
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol. , 21 March 2025
Sec. Stroke
Volume 16 - 2025 | https://doi.org/10.3389/fneur.2025.1539107
This article is part of the Research Topic Quality of Stroke Care: What Could Be Improved, and How? - Volume II View all 9 articles
Background and aims: The transformation of modified Rankin Scale (mRS) scores based on the corresponding utilities of health-related quality of life questionnaires can facilitate the capture of Patient-Centered Outcomes (PCO) in stroke. We aimed to derive utility-weighted modified Rankin Scale (UW-mRS) values by mapping mRS functional status to EQ-5D-3L scores in a population-based cohort of stroke patients.
Methods: The UW-mRS was obtained by analyzing the EQ5-D-3 L and mRS scores at 180 days after any stroke in the ÑANDU study, a large prospective community-based study in Chile. The mRS prediction was estimated using a linear regression adjusted by the EQ-5D-3L value. Generalized linear and binary logistic regression models were constructed to determine influencing factors of the UW-mRS, using STATA software (version 18.0).
Results: We included 773 patients presenting with any stroke during 2015–2016: 48% were female, with a mean age of 71 years (SD 13.8), and 85% had an acute ischemic stroke (AIS). 82% of patients had a low socioeconomic status, 50% had less than 12 years of formal education, and only 32% lived in urban areas. UW-mRS values for mRS categories 0–6 at 180 days were 0.913, 0.694, 0.425, 0.249, −0.102, −0.347 and 0, respectively. Multivariable analysis identified age > 70 years (Coefficient β [β] -0.038 [Standard error SE 0.018], p = 0.032), prior mRS score 3–5 (β −0.556 [SE 0.197], p < 0.001), ischemic stroke (β −0.066 [SE 0.025], p = 0.010), and National Institutes of Health Stroke Scale (NIHSS) at admission>5 (β −0.015 [SE 0.002], p < 0.001) as significant predictors of worse UW-mRS scores (R2 = 70%) in the overall group. Sex-disaggregated analysis showed that age > 70 years was a significant predictor in males (β −0.069 [SE 0.024], p = 0.006), while presenting an AIS had a greater impact on female’s worse UW-mRS score (β −0.087 [SE 0.033], p = 0.010).
Conclusion: These results present UW-mRS values derived from a population-based stroke study. Key determinants of health-related quality of life in post-stroke patients included age, prior disability, and stroke severity. Sex-disaggregated analysis revealed age being significant for males and AIS for females. Incorporating PCO as UW-mRS in stroke research can provide a more nuanced understanding of the impact of stroke on survivors, offering valuable insights for clinical decision-making and rehabilitation strategies across diverse healthcare contexts.
According to the most recent Global Burden of Disease (GBD) study, stroke remains one of the leading cause of death and disability combined worldwide (1). Between 1990 to 2019, the global burden of stroke, in terms of absolute number of cases, increased substantially, with the majority (86.0% of deaths and 89.0% of disability-adjusted life years, DALYs) residing in low- and lower-middle-income countries (LMICs) (2). Given the wide range of functional disability among stroke survivors, it is crucial to accurately measure and classify these impairments.
Several scales have been developed to categorize stroke patients. The modified Rankin Scale (mRS), a seven-level scale of global impairment and disability is widely used as a functional outcome measure in both clinical research and practice (3). While the mRS provides valuable insights into functional status, it does not reflect the broader impact on quality of life (4). Moreover, its power is limited when analyzed dichotomously and its indication of effect size is difficult to interpret when analyzed ordinally (5). Therefore, the development of a utility-weighted modified Rankin scale (UW-mRS), which incorporates a health utility scale as Patient Centered Outcome (PCO), is recommended and has been used in several recent clinical trials (6, 7).
Health utility weights represent the preference for a specific health outcome, allowing comparison of quality of life across different clinical settings (8). They range from perfect health (a score of 1) to outcomes worse than death (where death is scored as 0 and negative values indicate worse-than-death states). The utility approach offers several advantages: it aligns with the principles of economic evaluation, enables broad comparisons, and provides a detailed view of patients’ experiences, highlighting both improvements and declines in health status (8). Despite these benefits, the application of UW-mRS outside the clinical setting remains limited (9).
The aim of this study was to incorporate the quality-of-life perspective into functional scales and analyze its determinants, by developing the UW-mRS as an outcome measure for patients 180 days after suffering a stroke, using data from the Ñuble population between 2015 and 2017.
Individual participant data were pooled from the ÑANDU study, a large prospective community-based study in Chile, whose methodology and results have been previously published (10). At 180 days after the event, trained personnel conducted telephone interviews to evaluate the patients. Information was collected on recovery, dependency, and health-related quality of life.
