
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol. , 24 February 2025
Sec. Headache and Neurogenic Pain
Volume 16 - 2025 | https://doi.org/10.3389/fneur.2025.1558014
This article is part of the Research Topic Management of migraine in patients with coexistent conditions or comorbidities: from classic to novel therapies View all 3 articles
 Michail Vikelis1
Michail Vikelis1 Georgia Kourlaba2*
Georgia Kourlaba2* Lia Barba3
Lia Barba3 Konstantinos Bilias3
Konstantinos Bilias3 Elena Barbalia4
Elena Barbalia4 Argyro Solakidi5
Argyro Solakidi5 Dimitrios Trafalis5
Dimitrios Trafalis5 Katerina Lioliou2
Katerina Lioliou2 Sofia Zyga2
Sofia Zyga2 Theodoros Karapanayiotides6
Theodoros Karapanayiotides6 Dimos-Dimitrios Mitsikostas7
Dimos-Dimitrios Mitsikostas7Introduction: Migraine is a chronic, debilitating neurological disease affecting more than 1 billion patients, worldwide. Even though migraines are not life-threatening, they have profound effects on individuals, families, and society.
Objective: The aim of this study was to describe patients’ perspectives on socioeconomic and humanistic burden of migraine, as well as the unmet medical needs in the clinical management of migraine, in Greece.
Methods: A mixed study design of a Delphi panel and a focus group was conducted, in which 16 and 9 episodic migraine patients from the two Greek migraine patient associations participated, respectively. A structured questionnaire of 45 statements regarding burden of disease diagnosis, treatment and unmet needs was used to collect data at Delphi consensus panel. An open and balanced discussion with all participants took place, under the co-ordination of one moderator during the focus group. At each round of the Delphi panel, the percentage of participants who responded “Agree/Strongly Agree,” “Disagree/Strongly disagree” and “Neither Agree nor Disagree” was calculated. The consensus threshold was set at 70% of responses. A thematic analysis was performed for the focus group.
Results: Consensus was achieved on 34 out of 45 statements. Thematic analysis revealed that patients face severe problems at work due to a lack of understanding and awareness of migraine burden from colleagues and employees, they are forced to modify their daily activities to avoid migraine attacks, and they experience prolonged diagnostic and treatment journey since they visit different medical specialties until they find the one who will be able to effectively help them manage their migraine. Additionally, they expressed concerns regarding the management of their disease due to patient-physician communication gap, dissatisfaction with traditional oral preventive therapies and lack of therapeutic options for older ages and in case of existence of specific comorbidities.
Conclusion: Participants agreed that Migraine has a multifaceted impact on several aspects of patients’ lives. Patient-centered care, better training for healthcare providers, targeted therapies, and improved communication tools emerged as key factors in addressing the unmet medical needs of migraine sufferers.
Migraine is a chronic, debilitating neurological disorder that affects approximately 1.1 billion patients worldwide (1), with an estimated global prevalence of 14–15% (2). According to recent data, national estimates show that 8% of Greek population suffer from migraine, whereas gender wise the prevalence follows global trends (3). Migraine prevalence is highest among individuals in their most productive years, with the number of cases increasing with age and peaking between the ages of 30 and 34 for both males and females, while the prevalence in women is estimated to be 2–3 times higher than men (1, 4). Recent data suggest that headache disorders, including migraine, are ranked 14th among global causes of Disability-adjusted life years (DALYs) for all ages in both genders (4).
Migraine may manifest itself by various and heterogenous symptoms, with headache being one of them (5). In general, it is characterized by recurrent episodes of moderate to severe headaches that can last up to 72 h, if left untreated. Migraine attacks may also be accompanied by nausea, vomiting, photophobia, phonophobia, and depressive symptoms (1). In some cases migraine may be accompanied by transient focal neurological symptoms that usually precede or sometimes accompany the headache phase and are the manifestations of the migrainous aura (6). In addition, migraine is divided, based on monthly frequency into chronic migraine (CM) and episodic migraine (EM) (7). The International Classification of Headache Disorders (ICHD-3) criteria define CM as headache on ≥15 days a month for more than 3 months, which, on at least 8 days/month, has migrainous features or respond to migraine-specific analgesics (6). On the other hand, EM is characterized by less than 15 headache days monthly, with 8–14 days being classified as high frequency, and less than 8 days as moderate/low frequency episodic migraine (7, 8). According to the most recent epidemiological study, the 1% of Greek adult population suffers from CM, and 7.1% from EM (3). Μigraine often coexists with other disorders, such as depression, anxiety, epilepsy, chronic pain and cardiovascular events (9). In 2019, the Hellenic Headache Society conducted a consensus on migraine diagnosis and treatment to raise awareness, support practitioners, and improve patient care in Greece (10). According to this consensus diagnosis is based on patient history and clinical examination (10). In addition, as per this consensus, mild migraines are treated with high-dose simple analgesics, while moderate to severe cases require triptans, non-steroidal anti-inflammatory (NSAIDs), or a tailored combination (10). Preventive treatments include beta-blockers, flunarizine, valproate, topiramate, and candesartan for episodic migraines, and botulinum toxin or monoclonal antibodies targeting the CGRP pathway (anti-CGRP) for chronic or high-frequency migraines after failed prior treatments (10). Migraine translates into an immense clinical and financial burden both for migraineurs and society. More specifically, several day-to-day activities of patients’ lives such as work, school, and social, as well as overall quality of life, are frequently substantially affected (7, 8, 11–15). From an economic point of view, headache disorders have been associated with staggering costs, with estimations reaching up to €173 billion in Europe, with approximately 90% being attributed to indirect costs (16).
Migraine may also have a profound impact on patients’ quality of life and the healthcare economy (7, 8, 11–17). Despite significant advances in the field of treatment, the disease is still associated with substantial unmet medical needs, mostly due to underdiagnosis and undertreatment (18). Over the past decade, several Greek studies have been conducted in order to assess the burden of the disease, the epidemiology, and patients’ preferences (3, 19–27). These studies had been conducted using structured questionnaires providing strong numerical data but not allowing the participants to share details of their testimonies, and generated data regarding the novel treatments that were introduced for the first time in Greece (19, 28).
