
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol. , 17 September 2024
Sec. Neuro-Oncology and Neurosurgical Oncology
Volume 15 - 2024 | https://doi.org/10.3389/fneur.2024.1412471
 Yufei Liu1*†‡
Yufei Liu1*†‡ Haofei Hu2‡
Haofei Hu2‡ Wenjian Zheng1
Wenjian Zheng1 Zhong Deng1
Zhong Deng1 Jihu Yang1
Jihu Yang1 Xiejun Zhang1
Xiejun Zhang1 Zongyang Li1
Zongyang Li1 Lei Chen1
Lei Chen1 Fanfan Chen1
Fanfan Chen1 Nan Ji3
Nan Ji3 Guodong Huang1*†‡
Guodong Huang1*†‡Background: Reliable quantification of the association between hypertension requiring medication and postoperative 30-day mortality in adult patients who undergo craniotomy for tumor resection is limited. We aimed to explore the associations between these factors.
Materials and methods: This work was a retrospective cohort study that used propensity score matching (PSM) among 18,642 participants from the American College of Surgeons National Surgical Quality Improvement Program database between 2012 and 2015. Hypertension requiring medication and postoperative 30-day mortality were the independent and dependent target variables, respectively. PSM was conducted via nonparsimonious multivariate logistic regression to balance the confounders. Robust estimation methods were used to investigate the association between hypertension requiring medication and postoperative 30-day mortality.
Results: A total of 18,642 participants (52.6% male and 47.4% female) met our inclusion criteria; 7,116 (38.17%) participants with hypertension required medication and had a 3.74% mortality rate versus an overall mortality rate of 2.46% in the adult cohort of patients who underwent craniotomy for tumor resection. In the PSM cohort, the risk of postoperative 30-day mortality significantly increased by 39.0% among patients with hypertension who required medication (OR = 1.390, 95% confidence interval (CI): 1.071–1.804, p = 0.01324) after adjusting for the full covariates. Compared with participants without hypertension requiring medication, those with hypertension requiring medication had a 34.0% greater risk of postoperative 30-day mortality after adjusting for the propensity score (OR = 1.340, 95% CI: 1.040–1.727, p = 0.02366) and a 37.6% greater risk of postoperative 30-day mortality in the inverse probability of treatment weights (IPTW) cohort (OR = 1.376, 95% CI: 1.202, 1.576, p < 0.00001).
Conclusion: Among U.S. adult patients undergoing craniotomy for tumor resection, hypertension requiring medication is a notable contributor to 30-day mortality after surgery, with odds ratios ranging from 1.34 to 1.39.
Craniotomy, the fundamental surgical procedure for treating the vast majority of brain tumors, is associated with significant morbidity and mortality (1, 2). Postoperative 30-day mortality, which is a significant measure of mortality during the postoperative period, offers a reliable assessment of the safety of surgeries and the likelihood of postoperative complications in patients who undergo noncardiac procedures, including craniotomy (2–5). Hypertension, a rapidly increasing worldwide public health issue, is the primary contributor to cardiovascular disease and mortality (6–8).
Hypertension has been acknowledged as a risk factor for postoperative complications and/or mortality in numerous surgeries (9–14). Severe perioperative hypertension can result in excessive surgical bleeding, congestive heart failure, myocardial infarction and acute pulmonary oedema (15). A preoperative systolic blood pressure above 120 mmHg is associated with an increased mortality hazard ratio in cancer patients (16). Hypertension requiring medication was identified as a risk factor for complications occurring within 30 days after surgery in head and neck free tissue transfer (9). Hypertension significantly increases the incidence of postoperative complications during craniotomy for meningioma patients (11). In addition to being a predictor of reoperation for haematoma after craniotomy for tumors based on the analysis of the National Surgical Quality Improvement Program (ACS NSQIP) (12), hypertension was also found to be linked to greater cardiac complications in patients who underwent carotid endarterectomy (13). Hypertension requiring medication was recorded in the ACS NSQIP database. Limited research has been conducted on the correlation between hypertension requiring medication and postoperative 30-day mortality after craniotomy for tumor resection in adult patients. The traditional parsimonious regression model used in previous studies could result in biases caused by remaining or unmeasured confounding factors or overfitting the model (17), which could hinder the detection of the link between hypertension requiring medication and postoperative 30-day mortality. However, propensity score matching (PSM) was used to adjust for heterogeneity in the baseline characteristics (18–20). Hence, conducting a comprehensive retrospective study utilizing PSM data is imperative to assess the correlation between hypertension requiring medication and postoperative 30-day mortality. This study utilized real-world data from a sample of 18,642 adult patients who underwent craniotomy for tumor resection between 2012 and 2015.
The data were extracted from the ACS NSQIP for the present retrospective cross-sectional study. We freely obtained the raw data labeled [S1 Data] from Zhang et al.’s publication titled “Sepsis and Septic shock after craniotomy: Predicting significant patient safety and quality outcome measure.” The article can be accessed at the following website: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7498000/. The initial study included a total of 18,642 individuals who underwent craniotomy for brain tumors between 2012 and 2015. This research was published as an article available to the public, allowing unrestricted distribution, use, and reproduction under the Creative Commons Attribution License. The study was conducted at approximately 400 academic and community hospitals throughout the United States. Hence, our research utilized the provided dataset consisting of 18,642 individuals to conduct a secondary analysis without infringing upon the original authors’ rights.
