
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol. , 18 June 2024
Sec. Stroke
Volume 15 - 2024 | https://doi.org/10.3389/fneur.2024.1428198
 Craig Kurunawai1,2,3
Craig Kurunawai1,2,3 Chushuang Chen4,5
Chushuang Chen4,5 Matthew Willcour6
Matthew Willcour6 Aaron Tan1,3
Aaron Tan1,3 Joshua Mahadevan1,3
Joshua Mahadevan1,3 Michael Waters1
Michael Waters1 Jackson Harvey3
Jackson Harvey3 Joanne Van Eunen1,2
Joanne Van Eunen1,2 Karen Dixon1,2
Karen Dixon1,2 Bianca Piantedosi1,2
Bianca Piantedosi1,2 Andrew Bivard7,8*
Andrew Bivard7,8* Mark William Parsons4,5,9
Mark William Parsons4,5,9 Stephen M. Davis7,8
Stephen M. Davis7,8 Geoffrey Alan Donnan7,8
Geoffrey Alan Donnan7,8 Jim Jannes1,3
Jim Jannes1,3 Timothy Kleinig1,3
Timothy Kleinig1,3Background: Patients with a large vessel occlusion require a transfer from a primary stroke centre to access thrombectomy, often over significant distances in regional areas. We sought to optimise stroke care access in the regional South Australian Tele-Strokeservice (SATS) to improve patient access to thrombectomy.
Methods: We undertook a 24-month interventional historically controlled cohort study comparing acute stroke care metrics in the SATS. This consisted of a 12-month control period and a 12-month intervention monitoring period. The study intervention considered of an education package provided to the regional hospitals, a stroke neurologist roster to receive consultations and the intervention of a centralised tele-stroke system to provide treatment advice and organise patient transfers where needed. The SATS services 61 rural hospitals in South Australia, and Alice Springs in the Northern Territory. Suspected acute stroke patients presenting to the participating regional hospitals in SATS network where a telehealth consultation took place.
Results: Over the study period, there were 919 patient referrals, with 449 consultations in the pre-intervention phase and 470 in the post-intervention phase. Demographic features in both epochs were similar. The post-intervention phase was associated with shorter door-to-scan time (35 min, IQR: 18,70; vs. 49 min, IQR:25,102, p < 0.0001), faster door-to-thrombolysis time (58 min, IQR: 39,91, vs.83 min, IQR: 55,100, p = 0.0324) and a higher portion of patients treated with thrombectomy (54, 11.5% vs. 26, 5.8%, p = 0.002).
Conclusion: An optimised implementation of a streamlined telehealth platform with ongoing education and feedback to referring sites was associated with improved stroke workflow metrics and higher thrombectomy rates.
Stroke is the second leading cause of death and the most common cause of adult disability in the developed world (1). Stroke patients with a large vessel occlusion (LVO) face an especially devastating outcome due to the large volume of brain tissue affected, resulting in >50% of patients being dead or significantly disabled at 3 months without rapid and effective reperfusion treatment (2). The goal of acute ischemic stroke therapy is to either pharmacologically or mechanically remove the clot blocking the affected artery in order to restore blood flow to brain tissue that is ischaemic but still salvageable (the ischaemic penumbra). The efficacy of treatments for acute stroke has improved significantly over the last decade with the introduction of thrombectomy for patients with a large vessel occlusion and recent evidence supporting treatment for haemorrhage (3).
Stroke incidence is 20% higher in rural and remote areas (4), however the outcome of a patient presenting with a stroke to a regional hospital is associated with double the likelihood of significant lifelong disability than if a person were to have a stroke in a metropolitan area, likely from inequitable access to specialist services (5). Only 3% of patients in rural and remote areas of Australia have access to stroke specialists, compared to 77% of patients in metropolitan areas and treatment (6), if provided, is often considerably delayed for a condition where time to treatment is directly related to individual patient outcomes. In Australia, several tele-stroke services already exist and have reported success, such as the Victorian (7) and New South Wales tele-stroke services (8–10). However, much of Australia is un-covered with tele-stroke support despite evidence showing improved patient outcomes. There exist severe challenges in providing regional, low-volume stroke centres with adequate specialist cover and maintaining the local skillset where stroke presentations could make up as low as 1% of admissions. Importantly, telehealth services can often require significant costs to support the technology required in the remote consult.
