
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol., 12 February 2025
Sec. Neurotrauma
Volume 16 - 2025 | https://doi.org/10.3389/fneur.2025.1469725
This article is part of the Research TopicPerioperative neurocognitive disordersView all 5 articles
Background: Delirium is a common manifestation of acute brain dysfunction among patients in the Intensive Care Unit (ICU), afflicting an estimated 30–35% of this vulnerable population. The prevalence of delirium in ICU settings has catalyzed a surge in academic interest, as evidenced by a growing body of literature on the subject. This study seeks to synthesize the progress in understanding ICU delirium through a bibliometric analysis.
Methods: We conducted a comprehensive search of the Web of Science Core (WOS) Collection database for literature on ICU delirium, focusing on studies published between 2013 and 2023. Our analysis utilized two bibliometric software tools, Citespace and VOSviewer, to scrutinize the data across various dimensions, including country contributions, authorship patterns, publishing journals, key thematic terms, and other pertinent metrics, with the aim of identifying emerging trends in the field.
Results: Our search yielded a total of 1,178 publications on ICU delirium within the WOS database from January 2013 to June 2023. The United States emerged as the leading contributor in terms of published articles, with Ely, E. Wesley being the most prolific author, having published 85 articles, and “Critical Care Medicine” as the journal with the highest number of publications, totaling 105. The application of literature clustering and keyword analysis revealed that future research is poised to delve deeper into areas such as pediatric delirium, risk factors, and the development of preventive and therapeutic strategies.
Conclusion: This study employs bibliometric analysis to provide a multifaceted overview of the ICU delirium research landscape over the past decade. By examining the topic from various perspectives, we have not only mapped the current state of ICU delirium research but also illuminated potential avenues for future inquiry and areas of emphasis.
Delirium, a brief condition of mental disorientation and cognitive impairment, is characterized by signs of inattention and disordered thought patterns (1). Delirium can be precipitated by factors, such as advanced age, cardiac surgery, history of depression or stroke, physical restraints, mechanical ventilation, and physiological internal environmental dysfunction (2, 3). It is prevalent in the ICU, and in extreme cases, it can be fatal (4). Due to a number of risk factors that are present in critically sick patients, the incidence rate of delirium in the ICU ranges from 45 to 87% (5–8). There is evidence suggesting that delirium in the ICU is associated with prolonged hospital stays, increased hospitalization costs, and higher rates of morbidity and mortality (9–14). However, the rate of missed diagnosis of delirium in clinical practice remains as high as 55% ~ 60% (1), and no effective drug has been available to prevent and treat ICU delirium.
This essay aims to explore the representation of delirium in the ICU over the last ten years utilizing Citespace and VOSviewer software, to examine the impact, hotspots, and trends of relevant literature. Citespace, a free JAVA application developed by Professor Chaomei Chen in 2004, provides bibliometric analysis and visualization (15). VOS is another software program developed specifically for scientific mapping and bibliometric visualization (16). By employing these tools, researchers are able to effortlessly review the literature and quickly locate relevant publications (17). This not only aids in understanding the current trends and patterns within the research on ICU delirium but also facilitates the effective utilization of classic articles in future investigative efforts.
An investigation was conducted on the WOS database using the search term “delirium” AND (“intensive care unit” OR “ICU”). The search parameters were set as follows: the literature type was limited to “article,” the language was restricted to English, the time frame was from January 2013 to June 2023, and the index was specified as the Science Citation Index Expanded (SCI-E) within the Web of Science Core Collection. This collection encompasses a broad spectrum of high-quality scholarly literature and can serve as a more authoritative and representative data source. During the search process, we initially excluded documents irrelevant to the research topic. Subsequently, professional document management software (such as EndNote) was utilized to eliminate duplicate document records, ensuring that each document was counted only once in the analysis to guarantee data accuracy and reliability. In total, 1,178 articles were identified and included in the analysis. For further analysis, the final records were downloaded in.txt format and imported into visualization and bibliometric tools. The institution ranking was provided by Scimago Institutions Rankings (https://www.scimagoir.com/rankings.php), while the H-index for countries/regions was furnished by Scimago Journal and Country Rank (https://www.scimagojr.com/journalrank.php). The H-index represents the highest number of papers (H) that have been cited at least H times.
Bibliometric analysis was conducted using CiteSpace (https://citespace.podia.com/), covering aspects such as country, institution, author, keyword, category, reference, and journal. Time slicing (2013–2023), node types, and selection criteria (top 50 levels of most-cited or frequently occurring items) were included in the parameter settings.
CiteSpace generates knowledge maps composed of linkages and nodes. On these maps, the size of a node represents the quantity of articles, and the citation rings on the nodes denote the publication years. The degree of collaboration among nodes is manifested by the strength of the connections between them (18). The presence of red rings around a node signifies its high inter-node centrality and robust citation burstiness, and a node exhibiting both strong centrality and burstiness will yield a high sigma score (19). Keyword and author co-occurrences were visualized using VOSviewer software (version 1.6.18; https://www.vosviewer.com/). It distinguishes between research disciplines and themes using distinct colors and node sizes, making visual analysis of interdisciplinary research more intuitive and effective. In the co-occurrence map, larger nodes imply a higher frequency co-occurrence of the item. Origin 8.0 software was used to analyze the published data.
The evolution of ICU delirium-related literature papers in the WOS database from January 2013 to June 2023 is depicted in Figure 1. The results clearly demonstrate that the number of publications related to ICU delirium exhibits a steady increasing trend year by year. Significantly more publications emerged in 2021 compared to any other year, indicating the heightened level of research activity in this subject during that period. However, the figure also reveals that the number of publications dropped dramatically in 2019. The primary reason for this outcome might be that the COVID-19 pandemic hampered the research efforts, such as the cancelation or postponement of international academic conferences and the interruption of research projects. By analyzing the disparities in column height across years, we can visually assess the increasing or decreasing trend of research enthusiasm in this subject. This provides us with a reference for predicting the future direction of research.
Utilizing the VOSviewer software, we analyzed the authors and generated the author collaboration graph (Figure 2). Each node in the graph represents a different author. Τhe size of the nodes indicates the number of publications, and the proximity of the nodes indicates the degree of collaboration. Furthermore, the thickness of the connecting lines indicates the level of cooperation. According to the node size analysis, it is evident that Ely, E. Wesley is the author with the most publications (n = 85) and citations (6763). He also had a close cooperation with other authors. Meanwhile, the map shows that there are more than ten groups focus on ICU delirium, and the authors cooperated with each other both within and between groups. The top ten authors by the quantity of publications are listed in Table 1. Ely, E. Wesley, the most prolific author, has partnered with multidisciplinary experts from the ICU, psychology, and nursing to present a complete analysis of delirium in the ICU from different perspectives. In addition to helping international health organizations recognize the significance of ICU delirium, their work has aided in the creation and use of more precise and trustworthy diagnostic instruments, such as the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) (20). Ely, E. Wesley is dedicated to teaching and training healthcare professionals to identify and manage ICU delirium in order to improve clinical care and patients’ prognosis (21). Additionally, their research has provided the scientific foundation for the development of guidelines for the prevention and treatment of ICU delirium, which have been adopted globally.
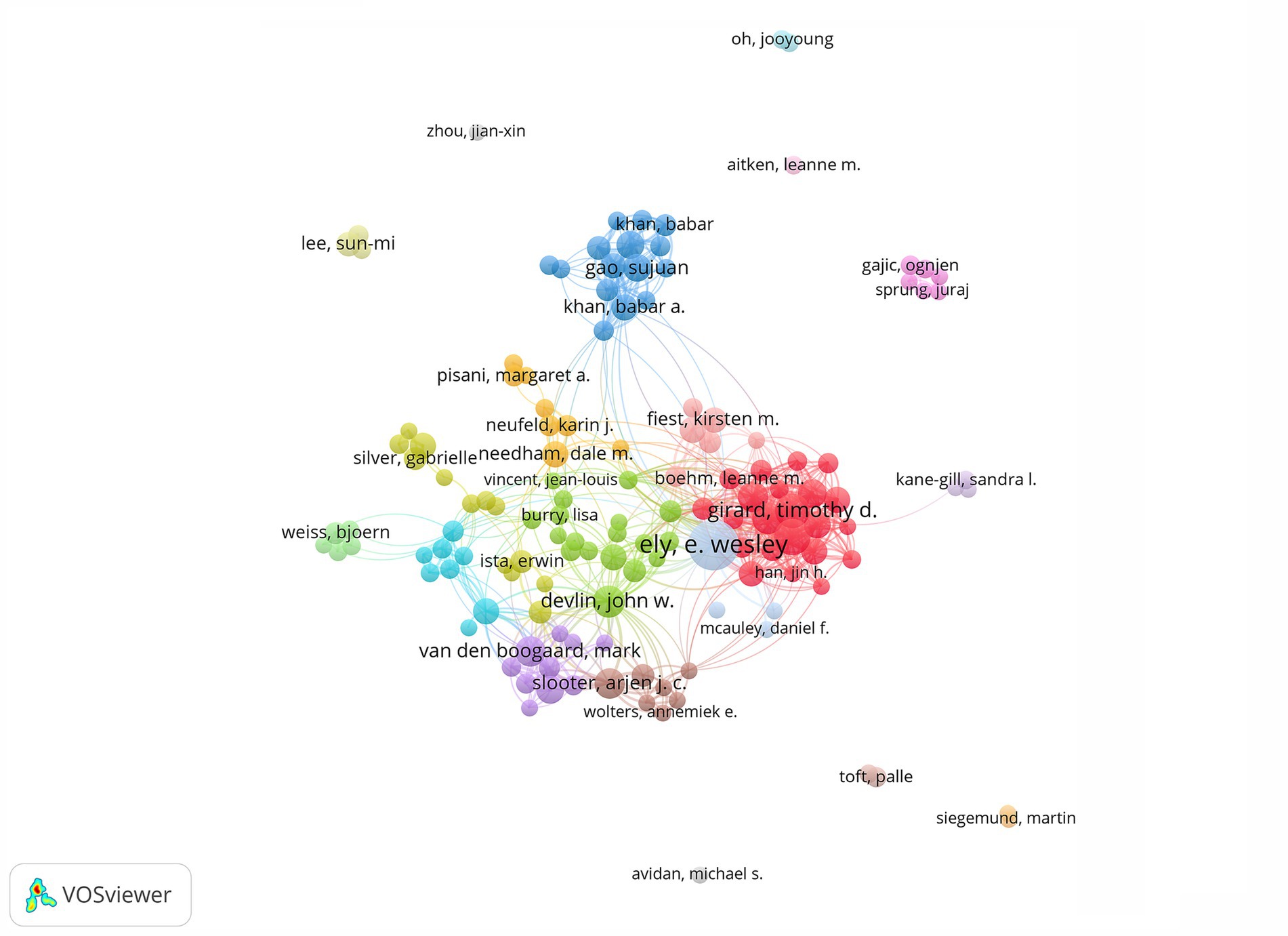
Figure 2. Visual map showing collaborations among authors. Each node symbolizes an individual author. The node’s size is scaled to reflect the volume of their published works, with larger nodes indicating a more prolific publication record. The connecting lines between nodes denote collaborative relationships, illustrating the interdisciplinary and cooperative nature of the research community.