The data collected in our study included the following variables: (1) continuous variables such as height, weight, and preoperative blood test indicators (hematocrit (HCT), sodium (Na), blood urea nitrogen (BUN), white blood cell (WBC) count, creatine (Cr), and platelet (PLT) count), as well as operating time; and (2) categorical variables, including sex, race, age range, diabetes status, smoking status, year of operation, functional health status, severe chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), hypertension requiring medication, preoperative transfusions, disseminated cancer, preoperative systemic sepsis, steroid use for chronic conditions, >10% loss of body weight in the last 6 months, bleeding disorders, emergency cases, and wound classification. More elaborate details were provided in the original study. Body mass index (BMI) (kg/m2) was calculated by dividing the square of height in meters by weight in kilograms. The data were collected in accordance with standardized conditions and processed via consistent procedures. Our study received exemption from the Clinical Research Ethics Committee of our center.
The focus is on the result of postoperative 30-day mortality, which refers to the occurrence of death within the initial 30 days following discharge from surgery. The variables of interest and the factors that May influence them were investigated. The exposure of interest was hypertension requiring medication. Typically, an individual is considered to have hypertension if their blood pressure is consistently at or above 140/90 mmHg. To be considered for surgery, the patient’s medical record must show that they have documented hypertension and that it is sufficiently severe to necessitate the use of antihypertensive medication (such as diuretics, beta blockers, angiotensin-converting enzyme (ACE) inhibitors, and calcium channel blockers) within 30 days before the main operative procedure or when they are being evaluated as potential candidates for surgery. Hypertension requiring medication was recorded as a categorical variable (yes/no). Patients without hypertension requiring medication were defined as patients who did not have high blood pressure or who had high blood pressure but did not have medication to control it before surgery.
The mean (standard deviation) or median (range) was used to express continuous variables with a normal or nonnormal distribution, respectively, whereas categorical variables were represented as the No. (%). To examine distinctions among various groups, we employed the t test (assuming a normal distribution), the chi-square test (for categorical variables), or Wilcoxon’s rank sum test (for skewed distributions). There were 730 patients (3.92%) with missing BMI values (weight and/or height), 1,532 patients (8.22%) with missing BUN values, 709 patients (3.8%) with missing Cr values, 592 patients (3.18%) with missing WBC values, 440 patients (2.36%) with missing HCT values, and 579 patients (3.11%) with missing PLT values. To address the missing data of covariants, multiple imputations were employed. The analysis of missing data utilized the assumption of missingness at random (MAR).
Creating a well-balanced group via PSM May help minimize notable disparities between patients with hypertension requiring medication and those without it (Table 1). For hypertension requiring medication, the PS was determined by employing an extensive multivariate logistic regression model, wherein hypertension served as the outcome variable and all other initial attributes were considered covariates (21). Table 1 shows the covariates used in the model. The matching variables consisted of BMI, HCT, Na, BUN, WBC, Cr, PLT, duration of surgery, sex, ethnicity, age group, presence of diabetes, smoking habits, year of surgery, functional health status, COPD, CHF, presurgical transfusions, disseminated cancer, presurgical systemic sepsis, use of steroids for chronic conditions, weight loss exceeding 10% in the last 6 months, bleeding disorders, emergency cases, and wound classification. The PSM utilized a 1:1 greedy algorithm that did not involve replacement and had a caliper width of 0.01. In addition, we attempted to locate a stricter caliper; however, the model that provided the closest match was 0.01. To assess the degree of balance between the matched groups, we calculated the standardized difference (SD) for each covariate at the beginning of the study. Satisfaction with the matching was considered acceptable if the standardized mean differences were less than 10% (22, 23). The C-index was computed for the logistic regression model employed in propensity score matching.
