- 1Department of Pathophysiology and Transplantation, Università degli Studi di Milano, Milan, Italy
- 2IRCCS Fondazione Don Carlo Gnocchi, Milan, Italy
- 3AIAS di Milano Onlus, Milan, Italy
- 4Laboratory of Computational Neuroimaging, IRCCS San Camillo Hospital, Venice, Italy
- 5Padova Neuroscience Center, Università degli Studi di Padova, Padua, Italy
- 6Department of Rehabilitation, San Carlo Borromeo Hospital, Milan, Italy
- 7Division of Physical and Rehabilitation Medicine, Fondazione Opera San Camillo, Presidio di Torino, Italy
- 8Department of Neurological Sciences, Neurorehabilitation Clinic, AOU delle Marche, Ancona, Italy
- 9Montecatone Rehabilitation Institute, Imola (BO), Italy
- 10Department of Biotechnological and Applied Clinical Sciences (DISCAB), University of L’Aquila, L'Aquila, Italy
- 11Department of Neuroscience, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health, University of Genoa, Genoa, Italy
- 12IRCCS Ospedale Policlinico San Martino, IRCCS, Genoa, Italy
- 13Laboratory Department of Experimental Medicine (DIMES), Section of Human Physiology, University of Genoa, Genoa, Italy
- 14Department of Biomedical and Neuromotor Sciences (DIBINEM), Alma Mater Studiorum - Università di Bologna, Bologna, Italy
- 15Unit of Occupational Medicine, IRCCS Azienda Ospedaliero-Universitaria di Bologna, Bologna, Italy
- 16Azienda Sanitaria Universitaria Giuliano Isontina (ASUGI), Trieste, Italy
Background and purpose: This study aimed to investigate the factors that influence physiotherapists’ decision in choosing restorative or compensatory rehabilitation during gait training in people with neurological disorders (PwNDs) and the different treatments used in the approaches.
Methods: This cross-sectional analysis used the baseline data from an observational cohort study. We analyzed data from 83 PwNDs (65 people after stroke, 5 with multiple sclerosis, and 13 with Parkinson’s disease) who underwent at least 10 sessions of physiotherapy (PT) focusing on gait function. Performance was quantified using the modified Dynamic Gait Index (MDGI), three impairment domains of Fugl–Meyer Assessment for lower extremity (mFM-LL), Activities-specific Balance Confidence (ABC), modified Barthel Index (mBI), Mini-Mental State Examination (MMSE), and Motivational Index (MI). Forty-three physiotherapists completed a treatment report form categorizing the rehabilitation approach and specifying treatments used (e.g., resistance training and proprioceptive exercises).
Results: Fifty-six subjects underwent restorative rehabilitation approach. The univariate predictors of restorative approach were being in the subacute phase with a disease onset of less than 180 days, (odds ratio [95%CI]; 3.27[1.19–9.24]), mFM-LL (1.25[1.11–1.44]), MMSE (0.85[0.67–1.00]), and number of sessions (1.03[1–1.01]). The backward stepwise analysis revealed an association between restorative and subacute phase (36.32[4.11–545.50]), mFM-LL (3.11[1.55–9.73]), mBI (1.79[1.08–3.77]), MMSE (0.46[0.25–0.71]), and the interaction between mFM-LL and mBI (0.99[0.98–1.00]). No statistically significant association between treatments used and approach was found (p = 0.46).
Discussion and conclusion: The restorative approach was more commonly used to improve gait. The main variables associated with this approach were: being in the subacute phase of the disease, a low level of impairment, and a high level of functional independence at baseline. However, few differences were found between the treatments used for the restorative or compensatory approaches, as similar PT treatments were used for both.
Introduction
People with neurological disorders (PwNDs) typically present limitations in performing functional tasks (1, 2). Therefore, a major focus of neurological rehabilitation is to maximize functional motor abilities, such as walking (3). It has been postulated that functional improvements occur due to a combination of two phenomena: (1) motor recovery via the relearning of premorbid motor skills and (2) motor compensation via learning new movement strategies (4).
Although both motor recovery and compensation can lead to functional improvements, the decision between the two approaches is not trivial. When motor recovery is prioritized, more emphasis is placed on movement quality, providing more feedback on movement performance, leading to the relearning of skilled movements. Conversely, when compensation is prioritized, physiotherapists train people to use assistive devices or other motor strategies. As a result, less attention is paid to the quality of the movement, and this could lead to different rehabilitation outcomes, as suggested by Krakauer (5).
The factors leading to the selection of motor recovery or compensation are unknown. The clinical decision-making process may be influenced by evidence-based practice recommendations and implicit, subjective theories based on clinical experience and contextual factors (6, 7). The physiotherapist’s expectation of good functional improvement may lead to the adoption of a restorative rather than a compensatory approach. Factors influencing the outcome of motor rehabilitation vary. These include people after stroke age, the severity of walking disabilities, and balance impairment at baseline (8, 9). For people with multiple sclerosis (MS), the impact of balance impairment, disease severity, and disease progression on gait rehabilitation outcomes is still under debate (10–12). In people with Parkinson’s disease (PD), age, motor and cognitive impairment, and disease severity were factors associated with gait improvements (13).
To date, no studies have examined the relationship between these factors and the clinical decision-making process in everyday clinical practice. Our hypothesis is that the restorative approach is chosen when a larger number of sessions are available and clinical characteristics suggest a good clinical outcome. The aim of this study was to investigate the factors influencing the choice between rehabilitation approaches. The secondary aim of this study was to investigate whether restorative or compensatory approaches consisted of different physiotherapy (PT) treatments in everyday clinical practice.
