- Third Department of Psychiatry, Yancheng Fourth People's Hospital, Yancheng, China
Background: Psychiatric disorders may be associated with an elevated risk of stroke; however, the existence of variations in this association between different populations remains controversial. Consequently, we conducted a comprehensive systematic review and meta-analysis to examine the magnitude of the relationship between psychiatric disorders and the risk of stroke.
Methods: The PubMed, Embase, and Cochrane Library databases were systematically searched to identify eligible studies from inception to April 2024. The aggregated findings were expressed as relative risks (RRs) with 95% confidence intervals (CIs), and the combined analysis was performed using a random-effects modeling approach. Further exploratory analyses were also performed using sensitivity and subgroup analyses.
Results: A total of 36 cohort studies, involving 25,519,635 individuals, were selected for analysis. We noted that depression (RR: 1.50; 95% CI: 1.34–1.68; p < 0.001), schizophrenia (RR: 1.74; 95% CI: 1.36–2.24; p < 0.001), and bipolar disorder (RR: 1.65; 95% CI: 1.27–2.14; p < 0.001) were associated with an elevated risk of stroke. Further exploratory analyses found that the association between depression and the risk of stroke differed according to the adjusted level (RR ratio: 0.77; 95% CI: 0.61–0.98; p = 0.034), and the association between schizophrenia and the risk of stroke differed according to the outcome definition (RR ratio: 0.68; 95% CI: 0.52–0.90; p = 0.006). Moreover, the association between bipolar disorder and the risk of stroke differed according to the study design (RR ratio: 0.68; 95% CI: 0.55–0.84; p < 0.001).
Conclusion: The significant association between psychiatric disorders and an elevated risk of stroke highlights the importance of enhanced monitoring and stroke prevention in patients with psychiatric disorders.
Systematic review registration: Our study was registered on the INPLASY platform (number: INPLASY202450049).
Introduction
By 2019, stroke remained the third leading cause of disability and the second leading cause of death globally due to its high incidence, disability rates, and mortality rates (1). Furthermore, stroke imposes a huge economic burden, leading to substantial healthcare expenditures and significant global impacts (2). Guidelines and recommendations for secondary stroke prevention at the national and international levels depend heavily on lifestyle changes (3). A previous study has shown that 90% of strokes are caused by 10 modifiable risk factors, either individually or in combination (4). By adopting lifestyle choices such as healthy eating, physical activity, maintaining normal body weight, moderate alcohol consumption, and avoiding smoking, stroke patients can lower their cardiovascular mortality rate by up to 92% over the next 10 years (5). Stroke patients typically have uncontrolled modifiable risk factors. In addition, the presence of multiple comorbidities is concerning as it is significantly associated with the prognosis of stroke patients (6).
Psychiatric disorders are a common issue in the global healthcare system. These disorders are considered a major cause of disability, contributing to 14% of the global disease burden (7). In some high-income countries, it is estimated that 40% of disabilities are caused by mental disorders (8). Psychiatric disorders are also common in the working population and are increasingly recognized due to their impact on the productivity of both employees and organizations (7). According to earlier reports, individuals diagnosed with severe psychiatric disorders (such as schizophrenia and bipolar disorder) have a life expectancy that is 15–20 years shorter than that of the general population, with cardiovascular disease being a significant cause of death among them (9–11). The relationship between psychiatric disorders and stroke is bidirectional. On the one hand, individuals with psychiatric disorders may have an increased risk of stroke, partly due to the impact of their mental health condition on other aspects of their physical health. On the other hand, stroke itself can lead to psychiatric disorders, as it affects the quality of life and psychological state of patients (12). To delve deeper into the potential causality between psychiatric disorders and the occurrence and development of stroke, we performed this systematic review and meta-analysis to assess the association between psychiatric disorders and the risk of stroke based on cohort studies.
Methods
Data sources, search strategy, and selection criteria
Based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines published in 2020, this review adhered to and reported the recommended items (13). Our study was registered on the INPLASY platform (number: INPLASY202450049). This meta-analysis included any cohort studies that examined the relationship between psychiatric disorders and the risk of stroke, without restrictions on language or publication status (published, in press, or ongoing). Studies were included if they met the following criteria: (1) Participants comprised those who were stroke-free at the start of the study; (2) The exposure variable included psychiatric disorders, such as bipolar disorder, schizophrenia, and depression; (3) controls consisted of individuals without psychiatric disorders; (4) outcomes compared the risk of stroke between individuals with and without psychiatric disorders; and (5) the study design necessitated a cohort structure for all included studies.
We retrieved articles that were published between inception and April 2024 from the PubMed, Embase, and Cochrane Library electronic databases using the search terms “bipolar disorder” OR “schizophrenia” OR “depression” AND (“stroke risk” OR “risk of stroke”). The details of the search strategy in each database is shown in Supplementary material 1. In addition, we meticulously examined the bibliographies of all relevant primary and review articles to identify further studies that met our criteria. The selection of the relevant studies was based on medical subject headings, research methodologies, patient cohorts, study design, specified exposures, and resultant outcome measures. The literature search was carried out independently by two authors using standardized methodologies. Any discrepancies encountered were resolved by the corresponding author until mutual agreement was achieved.
Data collection and quality assessment
The two authors extracted key information from the independent studies, including the study group name, publication year, study design, geographical region, study period, sample size, age range or mean age, male proportion, exposure and assessment methods, reported outcomes, follow-up duration, adjusted factors, and effect estimates with 95% confidence intervals (CIs). For studies reporting several multivariable-adjusted effect estimates, we selected the effect estimate with the maximal adjustment for potential confounders. The two authors then used the Newcastle–Ottawa Scale (NOS) for methodological quality assessment, which has been partially validated for the quality assessment of observational studies in meta-analyses (14). Any inconsistencies between the authors regarding the data collection and quality assessment were resolved by an additional author, who referred to the original studies.
