- 1Department of Acupuncture Moxibustion Massage Rehabilitation and Healthcare, Shandong College of Traditional Chinese Medicine, Yantai, Shandong, China
- 2College of Acupuncture Moxibustion and Massage, Shandong University of Traditional Chinese Medicine, Jinan, Shandong, China
- 3Department of Neurology, Shijingshan Teaching Hospital of Capital Medical University, Beijing Shijingshan Hospital, Beijing, China
Objective: This study intends to carry out a systematic review and meta-analysis of electroacupuncture combined with TDP in the treatment of peripheral facial paralysis.
Methods: CNKI, VIP, Wanfang, PubMed, Embase and Cochrane databases were searched for literatures on randomized or quasi-randomized controlled trials of electroacupuncture combined with TDP in the treatment of peripheral facial paralysis, and the references of the included studies were searched. Meta-analysis was performed using Stata15.0 software after risk of bias, quality assessment, and data extraction of the included articles by two reviewers independently.
Results: Fifteen articles were finally included, with approximately 1,568 participants (920 in the treatment group and 648 in the control group). Meta-analysis showed that the effective rate of electroacupuncture combined with TDP in the treatment of peripheral facial paralysis was not significantly different from other treatment methods ([RR = 1.05, 95%CI (0.97, 1.12), p = 0.226]), and the recovery rate was better than other treatment methods ([RR = 1.14, 95%CI (1.05, 1.24), p = 0.002]). Subgroup analysis showed that when stratified by the inclusion of minors in the study population, it was observed that in studies including minors, the combination of electroacupuncture and TDP therapy demonstrated superior efficacy in treating peripheral facial paralysis compared to other therapeutic modalities [OR = 1.14, 95% CI (1.03, 1.25), p = 0.011]. Conversely, in studies where the population comprised solely adults, no significant difference was found between the combination therapy and other treatments [OR = 1.15, 95% CI (0.99, 1.33), p = 0.059]; whether electroacupuncture alone or other treatment methods, the recovery rate of electroacupuncture combined with TDP in the treatment of peripheral facial paralysis was better than other methods.
Conclusion: Electroacupuncture combined with TDP is superior to other treatment methods in the treatment of peripheral facial paralysis.
1 Introduction
Peripheral facial paralysis, also known as idiopathic facial nerve palsy and Bell’s palsy, represents a prevalent neuropathy of the facial nerve (1). Clinically, it primarily manifests as impaired motor function of the facial muscles on the affected side, with incomplete or complete paralysis of the expression muscles on the affected side (2). Peripheral facial paralysis is considered a self-limiting condition, with a favorable prognosis if diagnosed and treated promptly and accurately (3). Research indicates that approximately two-thirds of patients may experience abnormal regeneration of the facial nerve, often accompanied by synkinesis and crocodile tears. Poor recovery of facial muscle control in some patients can lead to facial deformity and pain (4).
Various treatment modalities are available for peripheral facial paralysis, including symptomatic treatment in Western medicine (5, 6), external treatment in traditional Chinese medicine (7–9), and combination therapies (10, 11). Electroacupuncture is a commonly used external treatment, supported by evidence from some review studies (8, 12). However, existing research often focuses on the influence of electroacupuncture parameters such as waveform, frequency, and intervention timing on the treatment of peripheral facial paralysis. TDP (Teding Diancibo Pu) therapy, also known as the “Magic Lamp” or “Infrared Therapeutic Apparatus” (13), is a domestically developed electromagnetic spectrum therapy device in China. TDP emits micron-level electromagnetic waves, exerting effects such as promoting blood circulation, relieving stasis, and alleviating pain. The elements generated by TDP radiation can enhance endogenous enzyme activity, promote metabolism, and boost immunity. Additionally, TDP irradiation can increase the content of endorphins in the body, alleviating pain (14).
In recent years, numerous studies have focused on the use of electroacupuncture combined with TDP therapy for the treatment of peripheral facial paralysis. However, the results of these studies have been inconsistent due to variations in sample sizes and differences in study design (15–17). Additionally, there is a lack of robust evidence regarding the comparative efficacy of electroacupuncture combined with TDP therapy versus standalone electroacupuncture, conventional Western medications, or acupuncture in the treatment of peripheral facial paralysis. Therefore, this study aims to conduct a systematic review and Meta-analysis of randomized controlled trials on the use of electroacupuncture combined with TDP therapy for the treatment of peripheral facial paralysis. This evaluation will provide evidence-based support for the clinical implementation of electroacupuncture combined with TDP therapy in treating peripheral facial paralysis.
2 Materials and methods
2.1 Literature search strategy
A systematic search was conducted in PubMed, EMBASE, Cochrane Library, CNKI, VIP, and Wanfang databases for studies on the use of electroacupuncture combined with TDP therapy for peripheral facial paralysis published up to April 29, 2024. The search terms in Chinese included “peripheral facial palsy,” “facial neuritis,” “Bell’s palsy,” “Bell’s facial paralysis,” “idiopathic facial neuritis”; “electroacupuncture”; “TDP,” “hot lamp,” “magic lamp,” “electromagnetic wave,” and “infrared.” The search terms in English included “Bell’s Palsy,” “peripheral facial palsy,” “facial paralysis,” “facial neuritis”; “electroacupuncture”; and “TDP.”
2.2 Inclusion and exclusion criteria
Inclusion criteria: (1) study type: randomized controlled trials published in Chinese or English; (2) subjects: patients diagnosed with peripheral facial paralysis with detailed diagnostic criteria; (3) interventions: electroacupuncture combined with TDP therapy; the control group receiving other treatments such as standalone electroacupuncture, conventional Western medications, or acupuncture; and (4) outcomes: clinical efficacy including overall response rate and cure rate, facial nerve function score, facial disability index score, and adverse effects.
Exclusion criteria: (1) studies that were duplicate reports or from which valid data could not be extracted; (2) case reports, reviews, and conference abstracts; and (3) animal or cadaver studies.
2.3 Information extraction and quality evaluation
Two independent investigators meticulously screened the literature and extracted data in strict accordance with the inclusion and exclusion criteria. In cases of disagreement, discussions were held to reach a consensus. The extracted data included the first author, year of publication, geographical background, sample size, intervention measures, and outcome indicators.
