- 1Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Jinan, Shandong, China
- 2School of Acupuncture-Moxibustion and Tuina, Shandong University of Traditional Chinese Medicine, Jinan, Shandong, China
- 3Research Institute of Acupuncture and Moxibustion, Shandong University of Traditional Chinese Medicine, Jinan, Shandong, China
Objective: This study aims to evaluate the efficacy and safety of various acupuncture treatments in conjunction with multimodal analgesia (MA) for managing postoperative pain and improving knee function in patients undergoing total knee arthroplasty (TKA), based on the findings from clinical research indicating the potential benefits of acupuncture-related therapies in this context.
Methods: We searched Web of Science, PubMed, SCI-hub, Embase, Cochrane Library, China Biology Medicine (CBM), China National Knowledge Infrastructure (CNKI), Wanfang Data, and Chinese Scientific Journal Database (VIP) to collect randomized controlled trials of acupuncture-related therapies for post-TKA pain. After independent screening and data extraction, the quality of the included literature was evaluated. The potential for bias in the studies incorporated in the analysis was assessed according to the guidelines outlined in the Cochrane Handbook 5.1. Network meta-analysis (NMA) was conducted using RevMan 5.4 and Stata 16.0 software, with primary outcome measures including visual analog scale (VAS), pain pressure threshold (PPT), hospital for special surgery knee score (HSS), and knee joint range of motion (ROM). Furthermore, the interventions were ranked based on the SUCRA value.
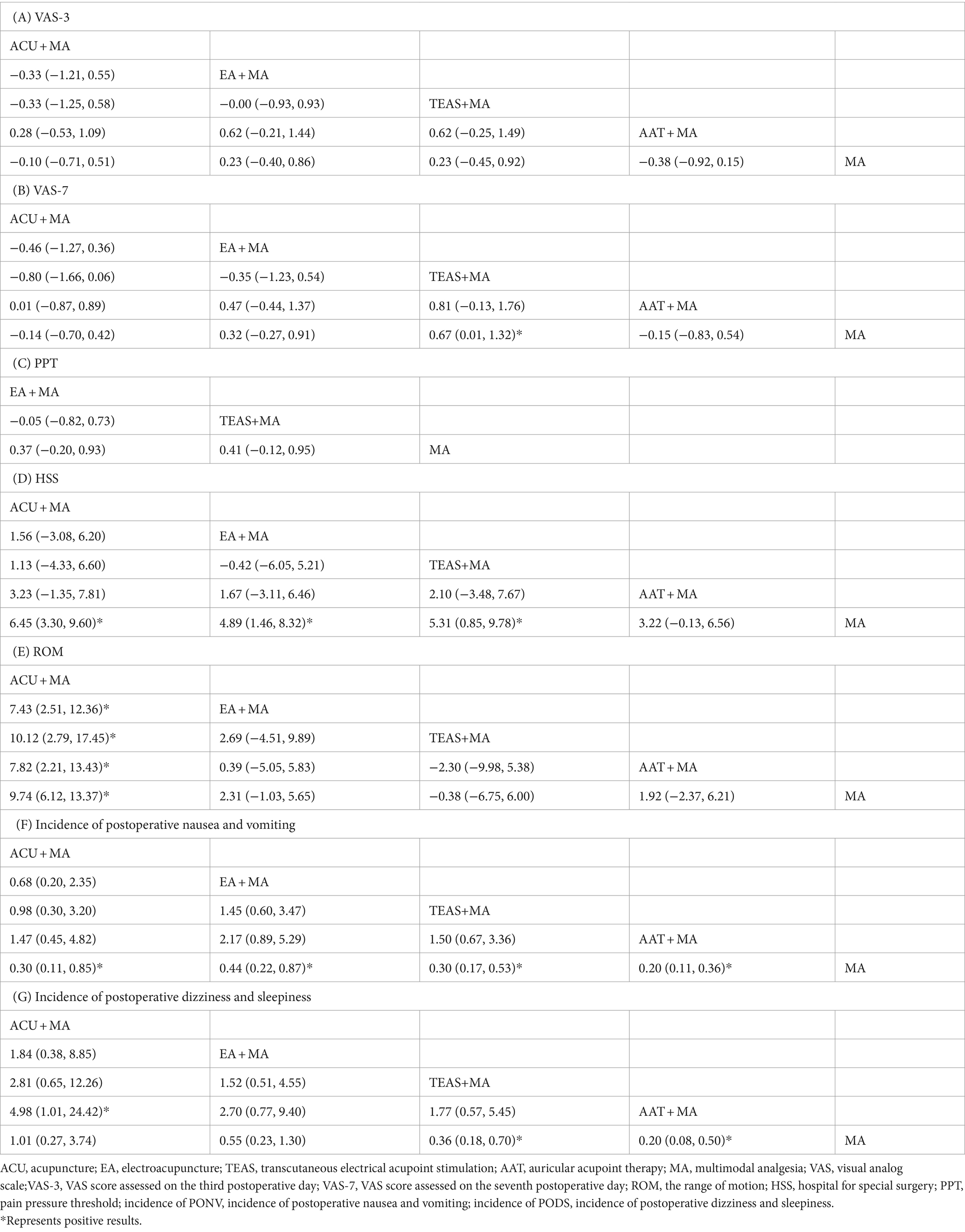
Results: We conducted an analysis of 41 qualifying studies encompassing 3,003 patients, examining the efficacy of four acupuncture therapies (acupuncture ACU, electroacupuncture EA, transcutaneous electrical acupoint stimulation TEAS, and auricular acupoint therapy AAT) in conjunction with multimodal analgesia (MA) and MA alone. The VAS results showed no significant difference in efficacy among the five interventions for VAS-3 score. However, TEAS+MA (SMD: 0.67; 95%CI: 0.01, 1.32) was more effective than MA alone for VAS-7 score. There was no significant difference in PPT score among the three interventions. ACU + MA (SMD: 6.45; 95%CI: 3.30, 9.60), EA + MA (SMD: 4.89; 95%CI: 1.46, 8.32), and TEAS+MA (SMD: 5.31; 95%CI: 0.85, 9.78) were found to be more effective than MA alone for HSS score. For ROM score, ACU + MA was more efficacious than EA + MA, TEAS+MA, and AAT + MA, MA. Regarding the incidence of postoperative adverse reactions, nausea and vomiting were more prevalent after using only MA. Additionally, the incidence of postoperative dizziness and drowsiness following ACU + MA (OR = 4.98; 95%CI: 1.01, 24.42) was observed to be higher compared to that after AAT + MA intervention. Similarly, the occurrence of dizziness and drowsiness after MA was found to be significantly higher compared to the following interventions: TEAS+MA (OR = 0.36; 95%CI: 0.18, 0.70) and AAT + MA (OR = 0.20; 95%CI: 0.08, 0.50). The SUCRA ranking indicated that ACU + MA, EA + MA, TEAS+MA, and AAT + MA displayed superior SUCRA scores for each outcome index, respectively.
Conclusion: For the clinical treatment of post-TKA pain, acupuncture-related therapies can be selected as a complementary and alternative therapy. EA + MA and TEAS+MA demonstrate superior efficacy in alleviating postoperative pain among TKA patients. ACU + MA is the optimal choice for promoting postoperative knee joint function recovery in TKA patients. AAT + MA is recommended for preventing postoperative adverse reactions.
Systematic review registration: https://www.crd.york.ac.uk/, identifier (CRD42023492859).
1 Background
The incidence of knee osteoarthritis (KOA) has significantly risen due to the acceleration of population aging and the increasing prevalence of obesity and overweight individuals. Data from the China Health and Retirement Longitudinal Study (CHARLS) database indicate that symptomatic knee osteoarthritis now affects 13.7 and 10.8% of individuals in southwest and northwest China, respectively (1). TKA, a well-established and effective reconstructive treatment, has demonstrated long-term efficacy in managing severe multi-compartmental knee osteoarthritis with deformity. When compared to basic treatment, pharmacological intervention, and reparative approaches for KOA, TKA demonstrates significant improvements in pain relief and joint function (2), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores, hospital for special surgery knee score (HSS), and overall quality of life during long-term follow-up.
The presence of pain after TKA is a significant factor that affects the outcomes of patient rehabilitation. According to the International Association for the Study of Pain (IASP) (3), pain is defined as an unpleasant sensory and emotional experience that is linked to actual or potential tissue damage and is influenced by biological, psychological, and social factors to varying extents. Pain can easily result in the development of depression, anger, and anxiety, which is why it is considered as the fifth vital sign (4). In contrast to total hip arthroplasty, it is imperative to incorporate high-intensity knee flexion and extension training after TKA to enhance functional activity and prevent complications such as postoperative knee stiffness. However, it is important to note that early functional exercise may potentially worsen postoperative pain. The relationship between postoperative pain and knee joint rehabilitation is reciprocal (5). The implementation of enhanced recovery after surgery (ERAS) in perioperative management has made it essential to effectively manage postoperative pain and knee swelling as an integral aspect of early rehabilitation (6).
Previous research has established that high levels of sedentary behavior put people with musculoskeletal conditions (such as osteoarthritis) at elevated risk for reduced physical function, increased physical frailty and blood pressure, and may increase mortality (7). However, physical activity provides a multitude of health advantages, encompassing the prevention and management of various ailments, such as hypertension, stroke, obesity, diabetes, and mental health disorders, such as anxiety and depression (8). Consequently, the World Health Organization has initiated the Global Action Plan on Physical Activity 2018–2030, with the objective of augmenting physical activity levels by 15% before 2030 (9). Regrettably, a concerning observation is that individuals undergoing total knee arthroplasty (TKA) often exhibit limited engagement in physical activity post-surgery (10), primarily due to their obesity that was present preoperatively. Merely, 5% of TKA patients adhere to national physical activity guidelines (11), which put them at increased risk of cardiovascular disease and cancer (12). The studies (13) have demonstrated that augmenting physical activity can effectively enhance gait function following TKA, with a realistic and appropriate target of approximately 3,000 steps per day for postoperative TKA patients. This suggests the attainability of heightened postoperative gait function. Additionally, another study (14) has revealed that initiating ambulation and engaging in 15–30 min of walking twice daily, commencing on the initial day after surgery, can significantly diminish the occurrence of thromboembolic complications subsequent to TKA. Consequently, it is imperative to augment physical activity following TKA.