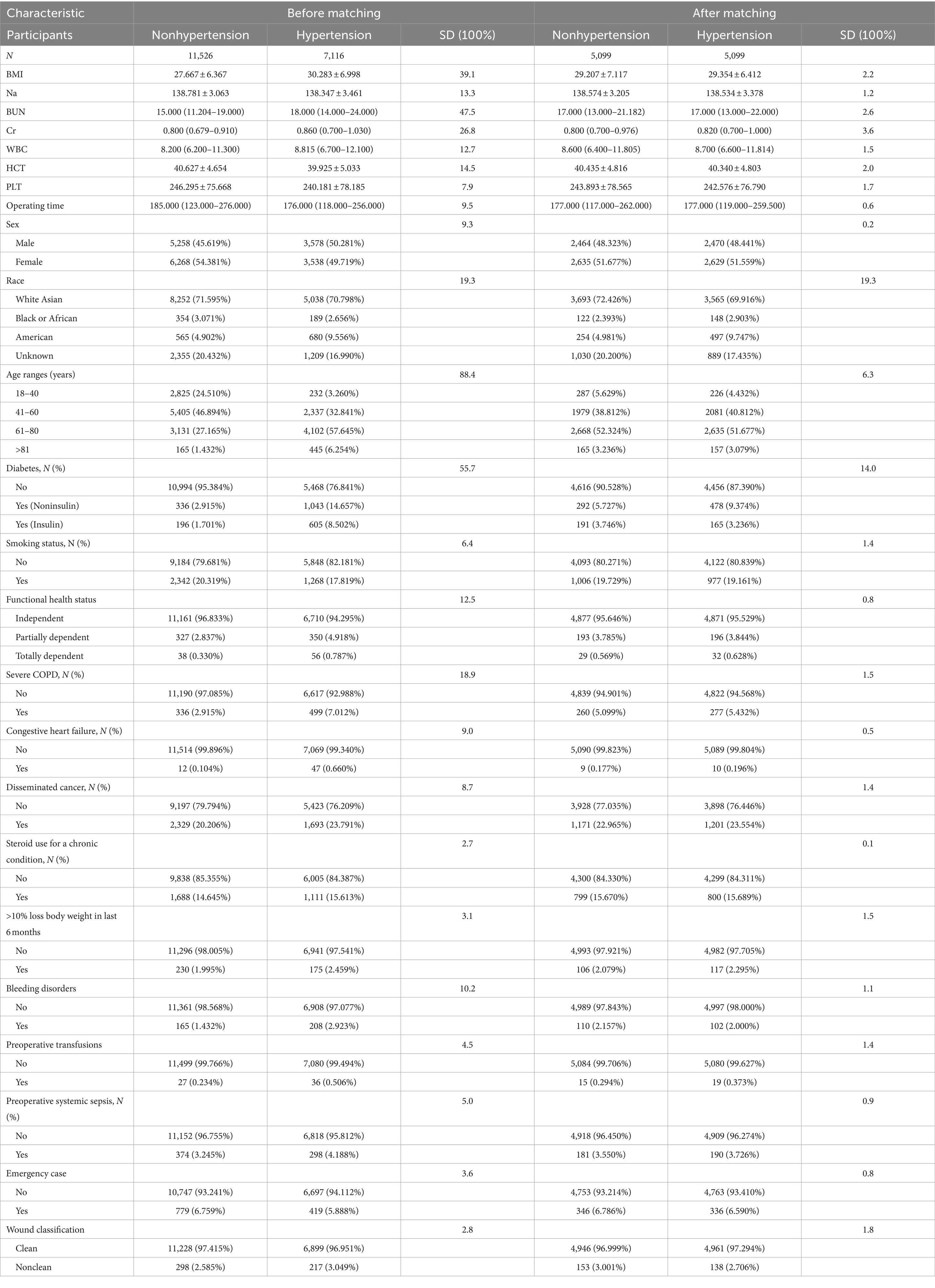
Table 1. Baseline characteristics before and after propensity score matching in the original cohort.
To determine the independent relationships between hypertension requiring medication and postoperative 30-day mortality, the researchers utilized the doubly robust estimation technique, which combines a multivariate regression model with a propensity score model. In sensitivity analyses, the inverse probability of treatment weight (IPTW) served as the weight for the estimated propensity score, 1/PS, for individuals with hypertension requiring medication and the inverse of 1 minus the propensity score, 1/(1–PS), for individuals without hypertension requiring medication (24). The IPTW was used to calculate a standardized effect estimate using all study participants as the reference population. In the sensitivity analysis, we included two additional association inference models in both the original cohort and the weighted cohort. The reported and compared effect sizes and p values were calculated from all of these models. All the results were reported based on the STROCSS statement (25). Furthermore, we investigated the possibility of unquantified confounding effects between hypertension requiring medication and the likelihood of postoperative 30-day mortality through the computation of E values (26).
Both Empower Stats (X & Y Solutions, Boston, MA, United States) and the statistical package R1 were utilized for the statistical analysis. We calculated ORs and 95% CIs. A significance level of less than 0.05 was used to indicate statistical significance.
A total of 18,642 individuals met the inclusion criteria (Figure 1), 52.6% of whom were male and 47.4% of whom were female. This population included 7,116 (38.17%) patients with hypertension requiring medication and 11,526 (61.83%) patients without hypertension requiring medication. Prior to PSM, several fundamental attributes differed between individuals with hypertension requiring medication and without hypertension requiring medication (Table 1). We found that individuals with hypertension requiring medication generally had higher BMIs; Na, BUN, and Cr levels; and WBC counts. With the use of one-to-one PSM, 5,099 patients with hypertension requiring medication were matched with 5,099 patients without hypertension requiring medication. Following the matching process, the majority of variables (excluding race and diabetes status) exhibited standardized differences of less than 10.0%, suggesting successful matching of propensity scores. Specifically, fundamental attributes exhibited minimal disparities between the two cohorts.
A logistic regression model was used to calculate the propensity score, resulting in a c-statistic of 0.794 (Figure 2).
With respect to the propensity score-matched cohort, we employed a binary logistic regression model to assess the association between hypertension requiring medication and postoperative 30-day mortality. We present the findings from unadjusted, minimally adjusted, fully adjusted, and propensity score-adjusted analyses simultaneously (Table 2). According to the basic model, hypertension requiring medication was strongly associated with postoperative 30-day mortality (OR = 1.366, 95% CI 1.060–1.758; p = 0.0157). Specifically, individuals with hypertension requiring medication had a 36.6% greater chance of experiencing postoperative 30-day mortality than did those without hypertension requiring medication. With minimal adjustments (adjusted for sex, race, and age groups), the strong correlation remained significant (OR = 1.386, 95% CI 1.074–1.788, p = 0.0121). We were also able to identify a significant correlation after accounting for all the covariates (sex, ethnicity, age groups, body mass index, hematocrit, sodium, blood urea nitrogen, white blood cell count, creatinine, platelet count, duration of surgery, diabetes, smoking habits, year of surgery, functional health status, severe chronic obstructive pulmonary disease, congestive heart failure, presurgical transfusions, metastatic cancer, presurgical systemic sepsis, steroid use for chronic illness, more than 10% weight loss in the past 6 months, bleeding disorders, emergency surgery, and wound classification) (odds ratio = 1.390, 95% CI 1.071–1.804, p = 0.01324). After adjusting for propensity scores, the likelihood of postoperative 30-day mortality increased by 34% among individuals with hypertension requiring medication (odds ratio = 1.340, 95% CI 1.0401.727, p = 0.02366). These findings suggest that patients with hypertension requiring medication prior to craniotomy have an increased risk of postoperative 30-day mortality.