The mRS is a widely used tool for assessing health outcomes in stroke patients (11). The mRS evaluates the level of disability by considering activity limitations and lifestyle changes. The scale has 7 grades, from 0 to 6: 0 means no symptoms, 5 means severe disability, and 6 indicates death (3).
The EuroQol EQ-5D-3L is a questionnaire designed to measure a patient’s health status preferences (12). It consists of 5 dimensions: mobility, self-care, usual activities, pain, and anxiety. Each dimension has 3 levels: no problems, some problems, and extreme problems, coded from 1 to 3 (13). The EQ-5D-3L health states are represented by a sequence of 5 numbers that describe each level within each dimension. For example, 11111 indicates perfect health, while 33333 represents the worst possible health state. The system defines 243 possible health states, each of which can be supplemented using a scoring or weighting system to convert profile data into a single numerical value: the EQ-5D-3L values (14). These scoring systems are typically preference-based, meaning that the problems in each dimension are weighted to reflect public perception of their severity. The EQ-5D-3L index values are constructed on a scale anchored at 1, representing full health, and 0, representing death (14).
The EQ-5D-3L value set was selected from a previous study conducted in Chile, which evaluated the health status of the general population using the Time Trade-Off technique (15). Patients who died during follow-up (mRS = 6) were assigned an EQ-5D-3L value of 0 (zero).
Quantitative variables were reported as means (SD) or medians (IQR) depending on normality (using K-S test) and were compared according normal/ non-normal distribution using the T test or Mann–Whitney U test. Qualitative variables were reported as absolute and percentage prevalence and were compared using the χ2 test or Fisher’s exact test, as appropriate.
UW-mRS scores were calculated only for patients alive during follow-up using an ordinary least squares regression model, with mRS scores as discrete ordinal dummy variables and EQ-5D scores as the continuous response variable, adhering to the methodology established by prior studies (16). UW-mRS scores were obtained and validated separately for acute ischemic stroke, intracerebral hemorrhage, and by sex. A simple linear regression analysis was performed to identify variables associated with UW-mRS scores. Multivariable linear regression models were subsequently used to evaluate factors influencing UW-mRS, including both variables significantly correlated in the simple analysis and those considered clinically relevant. This included sex, age over 70, low socioeconomic status, urban residence, prior disability (mRS 3–5), stroke type, and an NIHSS score above 5 at admission. An alfa level of 5% (p < 0.05) was considered significant, and 95% confidence intervals were used. Data were processed using STATA software (version 18.5).
Of the 1,103 patients who experienced a stroke between 2015 and 2016, 890 were a first-ever stroke. At 180 days post the acute event, 773 patients were evaluated, with a 13% loss to follow-up. Baseline characteristics are summarized in Table 1. The cohort consisted of 398 (51%) females, with a mean age of 70.6 years (14.1). Nearly half of the patients (386, 49.9%) had less than 12 years of formal education, and 533 (82%) were classified as having low socioeconomic status based on their public health insurance classification (17). 536 (65%) patients experienced an AIS, had a median NIHSS score of 5 (IQR 3–11), and a median hospital stay of 9 days (IQR 4–15).
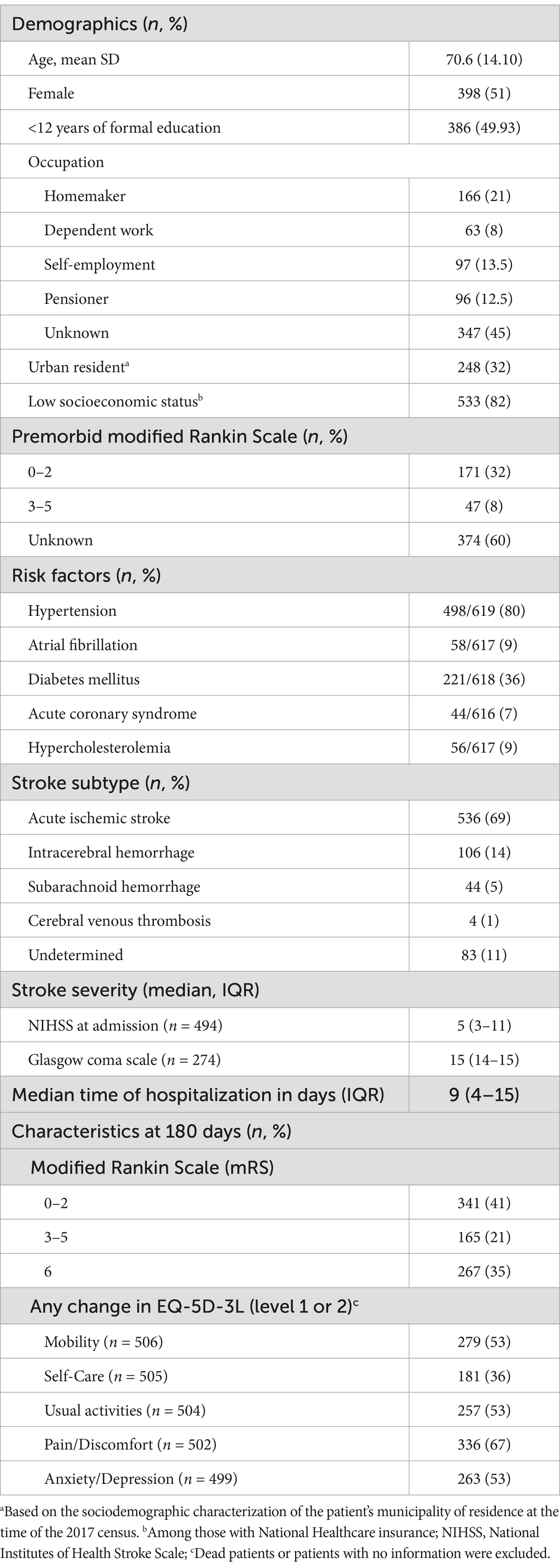
Table 1. Baseline characteristics of the 773 patients with first ever stroke (FES) followed at 180 days.