Statistical analysis
We analyzed the association between psychiatric disorders and the risk of stroke based on the effect estimates and their 95% CIs reported in each study. As this study’s analysis was based on a cohort design, we used the relative risk (RR) as the pooled effect estimate, and all analyses were conducted using a random-effects model to account for potential heterogeneity across the studies (15, 16). We used I2 and Q statistics to analyze potential heterogeneity among the studies. Heterogeneity was considered significant if I2 ≥ 50% or p < 0.10 (17, 18). We also systematically excluded each study from the meta-analysis and conducted a sensitivity analysis to assess the stability of the pooled conclusions and investigate the potential sources of heterogeneity (19). Subgroup analyses were also performed based on study design, geographical region, mean age, sex, stroke type, reported outcomes, follow-up duration, and adjusted levels, and the differences between the subgroups were compared using the interaction t-test, assuming the data followed a normal distribution (20). Publication bias was assessed using both qualitative and quantitative methods, including visual inspection of funnel plot symmetry, Egger’s test, and Begg’s test (21, 22). All reported p-values were two-sided, and a p-value of <0.05 was considered statistically significant for the meta-analysis. STATA software (version 12.0; Stata Corp, College Station, TX, USA) was used for the analysis.
Results
Literature search
The study selection process is shown in Figure 1. We initially identified 1,148 articles through the electronic searches, of which 1,012 were excluded after removing duplicates and irrelevant studies. After the full-text review of the remaining 136 articles, 92 articles were excluded, leaving 44 studies. Of these, a total of 36 study cohorts were selected for the final analysis (23–66). Manual searching of the reference lists of these studies did not identify any additional studies meeting the criteria. The general characteristics of the included studies are shown in Table 1, and the outcome ascertainment for each study is summarized in Supplementary material 2.
Study characteristics
Of the 36 included cohorts, 29 were prospective, while the remaining seven were retrospective. These studies involved a total of 25,519,635 individuals, and the sample size ranged from 494 to 10,631,208. Moreover, the follow-up duration ranged from 2.1 to 24.0 years. A total of 29 cohorts were performed in Western countries, while the remaining seven studies were conducted in Eastern countries. The quality of the studies was assessed using the NOS scoring system, and all included studies were of high quality. Among them, eight studies scored 9 stars, 16 studies scored 8 stars, and the remaining 12 studies scored 7 stars.
Depression
A total of 28 cohorts reported an association between depression and the risk of stroke. The summary RR indicated that depression was associated with an elevated risk of stroke (RR: 1.50; 95% CI: 1.34–1.68; p < 0.001), and significant heterogeneity was observed across the included studies (I2 = 82.3%; p < 0.001) (Figure 2). The sensitivity analysis indicated that the pooled conclusion for the relationship between depression and stroke risk remained stable after sequentially removing each study (Supplementary material 3 [Figure S1]). The subgroup analyses found that depression was associated with an elevated risk of stroke in most subsets, while no significant association was observed between depression and hemorrhagic stroke (Table 2). Furthermore, we found that the association between depression and stroke was significantly weaker in the subgroup with fully adjusted results compared to the subgroup with generally adjusted results (RR ratio: 0.77; 95% CI: 0.61–0.98; p = 0.034). There was no significant publication bias for the association between depression and the risk of stroke (p-value for the Egger’s test: 0.074; p-value for the Begg’s: 0.221; Supplementary material 4 [Figure S1]).
Schizophrenia
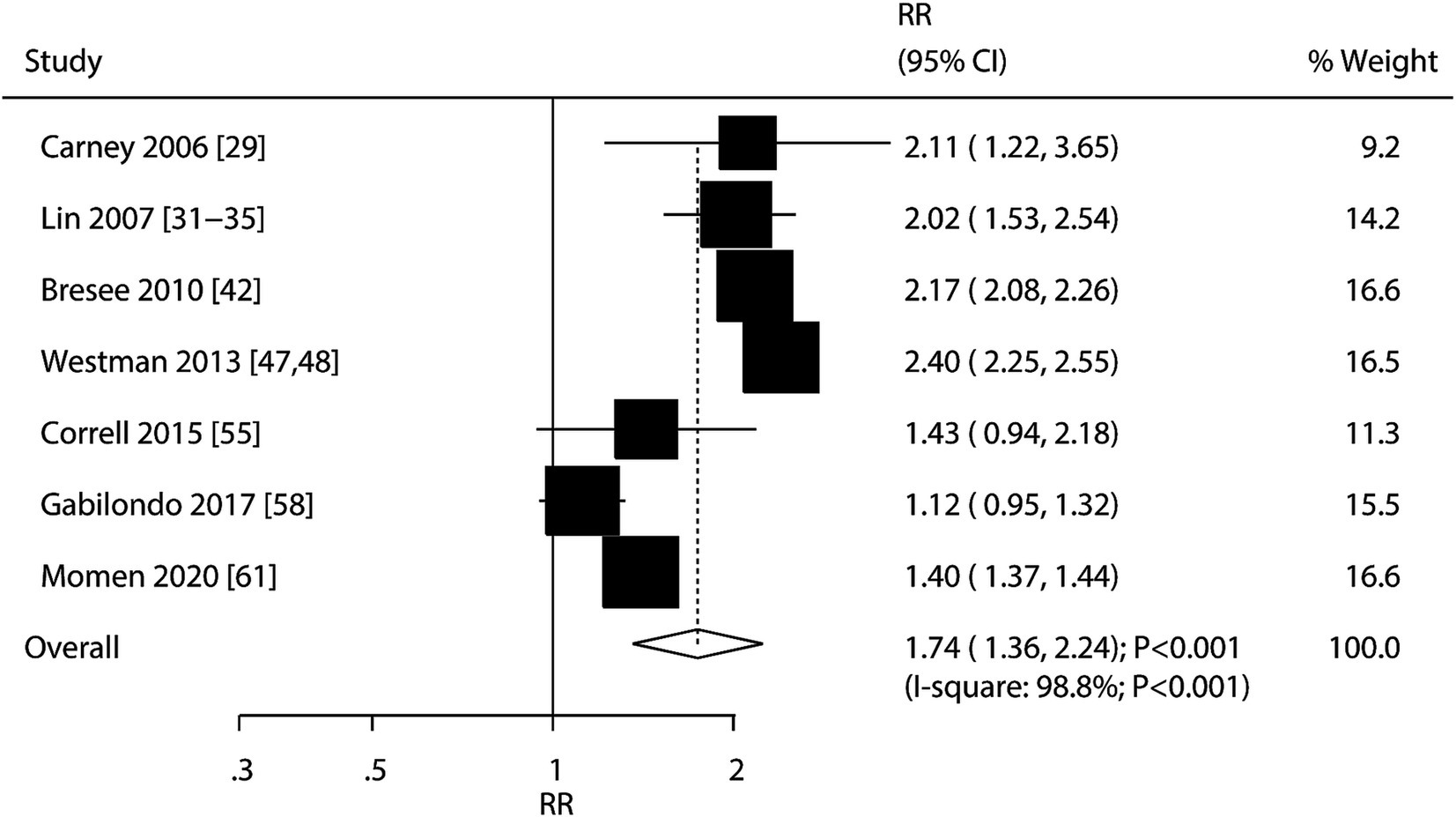
A total of seven cohorts reported an association between schizophrenia and the risk of stroke. We found that schizophrenia was associated with an elevated risk of stroke (RR: 1.74; 95% CI: 1.36–2.24; p < 0.001), and significant heterogeneity was observed among the included studies (I2 = 98.8%; p < 0.001) (Figure 3). The sensitivity analysis indicated that the pooled conclusion was robust and not altered by the removal of any particular study (Supplementary material 3 [Figure S2]). The results of the subgroup analyses were consistent with those of the overall analysis, and the relationship between schizophrenia and stroke risk remained significant (Table 2). Moreover, the strength of the association between schizophrenia and the risk of stroke incidence was weaker than that of the association between schizophrenia and the risk of stroke mortality (RR ratio: 0.68; 95% CI: 0.52–0.90; p = 0.006). No significant publication bias was observed for the association between schizophrenia and the risk of stroke (p-value for the Egger’s: 0.584; p-value for the Begg’s test: 1.000; Supplementary material 4 [Figure S2]).
