driving cessation and loss of personal autonomy (Wood et al., 2018). Interestingly, a number of studies have linked many age-related eye diseases to cognitive impairment and dementia (Chung et al., 2015; Gupta et al., 2019; Rong et al., 2019; Zhang et al., 2019; Belamkar et al., 2021). An increased occurrence of AMD has been found in patients with AD (Klaver et al., 1999; Nolan et al., 2014) and Ab has been also identified in retinal drusen, which are a hallmark of AMD (Ratnayaka et al., 2015). An association of glaucoma and AD is also under investigation (Ramirez et al., 2017; Zhao et al., 2021). Two longitudinal studies have shown that poorer visual acuity was often a predictor of higher dementia incidence over time (Lee et al., 2020; Tran et al., 2020). Chen et al. (2021) found a bidirectional association between VI and dementia. In a retrospective study of 10,676 individuals over 65 years, they reported that patients who present with VI at the first examination are more probable to develop dementia in the future. On the other hand, patients with dementia are at a greater risk to experience visual loss over time (Chen et al., 2021). A recent meta-analysis has also revealed a bidirectional relationship between VI and cognitive impairment, suggesting that VI is a risk factor of cognitive impairment and individuals with cognitive impairment were more likely to have VI, although more evidence is needed to confirm the latter finding (Vu et al., 2021). Another systematic meta-analysis concluded that VI is related to an increased risk of both dementia and cognitive impairment in older adults, hence screening and treating vision impairment may help to alleviate the global burden of dementia (Shang et al., 2021). Possible mechanisms for the association of low vision and impaired cognition include loss of visual sensory information with resulting neuronal atrophy, errors in perceptual processing and consequent decline in higher-order cognitive performance, restricted participation in mentally stimulating activities due to visual loss and other common risk factors for both dementia and VI, such as vascular disease (Chen et al., 2021; Shang et al., 2021; Vu et al., 2021).
To date, several studies have examined the driving ability of patients with AD, and although there is significant methodological heterogeneity, it is clear that AD negatively affects driving ability. However, there is still no consensus regarding the cognitive and driving tests that have the best predictive value for fitness-to-drive in patients. This review highlights the need to characterize in more detail the basic visual sensory status of AD patients participating in driving studies, and investigate the impact of vision abnormalities on their driving performance. Research has shown that visual parameters substantial for safe driving, such as visual acuity, visual field, contrast sensitivity, and color vision, may be impaired in AD, and this field deserves further investigation. Larger studies should aim to compare AD patients with intact vision, AD patients with ocular disease, and age-matched controls, in order to assess the relative contributions of primary vision and cognitive impairment on their driving ability.
Additionally, current evidence on the link between visual disorders and dementia suggests the need for early screening and detection of older adults with VI. The bidirectional association between VI and dementia warrants both the vision examination of cognitively impaired individuals and also the cognitive assessment of older adults with visual disorders (Chen et al., 2021; Shang et al., 2021; Vu et al., 2021). Vision screening and cognitive assessment of the older driver should aim to identify at-risk individuals and employ timely strategies for treatment of both cognitive and ocular problems. A multidisciplinary team approach by eye care professionals, neurologists, geriatricians, and primary care providers could play an important role in helping affected patients to preserve mobility and independence for as long as possible after the onset of dementia and at the same time minimize individual clinical and public health consequences.
The importance of the recent advances in ocular imaging of dementia patients lies in the early identification of in vivo retinal and optic nerve changes, which may underlie driving-specific VIs and may have a future role as predictors of disease severity and fitness-to-drive. The impact of these retinal alterations on visual acuity and visual function of AD patients, especially in terms of their driving ability, still remains to be elucidated. However, these research findings suggest that retinal imaging is a promising tool for assessment of at-risk individuals, and may prove useful in the future for assisting physicians to decisions regarding fitness-to-drive.