Importantly, the clinical indication for thrombectomy has widened considerably since its introduction, allowing more patients access to this life-saving and quality of life improving therapy. This includes the expansion of eligibility up to 24 h post symptom onset and the trials indication that patients with a large established volume of infarct core still benefit from treatment. As a result, any patient with a large vessel occlusion ischaemic stroke anywhere in Australia is now a potential reperfusion candidate (11). However, thrombectomy treatment is only offered in large cities, with very limited access in regional centres. Therefore, patients presented in regional centres require transfer, often by air, to the thrombectomy centre. This makes the acute stroke care pathway for regional hospitals quite significant, and requires multi-agency coordination for patient retrieval. Optimised telecommunication and health consult software is a vital platform for accurate and efficient telemedicine services to support patient care both on-site and for transfer. In this study, we sought to compare the efficiency and treatment rate of stroke patients presenting to regional hospitals covered by the South Australian Tele-Stroke network over a 12-month period where a combined technical and education quality improvement intervention was undertaken, compared to 12 months of consecutive historical controls.
The South Australian Tele-Stroke Service (SATS) covers 61 hospitals in South Australia and the Northern Territory (Figure 1) and operates 24 h, 7 days a week, 365 days a year. Patients with symptoms of suspected stroke were assessed by ED clinical staff clinically with standard items such as the NIHSS and a medical history recorded, and where indicated or a standard computed tomography (CT) stroke imaging. Stroke specialist Neurologists on the SATS roster were contacted for patients potentially eligible for reperfusion following ‘code stroke pathways incorporating the Recognition of Stroke in the Emergency Room (ROSIER) Scale (12) on a dedicated toll-free telephone number. In tandem with neuroimaging initiation [non-contrast CT (NCCT), CT angiogram (CTA) +/− CT perfusion (CTP)] this then prompted a telemedicine consult by the Stroke specialist neurologist who would evaluate the patient via videoconference and communicate with the local hospital clinicians, receiving a patient handover and recommending treatment or transfer for thrombectomy where appropriate after reviewing the CT imaging.
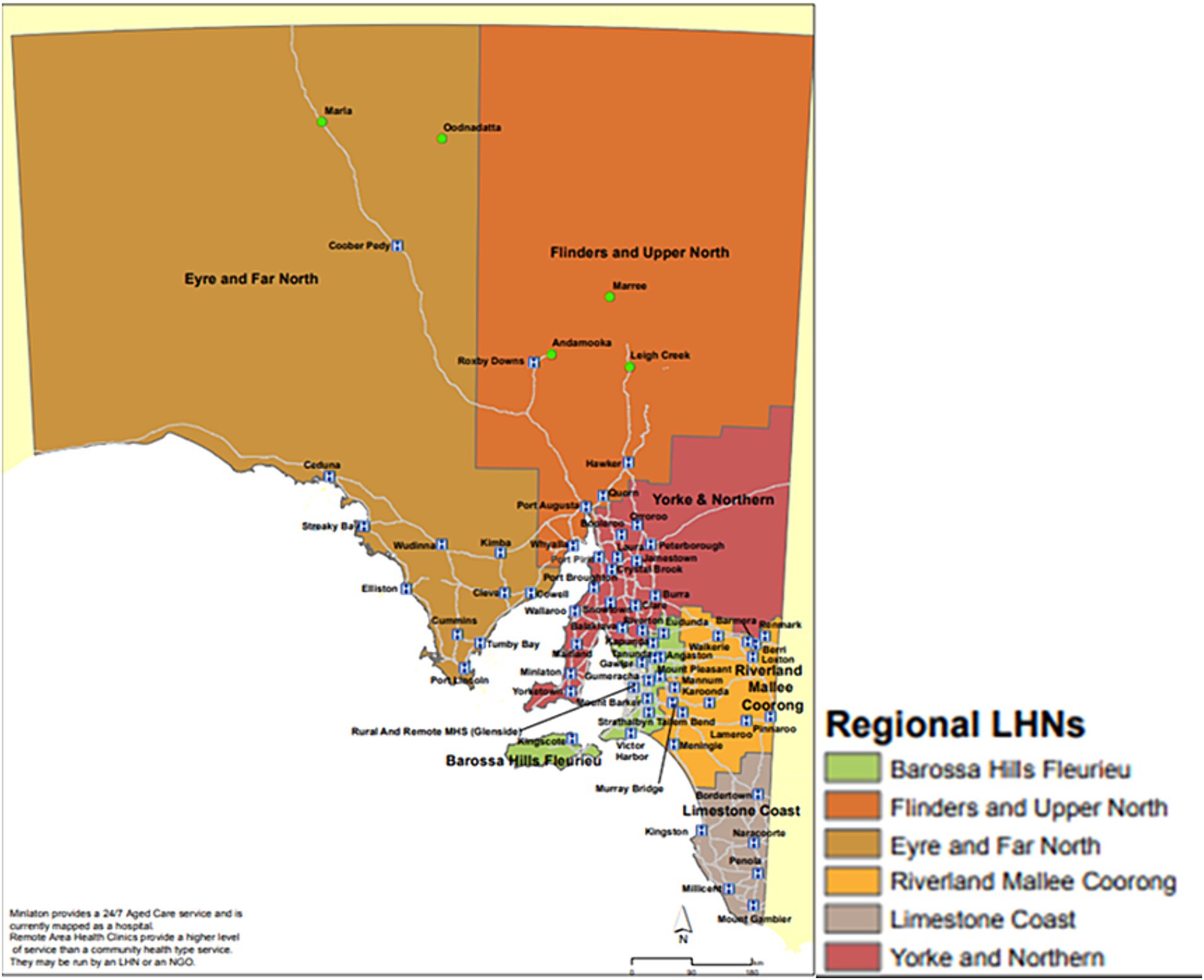
Figure 1. The South Australian Tele-Stroke Service (SATS) cover regional hospitals in South Australia and Alice Springs.