However, given that the landscape in migraine treatment has been rapidly changing over the last few years, it is crucial to capture a current snapshot from the patients’ standpoint regarding the migraine-related issues that they face. In this context, a Delphi survey followed by a Patients’ focus group were conducted to depict patients’ perspectives on socioeconomic and humanistic burden of migraine, as well as the unmet medical needs in the clinical management of migraine, in Greece.
To serve the objectives of the present study, a mixed design was selected. At first a modified Delphi consensus panel was conducted and then the findings of this panel were further elaborated through a patients’ focus group where they, through an open discussion, conveyed their personal experience of migraine. The Delphi method panel comprised three rounds over a period of 1 month (between March 20 and April 4, 2023). The patients’ focus group was held via videoconference lasting 3 h.
As for the Delphi panel, 20 members of the two active migraine associations in Greece were invited to participate. More specifically, the research team contacted the two Greek, migraine patient associations: the ‘Greek Society of Migraine and Headache Patients’ and the ‘Hellenic Headache Alliance.’ The Management Boards of these associations extended the invitation to 20 adult patients diagnosed with EM who were actively involved in their respective associations to voluntarily participate in the Delphi process. The selection of patients with EM in the study was based on the fact that it is the most common form of migraine according to epidemiological data, compared to CM (3). Additionally, although patients with EM may experience fewer than 15 migraine days per month, these episodes are significant enough to make them aware of the disease, thus making them more suitable for our study. Migraineurs who expressed interest in the invitation and provided their informed consent were recruited in the study, 13 members of ‘Greek Society of Migraine and Headache Patients’ and three members of the ‘Hellenic Headache Alliance’ (n = 16). Nine participants of the Delphi panel were randomly selected to participate in the focus group. All of them accepted the invitation and gave their consent to participation.
As for the Delphi panel, a structured online questionnaire, developed in Qualtrics (Provo, USA) by a steering committee of three neurologists and an expert of research methodology, was used for data collection. The questionnaire, consisting of 45 statements, was developed based on data identified through extensive literature research in PubMed database and other scientific society websites. These statements were divided into five thematic sections: Burden of migraine (11 statements), Economic burden of migraine (5 Statements), Diagnosis (8 Statements), Treatment (13 Statements) and Unmet medical need (8 Statements). The questionnaire was sent using individualized, secure links delivered by e-mail, ensuring anonymity and encouraging honest responses. A 5-point Likert scale was used to measure participants’ level of agreement with each statement (“Strongly Agree,” “Agree,” “Neither Agree nor Disagree,” “Disagree,” and “Strongly Disagree”). Response rate was augmented by e-mail reminders. Participants’ email addresses were not recorded. To facilitate convergence, the voting process was conducted in multiple (three) rounds. Upon completion of the initial round, the data were processed, and participants were provided with the consolidated results. A second round of voting was conducted including the statements which did not achieve consensus in the previous round, taking into consideration the results of the first round. After reprocessing the data from the second, a third and final round was carried out.
As for the focus group, an open and balanced discussion by all participants took place, under the co-ordination of one person (moderator). During the focus group, the results of the Delphi panel were presented, and the participants were encouraged by the moderator to comment on these, especially for statements on which consensus had not been reached. More specifically, the moderator during the meeting used prompts or probes to engage participants in deeper discussion: (a) prompting patients to provide more detail (“I would like to turn on the microphones and discuss this finding,” “I would like to hear your point of view”), (b) encouraging the continuous dialog (“What do you think is the reason for lack of consensus on this particular statement?”), and (c) summarizing and paraphrasing participants’ narratives to avoid confusion. Through the focus group process, the research team attentively listened to notes of the key words and topics to ensure all the valuable insights were collected from the patients’ perspective. The discussion was recorded and then fully transcribed verbatim, with the consent of all participants. The full literal transcription of the meeting, and the field notes of the research team were all gathered to perform a qualitative analysis.
As for the Delphi panel, the percentage of participants who responded “Agree/Strongly Agree,” “Disagree/Strongly disagree” and “Neither Agree nor Disagree” was calculated at each round. The consensus threshold was based on the guidelines proposed by Hasson et al. for the Delphi technique, according to which, a consensus level of 51–80% is recommended depending on the research objective, available resources, and other relevant factors (29). Given that the primary objective of this study was to identify unmet medical needs in migraine management, rather than to provide guidelines, the consensus threshold was set at 70% of responses, focusing on borderline options (“Strongly Agree,” “Agree,” “Disagree,” “Strongly Disagree”) (29).
As for the focus group, a thematic analysis was conducted through the provided minutes, by grouping meaningful units that refer to similar issues or content until the main topics emerged. Two researchers independently examined the minutes, to identify the relevant content. As soon as each individual analysis was completed, meetings between the two researchers were held to compare the results obtained and then to combine them. In the case of differences in opinion, theme identification was performed based on consensus. Afterwards, the research team held joint meetings to show, combine and integrate the results of the analysis from each researcher. Final themes were identified through collective discussion among all research members. Qualitative software was not utilized for data analysis.
Εthical approval of the study protocol was obtained from the Research Ethics Committee of the University of the Peloponnese. Prior their participation to the Delphi panel and focus group, all patients were required to provide written informed consent, after being thoroughly informed about the study’s purpose (29, 30). All the information obtained throughout the study cannot personally identify participants or their responses in this online survey (30). All research data was handled in accordance with the European and national regulations for the protection of personal data in scientific research.
Table 1 describes the demographics of the Delphi panel participants (n = 16). All panelists were adults, with a mean age of 42.8 years old (SD 8.2). The majority of the participants were women (64.3%) and all participants were employed. In terms of educational background, over half of the participants (57.14%) had completed post-graduate/doctoral studies, while 21.43% had received higher education.
Consensus was reached on twelve out of sixteen statements in this section, with five statements achieving 100% agreement in the first round (Table 2). No consensus was reached when patients were asked about experiencing a migraine-associated stigma and regarding health professionals’ incapability to fully understand the severity of the symptoms that people with migraine are experiencing. Moreover, consensus was not reached regarding the increased frequency of the visits to physicians and emergency hospital departments, and the frequent use of costly diagnostic tests.
