
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol., 11 April 2025
Sec. Endovascular and Interventional Neurology
Volume 16 - 2025 | https://doi.org/10.3389/fneur.2025.1453841
This article is part of the Research TopicIntracranial aneurysms, AVM and other vascular malformations, and connective tissue disorders as potential causes of stroke: Advances in diagnosis and therapeutics including novel neurosurgical techniquesView all 15 articles
 Xueqian Zhang1,2,3
Xueqian Zhang1,2,3 Yang Li4
Yang Li4 Kuochang Yin1,2,3
Kuochang Yin1,2,3 Zhiwei Hao5
Zhiwei Hao5 Yidian Fu1
Yidian Fu1 Qishuo Yang5
Qishuo Yang5 Guodong Xu1,2,3
Guodong Xu1,2,3 Peiyuan Lv1,2,3*
Peiyuan Lv1,2,3*Background and purpose: Endovascular recanalization and stenting has been used to treat patients with symptomatic chronic cerebral artery occlusion, including intracranial vertebrobasilar artery occlusion and internal carotid artery occlusion. Our challenge is to improve success rates and reduce the incidence of postoperative complications. This study sought to identify potential predictors for successful recanalization.
Methods: Our study included 103 consecutive patients between February 2021 and October 2024 with symptomatic chronic cerebral artery occlusion who were treated with endovascular recanalization. We recorded clinical information, laboratory and examination results, radiologic characteristics and procedural results of patients. Factors affecting surgical outcomes were analyzed by univariate and multivariate analyses.
Results: A total of 103 consecutive CCAO recanalization attempts were performed from February 2021 to October 2024 in 103 patients (78 men; age 61.1 ± 11.1 years; range: 32–81 years) with overall technical success rate 68.9%. Patients had chronic comorbidities such as hypertension (78, 75.7%), diabetes mellitus (32, 31.10%), and cardiac disease (12, 11.7%). 38 (36.9%) had a history of smoking, and 23 (22.3%) had a history of drinking. The rate of overall intraoperative complication was 10.7% (11/103). Multivariate analysis showed that stump morphology, smoking history, duration from last neurologic event (longer than 6 months or not), age, NLR were significantly associated with successful recanalization. According to the coefficients of the prediction model, the technical success rates were 100, 66.7 and 11.1% in patients with ≤6, 6–10, ≥10 points, respectively.
Conclusion: The morphology of occluded stumps, duration from last neurologic event, age, smoking history and NLR can be used to predict the outcome of vascular recanalization.
• This study covers a wide range of cases including internal carotid artery and vertebrobasilar artery system.
• This study identified five factors that affect the outcome of vascular recanalization.
• This study developed a scoring system for predicting surgical outcomes.
Chronic cerebral artery occlusion disease is currently the culprit that troubles a considerable number of cerebrovascular diseases patients with high recurrence rate and low quality of life. According to the location of vascular occlusion, it can be divided into anterior circulation occlusion and posterior circulation occlusion. The treatment of patients with chronic cerebral artery occlusion (CCAO) is controversial, especially those with symptoms of hypoperfusion or stroke. Even with active internal medicine medication treatment, 6–20% of CCAO patients still experience stroke events every year. The risk of ischemic stroke in such patients increased from 8% after 30 days of follow-up to 14% after 5 years of follow-up (1). The annual risk of recurrent stroke in patients with transient ischemic attack (TIA) or ischemic stroke associated with carotid artery occlusion is approximately 5–6% (2). That risk is approximately 12% per year in the subgroup of symptomatic ICA occlusive patients, in this subgroup, the hemodynamic state of the brain is impaired (3).
The proportion of patients with posterior circulation occlusion is not low in cerebral artery occlusive diseases. About 20% of ischemic stroke patients are caused by posterior circulation ischemia (4). According to literature statistics, the incidence of chronic vertebral artery occlusion in the Chinese population is higher than that in Caucasian (5). In patients with posterior circulation ischemia, the incidence of significant stenosis or occlusion at the origin of the vertebral artery is 32.1%, and the incidence of significant stenosis or occlusion in the intracranial segment of the vertebral artery is 32.4%; The incidence of vertebral artery stenosis or occlusion is very high in patients with posterior circulation ischemia (6). With the rapid development of neural intervention technology and surgical instruments, intervention recanalization technology has become increasingly mature. The number of research on chronic intracranial and extracranial artery occlusion and recanalization is also increasing year by year both domestically and internationally.
However, almost all studies only focus on anterior circulation occlusion, there is relatively few research on posterior circulation occlusion. In our study, we analyzed and summarized various cases of chronic cerebral artery occlusion treatment completed in the past 5 years, including the intracranial and extracranial segments of anterior circulation, as well as the intracranial and extracranial segments of posterior circulation. In the process, we analyzed and explored the feasibility, safety, and predictive factors for surgical success.
This study is a retrospective study conducted at our center. Every patient with CCAO were treated in a unified clinical management process including patient screening and exclusion criteria, surgical process management, perioperative management, and long-term follow-up. All patients have signed written informed consent forms. This study followed the principles of the Declaration of Helsinki and was approved by the Ethics Committee of Hebei General Hospital (No. 2024-LW-084).
All patients had received intensive medical treatment before intravascular treatment (including antiplatelet therapy and controlling atherosclerosis risk factors: blood pressure, plasma glucose, plasma lipid, smoking cessation, alcohol abstinence, etc.), but because of inadequate response to medication, there were still symptoms of cerebral ischemia caused by hypoperfusion. The responsible arteries of the selected patients include complete occlusion of the internal carotid artery (both the intracranial and extracranial segments), the middle cerebral artery, the vertebral artery (both the intracranial and extracranial segments) and the basilar artery. We recorded the time interval from the last appearance of symptoms (including ischemic stroke and transient ischemic attack) to surgery for each patient (each patient was over 30 days).
1. Age > 18 years;
2. Atherosclerotic CCAO defined as 100% cross-sectional truncation of the vascular lumen documented by computerized magnetic resonance angiography (MRA) or tomography angiography (CTA) and uniformly confirmed with digital subtraction angography (DSA);
3. Time from imaging diagnosis or from aggravation of clinical symptoms defined as change in National Institutes of Health Stroke Scale (NIHSS) score ≥ 4 or modified Rankin Scale (mRS) score ≥ 1 to recanalization was over 24 h;
4. Even after receiving active pharmacological treatment, the recurrence or exacerbation of neurological symptoms could not be ameliorated or controlled;
5. Perfusion imaging (CTP or MRP) shows low perfusion in the supply area of occluded arteries;
6. Each patient has at least one atherosclerosis risk factor such as hypertension, dyslipidemia, diabetes mellitus, smoking, etc.