There are 465 connecting lines that show the cooperative relationship between nations, and 66 nodes that represent 66 countries, with the United States, China, and Canada being the top three countries circled in red (Figure 3). This illustrates the dominance of developed nations in the field of international collaboration. The close ties across nations highlight the prevalence of ICU delirium. The red node of China indicates that the publications have a citation or frequency outbreak. In recent years, ICU delirium has received more attention in China, with extensive research on neurobiological mechanisms, treatments, etc.
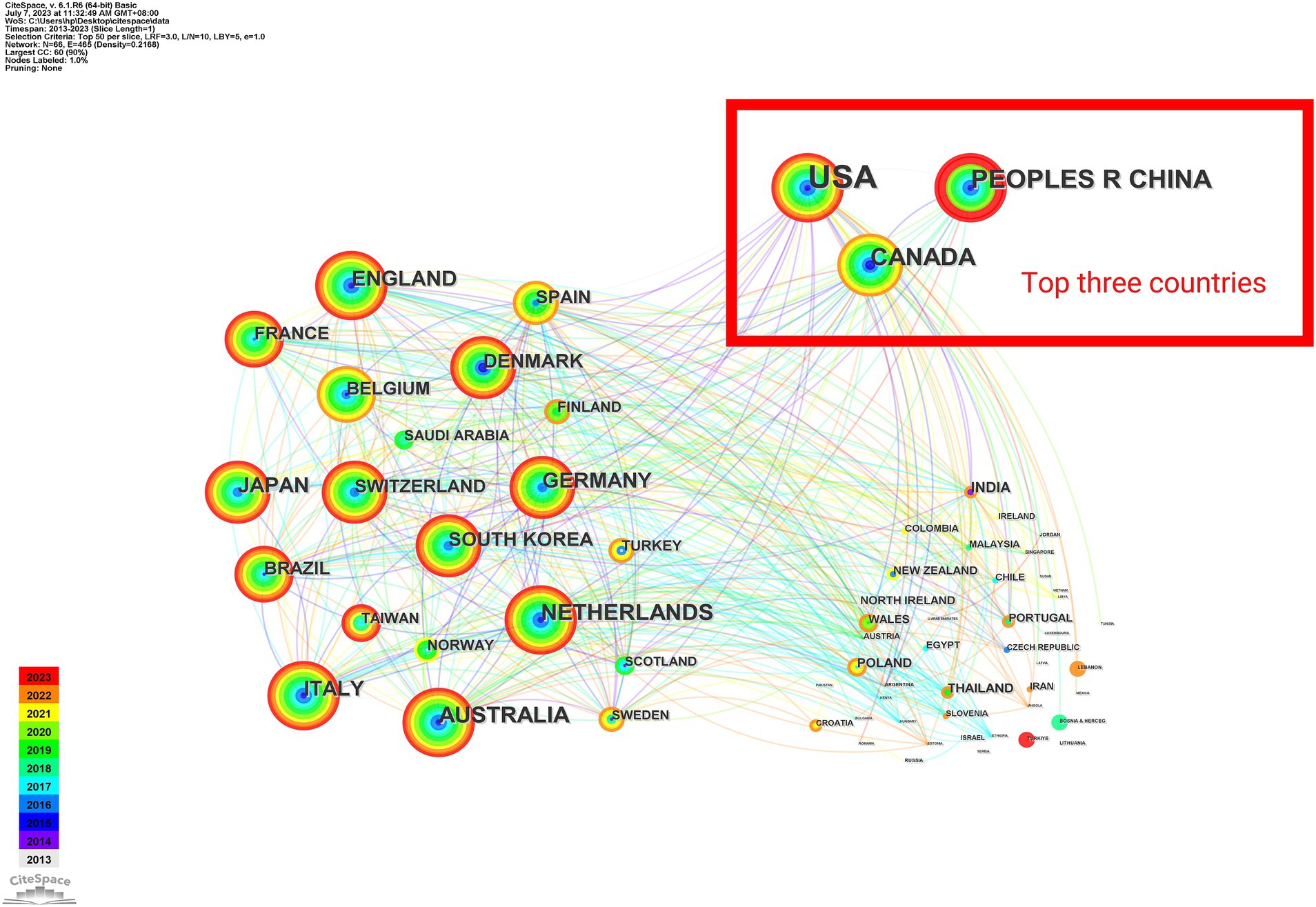
Figure 3. Map of country cooperation networks. Each node corresponds to a country. The size of the node is directly proportional to the quantity of scholarly documents published by that country, with larger nodes signifying a more extensive publication output. The lines interconnecting these nodes signify collaborative efforts, highlighting the interconnectedness and cooperative endeavors among nations in the realm of academic research.
Furthermore, 382 institutions published articles on this subject (Figure 4). Vanderbilt University is one of the institutions with the highest number of relevant articles published (121 in total), and the results cover a wide range of aspects such as the pathogenesis of delirium, diagnostic methods, preventive strategies, and therapeutic measures, and has a high number of citations (9885) (Table 2). This indicates that Vanderbilt University’s research in this field has been widely noticed and recognized, and has made significant contributions to the advancement of ICU delirium research.
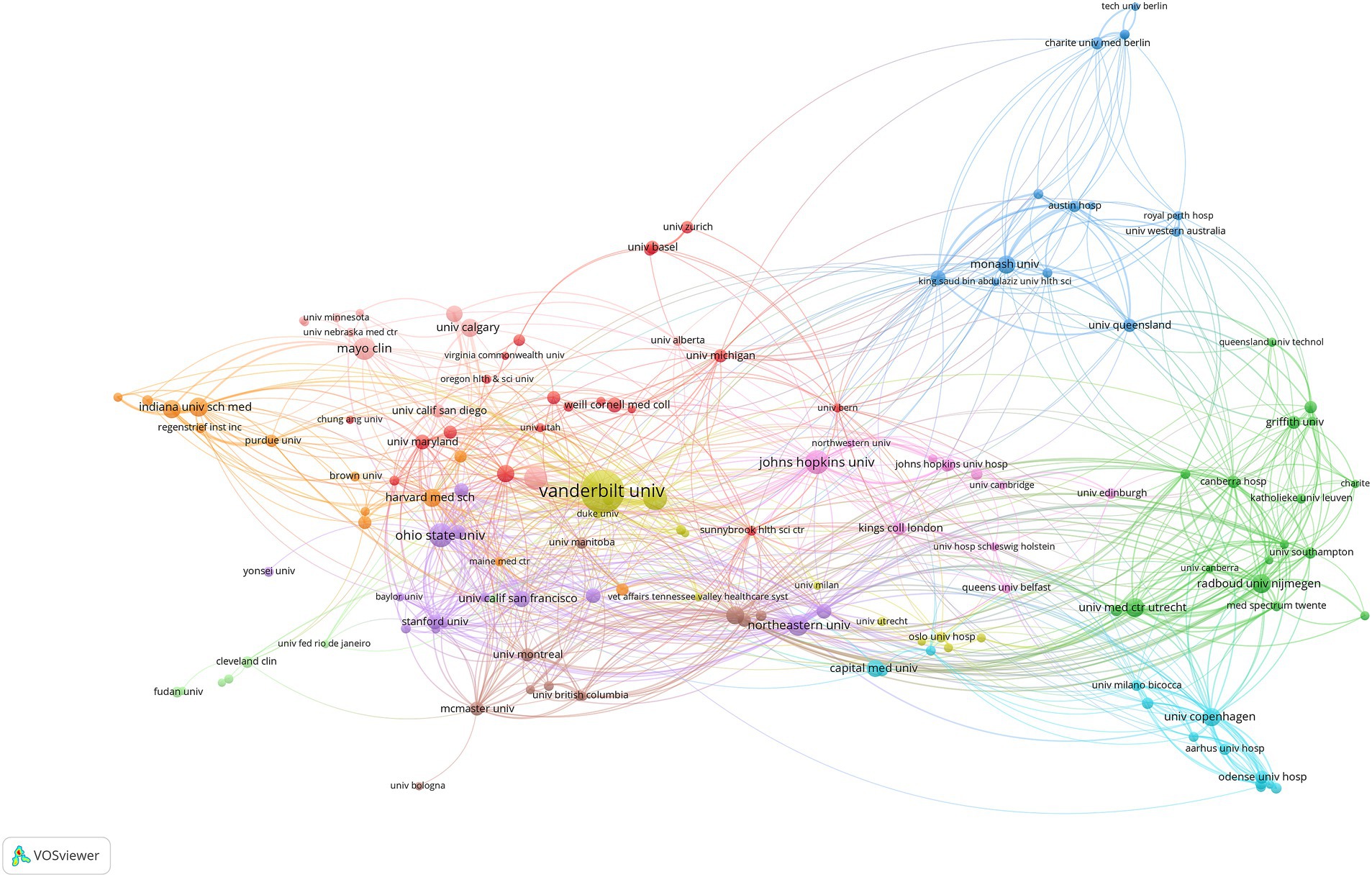
Figure 4. Collaborative map of institutions with publications >5. Each node embodies an institution, with its size indicative of the institution’s publication output—the larger the node, the more prolific the institution. The connections between nodes symbolize the co-authorship relationships, reflecting the collaborative efforts between the respective institutions.
