- Department of Neurology, Medical University of Warsaw, Warsaw, Poland
Progressive supranuclear palsy (PSP) is an atypical form of parkinsonism characterized by tauopathy, manifesting as oculomotor dysfunction, postural instability, akinesia, and cognitive/language impairments. The diagnosis and examination of PSP can be challenging, primarily due to the unclear and underexplored pathomechanisms involved, alongside absence of effective treatments. Clinical variants of PSP is the second most common form of neurodegenerative parkinsonism after Parkinson’s disease (PD). It is defined by a symmetrical akinetic-rigid syndrome (atypical parkinsonism) and vertical supranuclear gaze palsy. In contrast to PD, PSP often presents with gait instability, backward falls, and cognitive and behavioral changes at early disease stages. The classification of PSP has evolved since Richardson, Steele, and Olszewski’s initial reporting of the condition in 1963, which included a cohort of nine patients. Over the years, the definition of this disorder has evolved to encapsulate a group of patients with distinct clinical variants, notably the classical Richardson syndrome (RS) and several atypical phenotypes, each with significant implications for disease progression and quality of life (QoL). The 2017 Movement Disorder Society Diagnostic Criteria by Hoglinger et al., improved the sensitivity for detecting early and variant PSP presentations and provided more specific differential diagnoses for conditions such as PD and other forms of atypical parkinsonian syndromes. Owing to the growing interest in the disease’s progression, evaluating the QoL for patients with PSP has become crucial. This review emphasizes the significance of QoL evaluation and its feasibility for practical implications, serving as an initial foundation for future research focused on the well-being of individuals affected by PSP. Progressive supranuclear palsy (PSP) is an atypical form of parkinsonism characterized by tauopathy, manifesting as oculomotor dysfunction, postural instability, akinesia, and cognitive/language impairments. Diagnosing PSP is challenging owing to the lack of tools for differential examination. Additionally, the pathomechanism of this disease is not sufficiently understood, and no treatment is currently available. Owing to the growing interest in the disease’s progression, evaluating the quality of life (QoL) for patients with PSP has become crucial. This review emphasizes the significance of QoL evaluation and its feasibility for practical implications, serving as an initial foundation for future research focused on the well-being of individuals affected by PSP.
1 Introduction: clinical variants of PSP
Progressive supranuclear palsy (PSP) is a rare neurodegenerative parkinsonism with a prevalence of 1–18 per 100,000 compared to 1–2 per 1,000 in Parkinson’s disease (PD). It is characterized by symmetrical akinetic-rigid syndrome (atypical parkinsonism) and vertical supranuclear gaze palsy. In contrast to PD, PSP presents early with gait instability, backward falls, and cognitive and behavioral changes. Since 1963, when Richardson, Steele, and Olszewski (1) reported a series of nine patients, the definition of PSP has evolved to encompass a group of patients with distinct clinical variants. After the description of classical Richardson syndrome (RS), other specific atypical phenotypes of PSP have been discovered over the years (2). The recognition of different variants of PSP has expanded the concept into a group of several “subtypes,” with varied progression. These differences in the dynamics of patient deterioration significantly impact their quality of life (QoL).
The Movement Disorder Society Diagnostic Criteria, revised by Hoglinger et al. (4), has enhanced the sensitivity for detecting early and variant presentations of PSP, offering more precise differential diagnoses than the previous guidelines from the National Institute of Neurological Disorders and Stroke and the Society for PSP (NINDS-SPSP) (3). These guidelines emphasize four core functional domains: postural instability [P], oculomotor dysfunction [O], akinesia [A], and cognitive dysfunction [C]. By utilizing combinations of these domains, healthcare professionals can establish a diagnostic spectrum, classifying patients into three categories: probable PSP, possible PSP, and suggestive of PSP. Additional clinical indicators, such as levodopa resistance, dysphagia, spastic dysarthria, and photophobia, as well as specific radiological findings—such as predominant midbrain atrophy or hypometabolism and postsynaptic striatal dopaminergic degeneration—support the diagnostic process also play supportive roles in diagnosis. Among other symptoms, cognitive and behavioral abnormalities, including dysexecutive syndrome, bradyphrenia, impulsivity, disinhibition, perseveration, and reduced phonemic verbal fluency, can also complicate the assessment process. Currently, a neuropathological examination remains the only definitive diagnostic method for PSP (4).
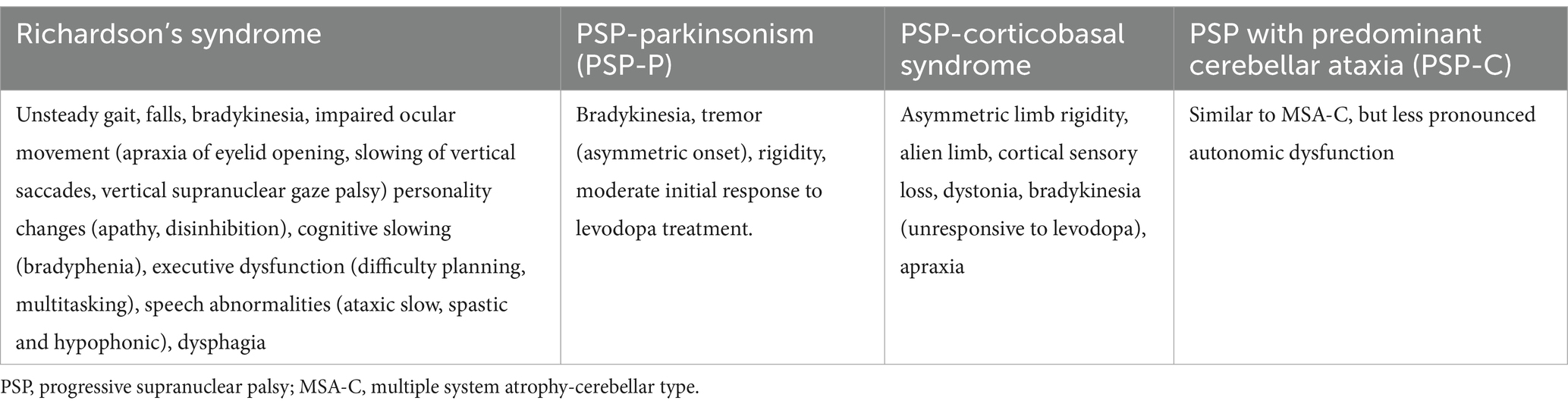
Differentiating various PSP phenotypes is essential given the prognostic differences and implications for future drug trials. PSP–Richardson syndrome (PSP-RS) encompasses the characteristics originally described by Steele et al., where patients typically present with relatively early falls, cognitive dysfunction, gaze abnormalities, and postural instability (lurching and falls backwards) in the initial stages of the disease (5). PSP-RS is the most common variant, accounting for 76% of autopsy-confirmed cases in a recent series (6), and is associated with a poorer prognosis compared to the PSP-parkinsonism (PSP-P) phenotype, featuring an average disease duration of 5.9 years (ranging from 5 to 8 years) and an average age of death at 72.1 years (7). Conversely, PSP-P is characterized by primary asymmetrical tremor, non-axial dystonia, and early bradykinesia, with a notable response to levodopa therapy. These features resemble those of idiopathic PD. Patients with PSP-P tend to have a longer survival rate (9.1 years) compared to those with PSP-RS. However, the overlap in clinical characteristics between these two variants presents a significant diagnostic challenge. Neuropsychological assessments, such as those utilizing the Frontal Assessment Battery (FAB), can aid in identifying the two most common PSP variants (8). Moreover, due to insufficient data on clinical and pathological patterns, less common variants of PSP have not yet been formally detailed in the MDSPSP criteria (9); consequently, their low incidence means these variants are described only briefly in contemporary literature, typically in case reports or small case series. The most common variants of the disease are outlined in Table 1.