We undertook a retrospective pre-post analysis of consecutive acute patients presenting to the regional hospitals in South Australia, where a telehealth consultation was provided by a central team of stroke-trained neurologists between January 2021 and December 2022. During this period, the number of sites covered and the standard stroke protocol was otherwise stable. This study sought to evaluate the impact of the dedicated telehealth platform “Zeus” and an education and ongoing quality improvement process as part of a broad intervention package. The study intervention was completed in December 2022.
During the study, a multidisciplinary stroke education program was continued for all clinical staff involved in both phases and is used for continuous feedback and quality improvement. The stroke education involved targeting rural and regional emergency department doctors and nurses in stroke care, as well as sharing expertise to improve stroke recognition, clinical assessments and scoring with the NIHSS, and process improvement options to treatment efficiency such as door-to-imaging or door-to-treatment times. During the post-intervention phase, the periodic data extracts enabled focused stroke metric feedback in both state-wide communities of practice forums that were held every 3 months. These forums would provide feedback on individual cases and identify pain points for discussion and solution mapping.
Additionally, monthly general sessions took place to provide ongoing feedback to sites around standard treatment metrics such as the number of patients assessed, the number of patients treated and time to imaging and treatment. The clinicians on the tele-stroke roster also met quarterly to review service data and share experiences to allow for improved communication to sites and between clinicians as a mechanism to enhance site feedback. Data collected pre and post-service implementation were standardised and aligned with clinical guidelines for acute stroke management.
We divided the analysis into two phases: pre-intervention from January to December 2021 and post-intervention of “Zeus” from January to December 2022. Clinical data were collected, including baseline National Institute of Health stroke scale (NIHSS), and pre-stroke modified Rankin Score (mRS). The date and time of stroke onset (or last date/time seen well), tele-stroke consult initiation, treatment decision, and time of thrombolysis were also collected. Door-to-scan was calculated as the time difference between patients’ arrival and the imaging, and door-to-thrombolytic time (DTT) was calculated as the difference between patient arrival and time of thrombolytic administration.