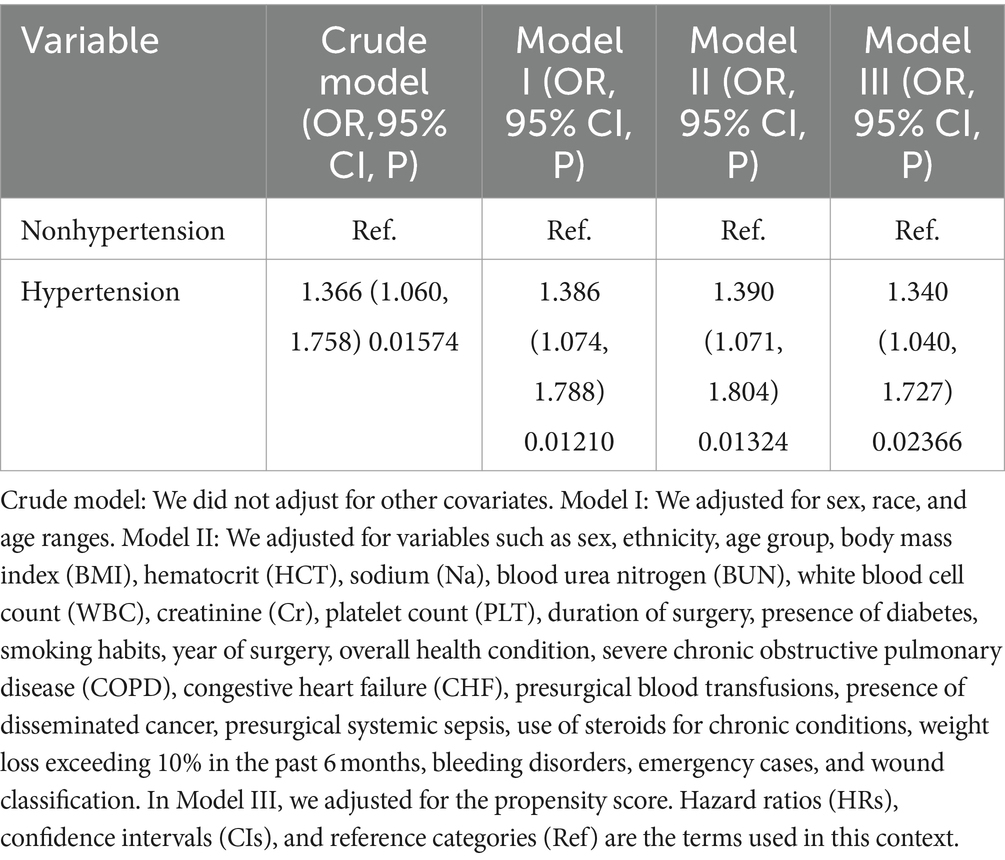
Table 2. Associations between hypertension requiring medication and postoperative 30-day mortality according to different models.
We used the IPTW to generate a weighted cohort. To guarantee the strength of the findings, we conducted a binary logistic regression analysis to evaluate the association between hypertension requiring medication and postoperative 30-day mortality in both the initial group and the weighted group. Table 3 displays the models that were not adjusted, minimally adjusted, or fully adjusted for the two cohorts. In both the initial group and the weighted group, we discovered a correlation between postoperative 30-day mortality and the probability of postoperative 30-day mortality. According to the full model, patients with hypertension requiring medication had a 39.2% greater risk of postoperative 30-day mortality in the original cohort (OR = 1.392, 95% CI 1.120, 1.729, p = 0.00285) and a 37.6% greater risk in the weighted cohort (OR = 1.376, 95% CI 1.202, 1.576, p < 0.00001) than patients without hypertension requiring medication.