Bipolar disorder
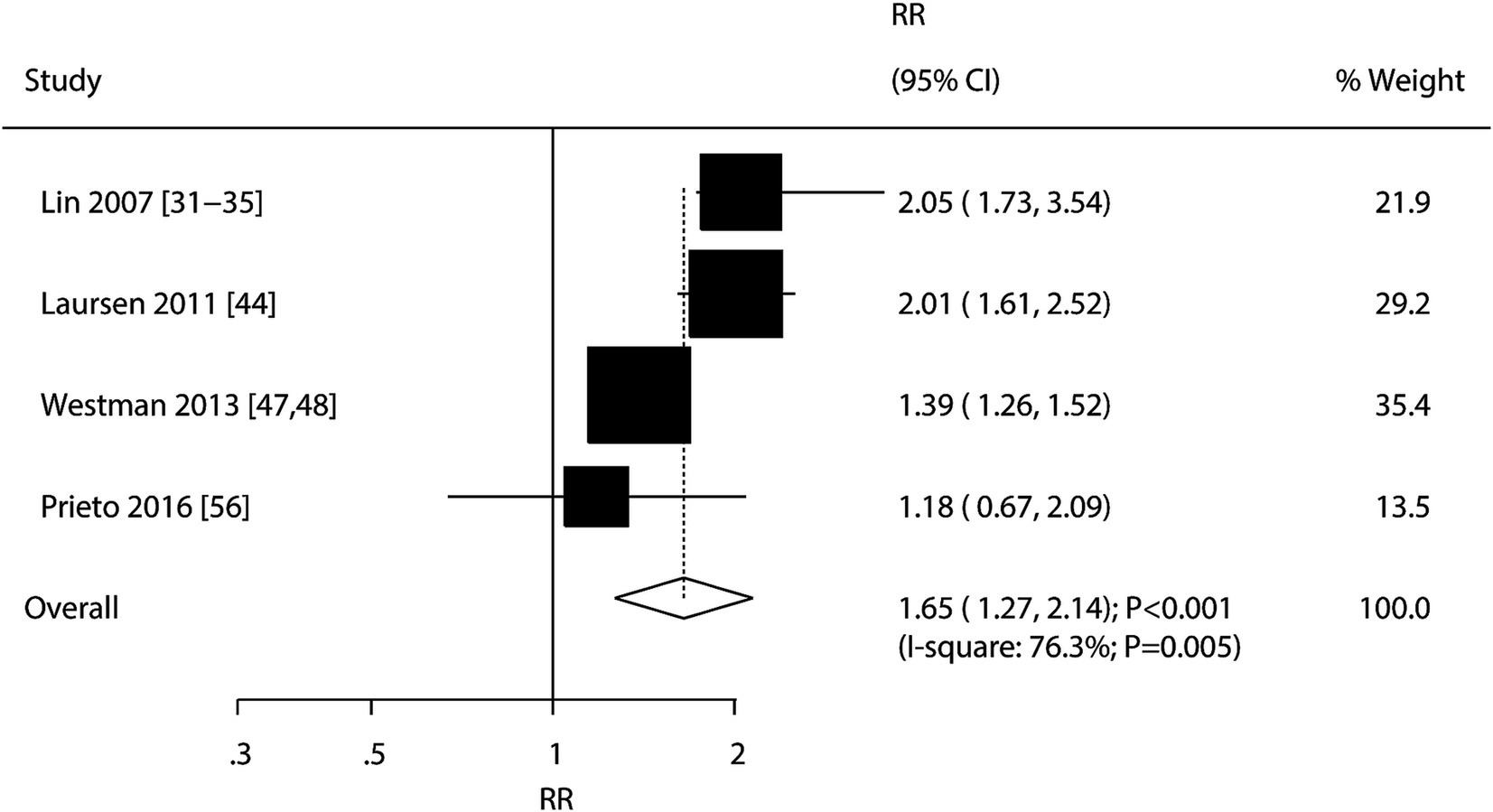
A total of four cohorts reported an association between bipolar disorder and the risk of stroke. The summary result indicated that bipolar disorder was associated with an elevated risk of stroke (RR: 1.65; 95% CI: 1.27–2.14; p < 0.001), and significant heterogeneity was detected across the included studies (I2 = 76.3%%; p = 0.005) (Figure 4). The pooled conclusion remained stable after sequentially removing each study (Supplementary material 3 [Figure S3]). The subgroup analyses found that bipolar disorder was associated with an elevated risk of stroke in all subsets, and the strength of the association between bipolar disorder and the risk of stroke in the prospective cohort studies was weaker than that in the retrospective cohort studies (RR ratio: 0.68; 95% CI: 0.55–0.84; p < 0.001; Table 2). There was no significant publication bias for the association between bipolar disorder and the risk of stroke (p-value for the Egger’s test: 0.473; p-value for the Begg’s test: 1.000; Supplementary material 4 [Figure S3]).