EP, DT, VS, and KL have been involved in drafting the manuscript or revising it critically for important intellectual content. ED and ET have given final approval of the version to be published. All authors made substantial contributions to conception and design, acquisition of data, and analysis and interpretation of data.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Aksan, N., Anderson, S. W., Dawson, J., Uc, E., and Rizzo, M. (2015). Cognitive functioning differentially predicts different dimensions of older drivers’ on-road safety. Accid. Anal. Prev. 75, 236–244. doi: 10.1016/j.aap.2014.12.007
Armstrong, R. A. (1996). Visual field defects in Alzheimer’s disease patients may reflect differential pathology in the primary visual cortex. Optom Vis. Sci. 73, 677–682. doi: 10.1097/00006324-199611000-00001
Aykan, U., Akdemir, M. O., Yildirim, O., and Varlibas, F. (2013). Screening for patients with mild Alzheimer Disease using frequency doubling technology perimetry. Neuroophthalmology 37, 239–246. doi: 10.3109/01658107.2013.830627
Bambo, M. P., Garcia-Martin, E., Gutierrez-Ruiz, F., Pinilla, J., Perez-Olivan, S., Larrosa, J. M., et al. (2015). Analysis of optic disk color changes in Alzheimer’s disease: a potential new biomarker. Clin. Neurol. Neurosurg. 132, 68–73. doi: 10.1016/j.clineuro.2015.02.016
Bambo, M. P., Garcia-Martin, E., Pinilla, J., Herrero, R., Satue, M., Otin, S., et al. (2014). Detection of retinal nerve fiber layer degeneration in patients with Alzheimer’s disease using optical coherence tomography: searching new biomarkers. Acta Ophthalmol. 92, e581–e582. doi: 10.1111/aos.12374
Barco, P. P., Baum, C. M., Ott, B. R., Ice, S., Johnson, A., Wallendorf, M., et al. (2015). Driving errors in persons with dementia. J. Am. Geriatr. Soc. 63, 1373–1380. doi: 10.1111/jgs.13508
Bayhan, H. A., Aslan Bayhan, S., Celikbilek, A., Tanık, N., and Gürdal, C. (2015). Evaluation of the chorioretinal thickness changes in Alzheimer’s disease using spectral-domain optical coherence tomography. Clin. Exp. Ophthalmol. 43, 145–151. doi: 10.1111/ceo.12386
Belamkar, A. V., Mansukhani, S. A., Savica, R., Spiegel, M. R., Hodge, D. O., and Sit, A. J. (2021). Incidence of dementia in patients with open-angle glaucoma: a population-based study. J. Glaucoma. 30, 227–234. doi: 10.1097/IJG.0000000000001774
Berisha, F., Feke, G. T., Trempe, C. L., McMeel, J. W., and Schepens, C. L. (2007). Retinal abnormalities in early Alzheimer’s disease. Invest. Ophthalmol. Vis. Sci. 48, 2285–2289. doi: 10.1167/iovs.06-1029
Bowers, A. R. (2016). Driving with homonymous visual field loss: a review of the literature. Clin. Exp. Optom. 99, 402–418. doi: 10.1111/cxo.12425
Brown, L. B., Ott, B. R., Papandonatos, G. D., Sui, Y., Ready, R. E., and Morris, J. C. (2005). Prediction of on-road driving performance in patients with early Alzheimer’s disease. J. Am. Geriatr. Soc. 53, 94–98. doi: 10.1111/j.1532-5415.2005.53017.x
Carr, D. B., Duchek, J., and Morris, J. C. (2000). Characteristics of motor vehicle crashes of drivers with dementia of the Alzheimer type. J. Am. Geriatr. Soc. 48, 18–22. doi: 10.1111/j.1532-5415.2000.tb03023.x
Carr, D. B., and Ott, B. R. (2010). The older adult driver with cognitive impairment: “It’s a very frustrating life”. JAMA 303, 1632–1641. doi: 10.1001/jama.2010.481
Cesareo, M., Martucci, A., Ciuffoletti, E., Mancino, R., Cerulli, A., Sorge, R. P., et al. (2015). Association between Alzheimer’s disease and glaucoma: a study based on Heidelberg retinal tomography and frequency doubling technology perimetry. Front. Neurosci. 9:479. doi: 10.3389/fnins.2015.00479
Chan, V. T. T., Sun, Z., Tang, S., Chen, L. J., Wong, A., Tham, C. C., et al. (2019). Spectral-domain OCT measurements in Alzheimer’s disease: a systematic review and meta-analysis. Ophthalmology 126, 497–510. doi: 10.1016/j.ophtha.2018.08.009
Chee, J. N., Rapoport, M. J., Molnar, F., Herrmann, N., O’Neill, D., Marottoli, R., et al. (2017). Update on the risk of motor vehicle collision or driving impairment with dementia: A collaborative international systematic review and meta-analysis. Am. J. Geriatr. Psychiatry 25, 1376–1390. doi: 10.1016/j.jagp.2017.05.007
Chen, S. P., Azad, A. D., and Pershing, S. (2021). Bidirectional association between visual impairment and dementia among older adults in the United States over time. Ophthalmology 128, 1276–1283. doi: 10.1016/j.ophtha.2021.02.021
Cheung, C. Y., Ong, Y. T., Ikram, M. K., Ong, S. Y., Li, X., Hilal, S., et al. (2014). Microvascular network alterations in the retina of patients with Alzheimer’s disease. Alzheimers Dement. 10, 135–142. doi: 10.1016/j.jalz.2013.06.009