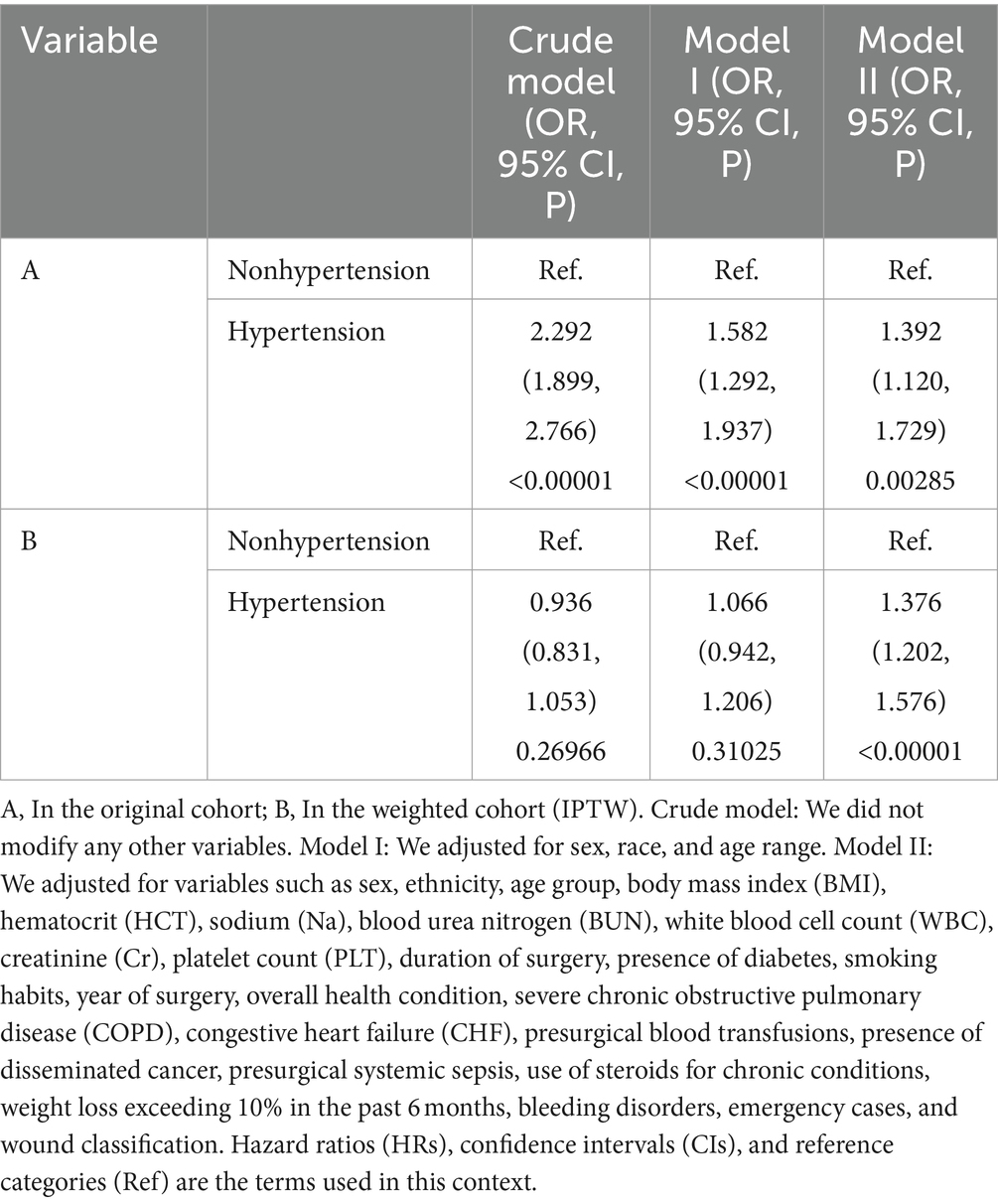
Table 3. Associations between hypertension requiring medication and postoperative 30-day mortality according to the original and weighted cohort (IPTW) models.
In addition, the authors generated an E value to assess the sensitivity to unmeasured confounding variables. The value of E was 2.13. The E value exceeded the relative risk associated with unmeasured confounders and hypertension requiring medication, indicating that unmeasured or unidentified confounders had minimal impact on the association between hypertension necessitating medication and postoperative 30-day mortality.
In current studies on various types of brain tumors, such as brain metastasis, meningioma, and glioblastoma (18, 27–30), PSM is commonly utilized to account for variations in baseline characteristics between two groups. After matching to balance the baseline characteristics of 16,335 participants in the 2012–2018 NSQIP database, the duration of surgery was shown to predict the prognosis following craniotomy for supratentorial brain tumors (29). Similarly, we adopted the PSM method to ensure homogeneity in the participants’ backgrounds. By utilizing information on hypertension requiring medication and postoperative 30-day mortality from the ACS NSQIP database, we discovered that employing three distinct approaches to manage potential bias did not yield significant disparities in the estimated impact, with odds ratios ranging from 1.340 (95% CI 1.040, 1.727) for the propensity score-matched analysis to 1.390 (95% CI 1.071, 1.804) after accounting for all covariates. This retrospective study of individualized PSMs revealed that hypertension requiring medication was a major factor influencing postoperative 30-day mortality after craniotomy for tumor resection in adult patients in the U.S., with odds ratios ranging from 1.34 to 1.39. Gaining comprehensive knowledge about hypertension requiring medication as a potential determinant of postoperative 30-day mortality will enhance our comprehension and communication of risks with patients, ultimately resulting in the development of more individualized prevention and management strategies.