Despite significant progress in understanding PSP, achieving a definitive diagnosis still hinges on neuropathological examination. Achieving early and reliable diagnosis still remains a significant clinical challenge driven by both patient demands for ante-mortem confirmation and clinicians’ needs for effective therapeutic trials allocation. As a result, there is an urgent need for improved diagnostic tools. At present, no disease-modifying therapies are available for PSP, and only a limited number of treatments have proven effective. Levodopa can provide symptomatic relief, but its efficacy is typically limited and short-lived in PSP-P patients, with rare benefits seen in those with PSP-RS (10); the impact of this treatment on overall disease duration remains unclear. Physical therapy may yield measurable improvements on clinical rating scales (5). While apraxia of eyelid opening may be improved by pretarsal Botulinum toxin injections, these interventions do not address the major clinical symptoms that ultimately lead to fatality in all PSP cases.
PSP faces significant challenges in clinical examination due to the low specificity of in vivo diagnostic tools and the lack of evidence-based methods. There is growing interest in exploring other aspects of the disease, such as the quality of life, which is particularly relevant given the pronounced deterioration and incurable nature of PSP. This review aims to synthesize current knowledge regarding the methods of evaluation of QoL in PSP, using scales specifically dedicated for this clinical entity, as well as those generally applicable to parkinsonisms. Additionally, the significance of QoL assessment was examined in the context of its limitations and future perspectives to enhance understanding and intervention strategies.
2 Methods
We performed a search of the PubMed database for studies published from the date of inception of the database up to August 2024, searching for the following key words: “Progressive Supranuclear Palsy,” “Quality of Life,” and their abbreviations; and “movement disorders.”
3 Importance of QoL studies
Combining preclinical and clinical findings with QoL analysis enhances our understanding of the disease’s natural progression and a more precise identification of progression factors. Considered a vital adjunct to clinical data (11), QoL studies provide insights into neurodegenerative diseases beyond PD, which have been insufficiently documented largely due to the low prevalence of parkinsonian syndromes other than PD, and thus the unavailability of large cohorts (12). Gathering subjective data about patients’ well-being and other facets of their lives enables healthcare providers to deliver more effective and personalized clinical care. This approach has garnered endorsements from the Food and Drug Administration (FDA) and the World Health Organization (WHO) as vital for ongoing care improvement and future drug development (13). By prioritizing the patient’s perspective on disease progression, we can enhance management strategies. Given that many patients exhibit a lack of insight into their functional deficits (anosognosia)—a phenomenon well studied in extrapyramidal disorders, including PSP and Alzheimer’s disease (14)—numerical scales for assessing progression could prove valuable for accurately evaluating patient needs.
QoL is a broad, multidimensional concept that reflects patients’ subjective perceptions regarding how their disease affects their overall well-being. It encompasses physical, mental, emotional, and social dimensions. Self-reported tools for QoL assessment, which can be generic (applicable for numerous diseases, i.e., universal) or disease-specific (ie. disease oriented), are continually being developed for clinical studies and practice to quantify disease impact on patients’ everyday lives, treatment efficacy, and health policy management (15, 16). Some QoL aspects, such as symptom perception, self-image, and life satisfaction—including social and economic factors—are inherently subjective; however, others can be objectively measured, including clinical manifestations of the disease and patients’ financial and social situations. The instruments presented below include both subjective and objective indicators. While data on QoL in PSP is less comprehensive compared to sporadic PD (17), recent years have seen an uptick in interest surrounding QoL in Parkinsonism, and some tools for capturing QoL have been developed, mostly based on quantitative scales (18).
In addition to predominant motor symptoms, non-motor symptoms (NMSs) significantly increase morbidity and disability in PD and other parkinsonian disorders, considerably affecting the QoL for patients and their caregivers (19, 20). Researchers have observed variable patterns in the prevalence of specific NMS that differentially impact individuals’ lives. A study involving 50 patients with PSP compared to 100 patients with PD identified insomnia, fatigue, and urinary dysfunction as the most common NMSs in PSP (21). Other studies have also highlighted gastrointestinal problems and fatigue as prevalent issues (22). The authors of the largest PSP cohort study (23) found that the most prevalent domains in both the PSP-RS and PSP-P subgroups were sleep/fatigue and sexual function; however, mood/cognition was severely impaired in RS, while gastrointestinal issues were more pronounced in PSP-P subtype. Despite some methodological limitations—such as the absence of case–control design and lack of comparisons to other parkinsonian disorders or healthy controls—these findings indicated issues that substantially contributed to a decrease in QoL and could be amenable to symptomatic treatment if recognized early in the disease trajectory.