The top 10 journals published between January 2013 and June 2023 are listed in Table 3, including the country of the journal, the number of articles, and the H-index. Five of them are from the US, four from the United Kingdom, and one from the Netherlands. The distribution of journals shows the impact of research in the field in different countries and regions, while the H-index also reflects the scholarly impact and quality of journals. Critical Care Medicine (n = 105) is the journal with the most publications and the highest citation frequency, and it has a high H-index. The premier journal in critical care medicine, Critical Care Medicine Journal, encompasses every aspect of acute and emergency care for patients who are acutely ill or injured. Journal of Critical Care, the second most prolific journal, focuses more on practical aspects of critical care, including clinical care delivery, nursing in critical care, and the improvement of quality of care in critical care units. Articles in these high-impact journals often represent cutting-edge research results and important research directions in the field, and can provide researchers with more valuable information. By analyzing the publication trends of journals, researchers can identify the hotspots of journals, adjust research direction and content, and improve the success rate of submissions.
Keywords can be utilized in bibliometrics to reflect research trends and hotspots in the field (22). Using VOSviewer, 143 terms with a frequency of at least five times were displayed. Each node in Figure 5 represents a distinct keyword, and the size of the node indicates how frequently the keyword occurs over time. The larger the node, the more frequently the keyword occurs, suggesting that the keyword is related to the research topic in the area that is receiving the most attention and could potentially be the hot spot direction of the study. The co-occurrence frequency of the keywords is the frequency of simultaneous appearance in the same literature. It is indicated by the line connecting the nodes, and the thicker the line, the stronger the association between the two keywords. The highly important terms were divided into 11 clusters, each denoted by a distinct color. “Delirium” is the biggest node, and terms like “antipsychotic agents,” “polypharmacy,” and “quetiapine” are linked to it. This implies a connection between the onset of delirium and the usage of various antipsychotics. The term “mechanical ventilation” is shown next to “intensive care unit,” suggesting that the use of mechanical ventilation increases the likelihood of developing delirium (23–25).
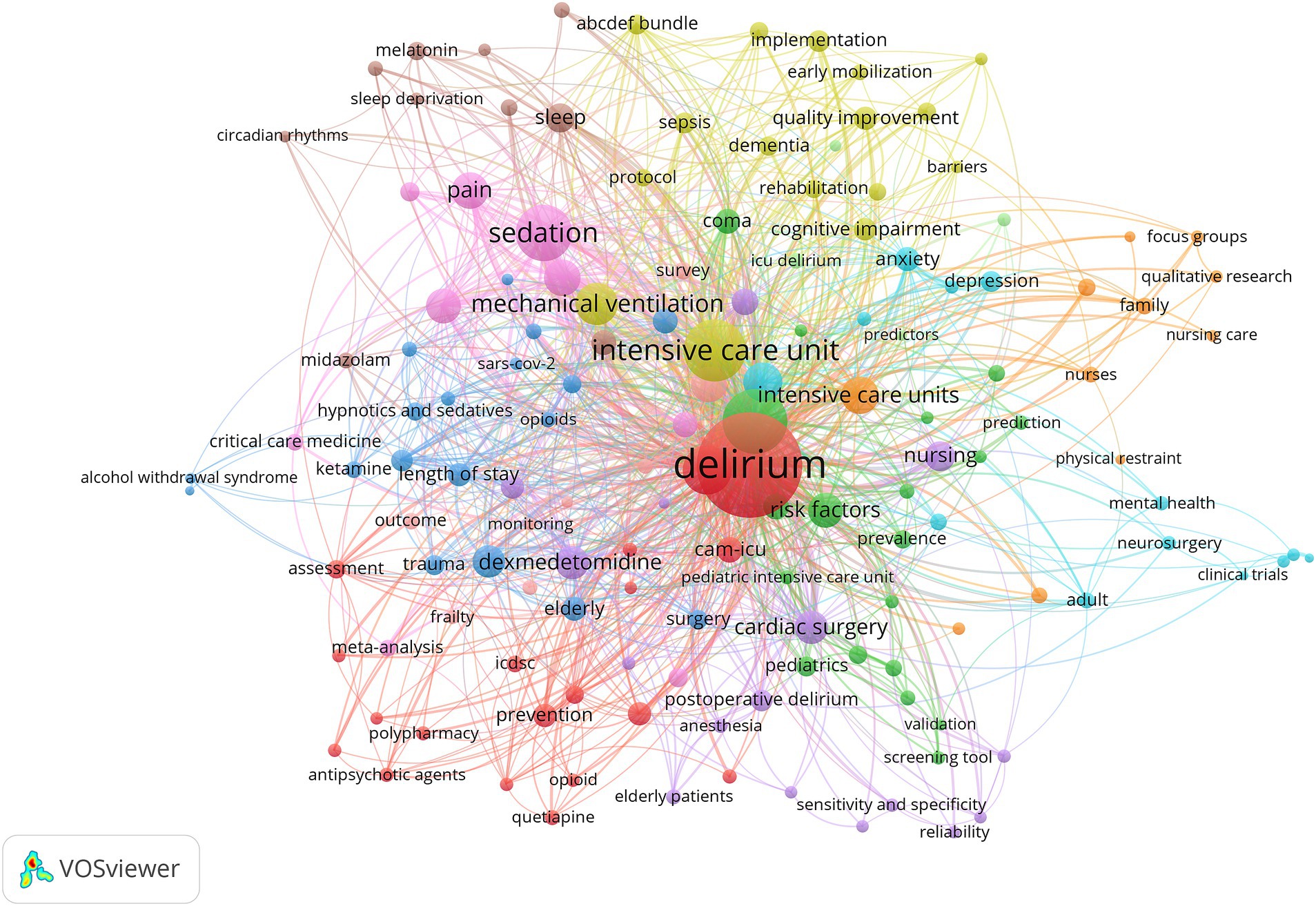
Figure 5. Co-occurrence network diagram of keywords that appear more than five times. Each node corresponds to a specific keyword, with its size reflecting the keyword’s frequency across various time periods. The links connecting these nodes signify the co-occurrence frequency of the associated keywords, indicating how often they appear together in publications.
Furthermore this study also applied CiteSpace to mutate keywords in the selected 1178 articles and obtained 25 mutated keywords as shown in Figure 6. They are principally classified as follows: research methodology (randomized controlled trial; protocol; controlled trial; model; guidelines), custodial ward (ICU; neurocritical care; pediatric intensive care unit), predisposing factor (mechanically ventilated patient; acute lung injury; hip fracture; ICU delirium; surgery; pain; delirium and cognitive disorder; dementia; disease; ill patient), prognosis and rehabilitation (lorazepam; daily interruption; physical rehabilitation; rehabilitation; survival; prevention; nurse). Burst keywords are words frequently cited over time which can reflect research trends (26). Figure 6 shows the entire period in blue with the citation burst duration in red. The most intensively cited keywords were randomized controlled trial (strength 6.78 time span 2013-2017) prevention (strength 6.65 time span 2020-2023) guideline (strength 6.45 time span 2019-2023) mechanically ventilated patient (strength 5.03 time span 2013-2014) acute lung injury (strength 5 time span 2013-2015). Early researchers used a large number of randomized controlled trials to test hypotheses and interventions laying the foundation for subsequent research. During the period from 2013 to 2015 “mechanically ventilated patients” and “acute lung injury” were the keywords with high citation intensity indicating that the research focus at that time was on the complications closely related to ICU delirium. In recent years researchers have taken a multi-pronged approach to preventing delirium by following a guiding route that involves early identification of risk factors optimization of treatment regimens and enhancement of healthcare training. In the future researchers can delve deeper into the complex network of interactions between risk factors develop more accurate risk prediction models and further explore the research areas represented by each keyword appearing in the "citation burst" during the research progress.