Discussion
In this meta-analysis involving 25,519,635 participants across 36 study cohorts, we found a significant increase in the risk of stroke associated with depression, schizophrenia, and bipolar disorder. Furthermore, this association persisted in almost all subgroups and remained statistically significant across different study designs and participant characteristics. In addition, the exploratory analysis results indicated that the association between depression and stroke differed when stratified by the adjusted level, and there were significant differences in the association between schizophrenia and the incidence and mortality of stroke. Finally, the association between bipolar disorder and the risk of stroke differed based on the study design.
Several systematic reviews and meta-analyses have already addressed the association between psychiatric disorders and the risk of stroke (67–69). Cai et al. conducted a meta-analysis of 17 cohort studies and found a positive association between depression and the risk of stroke. However, the exploratory analysis was not comprehensive, and the comparison results between the subgroups were not fully elaborated (67). Chu et al. identified 20 studies and found that schizophrenia was significantly associated with an increased risk of stroke morbidity and mortality (68). However, the majority of the studies included were not cohort studies, so they could not confirm a causal relationship between schizophrenia and the risk of stroke. Yuan et al. performed a meta-analysis of seven studies (six cohort studies and one case–control study) and found that bipolar disorder was associated with an elevated risk of both stroke morbidity and mortality (69). The analysis of this study was not based on cohort studies, and multiple studies reported on the same cohort, so the pooled conclusions might have been overestimated and could not prove a causal relationship between bipolar disorder and the risk of stroke. Therefore, the current study was performed to comprehensively illustrate the association between psychiatric disorders and the risk of stroke.
While our study provides valuable insights into the relationship between psychiatric disorders and stroke, several potential confounding factors could pose a threat to the causality of our findings. It is important to consider the following factors when interpreting the results: (1) older age and certain sex differences can influence both the presence of psychiatric disorders and the risk of stroke; (2) socioeconomic status, including income, education, and occupation, can confound the observed associations; (3) smoking and alcohol consumption are known risk factors for stroke and can also be associated with psychiatric disorders; (4) pre-existing medical conditions such as hypertension, diabetes, and cardiovascular disease can affect both the risk of psychiatric disorders and the risk of stroke; and (5) the use of certain medications, particularly those used to manage psychiatric disorders, can also confound the observed relationships.
The study found that the risk of stroke was significantly elevated in patients with depression, and this combined result was highly stable and consistent with those of previous meta-analyses (67). Several reasons could explain the significant association between depression and the risk of stroke: (1) patients with depression may experience physiological changes, such as increased sympathetic nervous system activity, elevated heart rate, and high blood pressure due to long-term exposure to stress, which could potentially increase the risk of stroke (70); (2) patients with depression may have increased platelet activity, leading to a higher risk of thrombosis and, consequently, an increased likelihood of stroke occurrence (71); (3) depression is associated with chronic inflammation and immune system dysfunction, and these inflammatory factors may impair vascular endothelial function, promote the development of atherosclerosis, and increase the risk of stroke (72, 73); (4) patients with depression are more likely to engage in unhealthy lifestyle choices, such as poor dietary habits, lack of exercise, smoking, and excessive drinking, which can increase the risk of stroke (74); and (5) the effects of antidepressants on metabolic parameters, including weight gain, hypertension, and hyperlipidemia, can promote the development of atherosclerosis and other cardiovascular diseases through various mechanisms, thereby increasing the risk of stroke. Specifically, weight gain can lead to obesity, which, in turn, triggers insulin resistance and inflammatory responses; hypertension damages the vascular endothelium, promoting arterial wall hardening and plaque formation; and hyperlipidemia increases cholesterol and triglyceride levels in the blood, accelerating the progression of atherosclerosis. These factors collectively contribute to an increased risk of stroke (75, 76). Furthermore, we found that the association between depression and the risk of stroke differed when stratified by the adjusted level. This could be due to the influence of the unadjusted confounders, which might have led to inaccuracies in the conclusions. Finally, the choice of confounding factors may also affect the detection of potential effect modification in study results. If a confounding factor itself interacts with exposure and outcome variables, adjusting for it may mask the presence of such interaction.
We found that schizophrenia was associated with an elevated risk of stroke. The main reasons for this result include the following: (1) Patients with schizophrenia often receive antipsychotic medications, which may increase the risk of cardiovascular diseases, including stroke. Some antipsychotic drugs, particularly second-generation or atypical antipsychotics, are known to have significant metabolic side effects that can contribute to these risks. Specifically, these medications can lead to several risk factors for cardiovascular diseases, including weight gain, hypertension, hyperlipidemia, insulin resistance and diabetes, and inflammatory markers (77). (2) Patients with schizophrenia often face issues such as sleep problems, poor dietary habits, lack of exercise, and other unhealthy lifestyle factors, which can also increase the risk of stroke (78). (3) Schizophrenia may be related to the patient’s physiological and psychological state, which may lead to increased inflammatory responses and abnormal stress responses, thereby increasing the risk of stroke (79). Furthermore, the relationship between schizophrenia and stroke risk was found to differ according to the outcome definition, which could be explained by the fact that the stroke mortality rate is significantly lower than the overall stroke incidence, which could have led to poor stability of the results.
The summary results indicated that bipolar disorder was associated with an elevated risk of stroke. The specific mechanisms that may contribute to the increased risk of stroke in patients with bipolar disorder include the following: (1) Vascular dysfunction: Patients with bipolar disorder may have vascular abnormalities, such as endothelial dysfunction and a tendency for thrombus formation, which can increase the risk of stroke (80). (2) Inflammatory response: Previous studies suggest that patients with bipolar disorder often exhibit chronic low-grade inflammation, and the release of inflammatory factors may promote atherosclerosis development, thereby increasing the risk of stroke (81). (3) Autonomic nervous system dysregulation: Patients with bipolar disorder may experience dysregulation of the autonomic nervous system, leading to abnormalities in blood pressure, heart rate, and other physiological parameters, which can elevate the risk of stroke (82). (4) Treatment-related adverse events: The medications used to treat bipolar disorder can have side effects that affect various physiological parameters, including blood coagulation, blood pressure, lipid levels, and other factors, thereby increasing the risk of stroke (83).