The implementation of multimodal analgesia in the perioperative pain management of TKA has gradually gained traction (15). Within the ERAS framework, multimodal analgesia not only plays a central role but also demonstrates a strong interconnection with other rehabilitation measures. The primary goal of perioperative pain management has evolved beyond solely providing pain relief to encompass facilitating the prompt recovery of patients as a whole (16). Moreover, when incorporating multimodal analgesia, careful attention must be paid to its effects on the entire ERAS system (17). Multimodal analgesia encompasses a range of interventions, both non-pharmacological and pharmacological, that aim to manage pain. Non-pharmacological interventions include acupuncture, moxibustion, massage, and psychological guidance. Pharmacological interventions involve the use of various drugs and delivery routes, such as traditional Chinese medicine, patient-controlled analgesia (PCA), regional nerve block, intravenous/oral administration of non-steroidal anti-inflammatory drugs (NSAIDs) and opioids, as well as periarticular multimodal drug injection (PMI) (18).
The administration of femoral nerve block, iliac fascia nerve block, adductor canal block, and sciatic nerve block to alleviate postoperative pain in TKA patients may lead to varying degrees of muscle strength decline in the quadriceps femoris, biceps femoris, gastrocnemius (19), and other related muscles. This decline in muscle strength is not beneficial for the isometric contraction rehabilitation exercise of these muscles following TKA. In multimodal analgesia, analgesics are commonly administered in a stepwise manner. For the management of mild pain, oral non-steroidal anti-inflammatory drugs (NSAIDs) and weak opioids, such as celecoxib, flurbiprofen axetil, and nalbuphine (20), are commonly prescribed. On the other hand, for moderate-to-severe pain, strong opioids or narcotic analgesics, such as morphine, butorphanol, and fentanyl (21), are typically utilized. It is important to note that traditional NSAIDs function as non-selective inhibitors of both COX − 1 and COX-2 enzymes. However, the presence of COX − 1 in the stomach, kidney, and platelets can result in an increased risk of adverse reactions, including gastrointestinal damage and bleeding (22). Selective COX-2 inhibitors, in contrast, specifically target COX-2 activity while exerting minimal influence on COX − 1; however, apprehensions have arisen regarding their cardiovascular safety profile and nephrotoxicity. Similarly, opioids employed for the management of moderate-to-severe pain are accompanied by notable adverse effects such as nausea, vomiting, constipation, respiratory depression, and cognitive impairment (23). These untoward effects have the potential to protract hospitalization duration, escalate hospitalization expenses, and induce anxiety among patients.
In the context of TKA surgery, there exist two primary categories: those in which the posterior cruciate ligament (PCL) is preserved and those in which it is not. A randomized controlled study (24) was conducted to investigate the effects of PCL preservation on patients who received a prosthesis. The hypothesis was that by maintaining the PCL, mechanical stress would stimulate PCL proprioceptors, leading to the activation of nerve reflexes and subsequent tightening of relevant muscles and ligaments. However, due to the loss of normal function in most patients, the formation of nerve reflexes proved challenging. Conversely, the prosthesis that replaces the posterior cruciate ligament does not maintain the integrity of the ligament itself. Instead, it utilizes a post and cassette structure to facilitate the rolling back mechanism and enhance knee joint flexion. Comparisons between TKA procedures with and without preservation of the PCL revealed no significant differences in VAS pain scores and HSS scores. The potential retention of proprioceptive sensation during knee flexion in patients with preserved PCL prostheses warrants further investigation to determine its potential benefits for subsequent knee rehabilitation (25). Danilo De Oliveira Silva’s findings (26) indicate that most of the patients (85%) who had undergone TKA using a posterior-stabilized (PS) prosthesis with routine patellar resurfacing reported absence of anterior knee pain at 12 months following surgery. The study conducted by White et al. (27) revealed that undergoing TKA, the Attune PS prosthesis exhibited a significantly lower overall occurrence of anterior knee pain (AKP) and knee crepitation in comparison with the PFC Sigma prosthesis (12.5% vs. 25.8%, p < 0.05). The occurrence of painful tremor was lower in both groups (1.0% vs. 4.1%), with no statistically significant difference, and there were no significant disparities observed in the four postoperative indices, namely, the HSS score, WOMAC score, ROM, and patient satisfaction. Both prostheses are extensively utilized in clinical practice, and the prevalence of residual knee pain was minimal after a 2-year follow-up period. A group of 47 TKA prostheses applied to 39 patients (32 women) were analyzed retrospectively. All the prostheses had been implanted by the same team of orthopedic surgeons using the same surgical method (cemented, with patella prosthesis and posterior stabilization with the sacrifice of the posterior cruciate ligament). It was found that male sex were considered good outcome predictors, underlying the importance of considering sex in understanding postoperative pain course; meanwhile, old preoperative age was considered as unfavorable underlying (28).
Due to the limitations of pharmacological therapy, a number of patients have turned to acupuncture as a supplementary and alternative treatment. Traditional Chinese Medicine (TCM) analgesia holds a crucial position in clinical practice for managing perioperative pain and should not be disregarded. Extensive research has consistently focused on acupuncture analgesia, with multiple clinical studies documenting its effectiveness in alleviating postoperative pain following TKA (29). Clinical reports on the utilization of acupuncture anesthesia in thyroid surgery and thoracic surgery have been documented as early as the 1980s. By integrating traditional Chinese medicine’s meridian and acupoint theory with nerve electrical stimulation technology, electroacupuncture and transcutaneous electrical acupoint stimulation present notable alternative therapeutic options (30). These methods not only exhibit clinical effectiveness but also mitigate labor costs and technical challenges associated with acupuncture treatment, while concurrently minimizing adverse reactions such as needle bending, bleeding, and infection. Research studies have demonstrated that the integration of transcutaneous electrical acupoint stimulation and electroacupuncture in the perioperative management of patients undergoing total knee arthroplasty (TKA) effectively mitigates pain, diminishes limb edema, expedites recovery (31), and aligns with the principles of ERAS. This incorporation of acupuncture techniques broadens the scope of clinical applications and garners acceptance from a growing cohort of surgeons. The ear is intricately linked to the body’s meridians, and auricular therapy represents a unique modality within the realm of acupuncture and moxibustion. This therapy involves the stimulation of specific areas on the auricle, known as auricular points, through the application of acupuncture or other methods, with the aim of diagnosing and treating various diseases (32). Numerous clinical studies have demonstrated the effectiveness of auricular point therapy in alleviating conditions such as traumatic pain (33), headache (34), postoperative wound pain, and neuropathic pain (35).
The study of the analgesic properties of acupuncture serves as a connection between traditional Chinese medicine and modern Western medicine. Through fundamental research, new insights have been gained regarding the mechanisms underlying acupuncture-induced pain relief, including the involvement of peripheral purine signaling (36) and TRPV channels (37), which expand upon the established central opioid peptide analgesia paradigm (38). Simultaneously, acupuncture therapies have been shown to modulate pain sensation, emotion, and memory (39), thereby enhancing the understanding of its analgesic mechanisms. The field of acupuncture research has long grappled with the challenge of bridging the gap between basic research and clinical practice, but there is growing anticipation that the analgesic mechanisms of acupuncture therapy will be increasingly validated through clinical trials. The four commonly utilized acupuncture-related therapies in clinical practice are traditional acupuncture, electroacupuncture, transcutaneous electrical acupoint stimulation, and auricular point therapy. Previous studies on postoperative pain following total knee arthroplasty have primarily compared various acupuncture-related therapies collectively against other interventions, emphasizing pairwise comparisons. Despite the widespread utilization of acupuncture, the existing evidence on its efficacy appears to be inconclusive. Various studies have yielded divergent findings. One systematic review demonstrated that acupuncture may improve postoperative pain management after total knee arthroplasty (TKA) (40), while a clinical trial suggested that acupuncture was not superior to pharmacological treatments (41). This study employed a network meta-analysis (NMA) approach to evaluate and rank four distinct types of acupuncture-related interventions in conjunction with multimodal analgesia for post-TKA pain relief. This study seeks to utilize the benefits of combining traditional Chinese and Western medicine to offer evidence-based recommendations for selecting the most optimal treatment approach in clinical settings.
2 Materials and methods
Our study was conducted based on the checklist of the preferred reporting items for systematic reviews and meta-analyses for network meta-analysis (PRISMA-NMA) guidelines (42) (Supplementary Appendix 1) and reporting items of systematic reviews and meta-analyses involving acupuncture (43). The PRISMA-NMA and PRISMA for acupuncture checklists are both updates to PRISMA. Based on the 27 items from the PRISMA checklist, the PRISMA-NMA checklist revised 11 items related to NMA and added 5 new items to guide and improve the writing and reporting for NMA, while PRISMA for acupuncture checklist revised 6 items related to acupuncture operations and added 5 new items to be better used for the systematic review about acupuncture therapies. The research has been registered in PROSPERO, with the registration website https://crd.york.ac.uk/PROSPERO/#recordDetails and registration number CRD42023492859.
2.1 Literature retrieval strategy
A computer search was conducted in five English databases (Web of Science, PubMed, SCI-hub, Embase, and Cochrane Library) and four Chinese databases [China Biology Medicine (CBM), China National Knowledge Infrastructure (CNKI), Wanfang Data, and Chinese Scientific Journal Database (VIP)] to collect all randomized controlled trials (RCTs) on acupuncture therapy for pain after TKA from the establishment of the database until November 1, 2023 (Supplementary Appendix 2). The retrieval strategy employed a combination of subject headings and free words which were adjusted based on different retrieval systems. Retrieval terms included acupuncture, electroacupuncture, auricular acupuncture, transcutaneous electrical acupoint stimulation, total knee arthroplasty, multimodal analgesia, and pain (Figure 1).
