- 1Department of Neurosurgery, Fondazione Policlinico Universitario “A. Gemelli” IRCCS, Rome, Italy
- 2Università Cattolica del Sacro Cuore, Rome, Italy
- 3Department of Life Sciences and Public Health, Fondazione Policlinico Universitario “A. Gemelli” IRCCS, Rome, Italy
Introduction: Limited data are available comparing the interposition and transposition techniques for microvascular decompression (MVD) in patients with trigeminal neuralgia (TN) secondary to vertebrobasilar dolichoectasia (VBD); this study aims to review current findings on TN associated with VBD and compare the interposition and transposition techniques in terms of surgical morbidity and patient outcomes.
Methods: Following the PRISMA guidelines, PubMed/Medline, Web of Science, and SCOPUS databases were searched to identify studies reporting patients undergoing MVD for TN secondary to VBD. The studies were divided into two groups, interposition and transposition, based on the microvascular decompression technique used. Studies not reporting the diagnostic criteria, included less than five cases, or were not available in English were excluded.
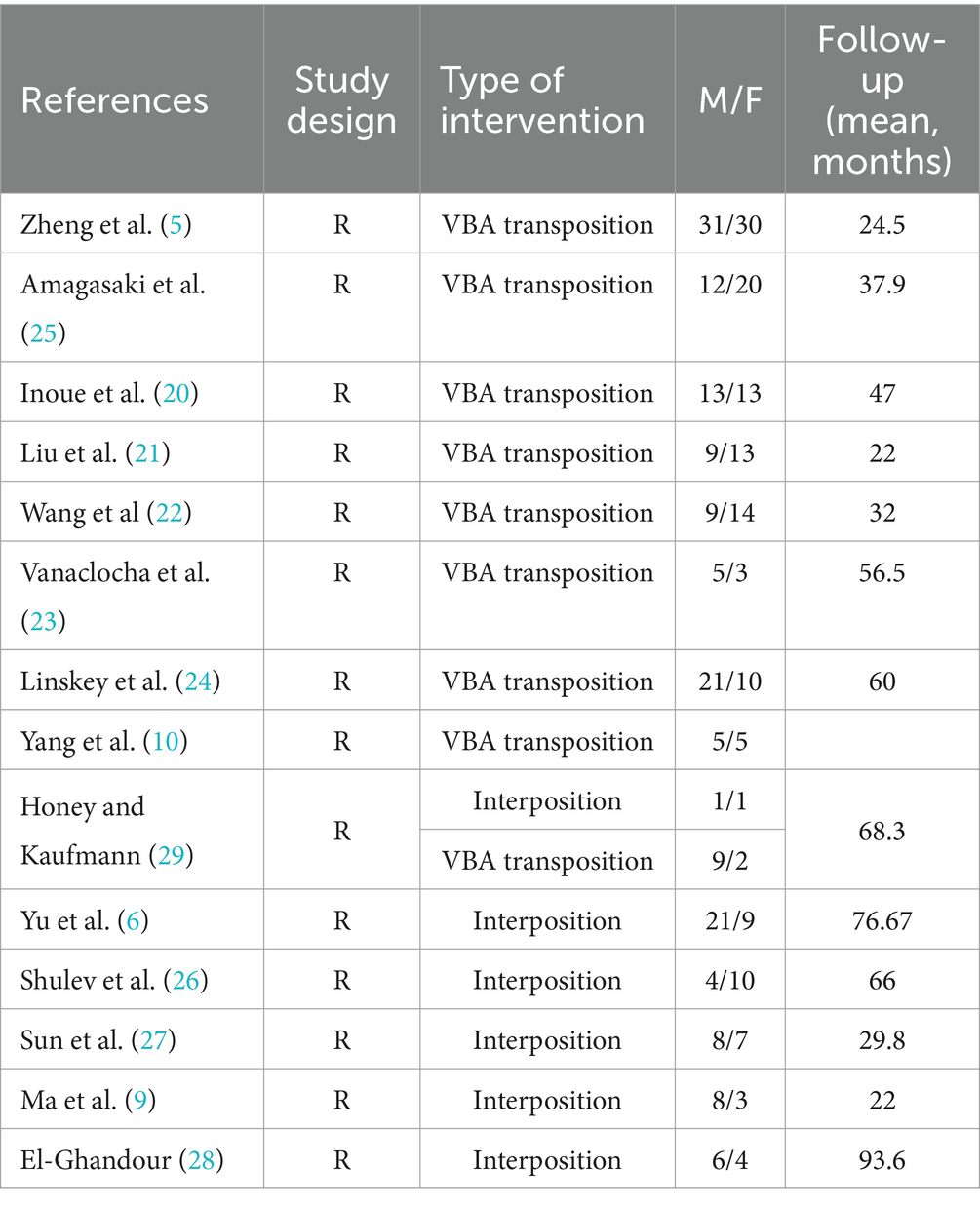
Results: Fourteen eligible papers were retrieved, of which five studies reported cases undergoing the interposition technique, eight studies for the transposition technique, and one study reported cases from both groups. Data including preoperative and postoperative BNI class, comorbidities, and postoperative complications were retrieved to analyze and compare the two techniques in terms of efficacy and long-term outcomes in treating TN secondary to VBD.
Conclusion: Both interposition and transposition techniques for MVD yield high rates of pain relief in patients with TN secondary to VBD. While both approaches demonstrate similar efficacy, the interposition method is associated with a lower rate of long-term complications. Further research, preferably through randomized prospective studies, is needed to refine surgical strategies and improve patient outcomes.
Introduction
Trigeminal neuralgia (TN) is a common chronic pain disorder characterized by recurrent episodes of electric shock-like or stabbing pain affecting the dermatomal distribution of trigeminal nerve branches (1, 2). Between 80 and 90% of the cases of TN are caused by a neurovascular conflict where the trigeminal nerve is compressed by an adjacent artery or a vein, with the superior cerebellar artery being the most implicated vessel (1, 3). Less commonly TN is secondary to vertebrobasilar dolichoectasia (VBD), a rare cerebrovascular abnormality characterized by an ectatic, elongated, and tortuous vertebrobasilar artery (VBA) complex (4). These abnormal vessels may sometimes compress, directly or indirectly—thorough displacements of adjacent vessels (5)—the root of the trigeminal nerve resulting in TN (6). Recent published studies report VBD-induced TN accounting for 2–7.7% of all cases of TN (1, 7–10).
At present, there is a global consensus that surgical intervention through microvascular decompression (MVD) is recommended for drug-resistant TN when an offending vessel causing neurovascular compression can be identified. In VBD-induced TN cases, given the unusual anatomy due to the wide and abnormally located vertebrobasilar artery complex, surgical risks are higher. Two techniques can be considered to address this condition: the interposition method and the transposition method. The former represents the standard MVD approach, routinely used in cases of classical TN due to neurovascular conflict; it requires the insertion of implants between the nerve and the offending vessel. The latter entails repositioning the VBA complex using various materials such as aneurysm clips, biomedical glues, Prolene sutures, tapes, and titanium plates. To date, current literature on this topic is scarce, with only one available study that directly compares the two techniques. The purpose of this systematic review and meta-analysis is to review current findings on TN associated with VBD and compare the two techniques in terms of surgical morbidity and postoperative outcomes.