There are several shortcomings of this study that warrant acknowledgment: (1) Given its reliance on both prospective and retrospective cohort studies, our findings might have been susceptible to uncontrolled recall biases and confounding influences. (2) Variations in the psychiatric disorder assessment criteria across different studies could have potentially skewed the evaluation of disease severity. (3) Although our analysis excluded other common psychiatric disorders, such as anxiety, the role of anxiety in stroke risk remains an important area for future research. (4) Inconsistencies in the covariates adjusted for in the reported effect sizes across the studies undermined the precision of establishing a connection between psychiatric disorders and stroke risk. (5) Not all studies provided detailed data on medication use, which prevented us from fully controlling for medication use when synthesizing the results. (6) The inherent constraints of a meta-analysis based solely on published literature, such as the exclusion of unpublished data and reliance on pooled data, hinder more nuanced and detailed analyses.
Conclusion
This study found an association between psychiatric disorders—depression, schizophrenia, and bipolar disorder—and an increased risk of stroke. Individuals with these disorders should adopt enhanced stroke prevention strategies to improve patient outcomes.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
ZH: Conceptualization, Data curation, Investigation, Writing – original draft, Writing – review & editing. WS: Conceptualization, Data curation, Writing – original draft. EC: Data curation, Formal analysis, Methodology, Writing – original draft. BC: Data curation, Formal analysis, Methodology, Writing – original draft. MZ: Data curation, Formal analysis, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2024.1444862/full#supplementary-material
References
1. GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet Neurol. (2021) 20:795–820. doi: 10.1016/S1474-4422(21)00252-0
2. Feigin, VL, Roth, GA, Naghavi, M, Parmar, P, Krishnamurthi, R, Chugh, S, et al. Global burden of stroke and risk factors in 188 countries, during 1990-2013: a systematic analysis for the global burden of disease study 2013. Lancet Neurol. (2016) 15:913–24. doi: 10.1016/S1474-4422(16)30073-4
3. GBD 2016 Stroke Collaborators. Global, regional, and national burden of stroke, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. (2019) 18:439–58. doi: 10.1016/S1474-4422(19)30034-1
4. O'Donnell, M, Xavier, D, Diener, C, Sacco, R, Lisheng, L, Zhang, H, et al. Rationale and design of INTERSTROKE: a global case-control study of risk factors for stroke. Neuroepidemiology. (2010) 35:36–44. doi: 10.1159/000306058
5. Bailey, RR. Lifestyle modification for secondary stroke prevention. Am J Lifestyle Med. (2016) 12:140–7. doi: 10.1177/1559827616633683
6. Bailey, RR, Phad, A, McGrath, R, and Haire-Joshu, D. Prevalence of five lifestyle risk factors among U.S. adults with and without stroke. Disabil Health J. (2019) 12:323–7. doi: 10.1016/j.dhjo.2018.11.003
7. Farahbakhsh, M, Faramarzi, E, Fakhari, A, Sadeghi, M, Barzegar, H, Norouzi, S, et al. The PERSIAN cohort: prevalence of psychiatric disorders among employees. Arch Iran Med. (2024) 27:72–8. doi: 10.34172/aim.2024.12
8. Henderson, S. Epidemiology of mental disorders: the current agenda. Epidemiol Rev. (2000) 22:24–8. doi: 10.1093/oxfordjournals.epirev.a018021
9. Nordentoft, M, Wahlbeck, K, Hällgren, J, Westman, J, Ösby, U, Alinaghizadeh, H, et al. Excess mortality, causes of death and life expectancy in 270,770 patients with recent onset of mental disorders in Denmark, Finland and Sweden. PLoS One. (2013) 8:e55176. doi: 10.1371/journal.pone.0055176
10. Hoang, U, Stewart, R, and Goldacre, MJ. Mortality after hospital discharge for people with schizophrenia or bipolar disorder: retrospective study of linked English hospital episode statistics, 1999-2006. BMJ. (2011) 343:d5422. doi: 10.1136/bmj.d5422
11. Ösby, U, Westman, J, Hällgren, J, and Gissler, M. Mortality trends in cardiovascular causes in schizophrenia, bipolar and unipolar mood disorder in Sweden 1987-2010. Eur J Pub Health. (2016) 26:867–71. doi: 10.1093/eurpub/ckv245
12. Sui, X, Liu, T, Liang, Y, and Zhang, B. Psychiatric disorders and cardiovascular diseases: a mendelian randomization study. Heliyon. (2023) 9:e20754. doi: 10.1016/j.heliyon.2023.e20754
13. Page, MJ, McKenzie, JE, Bossuyt, PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
14. Wells, G, Shea, B, and O’Connell, D. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa (ON): Ottawa Hospital Research Institute (2009).
15. DerSimonian, R, and Laird, N. Meta-analysis in clinical trials. Control Clin Trials. (1986) 7:177–88. doi: 10.1016/0197-2456(86)90046-2
16. Ades, AE, Lu, G, and Higgins, JP. The interpretation of random-effects meta-analysis in decision models. Med Decis Mak. (2005) 25:646–54. doi: 10.1177/0272989X05282643
17. Deeks, JJ, Higgins, JPT, and Altman, DG. Analyzing data and undertaking meta-analyses In: J Higgins and S Green, editors. Cochrane handbook for systematic reviews of interventions 5.0.1. Oxford, UK: The Cochrane Collaboration (2008)