Continuous data were assessed for normality using the Shapiro–Wilk method, with parametric data reported as mean (SD) and non-parametric data reported as median (IQR). Comparison of two groups was performed by the Student’s t-test (for parametric data) or the Wilcoxon Rank Sum test (for non-parametric data). For categorical variables, patient characteristics described as proportions and group comparison was conducted with Pearson Chi-squared test. Although comparisons between 2021 and 2022 data using the aforementioned tests for comparing two groups, differences between year-by-year data of the study period were tested using one-way analysis of variance (ANOVA) (parametric data) or Kruskal-Wallis (non-parametric) methodology. Data were analysed using STATA (V13.1, Stata Corp, College Station, Texas, United States), with alpha level set at 0.05.
For this study, there were 449 consultations in 40 regional hospitals performed in the pre-intervention phase (01/01/2021–31/12/2021) and 470 consultations in 52 hospitals performed in the post-intervention phase (01/01/2022–31/12/2022, Figures 2, 3). The median NIHSS of patients presenting in the pre-and post-intervention phase was similar (median 3, IQR: 1,7). The portion of patients with atrial fibrillation was similar between the pre-and post-intervention phases (77, 17.1% vs. 92, 19.6%, p = 0.394). The after-working-hours consultations were similar between the pre-and post-intervention phase (287, 63.9% vs. 293, 62.3%, p = 0.707, Table 1).
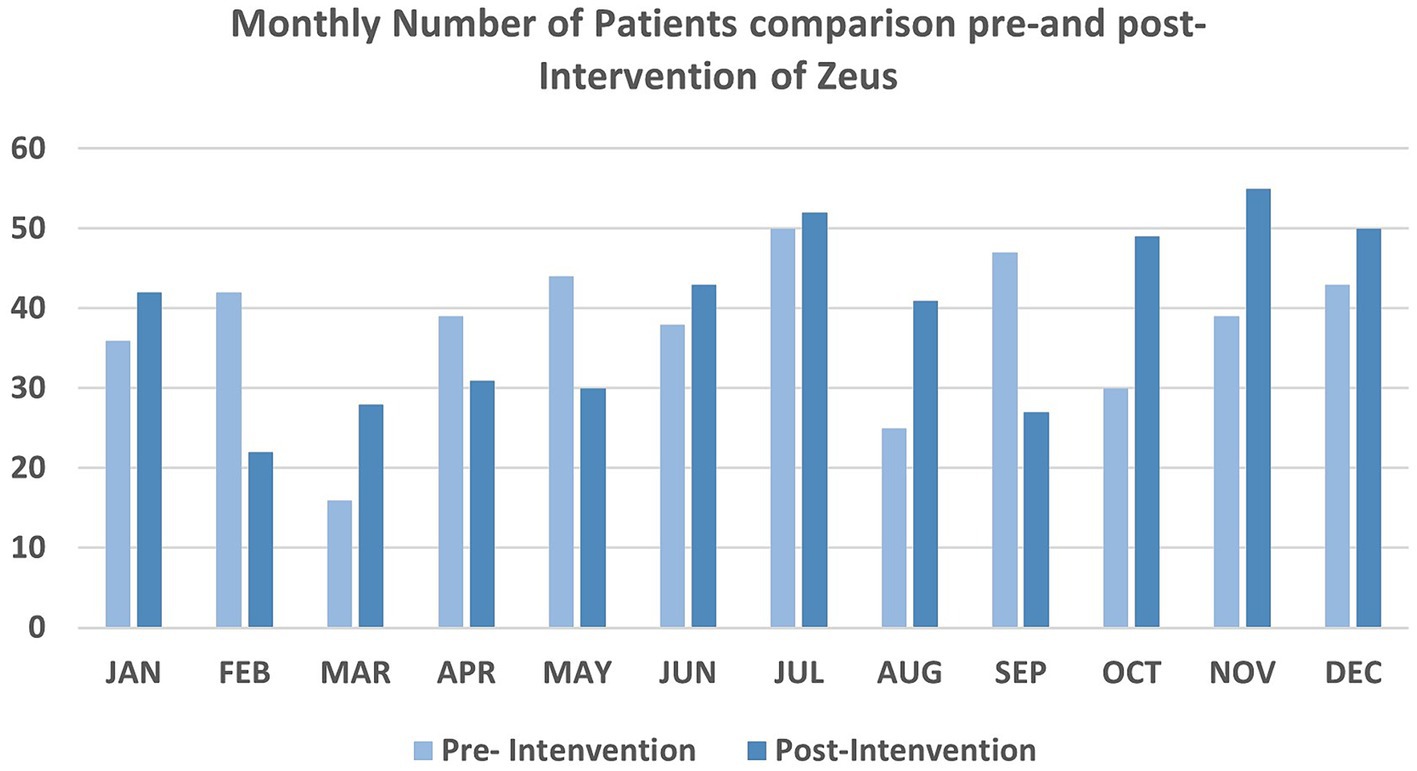
Figure 3. Number of patients using tele-stroke service comparison pre-and post-intervention in each month.