1. Nonatherosclerotic occlusion (vasculitis, trauma, dissection, or Moyamoya disease, etc.) or asymptomatic CCAO;
2. Known allergy or contraindication to heparin, aspirin, clopidogrel, metal, or general anesthesia;
3. Expected lifespan is less than 2 years caused by any other medical conditions;
4. Recurrence or aggravation of neurologic symptoms are not caused by the occluded artery;
5. Uncorrectable bleeding diathesis;
6. Refusing surgery due to personal financial burden;
7. Any other conditions not suitable for operation.
We collected the patient’s gender, age, duration of vascular occlusion, past history (hypertension, diabetes, coronary heart disease history), smoking history, drinking history, body mass index (BMI) and occluded stump morphology (the previous neurological symptoms were defined as ipsilateral transient ischemic attacks or ischemic stroke or amaurosis, we record the duration from the last neurological event to intervention, dividing patients into two categories based on whether it is longer than 6 months). Based on the cerebral angiography images, according to the angle formed by the plane of the stump and the vessel wall of the involved blood vessel, it is classified as follows: “sharp” type (≤45°) and “blunt” type (>45°). If the end presents a flat stump, it is the “flat” type; if there is no obvious stump, it is the “no stump” type.
In addition, we also collected and summarized serum laboratory data from various patients: fasting blood glucose value, neutrophil value, lymphocyte value, neutrophil to lymphocyte ratio, platelet count, fibrinogen platelet ratio, platelet lymphocyte ratio, extremely low-density lipoprotein, low-density lipoprotein, apolipoprotein B, triglycerides, cholesterol, uric acid, creatinine, INR, fibrinogen, D-dimer, and foaming test results.
In this study, the success of endovascular treatment was defined as residual stenosis rate < 50% and establishing grade 3 antegrade TICI flow, with surgical success as the primary endpoint event. TICI is divided into levels 0, 1, 2a, 2b, and 3 (7). The internal carotid artery (ICA) is classified into seven segments (8), namely C1, C2, C3, C4, C5, C6, and C7. The vertebral artery (VA) is classified into four segments, namely V1, V2, V3, and V4. The failure of endovascular treatment is defined when the occluded blood vessel cannot be recanalized after 30 min of repeated attempts and more than 300 milliliters of contrast agent have been consumed, the surgery ended accordingly.
The surgery is performed by experienced neurologists under general anesthesia. The guide catheter was advanced into the cervical VA or ICA as high as allowed by vessel tortuosity. A 0.014-inch microwire was carefully coaxially advanced with a microcatheter (Echelon 10) through the occluded segment. The Synchro microwire (200 cm) was our first choice, other micro wires such as Pilot microwires can be replaced appropriately based on the degree of tortuosity of the vascular pathway. After the 0.014-inch microwire with supporting microcatheter passed through the lesion, microcatheter angiography was performed to confirm that the tip of the microcatheter is in the true lumen of the blood vessel. Then, using exchange technology, place a 300 centimeter microwire into the distal vascular branch of the occluded artery. And use a balloon to dilate the narrow segment (at least 30 s). Properly sized balloon stents and self-expanding stents were used to cover narrow segments. Balloon dilation can be performed if the stent expansion is not sufficient.
Each patient should take aspirin, clopidogrel, or ticagrelor orally before surgery. The main lipid-lowering and plaque stabilizing drugs are atorvastatin and rosuvastatin. At the same time, pay attention to observing adverse drug reactions and maintain them for life. If there is a thrombotic event during surgery, tirofiban antiplatelet aggregation therapy can be added. Kang et al. systematically outlined perioperative protocols and pharmacological strategies for cerebral vascular occlusion recanalization (CVOR) procedures (9), and we also referred to this strategy in practical clinical applications.
All continuous variables were expressed as mean ± SD, and categorical variables in numbers and percentage. Chi square test is used to compare categorical data and logistic regression method is used to compare continuous data. All statistical analyses were 2-tailed, and p < 0.05 was accepted as statistically significant. Statistical analysis was conducted using R Programming Language (version 4.3.2). Sensitivity and specificity were measured using the Jordan index. To evaluate the sensitivity and specificity of the diagnostic method used in this study, Receiver Operating Characteristic (ROC) curve analysis was conducted. The area under the ROC curve (AUC) was also calculated by R Programming Language. An AUC of 0.5 indicates that the diagnostic test is no better than random chance, while an AUC of 1.0 represents a perfect diagnostic test. The optimal cut - off point for the diagnostic test was determined by maximizing the Youden’s index (sensitivity + specificity − 1). At this cut - off point, the balance between sensitivity and specificity was considered the most favorable for accurate diagnosis.
A total of 103 consecutive CCAO recanalization attempts were performed from February 2021 to October 2024 in 103 patients (78 men; age 61.1 ± 11.1 years; range: 32 to 81 years) with overall technical success rate 68.9%. Many patients had chronic comorbidities such as hypertension (78, 75.7%), diabetes mellitus (32, 31.10%), and cardiac disease (12, 11.7%). In addition, 38 (36.9%) had a history of smoking, and 23 (22.3%) had a history of drinking. The baseline clinical variables are summarized in Table 1.