18. Higgins, JP, Thompson, SG, Deeks, JJ, and Altman, DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
19. Tobias, A. Assessing the influence of a single study in meta-analysis. Stata Tech Bull. (1999) 47:15–7.
20. Altman, DG, and Bland, JM. Interaction revisited: the difference between two estimates. BMJ. (2003) 326:219. doi: 10.1136/bmj.326.7382.219
21. Egger, M, Smith, G, Schneider, M, and Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
22. Begg, CB, and Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics. (1994) 50:1088–101. doi: 10.2307/2533446
23. Wassertheil-Smoller, S, Applegate, WB, Berge, K, Chang, CJ, Davis, BR, Grimm, R Jr, et al. Change in depression as a precursor of cardiovascular events. SHEP cooperative research group (Systoloc hypertension in the elderly). Arch Intern Med. (1996) 156:553–61. doi: 10.1001/archinte.1996.00440050111012
24. Simons, LA, McCallum, J, Friedlander, Y, and Simons, J. Risk factors for ischemic stroke: Dubbo study of the elderly. Stroke. (1998) 29:1341–6. doi: 10.1161/01.STR.29.7.1341
25. Whooley, MA, and Browner, WS. Association between depressive symptoms and mortality in older women. Study of osteoporotic fractures research group. Arch Intern Med. (1998) 158:2129–35. doi: 10.1001/archinte.158.19.2129
26. Ostir, GV, Markides, KS, Peek, MK, and Goodwin, JS. The association between emotional well-being and the incidence of stroke in older adults. Psychosom Med. (2001) 63:210–5. doi: 10.1097/00006842-200103000-00003
27. Avendano, M, Kawachi, I, van, F, Boshuizen, H, Mackenbach, J, van, GAM, et al. Socioeconomic status and stroke incidence in the US elderly. Stroke. (2006) 37:1368–73. doi: 10.1161/01.STR.0000221702.75002.66
28. Yasuda, N, Mino, Y, Koda, S, and Ohara, H. The differential influence of distinct clusters of psychiatric symptoms, as assessed by the general health questionnaire, on cause of death in older persons living in a rural community of Japan. J Am Geriatr Soc. (2002) 50:313–20. doi: 10.1046/j.1532-5415.2002.50064.x
29. Carney, CP, Jones, L, and Woolson, RF. Medical comorbidity in women and men with schizophrenia: a population-based controlled study. J Gen Intern Med. (2006) 21:1133–7. doi: 10.1111/j.1525-1497.2006.00563.x
30. Kamphuis, MH, Kalmijn, S, Tijhuis, MA, Geerlings, M, Giampaoli, S, Nissinen, A, et al. Depressive symptoms as risk factor of cardiovascular mortality in older European men: the Finland, Italy and Netherlands elderly (FINE) study. Eur J Cardiovasc Prev Rehabil. (2006) 13:199–206. doi: 10.1097/01.hjr.0000188242.64590.92
31. Lin, HC, Tsai, SY, and Lee, HC. Increased risk of developing stroke among patients with bipolar disorder after an acute mood episode: a six-year follow-up study. J Affect Disord. (2007) 100:49–54. doi: 10.1016/j.jad.2006.09.016
32. Lin, HC, Hsiao, FH, Pfeiffer, S, Hwang, YT, and Lee, HC. An increased risk of stroke among young schizophrenia patients. Schizophr Res. (2008) 101:234–41. doi: 10.1016/j.schres.2007.12.485
33. Wu, HC, Chou, FH, Tsai, KY, Su, CY, Shen, SP, and Chung, TC. The incidence and relative risk of stroke among patients with bipolar disorder: a seven-year follow-up study. PLoS One. (2013) 8:e73037. doi: 10.1371/journal.pone.0073037
34. Chen, MH, Li, CT, Hsu, JW, Huang, KL, Lin, WC, Chang, WH, et al. Atopic diseases and subsequent ischemic stroke among patients with schizophrenia: a Nationwide longitudinal study. Psychosom Med. (2015) 77:1031–8. doi: 10.1097/PSY.0000000000000234
35. Tsao, WY, Hsu, JW, Huang, KL, Bai, YM, Su, TP, Li, CT, et al. Risk of cardiometabolic diseases among siblings of patients with bipolar disorder. J Affect Disord. (2019) 253:171–5. doi: 10.1016/j.jad.2019.04.094
36. Arbelaez, JJ, Ariyo, AA, Crum, RM, Fried, LP, and Ford, DE. Depressive symptoms, inflammation, and ischemic stroke in older adults: a prospective analysis in the cardiovascular health study. J Am Geriatr Soc. (2007) 55:1825–30. doi: 10.1111/j.1532-5415.2007.01393.x
37. Yan, T, Escarce, JJ, Liang, LJ, Longstreth, WT Jr, Merkin, SS, Ovbiagele, B, et al. Exploring psychosocial pathways between neighbourhood characteristics and stroke in older adults: the cardiovascular health study. Age Ageing. (2013) 42:391–7. doi: 10.1093/ageing/afs179
38. Gilsanz, P, Kubzansky, LD, Tchetgen Tchetgen, EJ, Wang, Q, Kawachi, I, Patton, KK, et al. Changes in depressive symptoms and subsequent risk of stroke in the cardiovascular health study. Stroke. (2017) 48:43–8. doi: 10.1161/STROKEAHA.116.013554
39. Kawamura, T, Shioiri, T, Takahashi, K, Ozdemir, V, and Someya, T. Survival rate and causes of mortality in the elderly with depression: a 15-year prospective study of a Japanese community sample, the Matsunoyama-Niigata suicide prevention project. J Investig Med. (2007) 55:106–14. doi: 10.2310/6650.2007.06040
40. Bos, MJ, Linden, T, Koudstaal, PJ, Hofman, A, Skoog, I, Breteler, M, et al. Depressive symptoms and risk of stroke: the Rotterdam study. J Neurol Neurosurg Psychiatry. (2008) 79:997–1001. doi: 10.1136/jnnp.2007.134965
41. Liebetrau, M, Steen, B, and Skoog, I. Depression as a risk factor for the incidence of first-ever stroke in 85-year-olds. Stroke. (2008) 39:1960–5. doi: 10.1161/STROKEAHA.107.490797
42. Bresee, LC, Majumdar, SR, Patten, SB, and Johnson, JA. Prevalence of cardiovascular risk factors and disease in people with schizophrenia: a population-based study. Schizophr Res. (2010) 117:75–82. doi: 10.1016/j.schres.2009.12.016