2.2 The literature inclusion criteria
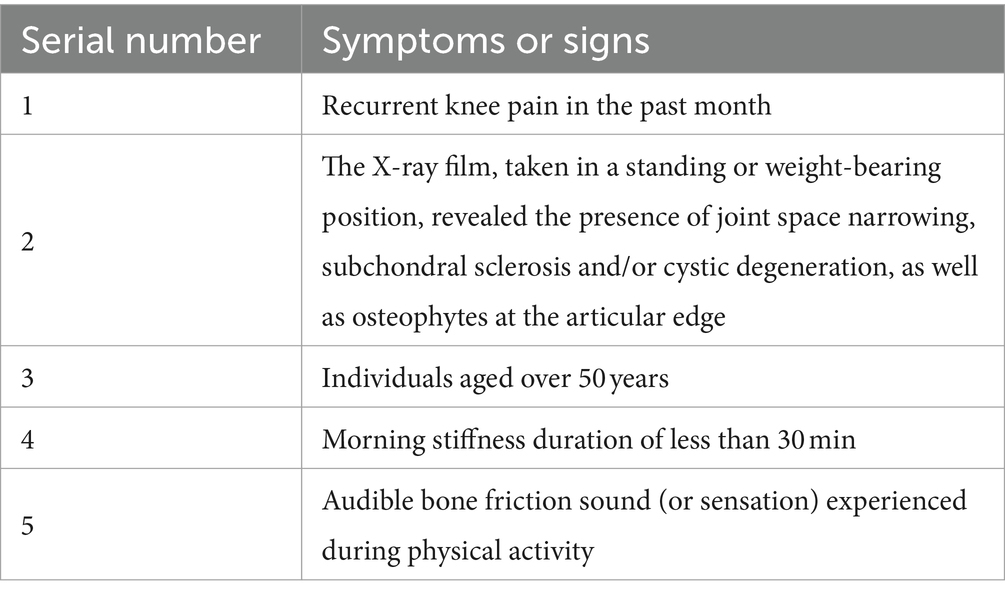
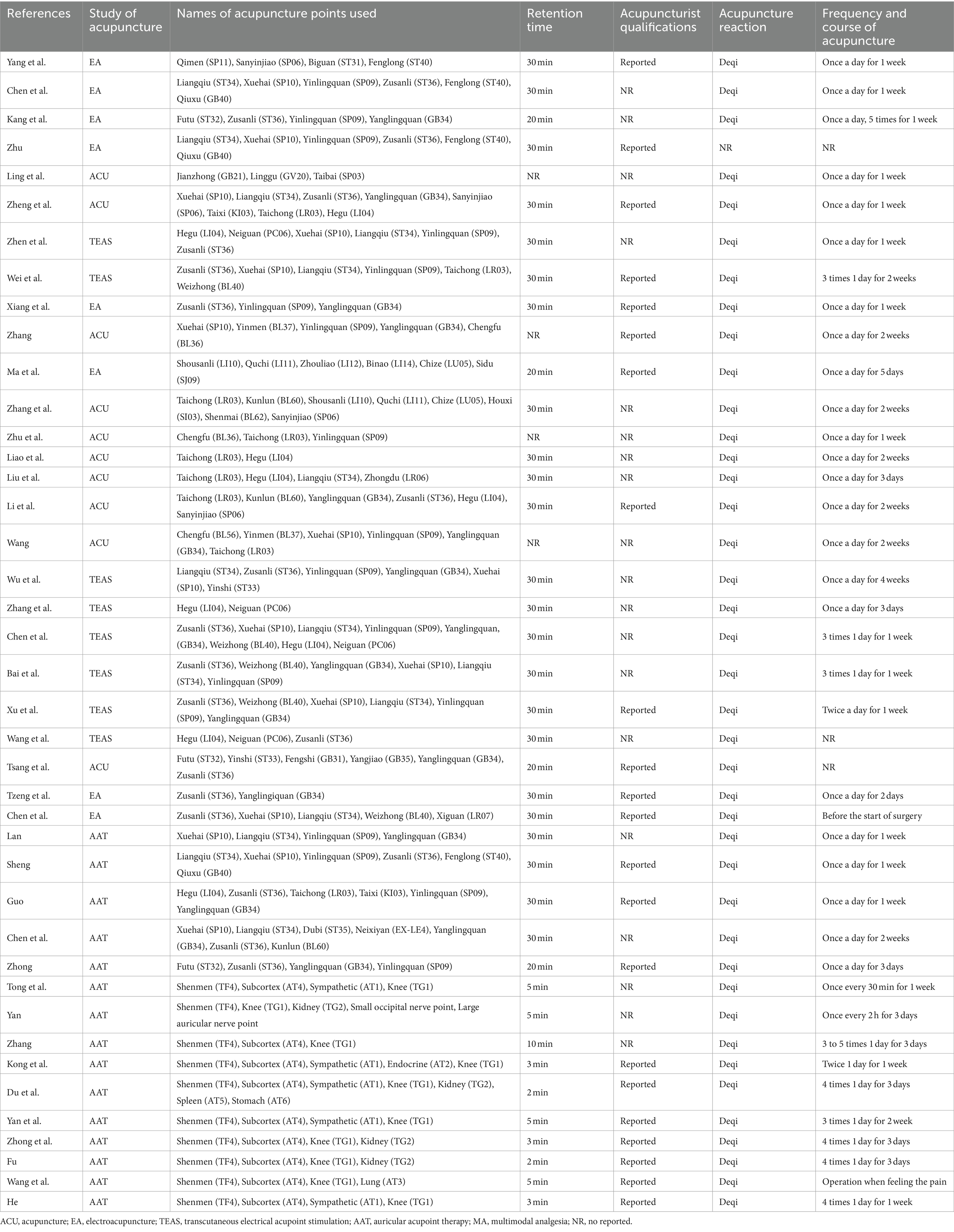
(1) The literature utilized in this study was a prospective randomized controlled trial (RCT). The inclusion criteria for the cases involved a diagnosis of knee osteoarthritis (44) based on the established diagnostic criteria for knee osteoarthritis (refer to Table 1). The cases were required to meet the first criterion and any two of the second, third, fourth, and fifth criteria. Additionally, the severity of knee osteoarthritis was assessed through the grading of knee X-ray films using the Kellgren-Lawrence method (45) (refer to Table 2). Subjects with Kellgren-Lawrence grades III and IV, necessitating TKA surgical intervention (46), will be encompassed. No limitations will be imposed on the patients’ age, gender, or race.
(2) The treatment group was administered various interventions, including acupuncture, transcutaneous electrical acupoint stimulation, electroacupuncture, and auricular acupuncture, in conjunction with multimodal analgesia (including one or more of analgesics, nervous block, and patient-controlled analgesia pump), while the control group solely received multimodal analgesia.
(3) The literature should contain original data pertaining to postoperative VAS score, preoperative and postoperative HSS score, preoperative and postoperative ROM measurements, preoperative and postoperative PPT score, and postoperative adverse events.
(4) The language of the literature could be either Chinese or English.
2.3 Exclusion criteria for literature
(1) The subjects in this study were diagnosed with knee arthritis, as indicated in Table 1. However, their Kellgren-Lawrence classification ranged from 0 to II, as shown in Table 2. Consequently, non-surgical therapy was chosen over TKA. The objective of this research was to conduct a randomized controlled trial to evaluate the efficacy of various acupuncture therapies in alleviating pain associated with knee arthritis.
(2) Non-randomized studies (NRSs) include non-randomized controlled clinical trials, self-control studies, historical control studies, cohort studies, case–control studies, and cross-sectional survey studies.
(3) Other non-penetrating stimuli (such as point ion penetration, laser irradiation, and magnetic therapy), other penetrating stimuli (such as head acupuncture, point injection, and point embedding), and special acupuncture methods (such as triangle needle, fire needle, and acupotomy).
(4) The control group received additional interventions, including psychological counseling and massage therapy.
(5) There was no original data in the literature, and the author could not be contacted.
(6) The authors of the literature were the same or showed the similar data results.
2.4 Primary and secondary outcomes
2.4.1 Primary outcome indicators
The primary outcome measures encompass two dimensions: first, the pain intensity experienced by the participants following TKA; second, the functional status of the knee joint in the participants prior to and post-TKA.
(1) Visual analog scale (VAS) score (47): A 10 cm long straight line is drawn on a blank sheet of paper, with “no pain” and “most severe pain” labeled at each end. The patient is instructed to indicate their pain level and psychological perception by marking a point on the line. The distance from the starting point to the marked point represents the intensity of pain. The study aims to assess the disparities in the VAS score between the third and seventh day after surgery, as well as the baseline value.
(2) The pain pressure threshold (PPT) (48) will be measured by applying pressure to the medial side of the knee joint, within a 3 cm range from the midpoint of the medial edge of the patella, using a digital pressure tester. The pressure will be gradually increased until the patient experiences pain, at which point it will be immediately ceased and the corresponding value recorded. The discrepancy between the PPT and the baseline value will then be calculated.
(3) The evaluation of the knee joint’s performance at hospital for special surgery (HSS) (49) encompasses various aspects, including pain, function, activity, muscle strength, flexion deformity, stability, and other relevant factors. A higher score on the HSS scale indicates better knee function. Additionally, the disparity between the HSS score and the initial value is computed to determine the improvement.
(4) The range of motion (ROM) (49) of the knee joint is assessed by measuring the extent of movement before and after TKA using a joint ruler. The discrepancy between ROM and the baseline value is then calculated.
2.4.2 Secondary outcome indicators
To further assess the effectiveness and safety of various acupuncture therapies, secondary outcome measures including the occurrence of postoperative nausea and vomiting, dizziness, and drowsiness were employed.
2.5 Literature screening and data extraction
Two researchers (YH and YX) independently conducted a comprehensive literature review and meticulously extracted relevant data. In concrete terms, the title and abstract were read and checked to exclude literature that did not meet the inclusion criteria. Then, the full texts of the potentially eligible studies were read to identify studies that could be included in this quantitative analysis. The results were cross-checked for accuracy, and in the event of any disagreement, a third researcher was consulted to reach a consensus.
Regarding data extraction, Excel 2016 was utilized to construct a systematic table encompassing pertinent information from eligible studies. This included: (1) general information: first author’s name, journal title, publication date, grouping details, and sample sizes in each group; (2) baseline characteristics: age distribution, disease duration, and pre-treatment measurements for each outcome indicator within every group; (3) intervention measures: type of acupuncture therapy administered, treatment frequency, and duration of treatment cycles; and (4) outcome indicators’ data along with post-treatment adverse reactions.