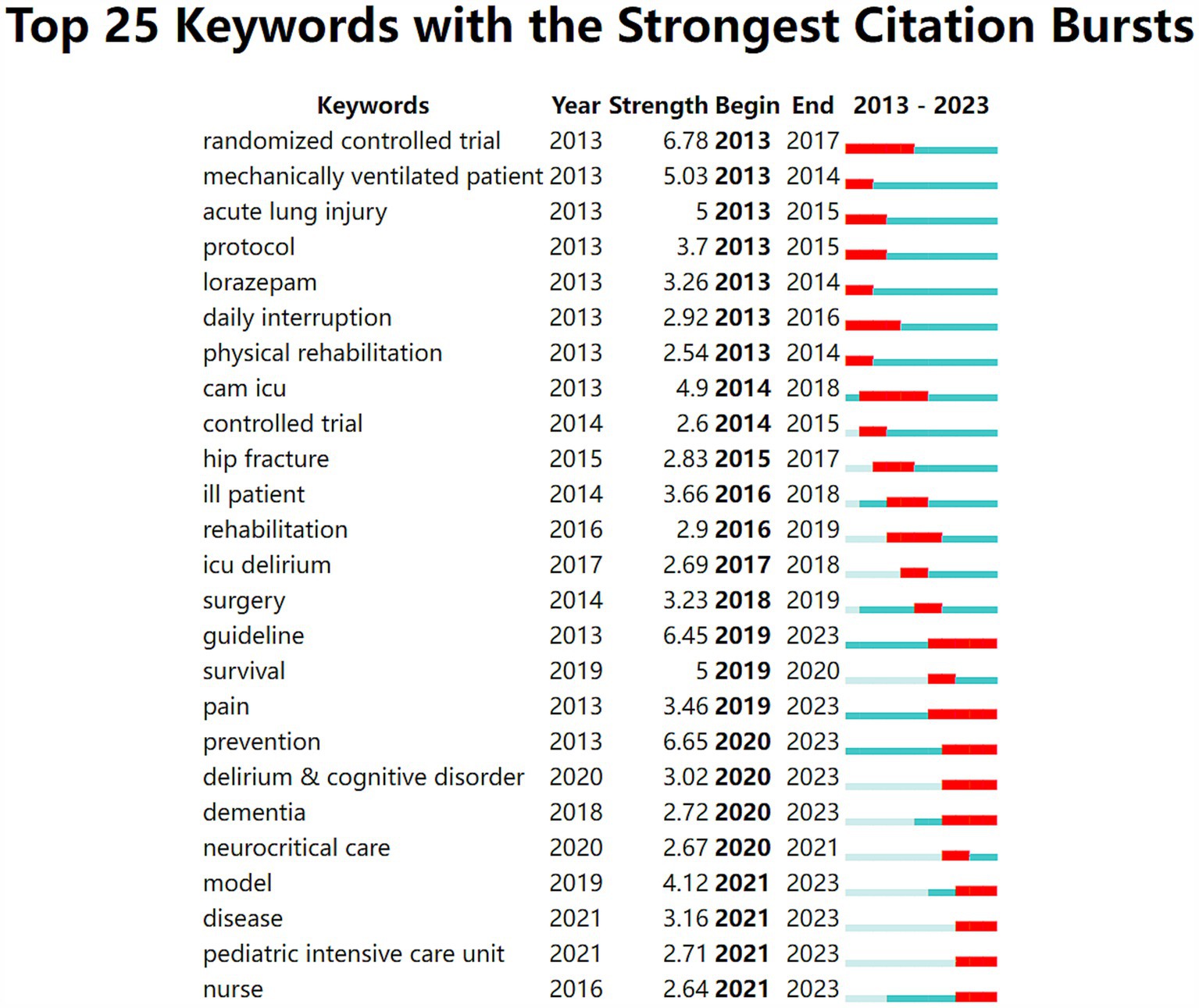
Figure 6. The blue line delineates the comprehensive timeline of the publication period under review, spanning from 2013 to 2023. The red line highlights a particular time frame associated with a burst word, which has experienced a significant surge in usage during a specific interval.
The term “co-cited references” refers to references that have been cited by more than one article. VOSviewer software was used to map the network among document references (Figure 7). A total of 253 documents had more than 20 citations. Larger nodes such as “Ely EW, 2004, Jama-j”, “Barr J, 2013, crit c”, and “Ely EW, 2001, Jama-j” belong to the key references in the field, and those with strong correlation are in the same color category. Based on the observation and data analysis of numerous ICU patients, it was discovered that delirium not only lengthens the time that patients require mechanical ventilation but also considerably raises their death rate (Ely Ew, 2004, Jama-j). This finding prompted clinicians to pay close attention to ICU delirium, and numerous studies began to concentrate on this subject in an effort to identify effective interventions, such as early rehabilitation exercises and optimization of the sedation strategy, to lower the incidence of delirium, thereby shortening the duration of mechanical ventilation and reducing the risk of patient death.
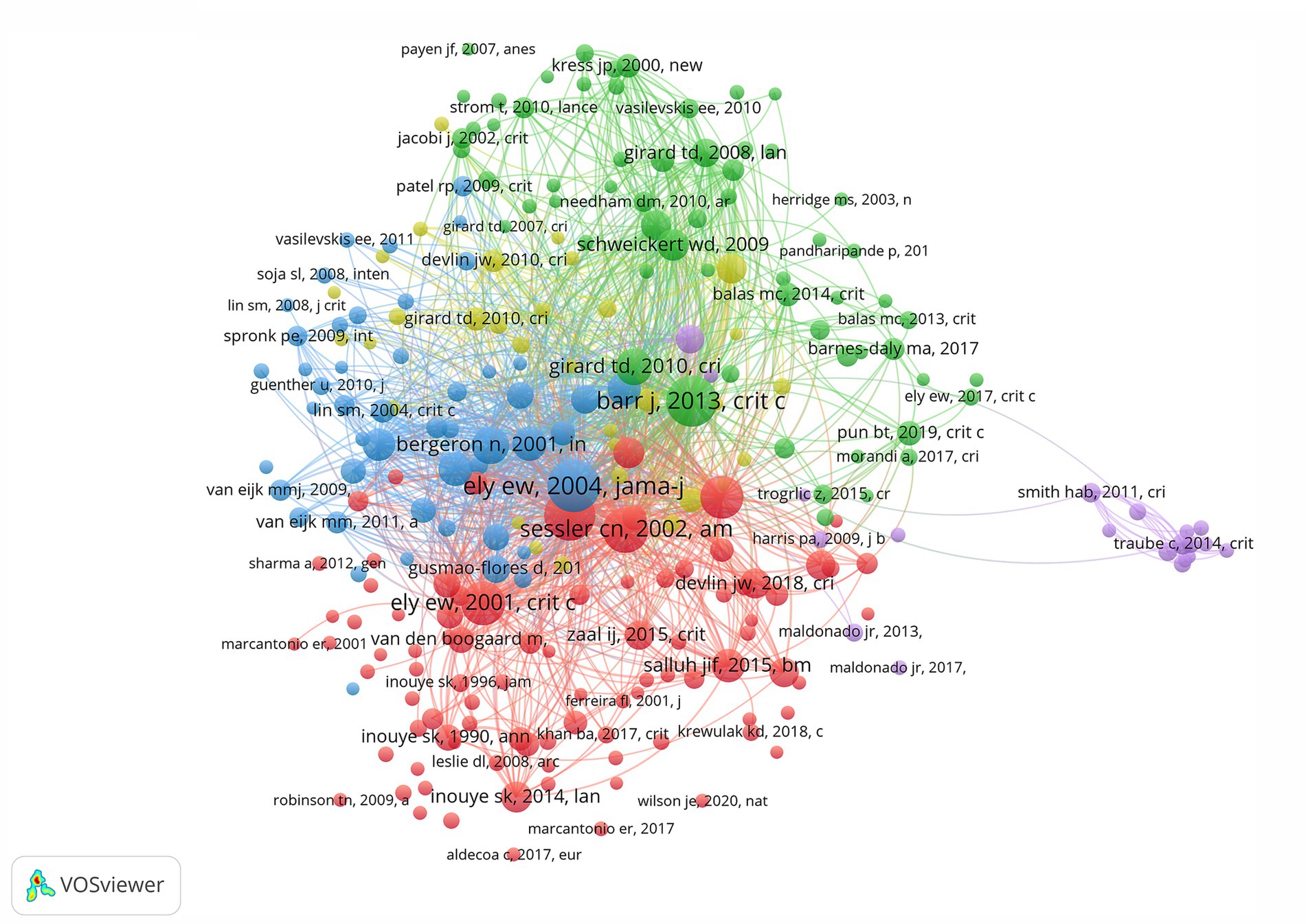
Figure 7. Co-citation analysis network diagram for references with more than 50 citations. The size of each node is proportional to the frequency of citations it has received. Larger nodes indicate that the associated research has garnered a higher number of citations. The connections between nodes illustrate the citation relationships, mapping out the academic lineage and scholarly influence among various studies.
In addition, 1,176 documents from the database were clustered using Citespace software to extract the noun terms in the titles of the documents, and to draw a time plot of the clusters according to the time and the size of the clusters. Finally, eleven clusters were obtained (Figure 8), including cluster 0 (circular rhythm), cluster 1 (risk factor), cluster 2 (critical illness), cluster 3 (double-blind placebo-controlled trial), cluster 4 (pain agitation), cluster 5 (ABCDEF bundle), cluster 6 (pediatric delirium), cluster 7 (cardiac surgery), cluster 8 (alcoholic withdrawal syndrome), cluster 9 (delirium knowledge), and cluster 10 (post-intensive care syndrome). It can also be seen that clusters 2 and 6 are still undergoing continuous evolution.

Figure 8. Time map of the best 11 co-cited network clusters in the ICU delirium references. Each cluster captures the research hotspots of a particular era, as delineated by the timeline.
According to the WOS database, a total of 1,176 publications about ICU delirium were published between 2013 and June 2023. Except for 2019, the number of publications showed an upward trend each year, with the highest number in 2021, indicating a growing interest in ICU delirium among scientists. Ely, E. Wesley, the scientist with the most publications, has focused his research on developing better treatments and improving outcomes for critically ill patients with ICU-acquired encephalopathies. This not only advances the understanding of ICU delirium but also reflects its dynamic nature. The United States is the nation with the most publications and also has the most journals and organizations, demonstrating its strong scientific foundation. In terms of journals, scientists might consider Critical Care Medicine as their target because it has the greatest number of published articles and a comparatively high H-index. To comprehend ICU delirium and guide future research, we have broadly grouped ICU delirium into several categories, including risk factors, clinical presentation, diagnosis, prevention and treatment, based on emerging keywords and literature clustering.