Methods
Study design
Data for this cross-sectional study were collected in a larger multicenter longitudinal prospective cohort study investigating the contents of neurological PT (see Supplementary Figure 1) (3). The multicenter network involved a total of nine facilities: four research/university hospitals, two general hospitals, and three rehabilitation centers. All centers provided multidisciplinary rehabilitation, including both outpatient and inpatient services.
The study was registered on clinicaltrial.gov (ID: NCT04386863) and was approved by the Ethical Committee of [redacted]. Recruitment began in June 2018 and ended in July 2021. The study was conducted in agreement with the Declaration of Helsinki, and all participants provided written informed consent.
Participants
A convenience sample was recruited for the study from a variety of rehabilitation facilities in order to minimize the potential for selection bias. All the eligible subjects were recruited consecutively. Participants were individuals after stroke and those with MS or PD who met the following inclusion criteria: age > 18 years and had received at least 10 20- to 50-min PT sessions aimed at improving walking function. Only subjects who were unable to understand the aims of the study and provide informed consent were excluded.
Experimental procedures
The recruited subjects followed rehabilitation programs set by a multidisciplinary team, including healthcare professionals and physicians. All participants underwent PT sessions foreseen by the National Healthcare System and were clinically assessed before the treatment. All clinical evaluations were performed by an experienced clinical researcher not involved in the PT sessions. For each participant, the physiotherapist who administered the treatment completed a treatment report form at the end of the rehabilitation program. In the case of a physiotherapist treating more than one subject, a form for each subject being treated was completed.
Clinical assessment
Demographic information, such as sex, age, and disease onset, was collected, along with clinical outcomes measured at the beginning of the rehabilitation program to characterize participants. Subjects with a disease onset of less than 180 days were considered subacute. Thus, subjects with MS and PD were considered all chronic. The modified Dynamic Gait Index (MDGI) is a clinical scale that was used to assess balance performances in dynamic tasks (the best score is 64 points), while the Activities-specific Balance Confidence (ABC) is a 16-item questionnaire used to rate individuals’ self-perceived balance confidence during various activities of daily living (100 points meaning complete confidence) (14–16).
Alterations of tactile and proprioceptive sensation, passive joint motion, and joint pain in the lower extremities were assessed using several items from the Fugl–Meyer Assessment for Lower Limb (mFM-LL) to use a reproducible and known assessment procedure. We selected these domains since they are useful for evaluating lower limb impairments not rated by functional tests (17). Scores for the sensation ranged from 0 to 10, scores of the passive joint motion ranged from 0 to 32, and finally, scores for the joint pain ranged from 0 to 20, with higher scores indicating lower levels of impairment. The sum of the scores of the three domains was calculated to provide a summary of sensory-motor impairments. Both lower limbs were assessed, but only the score from the most affected limb was considered for this study.
Finally, we used the modified Barthel index (mBI) to quantify functional independence (100 points meaning complete independence) and the Mini-Mental State Examination (MMSE) to assess cognitive functions (best score of 30 points) (18, 19). The Motivational Index (MI) was used to investigate participants’ motivation and engagement within the rehabilitation process (score from 7 to 35 points) (20).
Physiotherapist treatment report form
Through a treatment report form, we asked physiotherapists to identify the number of PT sessions provided, the approach used (by checkbox), and the treatments used during the PT program (see Supplementary Figure 2). The physiotherapists involved had to define the approach used during the rehabilitation program (restorative or compensatory) based on the purpose of the intervention provided, i.e., improving walking function. The definitions of restorative and compensatory approaches were provided to the physiotherapists. Restorative approach was defined as rehabilitation aimed at restoring premorbid walking patterns, while compensatory approach was defined as rehabilitation aimed at promoting new motor patterns to walk (4).
Statistical analysis
Each PwND was categorized as receiving a restorative or compensatory approach according to the physiotherapist’s classification. Then, the sample of PwNDs was split into two subgroups, one treated with a restorative approach and the other with a compensatory approach. Descriptive statistics consisted of group means and standard deviations of demographics and clinical outcomes.
Bivariate and multivariate logistic regression models were conducted using the approach (compensatory = 0; restorative = 1) as dependent variable and clinical measures as independent variables. All variables were used as predictors of the approach except for sex, which was considered a confounder. A bivariate analysis was performed using one independent predictor at a time. To improve stability and control for variance inflation, determinants were removed if collinearity was of concern in a model without interactions (variance inflation factor (VIF) > 5). All variables showing at least a weak association with the dependent variable (p < 0.1) were entered into a multivariate model. Since the interaction between variables measuring impairment and independence in activities of daily living was associated with the dependent variable, it was also included in the subsequent analyses. Finally, a backward stepwise logistic regression was used to identify the most parsimonious model using the stepAIC procedure from the MASS R library. Plots of residuals were used to check for the homogeneity of variance, and qq plots were used to check for normality of distributions of residuals, while Cook’s distance provided an indication of the presence of influential observations.
To verify the consistency of results, we carried out a sensitivity analysis running the same model on a subpopulation of people after stroke in the subacute phase only (onset<180 days), which was the largest subsample in our study.
To check the association between approaches and treatments provided during rehabilitation, we used contingency tables and an overall chi-squared test, removing treatments with less than 10 occurrences.