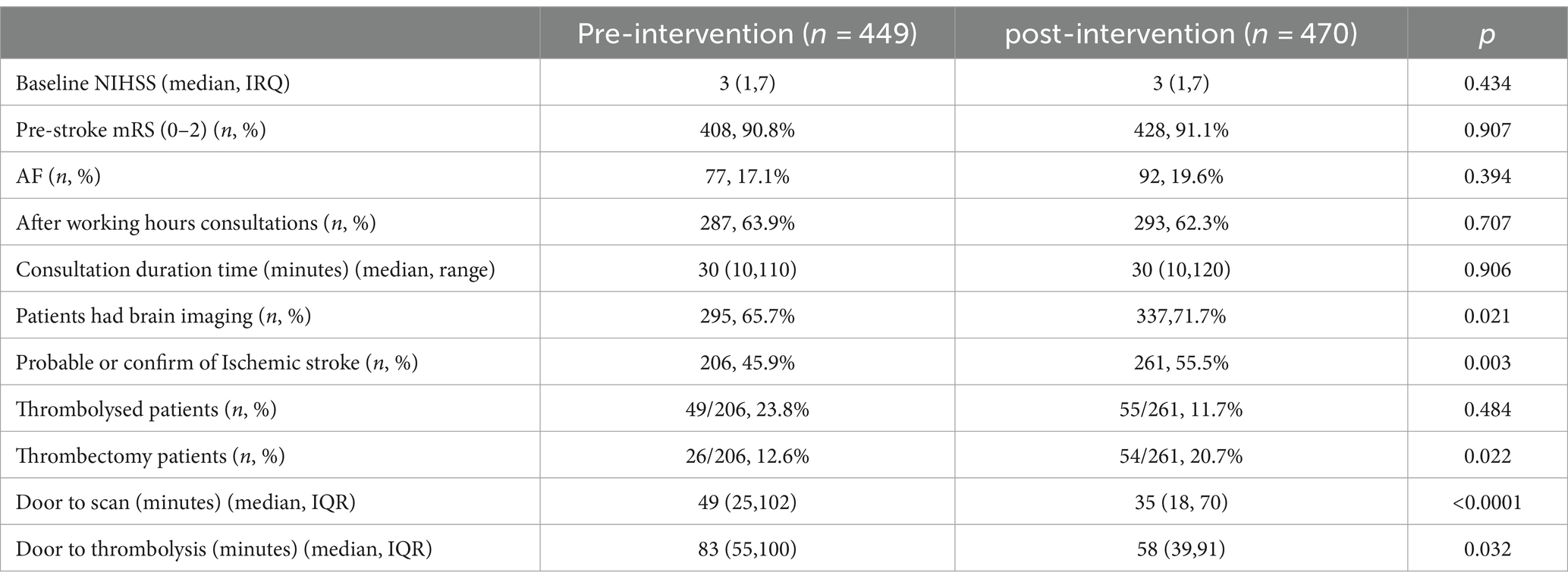
Table 1. Patient characteristics and workflow metrics of the South Australian Tele-Stroke Service (SATS).