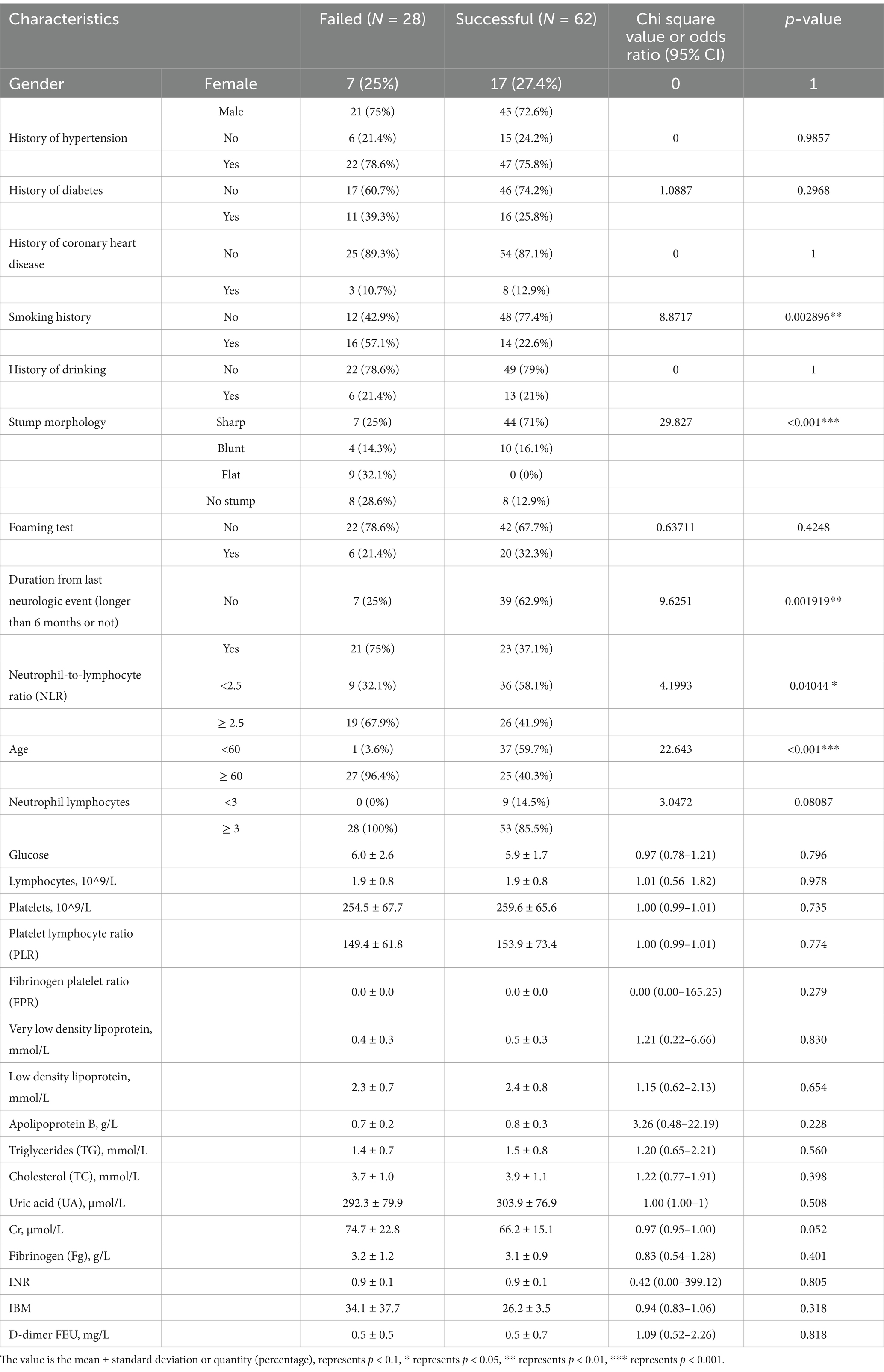
Table 1. Baseline characteristics of the studied patient population as stratified by failed or successful recanalization.
The rate of overall intraoperative complication was 10.7% (11/103).1 patient had occlusion of ophthalmic artery, 2 patient had a slight subarachnoid hemorrhage followed by microwire perforation, 1 patient had a slight intraparenchymal hemorrhage, 1 patient died of massive recanalization hemorrhage 2 day after the procedure, 2 patients had distal embolization accompanied by mild symptoms of limb hemiplegia. Four patients had reocclusion of instent thrombosis with progression of symptoms of hemiplegia in limbs. No patient dies in the failed recanalization group (Table 2).
Table 3 showed the score for predicting surgical success, as well as the success rates of different total score points. The success rate of surgery increases as the score decreases. The c-index on the basis of area under the curve for this scoring system in predicting technical success was 0.943 (95%CI: 0.8905–0.9862; P < 0.001), with a sensitivity of 71.28% and a specificity of 75.26 (Figure 1). This indicates that the effectiveness of the model score in predicting patient surgical is commendable.
According to the type of occlusion site (anterior or posterior circulation, as well as intracranial or extracranial segments), four surgical imaging data of example cases were showed separately as follows (Figures 2–5), including several key steps during surgical process. At the same time we provide corresponding specific descriptions in the diagram.
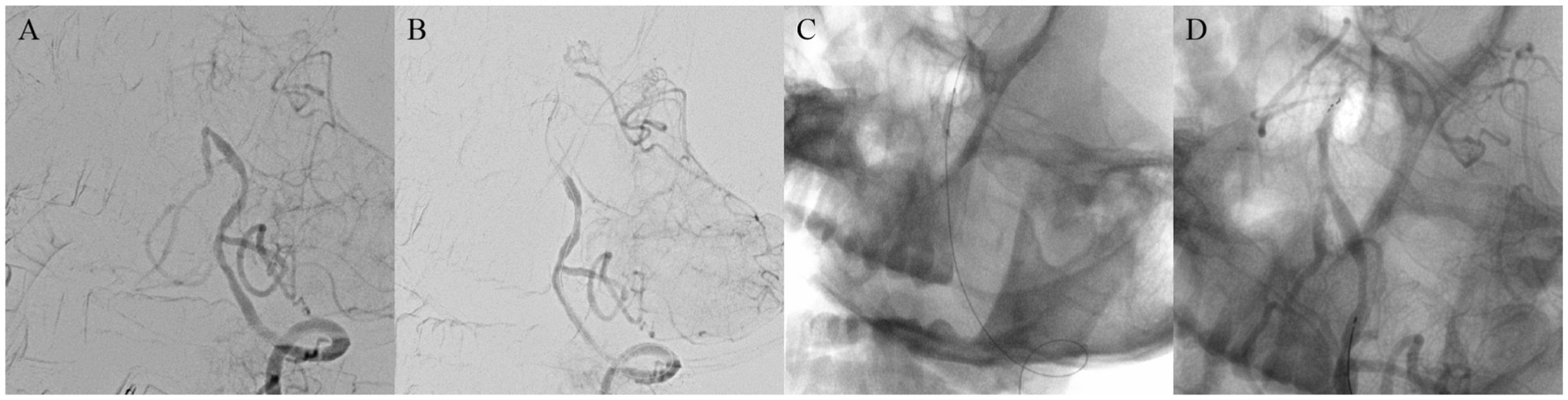
Figure 2. A 42-year-old man with lower basilar artery occlusion. Digital subtraction angiography confirmed occlusion of the basilar artery (A). Carefully probe the blocked section with a micro guide wire and confirm the true lumen of the blood vessel (B). Using balloon catheters to dilate narrow segments of the basilar artery (C). Successful recanalization of basilar artery occlusion, angiography shows good imaging of the basilar artery and bilateral posterior cerebral arteries, with normal blood flow velocity (D).