At 180 days post-acute event, 41% of patients had an mRS score of 0–2, 21% had a score of 3–5, and 35% had died (Table 1; Figure 1). Among patients with hemorrhagic stroke, 62% died, compared to 21% of those with an AIS (p < 0.001). No significant differences were observed in the distribution of mRS scores by sex (Supplementary Figures 1, 2).
In the EQ-5D-3L assessment, the most affected dimension was pain/discomfort (67%), followed by mobility and anxiety/depression (53%). Figure 2 shows the distribution of the EQ-5D-3L for each mRS category. There was a strong negative association between mRS and EQ-5D-3L index values overall (r = −0.82; p < 0.001; Supplementary Figure 3).
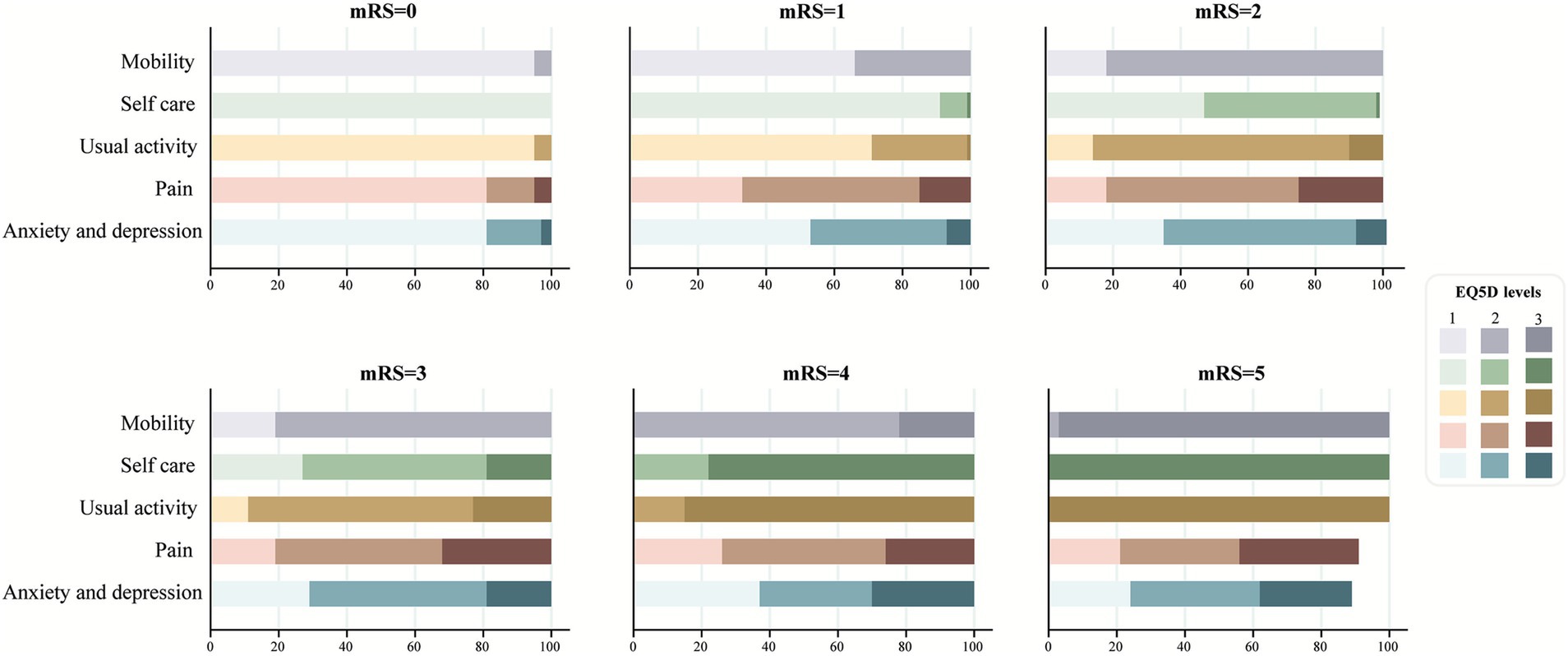
Figure 2. European quality of life 5-dimensional questionnaire utility scores by modified Rankin Scale scores at 180 days of follow up.