43. Peters, R, Pinto, E, Beckett, N, Swift, C, Potter, J, McCormack, T, et al. Association of depression with subsequent mortality, cardiovascular morbidity and incident dementia in people aged 80 and over and suffering from hypertension. Data from the hypertension in the very elderly trial (HYVET). Age Ageing. (2010) 39:439–45. doi: 10.1093/ageing/afq042
44. Laursen, TM, Munk-Olsen, T, and Gasse, C. Chronic somatic comorbidity and excess mortality due to natural causes in persons with schizophrenia or bipolar affective disorder. PLoS One. (2011) 6:e24597. doi: 10.1371/journal.pone.0024597
45. Pan, A, Okereke, OI, Sun, Q, Logroscino, G, Manson, JAE, Willett, WC, et al. Depression and incident stroke in women. Stroke. (2011) 42:2770–5. doi: 10.1161/STROKEAHA.111.617043
46. Majed, B, Arveiler, D, Bingham, A, Ferrieres, J, Ruidavets, JB, Montaye, M, et al. Depressive symptoms, a time-dependent risk factor for coronary heart disease and stroke in middle-aged men: the PRIME study. Stroke. (2012) 43:1761–7. doi: 10.1161/STROKEAHA.111.645366
47. Westman, J, Hällgren, J, Wahlbeck, K, Erlinge, D, Alfredsson, L, and Ösby, U. Cardiovascular mortality in bipolar disorder: a population-based cohort study in Sweden. BMJ Open. (2013) 3:e002373. doi: 10.1136/bmjopen-2012-002373
48. Westman, J, Eriksson, SV, Gissler, M, Hällgren, J, Prieto, ML, Bobo, WV, et al. Increased cardiovascular mortality in people with schizophrenia: a 24-year national register study. Epidemiol Psychiatr Sci. (2018) 27:519–27. doi: 10.1017/S2045796017000166
49. Köhler, S, Verhey, F, Weyerer, S, Wiese, B, Heser, K, Wagner, M, et al. Depression, non-fatal stroke and all-cause mortality in old age: a prospective cohort study of primary care patients. J Affect Disord. (2013) 150:63–9. doi: 10.1016/j.jad.2013.02.020
50. Péquignot, R, Tzourio, C, Péres, K, Ancellin, ML, Perier, MC, Ducimetière, P, et al. Depressive symptoms, antidepressants and disability and future coronary heart disease and stroke events in older adults: the three City study. Eur J Epidemiol. (2013) 28:249–56. doi: 10.1007/s10654-013-9765-3
51. Jackson, CA, and Mishra, GD. Depression and risk of stroke in midaged women: a prospective longitudinal study. Stroke. (2013) 44:1555–60. doi: 10.1161/STROKEAHA.113.001147
52. Gafarov, VV, Panov, DO, Gromova, EA, Gagulin, I, and Gafarova, A. The influence of depression on risk development of acute cardiovascular diseases in the female population aged 25-64 in Russia. Int J Circumpolar Health. (2013) 72:72. doi: 10.3402/ijch.v72i0.21223
53. Everson-Rose, SA, Roetker, NS, Lutsey, PL, Kershaw, KN, Longstreth, WT Jr, Sacco, RL, et al. Chronic stress, depressive symptoms, anger, hostility, and risk of stroke and transient ischemic attack in the multi-ethnic study of atherosclerosis. Stroke. (2014) 45:2318–23. doi: 10.1161/STROKEAHA.114.004815
54. Brunner, EJ, Shipley, MJ, Britton, AR, Stansfeld, SA, Heuschmann, PU, Rudd, AG, et al. Depressive disorder, coronary heart disease, and stroke: dose-response and reverse causation effects in the Whitehall II cohort study. Eur J Prev Cardiol. (2014) 21:340–6. doi: 10.1177/2047487314520785
55. Correll, CU, Joffe, BI, Rosen, LM, Sullivan, TB, and Joffe, RT. Cardiovascular and cerebrovascular risk factors and events associated with second-generation antipsychotic compared to antidepressant use in a non-elderly adult sample: results from a claims-based inception cohort study. World Psychiatry. (2015) 14:56–63. doi: 10.1002/wps.20187
56. Prieto, ML, Schenck, LA, Kruse, JL, Klaas, JP, Chamberlain, AM, Bobo, WV, et al. Long-term risk of myocardial infarction and stroke in bipolar I disorder: a population-based cohort study. J Affect Disord. (2016) 194:120–7. doi: 10.1016/j.jad.2016.01.015
57. Sun, J, Ma, H, Yu, C, Lv, J, Guo, Y, Bian, Z, et al. Association of Major Depressive Episodes with Stroke Risk in a prospective study of 0.5 million Chinese adults. Stroke. (2016) 47:2203–8. doi: 10.1161/STROKEAHA.116.013512
58. Gabilondo, A, Alonso-Moran, E, Nuño-Solinis, R, Orueta, JF, and Iruin, A. Comorbidities with chronic physical conditions and sex profiles of illness in schizophrenia. Results from PREST, a new health dataset. J Psychosom Res. (2017) 93:102–9. doi: 10.1016/j.jpsychores.2016.12.011
59. Zahodne, LB, Gilsanz, P, Glymour, MM, Gibbons, LE, Brewster, P, Hamilton, J, et al. Comparing variability, severity, and persistence of depressive symptoms as predictors of future stroke risk. Am J Geriatr Psychiatry. (2017) 25:120–8. doi: 10.1016/j.jagp.2016.10.009
60. Tsai, TY, Lu, MC, Livneh, H, Chiu, SY, Lai, NS, and Guo, HR. Does depression increase the risk of stroke in patients with rheumatoid arthritis? A population-based cohort study. BMJ Open. (2017) 7:e014233. doi: 10.1136/bmjopen-2016-014233
61. Momen, NC, Plana-Ripoll, O, Agerbo, E, Benros, ME, Børglum, AD, Christensen, MK, et al. Association between mental disorders and subsequent medical conditions. N Engl J Med. (2020) 382:1721–31. doi: 10.1056/NEJMoa1915784
62. Meza, E, Eng, CW, Sáenz, JL, Gilsanz, P, Glymour, MM, and Torres, JM. Elevated depressive symptoms and the risk of stroke among the Mexican older population. J Am Geriatr Soc. (2020) 68:2579–86. doi: 10.1111/jgs.16718
63. Sico, JJ, Kundu, S, So-Armah, K, Gupta, SK, Chang, CCH, Butt, AA, et al. Depression as a risk factor for incident ischemic stroke among HIV-positive veterans in the veterans aging cohort study. J Am Heart Assoc. (2021) 10:e017637. doi: 10.1161/JAHA.119.017637