Materials and methods
Search strategy
The systematic review was performed according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines (11) to investigate the outcomes of Microvascular decompression in patients with trigeminal neuralgia secondary to vertebrobasilar dolichoectasia (VBD) and compare the interposition technique to the transposition technique. A comprehensive literature search of PubMed, Web of Science, and Scopus was performed on for studies published in English from January 1991 to February 2024. Our systematic review was registered and accepted in PROSPERO database with the following ID: CRD42024523971. The keywords and the detailed search strategy are reported in Supplementary File 1. After searching the three databases, all results were collected. Duplicates were removed using Rayyan software (12). All remaining articles were then fully screened by 3 reviewers (FZ, VR, RC); a senior author (FS) resolved discrepancies.
Data extraction
From each study, the following data were extracted: author/s; year of publication; study design, number of patients enrolled; demographic data; mean follow-up time; patient comorbidities; reported prevalence of VBD-induced trigeminal neuralgia; trigeminal neuralgia characteristics (side and branches involved); additional vessels compressing the trigeminal nerve in addition to the VBA; postoperative complications (transient and permanent); preoperative BNI; postoperative BNI and BNI at last follow up.
Statistical analysis
Meta-regression and meta-analysis of proportions with binomial distribution were used to assess the effect of MVD transposition and interposition post-operatively and at the last follow-up. The pooled prevalence of BNI was calculated using the inverse variance method, adopting fixed effects models if the tests met the hypothesis of homogeneity, or random effects model otherwise (13). Heterogeneity across the included studies was analyzed using the Q test and the I2 index (values of 25, 50, and 75% are taken as low, medium, and high heterogeneity, respectively) (14). Subgroup analyses were performed by the intervention type. A forest plot was used to present the pooled prevalence. The leave-one-out sensitivity test was used to confirm that the findings were not driven by any single study. In addition, Egger’s tests were used to detect potential publication bias by examining the funnel plot symmetry. The odds ratio (OR) for the development of postoperative complications in both cohorts, including 95% confidence intervals (CI), was calculated. A p-value <0.05 indicated statistical significance. Statistical analyses were performed using STATA18 software.
Quality scoring
Three authors (FZ, VR, and RC) independently assessed the risk of bias for each included study using the Risk of Bias In Non-randomized Studies—of Interventions (ROBINS-I) tool (15). The quality of evidence for outcomes was assessed by the Joanna Briggs Institute (JBI) critical appraisal checklist (16).
Outcomes
The primary outcomes of this systematic review and meta-analysis were the following: (1) to determine the prevalence and clinical features of TN secondary to VBA, and (2) to analyze the different surgical strategies and related clinical outcomes and complication rate. We compared the efficacy of interposition and transposition methods by assessing the Barrow’s Neurological Institute (BNI) grade (17) (Table 1) post-operative and at last follow-up. BNI grades I–II were considered adequate pain relief, whereas BNI grades III–V indicated pain recurrence.

Table 1. Barrow Neurological Institute (BNI) pain intensity score (17).
Results
Literature review
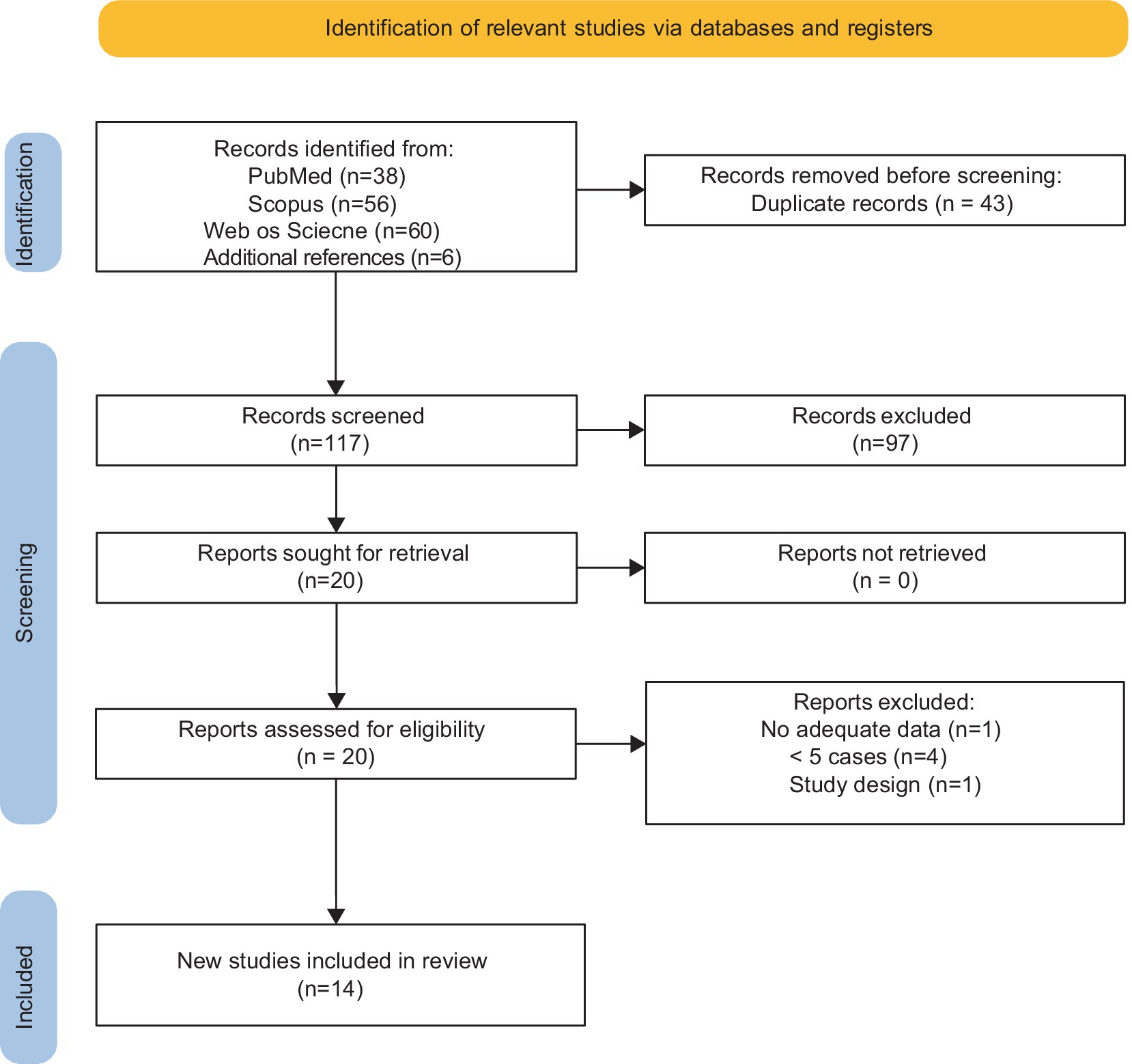
The search strategy yielded 160 results. After the removal of duplicates, articles were screened by title and abstract for relevance. The remaining articles were then screened via full text (see the PRISMA diagram shown in Figure 1). Studies meeting the defined criteria were included for quantitative analysis. The characteristics of the individual studies are presented in Table 2. Fourteen studies including 306 patients with trigeminal neuralgia secondary to VBD were analyzed in this review. All included studies presented a retrospective single-center design. The exclusion criteria were the following: (1) studies with less than five patients; (2) case reports; (3) review articles; (4) technical notes; (5) studies published in languages other than English with no available English translations; (6) case series not dealing with trigeminal neuralgia caused by VBA conflict; (7) case series with no specific data on surgical steps performed. Furthermore, we only included studies in which VBD was defined according to specific diagnostic criteria as first proposed by Ubogu and Zaidat (18): basilar artery (BA) or vertebral artery (VA) diameter > 4.5 mm, deviation of any portion >10 mm from the shortest expected course, BA length > 29.5 mm or intracranial VA length > 23.5 mm, BA bifurcation above the suprasellar cistern or any BA portion lying adjacent to the margin of the clivus or dorsum sellae (19).