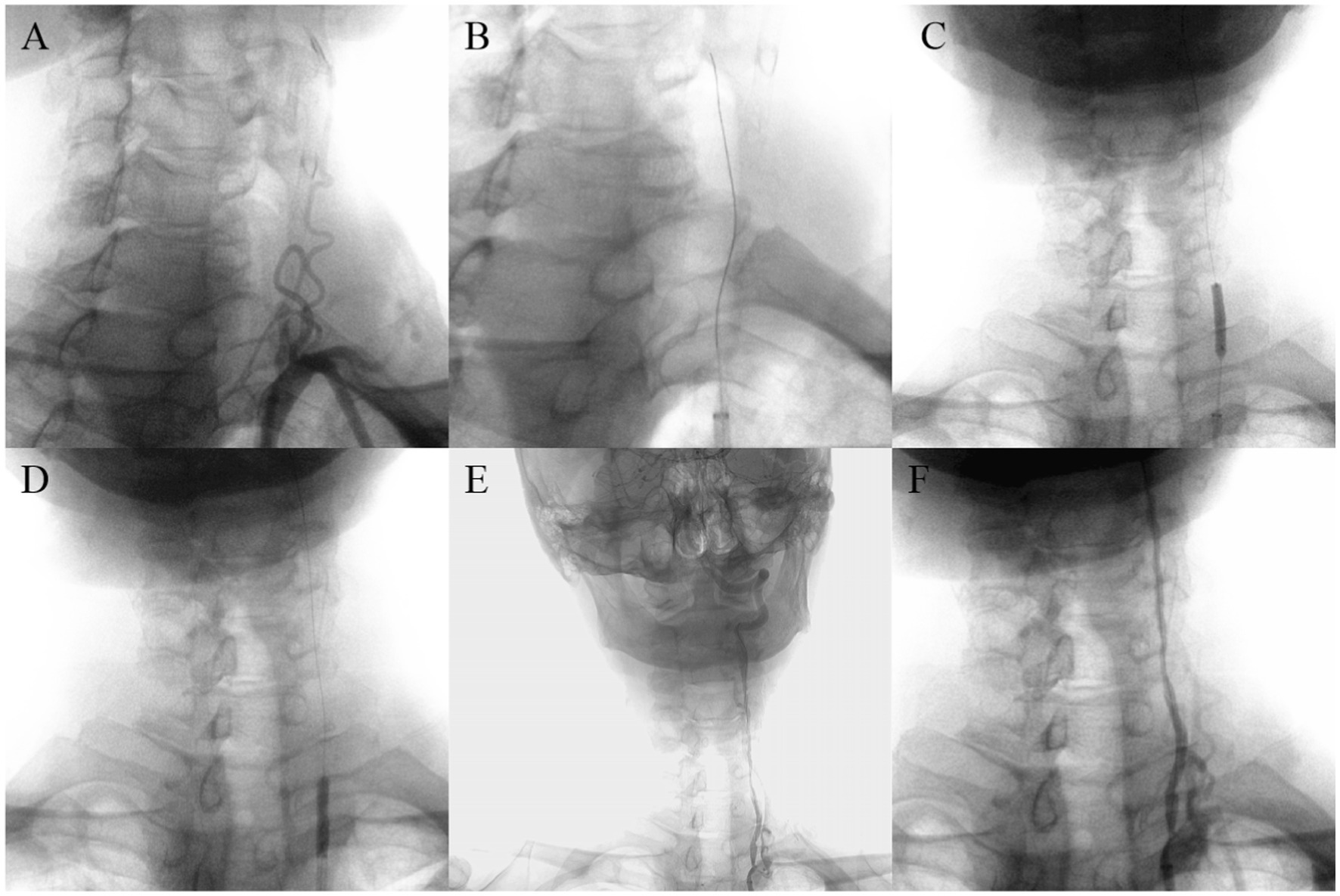
Figure 3. A 69-year-old man with left vertebral artery VI segment occlusion. Digital subtraction angiography confirmed occlusion of the left vertebral artery V1 segment without obvious stumps (A). Carefully probe the blocked section with loach guide wire (B). Using balloon catheters to dilate narrow segments of vertebral artery from far to near (C,D). Successful recanalization with good antegrade perfusion was achieved (E,F).
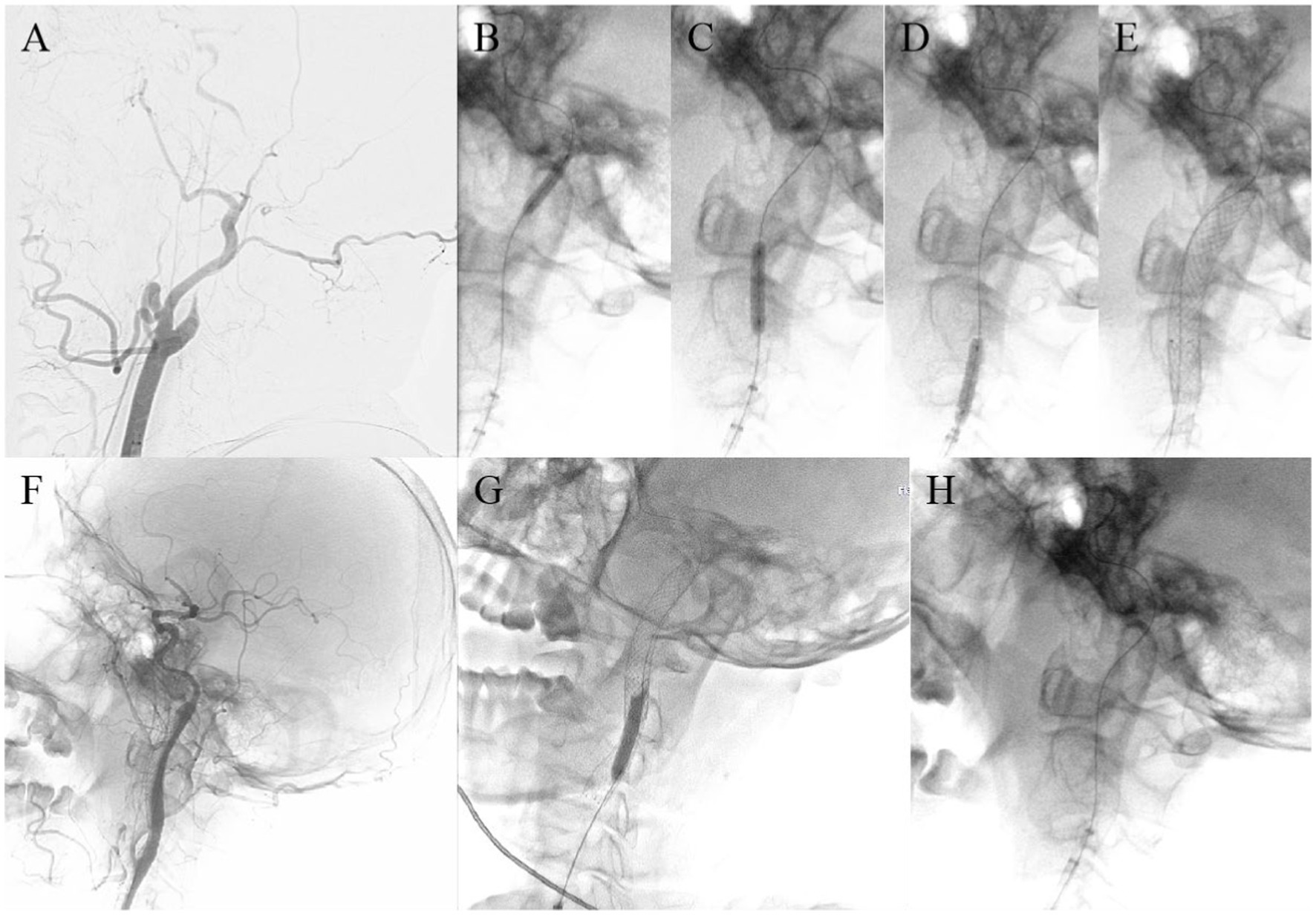
Figure 4. A 64-year-old man with left internal carotid artery C1 segment occlusion. Digital subtraction angiography confirmed occlusion of the left ICA (A). Carefully probe the blocked section with a micro guide wire and confirm the true lumen of the blood vessel (B). Using balloon catheters to dilate narrow segments of the internal carotid artery from far to near in sequence (C–E). Release carotid