In the pre-and post-intervention stage, 206 (45.90%) vs. 261 (55.5%) (p = 0.003) patients were diagnosed with a probable or confirmed ischaemic stroke. Following the study intervention, significantly more patients were treated with thrombectomy in the post-intervention phase compared to the pre-intervention phase (26/206, 12.6% vs. 54/261 20.7%, p = 0.022), but not thrombolysis (pre-intervention 49/206 23.8% vs. post-intervention 55/261, 21.1%, p = 0.484). Of the patients who received thrombolysis during the study period, those seen in the post-intervention phase were treated significantly faster with a median DTT reduction of 25 min (median DTT was 58 min in the post-intervention phase, IQR: 39, 91 vs. the pre-phase median DTT of 83 min, IQR: 55–100, p = 0.0324, Figure 4). The main benefit was seen in the patients’ reduction of the door to treatment, where 4 patients were thrombolysed within 30 min of regional hospital arrival in the pre-intervention phase, and no patients were thrombolysis within 30 min after arrival to the regional hospital in the pre-phase. Of the patients with a DTT over 90 min, there was no considerable difference between the phases (pre-17, post-14).
More patients underwent brain imaging during the post-intervention phase compared to the pre-intervention phase (337,71.7%, vs. 295,65.7%, p = 0.021), reflecting protocol awareness pre-intervention telehealth education and increased access to timely CT scanning. Furthermore, patients seen during the post-intervention phase had significantly shorter door-imaging times [pre-intervention median 35 min (IQR 18–70) vs. 49 min (IQR 25–102; p < 0.0001)]; 72 patients [16.4%_ were scanned within 15 min, and 138 patients (29.4%) were scanned within 30 min post-intervention, compared with 42 (9.4%) and 89 (19.8%) respectively]. Further, a reduction was seen in very long arrival to scan times, 58 (12.3%) patients with a door-scan time > 90 min post-intervention vs. 86 (19.2%) pre-intervention (p = 0.005). Time from regional hospital presentation to thrombectomy is quite long in South Australia due to the distances between towns and hospitals, as well as the limited infrastructure for patient transfers. During the study period, there was a trend to shorter time to thrombectomy in the post- intervention (median time to thrombectomy was 450 min, IQR: 353, 753 min, mean 706 min, and the range between 265 to 1,360 min) compared to the pre-intervention phase (median time to thrombectomy was 595 min, IQR: 532, 815 min, mean 717 min, and the range between 403 to 1725 min), however, the difference did not reach statistical significance (p = 0.9896).
During the study period, there were no changes in the time taken for the remote clinician assessment (the median was 30 min in the pre-intervention phase vs. 30 min in the post-intervention phase, p = 0.906). However, there was a trend towards a higher number of transfers being avoided during the post-intervention phase upon independent case review (206, 45.9% in the pre-intervention phase vs. 251, 53.4% in the post-intervention phase p = 0.271); however, did not reach significant difference. The total number of transfers between the study phases was similar (135, 30.6% in the pre-intervention phase vs. 135, 28.7% in the post-intervention phase, p = 0. 707), reflecting an increased stroke call volume and in-hospital recognition of stroke. Additionally, the mechanism of transfer changed from the road (44 /135, 32.6%, patients in the pre-intervention phase, 37/135, 27.4% patients in the post-intervention phase, p = 0.353) to air (55/135, 40.7%, patients in the pre-intervention phase, and 80/135, 59.3%, patients in the post-intervention phase, p = 0.002).
In this study, we compared the acute telestroke workflow metrics before and after a comprehensive intervention package consisting of improved telehealth technology, education and ongoing quality improvement feedback to sites. Our study found that a higher portion of patients who received thrombectomy in the post-intervention phase had shorter door-to-scan time and significantly faster door-to-thrombolysis time compared to the pre-intervention phase. The support of a seamless tele-stroke platform supported patient care, enhanced quality service improvement activities, and improved access to facilities for regional hospitals, such as imaging. Taken together, the use of education, implementation support and optimised technology led to an overall improved quality of care for patients presenting to regional hospitals in South Australia and the Northern Territory.