64. Cui, Y, Zhu, C, Lian, Z, Han, X, Xiang, Q, Liu, Z, et al. Prospective association between depressive symptoms and stroke risk among middle-aged and older Chinese. BMC Psychiatry. (2021) 21:532. doi: 10.1186/s12888-021-03492-9
65. Ford, CD, Gray, MS, Crowther, MR, Wadley, VG, Austin, AL, Crowe, MG, et al. Depressive symptoms and risk of stroke in a National Cohort of black and white participants from REGARDS. Neurol Clin Pract. (2021) 11:e454–61. doi: 10.1212/CPJ.0000000000000983
66. Shen, R, Zhao, N, Wang, J, Guo, P, Shen, S, Liu, D, et al. Association between level of depression and coronary heart disease, stroke risk and all-cause and cardiovascular mortality: data from the 2005-2018 National Health and nutrition examination survey. Front Cardiovasc Med. (2022) 9:954563. doi: 10.3389/fcvm.2022.954563
67. Cai, W, Ma, W, Mueller, C, Stewart, R, Ji, J, and Shen, WD. Association between late-life depression or depressive symptoms and stroke morbidity in elders: a systematic review and meta-analysis of cohort studies. Acta Psychiatr Scand. (2023) 148:405–15. doi: 10.1111/acps.13613
68. Chu, RST, Chong, RCH, Chang, DHH, Shan Leung, AL, Chan, JKN, Wong, CSM, et al. The risk of stroke and post-stroke mortality in people with schizophrenia: a systematic review and meta-analysis study. Psychiatry Res. (2024) 332:115713. doi: 10.1016/j.psychres.2024.115713
69. Yuan, M, Xiao, ZL, Zhou, HY, Rao, W, Huang, G, Nie, HB, et al. Bipolar disorder and the risk for stroke incidence and mortality: a meta-analysis. Neurol Sci. (2022) 43:467–76. doi: 10.1007/s10072-021-05348-2
70. Malyshev, AV, Sukhanova, IA, Ushakova, VM, Zorkina, YA, Abramova, OV, Morozova, AY, et al. Peptide LCGA-17 attenuates behavioral and neurochemical deficits in rodent models of PTSD and depression. Pharmaceuticals. (2022) 15:462. doi: 10.3390/ph15040462
71. Tagliarini, C, Carbone, MG, Pagni, G, Marazziti, D, and Pomara, N. Is there a relationship between morphological and functional platelet changes and depressive disorder? CNS Spectr. (2022) 27:157–90. doi: 10.1017/S1092852920001959
72. Millar, SR, Harrington, JM, Perry, IJ, and Phillips, CM. Lifestyle factors and BMI attenuate relationships between biomarkers of inflammation and depressive symptoms and well-being: a cross-sectional study. Brain Behav Immun Health. (2024) 37:100759. doi: 10.1016/j.bbih.2024.100759
73. Jha, MK, Cai, L, Minhajuddin, A, Fatt, CC, Furman, JL, Gadad, BS, et al. Dysfunctional adaptive immune response in adolescents and young adults with suicide behavior. Psychoneuroendocrinology. (2020) 111:104487. doi: 10.1016/j.psyneuen.2019.104487
74. Navarra-Ventura, G, Coronado-Simsic, V, Riera-Serra, P, Castro, A, García-Toro, M, Roca, M, et al. Associations between unhealthy lifestyle and depression: cross-sectional results from the Spanish National Health Survey. Span J Psychiatry Ment Health. (2023) S2950-2853:00035–2. doi: 10.1016/j.sjpmh.2023.08.001
75. Desai, R, Park, H, Brown, JD, Mohandas, R, and Smith, SM. Norepinephrine reuptake inhibitors and risk of antihypertensive treatment intensification and major adverse cardiovascular events in patients with stable hypertension and depression. Pharmacotherapy. (2022) 42:472–82. doi: 10.1002/phar.2686
76. Jellinger, KA. Pathomechanisms of vascular depression in older adults. Int J Mol Sci. (2021) 23:308. doi: 10.3390/ijms23010308
77. Nielsen, RE, Banner, J, and Jensen, SE. Cardiovascular disease in patients with severe mental illness. Nat Rev Cardiol. (2021) 18:136–45. doi: 10.1038/s41569-020-00463-7
78. Tous-Espelosin, M, de Azua, SR, Iriarte-Yoller, N, MartínezAguirre-Betolaza, A, Sanchez, PM, Corres, P, et al. Clinical, physical, physiological, and cardiovascular risk patterns of adults with schizophrenia: CORTEX-SP study: characterization of adults with schizophrenia. Psychiatry Res. (2021) 295:113580. doi: 10.1016/j.psychres.2020.113580
79. Long, Y, Wang, Y, Shen, Y, Huang, J, Li, Y, Wu, R, et al. Minocycline and antipsychotics inhibit inflammatory responses in BV-2 microglia activated by LPS via regulating the MAPKs/ JAK-STAT signaling pathway. BMC Psychiatry. (2023) 23:514. doi: 10.1186/s12888-023-05014-1
80. Schmitz, SL, Abosi, OJ, Persons, JE, Sinkey, CA, and Fiedorowicz, JG. Impact of mood on endothelial function and arterial stiffness in bipolar disorder. Heart Mind. (2018) 2:78–84. doi: 10.4103/hm.hm_20_19
81. Sırlıer Emir, B, Yıldız, S, Kazğan Kılıçaslan, A, Kurt, O, Uğur, K, Tabara, MF, et al. Inflammation markers in patients with bipolar disorder who have committed offenses and their relationship with criminal behavior. Medicina. (2023) 59:1725. doi: 10.3390/medicina59101725
82. Taylor, V, and MacQueen, G. Associations between bipolar disorder and metabolic syndrome: a review. J Clin Psychiatry. (2006) 67:1034–41. doi: 10.4088/JCP.v67n0704
Keywords: psychiatric disorders, stroke, meta-analysis, cohort studies, risk
Citation: Hu Z, Sun W, Cui E, Chen B and Zhang M (2024) Association between psychiatric disorders and the risk of stroke: a meta-analysis of cohort studies. Front. Neurol. 15:1444862. doi: 10.3389/fneur.2024.1444862
Edited by:
Narayanaswamy Venketasubramanian, Raffles Hospital, SingaporeReviewed by:
Félix Javier Jiménez-Jiménez, Hospital Universitario del Sureste, SpainLambert Zixin Li, Stanford University, United States
Malahat Akbarfahimi, Iran University of Medical Sciences, Iran
Copyright © 2024 Hu, Sun, Cui, Chen and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhonghou Hu, MTM5NjE5ODM4ODBAMTM5LmNvbQ==
 Zhonghou Hu
Zhonghou Hu Weishan Sun
Weishan Sun