The modified Jadad scale (18) was employed to evaluate the quality of the literature. This scale assesses literature quality based on the randomization method, whether allocation concealment was present, the correct implementation of blinding, and the description of withdrawals and dropouts. Mention “random,” “random allocation” and “random grouping” and so on, and score 1 point; If the use of’ double-blind’ is mentioned as 1 point, the double-blind method is correctly described as 2 points; The reasons and cases of withdrawal and loss of follow-up in each group were reported, and the number of cases was 1 point. Studies scoring 4–7 points were considered high-quality research, those scoring 1–2 points were deemed low-quality, and studies scoring 0 points were excluded from the research. The quality evaluation was conducted independently by two researchers, and any discrepancies were resolved through discussion to determine the final score.
2.4 Statistical analysis
Meta-analysis was performed using Stata15.0 statistical software. For categorical data, the effect size was estimated using the risk ratio (RR) and its 95% confidence interval (CI). For continuous data, the standardized mean difference (SMD) and its 95% CI were utilized. The I2 statistic was used to evaluate heterogeneity due to non-threshold effects. Specifically, when I2 ≥ 50%, the DerSimonian and Laird random-effects model was employed for meta-analysis; when I2 < 50%, the fixed-effects model was used.
3 Results
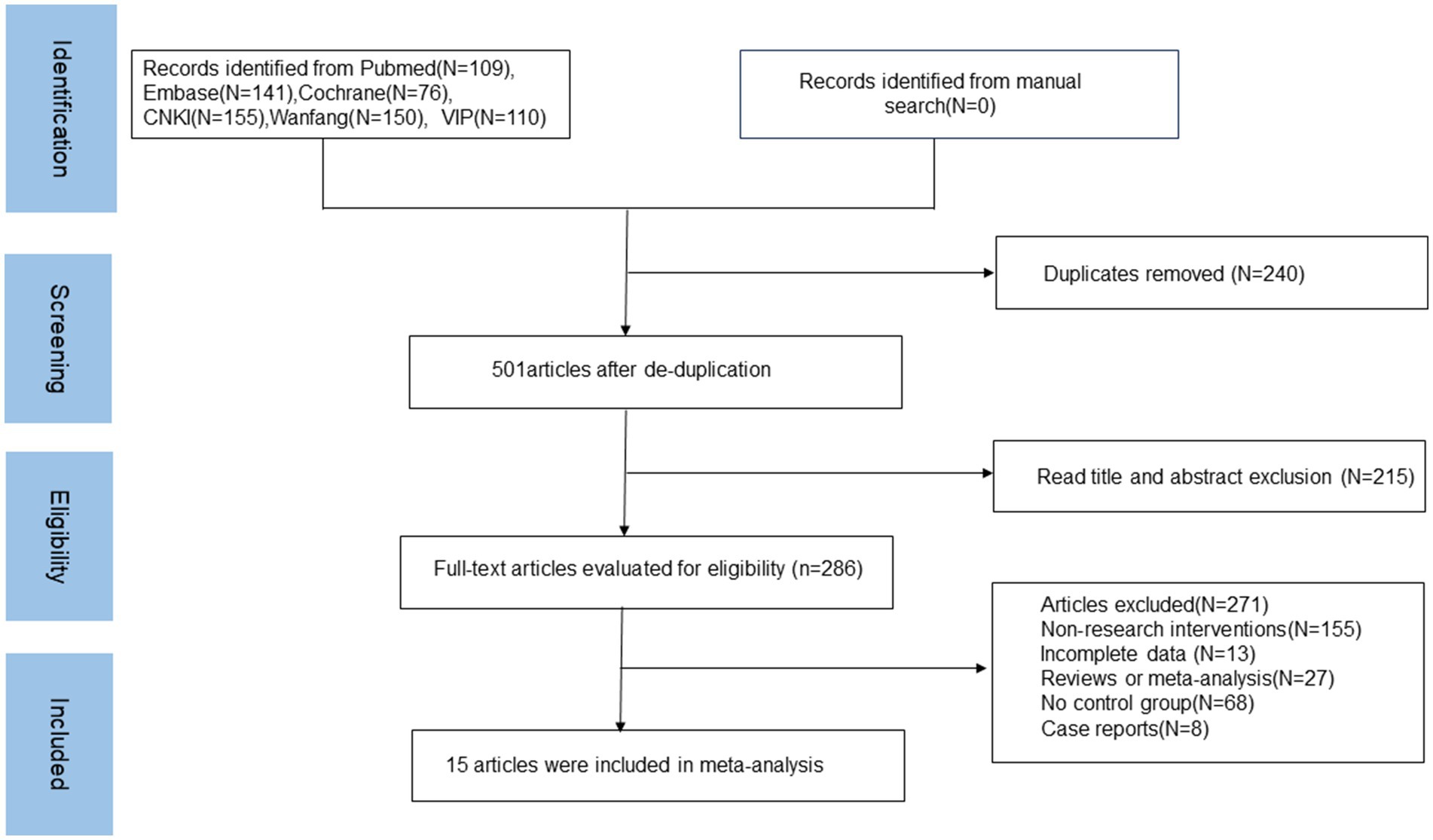
3.1 Literature screening results
A total of 741 articles were retrieved for this study. After removing 240 duplicate articles, 215 articles were excluded based on their titles and abstracts for being irrelevant. The remaining 286 articles were subjected to full-text screening, resulting in the inclusion of 15 articles in the meta-analysis. The literature screening process and results are depicted in Figure 1.