The UW-mRS values, calculated from the mean EQ-5D-3L utility scores from the Chilean population (15), across mRS categories 0–6 at 180 days, were: 0.913, 0.694, 0.425, 0.249, −0.102, −0.347 and 0, respectively (Table 2). When disaggregated by sex, females tended to have slightly lower UW-mRS values compared to males, though this difference was not statistically significant (p = 0.194, Figure 3a). In terms of stroke type, ischemic stroke survivors had lower UW-mRS scores than those with hemorrhagic stroke at 180 days post-acute event (Figure 3b).
A linear regression analysis was conducted to explore the relationship between UW-mRS scores and key variables. In the simple regression, significant associations were found between age > 70 years (Coefficient β [β] −0.007 [Standard error SE] 0.001, p < 0.001), lower socioeconomic status (β −0.075 [SE 0.040], p < 0.001), previous mRS score of 3–5 (β −0.607 [SE 0.018], p < 0.001), ischemic stroke subtype (β −0.025 [SE 0.041], p < 0.001), and NIHSS >5 at admission (β −0.273 [SE 0.028], p < 0.001) with worse outcome (Table 3). In the multivariable model, age > 70 years (β −0.038 [SE 0.018], p = 0.032), previous mRS score of 3–5 (β −0.556 [SE 0.197], p < 0.001), ischemic stroke (β −0.066 [SE 0.025] p = 0.010), and NIHSS >5 at admission (β −0.015 [SE 0.002], p < 0.001) remained significant predictors of lower UW-mRS scores, with an R2 of 70%. When the multivariable model was disaggregated by sex to assess potential differences, the previous mRS score of 3–5 and NIHSS >5 at admission were associated to worse UW-mRS in both sexes (Supplementary Table 1). Distinctly, age > 70 years was significant for males (β −0.069 [SE 0.024], p = 0.006) and having an AIS was significant for females (β −0.087 [SE 0.033], p = 0.010) (Figure 4; Supplementary Table 1). The model explained a similar proportion of variance in both groups, with an R2 of 69% for females and 72% for males (Supplementary Table 1).
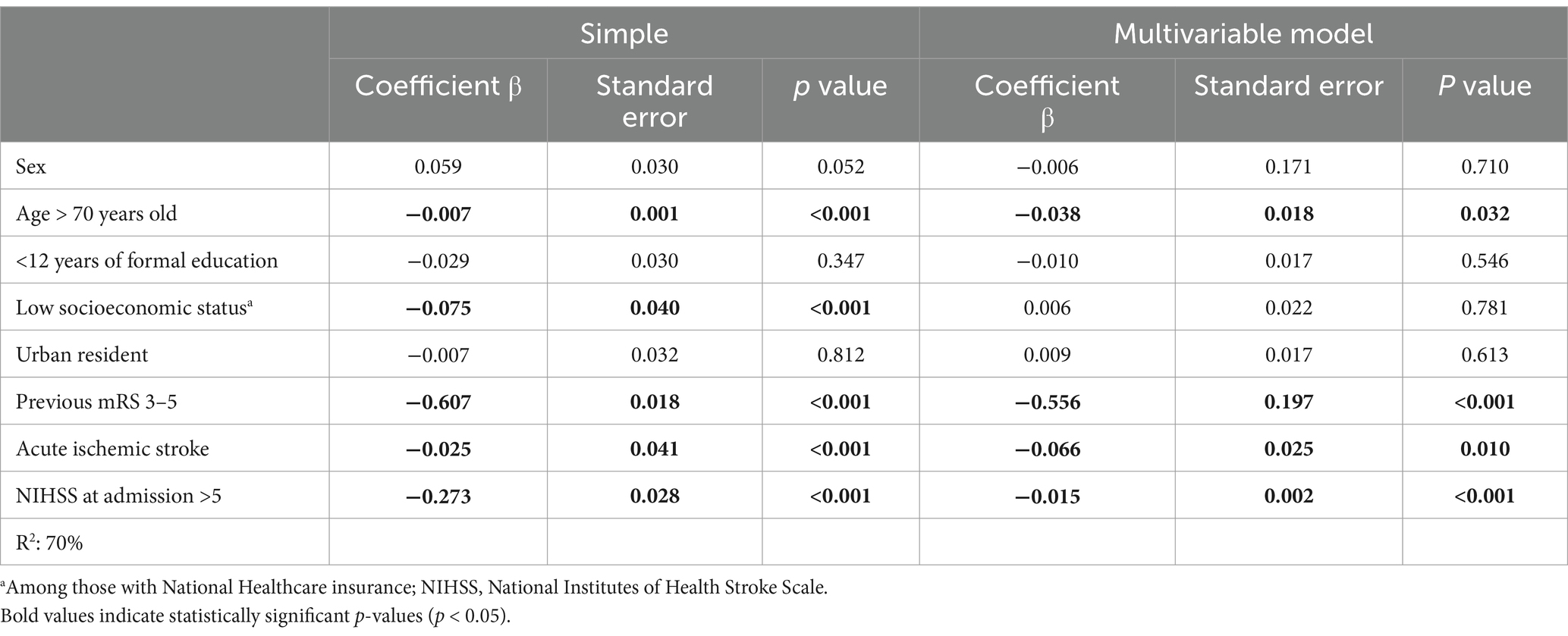
Table 3. Results of simple and multivariable linear regression models analyzing factors associated with UW-mRS scores.
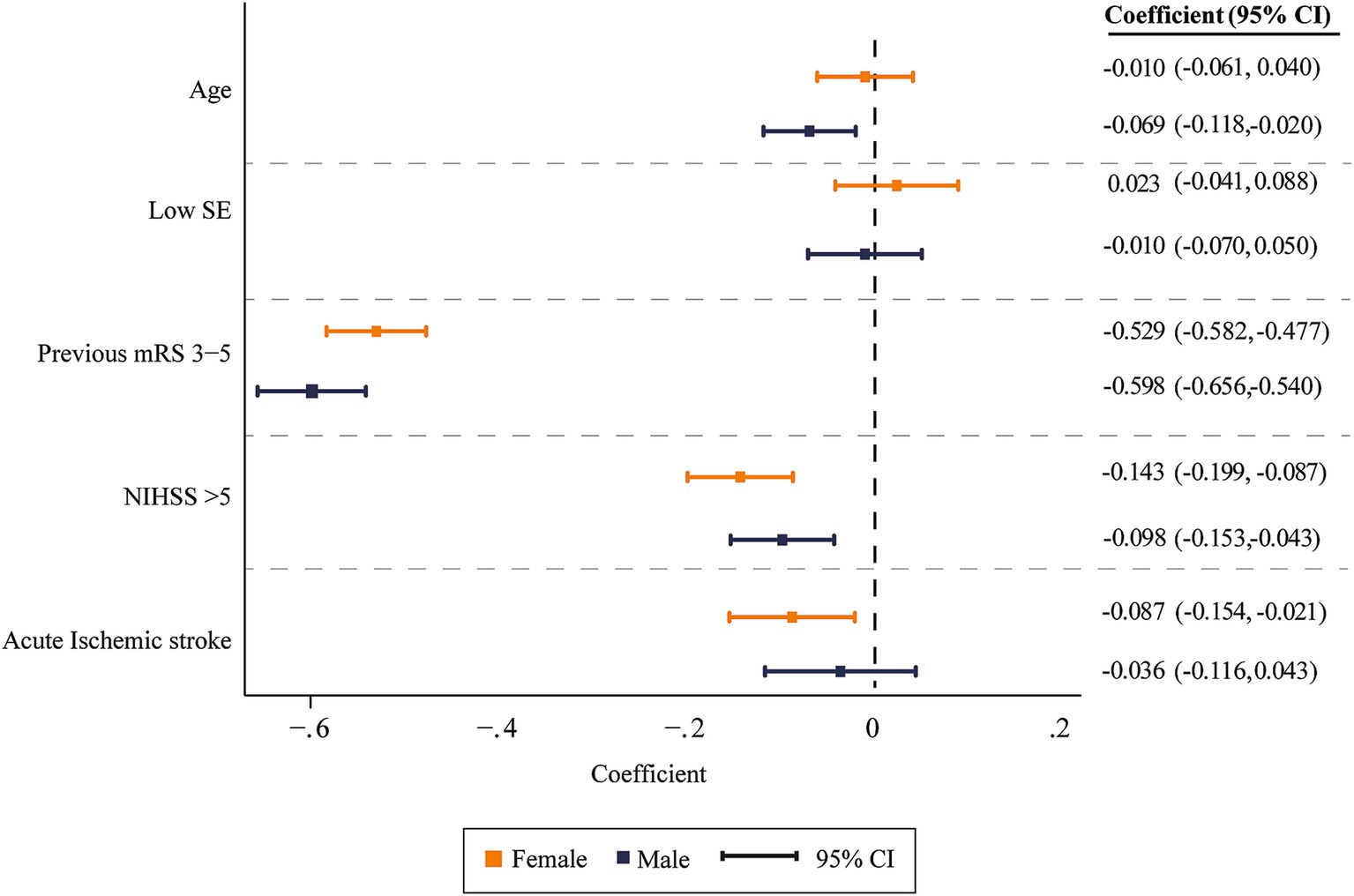
Figure 4. Multivariable model coefficients assessing risk factors by sex with 95% confidence intervals.