artery stent (F). The shape of the proximal attachment of the carotid stent for releasing carotid artery stents is slightly poor, and the morphology of arterial stent after release is perfect after redilation with a balloon (G). Successful recanalization of carotid artery occlusion, good imaging of the entire carotid artery, and normal blood flow velocity (H).
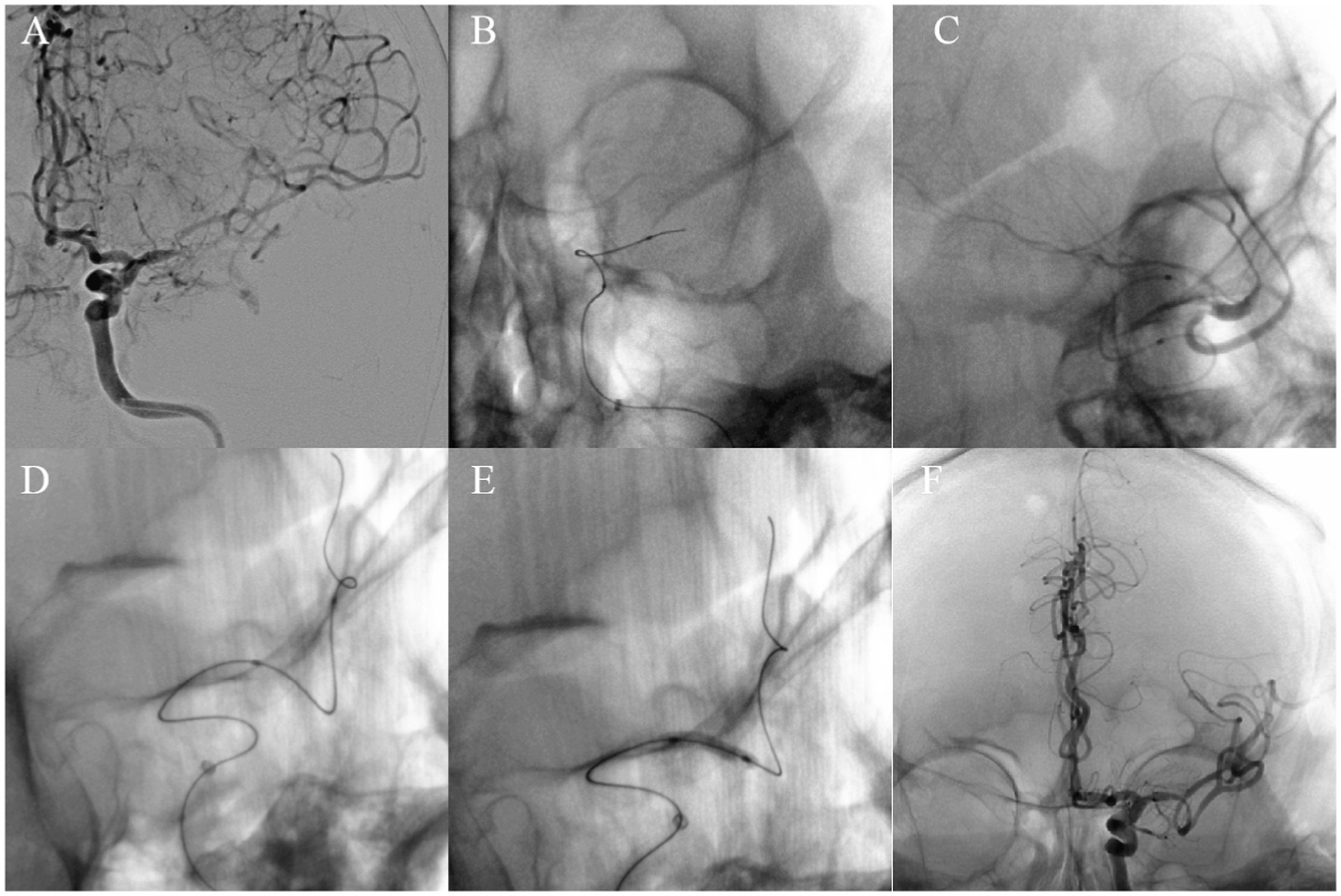
Figure 5. A 65-year-old man with left middle cerebral artery M1 segment occlusion. Digital subtraction angiography confirmed occlusion of the left MCA (A). Carefully probe the blocked section with a micro guide wire and confirm the true lumen of the blood vessel (B,C). Carefully placed the microwire beyond the M2 segment of the middle cerebral artery (D). Balloon dilation of the stenotic segment of the left middle cerebral arterye (E). Successful recanalization with good antegrade perfusion was achieved (F).