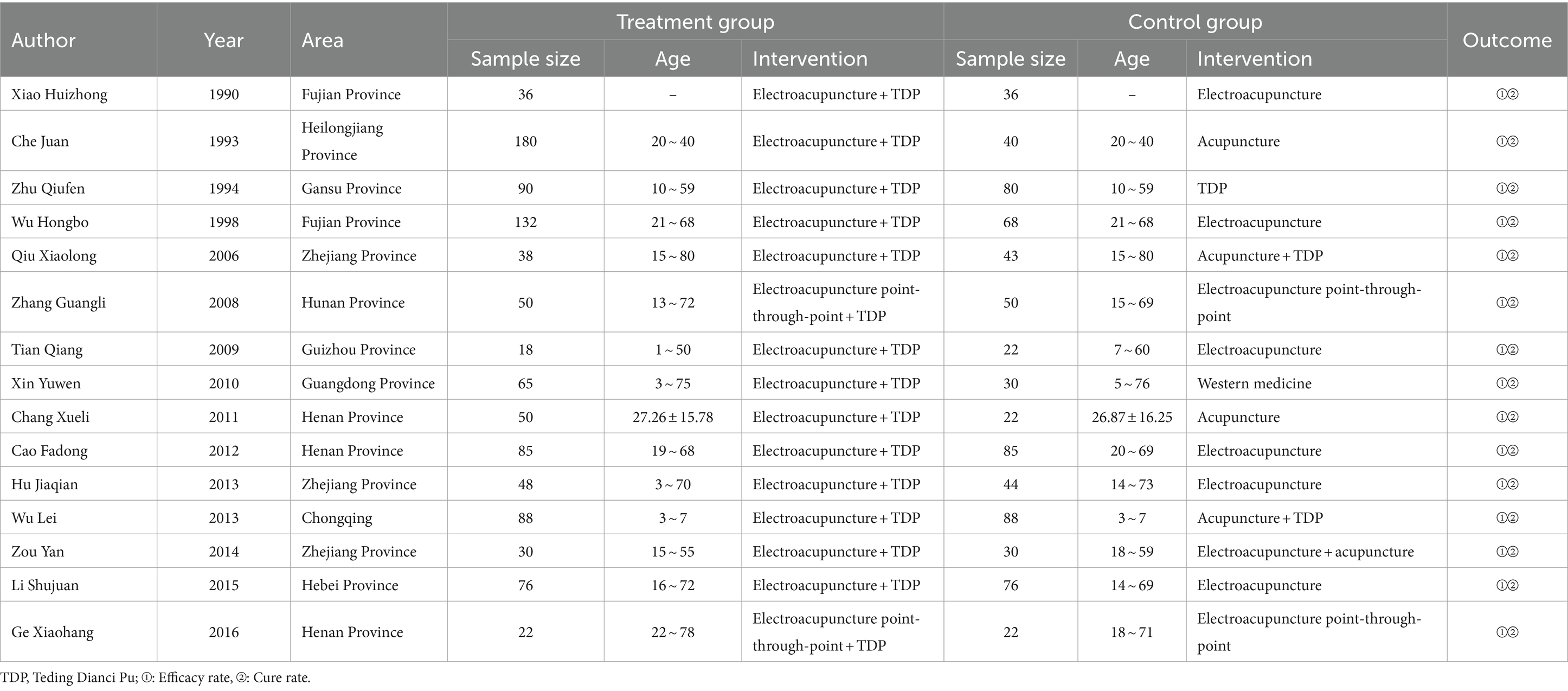
3.2 Basic information of included studies
A total of approximately 1,744 participants were included in all studies (1,008 in the treatment group and 736 in the control group). Table 1 summarizes the basic characteristics of the included studies. The study subjects were all from China. In 13 studies, the intervention for the treatment group was electroacupuncture combined with TDP (15–17, 19–27), while in two studies, the intervention was electroacupuncture point-through-point combined with TDP (28, 29). The control group interventions varied and included electroacupuncture (16, 19, 21–23, 25), acupuncture (15, 20), acupuncture combined with electroacupuncture (15, 20), Western medicine (17, 24), TDP therapy (26), electroacupuncture point-through-point (27), and acupuncture combined with TDP therapy (30). The majority of studies included participants who were minors (N = 11) (15–17, 21, 22, 24–27, 29, 30), while the remaining studies focused exclusively on adult subjects (N = 4) (19, 20, 23, 28).
3.3 Assessment of the quality of included studies
To evaluate the quality of the studies included, we utilized the Jadad scale. Detailed findings are presented in Table 2. The specific scores of the 15 included studies are as follows: there were 2 studies rated as high-quality literature with scores ranging from 4 to 7, both scoring 4 points. Thirteen studies were classified as low-quality literature with scores ≤3, including 2 studies scoring 3 points, 8 studies scoring 2 points, and 3 studies scoring 1 point. Generation of