The present study examined the distribution of health outcomes in a Chilean population-based cohort of patients who suffered an acute stroke. To our knowledge, this study is the first to derive a quality-of-life scale, like the EQ-5D-3L, using the UW-mRS in a community-based study, incorporating the patient perspective outside of controlled clinical settings. At 180 days post-stroke, 35% of patients had died, and among the survivors, the most affected dimension of the EQ-5D-3L were pain/discomfort, followed by mobility and anxiety/depression. These results align with studies comparing healthy populations in other countries within the region (18) and in countries like China (19).
The UW-mRS values demonstrated a gradual decline in utility as mRS scores increased, reflecting the expected deterioration in health-related quality of life as disability worsened. These findings corroborate those of Wang et al., who applied similar methodologies based on cohorts from clinical trials (16). Their reported utility values for mRS scores 0–6 were 0.96, 0.88, 0.74, 0.56, 0.25, −0.11, and 0, respectively. Notably, the utility values for mRS 4 and 5 were significantly lower in the Chilean population, resulting in negative values, which suggest a more severe perception of quality of life at the same mRS level compared to Wang et al.’s cohort. This variation may be attributed to cultural differences in health perception, disparities in access to healthcare, or other socioeconomic factors (7, 14) as well as the methodological differences between studies that derived the EQ-5D-3L value sets (18, 20). These findings underscore the importance of using population-specific utility values when calculating UW-mRS scores, as the choice of value set can significantly influence results and their interpretation, with important implications for clinical practice and research.
When analyzing the UW-mRS scores by sex, females were found to report worse health status than males for the same level of motor disability, though the differences were not statistically significant. Previous studies indicate that, on average, females score 0.03 points lower than males (21). These discrepancies may be explained by the influence of distinct cultural and social factors that shape how females perceive and report their health status (22), as well as to higher levels of anxiety or depression, pain, and discomfort compared to males (23). Interestingly, age over 70 years emerged as a significant predictor of worse UW-mRS scores in males, which may be explained by the fact that, at the time of stroke, females were significantly older than males (mean age 72.17 vs. 68.94 years respectively). Additionally, ischemic stroke was a significant predictor of poorer outcomes in females. Although the proportion of ischemic stroke was similar between sexes, a higher percentage of females who suffered ischemic stroke (30%) had mRS scores between 3 and 5 compared to males (21%), and the higher UW-mRS weights for ischemic stroke may have further accentuated its impact on females.
When comparing UW-mRS scores by stroke type, we found that the values for ischemic stroke were lower than those for ICH, and this impact was more relevant in women. The difference may be attributed to the greater severity typically associated with ICH and the higher early mortality rate among ICH patients during follow-up.
This study has strengths and limitations that must be acknowledged. Among its strengths, we identified key predictors of UW-mRS scores in stroke survivors, including age, prior mRS score, and NIHSS at admission, which aligns with previous findings (24). Notably, age over 70 years emerged as a significant predictor only in males, while acute ischemic stroke had a greater impact on females. These sex-specific insights are crucial for tailoring personalized treatment and rehabilitation strategies. The use of a population-based cohort from a low-income setting adds to the relevance of the findings, providing valuable reference data for understanding stroke recovery in real-world conditions and informing future healthcare policies.
However, there are also important limitations. The data come from a single population-based cohort in Chile, which may limit the generalizability of the findings. Despite this, the results are representative of a low-income population with high stroke risk factors and could serve as a reference for future population-based studies. The follow-up was conducted by telephone, though studies have validated this method’s effectiveness (25), and it was carried out by trained personnel. Additionally, we lacked consistent information on access to rehabilitation or post-stroke care, which may have influenced the reported quality of life perceptions. Lastly, using the ordinary least squares regression model to derive UW-mRS scores may not fully capture the complexity of outcomes across stroke subtypes and demographics. Future research should explore alternative models and validate the UW-mRS in diverse populations.