A significance level of p < 0.05 was set for all tests, and missing data were not imputed. All analyses were performed using R Statistical Software version 4.2.2 (R Core Team 2022).
Results
Participants characteristics
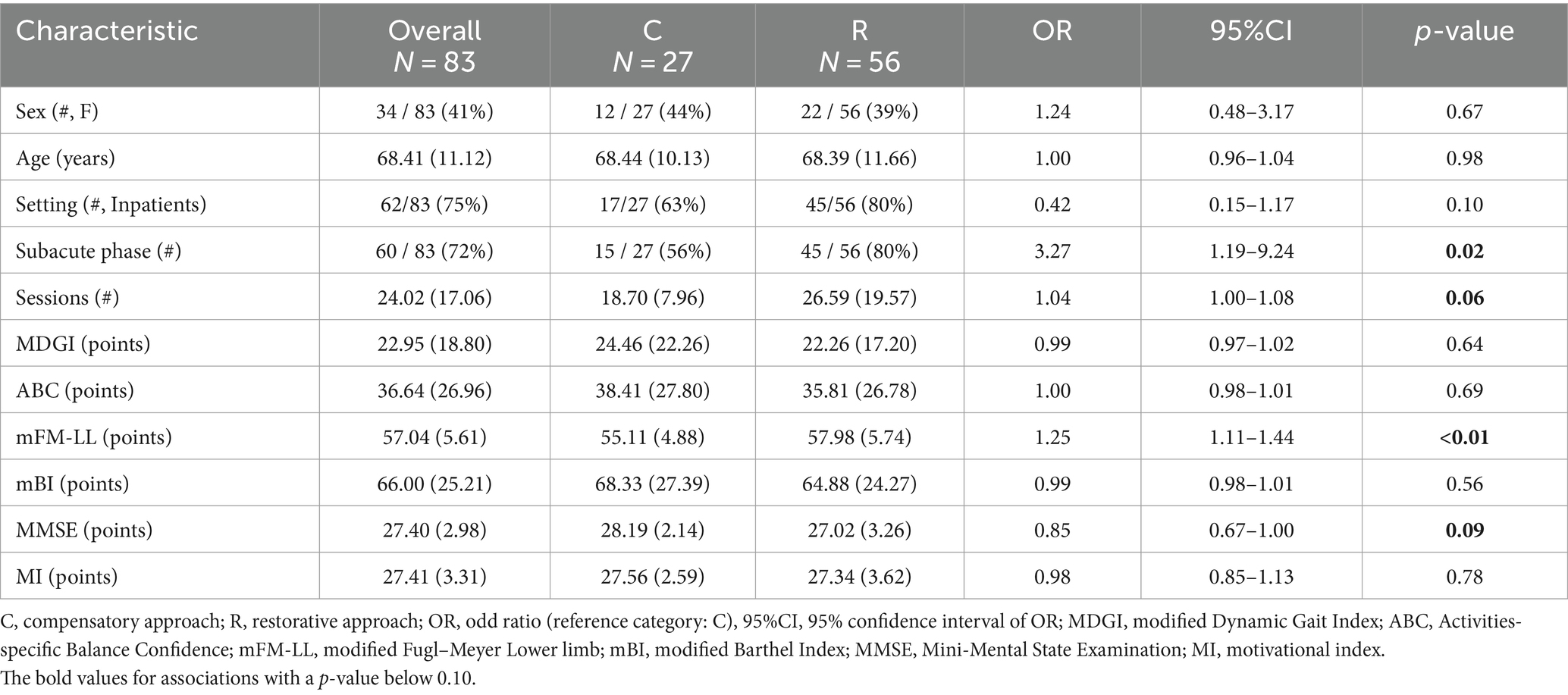
Data from 83 participants (65 people after stroke, 5 people with MS, and 13 people with PD) were analyzed, and demographic and clinical characteristics for the restorative and compensatory groups are shown in Table 1. A total of 43 physiotherapists were involved and completed the treatment form.
Factors identification
Whole sample
The univariate analyses revealed that subacute phase ((OR[95%CI] 3.28[1.19–9.24]), mFM-LL (1.25[1.11–1.44]), and MMSE 0.85[0.67–1.00]), and number of available sessions (1.04[1.00–1.08]) were associated with the restorative approach. These relationships are depicted in Supplementary Figure 3. Furthermore, the interaction between impairment and independence was also statistically associated with the restorative approach (0.99[0.98–1.00]).
Based on the results of the bivariate logistic regression analyses (see Table 1 and Supplementary Figure 3), we included five independent variables in the multivariate model: onset, mFM-LL, mBI, MMSE, and the number of sessions, along with the interaction between mFM-LL and mBI. The stepwise multivariate logistic regression result is presented in Table 2, with the associations represented in Figure 1.