Chung, S. D., Ho, J. D., Chen, C. H., Lin, H. C., Tsai, M. C., and Sheu, J. J. (2015). Dementia is associated with open-angle glaucoma: a population-based study. Eye 29, 1340–1346. doi: 10.1038/eye.2015.120
Coppola, G., Di Renzo, A., Ziccardi, L., Martelli, F., Fadda, A., Manni, G., et al. (2015). Optical coherence tomography in Alzheimer’s disease: a meta-analysis. PLoS One 10:e0134750. doi: 10.1371/journal.pone.0134750
Cormack, F. K., Tovee, M., and Ballard, C. (2000). Contrast sensitivity and visual acuity in patients with Alzheimer’s disease. Int. J. Geriatr. Psychiatry 15, 614–620. doi: 10.1002/1099-1166(200007)15:7<614::AID-GPS153>3.0.CO;2-0
Curcio, C. A., and Drucker, D. N. (1993). Retinal ganglion cells in Alzheimer’s disease and aging. Ann. Neurol. 33, 248–257. doi: 10.1002/ana.410330305
Danesh-Meyer, H. V., Birch, H., Ku, J. Y., Carroll, S., and Gamble, G. (2006). Reduction of optic nerve fibers in patients with Alzheimer disease identified by laser imaging. Neurology 67, 1852–1854. doi: 10.1212/01.wnl.0000244490.07925.8b
Davis, J., Hamann, C., Butcher, B., and Peek-Asa, C. (2020). The medical referral process and motor-vehicle crash risk for drivers with dementia. Geriatrics 5:91. doi: 10.3390/geriatrics5040091
Davis, J. D., Papandonatos, G. D., Miller, L. A., Hewitt, S. D., Festa, E. K., Heindel, W. C., et al. (2012). Road test and naturalistic driving performance in healthy and cognitively impaired older adults: does environment matter? J. Am. Geriatr. Soc. 60, 2056–2062. doi: 10.1111/j.1532-5415.2012.04206.x
Davis, R., and Owens, M. (2021). Self-Regulation of driving behaviors in persons with early-stage Alzheimer’s disease. J. Gerontol. Nurs. 47, 21–27. doi: 10.3928/00989134-20201209-01
Dawson, J. D., Anderson, S. W., Uc, E. Y., Dastrup, E., and Rizzo, M. (2009). Predictors of driving safety in early Alzheimer disease. Neurology 72, 521–527. doi: 10.1212/01.wnl.0000341931.35870.49
Dobbs, A. R. (1997). Evaluating the driving competence of dementia patients. Alzheimer Dis. Assoc. Disord. 11, (Suppl. 1), 8–12. doi: 10.1097/00002093-199706001-00003
Dubois, B., Villain, N., Frisoni, G. B., Rabinovici, G. D., Sabbagh, M., Cappa, S., et al. (2021). Clinical diagnosis of Alzheimer’s disease: Recommendations of the international working group. Lancet Neurol. 20, 484–496. doi: 10.1016/S1474-4422(21)00066-1
Duchek, J. M., Carr, D. B., Hunt, L., Roe, C. M., Xiong, C., Shah, K., et al. (2003). Longitudinal driving performance in early-stage dementia of the Alzheimer type. J. Am. Geriatr. Soc. 51, 1342–1347. doi: 10.1046/j.1532-5415.2003.51481.x
Eby, D. W., Silverstein, N. M., Molnar, L. J., LeBlanc, D., and Adler, G. (2012). Driving behaviors in early stage dementia: a study using in-vehicle technology. Accid. Anal. Prev. 49, 330–337. doi: 10.1016/j.aap.2011.11.021
Estevez-Gonzalez, A., Kulisevsky, J., Boltes, A., Otermin, P., and Garcia-Sanchez, C. (2003). Rey verbal learning test is a useful tool for differential diagnosis in the preclinical phase of Alzheimer’s disease: comparison with mild cognitive impairment and normal aging. Int. J. Geriatr. Psychiatry 18, 1021–1028. doi: 10.1002/gps.1010
Etienne, V., Marin-Lamellet, C., and Laurent, B. (2013). Mental flexibility impairment in drivers with early Alzheimer’s disease: a simulator-based study. IATSS Res. 37, 16–20. doi: 10.1016/j.iatssr.2013.06.005
Feke, G. T., Hyman, B. T., Stern, R. A., and Pasquale, L. R. (2015). Retinal blood flow in mild cognitive impairment and Alzheimer’s disease. Alzheimers Dement. 1, 144–151. doi: 10.1016/j.dadm.2015.01.004
Feng, Y. R., Meuleners, L., Stevenson, M., Heyworth, J., Murray, K., and Maher, S. (2020). Driver self-regulation practices in older drivers with and without mild cognitive impairment. Clin. Interv. Aging 15, 217–224. doi: 10.2147/CIA.S236998
Fitten, L. J., Perryman, K. M., Wilkinson, C. J., Little, R. J., Burns, M. M., Pachana, N., et al. (1995). Alzheimer and vascular dementias and driving. A prospective road and laboratory study. JAMA 273, 1360–1365. doi: 10.1001/jama.1995.03520410054026
Foley, D. J., Masaki, K. H., Ross, G. W., and White, L. R. (2000). Driving cessation in older men with incident dementia. J. Am. Geriatr. Soc. 48, 928–930. doi: 10.1111/j.1532-5415.2000.tb06889.x
Friedland, R. P., Koss, E., Kumar, A., Gaine, S., Metzler, D., Haxby, J. V., et al. (1988). Motor vehicle crashes in dementia of the Alzheimer type. Ann. Neurol. 24, 782–786. doi: 10.1002/ana.410240613
Friedman, D. S., Munoz, B., Massy, R. W., Bandeen-Roche, K., and West, S. K. (2002). Grating visual acuity using the preferential-looking method in elderly nursing home residents. Invest. Ophthalmol. Vis. Sci. 43, 2572–2578.