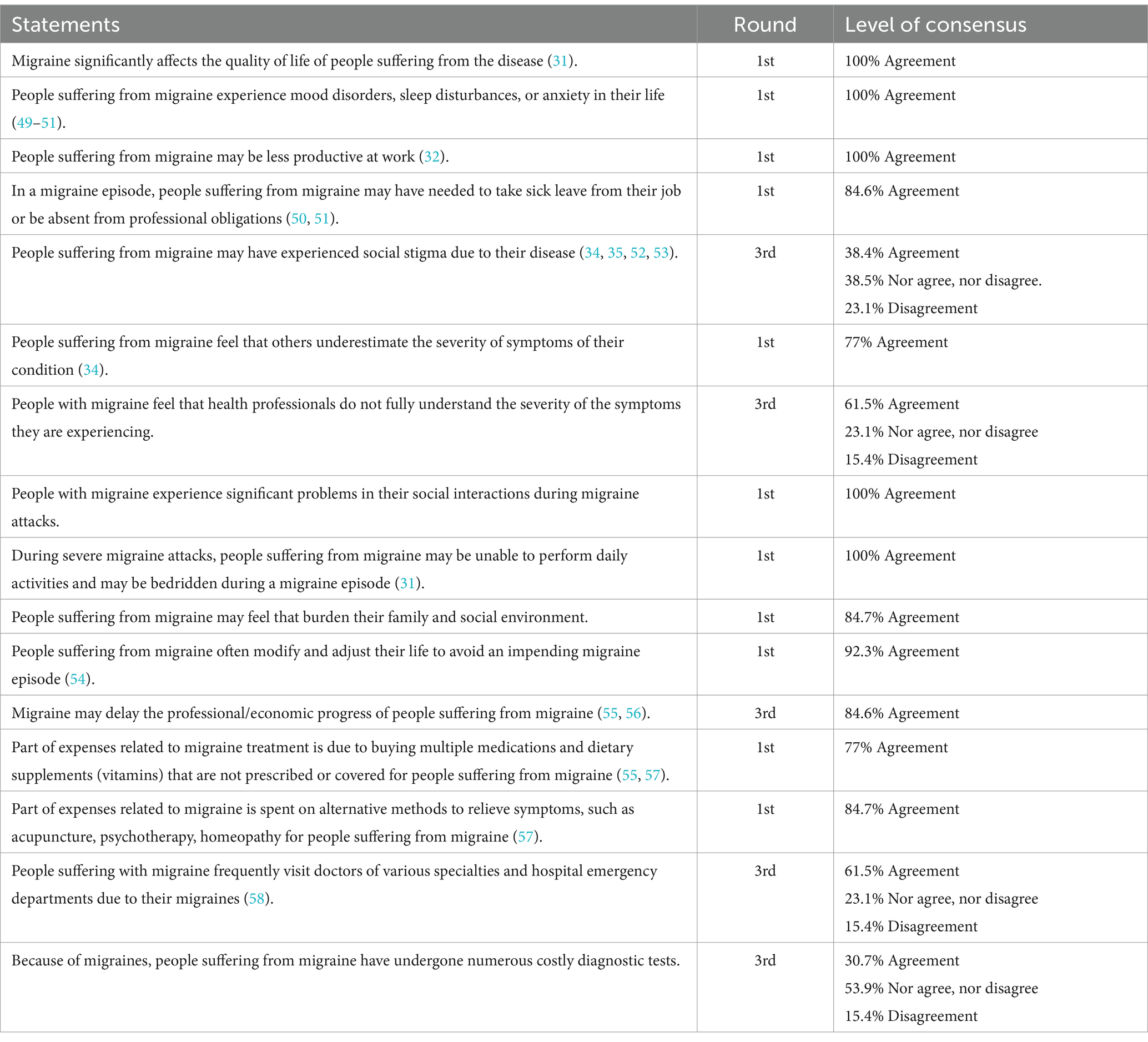
Table 2. Results regarding Burden of disease (quality of life, social impacts, psychological impacts, work-related impacts).
Regarding diagnosis, six out of eight statements garnered consensus among the panelists; two statements met with disagreement, while one achieved unanimous agreement (100%) (Table 3). No consensus was reached regarding the identification of the triggers that initiate a migraine episode and the association between the delay in diagnosis and the examination time spent by the physician.
In this section, nine out of thirteen statements reached consensus in agreement, with two of them achieving 100% agreement (Table 4). Consensus was not reached regarding about the use of opioids for the management of a migraine attack, the delayed relief time of recommended medications during a migraine attack, patients’ compliance with their doctor’s instructions on pharmaceutical treatment, and patients’ decision to discontinue preventive medications upon improvement.
A clear consensus was achieved regarding the existence of unmet medical needs, with seven out of eight statements aligning in agreement including two that reached unanimous agreement (100%) (Table 5). Consensus was not reached regarding whether a reduced number of medications would make adherence to migraine treatment easier.
The patients’ discussion during the focus group meeting was analyzed and three key themes emerged: (a) work and social life: lack of awareness and understanding; (b) limiting the impact of migraine on daily life; and (c) migraine management: late diagnosis, low treatment adherence and concerns about treatment. These three emerging themes were evident in the narratives retrieved from patients’ descriptions (Table 6).
Patients emphasized the need for sick leave during migraine attacks due to inability to fulfill professional obligations. However, lack of understanding from their colleagues and managers/employers discourages their absences from work. They emphasized that this lack of understanding from their workplace might stem from lack of awareness about migraine. In addition, patients noted that they avoid communicating their disease and self-isolate in order not to be a burden for their friends and family. On that basis, migraine patients do not communicate their condition, resulting in their self-isolation and self-stigmatization. Additionally, they commented that, as a term, the word “stigma” is perceived with a strong negative connotation. Some patients admitted feeling ashamed about their disease.