3.1 Scales in parkinsonism (including PSP) for QoL evaluation
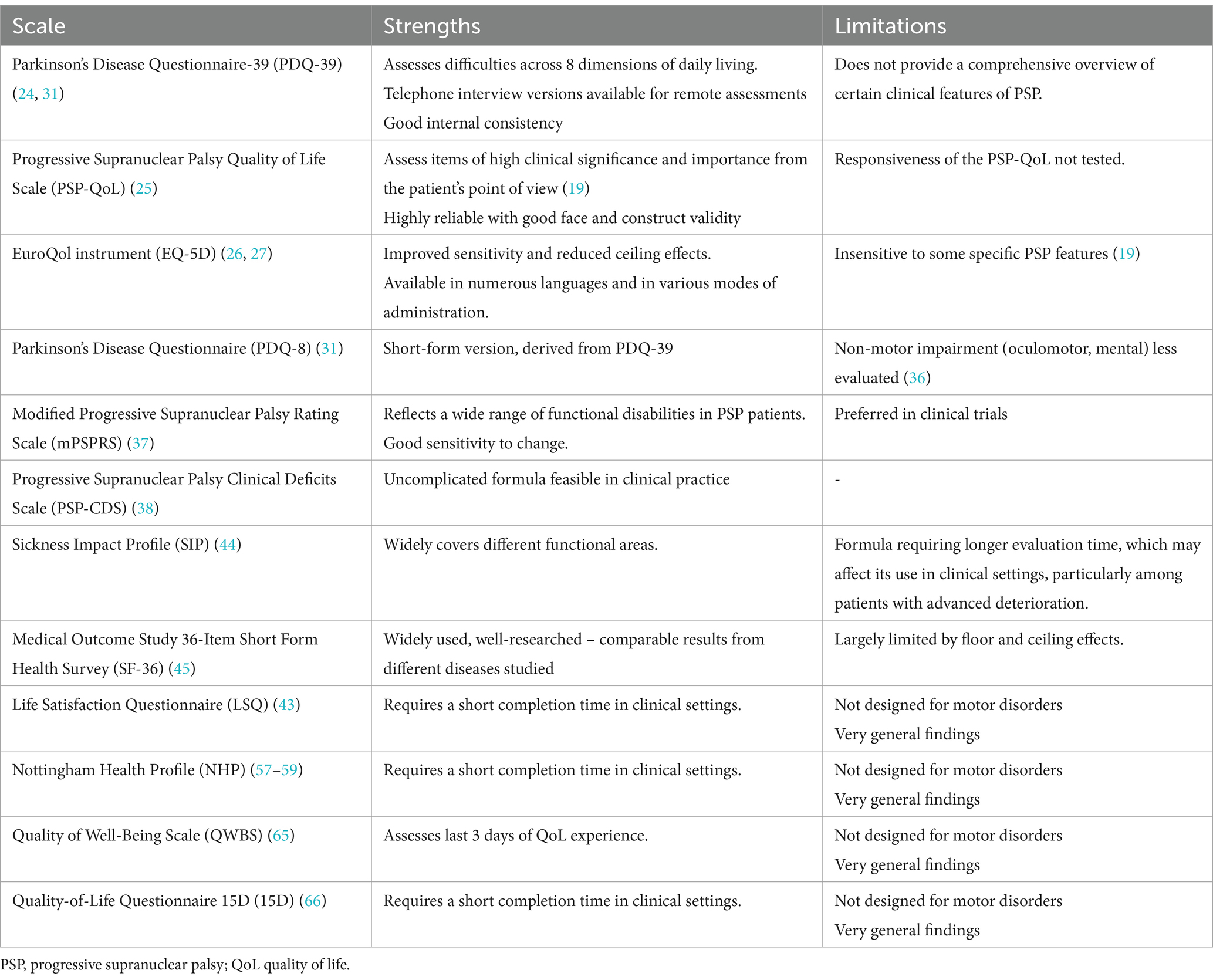
Widely used tools for QoL assessment in patients with PSP include the Parkinson’s Disease Questionnaire-39 (PDQ-39) (24), the Progressive Supranuclear Palsy Quality of Life Scale (PSP-QoL) (25), and the EuroQol instrument (EQ-5D) (26, 27). Although the PDQ-39 was primarily designed for PD, it can also be utilized for evaluating atypical parkinsonism conditions, including PSP. However, since it was not tailored for PSP, it fails to address certain prevalent symptoms of the disorder, such as muddled thinking, ocular motor dysfunction, confusion, and apathy (28).
The validation of these instruments for patients with PSP appears to be limited, as they do not encompass the unique aspects of the disease (including several aforementioned symptoms), which may lead to an underestimation of associated health problems (24).
3.2 Scales dedicated to PSP for QoL evaluation
The PSP-QoL scale was specifically developed to assess the distinct physical and mental domains experienced by patients with PSP. This scale comprises 45 patient-rated items that evaluate difficulties related to mental and physical tasks within the preceding month. It remains the only tool sufficiently validated for QoL assessment in this disease population (25). Its primary disadvantage is the time-consuming nature of its completion, which restricts its applicability in clinical settings; hence, a more streamlined QoL tool is required. Notably, this scale was developed using a large cohort of patients with PSP, focusing on crucial clinical features and including items with good discriminative power for different disease stages, indicating that the tool has good construct validity and high reliability. As such, it is recommended for use as a patient-reported outcome measure in clinical trials (25). However, the study associated with this tool underrepresented late-stage patients (as they were unable to complete the survey), raising questions about the tool’s applicability to those in advanced stages of the disease. Researchers did not differentiate between probable and possible PSP, as participants were diagnosed outside the study’s centers. Further validation is encouraged in diverse populations. In a study by Patnelyat et al. (29, 30) patients with PSP were evaluated to establish correlations between the PSP Rating Scale and the PSP-QoL. While the study indicated the PSP-QoL as a feasible method of self-assessment and revealed significant associations with the PSP Rating Scale, the authors cautioned that these correlations might differ between patients with Richardson syndrome and those with non-Richardson syndrome. Somewhat addressing the limitations of the PSP-QoL, the PDQ-8—a condensed version of eight representative questions from the PDQ-39 (31)—has gained traction in PD management, including clinical trials (32). However, its effectiveness specifically within the PSP population requires further investigation. In a larger cohort study (n = 132), Xin-Yi et al. (33) found that the PDQ-8 correlated well with the PSP-QoL in assessing QoL, indicating strong relevance of the PDQ-8 with each item of PSP-QoL. The authors highlighted that among the short scales used for QoL assessment in patients with parkinsonian disorders, the PDQ-8 was the most comparable to the PSP-QoL. The most significantly affected domains identified were mobility, activities of daily life, cognition, and communication—elements critical not only for the patients themselves but also for their caregivers in terms of recognizing levels of independence.