Demographic data and risk factors
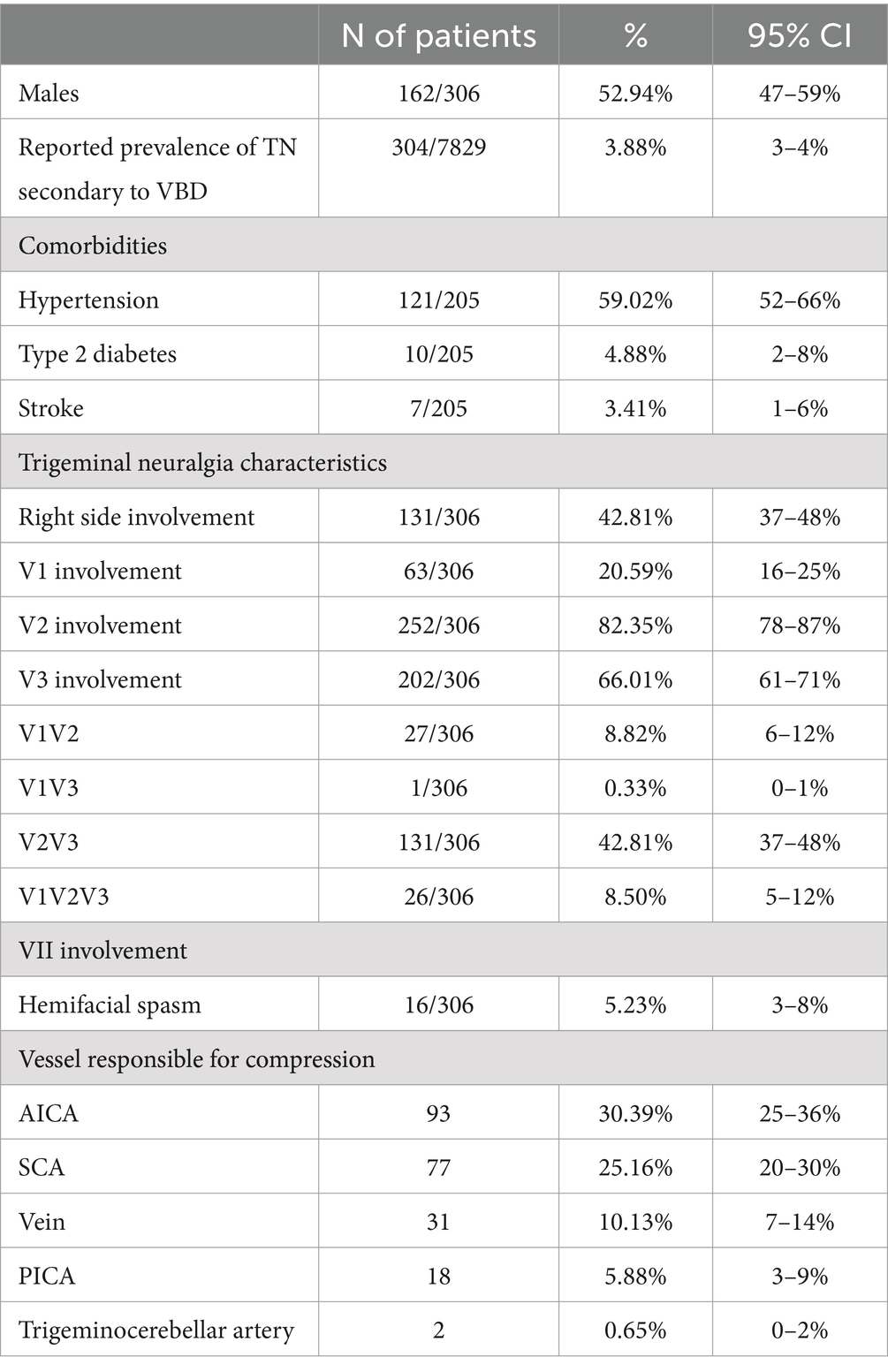
In our meta-analysis, the reported prevalence of vertebrobasilar dolichoectasia (VBD) among patients who underwent microvascular decompression (MVD) for trigeminal neuralgia ranged from 2 to 7% with a mean prevalence of 4%.
The mean age of patients varied between 54 and 68 years, with males comprising 53% (95% CI: 47–59%) of the cohort. Hypertension was reported in 59% (95% CI: 52–68%) of the patients. The right side was affected in 43% (95% CI: 37–48%) of patients, with the V2 branch being the most frequently involved, accounting for 82% (95% CI: 78–87%) of cases. The most common clinical presentation was the involvement of both V2 and V3 branches (43, 95% CI: 37–48%). Detailed data are reported in Table 3.
Surgical approach and intraoperative findings
In our analysis, we found the retrosigmoid suboccipital to be the most frequently used approach for MVD. Following this approach, the dura mater is incised along the sigmoid and transverse sinuses, then, after a gradual release of cerebrospinal fluid (CSF) from the lateral cerebellar cistern, the cerebellum is retracted medially to facilitate exposure. The arachnoid membrane is then dissected to provide full visualization of the lower cranial nerves.
Other than vertebrobasilar artery (VBA) compression, additional vessels were found to be compressing the trigeminal nerve. The anterior inferior cerebellar artery (AICA) and the superior cerebellar artery (SCA) were the most frequently reported additional offending vessels, involved in 30% (95% CI: 25–36%) and 25% (95% CI: 20–30%) of cases, respectively. Detailed data are reported in Table 3.
There were eight studies reporting patients treated with the transposition technique (5, 10, 20–25), and five studies reporting on the interposition technique (6, 9, 26–28). One case series included patients treated with either technique (29). In the transposition group (n = 224), VBA repositioning was achieved using various materials including Teflon sling/roll/pads/felt, biomedical glue, aneurysm clips, Ivalon sponge, autologous muscle, and silicon sheet. In the interposition group (n = 82) pieces of Teflon between the trigeminal nerve and the vessel responsible for the neurovascular conflict were placed, without forcing the repositioning of the vessel.