random sequences: Two studies employed randomization and described the correct randomization methods, while eight studies used randomization but did not describe the methods. Randomization concealment: Two studies only mentioned using random number methods or random number tables for random allocation but did not indicate whether this method prevented clinicians and participants from predicting the allocation sequence. Usage of blinding: None of the studies mentioned whether blinding was used.
3.4 Meta-analysis results
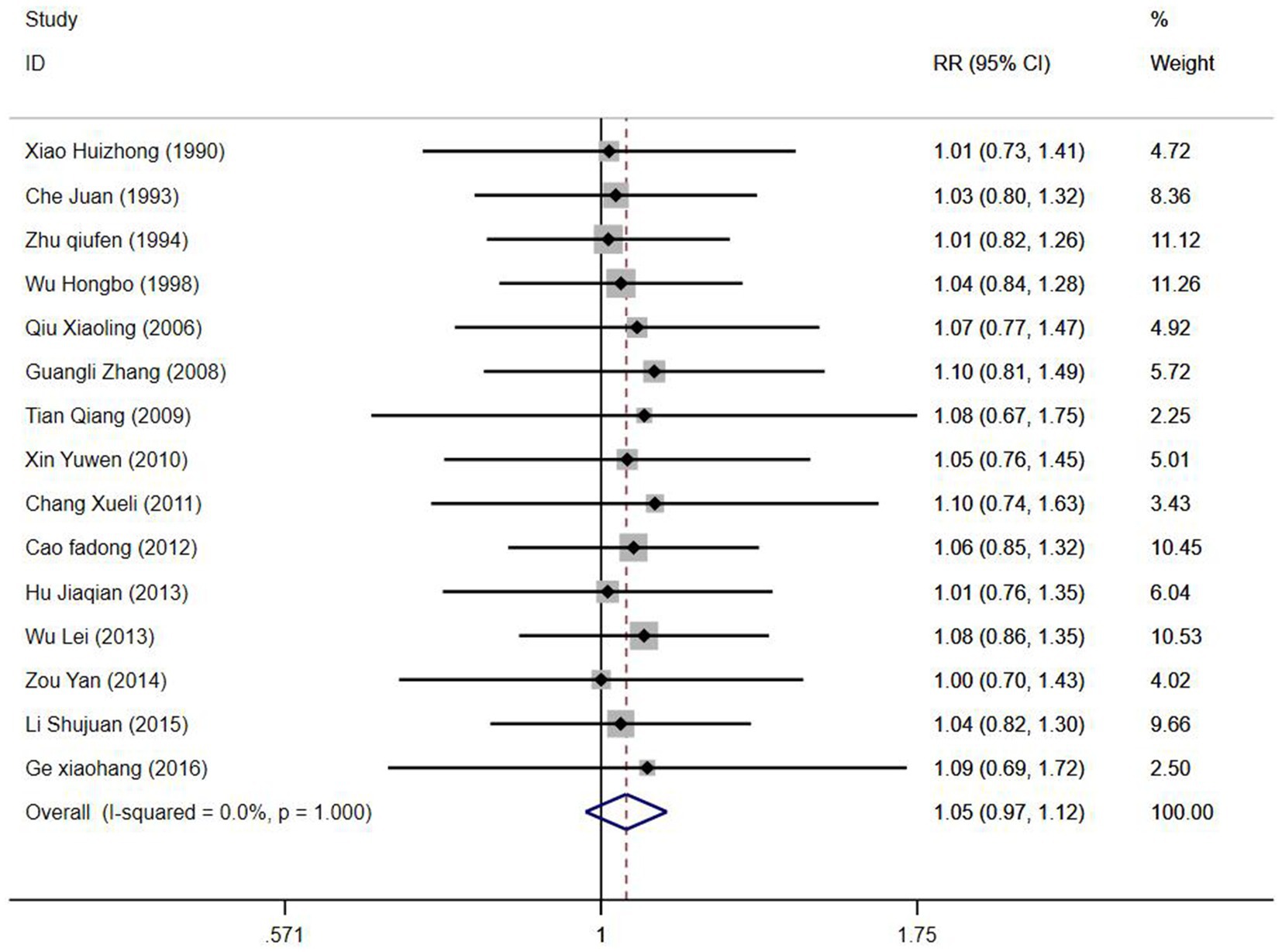
3.4.1 Efficiency rate
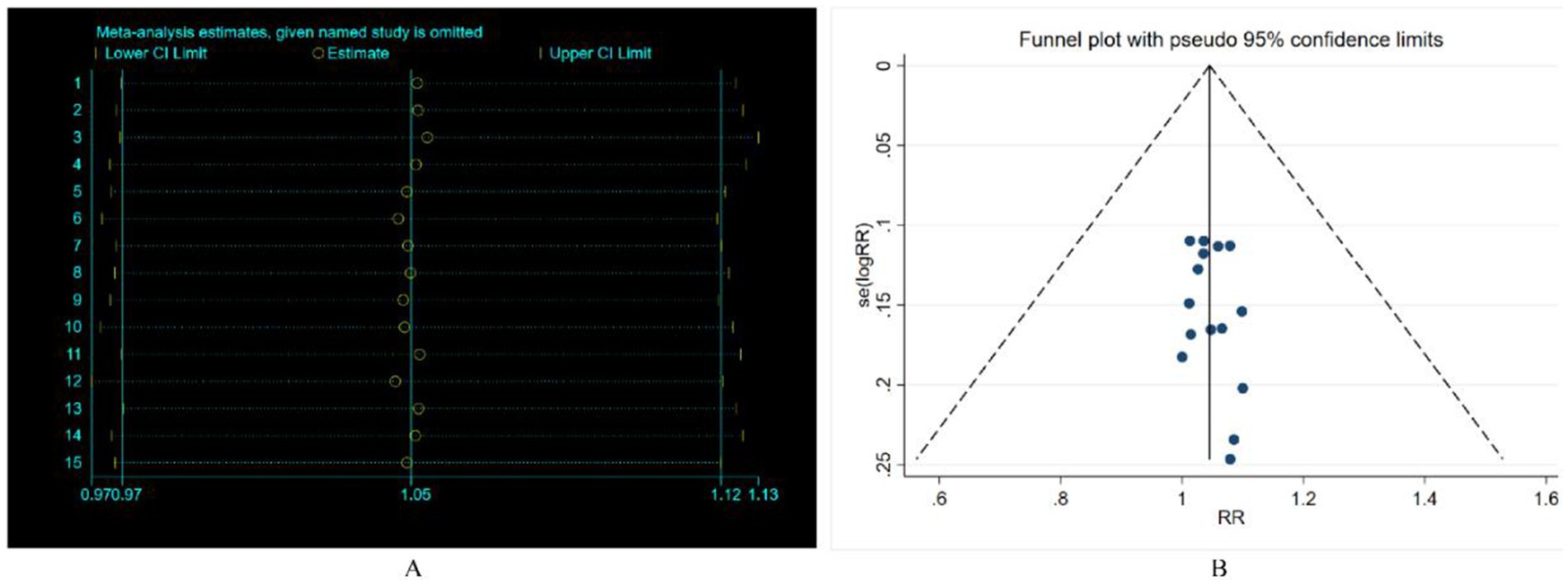
All included studies reported the overall efficacy rate. Heterogeneity test analysis indicated no statistical heterogeneity among the 15 studies (p = 1.00, I2 = 0%), thus employing a fixed-effects model for pooled analysis. Meta-analysis results (Figure 2) revealed no significant difference in overall efficacy rate between electroacupuncture combined with TDP treatment for peripheral facial paralysis and other treatment modalities [OR = 1.05, 95%CI (0.97, 1.12), p = 0.226]. Sensitivity analysis was conducted to assess the stability of the study findings. The results (Figure 3) indicated no significant changes, suggesting stability. Additionally, Egger’s test (T = 0.98, p = 0.345) and funnel plot results revealed no apparent publication bias (Figure 4). Stratification based on factors such as the inclusion of minors and whether electroacupuncture was used as a control intervention showed no significant variations in study outcomes (Figure 5).