Further analysis of the impact of several variables (e.g., disease duration, sex, NMSS, ESS, GDS, and MMSE) on the PSP-QoL total score showed that longer disease duration, depression (assessed using the Geriatric Depression Scale [GDS]), and daytime sleepiness (assessed by the ESS) were the most important determinants of QoL. To determine QoL, the established connections between GDS scores, NMSS, PSP Rating Scale (PSPrs), and ESS scores were all confirmed to be crucial for QoL assessment. Similar findings were noted in earlier studies of multiple system atrophy (MSA-P) and PSP (34). The simplicity of the PDQ-8 contributes to a high completion rate, with favorable feedback from patients. Furthermore, detailed comparisons between the two patient groups (PSP-RS vs. PSP non-RS) indicate a worse clinical course of the disease in patients with RS variant, particularly evident in both motor and non-motor symptoms (including deterioration in mood and cognitive function). A strong correlation between the PDQ-39 and PSP-QoL subscales (physical and mental) was also confirmed by Schrag et al. (25), highlighting the relationship between PSPrs and PSP-QoL along with the relevance of non-motor symptoms in patients’ QoL (29). Based on these findings, utilizing both assessment instruments is recommended.
Wiblin et al. emphasized the significance of particular aspects of social life—such as social network strength, family support, and personal disease insight—for the QoL of patients with PSP (17). Among the 19 patient-caregiver pairs studied, reduced QoL was found to be associated with speech difficulties, social life restrictions, and disease stigma. Although their results are based on semistructured interviews rather than formal QoL assessment tools discussed above, they pointed out that further evaluations using standardized scales would allow objective comparisons of patients’ well-being.
The Modified Progressive Supranuclear Palsy Rating Scale (PSPRS) has been devised to quantify and track the severity of major symptoms associated with PSP. In this questionnaire, a physician assesses each of the 28 items categorized into six domains: daily activities (based on patient history), mentation, bulbar symptoms, oculomotor function, limb motor skills, and disturbances in gait/midline (based on examination) (35).
Further evaluations of the tool indicate areas for refinement; for example, some items in the questionnaire reflect critical disease aspects, yet calculating maximum scores for these items does not effectively capture variances in clinical severity. In addition, some of the analyzed items were found to be interrelated or overlapping, indicating they may not need to be evaluated separately. Some items and their scores were also classified as minimally changeable over the course of disease progression, failing to accurately represent changes in a patient’s status (36). For these reasons, the removal of items such as tremors, limb dystonia, and dysphagia has been proposed to improve the consistency of the scale.
A modified version of the PSPRS, referred to as the mPSPRS, was also designed by Grotch et al. (37) by eliminating the following 14 items from the PSPRS that were identified as insensitive or overlapping: Irritability; sleep difficulty, grasping/imitative/utilizing behavior, voluntary left and right saccades, finger tapping, toe tapping, postural kinetics, or rest tremor. This simplification makes patient evaluation less time-consuming while yielding outcomes comparable in metric power to that of the original PSPRS. This modified version was evaluated by experts from the European section of the International Parkinson and Movement Disorder Society. A comparison between the PSPRS and mPSPRS was performed based on data from 86 participants in the TAUROS trial, which examined both baseline and 52-week follow-up data. They reported a strong positive correlation between the mPSPRS and PSPRS total scores. Some differences were observed between patients with RS and non-RS; however, the implications of these differences remain unclear. Given the equivalence, the authors recommend the mPSPRS for disease monitoring due to its demonstrated sensitivity to change and practicality in clinical practice (29).
Researchers highlight the high dropout rate among study participants, attributed to the rapid progression of the disease, which may influence their results. Nevertheless, they assumed that the mPSPRS could effectively depict changes within intervals as short as 52 or even 26 weeks. They also emphasized that the scale does not account for factors beyond emotional incontinence, despite evidence that problems such as bradyphrenia, disorientation, and behavioral changes play a key role in the mental sphere of the disease. Additionally, the study faced challenges in distinguishing between Richardson’s and non-RS forms of PSP, as some recruited patients were diagnosed according to the NINDS-SPSP diagnostic criteria; therefore, the sensitivity to changes in the mPSPRS may vary across these two subpopulations. In rarer forms of PSP phenotypes, a larger sample size would be necessary to detect any changes in mPSPRS scores, and further prospective studies are recommended to confirm the effectiveness of the tool. However, due to its ease of implementation and demonstrated sensitivity to change over time, the authors advocate for the mPSPRS as a valuable resource for routine clinical practice, particularly for assessing treatment effects in forthcoming disease-modifying trials.
The Progressive Supranuclear Palsy Clinical Deficits Scale (PSP-CDS) (38) comprises seven clinical domains: Akinesia-rigidity, Bradyphrenia, Communication, Dysphagia, Eye movements, Finger dexterity, and Gait & balance. Each domain is scored from 0 to 3, indicating no, mild, moderate, or severe deficits. Piot et al. found a good-to-excellent correlation between the total scores from the PSP-CDS and the clinical scales previously discussed for both PSP-RS and variant PSP (vPSP) phenotypes. To date, the PSP-CDS has been evaluated as sensitive, reliable, and easily applicable in both research and clinical contexts.
3.3 Other generic scales
In addition to the previously described tools, various generic questionnaires designed for patients PD are also applicable to other conditions. These include the Sickness Impact Profile (SIP), the Medical Outcome Study 36-Item Short Form Health Survey (SF-36), the Life Satisfaction Questionnaire (LSQ), the EuroQol EQ-5D, the WHOQOL-BREF, and the Quality of Well-Being Scale (QWBS) (39–43). All of these tools have been proven to be valid and reliable in assessing PD (41).
The Sickness Impact Profile (SIP) questionnaire was developed to assess 12 areas of functioning at the time of study that are sensitive to disease progression and may not be accurately reflected in other scales (e.g., SF-36, EQ-5D). However, the SIP’s extensive length (comprising 136 items) leads to a completion time of approximately 30 min. The SIP has also shown associations with key constructs relevant to PD, such as the Hoehn and Yahr scale, the Unified Parkinson’s Disease Rating Scale (UPDRS), and the SF-36 (44).
In contrast, the SF-36 is a shorter tool that requires approximately 9 min to complete and evaluates eight aspects of QoL over the 4 weeks preceding the survey. It is particularly effective in predicting disease progression but does possess certain upper and lower thresholds (45). The SF-36 demonstrates good reliability and discriminative validity (41, 46–49) and has been shown to respond partially to changes over time (50) and following intervention (30). One study indicated that it was more responsive than both the PDQ-39 and PDQUALIF (51).