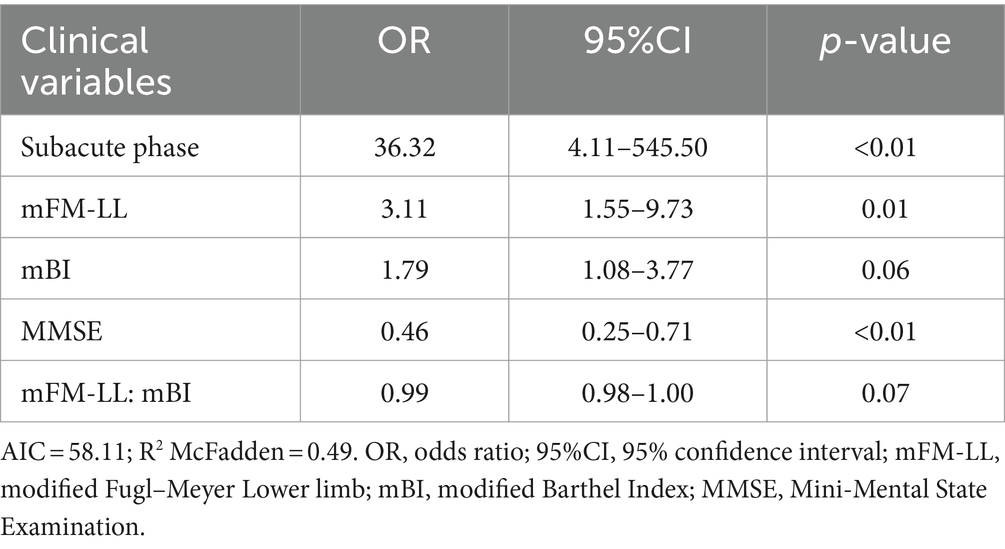
Table 2. Stepwise logistic regression model including best clinical predictors of restorative or compensatory approach.

Figure 1. Probability of having a restorative approach based on stepwise logistic regression analyses. MMSE, Mini-Mental State Examination; mFM-LL, modified Fugl–Meyer Lower limb; mBI, modified Barthel Index.
Being a subject after stroke during the subacute phase (onset <180 days), not severely impaired, and independent in daily life activities were associated with a higher probability of receiving a restorative rehabilitation approach. Cognitive status was significantly associated with a restorative approach, with more impaired subjects having a higher probability of receiving a restorative approach. In addition, the lower panel of Figure 1 shows the interaction between impairment and independence, where the probability of receiving a compensatory approach is high only in dependent participants (lower mBI scores) showing high levels of sensory-motor impairments (lower mFM-LL scores).
Subacute sample
We performed a stepwise multivariate logistic regression (Table 3) exclusively on the subacute population (onset<180 days). The multivariate model included independent variables associated with the restorative approach in the univariate analyses.
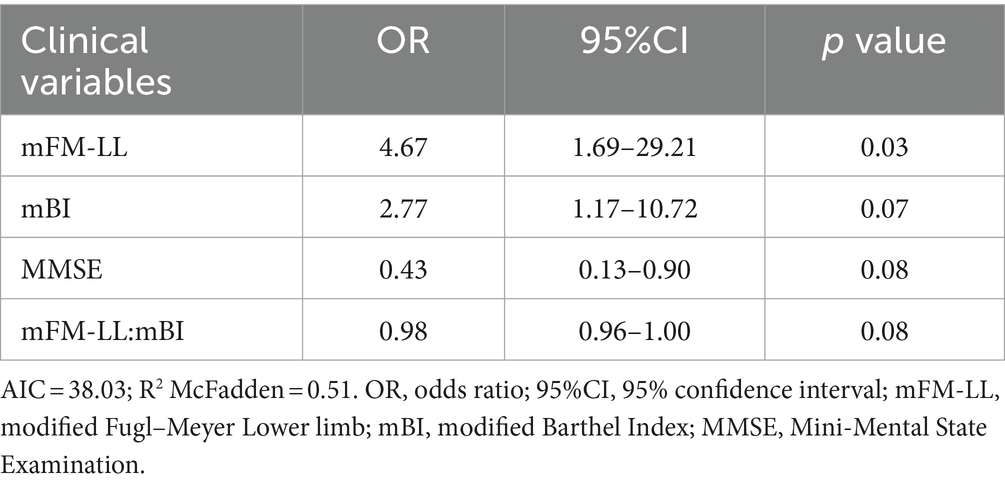
Table 3. Stepwise logistic regression model including best clinical predictors of restorative or compensatory approach on the subacute population.
As expected, the p-value increased due to the reduction in sample size. However, lower limb sensory-motor impairment was significantly associated with a higher probability of receiving the restorative approach, and the other predictors were close to statistical significance.
Contents of different rehabilitation approaches
Walking training, balance training, and proprioceptive exercises were the most prevalent treatments to improve walking in PwNDs (Supplementary Figure 4). Figure 2 shows the percentages of treatment used for restorative or compensatory approaches. Despite the differences observed across interventions, no statistically significant association between approach and treatment was found using the chi-square test (p = 0.46).