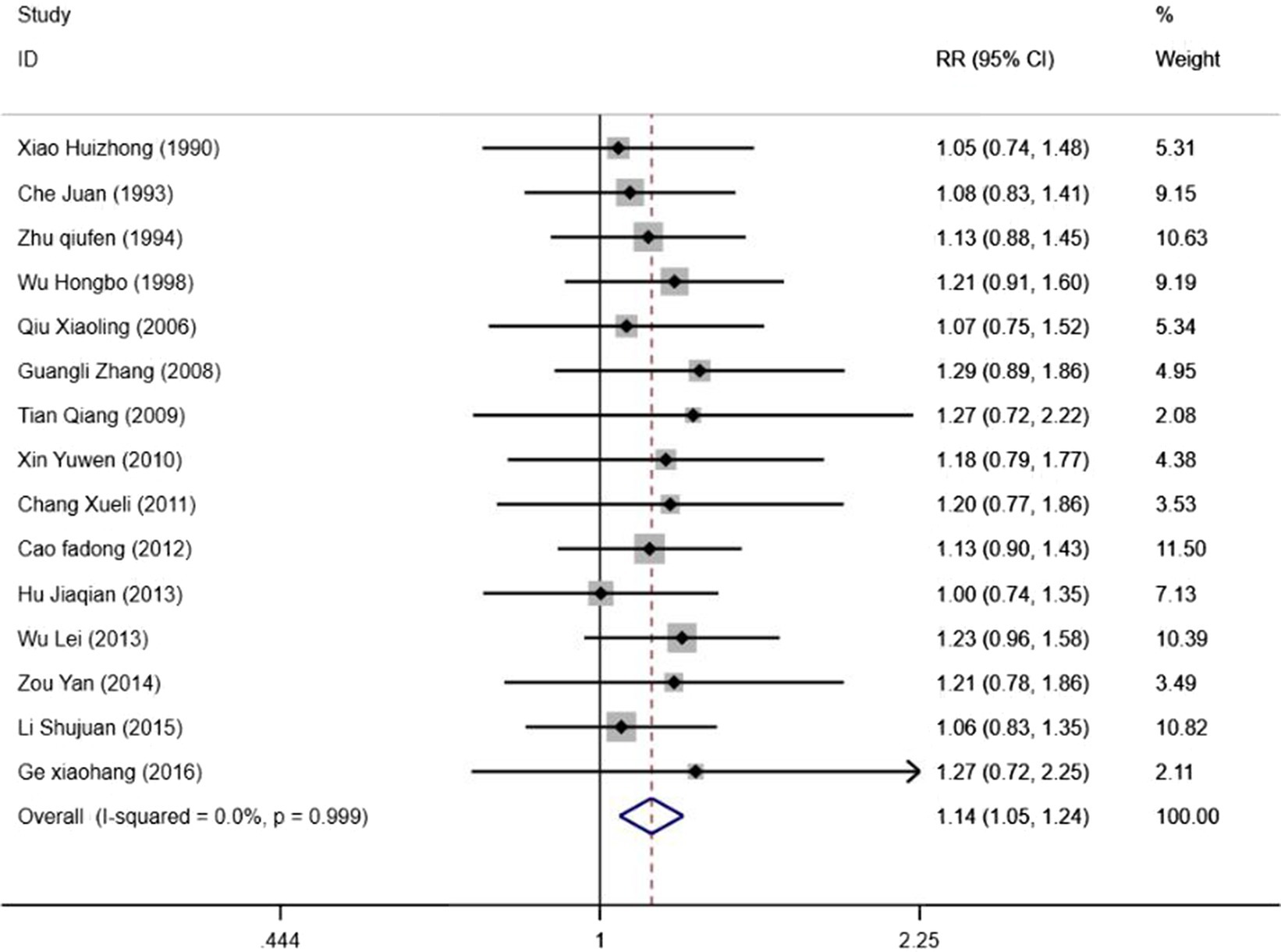
3.4.2 Cure rate
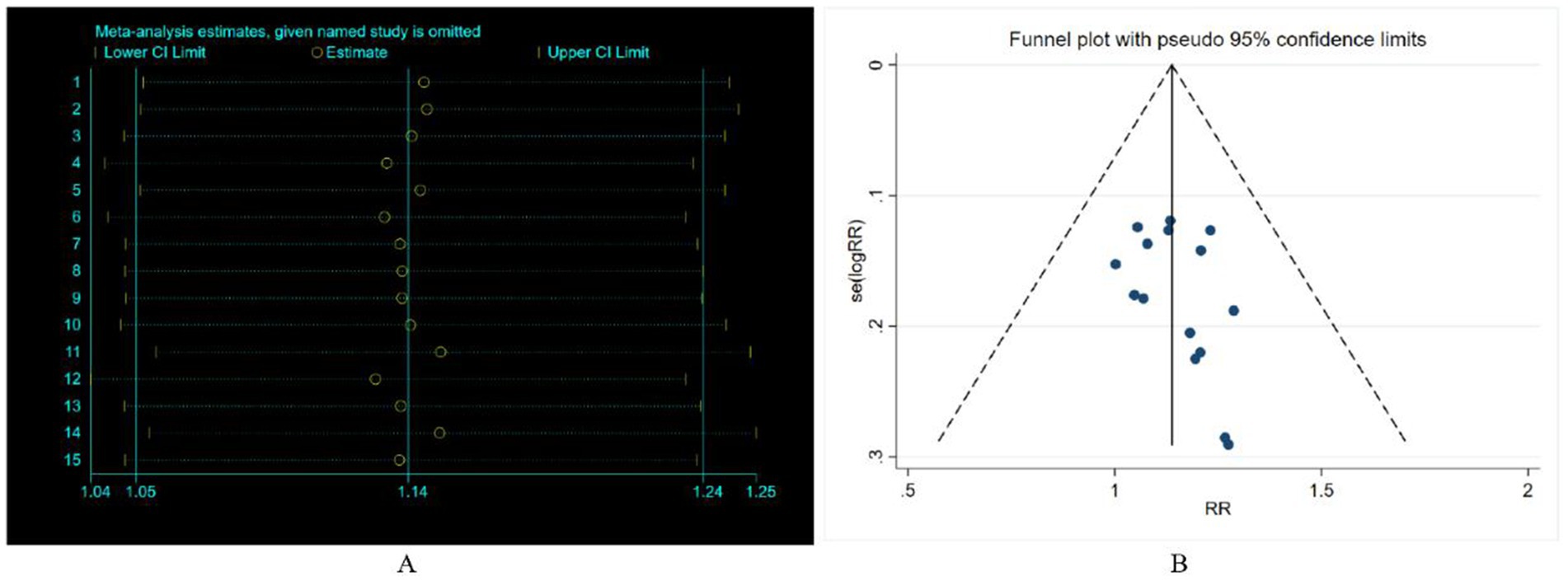
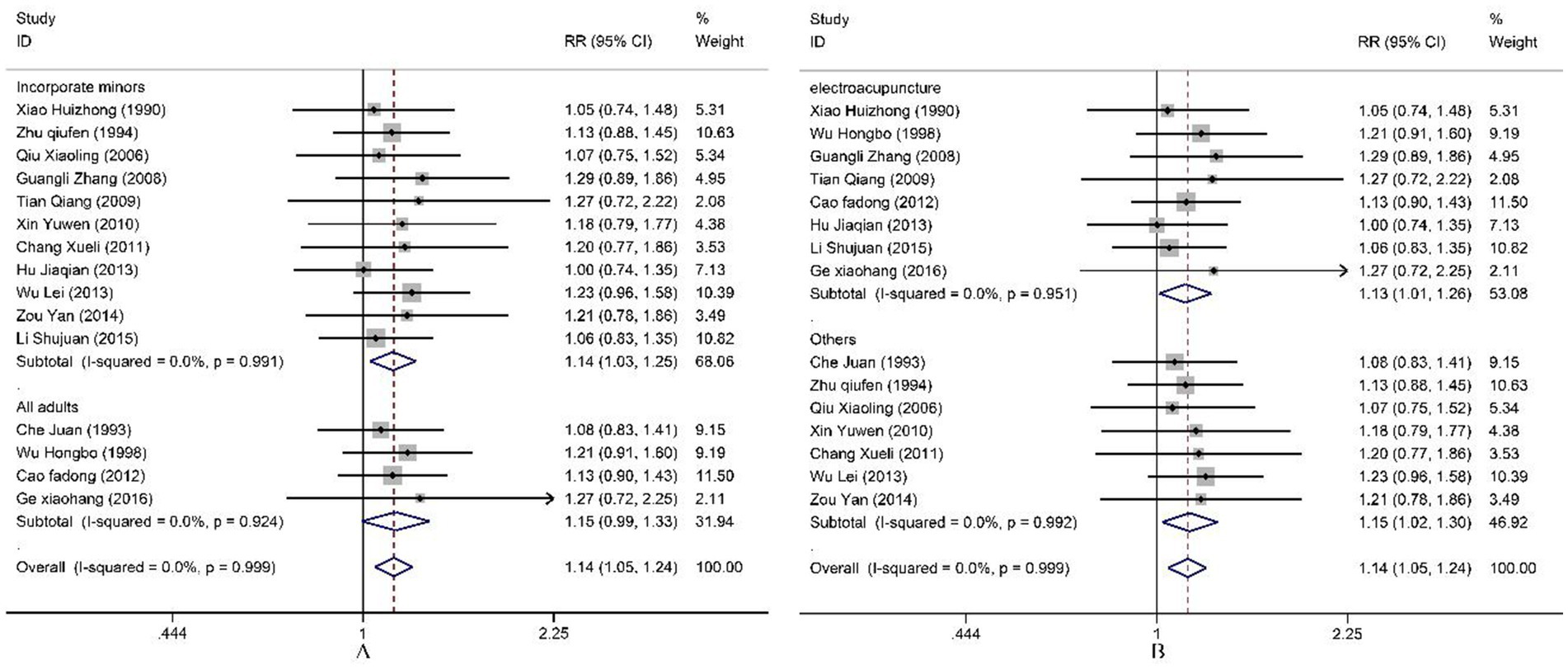
All included studies reported both cure rate and efficacy rate. Consequently, our study pooled the results for the cure rate. Heterogeneity testing revealed no statistical heterogeneity among the 15 studies (p = 1.00, I2 = 0.966%). Therefore, a fixed-effect model was employed for the combined analysis. The Meta-analysis results (Figure 5) demonstrate that electroacupuncture combined with TDP therapy significantly outperformed other treatment methods in terms of cure rate [OR = 1.14, 95%CI (1.05, 1.24), p = 0.002]. To assess the robustness of these findings, a sensitivity analysis was conducted (Figure 6). The results indicate that there were no significant changes, suggesting that the results are stable. Additionally, Egger’s test (T = 1.42, p = 0.180) and the funnel plot results revealed no significant publication bias (Figure 6). When stratified by the inclusion of minors in the study population, it was observed that in studies including minors, the combination of electroacupuncture and TDP therapy demonstrated superior efficacy in treating peripheral facial paralysis compared to other therapeutic modalities [OR = 1.14, 95% CI (1.03, 1.25), p = 0.011]. Conversely, in studies where the population comprised solely adults, no significant difference was found between the combination therapy and other treatments [OR = 1.15, 95% CI (0.99, 1.33), p = 0.059] (Figure 7). Stratification based on whether the control group interventions included electroacupuncture did not alter the results significantly. Regarding the rate of marked improvement, electroacupuncture combined with TDP therapy was superior to both monotherapy [OR = 1.13, 95% CI (1.01, 1.26), p = 0.032] and other therapeutic methods [OR = 1.15, 95% CI (1.02, 1.30), p = 0.020].
4 Discussion
Peripheral facial paralysis is an inflammatory disorder induced by various etiologies that result in facial nerve impairment. Presently, the incidence rate of peripheral facial paralysis in China ranks sixth among all neurological disorders, with approximately 3 million cases annually (31), surpassing the annual incidence rate of 20 per 100,000 in Western countries (32).