These results present UW-mRS values derived from a population-based stroke study, further supporting UW-mRS as a reliable measure of PCOs in post-stroke patients. Key determinants of health-related quality of life included age, prior disability, and stroke severity, with age over 70 years being a significant predictor for males and AIS having a greater impact on females. Incorporating UW-mRS as a PCO in future stroke research and clinical practice may provide a more nuanced understanding of the impact of stroke on survivors, offering valuable insights for clinical decision-making and rehabilitation strategies across diverse healthcare settings.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by scientific ethics committee of the Universidad del Desarrollo, Clínica Alemana School of Medicine in Santiago. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
CD: Data curation, Formal analysis, Investigation, Methodology, Visualization, Writing – original draft. GC: Data curation, Formal analysis, Investigation, Methodology, Writing – review & editing. LH: Methodology, Supervision, Validation, Writing – review & editing. PL: Conceptualization, Project administration, Supervision, Writing – review & editing. PM: Conceptualization, Methodology, Project administration, Supervision, Validation, Visualization, Writing – review & editing.
The author(s) declare that no financial support was received for the research and/or publication of this article.
PMV receives research grants from ANID Fondecyt Regular N° 1221837 and a Research Grant from Pfizer 7688348. PL reports research support from Clínica Alemana and Boehringer Ingelheim. Research grants from Clínica Alemana de Santiago during the conduct of the study, personal fees from Boehringer Ingelheim, and a Chilean Government research grant (ANID) for the ÑANDU project.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2025.1539107/full#supplementary-material
1. Li, X, Kong, X, Yang, C, Cheng, ZF, Lv, JJ, Guo, H, et al. Global, regional, and national burden of ischemic stroke, 1990–2021: an analysis of data from the global burden of disease study 2021. eClinicalMedicine. (2024) 75:102758. doi: 10.1016/j.eclinm.2024.102758
2. Feigin, VL, Stark, BA, Johnson, CO, Roth, GA, Bisignano, C, Abady, GG, et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Neurol. (2021) 20:795–820. doi: 10.1016/S1474-4422(21)00252-0
3. Saver, JL, Chaisinanunkul, N, Campbell, BCV, Grotta, JC, Hill, MD, Khatri, P, et al. Standardized nomenclature for modified Rankin scale global disability outcomes: consensus recommendations from stroke therapy academic industry roundtable XI. Stroke. (2021) 52:3054–62. doi: 10.1161/STROKEAHA.121.034480
4. Dijkland, SA, Voormolen, DC, Venema, E, Roozenbeek, B, Polinder, S, Haagsma, JA, et al. Utility-weighted modified Rankin scale as primary outcome in stroke trials: a simulation study. Stroke. (2018) 49:965–71. doi: 10.1161/STROKEAHA.117.020194
5. The Optimising Analysis of Stroke Trials (OAST) Collaboration. Can we improve the statistical analysis of stroke trials?: statistical reanalysis of functional outcomes in stroke trials. Stroke. (2007) 38:1911–5. doi: 10.1161/STROKEAHA.106.474080
6. Beal, AC. The Patient-Centered Outcomes Research Institute (PCORI) National Priorities for research and initial research agenda. JAMA. (2012) 307:1583–4. doi: 10.1001/jama.2012.500
7. Rebchuk, AD, O’Neill, ZR, Szefer, EK, Hill, MD, and Field, TS. Health utility weighting of the modified Rankin scale: a systematic review and Meta-analysis. JAMA Netw Open. (2020) 3:e203767. doi: 10.1001/jamanetworkopen.2020.3767
8. Feeny, D. Response to Lenert and Kaplan: a utility approach to the assessment of health-related quality of life. Med Care. (2000) 38:II151–4. doi: 10.1097/00005650-200009002-00022
9. Rethnam, V, Bernhardt, J, Dewey, H, Moodie, M, Johns, H, Gao, L, et al. Utility-weighted modified Rankin scale: still too crude to be a truly patient-centric primary outcome measure? Int J Stroke. (2020) 15:268–77. doi: 10.1177/1747493019830583
10. Lavados, PM, Hoffmeister, L, Moraga, AM, Vejar, A, Vidal, C, Gajardo, C, et al. Incidence, risk factors, prognosis, and health-related quality of life after stroke in a low-resource community in Chile (ÑANDU): a prospective population-based study. Lancet Glob Health. (2021) 9:e340–51. doi: 10.1016/S2214-109X(20)30470-8
11. Quinn, TJ, Dawson, J, Walters, MR, and Lees, KR. Functional outcome measures in contemporary stroke trials. Int J Stroke. (2009) 4:200–5. doi: 10.1111/j.1747-4949.2009.00271.x
12. Rabin, R, and Charro, FD. EQ-SD: a measure of health status from the EuroQol group. Ann Med. (2001) 33:337–43. doi: 10.3109/07853890109002087
13. EuroQol. (2018) User guides. Available online at: https://euroqol.org/information-and-support/documentation/user-guides/ (Accessed July 1, 2024)
14. Devlin, N, Parkin, D, and Janssen, B. Methods for analysing and reporting EQ-5D data. Cham: Springer International Publishing (2020).