Interposition vs. transposition: clinical outcomes and postoperative complications
The pooled analysis (Figure 2) demonstrated that the interposition approach resulted in post-operative Barrow Neurological Institute (BNI) grades I-II in 97% (95% CI: 84–100%, I2 = 59.5%, p = 0.03) of cases, compared to 98% (95% CI: 93–100%, I2 = 27.5%, p = 0.22) with the transposition approach. At the last follow-up, BNI I-II was observed in 95% (95% CI: 78–100%, I2 = 68%, p = 0.01) of patients treated with interposition and 96% (95% CI: 90–99%, I2 = 29.5%, p = 0.20) of those treated with transposition (Figure 3). After assessing the comparability of the two patient groups and stratifying by intervention type, the meta-regression estimated a BNI I-II rate of 96% for both the interposition group (95% CI: 71–98%) and the transposition group (95% CI: 77–98%) (Figure 4).
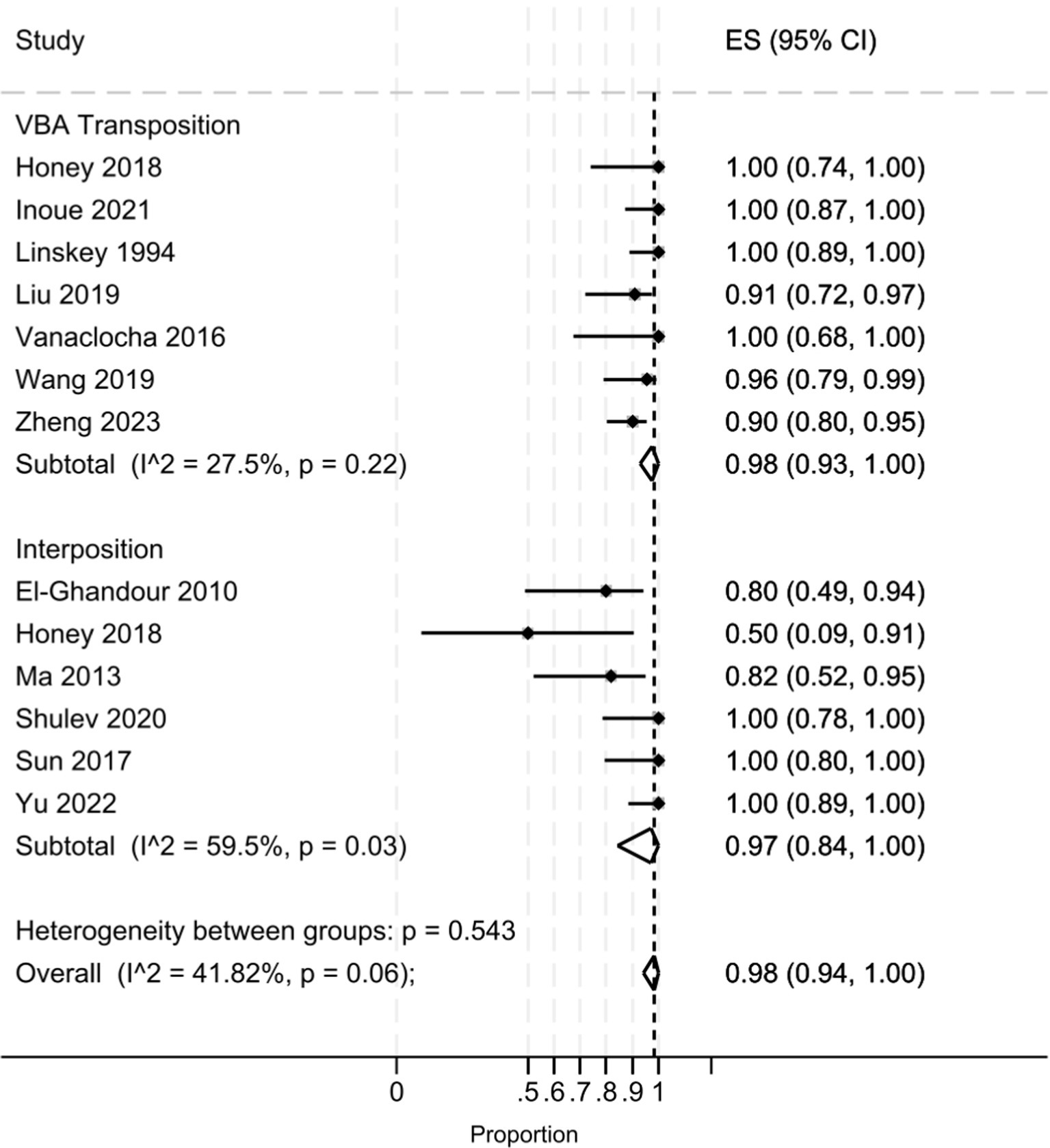
Figure 2. Forest plot detailing the pooled rate and 95% confidence intervals for the rate of post-operative BNI I-II in the VBA transposition group and the Interposition group.