Migraineurs live in fear of another migraine episode. As such, they modify their daily activities to avoid even a migraine attack per month, as even this will be a benefit to them. Patients mainly discussed the triggering mechanisms and how they widely vary among individuals. Some patients, despite acknowledging the existence of triggering mechanisms in migraine, noted that these mechanisms are not a sufficient and necessary condition for the existence or avoidance of a migraine attack. However, patients seem to believe that with appropriate treatment, they can stop modifying their lives to such a large extent and live more freely.
During the focus group, the patients reported various factors leading to the delayed diagnosis of migraine and consequently to its appropriate treatment. Many patients admitted that they have been self-medicating with over-the-counter drugs and pain relievers for a long period to control their disease, before seeking professional medical advice. Moreover, they mentioned that it takes them a long time to find the appropriate medical care, since they visit different medical specialties until they find the one who will be able to effectively help them manage their migraine. The need for effective migraine management peaks during middle age, resulting in the most persistent seeking of medical care. Physicians who are not specialized in Migraine/Headache disorders, seem to have inability to fully comprehend migraine patients and the severity of their symptoms seems to attribute to delay diagnosis, as well. Participants highlighted the need for further training of Physicians/Neurologists on headache disorders to increase their awareness. However, a noticeable improvement in physicians’ understanding of migraine during the last years was pointed out by patients.
Moreover, participants mentioned that they are subjected to various diagnostic tests when they wander between different medical specialties looking for their diagnosis, while a neurologist/migraine specialist can make a diagnosis based only on the patient’s detailed medical history. Many patients mentioned that clinical practice that involves costly diagnostic tests is considered outdated. However, they noted an interesting paradox in the Greek healthcare system; the fact that certain high-cost diagnostic tests (e.g., magnetic resonance imaging-MRI) have occasionally been requested for prescription and reimbursement of newer, more targeted to migraine treatments. Moreover, patients have actively reached out to the National Health Service Provider Agency (E.O.P.Y.Y.) to address and eliminate this practice.
During the discussion patients stated that there were high levels of dissatisfaction with the traditional oral preventive therapies because some of them were prescribed as off-label treatments. The patients’ expectation of immediate reduction of migraine attacks leads to disappointment that the desired outcome is not achieved and then to lower adherence to preventive migraine treatments. Moreover, patients’ non-adherence to preventive treatment of migraine and its early discontinuation may also be driven by the relief of their symptoms. In this context, patients emphasized the value of effective patient-physician communication in preventive treatment adherence. Moreover, patients noted that regular monitoring with neurologist visits every 3 months and adjustment of medication are crucial aspects of migraine management that might result in increased treatment adherence, particularly for those receiving preventive therapy. In addition, they highlighted the need for physicians to communicate treatment-related information clearly and comprehensibly. Furthermore, they highlighted the importance of easy-to-use aids, − such as applications, patient decision aids, apps, e-diaries, − in creating a patient-specific database from which both the physicians and patients can draw valuable conclusions. Finally, patients expressed their concern/agony about their therapeutic alternatives at older age and in case they suffer from specific comorbidities.
This study aimed to capture patients’ views and experiences to highlight the socioeconomic burden and the unmet medical needs regarding the clinical diagnosis and management of migraine, in a Greek, real-world setting. To the best of our knowledge, although, there have been Greek studies in the past which analyzed quantitatively patients’ preferences and satisfaction with treatment as well as the burden of disease, this is the first one to describe the experiences of migraineurs through a qualitative analysis (3, 19–21, 28).
Our results regarding patients’ day-to-day activities are in line with those of a previous Greek study, highlighting the need for patients to modify their lives during a migraine crisis or in order to avoid it (3). A plethora of studies have shown that migraineurs often find it difficult to carry out daily tasks, including substantial disruptions in their work efficiency, due to migraine episodes (31–33). In our findings, it was clear that despite the need for sick leave during migraine attacks, migraneurs rarely ask for sick leave, possibly due to social stigma from their colleagues and employers (3, 34, 35). There is evidence supporting that migraine patients may suffer from internalized stigma, a psychological and cognitive effect resulting from society’s negative perception of the disease (34). In our study, while patients emphasized that they felt underestimated by their social and family environment and struggled to communicate their disease, the social stigma associated with migraine was not fully expressed by them. This discrepancy, between our study and other published results could be attributed to the existence of negative connotations associated with the Greek term for “stigma.” Moreover, another possible explanation may be associated with the fact that patients tend to avoid stigmatization by bypassing any health-related discussion to avoid negative perceptions, but they are self-stigmatized. An Italian Delphi study focused on women with migraine, including patients in its panel, revealed that they also experience a high burden and are significantly impacted by stigma, which affects their well-being (36).
Our research revealed that Greek patients are self-medicated by receiving analgesics for years before seeking professional medical advice. This finding coincides with the observations published by Davies et al., according to which patients suffer between 6 and 10 years prior to seeking medical advice, resulting in delays receiving a formal migraine diagnosis (37). Late diagnosis, either due to patients’ negligence or due to the involvement of multiple physicians before referring to a headache specialist, remains a major challenge in migraine management. In the Italian Delphi study, highlighted that women with migraine often misinterpret their symptoms as unrelated to a disease, causing delays in seeking medical support (36). Thus, it is crucial to streamline the diagnostic process and raise awareness both among patients and healthcare providers.
Another topic of great importance in the treatment of migraine is patient’s adherence. Patients’ adherence is a multidimensional phenomenon (32). In line with previous studies, our study also stressed the importance of shared patient-physician decision-making in the course of their treatment (38, 39). In addition, similar to other published data (40), our study revealed that effective patient-physician communication has a significant impact on the patient’s adherence to the prescribed treatment regimens. These results illustrate the need to develop a patient-centered approach to establish relations of mutual trust between the patients and the healthcare systems and thus promote clinical decisions that will enhance treatment optimization.