2.6 Assessment of risk bias in included studies
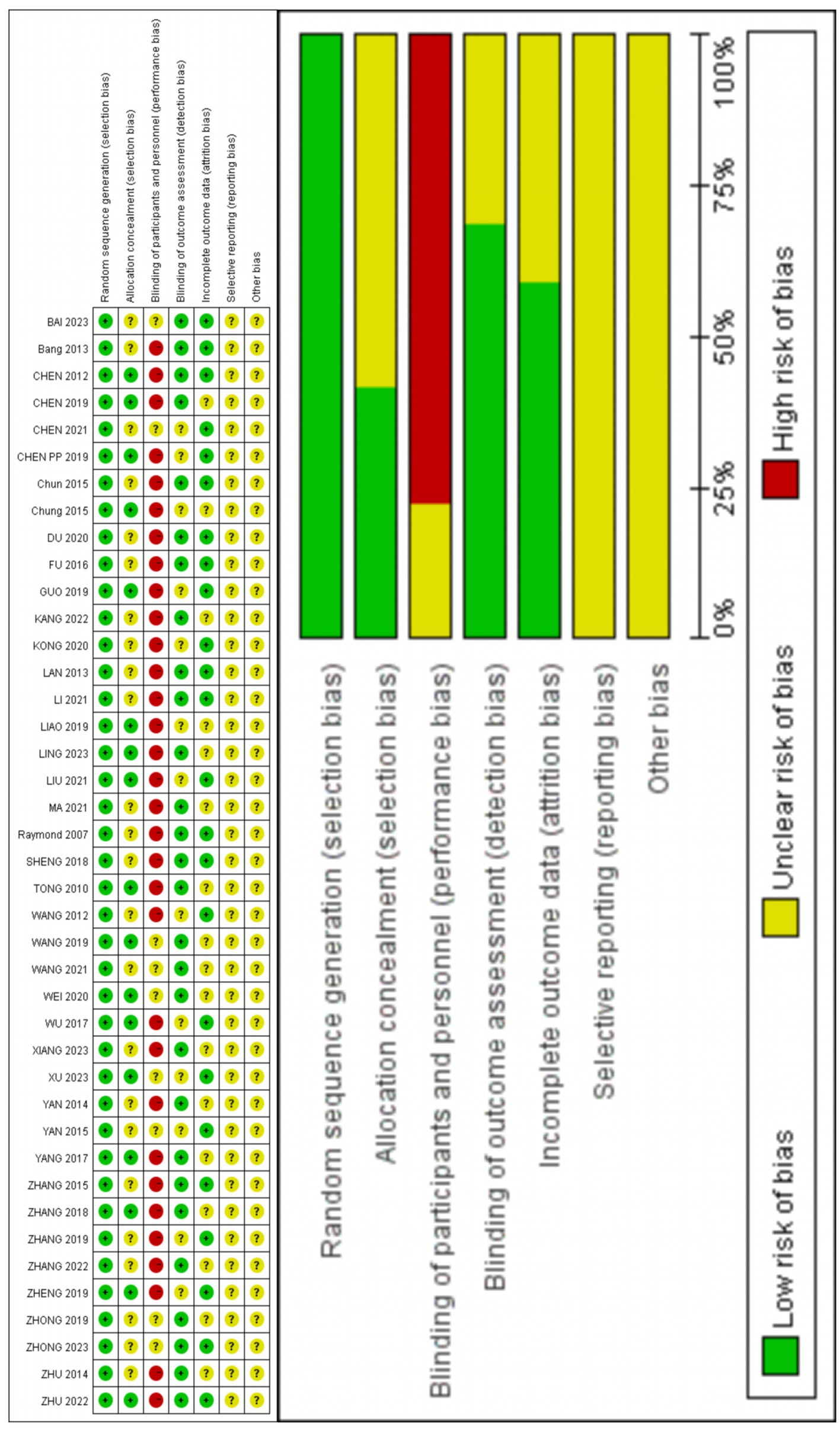
The Cochrane Handbook 5.1 was utilized for the assessment of risk bias in the included studies, encompassing randomization, assignment concealment, blinding of patients and staff, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other potential sources of bias (50, 51). In RevMan 5.4 software, we categorized the levels of risk as “high,” “low,” or “unclear,” respectively.
2.7 Statistical analysis
Software programs RevMan (Version 5.4) and Stata (Version16.0) were used to do statistical analysis. The study utilized odds ratios (ORs) and 95% confidence intervals (95% CIs) for dichotomous variables and mean differences ± standardized mean differences (SMD) and 95% CI for continuous variables.
Bias risk assessment was conducted using RevMan 5.4 software, and frequency science network meta-analysis was performed using Stata16.0. Data processing, network evidence graph drawing, network league table creation, and calculation of the surface under the cumulative ranking curve (SUCRA) were performed using the network and mvmeta package commands. The study was divided and restructured into all-paired two-arm trials if it had been a three-arm trial (52). In instances where closed loops were observed in the network evidence graph, indicating discrepancies among research findings, the ifplot command was employed to identify inconsistencies. The inconsistency factor (IF) value and its corresponding 95% confidence interval were computed for each closed loop to evaluate the consistency of direct and indirect comparison results. The fitting inconsistency test was performed on the closed loops formed in the network meta-analysis. If p > 0.05, the inconsistencies in direct and indirect comparisons were not statistically significant, and a consistency model could be used for meta-analysis. If there was no closed loop, the consistency model could be used directly. The SUCRA was generated with Stata16.0, which shows the SUCRA scores for all interventions, with higher SUCRA values denoting a higher treatment class. The closer the value was to 100%, the better the efficacy of the intervention (53). A funnel plot was constructed using Stata16.0 to examine potential publication bias within the included studies (54).
3 Results
3.1 Literature retrieval
After primary retrieval, a total of 2041 relevant literature were identified, comprising 1897 Chinese and 144 English publications. Following the removal of 1,695 duplicate articles, the remaining literature underwent screening based on titles and abstracts, resulting in the exclusion of 193 studies. Subsequently, after full-text evaluation, an additional 112 literature were excluded. Finally, a total of 41 literature (55–94) were included in this review (Figure 1 illustrates the specific inclusion process).
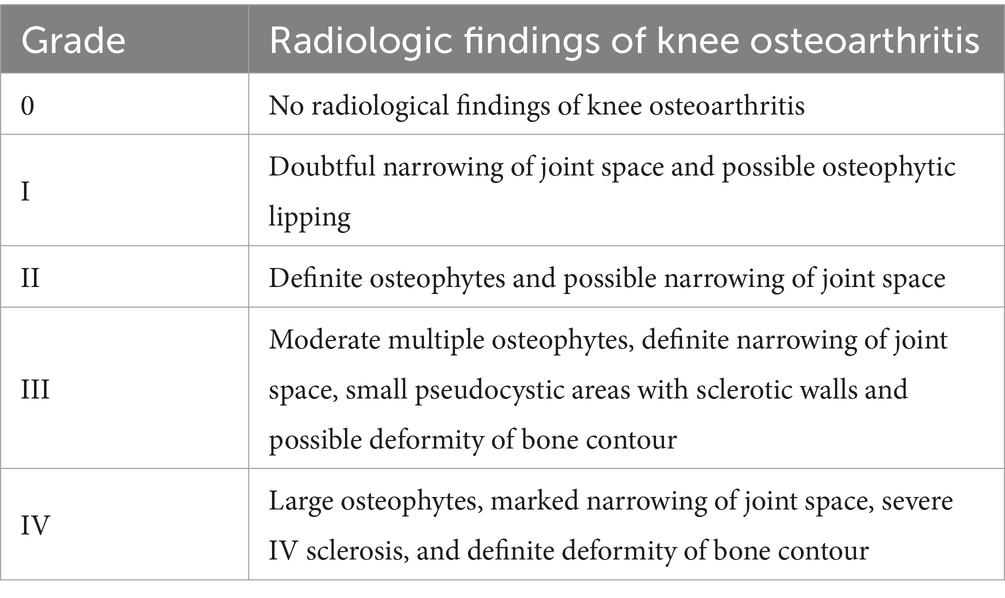
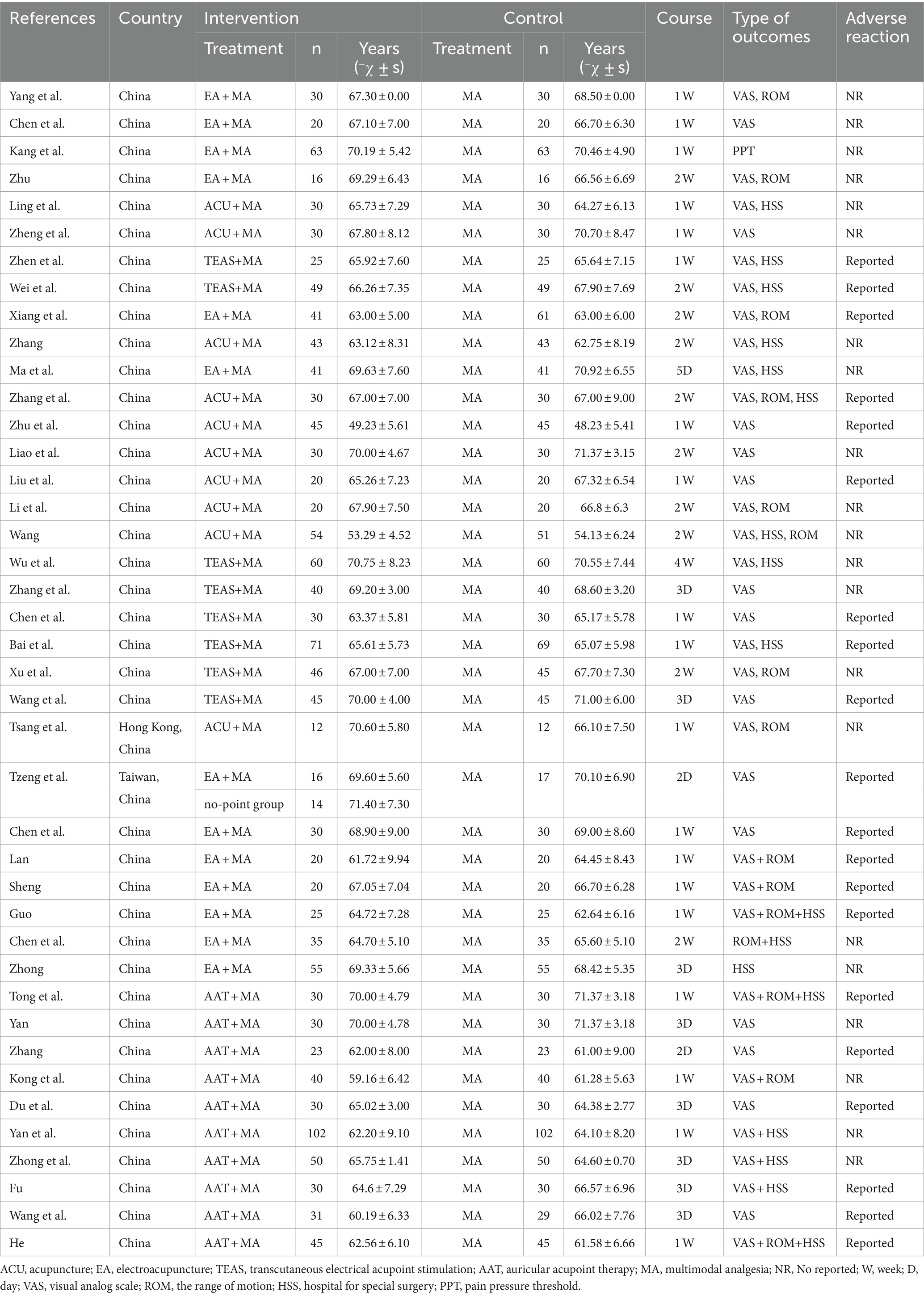
3.2 Basic characteristics of the included studies
In these selected studies (n = 41), four types of acupuncture therapy interventions were investigated: acupuncture alone, electroacupuncture, transcutaneous electrical acupoint stimulation (TEAS), and auricular therapy. These interventions were combined with perioperative multimodal analgesia. Among them, one study employed a three-arm trial design (57), while the rest utilized two-arm trials. Tables 3, 4 present detailed information regarding baseline characteristics and acupuncture methods used in the included studies.