In contemporary clinical practice, the predominant therapeutic approach for patients with peripheral facial paralysis involves pharmacological treatment. However, medication cycles typically require a longer recovery time, with poorer outcomes and prognosis for quality of life. In comparison, external treatments in traditional Chinese medicine exhibit significant therapeutic advantages in the clinical treatment of peripheral facial paralysis (33–35). Electroacupuncture demonstrates considerable benefits over conventional Western medicine (36) and acupuncture alone (30). Furthermore, the thermal effects generated by TDP electromagnetic waves have biological effects such as enhancing metabolism, improving microcirculation in lesioned tissues, reducing inflammation, providing analgesic effects, and boosting immunity (37). TDP has been proven to have significant therapeutic effects in many clinical fields, with its application becoming increasingly widespread. Therefore, this study aims to conduct a systematic review and meta-analysis of randomized controlled trials on electroacupuncture combined with TDP for the treatment of peripheral facial paralysis, to evaluate the effectiveness of electroacupuncture combined with TDP in treating peripheral facial paralysis.
The findings of this study indicate that the efficacy rate of electroacupuncture combined with TDP therapy for treating peripheral facial paralysis shows no significant difference when compared to other therapeutic methods. This consistency in results persists across various subgroups. There is a certain heterogeneity in this study, which is mainly caused by the different measures of the control group, the inconsistent evaluation criteria of curative effect and the small sample size. Notably, the recovery rate for peripheral facial paralysis treated with electroacupuncture combined with TDP therapy surpasses that of other methods. Subgroup analysis further reveals that, among pediatric populations, the recovery rate for electroacupuncture combined with TDP therapy is superior to other treatments. Regardless of whether the comparison is with standalone electroacupuncture or alternative therapies, the recovery rate for electroacupuncture combined with TDP therapy remains higher. However, it is crucial to note that the methodological quality and reporting standards of the included studies are generally low, and the sample sizes are limited, which constrains the overall reliability of this systematic review. In this sense, large randomized controlled trials with higher quality requirements need to be conducted to validate the efficacy of electroacupuncture combined with TDP in the treatment of peripheral facial palsy.