In terms of the treatment of CCAO, several previous studies have shown that the efficacy of surgical intervention is not very precise, and milestone EC-IC Bypass trial and Carotid Occlusion Surgery Study have not demonstrated any differences in fatal and non-fatal stroke between symptomatic CCAO patients in the surgical and medical groups within 2–5 years (10–12). And due to intolerance to hemodynamic fluctuations during surgery, the perioperative complications in the surgical group are relatively high (13). However, chronic CAO is associated with an annual incidence rate of stroke of 6–20%, despite aggressive medical treatment (14, 15). Intravascular recanalization of CCAO may provide the same recanalization advantage and have a higher safety advantage compared to surgical procedures, which can significantly reduce hemodynamic damage. The successful recanalization of postoperative CCAO patients can improve their cognitive function and quality of life (16–18). Unfortunately, endovascular treatment (ET) technology requires a high level of skill and experience from the surgeon, with potential complications including bleeding, pseudoaneurysm, and carotid cavernous sinus fistula (19), and the success or failure of the surgery is often difficult to predict. Therefore, preoperative evaluation of the system is crucial for identifying patients and lesion features with high success rates, which can help improve the success rate of surgery.
Up to now, experts have developed various predictive assessment scales through statistical analysis, but most of them are only targeted at patients with anterior circulation occlusion. Currently, there is a lack of predictive assessment scales suitable for patients with cerebral vascular occlusion that encompass both the anterior and posterior circulation. Especially there is relatively little research on posterior circulation occlusion.
Jin et al. proposed the application of The HRVWI score system to predict and analyze the successful recanalization of chronic internal carotid artery occlusion (CICAO) (20). Chen et al. developed a scoring system to predict the success rate of intravascular recanalization in CICAO. The predictive factors include absence of perforated stumps, reconstruction of the distal carotid artery in the communicating or ocular segment, and absence of neurological events. However, there is a certain degree of heterogeneity and bias in their research (21). On this basis, Zhou et al. improved the above scoring system and concluded that a residual stump, low levels of the digital ICA occlusion segment, and a short radiological occlusion time were identified as positive predictors of technical success. However, this prediction system is still only applicable to the carotid circulation system (22).
There is relatively little research on the opening of vertebrobasilar artery occlusion, and some scholars have discussed and analyzed it. Gao et al. demonstrated the feasibility and safety of internal veterinary art (ICVA) reanalysis (23). Zhao et al.’s study suggestions that endovascular regression for gut to chronic symptomatic astrological basic art occlusion (BAO) appear to be feasible in selected patients (24). Cai et al.’s research focuses on the treatment of chronic ventricular basic art occlusion in the starting segment (25).
Our study combines cases of the carotid artery system and the vertebrobasilar artery system for analysis, including patient baseline data, imaging characteristics, and laboratory examination data. The final prediction system is applicable to all types of CCAO cases. The final results showed that stump morphology, smoking history, duration from last neurological event (longer than 6 months or not), age, smoking history and neutral to lymphocyte ratio (NLR) were independent risk factors affecting recanalization success. And in this scoring system, we can predict the success rate of re communication based on the score.
It should be noted that there are many peculiarities in cases of vertebrobasilar artery system occlusion. For example, in patients with chronic occlusion of some vertebral arteries with no stump, we can use parallel compensatory vessels (such as the ascending carotid artery) for reverse patency, thereby ensuring the smooth completion of the surgery. However, there is no doubt that no stump is a negative impact factor on the success of the launch. This is also a limitation of this study. Supplementary Figure 1 shows one of the cases of reverse opening of the vertebral artery that we completed.
A study has found that factors affecting bleeding after mechanical thrombectomy for acute anterior circulation occlusion include NHISS score at admission, stroke history, neutrophils, lymphocytes, NLR, PLR, and FPE (26). More and more scholars are becoming enthusiastic about analyzing preoperative laboratory test data of patients in order to explore the influencing factors for predicting surgical outcomes. After occlusion of large blood vessels in the anterior circulation, ischemic brain tissue is stimulated to release various chemokines and cytokines, leading to the entry of white blood cells in the peripheral circulation into the ischemic site. Neutrophils are one of the invading cells and are correlated with the severity of the disease (27–30). Research has found that the accumulation of neutrophils in ischemic areas can exacerbate damage to brain tissue through the release of inflammatory mediators.
Meanwhile, the study also pointed out that severe damage to the blood–brain barrier increases the probability of postoperative bleeding. The interaction between neutrophils and platelets can trigger the formation of new blood clots and exacerbate vascular blockage. Neutrophils have the ability to adhere and aggregate on endothelial cells in ischemic tissue, hindering blood flow (31, 32). These research findings suggest a certain association between neutrophils and postoperative complications. In 2021, studies have indicated the impact of NLR on cerebral artery occlusion recanalization and elucidated its possible pathological mechanisms. When the NLR level is high, it indicates that the patient is likely to have a high neutrophil count or a low lymphocyte count. This situation undoubtedly increases the thrombus burden on occluded blood vessels, thereby increasing the difficulty of thrombectomy device operation and reducing the success rate of cerebral artery occlusion recanalization (33, 34). In our study, it was also confirmed that there is a correlation between NLR and the success rate of occlusive recanalization, and it can serve as a predictive factor, which helps us make relatively more accurate preoperative judgments.
Ter Schiphorst et al. pointed out that the presence of large vessel occlusions (LVO) could represent a “red flag” of PFO causality in stroke of undetermined etiology (35). Therefore, we attempted to explore whether there is a correlation between PFO and chronic occlusion and reperfusion of cerebral arteries. We conducted preoperative foam test screening for each patient, and the final results confirmed that there was no significant correlation between the two. The presence of PFO cannot predict surgical outcomes.
Although our scoring system is aimed at CCAO patients with different occlusions, the number of cases is still relatively small, especially in cases of vertebrobasilar artery occlusion. This may weaken the predictive ability of the scoring system. We still need to continue expanding case data. More prospective patients are needed in the future to validate current research results. On the other hand, for patients with occlusion of vertebral artery V1 segment, we can attempt reverse recanalization through the ascending carotid artery. Therefore, when predicting the surgical outcome of this type of patient, our application of a scoring system needs to take into account the patient’s arterial collateral compensation situation. In this study, the total number of cases with complications was 11. Considering that a relatively large data bias might occur if a subgroup analysis of complications was carried out, we decided to conduct statistical analysis after further accumulation of the sample size, so as to further enhance the clinical relevance of the research results.