The Life Satisfaction Questionnaire (LSQ) assesses general satisfaction and satisfaction with eight specific life domains, with responses rated on a six-point scale. The EQ-5D scale, with three levels of evaluation, is primarily designed to inform healthcare decision making and detects QoL changes across five health areas, including self-esteem during the study period. While the EQ-5D has a brief completion time of approximately 3 min, it has faced criticism for lacking sensitivity to QoL changes compared to other instruments (43). Nevertheless, some studies have established its correlation with UPDRS and SF-36 scores (52) and its capacity to discriminate between different stages of PD stages (53), as well as to respond to therapeutic interventions (54–56).
The Nottingham Health Profile (NHP) comprises 38 items requiring yes/no responses, covering eight domains. This tool has undergone validation in various populations (57, 58) and has been tested specifically in patients with PD, yielding acceptable validity in this cohort, supported by good internal consistency and a unidimensional factor structure (59). However, the stability of the NHP, as assessed through test–retest procedures, has not yet been evaluated in patients with PD. Unfortunately, floor effects were noticeable in the PDQ-39 results (60). Nevertheless, the NHP is responsive to interventions such as deep brain stimulation (61, 62) and demonstrates changes over time (63, 64).
The QWB system evaluates physical activity, mobility, social activity, and 27 symptoms, categorizing patients into one of 43 functional levels. The assessment is advised to be conducted with the assistance of trained professionals, taking approximately 10–15 min to complete. A specialized version tailored for patients undergoing deep brain stimulation treatment, known as the Questions on Life Satisfaction–Deep Brain Stimulation (QLS-DBS) module, has also been developed. Reports indicate moderate to high convergent validity of the QLS-MD module with the SF-36 and EQ-5D, while moderate convergent validity has been established for the QLSDBS (65).
The Quality-of-Life Questionnaire 15D (15D) comprises 15 questions, each representing 15 distinct dimensions, with five scoring options per question. Although several non-PD populations have indicated good psychometric properties, in the context of PD, the 15D has only undergone partial validation, with one study reporting correlations with the PDQ-39 and UPDRS scores for sections II and III (66).
Among the questionnaires developed exclusively for patients with PD, in addition to the PDQ-39 and PDQL, the PDQUALIF PIMS is a lesser-used questionnaire. This tool contains 32 domain-specific items along with one global item and features seven subscales. It includes many non-motor items, such as autonomic dysfunction, fatigue, sleep disturbances, and sexual function, and has demonstrated sensitivity to changes in clinical trials (67). It is believed that the QoL scales provide greater utility in evaluating the effectiveness of rehabilitation, pharmacological treatments, or neurosurgical interventions in patients compared to other assessment instruments (16).
Table 2 summarizes some strengths and limitations associated with these various assessment tools.
4 Limitations
The evaluation of the QoL of patients with PSP is affected by various limitations. Firstly, many of the aforementioned studies were primarily based on clinical examinations, which enabled only probable or possible diagnoses. Neuropathological verification, which provides the possibility of obtaining a definite diagnosis, is rarely performed following the death of patients who have undergone QoL assessments. The relatively rapid progression of PSP and the short life expectancy following diagnosis complicate the characterization of the disease, which is complicated by difficulties in examination of patients with early stage PSP and the limited access to patients with advanced-stage PSP owing to significant cognitive and motor disability. Additionally, owing to the boundaries in the clinical evaluation of patients with advanced-stage PSP, much of the available information stems predominantly from caregivers’ perspectives. Additionally, some studies reviewed herein were conducted prior to the release of the most recent diagnostic criteria established by Hoglinger et al. (4), which may not be as effective in diagnosing patients exhibiting non-Richardson syndrome. PSP being a rare disease makes the interpretation of the statistical outcomes of studies, especially the single-center studies, questionable in the context of the generalization of the results. Despite the notable differences in the disease progression of the two major subtypes—PSP-RS and PSP-P—some studies treat the PSP cohort as a homogeneous group, which may undermine the outcomes of these studies. The COVID-19 pandemic has imposed additional limitations on the examination of patients with significant motor disabilities, such as those seen in PSP. Among other limitations, owing due to limited cooperation with patients with PSP, the assessment of QoL may rely on isolated evaluations and do not allow for trend analyses.
5 Summary and perspectives
Based on data from the Adelphi PSP Disease Specific Programme™, a cross-sectional study including 242 patients, their families, and neurologists, Pillas et al. (68), highlighted the substantial burden of disease experienced by patients with PSP, their caregivers, and healthcare systems across all disease phenotypes. In this study, 67–100% of patients across various phenotypes exhibited moderate-to-severe disease severity at the time of enrollment, necessitating care from multiple healthcare professionals and constant care from a minimum of one caregiver. Despite minor statistical limitations—particularly concerning the representation of diverse patient populations and geographical variations—the authors underline the growing involvement of family and healthcare workers in managing disease progression. They also emphasize the pressing need for comprehensive patient management strategies applicable to all phenotypic manifestations of the disease. Adopting an inter-professional approach, healthcare professionals with family support may influence the QoL of patients with PSP (82).
In conclusion, PSP is regarded as an under-recognized and under-researched disease; thus, patients’ multifaceted needs often go unmet. It is recommended that a direct diagnostic journey and systematic follow-up be implemented at specialized movement disorder centers, where individualized education for patients and their caregivers can be provided, which may be potentially affect their QoL. Given the minimal response to symptomatic treatments, rapid disease progression, and short life expectancy, QoL should remain a focal point of attention. As the pathological mechanisms underlying atypical parkinsonism remain unknown, there is a pressing need for further research in this area to explore potential therapeutic interventions and address current patient care requirements. Additionally, more research is warranted regarding QoL, especially within the context of treatments evaluated in clinical trials.
Author contributions
MM: Conceptualization, Formal analysis, Investigation, Project administration, Validation, Writing – original draft, Writing – review & editing. NM-A: Formal analysis, Investigation, Writing – original draft, Writing – review & editing. PA: Formal analysis, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work is based on internal funds.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Richardson, JC, Steele, J, and Olszewski, J. Supranuclear optalmoplegia, pseudobulbar palsy, nuchal dystonia and dementia. A clinical report on eight cases of "Heterogenous system degeneration". Trans Am Neurol Assoc. (1963) 88:25–9.