Finally, from a treatment standpoint, our findings mirror the diverse and nuanced nature of the current therapeutic armamentarium for migraine. Overall, in accordance with existing evidence (41, 42), a high degree of dissatisfaction with traditional treatment options, was highlighted despite the plethora of available choices. Indeed, several migraine medications have safety profiles that are not always favorable, multiple interactions, several contraindications and age restrictions (43, 44). Furthermore, the need for specialized education by health care providers that has been previously reported, was also illustrated in our study (45). Undeniably, access to novel targeted therapies has revolutionized the landscape of migraine treatment, due to their efficacy and favorable safety profiles (3). The latter was also portrayed in our results. However, the need for developing safe and concurrently effective agents, especially for patients suffering from comorbidities such as cardiovascular diseases and people older than 65 years old, is still pending (32). According to a Dutch Delphi study with open-ended questions conducted among migraine patients, the primary concerns expressed by patients were the need for medications to act faster, relieve pain at an earlier stage, restore functionality quickly, and prevent recurrence (46).
In terms of improving treatment outcomes, our study showed that the incorporation of technology could facilitate seamless communication between patients and their clinicians. Existing evidence shows that the use of digital tools enables patients to easily record and share migraine-related information during medical visits, thus improving the quality of care and promoting better outcomes (47). However, while the available tools are promising for diary keeping, their daily use can be burdensome, often leading to reduced adherence or abandonment.
This study highlights several unmet needs that should be emphasized during clinical visits. Effective communication between patients and physicians is crucial for improving treatment adherence and patients’ satisfaction. Additionally, better education of healthcare providers on migraine management could reduce diagnostic delays and improve care. Finally, addressing patient dissatisfaction with traditional treatments and discussing newer, targeted therapies should be a priority in clinical practice to optimize health outcomes. Our study limitations are directly associated with the nature of the Delphi panel and focus group methodology. Specifically, limitations include the difficulty of generalizing the results to a wider population, due to small sample size and selection criteria of panelists (members of patients’ associations with EM), which is characteristic of the Delphi technique (48). The selection of patients with EM for the study was based on epidemiological data showing that it is the most common form of migraine compared to CM, and despite experiencing fewer than 15 migraine days per month, their episodes are significant enough to raise awareness of the disease, making them suitable for our study; however, this may limit the extrapolation of the results to the broader migraine population. However, these results offer important preliminary insights into the unmet needs and challenges faced by migraine patients, which may guide further research and clinical practice. Future studies should aim to recruit larger, more diverse, and representative patient populations to validate these findings. While in the case of Delphi panel entering data into an online platform is considered an advantage, it might also cause inconvenience for some panelists (48). Moreover, during the Delphi rounds, participants were unable to rephrase the statements, make comments, or request clarifications. This restriction may have led to misunderstandings or misinterpretations of specific statements, which in turn contributed to failure to reach consensus. In addition, despite the consent of participants to take part in the open discussion during the focus group, there was concern that they did not feel comfortable fully expressing themselves in front of an audience. However, this study offers an initial reference point to further design and conduct more focused and populated consensus studies in our country, as well as contributing to a deeper understanding of the perspectives of patients.
This study highlights migraine’s multifaceted impact on patients’ daily activities, productivity and overall quality of life. Moreover, our results underline the challenges associated with timely diagnoses and effective treatment. Patient-centered care, better education for healthcare providers, targeted therapies and improved communication tools emerged as key factors in addressing unmet needs of migraine patients. Continuous recording of such information so that it is taken into consideration both by physicians and health policy decision makers is essential. It is important to promote patients’ involvement in studies that incorporate their ideas or address their concerns, as well as improved implementation of research findings because inclusive approach ultimately leads to improved quality of care.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the Research Ethics Committee of the University of the Peloponnese. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
MV: Conceptualization, Methodology, Writing – review & editing. GK: Conceptualization, Formal analysis, Investigation, Methodology, Supervision, Writing – original draft. LB: Writing – review & editing. KB: Writing – review & editing. EB: Writing – review & editing. AS: Writing – review & editing. DT: Writing – review & editing. KL: Formal analysis, Investigation, Methodology, Writing – original draft. SZ: Writing – review & editing. TK: Conceptualization, Methodology, Writing – review & editing. D-DM: Conceptualization, Methodology, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was sponsored by Pfizer Hellas S. A. Pfizer was not involved in the management of participants' personal information, data analysis and results interpretation.
We extend our heartfelt gratitude to the patients from “Greek Society of Migraine and Headache Patients” and “Hellenic Headache Society” who participated in this study. Their willingness to contribute their time and health information is invaluable and has significantly enhanced the depth and quality of this study. We would also like to thank Assistant Professor Aspasia Panagiotou and Associate Professor Panagiotis Andriopoulos, employees of the University of Peloponnese, for their valuable contributions to the development of this manuscript.