Frittelli, C., Borghetti, D., Iudice, G., Bonanni, E., Maestri, M., Tognoni, G., et al. (2009). Effects of Alzheimer’s disease and mild cognitive impairment on driving ability: a controlled clinical study by simulated driving test. Int. J. Geriatr. Psychiatry 24, 232–238. doi: 10.1002/gps.2095
Frost, S., Kanagasingam, Y., Macaulay, S., Koronyo-Hamaoui, M., Koronyo, Y., Biggs, D., et al. (2014). Retinal amyloid fluorescence imaging predicts cerebral amyloid burden and Alzheimer’s disease. Alzheimers Dement. 10, 234–235. doi: 10.1016/j.jalz.2014.04.341
Fuermaier, A. B. M., Piersma, D., de Waard, D., Davidse, R. J., de Groot, J., Doumen, M. J. A., et al. (2019). Driving difficulties among patients with Alzheimer’s disease and other neurodegenerative disorders. J. Alzheimers Dis. 69, 1019–1030. doi: 10.3233/JAD-181095
Garcia-Martin, E. S., Rojas, B., Ramirez, A. I., de Hoz, R., Salazar, J. J., Yubero, R., et al. (2014). Macular thickness as a potential biomarker of mild Alzheimer’s disease. Ophthalmology 121, 1149–1151. doi: 10.1016/j.ophtha.2013.12.023
Gharbiya, M., Trebbastoni, A., Parisi, F., Manganiello, S., Cruciani, F., D’Antonio, F., et al. (2014). Choroidal thinning as a new finding in Alzheimer’s disease: evidence from enhanced depth imaging spectral domain optical coherence tomography. J. Alzheimers Dis. 40, 907–917. doi: 10.3233/JAD-132039
Gilmore, G. C., Wenk, H. E., Naylor, L. A., and Koss, E. (1994). Motion perception and Alzheimer’s disease. J. Gerontol. 49, 52–57. doi: 10.1093/geronj/49.2.p52
Goldstein, L. E., Muffat, J. A., Cherny, R. A., Moir, R. D., Ericsson, M. H., Huang, X., et al. (2003). Cytosolic beta-amyloid deposition and supranuclear cataracts in lenses from people with Alzheimer’s disease. Lancet 361, 1258–1265. doi: 10.1016/S0140-6736(03)12981-9
Graff-Radford, J., Yong, K. X. X., Apostolova, L. G., Bouwman, F. H., Carrillo, M., Dickerson, B. C., et al. (2021). New insights into atypical Alzheimer’s disease in the era of biomarkers. Lancet Neurol. 20, 222–234. doi: 10.1016/S1474-4422(20)30440-3
Guerreiro, R., and Bras, J. (2015). The age factor in Alzheimer’s disease. Genome Med. 7:106. doi: 10.1186/s13073-015-0232-5
Guo, L., Duggan, J., and Cordeiro, M. F. (2010). Alzheimer’s disease and retinal neurodegeneration. Curr. Alzheimer Res. 7, 3–14. doi: 10.2174/156720510790274491
Gupta, P., Gan, A. T. L., Man, R. E. K., Fenwick, E. K., Sabanayagam, C., Mitchell, P., et al. (2019). Association between diabetic retinopathy and incident cognitive impairment. Br. J. Ophthalmol. 103, 1605–1609. doi: 10.1136/bjophthalmol-2018-312807
Hebert, L. E., Weuve, J., Scherr, P. A., and Evans, D. A. (2013). Alzheimer disease in the United States (2010-2050) estimated using the 2010 census. Neurology 80, 1778–1783. doi: 10.1212/WNL.0b013e31828726f5
Hird, M. A., Egeto, P., Fischer, C. E., Naglie, G., and Schweizer, T. A. (2016). A systematic review and meta-analysis of on-road simulator and cognitive driving assessment in Alzheimer’s disease and mild cognitive impairment. J. Alzheimers Dis. 53, 713–729. doi: 10.3233/JAD-160276
Ho, C. Y., Troncoso, J. C., Knox, D., Stark, W., and Eberhart, C. G. (2014). Beta-amyloid, phospho-tau and alpha-synuclein deposits similar to those in the brain are not identified in the eyes of Alzheimer’s and Parkinson’s disease patients. Brain Pathol. 24, 25–32. doi: 10.1111/bpa.12070
Hof, P. R., Bouras, C., Constantinidis, J., and Morrison, J. H. (1990). Selective disconnection of specific visual association pathways in cases of Alzheimer’s disease presenting with Balint’s syndrome. J. Neuropathol. Exp. Neurol. 49, 168–184. doi: 10.1097/00005072-199003000-00008
Iseri, P. K., Altinaş, O., Tokay, T., and Yüksel, N. (2006). Relationship between cognitive impairment and retinal morphological and visual functional abnormalities in Alzheimer disease. J. Neuroophthalmol. 26, 18–24. doi: 10.1097/01.wno.0000204645.56873.26
Iverson, D. J., Gronseth, G. S., Reger, M. A., Classen, S., Dubinsky, R. M., Rizzo, M., et al. (2010). Practice parameter update: evaluation and management of driving risk in dementia: report of the quality standards subcommittee of the american academy of neurology. Neurology 74, 1316–1324. doi: 10.1212/WNL.0b013e3181da3b0f