Several prior investigations have indicated that high blood pressure is linked to hidden brain conditions, including cognitive Decline, cerebrovascular accidents, and subclinical abnormalities in the blood vessels of the brain (31–35). Hypertension causes alterations in cerebral small- and medium-to-large artery function and structure that can impair blood flow and are related to oxidative stress, endothelial dysfunction and inflammation (32–34). Dolui S et al. confirmed that intensive blood pressure treatment, compared with standard treatment, was associated with an increase, not a Decrease, in cerebral perfusion and was most notably associated with a history of cardiovascular disease (36). Severe perioperative hypertension can result in excessive surgical bleeding, which May increase mortality (12, 15). Dasenbrock et al. proposed that high blood pressure was a factor that could predict the need for a second surgery to remove a blood clot after skull surgery for a tumor, and the removal of the blood clot was strongly linked to a greater risk of death within 30 days after the operation (12). According to the aforementioned research, changes in the structure of the cerebral artery and cerebral blood flow, the occurrence of cerebral hemorrhage after surgery, and the presence of other cardiovascular ailments might significantly contribute to the 30-day mortality rate in brain tumor patients with hypertension requiring medication. Villela PB et al. reported that deaths associated with hypertensive diseases were mentioned up to 4 times more frequently in Brazil from 2004 to 2013 when evaluated as multiple causes of death rather than when selected as the primary cause of death. This finding highlights the critical importance of improving hypertension control to prevent fatalities (37).
Our research has certain notable advantages that should be acknowledged. To our knowledge, few retrospective investigations have utilized PSM to examine the correlation between hypertension requiring medication and 30-day mortality following craniotomy for tumor resection in adult patients. PSM aims to equalize the allocation of recorded baseline covariates to reduce the impact of observed confounding variables. To ensure the dependability of the findings, a sensitivity analysis was performed, specifically utilizing the IPTW method to create a weighted group. The relationship between hypertension requiring medication and postoperative 30-day mortality was subsequently investigated in this weighted cohort. Furthermore, compared with the majority of prior analogous investigations, our sample size was relatively large, and the participants were recruited from various centers.
Conversely, our study has several limitations that should be noted. First, because our study relies on a secondary examination of published information, we were unable to completely eliminate certain residual and/or unmeasured confounding variables that May influence the estimated correlation (for instance, various factors, including eating patterns, economic conditions, medication therapies, properties of noncancerous and cancerous tissues, and diverse categories and locations of brain tumors). The database used in our study lacked information on pharmacological treatments for hypertension. Nevertheless, we calculated the E value to assess the possible impact of unmeasured variables. The study utilized data gathered from a diverse and sizable population of individuals diagnosed with brain tumors. Therefore, the association and our other findings remain highly plausible. Further extensive investigations should gather and assess the effects of the aforementioned potential variables and information that were not incorporated in the current research.
This retrospective study of individualized PSMs revealed that hypertension requiring medication was a major factor influencing 30-day mortality after craniotomy for tumor resection in adult patients in the United States, with odds ratios ranging from 1.34 to 1.39. Among patients who required medication for hypertension and had high propensity scores, the risk of postoperative 30-day mortality increased by 34–39% compared with patients without hypertension requiring medication and had low propensity scores. In adult patients undergoing craniotomy for tumor resection, blood pressure is a risk factor that can be modified through interventions to prevent postoperative 30-day mortality. For patients with hypertension requiring medication, preoperative blood pressure should be controlled by drugs before craniotomy to reduce the risk of postoperative complications.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
The studies involving humans were approved by Clinical Research Ethics Committee of Shenzhen Second People’s Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because we examined data that had been gathered earlier, with patient information kept confidential.
YL: Data curation, Methodology, Writing – original draft, Conceptualization. HH: Formal analysis, Methodology, Writing – original draft. WZ: Writing – review & editing, Investigation. ZD: Conceptualization, Writing – original draft. JY: Writing – review & editing. XZ: Writing – review & editing, Investigation. ZL: Writing – original draft. LC: Investigation, Validation, Writing – review & editing. FC: Supervision, Validation, Writing – review & editing. NJ: Supervision, Writing – review & editing. GH: Supervision, Validation, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Shenzhen Second People’s Hospital Clinical Research Fund of the Guangdong Province High-level Hospital Construction Project (Grant no. 20233357023).
All the authors are grateful to Zhang et al. for supplying the information to be examined.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2024.1412471/full#supplementary-material
1. ^http://www.R-project.org, The R Foundation.