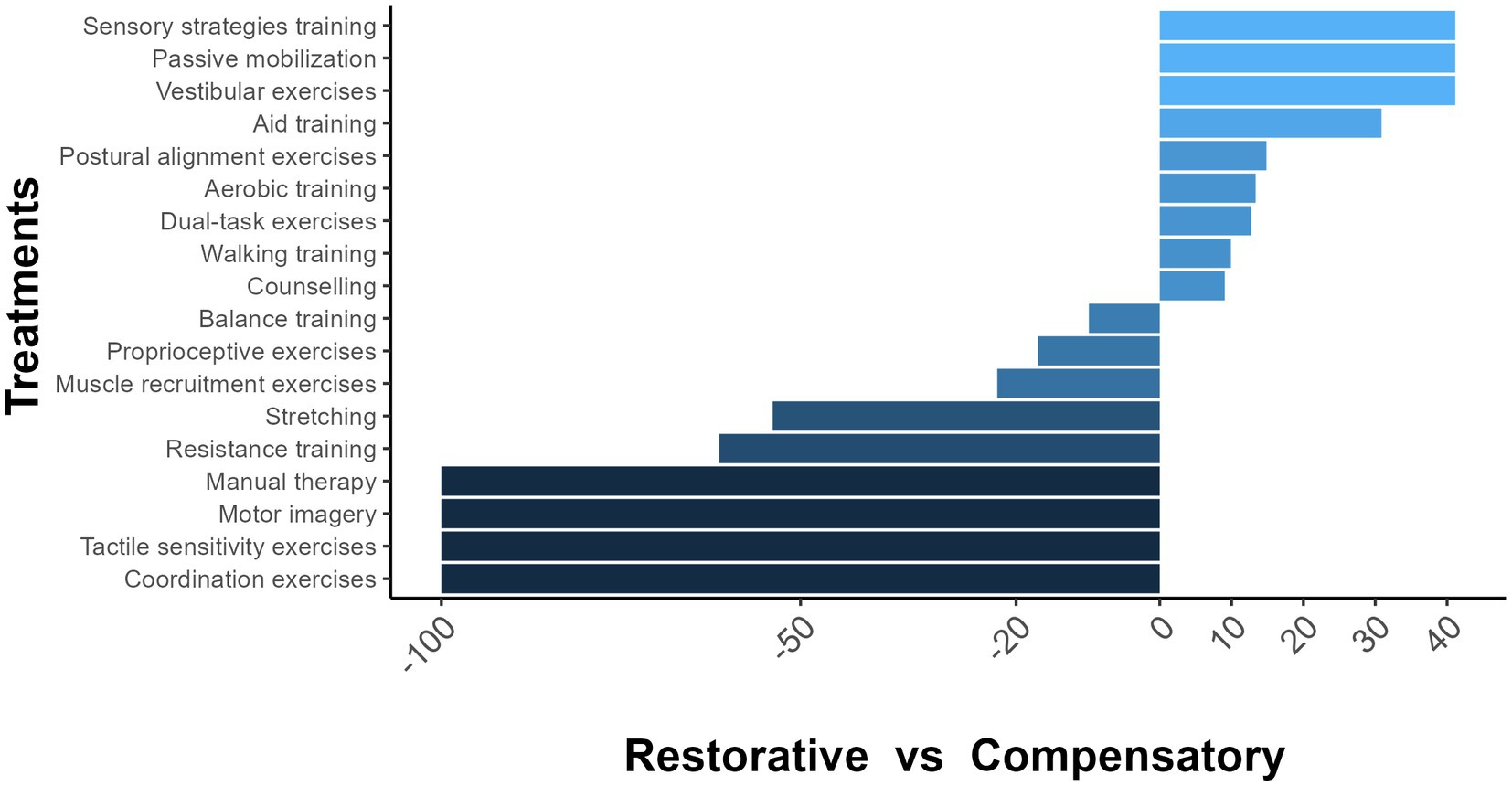
Figure 2. Percentages of treatment used in restorative and compensatory rehabilitation approaches. −100 = The treatment was administered for the restorative approach only. 100 = The treatment was administered for the compensatory approach only. 0 = The treatment was administered for both approaches.
Discussion
This unique observational study investigated the factors associated with the selection of restorative or compensatory approaches in PT clinical practice. We identified four main variables associated with the restorative rehabilitation approach: being in the subacute phase of the disease, having a low level of impairment at baseline with a high level of functional independence, and having lower cognitive performance.
The physiotherapists interviewed were all able to define their intervention as restorative or compensatory, indicating that the PT theoretical frameworks are well recognized by clinicians (4, 21). Both approaches were used to treat PwNDs, but the restorative approach was used more often than the compensatory approach in everyday clinical practice.
Our results suggest that specific clinical characteristics are associated with physiotherapists’ choice of approach. The factor that was most strongly associated with the restorative approach was the onset, with subacute subjects being 36 times more likely to receive restorative rehabilitation compared to chronic ones. The findings of this study support the a priori hypothesis that a physiotherapist’s decision-making process was influenced by the expectation of a good clinical outcome, and thus a restorative approach was more likely chosen.
Spontaneous neurological recovery is by far the largest contributor to behavioral restitution, and it is known that this phenomenon occurs during the first few weeks after stroke (subacute phase) (22, 23). Similarly, severe impairment was positively associated with worse clinical outcomes in longitudinal studies predicting walking recovery, and this association was also present when considering independence (mBI). Interestingly, we found a complex interaction between impairment and functional impendence. Severely impaired subjects were likely treated with a compensatory approach unless their independence level was high.
In other studies, preserved cognitive status was a predictor of good clinical outcome, which contrasts with our findings (24, 25). However, our results should be treated with caution, as the mean MMSE score was close to the highest score on the scale, meaning that the cognitive impairments measured by this test were rare in our sample. The MMSE has been widely used as a screening tool for dementia, but it has been criticized for not being sensitive enough to cognitive impairments specific to these populations, suggesting that other validated tests should be used in this population (26–28). Moreover, average MMSE scores were similar for subjects treated with a restorative and compensatory approach, and the association found between MMSE scores and the restorative approach was unexpected.
In contrast with our hypothesis, other variables associated with good clinical outcomes were not associated with the restorative approach. We anticipated that the age of individuals with PwNDs would influence the physiotherapist approach, with older subjects more likely to receive the compensatory approach. This expectation is based on previous reports indicating that older age is associated with poorer rehabilitation outcomes in individuals after stroke and in those with PD (13, 29). Similarly, balance performance and subjects’ motivation for PT were not considered in the choice of rehabilitation approach, although both factors have been shown to be associated with functional outcomes at the end of rehabilitation (9, 11, 12, 30).