Dimos-Dimitrios Mitsikostas, Michail Vikelis, and Theodoros Karapanayiotides received compensation from Pfizer for their services as members of the Steering Committee for this study. Konstantinos Bilias is the General Secretary of the “Greek Society of Migraine and Headache Patients,” which has received compensation from Pfizer for its representatives’ participation to the study, following the Code of Practice of Hellenic Association of Pharmaceutical Companies. Elena Barbalia is the President of the “Hellenic Headache Society,” which has received compensation from Pfizer for its representatives’ participation to the study, following the Code of Practice of Hellenic Association of Pharmaceutical Companies. Argyro Solakidi and Dimitrios Trafalis are employees of Pfizer Hellas S.A. Pfizer was not involved in the management of participants’ personal information, data analysis and results interpretation. Katerina Lioliou, Sofia Zyga and Georgia Kourlaba are employees of University of Peloponnese, which received funding from Pfizer in connection with the development of this manuscript.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
The authors declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Amiri, P, Kazeminasab, S, Nejadghaderi, SA, Mohammadinasab, R, Pourfathi, H, Araj-Khodaei, M, et al. Migraine: a review on its history, global epidemiology, risk factors, and comorbidities. Front Neurol. (2021) 12:800605. doi: 10.3389/fneur.2021.800605
2. Steiner, TJ, and Stovner, LJ. Global epidemiology of migraine and its implications for public health and health policy. Nat Rev Neurol. (2023) 19:109–17. doi: 10.1038/s41582-022-00763-1
3. Constantinidis, TS, Arvaniti, C, Fakas, N, Rudolf, J, Kouremenos, E, Giannouli, E, et al. A population-based survey for disabling headaches in Greece: prevalence, burden and treatment preferences. Cephalalgia. (2021) 41:810–20. doi: 10.1177/0333102421989630
4. Steiner, TJ, Stovner, LJ, Jensen, R, Uluduz, D, and Katsarava, Z. On behalf of lifting the burden: the global campaign against H. Migraine remains second among the world’s causes of disability, and first among young women: findings from GBD2019. J Headache Pain. (2020) 21:137. doi: 10.1186/s10194-020-01208-0
5. Karsan, N, and Goadsby, PJ. Migraine is more than just headache: is the link to chronic fatigue and mood disorders simply due to shared biological systems? Front Hum Neurosci. (2021) 15:646692. doi: 10.3389/fnhum.2021.646692
6. International Headache Society. Headache classification Committee of the International Headache Society (IHS) the international classification of headache disorders, 3rd edition. Cephalalgia. (2018) 38:1–211. doi: 10.1177/0333102417738202
7. Blumenfeld, AM, Varon, SF, Wilcox, TK, Buse, DC, Kawata, AK, Manack, A, et al. Disability, HRQoL and resource use among chronic and episodic migraineurs: results from the international burden of migraine study (IBMS). Cephalalgia. (2011) 31:301–15. doi: 10.1177/0333102410381145
8. Buse, DC, Reed, ML, Fanning, KM, Bostic, RC, and Lipton, RB. Demographics, headache features, and comorbidity profiles in relation to headache frequency in people with migraine: results of the American migraine prevalence and prevention (AMPP) study. Headache. (2020) 60:2340–56. doi: 10.1111/head.13966
9. Ashina, M, Katsarava, Z, Do, TP, Buse, DC, Pozo-Rosich, P, Ozge, A, et al. Migraine: epidemiology and systems of care. Lancet. (2021) 397:1485–95. doi: 10.1016/S0140-6736(20)32160-7
10. Kouremenos, E, Arvaniti, C, Constantinidis, TS, Giannouli, E, Fakas, N, Kalamatas, T, et al. Consensus of the Hellenic headache society on the diagnosis and treatment of migraine. J Headache Pain. (2019) 20:113. doi: 10.1186/s10194-019-1060-6
11. Martelletti, P, Schwedt, TJ, Lanteri-Minet, M, Quintana, R, Carboni, V, Diener, HC, et al. My migraine voice survey: a global study of disease burden among individuals with migraine for whom preventive treatments have failed. J Headache Pain. (2018) 19:115. doi: 10.1186/s10194-018-0946-z
12. Buse, D, Manack, A, Serrano, D, Reed, M, Varon, S, Turkel, C, et al. Headache impact of chronic and episodic migraine: results from the American migraine prevalence and prevention study. Headache. (2011) 52:3–17. doi: 10.1111/j.1526-4610.2011.02046.x
13. Ford, JH, Jackson, J, Milligan, G, Cotton, S, Ahl, J, and Aurora, SK. A real-world analysis of migraine: A cross-sectional study of disease burden and treatment patterns. Headache. (2017) 57:1532–44. doi: 10.1111/head.13202
14. Doane, MJ, Gupta, S, Fang, J, Laflamme, AK, and Vo, P. The humanistic and economic burden of migraine in Europe: a cross-sectional survey in five countries. Neurol Ther. (2020) 9:535–49. doi: 10.1007/s40120-020-00196-2
15. Ford, JH, Foster, SA, Nichols, RM, Tockhorn-Heidenreich, A, Ye, W, Jackson, J, et al. A real-world analysis of patient-reported outcomes in patients with migraine by preventive treatment eligibility status in the US and Europe. J Patient. (2020) 4:53. doi: 10.1186/s41687-020-00221-w
16. Linde, M, Gustavsson, A, Stovner, LJ, Steiner, TJ, Barré, J, Katsarava, Z, et al. The cost of headache disorders in Europe: the Eurolight project. Eur J Neurol. (2012) 19:703–11. doi: 10.1111/j.1468-1331.2011.03612.x
17. Jellestad, PL, Carlsen, LN, Westergaard, ML, Munksgaard, SB, Bendtsen, L, Lainez, M, et al. Economic benefits of treating medication-overuse headache - results from the multicenter COMOESTAS project. Cephalalgia. (2019) 39:274–85. doi: 10.1177/0333102418786265
18. Piccinni, C, Cevoli, S, Ronconi, G, Dondi, L, Calabria, S, Pedrini, A, et al. A real-world study on unmet medical needs in triptan-treated migraine: prevalence, preventive therapies and triptan use modification from a large Italian population along two years. J Headache Pain. (2019) 20:74. doi: 10.1186/s10194-019-1027-7
19. Dermitzakis, EV, Kouroudi, A, Argyriou, AA, Spingos, KC, Bilias, K, and Vikelis, M. Results of a web-based survey of 2105 Greek migraine patients in 2020: demographics, clinical characteristics, burden and the effects of the COVID-19 pandemic on the course of migraine. BMC Neurol. (2022) 22:440. doi: 10.1186/s12883-022-02968-9
20. Dermitzakis, EV, Bilias, K, Vlachou, E, Barmpa, E, and Vikelis, M. Results of an online survey of 1.091 patients with migraine in Greece in 2018. Epidemiological data, treatment options and effectiveness of treatment; the social, economic and emotional impact of the disease. Νευρολογία. (2018) 28:12–7.