Up to 80% of individuals in the ICU experience delirium, which typically manifests as neurologic impairment (3, 11). There are two types of risk factors for delirium in the ICU: susceptibility factors and precipitating factors. The susceptibility factors of ICU delirium include: (1) older adults (aged 65 and older) (27–30), (2) Pre-existing neurological disorders (such as dementia, cognitive impairment, depression, etc.) (31–34), (3) cancer (35), (4) patients undergoing major surgery, (5) multiple comorbidities (electrolyte disorders, severe hypoproteinemia, etc.) (36, 37), (6) drug and tobacco withdrawal (28), (7) sensory impairments (e.g., vision, hearing), and functional impairments (i.e., reduced activities of daily living) (38–40). Exposure of patients with susceptibility factors to precipitating factors will lead to the development of delirium. The following are the precipitating factors for the ICU delirium: (1) Drug use: anticholinergics (41), opioids (42), benzodiazepines (38, 43), psychoactive drugs (28). (2) Surgery: hip surgery in the elderly (44), prolonged extracorporeal circulation in cardiovascular surgery (45), (3) Environment: mechanical ventilation (20, 42), physical restraints, catheters, and various drains (3, 46), circadian rhythm (47), (4) Comorbidities: infections, multiorgan failure following surgery (48), anemia, malnutrition, etc. (49). Within the clinical setting, healthcare professionals ought to evaluate the delirium risk of patients more thoroughly. To lower the incidence of delirium, preventive measures should be taken beforehand and surveillance need to be enhanced for patients with risk factors.
Delirium typically occurs one or two days after the patient is admitted to ICU and lasts for an average of three days before improvement (20, 42, 50–53). Depending on the activity level during the episode, delirium can be categorized as hyperactive, hypoactive, or mixed delirium (54). Hyperactive delirium is characterized by restlessness, irritability, excitement, increased volume, hallucinations, etc., which is easy to detect. Clinically, such patients may be at an increased risk of self-injury and present a significant challenge to caregivers. Reduced activity, such as drowsiness, silence, lowered level of awareness and reduced spoken exchange, is a hallmark of hypoactive delirium, which is commonly seen in the elderly. Since hypoactive delirium is difficult to identify (1, 55), it may lead to a higher incidence of complications, such as lung infections and thrombosis. Mixed delirium may exhibit alternating features of hyperactive and hypoactive delirium within a brief period. These symptoms change with the course of the disease. In the ICU, hypoactive and mixed delirium account for more than 90% of patients (7, 56). Therefore, improving the ability of healthcare professionals to recognize delirium is crucial.
Timely detection, early diagnosis and treatment of delirium are critical to improving patient outcomes (57, 58). Diagnostic and Statistical Manual of Mental Disorders (DSM-5) is considered as the gold standard of diagnosis of delirium (54). The features of DSM-5 include: (1) Deficits in awareness and attention are characterized by a decline in orientation to the surroundings and a reduction in the capacity to focus, direct, sustain, and shift focus; (2) Attention and consciousness deficits that progress over hours or days, with fluctuating manifestations of the condition; (3) Being accompanied by cognitive deficits in memory, orientation, language, visuospatial awareness, or sensorimotor perception; (4) Not being able to be explained by other pre-existing neurologic cognitive deficits; and (5) evidence associated with the onset of delirium, such as drug intoxication or withdrawal, exposure to toxins, etc. Other possible symptoms include altered arousal, disorientation, confusion, improper words or behavior, disrupted circadian rhythm, psychomotor abnormalities and hallucinations.
Even though the DSM-5 is the most reliable tool for delirium diagnosis, its implementation requires high professional standards and is time-consuming and laborious, making its application in clinical work challenging. There are numerous patients in critical, complex, and rapidly evolving condition. Therefore, additional delirium assessment instruments have been developed in clinical practice, taking into account the unique characteristics of ICU patients, such as CAM-ICU, Intensive Care Delirium Screening Checklist (ICDSC), Nurses’ Delirium Screening Scale (Nu-DESC), Confusion, Tolerance, and Delirium (CTD), Nursing Evaluation of Elderly Comatose or Handicapped Mental state (NEECHAM), and Delirium Detection Score (DDS) (3, 59, 60). Among them, Confusion Assessment Method (CAM) is the most widely used, which has four clinical features: (1) acute change and a varying path; (2) inattentiveness; (3) disorganized thinking; and (4) altered awareness. If one of features 3 or 4 as well as criteria 1 and 2 are met, delirium can be diagnosed (61). CAM-ICU as well as 3D-CAM are further optimizations of CAM, which have a high degree of utility, sensitivity, and specificity (62). CAM-ICU can be used in patients who are using a mechanical ventilation system and unable to speak (57). The ICDSC consists of eight items (63), which examine altered awareness, inattention, psychomotor agitation or retardation, hallucinations, delusions or psychosis, inappropriate speech or mood, sleep–wake/cycle disruptions, and symptom fluctuations. The sensitivity and specificity of various assessment instruments vary. Although the CAM-ICU and ICDSC are the most precise and trustworthy evaluation instruments for delirium in adult ICU patients, a suitable one should be chosen based on patients’ unique circumstances and hospitals’ actual settings (64–74).
Early detection of delirium is critical to preventing its onset (75), and the cornerstone of ICU delirium care is nonpharmacologic prevention. Non-pharmacologic prevention may reduce the incidence of delirium by 50% (76), including (1) Early rehabilitation exercises: Early rehabilitation activities should be personalized and tailored to the patient’s specific condition and physical status. Simple physical exercises can commence as soon as the patient’s sedation level permits; when the patient’s condition stabilizes, the intensity and complexity of the activities can be gradually increased (77). It has been shown that early rehabilitative exercise reduces delirium duration by 2 day and is safer (78). (2) Psychosocial support: ICU delirium can also be effectively reduced by healthcare professionals and patients’ family members by actively asking patients about their needs, placing familiar objects around them, and giving appropriate psychological support (79, 80). (3) Improve sleep quality: In a study by Al-Aama et al. (81), melatonin was found to improve the quality of sleep and decrease the risk of delirium in elderly patients. Zaal (82) also revealed that improving the surroundings by reducing noise and increasing daylight exposure reduced the duration of delirium. (4) Avoid drugs such as antihistamines (e.g., diphenhydramine, methotrexate) (83, 84), benzodiazepine (e.g., lorazepam and midazolam) (53, 85, 86) tricyclic anxiety medications (e.g., amitriptyline, promethazine) (87), and other anticholinergic drugs (e.g., atropine, scopolamine) (41, 88). The creation of a delirium prevention team can help reduce postoperative delirium in terms of stress management, cognitive function improvement, and delirium risk factors assessment (89).
Medication and psychological / behavioral intervention are the primary treatments for delirium (90). Dexmedetomidine is a centrally active agonist of the alpha-2 adrenergic receptor with sedative, analgesic, and anxiety-relieving effects with no effect on patients’ cognitive performance. Research reveals that administering dexmedetomidine to ICU patients undergoing mechanical ventilation dramatically shortens the duration of delirium and expedites extubation (91). Postoperative intravenous administration of acetaminophen combined with dexmedetomidine or isoproterenol decreases the incidence of delirium (92). The incidence of delirium might be decreased by using exogenous melatonin. Nevertheless, the effect of melatonin has been inconsistent in clinical pilot studies. There was no statistically significant difference in the incidence of delirium in individuals with hip fractures between the melatonin and placebo groups; however, in an internal medicine ward trial involving elderly patients, melatonin treatment significantly decreased the risk of delirium (81, 93). Statins inhibit cholesterol synthesis and have anti-inflammatory and neuroprotective effects that may benefit patients with delirium (88).
The concept of clustering refers to assembling a series of effective treatment and care measures for a disease based on evidence-based medicine to improve the overall clinical outcome. For mechanically ventilated patients in ICU, there is currently a clustered care plan that includes the following: (1) assessment, prevention, and control of pain; (2) conducting spontaneous respiratory and arousal tests; (3) analgesic and sedation strategies; (4) assessment, prevention, and management of delirium; (5) early activity and exercise; and (6) family involvement and empowerment (94). By reducing the likelihood of delirium and the need for mechanical ventilation in the critical care unit, the above bundle improves patient outcomes (95–97). In addition, delirium duration can also be shortened by family-oriented psychotherapy, such as familiar surroundings and the company and comfort of loved ones. Improving the surrounding environment by reducing noise, music therapy (98) and increasing daylight exposure can shorten delirium duration (99–101). Nonpharmacologic preventive strategies, like improving the sleep environment and using drugs appropriately, can lower the risk of morbidity and improve prognosis. These strategies offer new options for clinical treatment as researchers better understand delirium. Research has been done to create customized therapy regimens to lower the incidence of delirium from a variety of angles depending on the presence of risk factors, intraoperative drugs, and other variables (102). This study gives physicians a thorough reference for managing and preventing postoperative delirium, which can help raise awareness of the condition, encourage better clinical practice prevention strategies, enhance patient outcomes, and cut down on medical resource waste.
There are some potential limitations in the current study. Firstly, this study only incorporated English-language literature published after 2013, restricted the publication type to “Article,” and excluded academic reports, conference papers, and other materials. Consequently, significant research findings from non-English-speaking nations may have been overlooked, introducing a language bias to the study. Secondly, the data utilized in this study was sourced from the WOS database, which is a fairly reliable information source. Although the WOS database furnished our study with highly dependable data, it might not comprehensively cover all the pertinent literature. It is recommended that future research consider multilingual literature and leverage additional databases such as Scopus to enhance the study’s accuracy and comprehensiveness.