In summary, CCAO is undoubtedly an important risk factor for ischemic stroke. Our study found that the morphology of occluded stumps, duration from last neurologic event (longer than 6 months or not), age, smoking history and NLR were independent predictors for successful recanalization. The scoring system we have established has high sensitivity and specificity in predicting successful reperfusion, and has a wide range of applications. However, further research is needed to verify its clinical practicality.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
The studies involving humans were approved by the Ethics Committee of Hebei General Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
XZ: Data curation, Formal analysis, Investigation, Methodology, Resources, Validation, Visualization, Writing – original draft. YL: Validation, Writing – review & editing. KY: Formal analysis, Investigation, Writing – review & editing. ZH: Investigation, Writing – review & editing. YF: Investigation, Writing – review & editing. QY: Investigation, Writing – review & editing. GX: Funding acquisition, Resources, Supervision, Writing – review & editing. PL: Funding acquisition, Methodology, Resources, Supervision, Writing – review & editing.
The author(s) declare that financial support was received for the research and/or publication of this article. This study was financially supported by grant from the Scientific and Technological Innovation 2030-Major Project Subject of “Brain Science and Brain-inspired Research” (Grant No. 2021ZD0201807) and the 2022 Medical Science Research Project Plan of Hebei Province (Grant No. 20220818).
The authors gratefully thank the reported patients for their cooperation in this research.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2025.1453841/full#supplementary-material
1. Persoon, S, Luitse, MJ, de Borst, GJ, van der Zwan, A, Algra, A, Kappelle, LJ, et al. Symptomatic internal carotid artery occlusion: a long-term follow-up study. J Neurol Neurosurg Psychiatry. (2011) 82:521–6. doi: 10.1136/jnnp.2010.208330
2. Klijn, CJ, Kappelle, LJ, Algra, A, and van Gijn, J. Outcome in patients with symptomatic occlusion of the internal carotid artery or intracranial arterial lesions: a meta-analysis of the role of baseline characteristics and type of antithrombotic treatment. Cerebrovasc Dis. (2001) 12:228–34. doi: 10.1159/000047708
3. Grubb, RL Jr, Derdeyn, CP, Fritsch, SM, Carpenter, DA, and Yundt, KDVideen TO, et al. Importance of hemodynamic factors in the prognosis of symptomatic carotid occlusion. JAMA. (1998) 280:1055–60. doi: 10.1001/jama.280.12.1055
4. Writing Group MembersMozaffarian, D, Benjamin, EJ, Go, AS, Arnett, DK, Blaha, MJ, et al. Heart disease and stroke Statistics-2016 update: a report from the American Heart Association. Circulation. (2016) 133:e38–e360. doi: 10.1161/CIR.0000000000000350
5. Wong, LK. Global burden of intracranial atherosclerosis. Int J Stroke. (2006) 1:158–9. doi: 10.1111/j.1747-4949.2006.00045.x
6. Caplan, L, Wityk, R, Pazdera, L, Chang, HM, Pessin, M, and Dewitt, L. New England Medical Center posterior circulation stroke registry II. Vascular Lesions. J Clin Neurol. (2005) 1:31–49. doi: 10.3988/jcn.2005.1.1.31
7. Zaidat, OO, Yoo, AJ, Khatri, P, Tomsick, TA, von Kummer, R, Saver, JL, et al. Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke. (2013) 44:2650–63. doi: 10.1161/STROKEAHA.113.001972
8. Shapiro, M, Becske, T, Riina, HA, Raz, E, Zumofen, D, Jafar, JJ, et al. Toward an endovascular internal carotid artery classification system. AJNR Am J Neuroradiol. (2014) 35:230–6. doi: 10.3174/ajnr.A3666
9. Kang, K, Yang, B, Gong, X, Chen, X, Gu, W, Ma, G, et al. Cerebral hemodynamic changes after endovascular recanalization of symptomatic chronic intracranial artery occlusion. Front Neurol. (2020) 11:318. doi: 10.3389/fneur.2020.00318
10. EC/IC Bypass Study Group. Failure of extracranial-intracranial arterial bypass to reduce the risk of ischemic stroke. Results of an international randomized trial. N Engl J Med. (1985) 313:1191–200. doi: 10.1056/NEJM198511073131904
11. Powers, WJ, Clarke, WR, Grubb, RL Jr, Videen TOAdams, HP Jr, Derdeyn, CP, et al. Extracranial-intracranial bypass surgery for stroke prevention in hemodynamic cerebral ischemia: the carotid occlusion surgery study randomized trial. JAMA. (2011) 306:1983–92. doi: 10.1001/jama.2011.1610
12. Grubb, RL Jr, Powers, WJ, Clarke, WR, Videen TOAdams, HP Jr, Derdeyn, CP, et al. Surgical results of the carotid occlusion surgery study. J Neurosurg. (2013) 118:25–33. doi: 10.3171/2012.9.JNS12551
13. Reynolds, MR, Grubb, RL Jr, Clarke, WR, Powers, WJ, Zipfel, GJ, Adams, HP Jr, et al. Investigating the mechanisms of perioperative ischemic stroke in the carotid occlusion surgery study. J Neurosurg. (2013) 119:988–95. doi: 10.3171/2013.6.JNS13312
14. Klijn, CJ, Kappelle, LJ, Tulleken, CA, and van Gijn, J. Symptomatic carotid artery occlusion. A reappraisal of hemodynamic factors. Stroke. (1997) 28:2084–93. doi: 10.1161/01.STR.28.10.2084
15. Flaherty, ML, Flemming, KD, McClelland, R, Jorgensen, NW, and Brown, RD Jr. Population-based study of symptomatic internal carotid artery occlusion: incidence and long-term follow-up. Stroke. (2004) 35:e349–52. doi: 10.1161/01.STR.0000135024.54608.3f
16. Lin, MS, Chiu, MJ, Wu, YW, Huang, CC, Chao, CC, Chen, YH, et al. Neurocognitive improvement after carotid artery stenting in patients with chronic internal carotid artery occlusion and cerebral ischemia. Stroke. (2011) 42:2850–4. doi: 10.1161/STROKEAHA.111.613133