3.3 Quality evaluation of the included literature
The risk bias assessment was independently conducted by two researchers (DZ and LW). The evaluation criteria consisted of seven items including randomization method, allocation concealment method, and blinding procedures for participants or outcome assessment. Of all the trials reviewed (n = 41), 41 (100%) described their random sequence generation process, while only 17 (42%) reported their allocation concealment method. None of the studies implemented blinding techniques for participants or outcome evaluation. Twenty-seven trials (65%) provided complete outcome data. It should be noted that due to the nature of acupuncture treatment involving active participation from both practitioners and patients during administration, implementing blind methods is challenging. The results of risk assessment are shown in Figure 2.
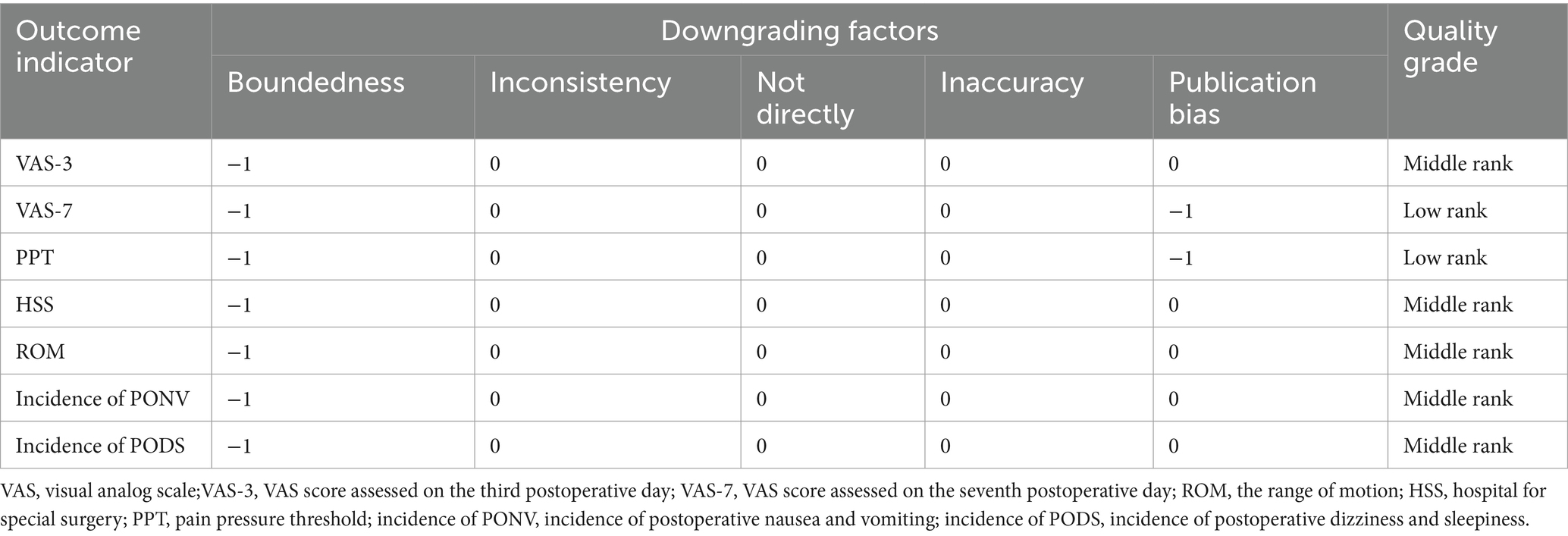
The quality of evidence of the included studies was evaluated according to the GRADE assessment method, and seven outcome indicators were analyzed. Evidence for VAS-3, HSS, ROM, incidence of PODS, and incidence of PONV was of medium quality. The quality of evidence for VAS-7 and PPT was low. The decline in quality was mainly caused by the limitations of randomization method and the blinding method as well as the imprecision due to the small sample size. The detailed quality assessment is shown in Table 5.
3.4 Results of network meta-analysis
3.4.1 Evidence network diagram of intervention measures
Stata16.0 was utilized to analyze the evidence network diagram of five intervention measures, where the size of each circle represents the sample size and the thickness of connecting lines indicates the number of RCTs using two intervention measures (Figure 3).
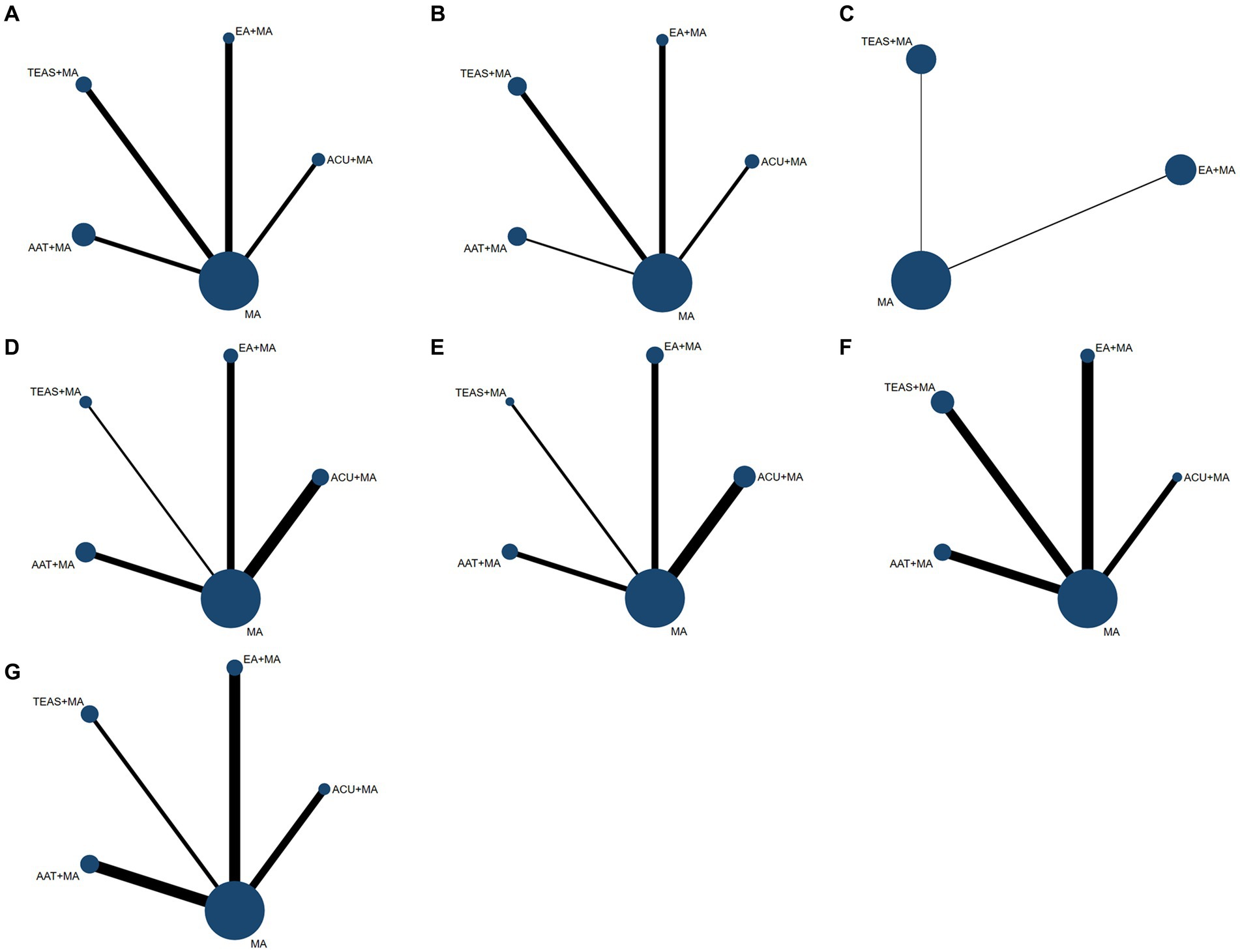
Figure 3. Network structure for treatment comparisons. (A) VAS-3 scores; (B) VAS-7 scores; (C) PPT scores; (D) HSS scores; (E) ROM scores; (F) incidence of postoperative nausea and vomiting; (G) incidence of postoperative dizziness and sleepiness. ACU, acupuncture; EA, electroacupuncture; TEAS, transcutaneous electrical acupoint stimulation; AAT, auricular acupoint therapy: MA, multimodal analgesia.
3.4.2 Conflict detection
The evidence network diagram presented in Figure 3 indicated the absence of closed-loop formation for both primary and secondary outcome indicators, thereby precluding the need for an inconsistency test.
3.4.3 Primary outcome indexes VAS-3, VAS-7, PPT, HSS, and ROM scores
(1) As shown in Figure 3A, a total of 29 RCTs mentioned VAS score on the third day after TKA, involving 2039 patients and 5 interventions including ACU + MA, EA + MA, TEAS+MA, AAT + MA, and MA. There was no significant difference in the efficacy of the five interventions in improving VAS score on the third day after TKA (Table 6).
(2) As shown in Figure 3B, a total of 21 RCTs mentioned VAS score on the seventh day after TKA, involving 1,447 patients and 5 interventions including ACU + MA, EA + MA, TEAS+MA, AAT + MA, and MA. In improving VAS score on the seventh day after TKA, TEAS+MA (SMD: 0.67; 95% CI: 0.01, 1.32) was superior to MA (Table 6).
(3) As shown in Figure 3C, a total of four RCTs mentioned postoperative PPT scores, involving 408 patients and 3 interventions: EA + MA, TEAS+MA, and MA. In terms of improving PPT scores after TKA, there was no significant difference in the efficacy of EA + MA, TEAS+MA, and MA interventions (Table 6).
(4) As shown in Figure 3D, a total of 15 RCTs mentioned postoperative HSS scores, involving 1,397 patients and 5 interventions including ACU + MA, EA + MA, TEAS+MA, AAT + MA, and MA. In terms of improving postoperative HSS scores after TKA, the three interventions including ACU + MA (SMD: 6.45; 95%CI: 3.30, 9.60), EA + MA (SMD: 4.89; 95%CI: 1.46, 8.32), and TEAS+MA (SMD: 5.31; 95%CI: 0.85, 9.78) were more effective than MA, which helped to promote early knee joint function recovery after TKA (Table 6).
(5) As shown in Figure 3E, a total of 18 RCTs mentioned postoperative ROM, involving 1,150 patients and 5 interventions including ACU + MA, EA + MA, TEAS+MA, AAT + MA, and MA. In terms of improving postoperative ROM scores after TKA, the efficacy of ACU + MA (SMD:7.43; 95%CI: 2.51, 12.36) was better than EA + MA, the efficacy of ACU + MA (SMD:10.12; 95%CI: 2.79, 17.45) was better than TEAS+MA, the efficacy of ACU + MA (SMD: 7.82; 95%CI: 2.21, 13.43) was better than AAT + MA, and the efficacy of ACU + MA (SMD: 9.74; 95%CI: 6.12, 13.37) was better than MA. It can be seen that ACU + MA has a significant advantage in improving postoperative ROM compared with other interventions (Table 6).