The current study reflects the research hotspots, trends, and research directions of ICU delirium over the past ten years. Per keywords analysis, the risk factors, clinical presentation, diagnosis, prevention and treatment of ICU delirium were reviewed. These findings will improve understanding of the current status of ICU delirium research and offer valuable information for further investigation.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
XM: Data curation, Formal analysis, Methodology, Project administration, Resources, Software, Visualization, Writing – original draft. QW: Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Visualization, Writing – original draft. YR: Data curation, Formal analysis, Resources, Software, Writing – original draft. XC: Conceptualization, Investigation, Methodology, Visualization, Writing – review & editing. HZ: Conceptualization, Funding acquisition, Supervision, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the National Natural Science Foundation of China (82071211 and 82371209) and Research and Innovation Team Project for Scientific Breakthroughs at Shanxi Bethune Hospital (2024ZHANCHI11).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Oh, ES, Fong, TG, Hshieh, TT, and Inouye, SK. Delirium in older persons: advances in diagnosis and treatment. Jama. (2017) 318:1161–74. doi: 10.1001/jama.2017.12067
2. Kong, D, Luo, W, Zhu, Z, Sun, S, and Zhu, J. Factors associated with post-operative delirium in hip fracture patients: what should we care. Eur J Med Res. (2022) 27:40. doi: 10.1186/s40001-022-00660-9
3. Ely, EW, Shintani, A, Truman, B, Speroff, T, Gordon, SM, Harrell, FE, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. Jama J Amer Med Assoc. (2004) 291:1753–62. doi: 10.1001/jama.291.14.1753
4. Inouye, SK, Westendorp, RGJ, and Saczynski, JS. Delirium in elderly people. Lancet. (2014) 383:911–22. doi: 10.1016/s0140-6736(13)60688-1
5. Pandharipande, P, Cotton, BA, Shintani, A, Thompson, J, Costabile, S, Truman Pun, B, et al. Motoric subtypes of delirium in mechanically ventilated surgical and trauma intensive care unit patients. Intensive Care Med. (2007) 33:1726–31. doi: 10.1007/s00134-007-0687-y
6. Meagher, DJ, and Trzepacz, PT. Motoric subtypes of delirium. Semin Clin Neuropsychiatry. (2000) 5:75–85. doi: 10.153/SCNP00500075
7. Peterson, JF, Pun, BT, Dittus, RS, Thomason, JWW, Jackson, JC, Shintani, AK, et al. Delirium and its motoric subtypes: a study of 614 critically ill patients. J Am Geriatr Soc. (2006) 54:479–84. doi: 10.1111/j.1532-5415.2005.00621.x
8. Cavallazzi, R, Saad, M, and Marik, PE. Delirium in the ICU: an overview. Ann Intensive Care. (2012) 2:49. doi: 10.1186/2110-5820-2-49
9. van den Boogaard, M, Schoonhoven, L, van der Hoeven, JG, van Achterberg, T, and Pickkers, P. Incidence and short-term consequences of delirium in critically ill patients: a prospective observational cohort study. Int J Nurs Stud. (2012) 49:775–83. doi: 10.1016/j.ijnurstu.2011.11.016
10. Thomason, JW, Shintani, A, Peterson, JF, Pun, BT, Jackson, JC, and Ely, EW. Intensive care unit delirium is an independent predictor of longer hospital stay: a prospective analysis of 261 non-ventilated patients. Crit Care. (2005) 9:R375–81. doi: 10.1186/cc3729
11. Ely, EW, Shintani, A, Truman, B, Speroff, T, Gordon, SM, Harrell, FE, et al. The impact of delirium in the intensive care unit on hospital length of stay. Intensive Care Med. (2001) 27:1892–900. doi: 10.1007/s00134-001-1132-2
12. Pisani, MA, Kong, SYJ, Kasl, SV, Murphy, TE, Araujo, KLB, and van Ness, PH. Days of delirium are associated with 1-year mortality in an older intensive care unit population. Am J Respir Crit Care Med. (2009) 180:1092–7. doi: 10.1164/rccm.200904-0537OC
13. Shehabi, Y, Riker, RR, Bokesch, PM, Wisemandle, W, Shintani, A, Ely, EW, et al. Delirium duration and mortality in lightly sedated, mechanically ventilated intensive care patients. Crit Care Med. (2010) 38:2311–8. doi: 10.1097/CCM.0b013e3181f85759
14. Milbrandt, EB, Deppen, S, Harrison, PL, Shintani, AK, Speroff, T, Stiles, RA, et al. Costs associated with delirium in mechanically ventilated patients. Crit Care Med. (2004) 32:955–62. doi: 10.1097/01.ccm.0000119429.16055.92
15. Chen, C. Searching for intellectual turning points: progressive knowledge domain visualization. Proc Natl Acad Sci USA. (2004) 101:5303–10. doi: 10.1073/pnas.0307513100
16. van Eck, NJ, and Waltman, L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. (2010) 84:523–38. doi: 10.1007/s11192-009-0146-3
17. Chen, C. Science mapping: a systematic review of the literature. J Data Inform Sci. (2017) 2:1–40. doi: 10.1515/jdis-2017-0006
18. Ji, L, and Li, F. Potential markers of neurocognitive disorders after cardiac surgery: a bibliometric and visual analysis. Front Aging Neurosci. (2022) 14:868158. doi: 10.3389/fnagi.2022.868158
19. Chen, C. Predictive effects of structural variation on citation counts. J Am Soc Inf Sci Technol. (2012) 63:431–49. doi: 10.1002/asi.21694
20. Ely, EW, Inouye, SK, Bernard, GR, Gordon, S, Francis, J, May, L, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA. (2001) 286:2703–10. doi: 10.1001/jama.286.21.2703
21. Ely, EW. The ABCDEF bundle: science and philosophy of how ICU liberation serves patients and families. Crit Care Med. (2017) 45:321–30. doi: 10.1097/CCM.0000000000002175
22. Li, HJ, An, HZ, Wang, Y, Huang, JC, and Gao, XY. Evolutionary features of academic articles co-keyword network and keywords co-occurrence network: based on two-mode affiliation network. Physica a-Statistical Mechanics Appl. (2016) 450:657–69. doi: 10.1016/j.physa.2016.01.017
23. Inouye, SK, Rushing, JT, Foreman, MD, Palmer, RM, and Pompei, P. Does delirium contribute to poor hospital outcomes? A three-site epidemiologic study. J Gen Intern Med. (1998) 13:234–42. doi: 10.1046/j.1525-1497.1998.00073.x
24. Caplan, JP. Don't ask, don't tell: delirium in the intensive care unit. Crit Care Med. (2009) 37:1129–30. doi: 10.1097/CCM.0b013e31819bb88a
25. Swigart, SE, Kishi, Y, Thurber, S, Kathol, RG, and Meller, WH. Misdiagnosed delirium in patient referrals to a university-based hospital psychiatry department. Psychosomatics. (2008) 49:104–8. doi: 10.1176/appi.psy.49.2.104
26. Aria, M, and Cuccurullo, C. Bibliometrix: An R-tool for comprehensive science mapping analysis. J Informet. (2017) 11:959–75. doi: 10.1016/j.joi.2017.08.007
27. Inouye, SK. Delirium in older persons. N Engl J Med. (2006) 354:1157–65. doi: 10.1056/NEJMra052321
28. Ouimet, S, Kavanagh, BP, Gottfried, SB, and Skrobik, Y. Incidence, risk factors and consequences of ICU delirium. Intensive Care Med. (2007) 33:66–73. doi: 10.1007/s00134-006-0399-8
29. Cole, MG. Delirium in elderly patients. Am J Geriatr Psychiatr. (2004) 12:7–21. doi: 10.1097/00019442-200401000-00002
30. Lin, WL, Chen, YF, and Wang, J. Factors associated with the development of Delirium in elderly patients in intensive care units. J Nurs Res. (2015) 23:322–9. doi: 10.1097/jnr.0000000000000082
31. Levkoff, SE, Evans, DA, Liptzin, B, Cleary, PD, Lipsitz, LA, Wetle, TT, et al. The occurrence and persistence of symptoms among elderly hospitalized patients. Arch Intern Med. (1992) 152:334–40. doi: 10.1001/archinte.1992.00400140082019
32. Lee, HB, Mears, SC, Rosenberg, PB, Leoutsakos, JMS, Gottschalk, A, and Sieber, FE. Predisposing factors for postoperative delirium after hip fracture repair in individuals with and without dementia. J Am Geriatr Soc. (2011) 59:2306–13. doi: 10.1111/j.1532-5415.2011.03725.x
33. Morimoto, Y, Yoshimura, M, Utada, K, Setoyama, K, Matsumoto, M, and Sakabe, T. Prediction of postoperative delirium after abdominal surgery in the elderly. J Anesth. (2009) 23:51–6. doi: 10.1007/s00540-008-0688-1
34. Greene, NH, Attix, DK, Weldon, BC, Smith, PJ, McDonagh, DL, and Monk, TG. Measures of executive function and depression identify patients at risk for postoperative delirium. Anesthesiology. (2009) 110:788–95. doi: 10.1097/aln.0b013e31819b5ba6
35. Lawlor, PG, Gagnon, B, Mancini, IL, Pereira, JL, Hanson, J, Suarez-Almazor, ME, et al. Occurrence, causes, and outcome of delirium in patients with advanced cancer: a prospective study. Arch Intern Med. (2000) 160:786–94. doi: 10.1001/archinte.160.6.786