17. Chen, YH, Lin, MS, Lee, JK, Chao, CL, Tang, SC, Chao, CC, et al. Carotid stenting improves cognitive function in asymptomatic cerebral ischemia. Int J Cardiol. (2012) 157:104–7. doi: 10.1016/j.ijcard.2011.10.086
18. Huang, CC, Chen, YH, Lin, MS, Lin, CH, Li, HY, Chiu, MJ, et al. Association of the recovery of objective abnormal cerebral perfusion with neurocognitive improvement after carotid revascularization. J Am Coll Cardiol. (2013) 61:2503–9. doi: 10.1016/j.jacc.2013.02.059
19. Lin, MS, Lin, LC, Li, HY, Lin, CH, Chao, CC, Hsu, CN, et al. Procedural safety and potential vascular complication of endovascular recanalization for chronic cervical internal carotid artery occlusion. Circ Cardiovasc Interv. (2008) 1:119–25. doi: 10.1161/CIRCINTERVENTIONS.108.772350
20. Jin, W, Ye, X, Chen, X, Duan, R, Zhao, Y, Zhang, Y, et al. A score system used to screen the suitability for recanalization in carotid artery occlusions. Biotechnol Genet Eng Rev. (2023) 14:1–16. doi: 10.1080/02648725.2023.2202522
21. Chen, YH, Leong, WS, Lin, MS, Huang, CC, Hung, CS, Li, HY, et al. Predictors for successful endovascular intervention in chronic carotid artery total occlusion. JACC Cardiovasc Interv. (2016) 9:1825–32. doi: 10.1016/j.jcin.2016.06.015
22. Zhou, C, Cao, YZ, Jia, ZY, Zhao, LB, Lu, SS, Shi, HB, et al. Endovascular recanalization of symptomatic chronic ICA occlusion: procedural outcomes and radiologic predictors. AJNR Am J Neuroradiol. (2023) 44:303–10. doi: 10.3174/ajnr.A7804
23. Gao, P, Wang, Y, Ma, Y, Yang, Q, Song, H, Chen, Y, et al. Endovascular recanalization for chronic symptomatic intracranial vertebral artery total occlusion: experience of a single center and review of literature. J Neuroradiol. (2018) 45:295–304. doi: 10.1016/j.neurad.2017.12.023
24. Zhao, W, Zhang, J, Song, Y, Sun, L, Zheng, M, Yin, H, et al. Endovascular recanalization for symptomatic subacute to chronic atherosclerotic basilar artery occlusion. Front Neurol. (2019) 10:1290. doi: 10.3389/fneur.2019.01290
25. Cai, X, Huang, L, Chen, X, Sun, J, and Gao, F. Endovascular revascularization of chronically occluded vertebral artery: single-center experience. Wideochir Inne Tech Maloinwazyjne. (2021) 16:211–8. doi: 10.5114/wiitm.2020.97445
26. Chen, J, Huang, C, Hong, C, Ye, L, and Yao, B. Regression analysis of bleeding factors and the correlation between FPE and NLR after mechanical thrombectomy for acute anterior circulation large vessel occlusion. Biotechnol Genet Eng Rev. (2023) 1-12:1–12. doi: 10.1080/02648725.2023.2186611
27. Hao, JH, Liu, WD, Wang, ZD, Wang, PJ, Zhang, M, Jiang, QL, et al. Retrospective analysis of mechanical thrombectomy for distal branch occlusion of middle cerebral artery. Zhonghua Yi Xue Za Zhi. (2020) 100:1240–4. doi: 10.3760/cma.j.cn112137-20191120-02531
28. Bai, X, Zhang, X, Zhang, Y, Yang, W, Wang, T, Feng, Y, et al. Mechanical thrombectomy in nonagenarians: a systematic review and meta-analysis. Transl Stroke Res. (2021) 12:394–405. doi: 10.1007/s12975-021-00894-5
29. Jang, KM, Choi, HH, Nam, TK, and Byun, JS. Clinical outcomes of first-pass effect after mechanical thrombectomy for acute ischemic stroke: a systematic review and meta-analysis. Clin Neurol Neurosurg. (2021) 211:107030. doi: 10.1016/j.clineuro.2021.107030
30. Lee, EJ, Bae, J, Jeong, HB, Lee, EJ, Jeong, HY, and Yoon, BW. Effectiveness of mechanical thrombectomy in cancer-related stroke and associated factors with unfavorable outcome. BMC Neurol. (2021) 21:57. doi: 10.1186/s12883-021-02086-y
31. Ma, C, Hui, Q, Gao, X, Xu, D, Tang, B, Pen, M, et al. The feasibility of dual-energy CT to predict the probability of symptomatic intracerebral haemorrhage after successful mechanical thrombectomy. Clin Radiol. (2021) 76:316.e9–316.e18. doi: 10.1016/j.crad.2020.12.013
32. Yen, HH, Chien, C, Lee, IH, Chen, SP, Luo, CB, Lin, CJ, et al. Application of flat-panel volume computed tomography to evaluate cerebral hemorrhage after mechanical thrombectomy of acute embolic stroke of the anterior circulation. J Comput Assist Tomogr. (2021) 45:919–25. doi: 10.1097/RCT.0000000000001203
33. Borggrefe, J, Goertz, L, Abdullayev, N, Hokamp, NG, Kowoll, CM, Onur, Ö, et al. Mechanical thrombectomy with the novel NeVa M1 stent retriever: do the drop zones represent a risk or a benefit. World Neurosurg. (2021) 148:e121-121e129. doi: 10.1016/j.wneu.2020.12.075
34. Portela de Oliveira, E, Chakraborty, S, Patel, M, Finitsis, S, and Iancu, D. Value of high-density sign on CT images after mechanical thrombectomy for large vessel occlusion in predicting hemorrhage and unfavorable outcome. Neuroradiol J. (2021) 34:120–7. doi: 10.1177/1971400920975259
Keywords: chronic cerebral artery occlusion, endovascular treatment, chronically occluded internal carotid artery, basilar artery occlusion, neutrophil-to-lymphocyte ratio
Citation: Zhang X, Li Y, Yin K, Hao Z, Fu Y, Yang Q, Xu G and Lv P (2025) Endovascular recanalization of symptomatic chronic cerebral artery occlusion: predictors for successful recanalization and perioperative complications. Front. Neurol. 16:1453841. doi: 10.3389/fneur.2025.1453841
Received: 23 July 2024; Accepted: 21 March 2025;
Published: 11 April 2025.
Edited by:
Stefano Maria Priola, Health Sciences North, CanadaReviewed by:
Bo Yang, Beijing Jiangong Hospital, ChinaCopyright © 2025 Zhang, Li, Yin, Hao, Fu, Yang, Xu and Lv. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Peiyuan Lv, cGVpeXVhbmx1MkAxNjMuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.