2. Lopez, G, Bayulkem, K, and Hallett, M. Progressive supranuclear palsy (PSP): Richardson syndrome and other PSP variants. Acta Neurol Scand. (2016) 134:242–9. doi: 10.1111/ane.12546
3. Respondek, G, Grimm, MJ, Piot, I, Arzberger, T, Compta, Y, Englund, E, et al. Movement Disorder Society-endorsed progressive Supranuclear palsy study group. Validation of the movement disorder society criteria for the diagnosis of 4-repeat tauopathies. Mov Disord. (2020) 35:171–6. doi: 10.1002/mds.27872
4. Höglinger, GU, Respondek, G, Stamelou, M, Kurz, C, Josephs, KA, Lang, AE, et al. Movement Disorder Society-endorsed PSP Study Group. Clinical diagnosis of progressive supranuclear palsy: The movement disorder society criteria. Mov Disord. (2017) 32:853–864. doi: 10.1002/mds.26987
5. Williams, DR, de Silva, R, Paviour, DC, Pittman, A, Watt, HC, Kilford, L, et al. Characteristics of two distinct clinical phenotypes in pathologically proven progressive supranuclear palsy: Richardson's syndrome and PSP-parkinsonism. Brain. (2005) 128:1247–58. doi: 10.1093/brain/awh488
6. Respondek, G, Stamelou, M, Kurz, C, Ferguson, LW, Rajput, A, Chiu, WZ, et al. The phenotypic spectrum of progressive supranuclear palsy: a retrospective multicenter study of 100 definite cases. Mov Disord. (2014) 29:1758–66. doi: 10.1002/mds.26054
7. Coyle-Gilchrist, IT, Dick, KM, Patterson, K, Vázquez Rodríquez, P, Wehmann, E, Wilcox, A, et al. Prevalence, characteristics, and survival of frontotemporal lobar degeneration syndromes. Neurology. (2016) 86:1736–43. doi: 10.1212/WNL.0000000000002638
8. Alster, P, Migda, B, Madetko, N, Duszyńska-Wąs, K, Drzewińska, A, Charzyńska, I, et al. The role of frontal assessment battery and frontal lobe single-photon emission computed tomography in the differential diagnosis of progressive Supranuclear palsy variants and Corticobasal syndrome-a pilot study. Front Neurol. (2021) 12:630153. doi: 10.3389/fneur.2021.630153
9. Ali, F, Botha, H, Whitwell, JL, and Josephs, KA. Utility of the movement disorders society criteria for progressive Supranuclear palsy in clinical practice. Mov Disord Clin Pract. (2019) 6:436–9. doi: 10.1002/mdc3.12807
10. Lang, AE . Treatment of progressive supranuclear palsy and corticobasal degeneration. Mov Disord. (2005) 20:S83–91. doi: 10.1002/mds.20545
11. Merkies, IS, Schmitz, PI, van der Meché, FG, Samijn, JP, and van Doorn, PA. Inflammatory neuropathy cause and treatment (INCAT) group. Quality of life complements traditional outcome measures in immune-mediated polyneuropathies. Neurology. (2002) 59:84–91. doi: 10.1212/wnl.59.1.84
12. Meissner, WG, Foubert-Samier, A, Dupouy, S, Gerdelat-Mas, A, Debs, R, Marquant, F, et al. Assessment of quality of life with the multiple system atrophy health-related quality of life scale. Mov Disord. (2012) 27:1574–7. doi: 10.1002/mds.25174
13. Maritz, R, Aronsky, D, and Prodinger, B. The international classification of functioning, disability and health (ICF) in electronic health records. A systematic literature review. Appl Clin Inform. (2017) 8:964–80. doi: 10.4338/ACI-2017050078
14. Jost, ST, Ray Chaudhuri, K, Ashkan, K, Loehrer, PA, Silverdale, M, Rizos, A, et al. Subthalamic stimulation improves quality of sleep in Parkinson disease: a 36-month controlled study. J Parkinsons Dis. (2021) 11:323–35. doi: 10.3233/jpd-202278
15. Karimi, M, and Brazier, J. Health, health-related quality of life, and quality of life: what is the difference? PharmacoEconomics. (2016) 34:645–9. doi: 10.1007/s40273-016-0389-9
16. Martinez-Martin, P, Jeukens-Visser, M, Lyons, KE, Rodriguez-Blazquez, C, Selai, C, Siderowf, A, et al. Health-related quality-of-life scales in Parkinson's disease: critique and recommendations. Mov Disord. (2011) 26:2371–80. doi: 10.1002/mds.23834
17. Wiblin, L, Durcan, R, Lee, M, and Brittain, K. The importance of connection to others in QoL in MSA and PSP. Parkinsons Dis. (2017) 2017:1–9. doi: 10.1155/2017/5283259
18. Schrag, A, Geser, F, Stampfer-Kountchev, M, Seppi, K, Sawires, M, Köllensperger, M, et al. Health-related quality of life in multiple system atrophy. Mov Disord. (2006) 21:809–15. doi: 10.1002/mds.20808
19. Ou, R, Song, W, Wei, Q, Chen, K, Cao, B, Hou, Y, et al. Characteristics of nonmotor symptoms in progressive Supranuclear palsy. Parkinsons Dis. (2016) 2016:9730319. doi: 10.1155/2016/9730319
20. Lee, CN, Kim, M, Lee, HM, Jang, JW, Lee, SM, Kwon, DY, et al. The interrelationship between non-motor symptoms in atypical parkinsonism. J Neurol Sci. (2013) 327:15–21. doi: 10.1016/j.jns.2013.01.034
21. Radicati, FG, Martinez Martin, P, Fossati, C, Chaudhuri, KR, Torti, M, Rodriguez Blazquez, C, et al. Non motor symptoms in progressive supranuclear palsy: prevalence and severity. NPJ Parkinsons Dis. (2017) 3:35. doi: 10.1038/s41531-017-0037-x
22. Colosimo, C, Morgante, L, Antonini, A, Barone, P, Avarello, TP, Bottacchi, E, et al. Non-motor symptoms in atypical and secondary parkinsonism: the PRIAMO study. J Neurol. (2010) 257:5–14. doi: 10.1007/s00415-009-5255-7
23. Chaithra, SP, Prasad, S, Holla, VV, Stezin, A, Kamble, N, Yadav, R, et al. The non-motor symptom profile of progressive Supranuclear palsy. J Mov Disord. (2020) 13:118–26. doi: 10.14802/jmd.19066
24. Schrag, A, Selai, C, Davis, J, Lees, AJ, Jahanshahi, M, and Quinn, N. Health-related quality of life in patients with progressive supranuclear palsy. Mov Disord. (2003) 18:1464–9. doi: 10.1002/mds.10583