3.4.4 Secondary outcome indicators: incidence of adverse reactions
(1) As shown in Figure 3F, a total of 21 RCTs mentioned the incidence of postoperative nausea and vomiting, involving 1,389 patients and 5 interventions: ACU + MA, EA + MA, TEAS+MA, AAT + MA, and MA. The occurrence of postoperative nausea and vomiting was significantly lower with ACU + MA (OR = 0.30; 95%CI: 0.11, 0.85), EA + MA (OR = 0.44; 95%CI: 0.22, 0.87), TEAS+MA (OR = 0.30; 95%CI: 0.17, 0.53), and AAT + MA (OR = 0.20; 95%CI: 0.11, 0.36) compared to MA (Table 6).
(2) As shown in Figure 3G, a total of 16 RCTs mentioned the incidence of postoperative dizziness and drowsiness, involving 1,076 patients and 5 interventions: ACU + MA, EA + MA, TEAS+MA, AAT + MA, and MA. The occurrence of postoperative dizziness and drowsiness was higher with ACU + MA (OR = 4.98; 95%CI: 1.01, 24.42) than with AAT + MA; the incidence of postoperative dizziness and drowsiness was lower with TEAS+MA (OR = 0.36; 95%CI: 0.18, 0.70) and AAT + MA (OR = 0.20; 95%CI: 0.08, 0.50) than with MA (Table 6).
The incidence of adverse reactions in the study utilizing acupuncture-related therapy as an intervention measure was generally lower compared to that of the simple multimodal analgesia scheme, thereby indicating the safety and efficacy of applying acupuncture-related therapy during the perioperative period of TKA.
3.4.5 SUCRA probability ranking
(1) As shown in Table 7 and Figure 4A, in terms of improving VAS score on the third day after surgery, the SUCRA probability ranking results showed that EA + MA (SUCRA = 74.2%) > TEAS+MA (SUCRA = 73.3%) > MA (SUCRA = 51.1%) > ACU + MA (SUCRA = 39.7%) > AAT + MA (SUCRA = 11.8%).
(2) As shown in Table 7 and Figure 4B, in terms of improving VAS score on the seventh day after surgery, the SUCRA probability ranking results showed that TEAS+MA (SUCRA = 92.0%) > EA + MA (SUCRA = 69.6%) > MA (SUCRA = 37.8%) > AAT + MA (SUCRA = 25.6%) > ACU + MA (SUCRA = 24.9%).
(3) As shown in Table 7 and Figure 4C, in terms of improving postoperative PPT score, the SUCRA probability ranking results showed that TEAS+MA (SUCRA = 74.4%) > EA + MA (SUCRA = 67.1%) > MA (SUCRA = 8.2%).
(4) As shown in Table 7 and Figure 4D, in terms of improving postoperative HSS score, the SUCRA probability ranking results showed that ACU + MA (SUCRA = 83.2%) > TEAS+MA (SUCRA = 66.5%) > EA + MA (SUCRA = 61.2%) > AAT + MA (SUCRA = 38.0%) > MA (SUCRA = 1.0%).
(5) As shown in Table 4 and Figure 4E, in terms of improving postoperative ROM score, the SUCRA probability ranking results showed that ACU + MA (SUCRA = 99.9%) > EA + MA (SUCRA = 55.9%) > AAT + MA (SUCRA = 49.6%) > TEAS+MA (SUCRA = 24.1%) > MA (SUCRA = 20.5%).
(6) As shown in Table 7 and Figure 4F, the SUCRA probability ranking results for the incidence of postoperative nausea and vomiting were as follows: MA (SUCRA = 99.5%) > EA + MA (SUCRA = 62.4%) > TEAS+MA (SUCRA = 39.0%) > ACU + MA (SUCRA = 37.4%) > AAT + MA (SUCRA = 11.7%).
(7) As indicated in Table 7 and Figure 4G, the SUCRA probability ranking results demonstrate that MA (SUCRA = 85.0%) exhibits a higher incidence of postoperative dizziness and drowsiness compared to ACU + MA (SUCRA = 79.6%), EA + MA (SUCRA = 50.8%), TEAS+MA (SUCRA = 28.7%), and AAT + MA (SUCRA = 5.9%).
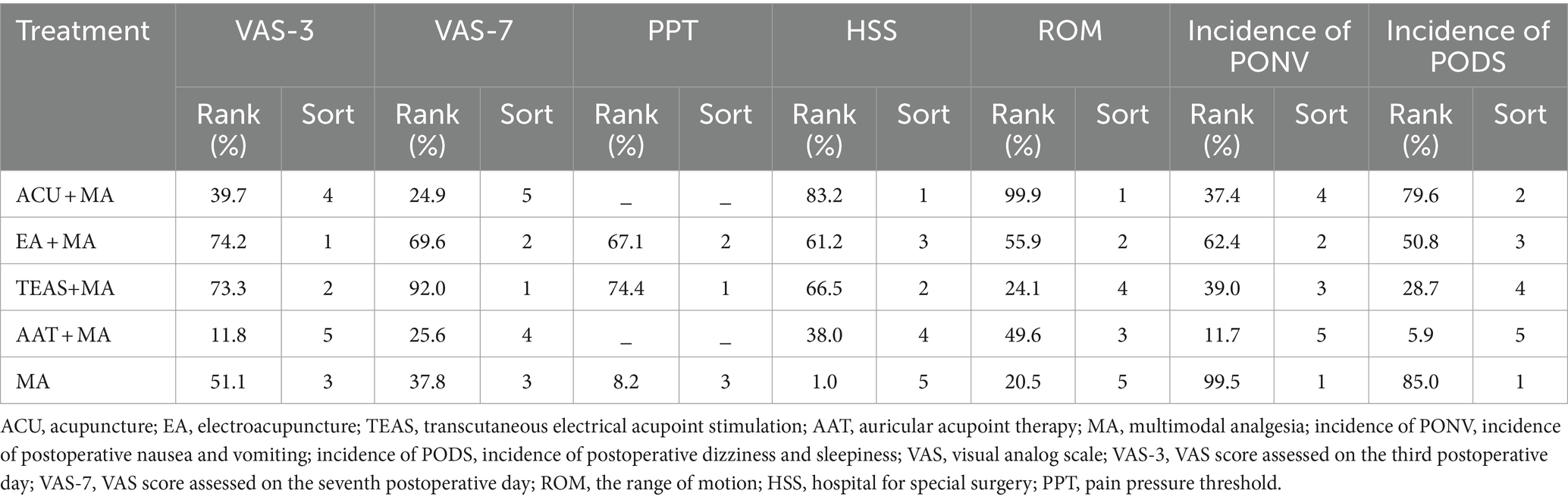
Table 7. Ranking of SUCRA for each outcome index after TKA using different acupuncture therapy combined with multimodal analgesia.
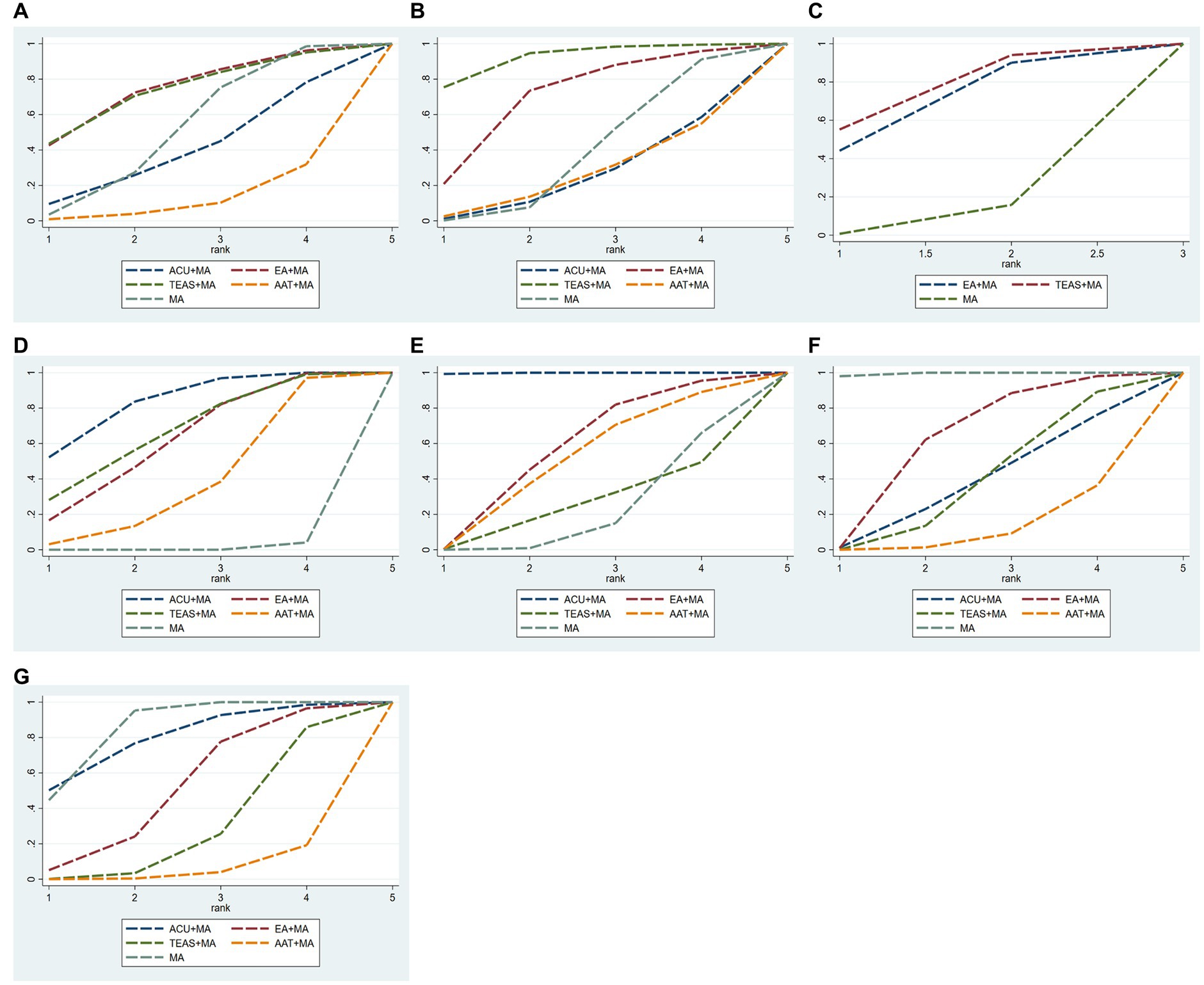
Figure 4. SUCRA probability ranking of interventions. (A) VAS-3 scores; (B) VAS-7 scores; (C) PPT scores; (D) HSS scores; (E) ROM scores; (F) incidence of postoperative nausea and vomiting; (G) incidence of postoperative dizziness and sleepiness. ACU, acupuncture; EA, electroacupuncture; TEAS, transcutaneous electrical acupoint stimulation; AAT, auricular acupoint therapy; MA, multimodal analgesia.