Previous studies have shown that telehealth programs improve stroke care in regional areas (7, 13, 14). However, significant challenges still exist in providing regional, low-volume stroke centres with adequate specialist cover with telehealth programs. In the post-intervention phase, the South Australian Tele-Stroke Service (SATS) had more participating regional hospitals using telehealth programs to access acute suspect stroke patients with neurologist consultation. Our study showed that delivering ongoing education and enabling clinicians access to vital acute stroke patient data improved the acute stroke workflows and led to improved time to reperfusion for regional patients. Importantly, during the study, there were changes to the patient care pathway, seen with the increased use of air retrievals. While this change to air-based retrieval did not show a decrease in the time to thrombectomy, it likely contributed to the increased access to thrombectomy for the regional centres. Lastly, the shift to an air-based retrieval model highlights the significant distances that patients have to travel in order to access thrombectomy services in regional South Australia and the Northern Territory.
A limitation of this study was the retrospective data Research Topic for the control period; Information on patients’ outcomes was limited due to the limited record of patients’ follow-up information and challenges in contacting patients after repatriation. Additionally, part of the study was conducted during the COVID-19 pandemic and our study result and the ability to follow-up patients was impacted. Lastly, during the study period, there may have been other quality improvement processes taking place, which may have contributed to the study results.
The intervention of an optimised and customised workflow for telehealth in stroke, with ongoing quality improvement feedback, led to significant improvements in health service delivery from reperfusion treatments for patients presenting to hospitals in regional South Australia and the Northern Territory which have traditionally had limited access to acute stroke care.
The datasets presented in this article are not readily available because anonymized data not published within this article will be made available by request from qualified investigators whose proposal of data use has been approved by an independent review committee. Requests to access the datasets should be directed to AB email: YWJpdmFyZEB1bmltZWxiLmVkdS5hdQ==.
The studies involving humans were approved by the Central Adelaide Local Health Network Human Research Ethics Committee (CALHN HREC; CALHN Reference Number: 19347). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent from the patients/participants or patients/participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
CK: Data curation, Writing – original draft, Writing – review & editing, Conceptualization, Methodology, Project administration. CC: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. MaW: Conceptualization, Data curation, Validation, Visualization, Writing – review & editing. AT: Data curation, Investigation, Methodology, Writing – review & editing. JM: Data curation, Investigation, Methodology, Writing – review & editing. MiW: Conceptualization, Data curation, Investigation, Methodology, Writing – review & editing. JH: Data curation, Formal analysis, Methodology, Visualization, Writing – review & editing. JE: Data curation, Project administration, Writing – review & editing. KD: Data curation, Project administration, Writing – review & editing. BP: Data curation, Project administration, Writing – review & editing. AB: Conceptualization, Data curation, Investigation, Methodology, Project administration, Resources, Supervision, Visualization, Writing – review & editing. MP: Resources, Visualization, Writing – review & editing. SD: Resources, Supervision, Writing – review & editing. GD: Supervision, Visualization, Writing – review & editing. JJ: Data curation, Investigation, Methodology, Writing – review & editing. TK: Conceptualization, Data curation, Investigation, Project administration, Resources, Supervision, Visualization, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The study received support from the grant: The Medical Research Future Fund (MRFF)_Frontier Health and Medical Research (2020) (SD and GD).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Katan, M, and Luft, A. Global burden of stroke. Semin Neurol. (2018) 38:208–11. doi: 10.1055/s-0038-1649503