36. Balas, MC, Happ, MB, Yang, W, Chelluri, L, and Richmond, T. Outcomes associated with Delirium in older patients in surgical ICUs. Chest. (2009) 135:18–25. doi: 10.1378/chest.08-1456
37. Zhang, DF, Su, X, Meng, ZT, Cui, F, Li, HL, Wang, DX, et al. Preoperative severe hypoalbuminemia is associated with an increased risk of postoperative delirium in elderly patients: results of a secondary analysis. J Crit Care. (2018) 44:45–50. doi: 10.1016/j.jcrc.2017.09.182
39. Lindroth, H, Bratzke, L, Purvis, S, Brown, R, Coburn, M, Mrkobrada, M, et al. Systematic review of prediction models for delirium in the older adult inpatient. BMJ Open. (2018) 8:e019223. doi: 10.1136/bmjopen-2017-019223
40. Marcantonio, ER, Goldman, L, Mangione, CM, Ludwig, LE, Muraca, B, Haslauer, CM, et al. A clinical prediction rule for delirium after elective noncardiac surgery. JAMA. (1994) 271:134–9. doi: 10.1001/jama.1994.03510260066030
41. Burry, LD, Williamson, DR, Mehta, S, Perreault, MM, Mantas, I, Mallick, R, et al. Delirium and exposure to psychoactive medications in critically ill adults: a multi-Centre observational study. J Crit Care. (2017) 42:268–74. doi: 10.1016/j.jcrc.2017.08.003
42. Dubois, MJ, Bergeron, N, Dumont, M, Dial, S, and Skrobik, Y. Delirium in an intensive care unit: a study of risk factors. Intensive Care Med. (2001) 27:1297–304. doi: 10.1007/s001340101017
43. Sury, MRJ, Billingham, I, Russell, GN, Hopkins, CS, Thornington, R, and Vivori, E. Acute benzodiazepine withdrawal syndrome after midazolam infusions in children. Crit Care Med. (1989) 17:301–2. doi: 10.1097/00003246-198903000-00027
44. Wang, CG, Qin, YF, Wan, X, Song, LC, Li, ZJ, and Li, H. Incidence and risk factors of postoperative delirium in the elderly patients with hip fracture. J Orthop Surg Res. (2018) 13:186. doi: 10.1186/s13018-018-0897-8
45. Berian, JR, Zhou, L, Russell, MM, Hornor, MA, Cohen, ME, Finlayson, E, et al. Postoperative Delirium as a target for surgical quality improvement. Ann Surg. (2018) 268:93–9. doi: 10.1097/sla.0000000000002436
46. Chaiwat, O, Chanidnuan, M, Pancharoen, W, Vijitmala, K, Danpornprasert, P, Toadithep, P, et al. Postoperative delirium in critically ill surgical patients: incidence, risk factors, and predictive scores. BMC Anesthesiol. (2019) 19:39. doi: 10.1186/s12871-019-0694-x
47. Coppola, S, Caccioppola, A, and Chiumello, D. Internal clock and the surgical ICU patient. Curr Opin Anaesthesiol. (2020) 33:177–84. doi: 10.1097/ACO.0000000000000816
48. Turkel, SB, and Tavaré, CJ. Delirium in children and adolescents. J Neuropsychiatry Clin Neurosci. (2003) 15:431–5. doi: 10.1176/jnp.15.4.431
49. Jung, P, Pereira, MA, Hiebert, B, Song, X, Rockwood, K, Tangri, N, et al. The impact of frailty on postoperative delirium in cardiac surgery patients. J Thorac Cardiovasc Surg. (2015) 149:869–875.e2. doi: 10.1016/j.jtcvs.2014.10.118
50. Bamalwa, M, Mahmood, SN, and Praharaj, SK. Delirium in cardiac ICU patients. Ann Clin Psychiatry. (2016) 28:51–5.
51. Thorsteinsdóttir, SA, Sveinsdóttir, H, and Snædal, J. Delirium after open cardiac surgery:systematic review of prevalence, risk factors and consequences. Laeknabladid. (2015) 101:305–11. doi: 10.17992/lbl.2015.06.31
52. Girard, TD, Kress, JP, Fuchs, BD, Thomason, JWW, Schweickert, WD, Pun, BT, et al. Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care (awakening and breathing controlled trial): a randomised controlled trial. Lancet. (2008) 371:126–34. doi: 10.1016/S0140-6736(08)60105-1
53. Pandharipande, P, Cotton, BA, Shintani, A, Thompson, J, Pun, BT, Morris JA Jr,, et al. Prevalence and risk factors for development of delirium in surgical and trauma intensive care unit patients. J Trauma. (2008) 65:34–41. doi: 10.1097/TA.0b013e31814b2c4d
54. Gnanavel, S, and Robert, RS. Diagnostic and statistical manual of mental disorders, fifth edition, and the impact of events scale-revised. Chest. (2013) 144:1974. doi: 10.1378/chest.13-1691
55. Meagher, DJ, Leonard, M, Donnelly, S, Conroy, M, Adamis, D, and Trzepacz, PT. A longitudinal study of motor subtypes in delirium: relationship with other phenomenology, etiology, medication exposure and prognosis. J Psychosom Res. (2011) 71:395–403. doi: 10.1016/j.jpsychores.2011.06.001
56. Vasilevskis, EE, Han, JH, Hughes, CG, and Ely, EW. Epidemiology and risk factors for delirium across hospital settings. Best Pract Res Clin Anaesthesiol. (2012) 26:277–87. doi: 10.1016/j.bpa.2012.07.003
57. Zalon, ML, Sandhaus, S, Kovaleski, M, and Roe-Prior, P. Hospitalized older adults with established Delirium: recognition, documentation, and reporting. J Gerontol Nurs. (2017) 43:32–40. doi: 10.3928/00989134-20161109-01
58. van Eijk, MM, van den Boogaard, M, van Marum, RJ, Benner, P, Eikelenboom, P, Honing, ML, et al. Routine use of the confusion assessment method for the intensive care unit: a multicenter study. Am J Respir Crit Care Med. (2011) 184:340–4. doi: 10.1164/rccm.201101-0065OC
59. Spronk, PE, Riekerk, B, Hofhuis, J, and Rommes, JH. Occurrence of delirium is severely underestimated in the ICU during daily care. Intensive Care Med. (2009) 35:1276–80. doi: 10.1007/s00134-009-1466-8
60. Luetz, A, Heymann, A, Radtke, FM, Chenitir, C, Neuhaus, U, Nachtigall, I, et al. Different assessment tools for intensive care unit delirium: which score to use? Crit Care Med. (2010) 38:409–18. doi: 10.1097/CCM.0b013e3181cabb42
61. Maybrier, HR, Mickle, AM, Escallier, KE, Lin, N, Schmitt, EM, Upadhyayula, RT, et al. Reliability and accuracy of delirium assessments among investigators at multiple international centres. BMJ Open. (2018) 8:e023137. doi: 10.1136/bmjopen-2018-023137
62. Wang, C, Wu, Y, Yue, P, Ely, EW, Huang, J, Yang, X, et al. Delirium assessment using confusion assessment method for the intensive care unit in Chinese critically ill patients. J Crit Care. (2013) 28:223–9. doi: 10.1016/j.jcrc.2012.10.004
63. Bergeron, N, Dubois, MJ, Dumont, M, Dial, S, and Skrobik, Y. Intensive care Delirium screening checklist: evaluation of a new screening tool. Intensive Care Med. (2001) 27:859–64. doi: 10.1007/s001340100909
64. Barr, J, Fraser, GL, Puntillo, K, Ely, EW, Gélinas, C, Dasta, JF, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. (2013) 41:263–306. doi: 10.1097/CCM.0b013e3182783b72
65. Tobar, E, Romero, C, Galleguillos, T, Fuentes, P, Cornejo, R, Lira, MT, et al. Confusion assessment method for diagnosing delirium in ICU patients (CAM-ICU): cultural adaptation and validation of the Spanish version. Med Intensiva. (2010) 34:4–13. doi: 10.1016/j.medin.2009.04.003
66. Lin, SM, Liu, CY, Wang, CH, Lin, HC, Huang, CD, Huang, PY, et al. The impact of delirium on the survival of mechanically ventilated patients. Crit Care Med. (2004) 32:2254–9. doi: 10.1097/01.ccm.0000145587.16421.bb
67. Toro, AC, Escobar, LM, Franco, JG, Díaz-Gómez, JL, Muñoz, JF, Molina, F, et al. Spanish version of the CAM-ICU (confusion assessment method for the intensive care unit). Pilot study of validation. Med Intensiva. (2010) 34:14–21. doi: 10.1016/j.medin.2009.07.002
68. Gusmao-Flores, D, Salluh, JI, Dal-Pizzol, F, Ritter, C, Tomasi, CD, Lima, MA, et al. The validity and reliability of the Portuguese versions of three tools used to diagnose delirium in critically ill patients. Clinics. (2011) 66:1917–22. doi: 10.1590/s1807-59322011001100011
69. Mitasova, A, Kostalova, M, Bednarik, J, Michalcakova, R, Kasparek, T, Balabanova, P, et al. Poststroke delirium incidence and outcomes: validation of the confusion assessment method for the intensive care unit (CAM-ICU). Crit Care Med. (2012) 40:484–90. doi: 10.1097/CCM.0b013e318232da12
70. Heo, EY, Lee, BJ, Hahm, BJ, Song, EH, Lee, HA, Yoo, CG, et al. Translation and validation of the Korean confusion assessment method for the intensive care unit. BMC Psychiatry. (2011) 11:94. doi: 10.1186/1471-244x-11-94
71. Chuang, WL, Lin, CH, Hsu, WC, Ting, YJ, Lin, KC, and Ma, SC. Evaluation of the reliability and validity of the Chinese version of the confusion assessment method for the intensive care unit. Hu Li Za Zhi. (2007) 54:45–52.