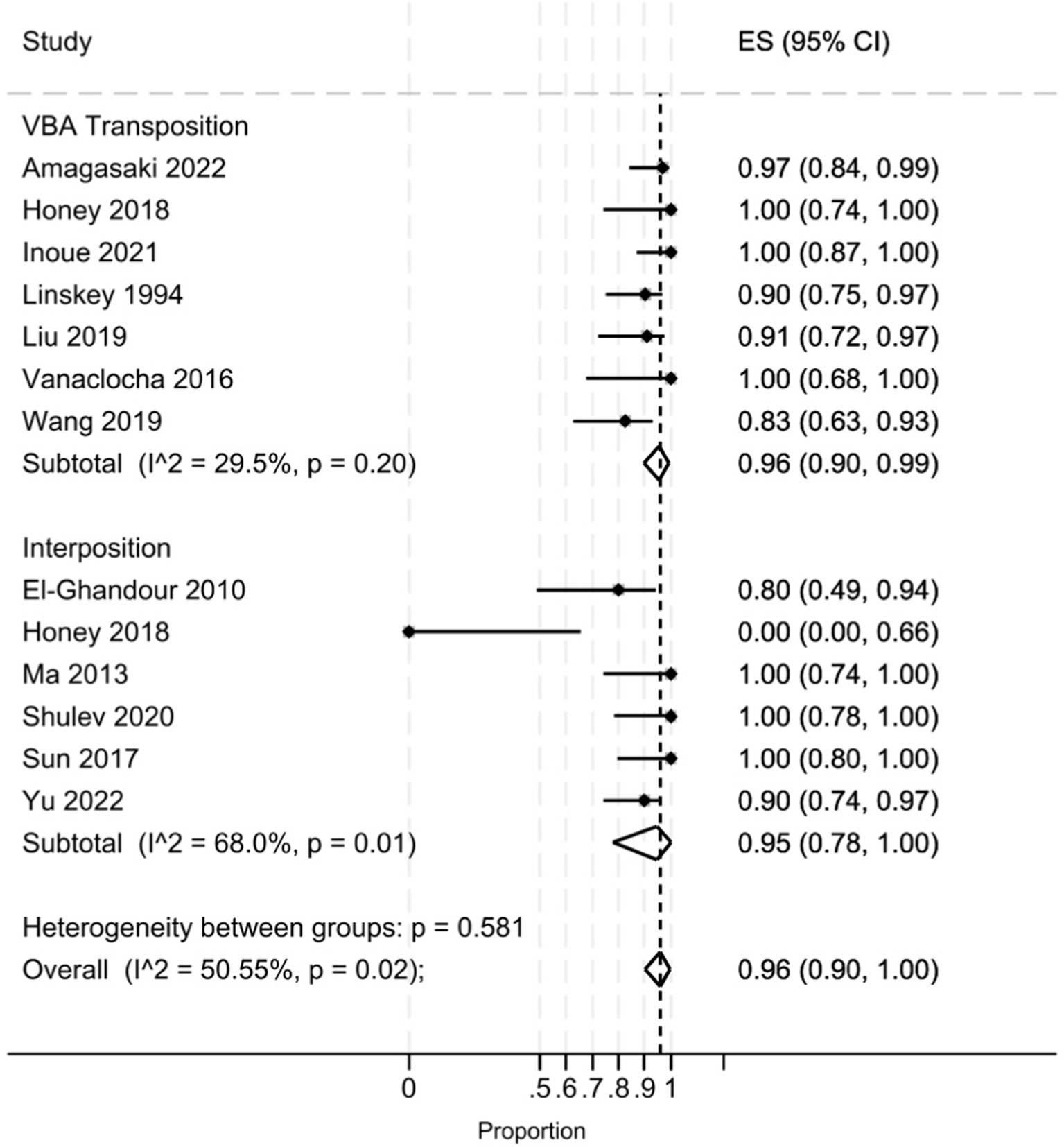
Figure 3. Forest plot detailing the pooled rate and 95% confidence intervals for the rate of BNI I-II in the VBA transposition group and the Interposition group at last follow-up.
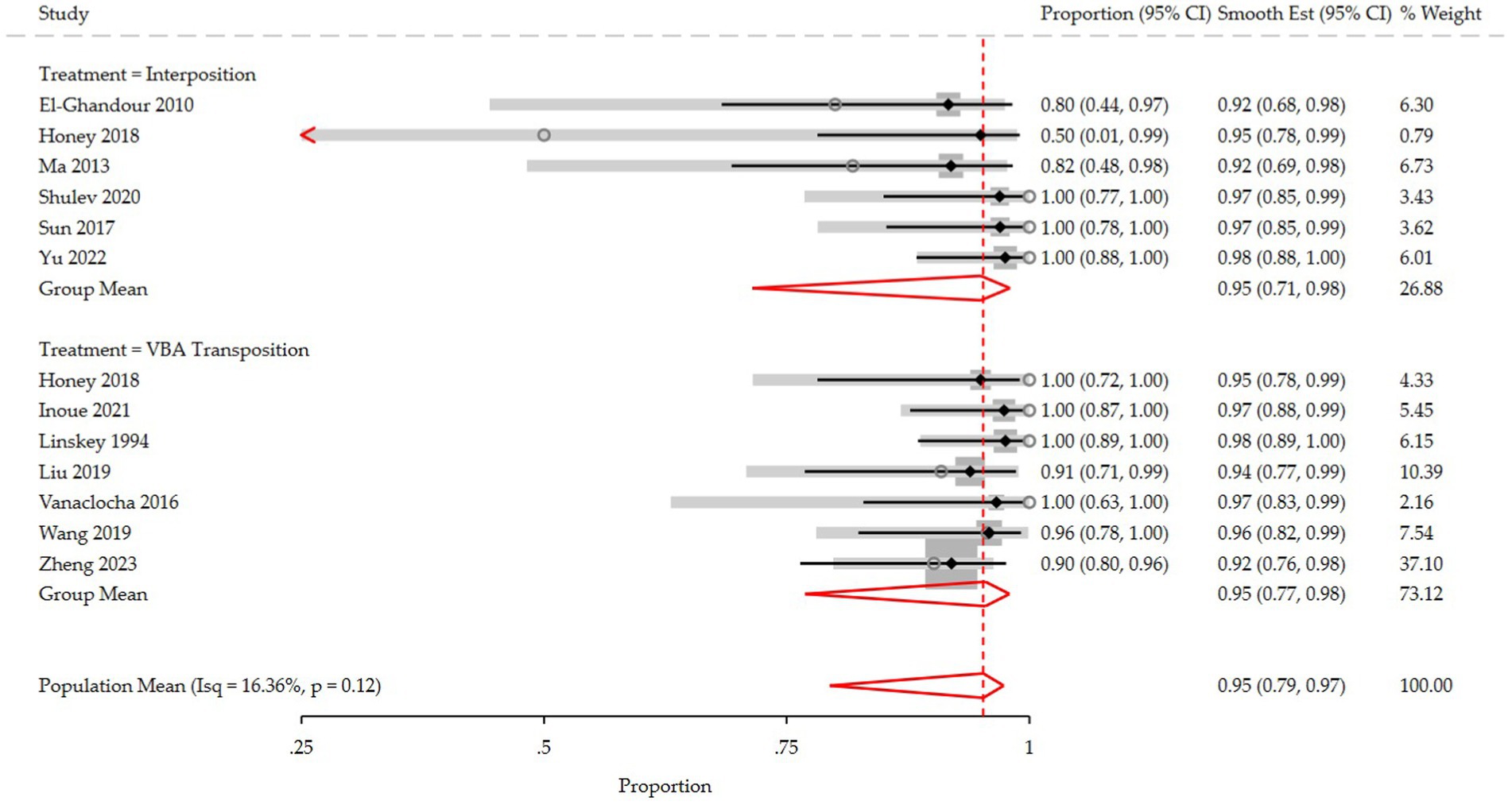
Figure 4. Forest plot detailing the meta-regression rate and 95% confidence intervals for the rate of post-operative BNI I-II in the VBA transposition group and the Interposition group.