1. Cinotti, R, Bruder, N, Srairi, M, Paugam-Burtz, C, Beloeil, H, Pottecher, J, et al. Prediction score for postoperative neurologic complications after brain tumor craniotomy: a multicenter observational study. Anesthesiology. (2018) 129:1111–20. doi: 10.1097/ALN.0000000000002426
2. Senders, JT, Muskens, IS, Cote, DJ, Goldhaber, NH, Dawood, HY, Gormley, WB, et al. Thirty-day outcomes after craniotomy for primary malignant brain tumors: a national surgical quality improvement program analysis. Neurosurgery. (2018) 83:1249–59. doi: 10.1093/neuros/nyy001
3. Devereaux, PJ, Biccard, BM, Sigamani, A, Xavier, D, Chan, M, Srinathan, SK, et al. Association of postoperative high-sensitivity troponin levels with myocardial injury and 30-day mortality among patients undergoing noncardiac surgery. JAMA. (2017) 317:1642–51. doi: 10.1001/jama.2017.4360
4. Smith, T, Li, X, Nylander, W, and Gunnar, W. Thirty-day postoperative mortality risk estimates and 1-year survival in veterans health administration surgery patients. JAMA Surg. (2016) 151:417–22. doi: 10.1001/jamasurg.2015.4882
5. Liu, Y, Hu, H, Han, Y, Li, L, Li, Z, Zhang, L, et al. Body mass index has a nonlinear association with postoperative 30-day mortality in patients undergoing craniotomy for tumors in men: an analysis of data from the ACS NSQIP database. Front Endocrinol (Lausanne). (2022) 13:868968. doi: 10.3389/fendo.2022.868968
6. Lewington, S, Lacey, B, Clarke, R, Guo, Y, Kong, XL, Yang, L, et al. The burden of hypertension and associated risk for cardiovascular mortality in China. JAMA Intern Med. (2016) 176:524–32. doi: 10.1001/jamainternmed.2016.0190
7. Armas, RN, Dobell, E, Lacey, B, Varona-Perez, P, Burrett, JA, Lorenzo-Vazquez, E, et al. Burden of hypertension and associated risks for cardiovascular mortality in Cuba: a prospective cohort study. Lancet Public Health. (2019) 4:e107–15. doi: 10.1016/S2468-2667(18)30210-X
8. Van den Meiracker, AH. A global approach to hypertension. EuroIntervention. (2013) 9:R16–20. doi: 10.4244/EIJV9SRA4
9. Brauer, PR, Byrne, PJ, Prendes, BL, Ku, JA, Ciolek, PJ, Jia, X, et al. Association between hypertension requiring medication and 30-day outcomes in head and neck microvascular surgery. Head Neck. (2022) 44:168–76. doi: 10.1002/hed.26907
10. Lin, JJ, Conroy, PC, Romero-Hernandez, F, Yilma, M, Feng, J, Hirose, K, et al. Hypertension requiring medication use: a silent predictor of poor outcomes after pancreaticoduodenectomy. J Gastrointest Surg. (2023) 27:328–36. doi: 10.1007/s11605-022-05577-6
11. Sughrue, ME, Rutkowski, MJ, Shangari, G, Chang, HQ, Parsa, AT, Berger, MS, et al. Risk factors for the development of serious medical complications after resection of meningiomas. Clinical article. J Neurosurg. (2011) 114:697–704. doi: 10.3171/2010.6.JNS091974
12. Dasenbrock, HH, Yan, SC, Chavakula, V, Gormley, WB, Smith, TR, Claus, EB, et al. Unplanned reoperation after craniotomy for tumor: a national surgical quality improvement program analysis. Neurosurgery. (2017) 81:761–71. doi: 10.1093/neuros/nyx089
13. Dakour, AH, Paracha, N, Nejim, B, Locham, S, and Malas, MB. Anesthetic type and hospital outcomes after carotid endarterectomy from the vascular quality initiative database. J Vasc Surg. (2018) 67:1419–28. doi: 10.1016/j.jvs.2017.09.028
14. El, MM, and Rahman, IA. Perioperative morbidity and mortality of laparoscopic sleeve gastrectomy (LSG) in a single-surgeon experience on 892 patients over 11 years. World J Surg. (2023) 47:2809–15. doi: 10.1007/s00268-023-07123-0
15. Gill, R, and Goldstein, S. Evaluation and management of perioperative hypertension. Treasure Island, FL: StatPearls Publishing (2023).
16. Yu, HC, Luo, YX, Peng, H, Wang, XL, Yang, ZH, Huang, MJ, et al. Association of perioperative blood pressure with long-term survival in rectal cancer patients. Chin J Cancer. (2016) 35:38. doi: 10.1186/s40880-016-0100-8
17. Siu, JM, McCarty, JC, Gadkaree, S, Caterson, EJ, Randolph, G, Witterick, IJ, et al. Association of Vessel-Sealant devices vs conventional hemostasis with postoperative neck hematoma after thyroid operations. JAMA Surg. (2019) 154:e193146. doi: 10.1001/jamasurg.2019.3146
18. Chen, PC, Yeh, YM, Chu, CT, Su, PF, Chiu, PH, Lin, BW, et al. HER2 amplification in colorectal cancer with brain metastasis: a propensity score matching study. Eur J Cancer. (2023) 181:62–9. doi: 10.1016/j.ejca.2022.12.019
19. Gerritsen, J, Zwarthoed, RH, Kilgallon, JL, Nawabi, NL, Jessurun, C, Versyck, G, et al. Effect of awake craniotomy in glioblastoma in eloquent areas (GLIOMAP): a propensity score-matched analysis of an international, multicentre, cohort study. Lancet Oncol. (2022) 23:802–17. doi: 10.1016/S1470-2045(22)00213-3
20. Kann, BH, Lester-Coll, NH, Park, HS, Yeboa, DN, Kelly, JR, Baehring, JM, et al. Adjuvant chemotherapy and overall survival in adult medulloblastoma. Neuro-Oncology. (2017) 19:now150–69. doi: 10.1093/neuonc/now150