In addition, we expected that a greater number of available sessions would influence the physiotherapist’s decision to select a restorative approach, as the time spent in rehabilitation should result in an increased therapy dosage (31, 32). The lack of association between the number of sessions and the restorative approach may be due to a lack of strong evidence supporting a dose–response effect in PwNDs (33–35).
Walking training, balance training, and proprioceptive exercises were frequently used to improve walking function in accordance with international guidelines for stroke, MS, and PD (35–37). It should be noted that a comprehensive data collection on the content of gait rehabilitation was beyond the scope of this study, as this topic has been investigated elsewhere (3). The treatments described in this study are limited to the everyday clinical practice of the participating rehabilitation centers. Other common PT approaches, such as dance or aqua therapy (38, 39), were not investigated.
Our findings indicated that certain interventions were exclusive to the restorative approach, such as manual therapy and motor imagery. However, most treatments used were similar for both approaches, resulting in a non-statistically significant difference. A more detailed description of the PT treatments is needed to understand the specifics between the restorative and compensatory approaches.
The study has certain limitations. The definitions of compensation and restitution in PwNDs, by Levin et al. (4), were used in this investigation. However, different interpretations of these concepts among physiotherapists represent a potential for subjective bias in their responses. Furthermore, we asked physiotherapists to classify their interventions on PwNDs at the conclusion of the PT program. Some interventions may have started with a restorative approach and then shifted to a compensatory approach or vice versa from session to session, depending on the needs of PwNDs. It was not possible to collect this type of information using our physiotherapist treatment report form.
No information was collected on the composition of the multidisciplinary rehabilitation team.
Finally, we did not consider other variables that have already been identified as predictors of good rehabilitation outcomes, such as the early presence of lower limb spasticity and muscle strength (40) or disease severity (12, 13, 41).
Conclusion
In this sample, a restorative approach was often used in neurological rehabilitation. The main factor that influenced the choice of a restorative approach was predicted clinical improvement.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of the Don Gnocchi Foundation. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
FMes: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Writing – original draft, Writing – review & editing. TB: Data curation, Formal analysis, Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing. FMar: Data curation, Investigation, Methodology, Writing – original draft, Writing – review & editing. SS: Data curation, Investigation, Writing – original draft, Writing – review & editing. CA: Data curation, Investigation, Writing – original draft, Writing – review & editing. SB: Data curation, Investigation, Writing – original draft, Writing – review & editing. VB: Data curation, Investigation, Writing – original draft, Writing – review & editing. FMat: Data curation, Investigation, Writing – original draft, Writing – review & editing. EP: Data curation, Investigation, Writing – original draft, Writing – review & editing. MP: Data curation, Investigation, Writing – original draft, Writing – review & editing. AT: Data curation, Investigation, Methodology, Writing – original draft, Writing – review & editing. SM: Funding acquisition, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing. DC: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Italian Association of Physiotherapy (Associazione Italiana Fisioterapia – AIFI) and was also supported and funded by the Italian Ministry of Health – Ricerca Corrente 2021.
Acknowledgments
The authors thank Cristina Simionato, Carolina Colombo, Gloria Garavaglia, Marco Della Gaspera, Valeria Boz, Marta Bianchessi, Michele Gennuso, and Sara Bartolucci for providing support during data collection. The authors are also grateful to Kevin Bateman for proofreading the final version of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2024.1368973/full#supplementary-material
References
1. Shah, VV, McNames, J, Mancini, M, Carlson-Kuhta, P, Spain, RI, Nutt, JG, et al. Laboratory versus daily life gait characteristics in patients with multiple sclerosis, Parkinson’s disease, and matched controls. J Neuroeng Rehabil. (2020) 17:159. doi: 10.1186/s12984-020-00781-4
2. Louie, DR, Simpson, LA, Ben, MW, Field, TS, Yao, J, and Eng, JJ. Prevalence of walking limitation after acute stroke and its impact on discharge to home. Phys Ther. (2022) 102:pzab246. doi: 10.1093/ptj/pzab246
3. Bowman, T, Mestanza Mattos, FG, Salvalaggio, S, Marazzini, F, Allera Longo, C, Bocini, S, et al. Classification and quantification of physical therapy interventions across multiple neurological disorders: an Italian multicenter network. J Clin Med. (2023) 12:6483. doi: 10.3390/jcm12206483
4. Levin, MF, Kleim, JA, and Wolf, SL. What do Motor “recovery” and “compensation” mean in patients following stroke? Neurorehabil Neural Repair. (2009) 23:313–9. doi: 10.1177/1545968308328727
5. Krakauer, JW, and Carmichael, ST. Broken movement: the neurobiology of motor recovery after stroke. Cambridge (Massachusetts): The MIT Press. (2017):171–172.