Jindahra, P., Hedges, T. R., Mendoza-Santiesteban, C. E., and Plant, G. T. (2010). Optical coherence tomography of the retina: applications in neurology. Curr. Opin. Neurol. 23, 16–23. doi: 10.1097/WCO.0b013e328334e99b
Kasneci, E., Sippel, K., Aehling, K., Heister, M., Rosenstiel, W., Schiefer, U., et al. (2014). Driving with binocular visual field loss? A study on a supervised on-road parcours with simultaneous eye and head tracking. PLoS One 9:e87470. doi: 10.1371/journal.pone.0087470
Katz, B., and Rimmer, S. (1989). Ophthalmologic manifestations of Alzheimer’s disease. Surv. Ophthalmol. 34, 31–43. doi: 10.1016/0039-6257(89)90127-6
Katz, B., Rimmer, S., Iragui, V., and Katzman, R. (1989). Abnormal pattern electroretinogram in Alzheimer’s disease: evidence for retinal ganglion cell degeneration? Ann. Neurol. 26, 221–225. doi: 10.1002/ana.410260207
Kesler, A., Vakhapova, V., Korczyn, A. D., Naftaliev, E., and Neudorfer, M. (2011). Retinal thickness in patients with mild cognitive impairment and Alzheimer’s disease. Clin. Neurol. Neurosurg. 113, 523–526. doi: 10.1016/j.clineuro.2011.02.014
Kim, H. J., Ryou, J. H., Choi, K. T., Kim, S. M., Kim, J. T., and Han, D. H. (2022). Deficits in color detection in patients with Alzheimer disease. PLoS One 17:e0262226. doi: 10.1371/journal.pone.0262226
Kirbas, S., Turkyilmaz, K., Anlar, O., Tufekci, A., and Durmus, M. (2013). Retinal nerve fiber layer thickness in patients with Alzheimer disease. J. Neuroophthalmol. 33, 58–61. doi: 10.1097/WNO.0b013e318267fd5f
Klaver, C. C., Ott, A., Hofman, A., Assink, J. J., Breteler, M. M., and de Jong, P. T. (1999). Is age-related maculopathy associated with Alzheimer’s disease? The Rotterdam Study. Am. J. Epidemiol. 150, 963–968. doi: 10.1093/oxfordjournals.aje.a010105
Koronyo, Y., Biggs, D., Barron, E., Boyer, D. S., Pearlman, J. A., Au, W. J., et al. (2017). Retinal amyloid pathology and proof-of-concept imaging trial in Alzheimer’s disease. JCI Insight 2:e93621. doi: 10.1172/jci.insight.93621
Koronyo, Y., Salumbides, B. C., Black, K. L., and Koronyo-Hamaoui, M. (2012). Alzheimer’s disease in the retina: imaging retinal aβ plaques for early diagnosis and therapy assessment. Neurodegener. Dis. 10, 285–293. doi: 10.1159/000335154
Koronyo-Hamaoui, M., Koronyo, Y., Ljubimov, A. V., Miller, C. A., Ko, M. K., Black, K. L., et al. (2011). Identification of amyloid plaques in retinas from Alzheimer’s patients and noninvasive in vivo optical imaging of retinal plaques in a mouse model. Neuroimage 54, (Suppl. 1), S204–S217. doi: 10.1016/j.neuroimage.2010.06.020
Kusne, Y., Wolf, A. B., Townley, K., Conway, M., and Peyman, G. A. (2017). Visual system manifestations of Alzheimer’s disease. Acta Ophthalmol. 95, e668–e676. doi: 10.1111/aos.13319
La Morgia, C., Ross-Cisneros, F. N., Koronyo, Y., Hannibal, J., Gallassi, R., Cantalupo, G., et al. (2016). Melanopsin retinal ganglion cell loss in Alzheimer disease. Ann. Neurol. 79, 90–109. doi: 10.1002/ana.24548
Lee, A. T. C., Richards, M., Chan, W. C., Chiu, H. F. K., Lee, R. S. Y., and Lam, L. C. W. (2020). Higher dementia incidence in older adults with poor visual acuity. J. Gerontol. A Biol. Sci. Med. Sci. 75, 2162–2168. doi: 10.1093/gerona/glaa036
Lincoln, N. B., Radford, K. A., Lee, E., and Reay, A. C. (2006). The assessment of fitness to drive in people with dementia. Int. J. Geriatr. Psychiatry 21, 1044–1051. doi: 10.1002/gps.1604
Liu, B., Rasool, S., Yang, Z., Glabe, C. G., Schreiber, S. S., Ge, J., et al. (2009). Amyloid-peptide vaccinations reduce {beta}-amyloid plaques but exacerbate vascular deposition and inflammation in the retina of Alzheimer’s transgenic mice. Am. J. Pathol. 175, 2099–2110. doi: 10.2353/ajpath.2009.090159
Lu, Y., Li, Z., Zhang, X., Ming, B., Jia, J., Wang, R., et al. (2010). Retinal nerve fiber layer structure abnormalities in early Alzheimer’s disease: evidence in optical coherence tomography. Neurosci. Lett. 480, 69–72. doi: 10.1016/j.neulet.2010.06.006
Mauri, M., Sinforiani, E., Cuzzoni, M. G., Bono, G., and Zucchella, C. (2014). Driving habits in patients with dementia: a report from Alzheimer’s disease assessment units in northern Italy. Funct. Neurol. 29, 107–112.