15. Zarate, V, Kind, P, Valenzuela, P, Vignau, A, Olivares-Tirado, P, and Munoz, A. Social valuation of EQ-5D health states: the Chilean case. Value Health. (2011) 14:1135–41. doi: 10.1016/j.jval.2011.09.002
16. Wang, X, Moullaali, TJ, Li, Q, Berge, E, Robinson, TG, Lindley, R, et al. Utility-weighted modified Rankin scale scores for the assessment of stroke outcome: pooled analysis of 20 000+ patients. Stroke. (2020) 51:2411–7. doi: 10.1161/STROKEAHA.119.028523
17. Beneficiarios Fonasa. (2024) Fonasa. Available at: https://nuevo.fonasa.gob.cl/tramos/ (Accessed March 10, 2025).
18. Tejada, RA, Gibbons, L, Belizán, M, Gutierrez, EL, Reyes, N, and Augustovski, FA. Comparison of EQ-5D values sets among South American countries. Value Health Regional Issues. (2021) 26:56–65. doi: 10.1016/j.vhri.2021.02.001
19. Mei, Y, Zhang, Z, Wu, H, Hou, J, Liu, XT, Sang, SX, et al. Health-related quality of life and its related factors in survivors of stroke in rural China: a large-scale cross-sectional study. Front Public Health. (2022) 10:810185. doi: 10.3389/fpubh.2022.810185
20. Xie, F, Gaebel, K, Perampaladas, K, Doble, B, and Pullenayegum, E. Comparing EQ-5D valuation studies: a systematic review and methodological reporting checklist. Med Decis Mak. (2014) 34:8–20. doi: 10.1177/0272989X13480852
21. Dolan, P, Gudex, C, Kind, P, and Williams, A. The time trade-off method: results from a general population study. Health Econ. (1996) 5:141–54. doi: 10.1002/(SICI)1099-1050(199603)5:2<141::AID-HEC189>3.0.CO;2-N
22. Lee, KH, Xu, H, and Wu, B. Gender differences in quality of life among community-dwelling older adults in low- and middle-income countries: results from the study on global AGEing and adult health (SAGE). BMC Public Health. (2020) 20:114. doi: 10.1186/s12889-020-8212-0
23. Joundi, RA, Adekanye, J, Leung, AA, Ronksley, P, Smith, EE, Rebchuk, AD, et al. Health state utility values in people with stroke: a systematic review and Meta-analysis. JAHA. (2022) 11:e024296. doi: 10.1161/JAHA.121.024296
24. Rost, NS, Bottle, A, Lee, J, Randall, M, Middleton, S, Shaw, L, et al. Stroke severity is a crucial predictor of outcome: an international prospective validation study. JAHA. (2016) 5:e002433. doi: 10.1161/JAHA.115.002433
Keywords: patient-centered outcomes, stroke, utility-weighted, modified Rankin Scale, community-based study
Citation: Delfino C, Cavada G, Hoffmeister L, Lavados P and Muñoz Venturelli P (2025) Patient centered outcomes in stroke: utility-weighted modified Rankin Scale results in a community-based study. Front. Neurol. 16:1539107. doi: 10.3389/fneur.2025.1539107
Received: 03 December 2024; Accepted: 04 March 2025;
Published: 21 March 2025.
Edited by:
Hrvoje Budincevic, University Hospital Sveti Duh, CroatiaReviewed by:
Stela Rutovic, Clinical Hospital Dubrava, CroatiaCopyright © 2025 Delfino, Cavada, Hoffmeister, Lavados and Muñoz Venturelli. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Paula Muñoz Venturelli, cGF1bXVub3pAdWRkLmNs
†Orcid: Carlos Delfino, https://orcid.org/0000-0002-4834-2718
Gabriel Cavada, https://orcid.org/0000-0002-3558-0266
Lorena Hoffmeister, https://orcid.org/0000-0002-5963-2876
Pablo Lavados, https://orcid.org/0000-0002-9118-9093
Paula Muñoz Venturelli, https://orcid.org/0000-0003-1869-2255
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.