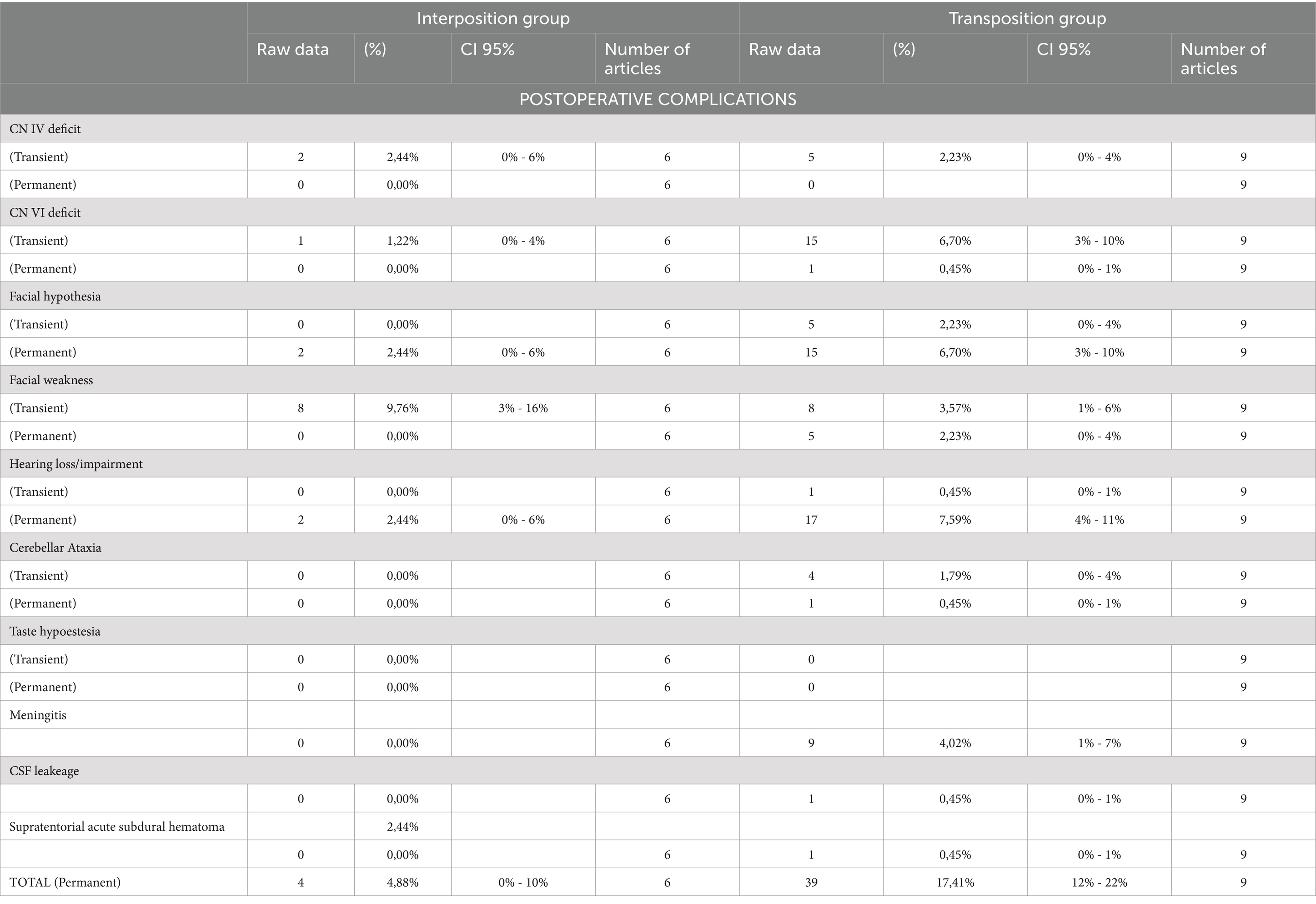
However, the interposition group showed a significantly lower pooled complication rate compared to the transposition group (4.88% vs 17.41%; OR 0.24, 95% CI 8-70%, p = 0.009). Early postoperative complications in the interposition group included facial weakness (10%, 95% CI: 3-16%), facial hypoesthesia (2%, 95% CI: 0-6%), and hearing impairment (2%, 95% CI: 0-6%). Notably, all cases of facial weakness resolved, while facial hypoesthesia and hearing loss persisted at the last follow-up.
In contrast, the transposition group had higher rates of complications: fifteen patients (7%, 95% CI: 3–10%) experienced permanent facial hypoesthesia, and seventeen patients (8%, 95% CI: 4–11%) reported permanent hearing impairment. Additionally, nine patients developed postoperative meningitis (4%, 95% CI: 1–7%). Details on the rate of postoperative complications are shown in Table 4.
Discussion
Vertebrobasilar dolichoectasia (VBD; from the Greek dolicho, “elongated,” and ectasia, “dilated”) is an uncommon cause of trigeminal neuralgia (TN). It refers to a vascular abnormality characterized by expansion, elongation, and tortuosity of the vertebrobasilar system. Di Carlo et al. previously performed a meta-analysis and systematic review on VBD-related TN (30), and more recently, we published an updated narrative review on the topic (31). However, neither of these works included a quantitative comparison of the interposition and transposition techniques. The current study aims to address that gap by directly comparing these surgical approaches and evaluating their outcomes.
Epidemiology and clinical characteristics
The etiopathogenesis of VBD is still largely unknown, but evidence points toward a multifactorial process combining congenital vascular wall abnormalities with acquired factors related to atherosclerosis (32, 33). Our analysis found that 52.94% of the population were males, and hypertension was present in 59.02% of cases. These findings align with the literature, indicating that patients with VBD-related TN are more likely to be older males with a history of hypertension, diabetes, hyperlipidemia, and myocardial infarction (6, 8, 23, 24, 28, 34). Addressing these risk factors postoperatively may improve long-term outcomes and potentially delay or prevent pain recurrence to a certain extent, though further research is needed to confirm this statement (5).
Our study found that the left side was more frequently affected (57.19%), consistent with previous findings (30). Left predominance may be related to hemodynamic and anatomical factors, as blood flow and shear stress are higher in the left VA than the right one (since the left subclavian artery, from which the VA arises, originates directly from the aortic arch), resulting in an asymmetric blood flow to the basilar artery with subsequent elongation and curvation of the VBA complex toward the weaker vertebral artery (6).
The V2 and V3 branches of the trigeminal nerve were affected in most cases (82.35 and 66.01%, respectively), due to the compression from below, leaving the rostral V1 branch intact. VBD-related TN often showed multiple vessels contributing to the neurovascular conflict: in 30.39% of cases, an AICA+VBA combination was found, while SCA + VBA was found in 25.16% of patients.
Clinical outcomes and surgical technique
Microvascular decompression (MVD) is the most effective surgical option for classic TN refractory to medical treatment (35–38). However, when the compression is secondary to VBA dolichoectasia, there is no universally accepted method for isolating the offending vessel. Generally, two approaches are performed: the interposition method and the transposition method. The transposition method theoretically reduces the risk of adhesion and granuloma formation at the decompression site, which are key factors in the recurrence of symptoms post-MVD. However, this method is often more time-consuming, complex, and potentially hazardous compared to the interposition method. The interposition method, which involves placing patches between the REZ and the offending vessels, is relatively straightforward and effective in relieving nerve compression. Despite some support for the interposition method, many experts believe it may result in inadequate decompression, thus diminishing the efficacy of MVD.
Our pooled analysis indicated that the transposition group had slightly higher rates of postoperative pain relief (considered as post-operative BNI score of 1–2) than the interposition group. However, this finding may be influenced by the higher heterogeneity of the interposition group in the included studies (I2 59.5 and 27.5% in the interposition and transposition group, respectively, p = 0543). Indeed, the meta-regression analysis revealed an identical post-operative BNI group mean score (96%) for both techniques, suggesting they are comparable in terms of immediate pain relief.