21. Ahmed, A, Husain, A, Love, TE, Gambassi, G, Dell'Italia, LJ, Francis, GS, et al. Heart failure, chronic diuretic use, and increase in mortality and hospitalization: an observational study using propensity score methods. Eur Heart J. (2006) 27:1431–9. doi: 10.1093/eurheartj/ehi890
22. Navale, SM, Szubski, CR, Klika, AK, Schiltz, NK, Desai, PP, and Barsoum, WK. The impact of solid organ transplant history on inpatient complications, mortality, length of stay, and cost for primary total hip arthroplasty admissions in the United States. J Arthroplast. (2017) 32:1107–1116.e1. doi: 10.1016/j.arth.2016.10.017
23. Brito, JP, Deng, Y, Ross, JS, Choi, NH, Graham, DJ, Qiang, Y, et al. Association between generic-to-generic levothyroxine switching and thyrotropin levels among US adults. JAMA Intern Med. (2022) 182:418–25. doi: 10.1001/jamainternmed.2022.0045
24. Robins, JM, Hernan, MA, and Brumback, B. Marginal structural models and causal inference in epidemiology. Epidemiology. (2000) 11:550–60. doi: 10.1097/00001648-200009000-00011
25. Mathew, G, Agha, R, Albrecht, J, Goel, P, Mukherjee, I, Pai, P, et al. STROCSS 2021: strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Int J Surg. (2021) 96:106165. doi: 10.1016/j.ijsu.2021.106165
26. Haneuse, S, VanderWeele, TJ, and Arterburn, D. Using the E-value to assess the potential effect of unmeasured confounding in observational studies. JAMA. (2019) 321:602–3. doi: 10.1001/jama.2018.21554
27. Chan, AY, Choi, EH, Oh, MY, Vadera, S, Chen, JW, Golshani, K, et al. Elective versus nonelective brain tumor resections: a 5-year propensity score matching cost comparison analysis. J Neurosurg. (2022) 136:40–4. doi: 10.3171/2020.12.JNS203401
28. Oya, S, Ikawa, F, Ichihara, N, Wanibuchi, M, Akiyama, Y, Nakatomi, H, et al. Effect of adjuvant radiotherapy after subtotal resection for WHO grade I meningioma: a propensity score matching analysis of the brain tumor registry of Japan. J Neuro-Oncol. (2021) 153:351–60. doi: 10.1007/s11060-021-03775-x
29. McHayle, A, Pertsch, NJ, Toms, SA, and Weil, RJ. Operative duration and early outcomes in patients having a supratentorial craniotomy for brain tumor: a propensity matched analysis. J Clin Neurosci. (2021) 92:207–14. doi: 10.1016/j.jocn.2021.08.005
30. Wang, Z, Li, J, Yuan, Y, Li, T, Zuo, M, and Liu, Y. Prognostic significance of preoperative systemic inflammation response index in newly diagnosed glioblastoma patients underwent gross total resection: a propensity score matching analysis. World J Surg Oncol. (2022) 20:137. doi: 10.1186/s12957-022-02588-0
31. Ma, Y, Yilmaz, P, Bos, D, Blacker, D, Viswanathan, A, Ikram, MA, et al. Blood pressure variation and subclinical brain disease. J Am Coll Cardiol. (2020) 75:2387–99. doi: 10.1016/j.jacc.2020.03.043
32. Di Chiara, T, Del, CA, Daidone, M, Scaglione, S, Norrito, RL, Puleo, MG, et al. Pathogenetic mechanisms of hypertension-brain-induced complications: focus on molecular mediators. Int J Mol Sci. (2022) 23:23. doi: 10.3390/ijms23052445
33. Liu, W, Huang, X, Liu, X, Ortega, D, Chen, L, Chen, Z, et al. Uncontrolled hypertension associates with subclinical cerebrovascular health globally: a multimodal imaging study. Eur Radiol. (2021) 31:2233–41. doi: 10.1007/s00330-020-07218-5
34. Pires, PW, Dams, RC, Matin, N, and Dorrance, AM. The effects of hypertension on the cerebral circulation. Am J Physiol Heart Circ Physiol. (2013) 304:H1598–614. doi: 10.1152/ajpheart.00490.2012
35. Kelly, DM, and Rothwell, PM. Blood pressure and the brain: the neurology of hypertension. Pract Neurol. (2020) 20:100–8. doi: 10.1136/practneurol-2019-002269
36. Dolui, S, Detre, JA, Gaussoin, SA, Herrick, JS, Wang, D, Tamura, MK, et al. Association of intensive vs standard blood pressure control with cerebral blood flow: secondary analysis of the SPRINT MIND randomized clinical trial. JAMA Neurol. (2022) 79:380–9. doi: 10.1001/jamaneurol.2022.0074
Keywords: brain tumor, craniotomy, hypertension, propensity score matching, mortality
Citation: Liu Y, Hu H, Zheng W, Deng Z, Yang J, Zhang X, Li Z, Chen L, Chen F, Ji N and Huang G (2024) Association between hypertension requiring medication and postoperative 30-day mortality in adult patients with tumor craniotomy: an analysis of data using propensity score matching. Front. Neurol. 15:1412471. doi: 10.3389/fneur.2024.1412471
Received: 05 April 2024; Accepted: 06 September 2024;
Published: 17 September 2024.
Edited by:
Yuankun Cai, Wuhan University, ChinaReviewed by:
Chaobin Wang, Luoyang Central Hospital Affiliated to Zhengzhou University, ChinaCopyright © 2024 Liu, Hu, Zheng, Deng, Yang, Zhang, Li, Chen, Chen, Ji and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Guodong Huang, aHVhbmdndW9kb25nQGVtYWlsLnN6dS5lZHUuY24=; Yufei Liu, NDcxODc5NjEwQHFxLmNvbQ==
†ORCID: Yufei Liu, https://orcid.org/0000-0002-7570-6978
Guodong Huang, https://orcid.org/0000-0002-2848-7581
‡These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.