2. Malhotra, K, Gornbein, J, and Saver, JL. Ischemic strokes due to large-vessel occlusions contribute disproportionately to stroke-related dependence and death: a review. Front Neurol. (2017) 8:651. doi: 10.3389/fneur.2017.00651
3. Anderson, CS, Heeley, E, Huang, Y, Wang, J, Stapf, C, Delcourt, C, et al. Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage. N Engl J Med. (2013) 368:2355–65. doi: 10.1056/NEJMoa1214609
4. Howard, G, Kleindorfer, DO, Cushman, M, Long, DL, Jasne, A, Judd, SE, et al. Contributors to the excess stroke mortality in rural areas in the United States. Stroke. (2017) 48:1773–8. doi: 10.1161/STROKEAHA.117.017089
5. Georgakakos, PK, Swanson, MB, Ahmed, A, and Mohr, NM. Rural stroke patients have higher mortality: an improvement opportunity for rural emergency medical services systems. J Rural Health. (2022) 38:217–27. doi: 10.1111/jrh.12502
6. Cadilhac, DA, Kilkenny, MF, Longworth, M, Pollack, MR, and Levi, CR. Metropolitan-rural divide for stroke outcomes: do stroke units make a difference? Intern Med J. (2011) 41:321–6. doi: 10.1111/j.1445-5994.2010.02280.x
7. Bladin, CF, Kim, J, Bagot, KL, Vu, M, Moloczij, N, Denisenko, S, et al. Improving acute stroke care in regional hospitals: clinical evaluation of the Victorian stroke telemedicine program. Med J Aust. (2020) 212:371–7. doi: 10.5694/mja2.50570
8. Garcia-Esperon, C, Chew, BLA, Minett, F, Cheah, J, Rutherford, J, Wilsmore, B, et al. Impact of an outpatient telestroke clinic on management of rural stroke patients. Aust J Rural Health. (2022) 30:337–42. doi: 10.1111/ajr.12849
9. Tran, L, Lin, L, Spratt, N, Bivard, A, Chew, BLA, Evans, JW, et al. Telestroke assessment with perfusion CT improves the diagnostic accuracy of stroke vs. Mimic Front Neurol. (2021) 12:745673. doi: 10.3389/fneur.2021.745673
10. Kashida, YT, Garcia-Esperon, C, Lillicrap, T, Miteff, F, Garcia-Bermejo, P, Gangadharan, S, et al. The need for structured strategies to improve stroke Care in a Rural Telestroke Network in northern New South Wales, Australia: an observational study. Front Neurol. (2021) 12:645088. doi: 10.3389/fneur.2021.645088
11. Garcia-Esperon, C, Wu, TY, Carraro do Nascimento, V, Yan, B, Kurunawai, C, Kleinig, T, et al. Ultra-Long transfers for endovascular Thrombectomy-Mission impossible?: the Australia-New Zealand experience. Stroke. (2023) 54:151–8. doi: 10.1161/STROKEAHA.122.040480
12. Nor, AM, Davis, J, Sen, B, Shipsey, D, Louw, SJ, Dyker, AG, et al. The recognition of stroke in the emergency room (ROSIER) scale: development and validation of a stroke recognition instrument. Lancet Neurol. (2005) 4:727–34. doi: 10.1016/S1474-4422(05)70201-5
13. Müller-Barna, P, Hubert, GJ, Boy, S, Bogdahn, U, Wiedmann, S, Heuschmann, PU, et al. TeleStroke units serving as a model of care in rural areas: 10-year experience of the TeleMedical project for integrative stroke care. Stroke. (2014) 45:2739–44. doi: 10.1161/STROKEAHA.114.006141
Keywords: Telestroke, tele-medecine, ischaemia stroke, thrombolys, thrombectomy
Citation: Kurunawai C, Chen C, Willcour M, Tan A, Mahadevan J, Waters M, Harvey J, Van Eunen J, Dixon K, Piantedosi B, Bivard A, Parsons MW, Davis SM, Donnan GA, Jannes J and Kleinig T (2024) Implementation of an optimised tele-medicine platform for stroke in South Australia improves patient care. Front. Neurol. 15:1428198. doi: 10.3389/fneur.2024.1428198
Received: 05 May 2024; Accepted: 30 May 2024;
Published: 18 June 2024.
Edited by:
Christoph Gumbinger, Heidelberg University, GermanyReviewed by:
Hrvoje Budincevic, University Hospital Sveti Duh, CroatiaCopyright © 2024 Kurunawai, Chen, Willcour, Tan, Mahadevan, Waters, Harvey, Van Eunen, Dixon, Piantedosi, Bivard, Parsons, Davis, Donnan, Jannes and Kleinig. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Andrew Bivard, YWJpdmFyZEB1bmltZWxiLmVkdS5hdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.