There are several limitations inherent in this study. Firstly, both the treatment and control groups utilized electroacupuncture for peripheral facial paralysis; however, there was no description of the waveform or timing of the electroacupuncture application. Variations in waveform (38, 39) and timing (40, 41) can significantly impact the efficacy of treatment for peripheral facial paralysis. Secondly, the control group was subjected to multiple therapeutic interventions, which may have confounded the results and affected their generalizability. The sample size of the included research is small, and the research results may lack representativeness. Furthermore, none of the included studies employed blinding techniques, potentially introducing a degree of bias into the findings. It is suggested that large-scale, high-quality randomized controlled trials should be carried out in future research, and stricter blind method and randomization procedures should be included. In addition, it is suggested that the measurement of the results should be further standardized.
5 Conclusion
Meta-analysis showed that the effective rate of electroacupuncture combined with TDP in the treatment of peripheral facial paralysis was not significantly different from other treatment methods, and the recovery rate was better than other treatment methods. Subgroup analysis showed that the recovery rate of electroacupuncture combined with TDP in the treatment of peripheral facial paralysis was better than other methods in the minor population; whether electroacupuncture alone or other treatment methods, the recovery rate of electroacupuncture combined with TDP in the treatment of peripheral facial paralysis was better than other methods.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
H-WG: Writing – original draft, Writing – review & editing. Q-CX: Writing – original draft, Writing – review & editing. Z-HL: Writing – original draft, Writing – review & editing. WC: Writing – original draft, Writing – review & editing. YL: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by Joint Project between the Science and Technology Department of State Administration of Traditional Chinese Medicine and Shandong Province China (GZY-KJS-SD-2023-050) and High-level Talent Project of Traditional Chinese Medicine in Shandong Province China (LWH [2023] No. 143) and Acupuncture and Moxibustion, a key subject of traditional Chinese medicine in Shandong province (LWTCMSEZ [2022] No. 4).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2024.1450312/full#supplementary-material
References
1. Baugh, RF, Basura, GJ, Ishii, LE, Schwartz, SR, Drumheller, CM, Burkholder, R, et al. Clinical practice guideline: Bell's palsy. Otolaryngol Head Neck Surg. (2013) 149:S1–S27. doi: 10.1177/0194599813505967
2. Yunyun, B, Lin, C, Yiwu, D, Chen, L, Zhang, ZQ, Bu, YY, et al. Clinical guidelines for the treatment of idiopathic facial paralysis in China (2022 edition). Neural Injury Funct Reconstruct. (2023) 18:1–12. doi: 10.16780/j.cnki.sjssgncj.20220639
3. de Almeida, JR, Guyatt, GH, Sud, S, Dorion, J, Hill, MD, Kolber, MR, et al. Management of Bell palsy: clinical practice guideline. CMAJ. (2014) 186:917–22. doi: 10.1503/cmaj.131801
5. Han, PJ, Guo, KF, He, JY, and Jin, GX. Observation on the efficacy of facial muscle functional training combined with hormone treatment for acute stage Bell's facial paralysis. J Med Theory Pract. (2021) 34:2773–5. doi: 10.19381/j.issn.1001-7585.2021.16.012
6. Zhang, HY. Effect of small needle knife cooperated with hyperbaric oxygen and neurotrophic drugs in the treatment of intractable facial paralysis. China Med Herald. (2017) 14:163–6.
7. Fang, LJ, Xu, Y, and Wang, CY. Research Progress on acupuncture and Moxibustion for sequelae of peripheral facial paralysis. New Chin Med. (2023) 55:190–3. doi: 10.13457/j.cnki.jncm.2023.03.042
8. Wang, WH, Jiang, RW, and Liu, NC. Electroacupuncture is effective for peripheral facial paralysis: a meta-analysis. Evid Based Complement Alternat Med. (2020) 2020:5419407. doi: 10.1155/2020/5419407
9. Yang, LS, Zhou, DF, Zheng, SZ, Zhao, BM, Li, HG, Chen, QQ, et al. Early intervention with acupuncture improves the outcome of patients with Bell's palsy: a propensity score-matching analysis. Front Neurol. (2022) 13:943453. doi: 10.3389/fneur.2022.943453
10. Chen, WQ, and Li, Q. Electroacupuncture combined with Qianzhengsan decoction for the treatment of peripheral facial paralysis: a retrospective study. Medicine. (2022) 101:e30740. doi: 10.1097/MD.0000000000030740
11. Liu, X. Clinical observation on 60 cases of facial neuritis treated by Electroacupuncture combined with microwave and intermediate frequency pulse electric. China Med Device Informat. (2022) 28:131–3. doi: 10.3969/j.issn.1006-6586.2022.02.044
12. Yu, J, Sun, ZR, and Li, HL. Consideration on intervening time of acupuncture and Moxibustion in treating peripheral facial paralysis as well as diversification of treatment methods. J Shandong Univ Tradit Chin Med. (2020) 44:333–8. doi: 10.16294/j.cnki.1007-659x.2020.03.022
13. Zhao, HT. Failure analysis and maintenance of TDP. Med Equip. (2015) 7:125. doi: 10.3969/j.issn.1002-2376.2015.07.078
14. Barolet, D, Christiaens, F, and Hamblin, MR. Infrared and skin: friend or foe. J Photochem Photobiol B. (2016) 155:78–85. doi: 10.1016/j.jphotobiol.2015.12.014
15. Chang, XL. The observation of treating peripheral facial paralysis by electro-acupuncture plus TDP. Clin J Chin Med. (2011) 3:65–6. doi: 10.3969/j.issn.1674-7860.2011.13.035
16. Li, SJ, and Liu, WH. Clinical analysis of 76 cases of peripheral facial paralysis treated with electroacupuncture plus microwave synthesis. J Hebei North Univ. (2015) 3:81–2. doi: 10.3969/j.issn.1673-1492.2015.03.022
17. Zou, Y, Ma, ZR, Shen, JP, and Liu, WZ. Acupuncture combined with electroacupuncture therapy plus TDP irradiation for the treatment of peripheral facial paralysis in 30 cases. Tradit Chin Med Res. (2014) 27:62–3. doi: 10.3969/j.issn.1001-6910.2014.02.31
18. Oremus, M, Wolfson, C, Perrault, A, Demers, L, Momoli, F, and Moride, Y. Interrater reliability of the modified Jadad quality scale for systematic reviews of Alzheimer's disease drug trials. Dement Geriatr Cogn Disord. (2001) 12:232–6. doi: 10.1159/000051263
19. Cao, FD. Clinical observation of electroacupuncture combined with TDP in the treatment of peripheral facial paralysis. Chin Commun Doct. (2012) 14:185. doi: 10.3969/j.issn.1007-614x.2012.23.170
20. Che, J, Li, L, and Zhao, LZ. Effect of electroacupuncture and TDP irradiation in the treatment of 180 cases of peripheral facial paralysis. J Mudanjiang Med Coll. (1993) 1:32.