25. Schrag, A, Selai, C, Quinn, N, Lees, A, Litvan, I, Lang, A, et al. Measuring quality of life in PSP: the PSP-QoL. Neurology. (2006) 67:39–44. doi: 10.1212/01.wnl.0000223826.84080.97
26. Xiao, Y, Zhang, L, Wei, Q, Ou, R, Hou, Y, Liu, K, et al. Health-related quality of life in patients with multiple system atrophy using the EQ-5D-5L. Brain Behav. (2022) 12:e2774. doi: 10.1002/brb3.2774
27. Schrag, A, Sheikh, S, Quinn, NP, Lees, AJ, Selai, C, Mathias, C, et al. A comparison of depression, anxiety, and health status in patients with progressive supranuclear palsy and multiple system atrophy. Mov Disord. (2010) 25:1077–81. doi: 10.1002/mds.22794
28. Santangelo, G, Cuoco, S, Pellecchia, MT, Erro, R, Barone, P, and Picillo, M. Comparative cognitive and neuropsychiatric profiles between Parkinson's disease, multiple system atrophy and progressive supranuclear palsy. J Neurol. (2018) 265:2602–13. doi: 10.1007/s00415-018-9038-x
29. Pantelyat, A, Higginbotham, L, Rosenthal, L, Lanham, D, Nesspor, V, AlSalihi, M, et al. Association of Progressive Supranuclear Palsy Rating Scale with progressive Supranuclear palsy quality of life scale. Neurodegener Dis. (2020) 20:139–46. doi: 10.1159/000514519
30. Siderowf, A, Jaggi, JL, Xie, SX, Loveland-Jones, C, Leng, L, Hurtig, H, et al. Long-term effects of bilateral subthalamic nucleus stimulation on health-related quality of life in advanced Parkinson's disease. Mov Disord. (2006) 21:746–53. doi: 10.1002/mds.20786
31. Peto, V, Jenkinson, C, and Fitzpatrick, R. PDQ-39: a review of the development, validation and application of a Parkinson's disease quality of life questionnaire and its associated measures. J Neurol. (1998) 245:S10–4. doi: 10.1007/pl00007730
32. Landers, MR, and Ellis, TD. A Mobile app specifically designed to facilitate exercise in Parkinson disease: single-cohort pilot study on feasibility, safety, and signal of efficacy. JMIR Mhealth Uhealth. (2020) 8:e18985. doi: 10.2196/18985
33. Li, XY, Chen, MJ, Liang, XN, Yao, RX, Shen, B, Wu, B, et al. Progressive Supranuclear palsy Neuroimage initiative (PSPNI). PDQ-8: a simplified and effective tool measuring life quality in progressive Supranuclear palsy. J Parkinsons Dis. (2023) 13:83–91. doi: 10.3233/JPD-223553
34. He, SJ, Liu, ZY, Yang, YJ, Shen, C, Du, YJ, Zhou, XY, et al. Considerations before initiating therapy in parkinsonism: basing on the quality of life. J Neurol. (2019) 266:3119–25. doi: 10.1007/s00415-019-09545-0
35. Golbe, LI, and Ohman-Strickland, PA. A clinical rating scale for progressive supranuclear palsy. Brain. (2007) 130:1552–65. doi: 10.1093/brain/awm032
36. Hall, DA, Stebbins, GT, Litvan, I, Bordelon, Y, Riley, DE, Leverenz, J, et al. Clinimetric analysis of the motor section of the progressive Supranuclear palsy rating scale: reliability and factor analysis. Mov Disord Clin Pract. (2015) 3:65–7. doi: 10.1002/mdc3.12243
37. Grötsch, MT, Respondek, G, Colosimo, C, Compta, Y, Corvol, JC, Ferreira, J, et al. Study group, the ProPSP study group, and the Movement Disorder Society-endorsed PSP study group. A modified progressive Supranuclear palsy rating scale. Mov Disord. (2021) 36:1203–15. doi: 10.1002/mds.28470
38. Piot, I, Schweyer, K, Respondek, G, Stamelou, M, DescribePSP study group; ProPSP study group; MDS-endorsed PSP study groupSckopke, P, et al. The progressive Supranuclear palsy clinical deficits scale. Mov Disord. (2020) 35:650–61. doi: 10.1002/mds.27964,
39. Canter, GJ, De La Torre, R, and Mier, M. A method for evaluating disability in patients with Parkinson's disease. J Nerv Ment Dis. (1961) 133:143–7. doi: 10.1097/00005053-196108000-00010
40. Diamond, SG, and Markham, CH. Evaluating the evaluations: or how to weigh the scales of parkinsonian disability. Neurology. (1983) 33:1098–9. doi: 10.1212/wnl.33.8.1098
41. Jenkinson, C, Peto, V, Fitzpatrick, R, Greenhall, R, and Hyman, N. Self-reported functioning and well-being in patients with Parkinson's disease: comparison of the short-form health survey (SF-36) and the Parkinson's disease questionnaire (PDQ-39). Age Ageing. (1995) 24:505–9. doi: 10.1093/ageing/24.6.505
42. Skevington, SM, Lotfy, M, and O'Connell, KAWHOQOL Group. The World Health Organization's WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res. (2004) 13:299–310. doi: 10.1023/B:QURE.0000018486.91360.00
43. Brooks, R . EuroQol: the current state of play. Health Policy. (1996) 37:53–72. doi: 10.1016/0168-8510(96)00822-6
44. Longstreth, WT Jr, Nelson, L, Linde, M, and Muñoz, D. Utility of the sickness impact profile in Parkinson's disease. J Geriatr Psychiatry Neurol. (1992) 5:142–8. doi: 10.1177/002383099200500303
45. Peto, V, Jenkinson, C, Fitzpatrick, R, and Greenhall, R. The development and validation of a short measure of functioning and well being for individuals with Parkinson's disease. Qual Life Res. (1995) 4:241–8. doi: 10.1007/BF02260863
46. Kuopio, AM, Marttila, RJ, Helenius, H, Toivonen, M, and Rinne, UK. The quality of life in Parkinson's disease. Mov Disord. (2000) 15:216–23. doi: 10.1002/1531-8257(200003)15:2<216::aid-mds1003>3.0.co;2-#
47. Rubenstein, LM, Voelker, MD, Chrischilles, EA, Glenn, DC, Wallace, RB, and Rodnitzky, RL. The usefulness of the functional status questionnaire and medical outcomes study short form in Parkinson's disease research. Qual Life Res. (1998) 7:279–90. doi: 10.1023/a:1024973611880