In the study by Chai et al. (8), the authors compared the transposition and interposition techniques and found that the transposition group was associated with significantly better outcomes in terms of post-operative BNI score and pain-recurrence rate. They attributed these findings to several factors: given that in VBD the offending vessel is larger than AICA, SCA, and other vessels usually involved in classic TN, the interposition technique requires an increased amount of Teflon to achieve optimal decompression, posing a risk of applying additional pressure from excessive material used; additionally, the transposition technique can directly address the pulsatile transmission of the dolichoectatic VBA, which is believed to contribute to TN development and recurrence.
Despite these advantages, the transposition method is associated with higher postoperative complication rates. We found permanent facial hypoesthesia in 7% of cases and permanent hearing impairment in 8% at the last follow-up. It is also worth noting that the dolichoectatic arteries generally present with atherosclerosis, abnormal course, increased diameter, low elasticity, and limited mobility. These factors significantly increase the complexity of the surgery, particularly during vessel displacement, posing potential risks such as plaque dislodgement, rupture of branch vessels, and vasospasm (26).
Strength and limitations
Our study has some limitations. The included articles were only small, retrospective, and single-institution case series and the reported data were incomplete in many of these. Follow-up ranged from 1 year up to 15 years, which may not provide a homogeneous long-term perspective. Additionally, the interposition group had fewer cases and greater heterogeneity across the included studies compared to the transposition group. This variability complicates direct comparison of data and necessitates caution when interpreting results. Despite these limitations, our study is the only meta-analysis comparing the interposition and transposition techniques for VBD-related TN, providing valuable insights into their relative efficacy and complications.
Future research should focus on larger, prospective studies with standardized reporting to better compare these techniques and refine surgical strategies to improve patient outcomes.
Conclusion
Vascular compression is a frequent and treatable cause of essential trigeminal neuralgia. Even in the rare and complex case of a dolichoectatic vertebrobasilar artery, the microsurgical decompression method can provide excellent long-term outcomes in patients with TN who do not respond to medication. In our revision study, interposition and transposition groups revealed an identical post-operative BNI group mean score (96%) suggesting they are comparable in terms of immediate pain relief. However the transposition group is associated with higher postoperative complication rates.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
FS: Conceptualization, Methodology, Supervision, Validation, Visualization, Writing – review & editing. FZ: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. VR: Conceptualization, Data curation, Investigation, Methodology, Writing – original draft. FB: Data curation, Formal analysis, Investigation, Resources, Writing – original draft. RC: Data curation, Investigation, Writing – original draft. MV: Conceptualization, Funding acquisition, Resources, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2024.1474553/full#supplementary-material
References
1. Apra, C, Lefaucheur, JP, le Guérinel, C, Caroline, A, Jean-Pascal, L, and Guérinel, CL. Microvascular decompression is an effective therapy for trigeminal neuralgia due to dolichoectatic basilar artery compression: case reports and literature review. Neurosurg Rev. (2017) 40:577–82. doi: 10.1007/s10143-017-0812-5
2. Sindou, M, Keravel, Y, Abdennebi, B, and Szapiro, J. Neurosurgical treatment of trigeminal neuralgia. Direct approach of percutaneous method? Neurochirurgie. (1987) 33:89–111.
3. Bašić, KV. Accommodation to diagnosis of trigeminal neuralgia. Acta Clin Croat. (2017) 56:157–61. doi: 10.20471/acc.2017.56.01.21
4. Smoker, WRK, Corbett, JJ, Gentry, LR, Keyes, WD, Price, MJ, and Mckuske, S. High-resolution computed tomography of the basilar artery: 2. Vertebrobasilar dolichoectasia: clinical pathologic correlation and review. AJNR Am J Neuroradiol. (1986) 7:61–72.
5. Zheng, W, Wang, L, Wang, H, Zhou, H, and Du, Q. Trigeminal neuralgia caused by vertebrobasilar dolichoectasia: efficacy of stepwise decompression technique. Acta Neurochir. (2023) 165:3019–26. doi: 10.1007/s00701-023-05691-7
6. Yu, F, Yin, J, Lu, P, Zhao, ZY, Zhang, YQ, and Men, XZ. Microvascular decompression by interposition method for treatment of trigeminal neuralgia due to vertebrobasilar dolichoectasia: a retrospective single-center study. Neurosurg Rev. (2022) 45:2709–15. doi: 10.1007/s10143-022-01776-6
7. Park, KJ, Kondziolka, D, Kano, H, Berkowitz, O, Ahmed, SF, Liu, X, et al. Outcomes of Gamma Knife surgery for trigeminal neuralgia secondary to vertebrobasilar ectasia. J Neurosurg. (2012) 116:73–81. doi: 10.3171/2011.8.JNS11920
8. Chai, S, Xu, H, Wang, Q, Li, J, Wang, J, Wang, Y, et al. Microvascular decompression for trigeminal neuralgia caused by vertebrobasilar dolichoectasia: interposition technique versus transposition technique. Acta Neurochir. (2020) 162:2811–21. doi: 10.1007/s00701-020-04572-7
9. Ma, X, Sun, X, Yao, J, Ni, S, Gong, J, Wang, J, et al. Clinical analysis of trigeminal neuralgia caused by vertebrobasilar dolichoectasia. Neurosurg Rev. (2013) 36:573–8. doi: 10.1007/s10143-013-0468-8
10. Yang, XS, Li, ST, Zhong, J, Zhu, J, Du, Q, Zhou, QM, et al. Microvascular decompression on patients with trigeminal neuralgia caused by ectatic vertebrobasilar artery complex: technique notes. Acta Neurochir. (2012) 154:793–7. doi: 10.1007/s00701-012-1320-6
11. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
12. Ouzzani, M, Hammady, H, Fedorowicz, Z, and Elmagarmid, A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. (2016) 5:210. doi: 10.1186/s13643-016-0384-4
13. Higgins, JPT, Thompson, SG, Deeks, JJ, and Altman, DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
14. Huedo-Medina, TB, Sánchez-Meca, J, Marín-Martínez, F, and Botella, J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods. (2006) 11:193–206. doi: 10.1037/1082-989X.11.2.193
15. Sterne, JA, Hernán, MA, Reeves, BC, Savović, J, Berkman, ND, Viswanathan, M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. (2016):355. doi: 10.1136/bmj.i4919
16. Munn, Z, Barker, TH, Moola, S, Tufanaru, C, Stern, C, McArthur, A, et al. Methodological quality of case series studies: an introduction to the JBI critical appraisal tool. JBI Evid Synth. (2020) 18:2127–33. doi: 10.11124/JBISRIR-D-19-00099
17. Rogers, CL, Shetter, AG, Fiedler, JA, Smith, KA, Han, PP, Speiser, BL, et al. Gamma knife radiosurgery for trigeminal neuralgia: the initial experience of the Barrow Neurological Institute. Int J Radiat Oncol Biol Phys. (2000) 47:1013–9. doi: 10.1016/s0360-3016(00)00513-7
18. Ubogu, EE, and Zaidat, OO. Vertebrobasilar dolichoectasia diagnosed by magnetic resonance angiography and risk of stroke and death: a cohort study. J Neurol Neurosurg Psychiatry. (2004) 75:22–6.