21. Hu, JQ, and Li, KP. Electro-acupuncture plus TDP treating 48 cases of peripheral facial paralysis. Liaoning J Tradit Chin Med. (2013) 40:2574–5. doi: 10.13192/j.issn.1000-1719.2013.12.074
22. Tian, Q, Li, Y, Zhang, SZ, Luo, CL, Wang, YJ, and Nie, ZH. Analysis of the therapeutic effect of electroacupuncture with TDP lamp irradiation in the treatment of peripheral facial paralysis. J Zunyi Med Univ. (2009) 32:467–70. doi: 10.3969/j.issn.1000-2715.2009.05.012
23. Wu, HB. Therapeutic effect of electroacupuncture with TDP in the treatment of peripheral facial paralysis in 132 cases. Fujian Med J. (1998) 20:96-96.
24. Wu, L. Observations on 88 cases of acute peripheral facial paralysis in young children treated with electroacupuncture. Proceedings of the 4th International Science and Technology Conference on the Modernization of Traditional Chinese Medicine. (2013):1–5.
25. Xiao, HZ. Comparison of the efficacy of electroacupuncture and TDP in the treatment of peripheral facial paralysis in 72 cases. J Sichuan Tradit Chin Med. (1990) 3:50.
26. Xin, YW. Electroacupuncture and TDP treatment for facial nerve palsy in 65 cases. Inner Mong J Tradit Chin Med. (2010) 29:31–2. doi: 10.3969/j.issn.1006-0979.2010.10.040
27. Zhu, QF. Treatment of 90 cases of acute facial neuritis with TDP plus electroacupuncture. Chin Acupunct Moxibust. (1994) S1:421.
28. Ge, XH, Meng, FD, and Liu, LX. Observation on the curative effect of penetration needling combined with TDP in the treatment of 22 patients with peripheral facial nerve paralysis. Chine Commun Doct. (2016) 32:87–8. doi: 10.3969/j.issn.1007-614x.2016.1.54
29. Zhang, GL. Effect of electroacupuncture point-through-point and TDP in the treatment of peripheral facial neuritis in 50 cases. Chin J Tradit Med Sci Technol. (2008) 15:4. doi: 10.3969/j.issn.1005-7072.2008.02.070
30. Qiu, XL. Effect of electroacupuncture with TDP lamp in the treatment of facial nerve paralysis in 78 cases In: The fifth academic seminar of neurology professional Committee of Zhejiang Association of integrated Chinese and Western medicine integrated neurology class. Ninghai, Zhejiang, China: (2006). 2.
31. Tm, O. Medical Management of Acute Facial Paralysis. Otolaryngol Clin N Am. (2018) 51:1051–75. doi: 10.1016/j.otc.2018.07.004
32. Neurology Branch of the Chinese Medical Association, neuromuscular disease Group of Neurology Branch of the Chinese Medical Association, Electromyography and Clinical Neurophysiology Group of Neurology Branch of the Chinese Medical Association . Chinese guidelines for the diagnosis and treatment of idiopathic facial nerve palsy. Chin J Neurol. (2016) 2:84–6. doi: 10.3760/cma.j.issn.1006-7876.2016.02.002
33. Li, M, Zhu, SS, Wan, QR, Ruan, JG, Wang, YJ, Xu, TS, et al. Effect of warm acupuncture at Yifeng (TE 17) on facial paralysis with periauricular pain during pregnancy. Zhongguo Zhen Jiu. (2020) 40:1281–5. doi: 10.13703/j.0255-2930.20191128-k0002
34. Wang, B, Wang, JW, and Li, H. Observation on therapeutic effect of peripheral facial paralysis treated by string puncture combined with electroacupuncture. Zhongguo Zhen Jiu. (2011) 31:47–50.
35. Zhu, P, Wang, H, Zhang, L, and Jiang, X. Deep learning-based surface nerve electromyography data of E-health Electroacupuncture in treatment of peripheral facial paralysis. Comput Math Methods Med. (2022) 2022:8436741–12. doi: 10.1155/2022/8436741
36. Xiao, SH. Clinical effects of electroacupuncture in the treatment of peripheral facial paralysis. Bao Jian Wen Hui. (2023) 24:61–4.
37. Ye, C. Clinical observation on curative of massage combined with TDP in the treatment of tibial fatigue periostitis. Guangdong: Guangzhou University of Traditional Chinese Medicine (2017).
38. Tong, ZZ. Clinical observation of low-frequency electrical stimulation in the treatment of facial paralysis. Master. (2012)
39. Chen, Q, Chen, F, Li, YN, Bao, WT, and Zhang, H. Clinical efficacy of electroacupuncture dilatational wave treatment of acute-stage facial paralysis. Acupunct Electrother Res. (2021) 46:405–18. doi: 10.3727/036012921X16237619666085
40. Qu, QW, and Xiong, T. Clinical observation on electroacupuncture for treatment of peripheral facial paralysis at different stages. Zhongguo Zhen Jiu. (2005) 25:323–5.
Keywords: peripheral facial paralysis, electroacupuncture, TDP, meta-analysis, complementary therapies
Citation: Gao H-W, Xia Q-C, Li Z-H, Chen W and Lu Y (2024) Efficacy analysis of electroacupuncture plus TDP in the treatment of peripheral facial paralysis: a systematic review and meta-analysis. Front. Neurol. 15:1450312. doi: 10.3389/fneur.2024.1450312
Edited by:
Jun Zhong, Shanghai Jiao Tong University, ChinaReviewed by:
Xiangping Peng, Waseda University, JapanShu-Yun Guo, Second Hospital of Hebei Medical University, China
Copyright © 2024 Gao, Xia, Li, Chen and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Lu, bHUzdXlhbjVfNGYwamFAeWVhaC5uZXQ=
†These authors have contributed equally to this work
 Hua-Wei Gao1†
Hua-Wei Gao1† Yan Lu
Yan Lu