6. Edwards, I, Jones, M, Carr, J, Braunack-Mayer, A, and Jensen, GM. Clinical reasoning strategies in physical therapy. Phys Ther. (2004) 84:312–30; discussion 331–5. doi: 10.1093/ptj/84.4.312
7. Duong, QH, Pham, TN, Reynolds, L, Yeap, Y, Walker, S, and Lyons, K. A scoping review of therapeutic reasoning process research. Adv Health Sci Educ Theory Pract. (2023) 28:1289–310. doi: 10.1007/s10459-022-10187-7
8. Kwah, L, and Herbert, R. Prediction of walking and arm recovery after stroke: a critical review. Brain Sci. (2016) 6:53. doi: 10.3390/brainsci6040053
9. Harvey, RL. Predictors of functional outcome following stroke. Phys Med Rehabil Clin N Am. (2015) 26:583–98. doi: 10.1016/j.pmr.2015.07.002
10. Groppo, E, Signori, A, Sormani, MP, Grosso, C, Mantia, LL, Cattaneo, D, et al. Predictors of hospital-based multidisciplinary rehabilitation effects in persons with multiple sclerosis: a large-scale, single-Centre study. Mult Scler J Exp Transl Clin. (2019) 5:205521731984367. doi: 10.1177/2055217319843673
11. Cattaneo, D, Coote, S, Rasova, K, Gervasoni, E, Groppo, E, Prokopiusova, T, et al. Factors influencing balance improvement in multiple sclerosis rehabilitation: a pragmatic multicentric trial. Ann Phys Rehabil Med. (2020) 63:93–8. doi: 10.1016/j.rehab.2019.05.007
12. Liberatore, G, Clarelli, F, Nuara, A, Ungaro, D, Gatti, R, Rovaris, M, et al. Predictors of effectiveness of multidisciplinary rehabilitation treatment on motor dysfunction in multiple sclerosis. Mult Scler J. (2014) 20:862–70. doi: 10.1177/1352458513508834
13. Combs-Miller, SA, and Moore, ES. Predictors of outcomes in exercisers with Parkinson disease: a two-year longitudinal cohort study. NeuroRehabilitation. (2019) 44:425–32. doi: 10.3233/NRE-182641
14. Nilsagård, Y, Carling, A, and Forsberg, A. Activities-specific balance confidence in people with multiple sclerosis. Mult Scler Int. (2012) 2012:1–8. doi: 10.1155/2012/613925
15. Botner, EM, Miller, WC, and Eng, JJ. Measurement properties of the activities-specific balance confidence scale among individuals with stroke. Disabil Rehabil. (2005) 27:156–63. doi: 10.1080/09638280400008982
16. Franchignoni, F, Giordano, A, Ronconi, G, Rabini, A, and Ferriero, G. Rasch validation of the activities-specific balance confidence scale and its short versions in patients with Parkinson’s disease. J Rehabil Med. (2014) 46:532–9. doi: 10.2340/16501977-1808
17. Fugl-Meyer, AR, Jaasko, L, Leyman, I, Olsson, S, and Steglind, S. The post-stroke hemiplegic patient. 1. A method for evaluation of physical performance. Scand J Rehabil Med. (1975) 7:13–31.
18. Shah, S, Vanclay, F, and Cooper, B. Improving the sensitivity of the Barthel index for stroke rehabilitation. J Clin Epidemiol. (1989) 42:703–9. doi: 10.1016/0895-4356(89)90065-6
19. Folstein, MF, Folstein, SE, and McHugh, PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. (1975) 12:189–98. doi: 10.1016/0022-3956(75)90026-6
20. White, GN, Cordato, D, O'Rourke, F, and Mendis, RL. Validation of the stroke rehabilitation motivation scale: a pilot study. Asian J Gerontol Geriatr. (2012) 7:80–7.
21. Hughes, S, Murray, CM, McMullen-Roach, S, and Berndt, A. A profile of practice: the occupational therapy process in community aged care in Australia. Aust Occup Ther J. (2023) 70:366–79. doi: 10.1111/1440-1630.12860
22. Swayne, OBC, Rothwell, JC, Ward, NS, and Greenwood, RJ. Stages of motor output reorganization after hemispheric stroke suggested by longitudinal studies of cortical physiology. Cereb Cortex. (2008) 18:1909–22. doi: 10.1093/cercor/bhm218
23. Feigin, V, Norrving, B, Sudlow, CLM, and Sacco, RL. Updated criteria for population-based stroke and transient ischemic attack incidence studies for the 21st century. Stroke. (2018) 49:2248–55. doi: 10.1161/STROKEAHA.118.022161
24. Wang, YH, Yang, YR, Pan, PJ, and Wang, RY. Modeling factors predictive of functional improvement following acute stroke. J Chin Med Assoc. (2014) 77:469–76. doi: 10.1016/j.jcma.2014.03.006
25. Ginex, V, Vanacore, N, Lacorte, E, Sozzi, M, Pisani, L, Corbo, M, et al. General cognition predicts post-stroke recovery defined through minimal clinically important difference (MCID): a cohort study in an Italian rehabilitation clinic. Eur J Phys Rehabil Med. (2015) 51:597–606.