Mendez, M. F., Mendez, M. A., Martin, R., Smyth, K. A., and Whitehouse, P. J. (1990). Complex visual disturbances in Alzheimer’s disease. Neurology 40(3 Pt 1), 439–443. doi: 10.1212/WNL.40.3_Part_1.439
Nichols, E., Steinmetz, J. D., Vollset, S. E., Fukutaki, K., Chalek, J., Abd-Allah, F., et al. (2022). Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019. Lancet Public Health 7, 105–125. doi: 10.1016/S2468-2667(21)00249-8
Nolan, J. M., Loskutova, E., Howard, A. N., Moran, R., Mulcahy, R., Stack, J., et al. (2014). Macular pigment, visual function, and macular disease among subjects with Alzheimer’s disease: an exploratory study. J. Alzheimers Dis. 42, 1191–1202. doi: 10.3233/JAD-140507
Ott, B. R., and Daiello, L. A. (2010). How does dementia affect driving in older patients? Aging Health 6, 77–85. doi: 10.2217/ahe.09.83
Ott, B. R., Festa, E. K., Amick, M. M., Grace, J., Davis, J. D., and Heindel, W. C. (2008). Computerized maze navigation and on-road performance by drivers with dementia. J. Geriatr. Psychiatry Neurol. 21, 18–25. doi: 10.1177/0891988707311031
Ott, B. R., Heindel, W. C., Whelihan, W. M., Caron, M. D., Piatt, A. L., and DiCarlo, M. A. (2003). Maze test performance and reported driving ability in early dementia. J. Geriatr. Psychiatry Neurol. 16, 151–155. doi: 10.1177/0891988703255688
Owsley, C., and McGwin, G. Jr. (1999). Vision impairment and driving. Surv. Ophthalmol. 43, 535–550. doi: 10.1016/S0039-6257(99)00035-1
Pache, M., Smeets, C. H., Gasio, P. F., Savaskan, E., Flammer, J., Wirz-Justice, A., et al. (2003). Colour vision deficiencies in Alzheimer’s disease. Age Ageing 32, 422–426. doi: 10.1093/ageing/32.4.422
Papageorgiou, E., Hardiess, G., Ackermann, H., Wiethoelter, H., Dietz, K., Mallot, H. A., et al. (2012). Collision avoidance in persons with homonymous visual field defects under virtual reality conditions. Vis. Res. 52, 20–30. doi: 10.1016/j.visres.2011.10.019
Paquet, C., Boissonnot, M., Roger, F., Dighiero, P., Gil, R., and Hugon, J. (2007). Abnormal retinal thickness in patients with mild cognitive impairment and Alzheimer’s disease. Neurosci. Lett. 420, 97–99. doi: 10.1016/j.neulet.2007.02.090
Parisi, V., Restuccia, R., Fattapposta, F., Mina, C., Bucci, M. G., and Pierelli, F. (2001). Morphological and functional retinal impairment in Alzheimer’s disease patients. Clin. Neurophysiol. 112, 1860–1867. doi: 10.1016/S1388-2457(01)00620-4
Perrin, R. J., Fagan, A. M., and Holtzman, D. M. (2009). Multimodal techniques for diagnosis and prognosis of Alzheimer’s disease. Nature 461, 916–922. doi: 10.1038/nature08538
Polo, V., Rodrigo, M. J., Garcia-Martin, E., Otin, S., Larrosa, J. M., Fuertes, M. I., et al. (2017). Visual dysfunction and its correlation with retinal changes in patients with Alzheimer’s disease. Eye 31, 1034–1041. doi: 10.1038/eye.2017.23
Ramirez, A. I., de Hoz, R., Salobrar-Garcia, E., Salazar, J. J., Rojas, B., Ajoy, D., et al. (2017). The role of microglia in retinal neurodegeneration: Alzheimer’s disease, Parkinson, and Glaucoma. Front. Aging Neurosci. 9:214. doi: 10.3389/fnagi.2017.00214
Ratnayaka, J. A., Serpell, L. C., and Lotery, A. J. (2015). Dementia of the eye: the role of amyloid beta in retinal degeneration. Eye 29, 1013–1026. doi: 10.1038/eye.2015.100
Reger, M. A., Welsh, R. K., Watson, G. S., Cholerton, B., Baker, L. D., and Craft, S. (2004). The relationship between neuropsychological functioning and driving ability in dementia: a meta-analysis. Neuropsychology 18, 85–93. doi: 10.1037/0894-4105.18.1.85
Risacher, S. L., Wudunn, D., Pepin, S. M., MaGee, T. R., McDonald, B. C., Flashman, L. A., et al. (2013). Visual contrast sensitivity in Alzheimer’s disease, mild cognitive impairment, and older adults with cognitive complaints. Neurobiol. Aging 34, 1133–1144. doi: 10.1016/j.neurobiolaging.2012.08.007
Rizzo, M. (1993). ‘Bálint’s syndrome’ and associated visuospatial disorders. Baillieres Clin. Neurol. 2, 415–437.