3.4.6 Publication bias test
The adjustment-comparison funnel plots were constructed to assess publication bias for both primary and secondary outcome indicators. However, the asymmetry observed in the HSS score “comparison-adjustment” funnel plots suggests potential publication bias among the included studies. Additionally, some studies examining the primary outcome indicators deviated from the 95% confidence interval of the funnel plot, indicating a possible small sample effect (Figure 5).
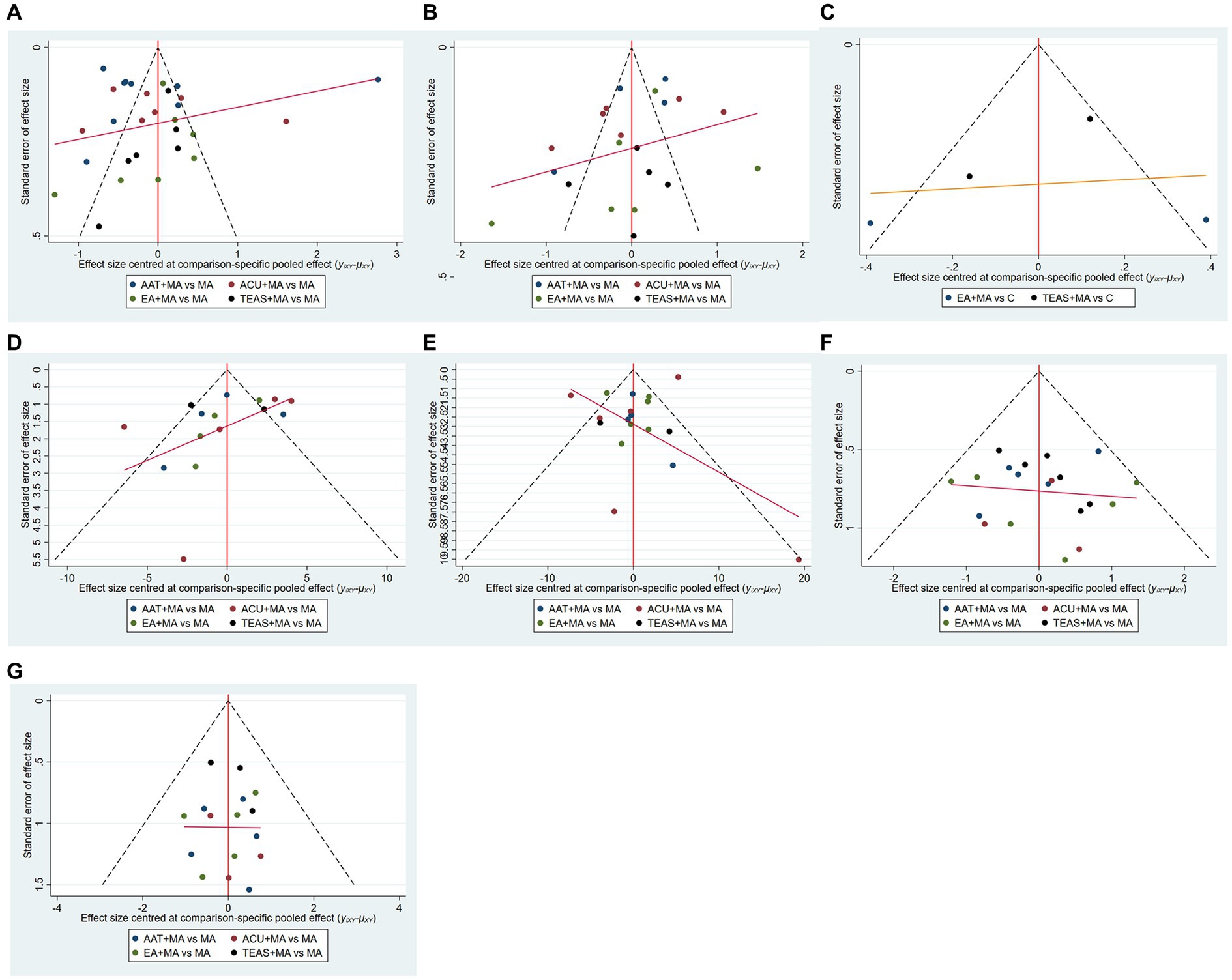
Figure 5. Funnel diagram. (A) VAS-3 scores; (B) VAS-7 scores; (C) PPT scores; (D) HSS scores; (E) ROM scores; (F) incidence of postoperative nausea and vomiting; (G) incidence of postoperative dizziness and sleepiness. ACU, acupuncture; EA, electroacupuncture; TEAS, transcutaneous electrical acupoint stimulation.
4 Discussion
This network meta-analysis included 41 randomized controlled trials involving 3,003 patients who underwent TKA. It aimed to explore the effectiveness and safety of different acupuncture therapies in reducing postoperative pain after TKA, evaluating them based on four outcome indicators and the incidence of adverse reactions. The results revealed that EA + MA and TEAS+MA demonstrated superior efficacy in improving the postoperative VAS score of TKA patients. ACU + MA showed better efficacy in enhancing the postoperative ROM score and HSS score of TKA patients. In terms of adverse reactions, AAT + MA effectively reduced the occurrence of postoperative nausea, vomiting, dizziness, and drowsiness. Furthermore, EA + MA, TEAS+MA, and AAT + MA all exhibited better efficacy than MA alone while establishing the safety profile of acupuncture-related therapies for TKA.
The NMA method utilized in this study compared the effectiveness of various acupuncture therapies for postoperative pain and joint function recovery through indirect data analysis, compensating for the lack of direct evidence. These findings provide some support for acupuncture-related treatments to enhance postoperative pain management and facilitate early rehabilitation. In contrast to traditional meta-analyses (95), this study employed the NMA approach to comprehensively assess the included literature and rank different acupuncture therapies. Furthermore, our results confirmed the potential benefits of acupuncture-related interventions in improving postoperative pain and promoting early rehabilitation. Notably, common complications following TKA include nausea, vomiting, dizziness, and drowsiness that can cause significant discomfort for patients. Such symptoms may trigger a self-protective response that makes patients feel seriously ill and leads to reduced activity levels as well as negative attitudes toward early rehabilitation. Therefore, we also evaluated the incidence of adverse reactions after TKA.
The primary objective of TKA is to alleviate the pain associated with knee arthritis, enhance knee joint functionality, and enhance the overall quality of life for patients. However, the occurrence of severe postoperative pain following TKA is a prevalent adverse event that can impede the progress of rehabilitation training. In 1998, Wulf et al. (96) introduced the notion of external focus of attention (EFA), which has garnered significant attention within the realm of rehabilitation medicine (97). The concept of EFA pertains to the process of engaging in actions, specifically skill learning, by directing attention toward the surrounding environment of the action, including sports equipment, the intended goal, and the resultant effect. In contrast, the traditional approach known as Internal Focus of Attention (IFA) centers attention on the action itself, focusing on the involved joints and muscles. EFA aiming at the movement effect has been reported to have more efficacy than IFA aiming at movement characteristics in healthy subjects (98). Research findings have consistently demonstrated that the implementation of EFA, as opposed to IFA, significantly contributes to the restoration of motor function in patients afflicted with anterior cruciate ligament injury (99), ankle sprain (99), stroke (99), and Parkinson’s disease (97). Giacomo Rossettini’s research has revealed that the EFA strategy influences positively the motor performance more than IFA and control and is preferred by the subjects (98). Acupuncture therapy is commonly employed in the rehabilitation of musculoskeletal disorders, including post-total knee arthroplasty. In this study, the acupuncture practitioner primarily instructs patients to perform the EFA strategy, such as attempting to kick a training bat held by the practitioner, as part of the treatment. Postoperative rehabilitation exercise plays a crucial role in mitigating complications, such as knee stiffness and limited activity, for patients undergoing TKA. In clinical practice, it is commonly recommended that patients achieve a knee flexion of 90°and a knee extension of 0°after TKA, to fulfill the general activity requirements (100). The rehabilitation exercise regimen primarily encompasses active knee extension training, straight leg lifting training, and passive knee flexion and extension exercises, with a gradual increment in the angle of knee flexion exercise, while encouraging patients to get out of bed as soon as possible with crutches (101).
The postoperative pain experienced by patients undergoing TKA has detrimental effects on both their physical functioning during exercise and their mental wellbeing. If joint mobility remains restricted and deformities persist following the surgical procedure, it can easily trigger negative emotions. A study conducted by researchers (102) demonstrated a significant correlation (r = 0.40, p < 0.001) between the severity of depression and the intensity of pain experienced by patients 48 h after the surgery. Postoperative pain is a common adverse event following TKA, with multifaceted causes including mechanical pain resulting from surgical damage to the knee joint and surrounding tissues (103), spasm pain caused by vascular stenosis, tissue ischemia, and edema due to intraoperative tourniquet application (37), neuropathic pain caused by perioperative nerve compression, nerve ischemia, and hypoxia (such as anterolateral knee epidermal nerve injury) (104), and idiopathic pain caused by emotional factors. Although multimodal analgesia schemes have been used in clinical practice for over 20 years to treat post-TKA pain, reports indicate that 10–34% of patients still experience severe pain. Acupuncture has been found to exert peripheral analgesic effects through purinergic signals, the endocannabinoid system, peripheral endogenous opioid peptides, and transient receptor potential vanilloid subfamily (TRPV) channels (36, 105). The reward system and limbic system are related to the central loop of acupuncture-induced pain reduction; among these regions, the rostral anterior cingulate cortex (rACC) is a key brain region. Cannabinoid receptors and dopamine receptors in the brain are closely associated with acupuncture’s ability to relieve pain (106). While different acupuncture therapies operate on floodgate theory mechanisms for their mechanism of action, their afferent effect mechanisms differ. Acupuncture and electroacupuncture regulate dorsal root nerves’ transient potential receptor 1 and purinergic signal P2X3 for analgesic effects (107), while auricular therapy and TEAS may be related to the activation of subcutaneous class C afferent nerve fibers and class A nerve fibers (108). Which afferent effect mechanism is more effective is still unclear. Both acupuncture therapy and exercise therapy have been shown to have a significant therapeutic impact on the rehabilitation process following total knee arthroplasty. The combination of acupuncture therapy and exercise rehabilitation training specifically targets the affected knee joint. Acupuncture therapy effectively alleviates postoperative pain, while exercise therapy promotes active movement and strengthening of the knee joint. The application of acupuncture therapy has been found to enhance local blood circulation, mitigate inflammatory response, and effectively promote detumescence and analgesia. Concurrently, exercise therapy has been shown to enhance the flexion and extension movement function of the knee joint, as well as augment muscle strength (109). The integration of these two treatment modalities effectively addresses the limitations associated with relying solely on a single rehabilitation approach (110).