19. Stone, JL, Lichtor, T, and Crowell, RM. Microvascular sling decompression for trigeminal neuralgia secondary to ectatic vertebrobasilar compression. J Neurosurg. (1993) 79:943–5. doi: 10.3171/jns.1993.79.6.0943
20. Inoue, T, Shitara, S, Goto, Y, Prasetya, M, and Fukushima, T. Microvascular decompression for trigeminal neuralgia attributable to the vertebrobasilar artery: decompression technique and significance of separation from the nerve root. Acta Neurochir Suppl. (2021) 163:1037–43. doi: 10.1007/s00701-020-04563-8
21. Liu, J, Chen, Z, Feng, T, Jiang, B, Yuan, Y, and Yu, Y. Biomedical glue sling technique in microvascular decompression for trigeminal neuralgia caused by atherosclerotic Vertebrobasilar artery: a description of operative technique and clinical outcomes. World Neurosurg. (2019) 128:e74–80. doi: 10.1016/j.wneu.2019.03.289
22. Wang, X, Wang, H, Chen, S, Liang, H, Wang, H, Xu, M, et al. The long-term clinical outcomes of microvascular decompression for treatment of trigeminal neuralgia compressed by the vertebra-basilar artery: a case series review. BMC Neurol. (2019) 19:217. doi: 10.1186/s12883-019-1450-z
23. Vanaclocha, V, Herrera, JM, Martínez-Gómez, D, Rivera-Paz, M, Calabuig-Bayo, C, and Vanaclocha, L. Is there a safe and effective way to treat trigeminal neuralgia associated with Vertebrobasilar Dolichoectasia? Presentation of 8 cases and literature review. World Neurosurg X Elsevier Inc. (2016) 96:516–29. doi: 10.1016/j.wneu.2016.08.085
24. Linskey, ME, Jho, HD, and Jannetta, PJ. Microvascular decompression for trigeminal neuralgia caused by vertebrobasilar compression. J Neurosurg. (1994) 81:1–9. doi: 10.3171/jns.1994.81.1.0001
25. Amagasaki, K, Takusagawa, Y, Tatebayashi, K, and Nakaguchi, H. Macrovascular decompression with the transposition method using Teflon sling for trigeminal neuralgia caused by the Vertebrobasilar artery. World Neurosurg. (2022) 167:e1395–401. doi: 10.1016/j.wneu.2022.09.049
26. Shulev, YA, Gordienko, KS, Trashin, AV, and Pechiborshch, DA. Microvascular decompression in trigeminal neuralgia following vertebrobasilar dolichoectasia. Zhurnal Voprosy Nejrokhirurgii Imeni NN Burdenko. (2020) 84:50–63. doi: 10.17116/neiro20208405150
27. Sun, S, Jiang, W, Wang, J, Gao, P, Zhang, X, Jiao, L, et al. Clinical analysis and surgical treatment of trigeminal neuralgia caused by vertebrobasilar dolichoectasia: a retrospective study. Int J Surg. (2017) 41:183–9. doi: 10.1016/j.ijsu.2017.04.015
28. El-Ghandour, NMF. Microvascular decompression in the treatment of trigeminal neuralgia gaused by vertebrobasilar ectasia. Neurosurgery. (2010) 67:330–7. doi: 10.1227/01.NEU.0000371978.86528.60
29. Honey, CM, and Kaufmann, AM. Trigeminal neuralgia due to vertebrobasilar artery compression. World Neurosurg. (2018) 118:e155–60. doi: 10.1016/j.wneu.2018.06.145
30. Di Carlo, DT, Benedetto, N, Marani, W, Montemurro, N, and Perrini, P. Microvascular decompression for trigeminal neuralgia due to vertebrobasilar artery compression: a systematic review and meta-analysis. Neurosurg Rev. (2022) 45:285–94. doi: 10.1007/s10143-021-01606-1
31. Visocchi, M, Zeoli, F, and Signorelli, F. Microvascular Decompression for Trigeminal Neuralgia Secondary to Vertebrobasilar Dolichoectasia: Review of the Literature and Illustrative Case. J Clin Med [Internet]. (2024) 13:6342.
32. Campos, WK, Guasti, AA, da Silva, BF, and Guasti, JA. Trigeminal neuralgia due to vertebrobasilar dolichoectasia. Case Rep Neurol Med. (2012) 2012:1–3. doi: 10.1155/2012/367304
33. Passero, SG, and Rossi, S. Natural history of vertebrobasilar dolichoectasia. Neurology. (2008) 70:66–72. doi: 10.1212/01.wnl.0000286947.89193.f3
34. Wang, Y, and Cheng, W. Vertebrobasilar dolichoectasia and basilar artery dissection presenting with trigeminal neuralgia: a case report. Front Neurol. (2019) 10:10. doi: 10.3389/fneur.2019.00491
35. Kraemer, JL, Pereira Filho, A de A, David, G de, and Faria, M de B. Vertebrobasilar dolichoectasia as a cause of trigeminal neuralgia: the role of microvascular decompression. Case report. Arq Neuropsiquiatr. (2006) 64:128–31. doi: 10.1590/S0004-282X2006000100027
36. Ashkan, K, and Marsh, H. Microvascular decompression for trigeminal neuralgia in the elderly: a review of the safety and efficacy. Neurosurgery. (2004) 55:840–50. doi: 10.1227/01.NEU.0000137660.06337.C5
37. Jannetta, PJ. Arterial compression of the trigeminal nerve at the pons in patients with trigeminal neuralgia. J Neurosurg. (2007) 107:216–37. doi: 10.3171/JNS-07/07/0216
Keywords: microvascular decompression, vertebrobasilar dolichoectasia, trigeminal neuralgia, interposition, transposition
Citation: Signorelli F, Zeoli F, Rastegar V, Beccia F, Caronna R and Visocchi M (2024) Interposition versus transposition technique in microvascular decompression for trigeminal neuralgia secondary to vertebrobasilar dolichoectasia: a systematic review and pooled meta-analysis. Front. Neurol. 15:1474553. doi: 10.3389/fneur.2024.1474553
Edited by:
Massimiliano Valeriani, University of Rome Tor Vergata, ItalyReviewed by:
Christian Scheiwe, University Hospital Freiburg, GermanyRoberta Costanzo, University of Palermo, Italy
Copyright © 2024 Signorelli, Zeoli, Rastegar, Beccia, Caronna and Visocchi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fabio Zeoli, ZmFiaW8uemVvbGkwMUBpY2F0dC5pdA==
 Francesco Signorelli
Francesco Signorelli Fabio Zeoli
Fabio Zeoli Valid Rastegar
Valid Rastegar Flavia Beccia
Flavia Beccia Riccardo Caronna
Riccardo Caronna Massimiliano Visocchi
Massimiliano Visocchi