Rizzo, M., and Hurtig, R. (1987). Looking but not seeing: attention, perception, and eye movements in simultanagnosia. Neurology 37, 1642–1648. doi: 10.1212/WNL.37.10.1642
Rizzo, M., McGehee, D. V., Dawson, J. D., and Anderson, S. N. (2001). Simulated car crashes at intersections in drivers with Alzheimer disease. Alzheimer Dis. Assoc. Disord. 15, 10–20. doi: 10.1097/00002093-200101000-00002
Rizzo, M., Reinach, S., McGehee, D., and Dawson, J. (1997). Simulated car crashes and crash predictors in drivers with Alzheimer disease. Arch. Neurol. 54, 545–551. doi: 10.1001/archneur.1997.00550170027011
Rong, S. S., Lee, B. Y., Kuk, A. K., Yu, X. T., Li, S. S., Li, J., et al. (2019). Comorbidity of dementia and age-related macular degeneration calls for clinical awareness: a meta-analysis. Br. J. Ophthalmol. 103, 1777–1783. doi: 10.1136/bjophthalmol-2018-313277
Sadun, A. A., and Bassi, C. J. (1990). Optic nerve damage in Alzheimer’s disease. Ophthalmology 97, 9–17. doi: 10.1016/S0161-6420(90)32621-0
Schön, C., Hoffmann, N. A., Ochs, S. M., Burgold, S., Filser, S., Steinbach, S., et al. (2012). Long-term in vivo imaging of fibrillar tau in the retina of P301S transgenic mice. PLoS One 7:e53547. doi: 10.1371/journal.pone.0053547
Seiler, S., Schmidt, H., Lechner, A., Benke, T., Sanin, G., Ransmayr, G., et al. (2012). Driving cessation and dementia: Results of the prospective registry on dementia in Austria (PRODEM). PLoS One 7:52710. doi: 10.1371/journal.pone.0052710
Sekuler, R., and Ball, K. (1986). Visual localization: age and practice. J. Opt. Soc. Am. 3:864. doi: 10.1364/JOSAA.3.000864
Shang, X., Zhu, Z., Wang, W., Ha, J., and He, M. (2021). The association between vision impairment and incidence of dementia and cognitive impairment: a systematic review and meta-analysis. Ophthalmology 128, 1135–1149. doi: 10.1016/j.ophtha.2020.12.029
Silverstein, N. M. (2008). “Alzheimer’s disease and fitness to drive,” in Proceedings of the AAA foundation for traffic safety conference, Washington, DC.
Stothart, G., Kazanina, N., Näätänen, R., Haworth, J., and Tales, A. (2015). Early visual evoked potentials and mismatch negativity in Alzheimer’s disease and mild cognitive impairment. J. Alzheimers Dis. 44, 397–408. doi: 10.3233/JAD-140930
Swan, G., Shahin, M., Albert, J., Herrmann, J., and Bowers, A. R. (2019). The effects of simulated acuity and contrast sensitivity impairments on detection of pedestrian hazards in a driving simulator. Transp. Res. F Traffic Psychol. Behav. 64, 213–226. doi: 10.1016/j.trf.2019.05.003
Tales, A., Troscianko, T., Lush, D., Haworth, J., Wilcock, G. K., and Butler, S. R. (2001). The pupillary light reflex in aging and Alzheimer’s disease. Aging 13, 473–478.