72. Salluh, JI, Dal-Pizzol, F, Mello, PV, Friedman, G, Silva, E, Teles, JM, et al. Delirium recognition and sedation practices in critically ill patients: a survey on the attitudes of 1015 Brazilian critical care physicians. J Crit Care. (2009) 24:556–62. doi: 10.1016/j.jcrc.2009.04.004
73. Patel, RP, Gambrell, M, Speroff, T, Scott, TA, Pun, BT, Okahashi, J, et al. Delirium and sedation in the intensive care unit: survey of behaviors and attitudes of 1384 healthcare professionals. Crit Care Med. (2009) 37:825–32. doi: 10.1097/CCM.0b013e31819b8608
74. Gusmao-Flores, D, Salluh, JI, Chalhub, RA, and Quarantini, LC. The confusion assessment method for the intensive care unit (CAM-ICU) and intensive care delirium screening checklist (ICDSC) for the diagnosis of delirium: a systematic review and meta-analysis of clinical studies. Crit Care. (2012) 16:R115. doi: 10.1186/cc11407
75. Jing, GW, Xie, Q, Tong, J, Liu, LZ, Jiang, X, and Si, L. Early intervention of perioperative Delirium in older patients (>60 years) with hip fracture: a randomized controlled study. Orthop Surg. (2022) 14:885–91. doi: 10.1111/os.13244
76. Hshieh, TT, Yue, J, Oh, E, Puelle, M, Dowal, S, Travison, T, et al. Effectiveness of multicomponent nonpharmacological delirium interventions: a meta-analysis. JAMA Intern Med. (2015) 175:512–20. doi: 10.1001/jamainternmed.2014.7779
77. Mart, MF, Williams Roberson, S, Salas, B, Pandharipande, PP, and Ely, EW. Prevention and Management of Delirium in the intensive care unit. Semin Respir Crit Care Med. (2021) 42:112–26. doi: 10.1055/s-0040-1710572
78. Schweickert, WD, Pohlman, MC, Pohlman, AS, Nigos, C, Pawlik, AJ, Esbrook, CL, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. (2009) 373:1874–82. doi: 10.1016/S0140-6736(09)60658-9
79. Martinez, FT, Tobar, C, Beddings, CI, Vallejo, G, and Fuentes, P. Preventing delirium in an acute hospital using a non-pharmacological intervention. Age Ageing. (2012) 41:629–34. doi: 10.1093/ageing/afs060
80. Sampson, EL, West, E, and Fischer, T. Pain and delirium: mechanisms, assessment, and management. Eur Geriatr Med. (2020) 11:45–52. doi: 10.1007/s41999-019-00281-2
81. al-Aama, T, Brymer, C, Gutmanis, I, Woolmore-Goodwin, S, Esbaugh, J, and Dasgupta, M. Melatonin decreases delirium in elderly patients: a randomized, placebo-controlled trial. Int J Geriatr Psychiatry. (2011) 26:687–94. doi: 10.1002/gps.2582
82. Zaal, IJ, Spruyt, CF, Peelen, LM, van Eijk, MMJ, Wientjes, R, Schneider, MME, et al. Intensive care unit environment may affect the course of delirium. Intensive Care Med. (2013) 39:481–8. doi: 10.1007/s00134-012-2726-6
83. Shinohara, M, and Yamada, M. Drug-induced cognitive impairment. Brain Nerve. (2016) 68:421–8. doi: 10.11477/mf.1416200415
84. Nakamizo, T, Kanda, T, Kudo, Y, Sugawara, E, Hashimoto, E, Okazaki, A, et al. Effects of uncomfortable care and histamine H2-antagonists on delirium in acute stroke: a propensity score analysis. J Neurol Sci. (2021) 420:117251. doi: 10.1016/j.jns.2020.117251
85. Pisani, MA, Murphy, TE, Araujo, KLB, Slattum, P, van Ness, PH, and Inouye, SK. Benzodiazepine and opioid use and the duration of intensive care unit delirium in an older population. Crit Care Med. (2009) 37:177–83. doi: 10.1097/CCM.0b013e318192fcf9
86. Pandharipande, P, Shintani, A, Peterson, J, Pun, BT, Wilkinson, GR, Dittus, RS, et al. Lorazepam is an independent risk factor for transitioning to delirium in intensive care unit patients. Anesthesiology. (2006) 104:21–6. doi: 10.1097/00000542-200601000-00005
87. Duggal, HS. Delirium associated with amitriptyline/fluconazole drug. Gen Hosp Psychiatry. (2003) 25:297–8. doi: 10.1016/s0163-8343(03)00052-5
88. Han, L, McCusker, J, Cole, M, Abrahamowicz, M, Primeau, F, and Élie, M. Use of medications with anticholinergic effect predicts clinical severity of delirium symptoms in older medical inpatients. Arch Intern Med. (2001) 161:1099–105. doi: 10.1001/archinte.161.8.1099
89. Deeken, F, Sánchez, A, Rapp, MA, Denkinger, M, Brefka, S, Spank, J, et al. Outcomes of a Delirium prevention program in older persons after elective surgery: a stepped-wedge cluster randomized clinical trial. JAMA Surg. (2022) 157:e216370. doi: 10.1001/jamasurg.2021.6370
90. Sahawneh, F, and Boss, L. Non-pharmacologic interventions for the prevention of delirium in the intensive care unit: An integrative review. Nurs Crit Care. (2021) 26:166–75. doi: 10.1111/nicc.12594
91. Riker, RR, Shehabi, Y, Bokesch, PM, Ceraso, D, Wisemandle, W, Koura, F, et al. Dexmedetomidine vs midazolam for sedation of critically ill patients: a randomized trial. JAMA. (2009) 301:489–99. doi: 10.1001/jama.2009.56
92. Subramaniam, B, Shankar, P, Shaefi, S, Mueller, A, O’Gara, B, Banner-Goodspeed, V, et al. Effect of intravenous acetaminophen vs placebo combined with Propofol or Dexmedetomidine on postoperative Delirium among older patients following cardiac surgery: the DEXACET randomized clinical trial. JAMA. (2019) 321:686–96. doi: 10.1001/jama.2019.0234
93. de Jonghe, A, van Munster, B, Goslings, JC, Kloen, P, van Rees, C, Wolvius, R, et al. Effect of melatonin on incidence of delirium among patients with hip fracture: a multicentre, double-blind randomized controlled trial. CMAJ. (2014) 186:E547–56. doi: 10.1503/cmaj.140495
94. Marra, A, Ely, EW, Pandharipande, PP, and Patel, MB. The ABCDEF bundle in critical care. Crit Care Clin. (2017) 33:225–43. doi: 10.1016/j.ccc.2016.12.005
95. Pun, BT, Balas, MC, Barnes-Daly, MA, Thompson, JL, Aldrich, JM, Barr, J, et al. Caring for critically ill patients with the ABCDEF bundle: results of the ICU liberation collaborative in over 15,000 adults. Crit Care Med. (2019) 47:3–14. doi: 10.1097/CCM.0000000000003482
96. Barnes-Daly, MA, Phillips, G, and Ely, EW. Improving hospital survival and reducing brain dysfunction at seven California community hospitals: implementing PAD guidelines via the ABCDEF bundle in 6,064 patients. Crit Care Med. (2017) 45:171–8. doi: 10.1097/ccm.0000000000002149
97. Balas, MC, Vasilevskis, EE, Olsen, KM, Schmid, KK, Shostrom, V, Cohen, MZ, et al. Effectiveness and safety of the awakening and breathing coordination, delirium monitoring/management, and early exercise/mobility bundle. Crit Care Med. (2014) 42:1024–36. doi: 10.1097/ccm.0000000000000129
98. Johnson, K, Fleury, J, and McClain, D. Music intervention to prevent delirium among older patients admitted to a trauma intensive care unit and a trauma orthopaedic unit. Intensive Crit Care Nurs. (2018) 47:7–14. doi: 10.1016/j.iccn.2018.03.007
99. Foster, J, and Kelly, M. A pilot study to test the feasibility of a nonpharmacologic intervention for the prevention of delirium in the medical intensive care unit. Clin Nurse Spec. (2013) 27:231–8. doi: 10.1097/NUR.0b013e3182a0b9f9
100. Moon, KJ, and Lee, SM. The effects of a tailored intensive care unit delirium prevention protocol: a randomized controlled trial. Int J Nurs Stud. (2015) 52:1423–32. doi: 10.1016/j.ijnurstu.2015.04.021
101. Hanison, J, and Conway, D. A multifaceted approach to prevention of delirium on intensive care. BMJ Qual Improv Rep. (2015) 4:u209656. doi: 10.1136/bmjquality.u209656.w4000
Keywords: delirium, intensive care unit, ICU, Citespace, VOSviewer
Citation: Ma X, Wu Q, Ran Y, Cao X and Zheng H (2025) A bibliometric analysis on delirium in intensive care unit from 2013–2023. Front. Neurol. 16:1469725. doi: 10.3389/fneur.2025.1469725
Received: 24 July 2024; Accepted: 22 January 2025;
Published: 12 February 2025.
Edited by:
Yucheng Xiao, Indiana University, United StatesReviewed by:
Tao Tao, Southern Medical University, ChinaCopyright © 2025 Ma, Wu, Ran, Cao and Zheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hua Zheng, aHpoZW5nQGh1c3QuZWR1LmNu
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.