21. Mitsikostas, DD, Belesioti, I, Arvaniti, C, Mitropoulou, E, Deligianni, C, Kasioti, E, et al. Patients' preferences for headache acute and preventive treatment. J Headache Pain. (2017) 18:102. doi: 10.1186/s10194-017-0813-3
22. Vikelis, M, Rikos, D, Argyriou, AA, Papachristou, P, Rallis, D, Karapanayiotides, T, et al. Preferences and perceptions of 617 migraine patients on acute and preventive migraine treatment attributes and clinical trial endpoints. Expert Rev Neurother. (2024) 24:815–26. doi: 10.1080/14737175.2024.2365312
23. Mitsikostas, DD, Gatzonis, S, Thomas, A, Kalfakis, N, IIias, A, and Papageoergiou, C. An epidemiological study of headaches among medical students in Athens. Headache. (1996) 36:561–4. doi: 10.1046/j.1526-4610.1996.3609561.x
24. Mitsikostas, DD, Tsaklakidou, D, Athanasiadis, N, and Thomas, A. The prevalence of headache in Greece: correlations to latitude and climatological factors. Headache. (1996) 36:168–73. doi: 10.1046/j.1526-4610.1996.3603168.x
25. Mitsikostas, DD, Thomas, A, Gatzonis, S, Ilias, A, and Papageorgiou, C. An epidemiological study of headache among the monks of Athos (Greece). Headache. (1994) 34:539–41. doi: 10.1111/j.1526-4610.1994.hed3409539.x
26. Constantinidis, TS, Arvaniti, C, Fakas, N, Rudolf, J, Kouremenos, E, Giannouli, E, et al. The prevalence and burden of medication overuse headache in Greece. Cephalalgia. (2023) 43:3331024231184909. doi: 10.1177/03331024231184909
27. Mantonakis, L, Belesioti, I, Deligianni, CI, Natsis, V, Mitropoulou, E, Kasioti, E, et al. Depression and anxiety symptoms in headache disorders: an observational, cross-sectional study. Neurol Int. (2024) 16:356–69. doi: 10.3390/neurolint16020026
28. Dermitzakis, EV, Argyriou, AA, Bilias, K, Barmpa, E, Liapi, S, Rikos, D, et al. Results of a web-based survey on 2565 Greek migraine patients in 2023: demographic data, imposed burden and satisfaction to acute and prophylactic treatments in the era of new treatment options. J Clin Med. 13:13. doi: 10.3390/jcm13102768
29. Hasson, F, Keeney, S, and McKenna, H. Research guidelines for the Delphi survey technique. J Adv Nurs. (2000) 32:1008–15. doi: 10.1046/j.1365-2648.2000.t01-1-01567.x
30. Slade, SC, Dionne, CE, Underwood, M, and Buchbinder, R. Standardised method for reporting exercise programmes: protocol for a modified Delphi study. BMJ Open. (2014) 4:e006682. doi: 10.1136/bmjopen-2014-006682
31. Al Ghadeer, HA, AlSalman, SA, Albaqshi, FM, Alsuliman, SR, Alsowailem, FA, Albusror, HA, et al. Quality of life and disability among migraine patients: a single-center study in AlAhsa, Saudi Arabia. Cureus. (2021) 13:e19210. doi: 10.7759/cureus.19210
32. Ailani, J, Burch, RC, and Robbins, MS. Board of Directors of the American headache S. The American headache society consensus statement: update on integrating new migraine treatments into clinical practice. Headache. (2021) 61:1021–39. doi: 10.1111/head.14153
33. Burton, WN, Schultz, AB, Shepherd, ME, and Hines, D. Migraine headache in an employed population: demographics, health risks, pharmaceutical utilization, and productivity loss. J Occup Environ Med. (2022) 64:679–85. doi: 10.1097/JOM.0000000000002564
34. Parikh, SK, and Young, WB. Migraine: stigma in society. Curr Pain Headache Rep. (2019) 23:8. doi: 10.1007/s11916-019-0743-7
35. Young, WB, Park, JE, Tian, IX, and Kempner, J. The stigma of migraine. PLoS One. (2013) 8:e54074. doi: 10.1371/journal.pone.0054074
36. Cevoli, S, Barbanti, P, Finocchi, C, Benedan, L, Mariani, P, Orthmann, N, et al. Improvement in diagnostic-therapeutic care pathways for women with migraine: an Italian Delphi panel. Front Neurol. (2024) 15:1436258. doi: 10.3389/fneur.2024.1436258
37. Davies, PTG, Lane, RJM, Astbury, T, Fontebasso, M, Murphy, J, and Matharu, M. The long and winding road: the journey taken by headache sufferers in search of help. Prim Health Care Res Dev. (2019) 20:e4. doi: 10.1017/S1463423618000324
38. Packard, RC. What does the headache patient want? Headache. (1979) 19:370–4. doi: 10.1111/j.1526-4610.1979.hed1907370.x
39. Porta-Etessam, J, Santos-Lasaosa, S, Rodríguez-Vico, J, Núñez, M, Ciudad, A, Díaz-Cerezo, S, et al. Evaluating the impact of a training program in shared decision-making for neurologists treating people with migraine. Neurol Ther. (2023) 12:1319–34. doi: 10.1007/s40120-023-00495-4
40. Buse, DC, and Lipton, RB. Facilitating communication with patients for improved migraine outcomes. Curr Pain Headache Rep. (2008) 12:230–6. doi: 10.1007/s11916-008-0040-3
41. Edmeads, J, Lainez, JM, Brandes, JL, Schoenen, J, and Freitag, F. Potential of the migraine disability assessment (MIDAS) questionnaire as a public health initiative and in clinical practice. Neurology. (2001) 56:S29–34. doi: 10.1212/WNL.56.suppl_1.S29
42. Silberstein, SD, and Rosenberg, J. Multispecialty consensus on diagnosis and treatment of headache. Neurology. (2000) 54:1553. doi: 10.1212/WNL.54.8.1553
43. American Headache Society. The American headache society position statement on integrating new migraine treatments into clinical practice. Headache. (2019) 59:1–18. doi: 10.1111/head.13456
44. Steiner, TJ, Jensen, R, Katsarava, Z, Linde, M, MacGregor, EA, Osipova, V, et al. Aids to management of headache disorders in primary care. J Headache Pain. (2019) 20:1–52. doi: 10.1186/s10194-018-0899-2