48. Hagell, P, Törnqvist, AL, and Hobart, J. Testing the SF-36 in Parkinson's disease. Implications for reporting rating scale data. J Neurol. (2008) 255:246–54. doi: 10.1007/s00415-008-0708-y
49. Den Oudsten, BL, Van Heck, GL, and De Vries, J. The suitability of patient-based measures in the field of Parkinson's disease: a systematic review. Mov Disord. (2007) 22:1390–401. doi: 10.1002/mds.21539
50. Schrag, A, Spottke, A, Quinn, NP, and Dodel, R. Comparative responsiveness of Parkinson's disease scales to change over time. Mov Disord. (2009) 24:813–8. doi: 10.1002/mds.22438
51. Brown, CA, Cheng, EM, Hays, RD, Vassar, SD, and Vickrey, BG. SF-36 includes less Parkinson disease (PD)-targeted content but is more responsive to change than two PD-targeted health-related quality of life measures. Qual Life Res. (2009) 18:1219–37. doi: 10.1007/s11136-009-9530-y
52. Schrag, A, Selai, C, Jahanshahi, M, and Quinn, NP. The EQ-5D--a generic quality of life measure-is a useful instrument to measure quality of life in patients with Parkinson's disease. J Neurol Neurosurg Psychiatry. (2000) 69:67–73. doi: 10.1136/jnnp.69.1.67
53. Siderowf, A, Ravina, B, and Glick, HA. Preference-based quality-of-life in patients with Parkinson's disease. Neurology. (2002) 59:103–8. doi: 10.1212/wnl.59.1.103
54. Noyes, K, Dick, AW, and Holloway, RGParkinson Study Group. Pramipexole versus levodopa in patients with early Parkinson's disease: effect on generic and disease-specific quality of life. Value Health. (2006) 9:28–38. doi: 10.1111/j.1524-4733.2006.00078.x
55. Martinez-Martin, P, and Kurtis, MM. Systematic review of the effect of dopamine receptor agonists on patient health-related quality of life. Parkinsonism Relat Disord. (2009) 15:S58–64. doi: 10.1016/S1353-8020(09)70837-5
56. Martinez-Martin, P, and Deuschl, G. Effect of medical and surgical interventions on health-related quality of life in Parkinson's disease. Mov Disord. (2007) 22:757–65. doi: 10.1002/mds.21407
57. Hunt, SM, McKenna, SP, McEwen, J, Backett, EM, Williams, J, and Papp, E. A quantitative approach to perceived health status: a validation study. J Epidemiol Community Health. (1980) 34:281–6. doi: 10.1136/jech.34.4.281
58. Hunt, SM, McKenna, SP, McEwen, J, Williams, J, and Papp, E. The Nottingham health profile: subjective health status and medical consultations. Soc Sci Med A. (1981) 15:221–9. doi: 10.1016/0271-7123(81)90005-5
59. Wann-Hansson, C, Klevsgård, R, and Hagell, P. Cross-diagnostic validity of the Nottingham health profile index of distress (NHPD). Health Qual Life Outcomes. (2008) 6:47. doi: 10.1186/1477-7525-6-47
60. Hagell, P, Whalley, D, McKenna, SP, and Lindvall, O. Health status measurement in Parkinson's disease: validity of the PDQ-39 and Nottingham health profile. Mov Disord. (2003) 18:773–83. doi: 10.1002/mds.10438
61. Erola, T, Karinen, P, Heikkinen, E, Tuominen, J, Haapaniemi, T, Koivukangas, J, et al. Bilateral subthalamic nucleus stimulation improves health-related quality of life in parkinsonian patients. Parkinsonism Relat Disord. (2005) 11:89–94. doi: 10.1016/j.parkreldis.2004.08.006
62. Hariz, GM, Lindberg, M, Hariz, MI, and Bergenheim, AT. Gender differences in disability and health-related quality of life in patients with Parkinson's disease treated with stereotactic surgery. Acta Neurol Scand. (2003) 108:28–37. doi: 10.1034/j.1600-0404.2003.00092.x
63. Forsaa, EB, Larsen, JP, Wentzel-Larsen, T, Herlofson, K, and Alves, G. Predictors and course of health-related quality of life in Parkinson's disease. Mov Disord. (2008) 23:1420–7. doi: 10.1002/mds.22121
64. Karlsen, KH, Tandberg, E, Arsland, D, and Larsen, JP. Health related quality of life in Parkinson's disease: a prospective longitudinal study. J Neurol Neurosurg Psychiatry. (2000) 69:584–9. doi: 10.1136/jnnp.69.5.584
65. Kuehler, A, Henrich, G, Schroeder, U, Conrad, B, Herschbach, P, and Ceballos-Baumann, A. A novel quality of life instrument for deep brain stimulation in movement disorders. J Neurol Neurosurg Psychiatry. (2003) 74:1023–30. doi: 10.1136/jnnp.74.8.1023
66. Haapaniemi, TH, Sotaniemi, KA, Sintonen, H, and Taimela, E. The generic 15D instrument is valid and feasible for measuring health related quality of life in Parkinson's disease. J Neurol Neurosurg Psychiatry. (2004) 75:976–83. doi: 10.1136/jnnp.2003.015693
67. Welsh, M, MP, MD, Holloway, RG, Plumb, S, Pfeiffer, R, Hubble, J, et al. Development and testing of the Parkinson's disease quality of life scale. Mov Disord. (2003) 18:637–45. doi: 10.1002/mds.10424
Keywords: atypical parkinsonism, quality of life, progressive supranuclear palsy, neurodegenerative diseases, tauopathy, patient-reported outcomes
Citation: Markiewicz M, Madetko-Alster N and Alster P (2024) Quality of life in patients with progressive supranuclear palsy: a review of literature and implications for practice. Front. Neurol. 15:1476488. doi: 10.3389/fneur.2024.1476488
Edited by:
Arun Singh, University of South Dakota, United StatesReviewed by:
Marina Peball, Medical University of Innsbruck, AustriaLydia Chougar, Université Paris-Sorbonne, France
Copyright © 2024 Markiewicz, Madetko-Alster and Alster. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Michał Markiewicz, Z3dpZG9uLm1hcmtAZ21haWwuY29t; Piotr Alster, cGlvdHIuYWxzdGVyQGdtYWlsLmNvbQ==
 Michał Markiewicz
Michał Markiewicz Natalia Madetko-Alster
Natalia Madetko-Alster Piotr Alster
Piotr Alster