26. Ciesielska, N, Sokołowski, R, Mazur, E, Podhorecka, M, Polak-Szabela, A, and Kędziora-Kornatowska, K. Is the Montreal Cognitive Assessment (MoCA) test better suited than the Mini-Mental State Examination (MMSE) in mild cognitive impairment (MCI) detection among people aged over 60? Meta-analysis. Psychiatr Pol. (2016) 50:1039–52. doi: 10.12740/PP/45368
27. Suda, S, Muraga, K, Ishiwata, A, Nishimura, T, Aoki, J, Kanamaru, T, et al. Early cognitive assessment following acute stroke: feasibility and comparison between mini-mental state examination and Montreal cognitive assessment. J Stroke Cerebrovasc Dis. (2020) 29:104688. doi: 10.1016/j.jstrokecerebrovasdis.2020.104688
28. Freitas, S, Batista, S, Afonso, AC, Simões, MR, de Sousa, L, Cunha, L, et al. The Montreal cognitive assessment (MoCA) as a screening test for cognitive dysfunction in multiple sclerosis. Appl Neuropsychol Adult. (2018) 25:57–70. doi: 10.1080/23279095.2016.1243108
29. Pellicciari, L, Sodero, A, Campagnini, S, Guolo, E, Basagni, B, Castagnoli, C, et al. Factors influencing trunk control recovery after intensive rehabilitation in post-stroke patients: a multicentre prospective study. Top Stroke Rehabil. (2023) 30:109–18. doi: 10.1080/10749357.2021.2016099
30. Rapolienė, J, Endzelytė, E, Jasevičienė, I, and Savickas, R. Stroke patients motivation influence on the effectiveness of occupational therapy. Rehabil Res Pract. (2018) 2018:1–7. doi: 10.1155/2018/9367942
31. Clark, B, Whitall, J, Kwakkel, G, Mehrholz, J, Ewings, S, and Burridge, J. The effect of time spent in rehabilitation on activity limitation and impairment after stroke. Cochrane Database Syst Rev. (2021) 2021:CD012612. doi: 10.1002/14651858.CD012612.pub2
32. Boyne, P, Billinger, SA, Reisman, DS, Awosika, OO, Buckley, S, Burson, J, et al. Optimal intensity and duration of walking rehabilitation in patients with chronic stroke. JAMA Neurol. (2023) 80:342–51. doi: 10.1001/jamaneurol.2023.0033
33. Lang, CE, Lohse, KR, and Birkenmeier, RL. Dose and timing in neurorehabilitation. Curr Opin Neurol. (2015) 28:549–55. doi: 10.1097/WCO.0000000000000256
34. Corrini, C, Gervasoni, E, Perini, G, Cosentino, C, Putzolu, M, Montesano, A, et al. Mobility and balance rehabilitation in multiple sclerosis: a systematic review and dose-response meta-analysis. Mult Scler Relat Disord. (2023) 69:104424. doi: 10.1016/j.msard.2022.104424
35. Ni, M, Hazzard, JB, Signorile, JF, and Luca, C. Exercise guidelines for gait function in Parkinson’s disease: a systematic review and meta-analysis. Neurorehabil Neural Repair. (2018) 32:872–86. doi: 10.1177/1545968318801558
36. Henze, T. Recommendation on rehabilitation services for persons with multipe sclerosis in Europe. (2012). Available at: https://www.eurims.org/News/recommendations-on-rehabilitation-services-for-persons-with-multiple-sclerosis-in-europe.html.
37. Teasell, R, Salbach, NM, Foley, N, Mountain, A, Cameron, JI, Jong,, et al. Canadian stroke best practice recommendations: rehabilitation, recovery, and community participation following stroke. Part one: rehabilitation and recovery following stroke; 6th edition update 2019. Int J Stroke (2020);15:763–788. doi: 10.1177/1747493019897843
38. Carroll, LM, MegE, M, O’Connor, WT, Volpe, D, Salsberg, J, and Clifford, AM. Evidence-based aquatic therapy guidelines for Parkinson’s disease: an international consensus study. J Parkinsons Dis. (2022) 12:621–37. doi: 10.3233/JPD-212881
39. Emmanouilidis, S, Hackney, ME, Slade, SC, Heng, H, Jazayeri, D, and Morris, ME. Dance is an accessible physical activity for people with Parkinson’s disease. Parkinsons Dis. (2021) 2021:1–20. doi: 10.1155/2021/7516504
40. Veerbeek, JM, Van Wegen, EEH, Harmeling-Van der Wel, BC, and Kwakkel, G. Is accurate prediction of gait in nonambulatory stroke patients possible within 72 hours poststroke? Neurorehabil Neural Repair. (2011) 25:268–74. doi: 10.1177/1545968310384271
Keywords: neurological rehabilitation, physical therapy modalities, stroke, multiple sclerosis, Parkinson’s disease
Citation: Mestanza Mattos FG, Bowman T, Marazzini F, Salvalaggio S, Allera Longo C, Bocini S, Bonci V, Materazzi FG, Pelosin E, Putzolu M, Turolla A, Mezzarobba S and Cattaneo D (2024) Factors influencing physiotherapy decisions between restorative and compensatory gait rehabilitation: an Italian multicenter study. Front. Neurol. 15:1368973. doi: 10.3389/fneur.2024.1368973
Edited by:
Meg E. Morris, La Trobe University, AustraliaReviewed by:
Louise Carroll, Health Services Executive Ireland, IrelandPerin Cecilia, University of Milano-Bicocca, Italy
Copyright © 2024 Mestanza Mattos, Bowman, Marazzini, Salvalaggio, Allera Longo, Bocini, Bonci, Materazzi, Pelosin, Putzolu, Turolla, Mezzarobba and Cattaneo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fabiola G. Mestanza Mattos, ZmFiaW9sYS5tZXN0YW56YUB1bmltaS5pdA==
†These authors have contributed equally to this work
 Fabiola G. Mestanza Mattos
Fabiola G. Mestanza Mattos Thomas Bowman2†
Thomas Bowman2† Silvia Salvalaggio
Silvia Salvalaggio Viviana Bonci
Viviana Bonci Elisa Pelosin
Elisa Pelosin Martina Putzolu
Martina Putzolu Andrea Turolla
Andrea Turolla Susanna Mezzarobba
Susanna Mezzarobba