45. Pozo-Rosich, P, Lucas, C, Watson, DPB, Gaul, C, Ramsden, E, Ritter, S, et al. Burden of migraine in patients with preventive treatment failure attending European headache specialist centers: real-world evidence from the BECOME study. Pain Ther. (2021) 10:1691–708. doi: 10.1007/s40122-021-00331-3
46. Smelt, AF, Louter, MA, Kies, DA, Blom, JW, Terwindt, GM, van der Heijden, GJ, et al. What do patients consider to be the most important outcomes for effectiveness studies on migraine treatment? Results of a Delphi study. PLoS One. (2014) 9:e98933. doi: 10.1371/journal.pone.0098933
47. Dodick, DW, Tepper, SJ, Lipton, RB, Buse, DC, Stewart, WF, Bayliss, M, et al. Improving medical communication in migraine management: A modified Delphi study to develop a digital migraine tracker. Headache. (2018) 58:1358–72. doi: 10.1111/head.13426
48. Fink-Hafner, D, Dagen, T, Doušak, M, Novak, M, and Hafner-Fink, M. Delphi method: strengths and weaknesses. Adv Methodol Stat. (2019) 16:1–19. doi: 10.51936/fcfm6982
49. Silberstein, SD, and Lipton, RB. Epidemiology of migraine. Neuroepidemiology. (1993) 12:179–94. doi: 10.1159/000110317
50. Minen, MT, Begasse De Dhaem, O, Kroon Van Diest, A, Powers, S, Schwedt, TJ, Lipton, R, et al. Migraine and its psychiatric comorbidities. J Neurol Neurosurg Psychiatry. (2016) 87:741–9. doi: 10.1136/jnnp-2015-312233
51. Morgan, I, Eguia, F, Gelaye, B, Peterlin, BL, Tadesse, MG, Lemma, S, et al. Sleep disturbances and quality of life in sub-Saharan African migraineurs. J Headache Pain. (2015) 16:18. doi: 10.1186/s10194-015-0504-x
52. Steiner, TJ, Stovner, LJ, and Vos, T. GBD 2015: migraine is the third cause of disability in under 50s. J Headache Pain. (2016) 17:104. doi: 10.1186/s10194-016-0699-5
53. Jacoby, A. Felt versus enacted stigma: a concept revisited. Evidence from a study of people with epilepsy in remission. Soc Sci Med. (1994) 38:269–74.
54. Lo, SH, Gallop, K, Smith, T, Powell, L, Johnston, K, Hubig, LT, et al. Real-world experience of interictal burden and treatment in migraine: a qualitative interview study. J Headache Pain. (2022) 23:1–10. doi: 10.1186/s10194-022-01429-5
55. Bonafede, M, Sapra, S, Shah, N, Tepper, S, Cappell, K, and Desai, P. Direct and indirect healthcare resource utilization and costs among migraine patients in the United States. Headache. (2018) 58:700–14. doi: 10.1111/head.13275
56. Gilligan, AM, Foster, SA, Sainski-Nguyen, A, Sedgley, R, Smith, D, and Morrow, P. Direct and indirect costs among United States commercially insured employees with migraine. J Occup Environ Med. (2018) 60:1120–7. doi: 10.1097/JOM.0000000000001450
57. Gibbs, SN, Shah, S, Deshpande, CG, Bensink, ME, Broder, MS, Dumas, PK, et al. United States Patients' perspective of living with migraine: country-specific results from the global "my migraine voice" survey. Headache. (2020) 60:1351–64. doi: 10.1111/head.13829
58. Kikui, S, Chen, Y, Todaka, H, Asao, K, Adachi, K, and Takeshima, T. Burden of migraine among Japanese patients: a cross-sectional National Health and wellness survey. J Headache Pain. (2020) 21:110. doi: 10.1186/s10194-020-01180-9
59. Negro, A, Sciattella, P, Rossi, D, Guglielmetti, M, Martelletti, P, and Mennini, FS. Cost of chronic and episodic migraine patients in continuous treatment for two years in a tertiary level headache centre. J Headache Pain. (2019) 20:120. doi: 10.1186/s10194-019-1068-y
60. Baos, V, Ester, F, Castellanos, A, Nocea, G, Caloto, MT, and Gerth, WC. Use of a structured migraine diary improves patient and physician communication about migraine disability and treatment outcomes. Int J Clin Pract. (2005) 59:281–6. doi: 10.1111/j.1742-1241.2005.00469.x
61. Patwardhan, M, Coeytaux, RR, Deshmukh, R, and Samsa, G. What is the impact of physician communication and patient understanding in the management of headache? Neuropsychiatr Dis Treat. (2007) 3:893–7. doi: 10.2147/NDT.S493
62. Stone, MT, Weed, V, and Kulich, RJ. Opioid treatment of migraine: risk factors and behavioral issues. Curr Pain Headache Rep. (2016) 20:51. doi: 10.1007/s11916-016-0581-9
63. Takahashi, TT, Ornello, R, Quatrosi, G, Torrente, A, Albanese, M, Vigneri, S, et al. Medication overuse and drug addiction: a narrative review from addiction perspective. J Headache Pain. (2021) 22:32. doi: 10.1186/s10194-021-01224-8
64. Mitsikostas, DD, Alexoudi, A, Arvaniti, C, Giannouli, E, Kouremenos, Ε, Constantinidis, TS, et al. Hellenic headache society recommendations for the use of monoclonal antibodies targeting the calcitonin gene-related peptide pathway for the prevention of migraine and cluster headache—2023 update. SN Compr Clin Med. (2023) 5:118. doi: 10.1007/s42399-023-01452-w
Keywords: migraine, Delphi consensus, patients, burden, unmet needs, Greece
Citation: Vikelis M, Kourlaba G, Barba L, Bilias K, Barbalia E, Solakidi A, Trafalis D, Lioliou K, Zyga S, Karapanayiotides T and Mitsikostas D-D (2025) The unmet needs in management, the treatment gap and the burden of migraine in Greece: a Delphi consensus and focus group study from patients’ perspective. Front. Neurol. 16:1558014. doi: 10.3389/fneur.2025.1558014
Received: 09 January 2025; Accepted: 10 February 2025;
Published: 24 February 2025.
Edited by:
Antonio Russo, University of Campania Luigi Vanvitelli, ItalyReviewed by:
Raffaele Ornello, University of L’Aquila, ItalyCopyright © 2025 Vikelis, Kourlaba, Barba, Bilias, Barbalia, Solakidi, Trafalis, Lioliou, Zyga, Karapanayiotides and Mitsikostas. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Georgia Kourlaba, g.kourlaba@uop.gr
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.