Tas, A., Yolcu, U., Ilhan, A., and Gundogan, F. C. (2015). Detection of retinal nerve fibre layer degeneration in patients with Alzheimer’s disease using optical coherence tomography: searching new biomarkers. Acta Ophthalmol. 93:e507. doi: 10.1111/aos.12614
Thiyagesh, S. N., Farrow, T. F., Parks, R. W., Accosta-Mesa, H., Young, C., Wilkinson, I. D., et al. (2009). The neural basis of visuospatial perception in Alzheimer’s disease and healthy elderly comparison subjects: An fMRI study. Psychiatry Res. 172, 109–116. doi: 10.1016/j.pscychresns.2008.11.002
Tran, E. M., Stefanick, M. L., Henderson, V. W., Rapp, S. R., Chen, J. C., Armstrong, N. M., et al. (2020). Association of visual impairment with risk of incident dementia in a women’s health initiative population. JAMA Ophthalmol. 138, 624–633. doi: 10.1001/jamaophthalmol.2020.0959
Trick, G. L., Barris, M. C., and Bickler-Bluth, M. (1989). Abnormal pattern electroretinograms in patients with senile dementia of the Alzheimer type. Ann. Neurol. 26, 226–231. doi: 10.1002/ana.410260208
Trick, G. L., Trick, L. R., Morris, P., and Wolf, M. (1995). Visual field loss in senile dementia of the Alzheimer’s type. Neurology 45, 68–74. doi: 10.1212/WNL.45.1.68
Tsai, C. S., Ritch, R., Schwartz, B., Lee, S. S., Miller, N. R., Chi, T., et al. (1991). Optic nerve head and nerve fiber layer in Alzheimer’s disease. Arch. Ophthalmol. 109, 199–204. doi: 10.1001/archopht.1991.01080020045040
Tuokko, H., Tallman, K., Beattie, B. L., Cooper, P., and Weir, J. (1995). An examination of driving records in a dementia clinic. J. Gerontol. B Psychol. Sci. Soc. Sci. 50, S173–S181. doi: 10.1093/geronb/50B.3.S173
Uc, E. Y., Rizzo, M., Anderson, S. W., Shi, Q., and Dawson, J. D. (2004). Driver route-following and safety errors in early Alzheimer disease. Neurology 63, 832–837. doi: 10.1212/01.WNL.0000139301.01177.35
Uc, E. Y., Rizzo, M., Anderson, S. W., Shi, Q., and Dawson, J. D. (2005). Driver landmark and traffic sign identification in early Alzheimer’s disease. J. Neurol. Neurosurg. Psychiatry 76, 764–768. doi: 10.1136/jnnp.2004.049338
Vella, K., and Lincoln, N. B. (2014). Comparison of assessments of fitness to drive for people with dementia. Neuropsychol. Rehabil. 24, 770–783. doi: 10.1080/09602011.2014.903197
Vu, T. A., Fenwick, E. K., Gan, A. T. L., Man, R. E. K., Tan, B. K. J., Gupta, P., et al. (2021). The bidirectional relationship between vision and cognition: a systematic review and meta-analysis. Ophthalmology 128, 981–992. doi: 10.1016/j.ophtha.2020.12.010
Williams, M. A., McGowan, A. J., Cardwell, C. R., Cheung, C. Y., Craig, D., Passmore, P., et al. (2015). Retinal microvascular network attenuation in Alzheimer’s disease. Alzheimers Dement. 1, 229–235. doi: 10.1016/j.dadm.2015.04.001
Wood, J. M. (2019). 2015 Glenn A. Fry award lecture. Optometry Vis. Sci. 96, 626–636. doi: 10.1097/OPX.0000000000001421
Wood, J. M., Black, A. A., Dingle, K., Rutter, C., DiStefano, M., Koppel, S., et al. (2022). Impact of vision disorders and vision impairment on motor vehicle crash risk and on-road driving performance: a systematic review. Acta Ophthalmol. 100, 339–367. doi: 10.1111/aos.14908
Wood, J. M., Black, A. A., Mallon, K., Kwan, A. S., and Owsley, C. (2018). Effects of age-related macular degeneration on driving performance. Invest. Ophthalmol. Vis. Sci. 59, 273–279. doi: 10.1167/iovs.17-22751
Wood, J. M., and Carberry, T. P. (2004). Older drivers and cataracts: measures of driving performance before and after cataract surgery. Transport. Res. Rec. 1865, 7–13. doi: 10.3141/1865-02
World Health Organization [WHO] (2021). International statistical classification of diseases and related health problems 11th revision. Geneva: World Health Organization [WHO].
Yang, Q., Wang, T., Su, N., Xiao, S., and Kapoula, Z. (2013). Specific saccade deficits in patients with Alzheimer’s disease at mild to moderate stage and in patients with amnestic mild cognitive impairment. Age (Dordr) 35, 1287–1298. doi: 10.1007/s11357-012-9420-z
Zhang, H. J., Mi, X. S., and So, K. F. (2019). Normal tension glaucoma: from the brain to the eye or the inverse? Neural Regen. Res. 14, 1845–1850. doi: 10.4103/1673-5374.259600
Zhao, W., Lv, X., Wu, G., Zhou, X., Tian, H., Qu, X., et al. (2021). Glaucoma is not associated with Alzheimer’s disease or dementia: A meta-analysis of cohort studies. Front. Med. (Lausanne) 8:688551. doi: 10.3389/fmed.2021.688551
Keywords: driving, dementia, Alzheimer’s disease (AD), cognitive impairment (CI), visual impairment, retinal imaging
Citation: Papageorgiou E, Tsirelis D, Lazari K, Siokas V, Dardiotis E and Tsironi EE (2022) Visual disorders and driving ability in persons with dementia: A mini review. Front. Hum. Neurosci. 16:932820. doi: 10.3389/fnhum.2022.932820
Received: 30 April 2022; Accepted: 11 November 2022;
Published: 29 November 2022.
Edited by:
Sieu Kieu Khuu, University of New South Wales, AustraliaReviewed by:
Sharon Oberstein, University of New South Wales, AustraliaCopyright © 2022 Papageorgiou, Tsirelis, Lazari, Siokas, Dardiotis and Tsironi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Evangelia E. Tsironi, ZV90c2lyb25pQGhvdG1haWwuY29t
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.