A meta-analysis study revealed a correlation between pain intensity in musculoskeletal disorders and somatoperception (SoP), space perception (SpP), and body ownership (BO). Following TKA procedures, there was an increase in SoP, SpP, and BO at 3 and 6 weeks post-surgery as pain intensity decreased. Patients with knee osteoarthritis exhibited higher levels of somatosensory dysfunction compared to healthy individuals, while those with fibromyalgia were more susceptible to experiencing bodily illusions. While the precise correlation between pain intensity and the three (SoP, SpP, BO) remains uncertain, it is plausible to posit that the interplay between pain and sensory dysfunction may significantly influence clinical outcomes (111). Previous research (112) has indicated that a majority of individuals diagnosed with knee osteoarthritis (KOA) experience varying levels of proprioception impairments and diminished accuracy. Proprioception is a crucial factor in upholding knee posture and stability during both stationary and active movements as it collaborates with the vestibular and visual systems within a closed loop. Following TKA, patients may restrict their range of motion due to apprehension of pain or unsuitable environmental circumstances, consequently resulting in compromised sensorimotor control functionality. The sensorimotor control disorder of the knee joint, resulting from post-TKA pain, is regarded as a stress response mechanism aimed at reducing further stimulation of painful tissue (113). Over time, this disorder may lead to fatigue and tissue damage in the muscle groups adjacent to the knee joint, exacerbate pain by sensitizing both the peripheral and central nervous systems, and contribute to the disruption of movement patterns (114). Acupuncture is a complex somatosensory stimulation that triggers a wide range of effects in the body (115). Neuroimaging studies have suggested that acupuncture-induced cortical activation mainly reflects the somatosensory, affective, and cognitive processing of pain (116). Genuine acupuncture stimulated several networks of brain activation, including ACC (pregenual anterior, dorsal anterior, and middle), prefrontal cortex, and the parahippocampus (117). The anterior insula is well known for its integrative role in afferent and visceral information and representation of subjective feeling in diverse domains, including pain perception (118). The activation of the ACC also triggers the endogenous analgesia system and modulates sensory transmission at the level of the spinal cord via descending inhibitory modulation (119). The findings of a meta-analysis were that proprioceptive training seemed to alleviate pain and improve the walking speed of patients with knee OA (120). Nevertheless, acupuncture therapy can enhance proprioception of knee joints in patients with osteoarthritis. Simultaneously, acupuncture stimulation increases tactile sensitivity in the ACC and parahippocampus and also strongly influences pain perception in the two-point discrimination task. Acupuncture stimulation leads to the activation of brain regions such as the posterior frontal lobe and anterior cingulate cortex, but the involved interoceptive-autonomic neural network still needs further study (121). Another study concluded that acupuncture may offer analgesic effect that is not dependent on precisely where the needles are inserted so much as that the patient attends to where they are inserted. The mechanism is improvement in self-perception mediated through the sensory discrimination-like qualities of acupuncture (122).
Acupuncture has been found to elicit immune cell stimulation, particularly the activation of regulatory T cells (Treg cells), resulting in increased production of IL − 10 (123). This process also aids in regulating the decrease of macrophages and neutrophils, thereby inhibiting the expression of pro-inflammatory mediators such as IL − 1β, NLRP3, and TNF-α. Consequently, acupuncture demonstrates anti-inflammatory and analgesic effects. Additionally, acupuncture directly activates endogenous opioids, such as enkephalin and β-endorphin, in both the central and peripheral systems, thereby contributing to its analgesic effects (124). In addition to conventional analgesic methods, acupuncture has the potential to alleviate pain indirectly through various mechanisms, including the placebo effect (125), modulation of patients’ negative emotions, and alteration of the contextual effect (CE) (126). The placebo effect (125) associated with sham acupuncture refers to the phenomenon wherein patients do not receive genuine acupuncture treatment, yet experience symptom relief due to their “psychological belief” in the efficacy of the ineffective therapy. The mechanism of the placebo analgesic effect and acupuncture analgesia exhibits similarities. Research employing μ opioid selective tracing and positron emission tomography (PET) to examine the analgesic impact of sham acupuncture demonstrated the presence of endogenous opioids being released in areas associated with pain regulation (127), such as the dorsolateral prefrontal cortex (DLPFC), anterior cingulate cortex (rACC), and periaqueductal gray (PAG). Functional magnetic resonance imaging (fMRI) investigations have additionally demonstrated a decrease in pseudo-needle-induced signals within pain-sensitive cerebral areas, namely, the thalamus and the insular cortex, potentially associated with the alleviation of pain through pseudo-needles (128). Moreover, the placebo response elicited by sham acupuncture involving skin penetration exhibits a greater magnitude of effect compared to sham acupuncture devoid of skin penetration (129). Placebo effect of sham acupuncture incarnates the psychosomatic co-governance of Chinese medicine and also conforms to modern biological–psychological–social–medical philosophy. The anterior cingulate cortex (ACC) serves as the regulatory hub for emotional activity within the limbic system, and it exhibits fiber connections with various brain regions (130). Within the ACC, there exists excitatory glutamate N-methyl-D-aspartate (NMDA), which has garnered considerable interest in the context of pain aversion. Specifically, the NR2 subtype of NMDA is implicated in the modulation of nociceptive perception within the central nervous system and assumes a pivotal role in the development of pain. Acupuncture has been shown to decrease the levels of NR2A and NR2B proteins in the ACC brain region, resulting in a reduction in the excitability of ACC neurons. This downregulation of phosphorylation levels in the ACC contributes to the alleviation of pain aversion and ultimately diminishes the pain experience in patients (131, 132). Contextual factors (CFs) are components of all therapeutic encounters and may constitute the entirety of the perceived effects of the intervention itself or be additive to effects of interventions such as pharmacological and non-pharmacological treatments (133). CFs are perceived cues that affect both the patient and practitioner. Different categories of CFs exist, encompassing patient characteristics, practitioner characteristics, treatment characteristics, the dynamics between the patient and practitioner, and the setting in which the encounter takes place. The size of the observed clinical effects related to CFs can vary significantly based on the patient’s attributes, the practitioner involved, the specific condition being addressed, and the intervention employed. Notably, acupuncture treatment presents a unique challenge in blinding, resulting in a heightened expectation-related placebo effect compared to other placebos (134). For instance, the acupuncturist’s expertise and effective communication foster positive treatment expectations, which frequently correlate with improved treatment outcomes. A significant percentage of postoperative pain relief may be attributed to patients being informed about how the acupuncture therapy will likely impact on their postoperative pain, thus channeling an effective placebo response (135). Expectation-dependent placebo responses are, in principle, mediated by the endogenous opioid system, and the ventromedial prefrontal cortex (vmPFC), the dorsolateral prefrontal cortex (dlPFC), the lateral orbitofrontal cortex (lOFC), hypothalamus, and periaqueductal gray are generally regarded as crucial (136–138). The expectation-dependent placebo effect is similar to acupuncture analgesia, showing that an opioid-dependent cortical network becomes activated during a placebo response. The challenge of managing patients’ expectations in musculoskeletal pain remains a significant issue. Clinicians must carefully determine the appropriate timing and approach to address negative expectations, weighing the potential benefits of minimizing nocebo effects against the potential risks of jeopardizing the therapeutic alliance and increasing drop-out rates. Clinicians may use the intensity of patients’ expectations as a gauge to determine whether a direct challenge (i.e., optimization) or an indirect challenge of their beliefs (i.e., violation) is more appropriate, to preserve the therapeutic alliance and avoid damages (139).
Currently, total knee arthroplasty stands as the most efficacious intervention for advanced rheumatoid arthritis (RA), a prevalent inflammatory arthropathy (IA). It is noteworthy that a significant proportion of patients undergoing total knee arthroplasty for advanced RA present with comorbidities. A meta-analysis (140) reveals a substantial rise in the prevalence of fibromyalgia (FM) among individuals with inflammatory arthritis, with rates reaching 18–24% in those with RA. FM is typified by widespread and enduring musculoskeletal pain, frequently accompanied by psychological conditions such as anxiety and depression (141). The studies have found objective alterations or dysfunctions of the large Aβ and of the group of thin Aδ and C fibers (the so-called “small-fibers”) in approximately 50% of FM patients (142). It is believed that the analgesic effects of electroacupuncture and transcutaneous electrical acupoint stimulation are mediated by the activation of these nerve fibers. This network meta-analysis demonstrates that acupoints, including Sanyinjiao (SP06), Zusanli (ST36), Hegu (LI04), and Taichong (LR03), exhibit potential for pain management following TKA. Specifically, acupuncture at Sanyinjiao exhibits the ability to mitigate hyperactivity within the hypothalamic–pituitary–adrenal (HPA) axis by reducing serum levels of norepinephrine and cortisol, thereby ameliorating non-specific symptoms associated with FM, such as insomnia, anxiety, and depression (143). Furthermore, acupuncture at Zusanli exhibits potential in the treatment of rheumatic immune diseases through immunoregulatory mechanisms and the inhibition of inflammatory cytokine release (144). Acupuncture administered at the Hegu acupoint has been found to stimulate the release of plasma β-endorphin, regulate the activity of the hypothalamic–pituitary system, and suppress both pain perception and emotional response (145). Similarly, acupuncture at the Taichong acupoint has been observed to induce alterations in brain activation signals and provide symptomatic relief for emotional and pain-related disorders (146). Consequently, acupuncture therapy not only effectively addresses postoperative pain and enhances knee function following TKA but also demonstrates clinical efficacy in the treatment of fibromyalgia, potentially exhibiting multiple therapeutic effects.
There are still some limitations in this study: (1) As a result of the distinctive characteristics inherent in acupuncture practice, certain studies failed to furnish comprehensive details regarding the specific randomization and blinding techniques employed during implementation. Since acupuncture operations cannot be blinded to patients, the principle of triple separation of clinical operators, efficacy evaluators, and statistical analysts can be utilized. (2) The risk of bias assessment of the included studies was mostly unclear, and the quality of the literature was low. Therefore, in future studies, reporting should be based on the Consolidated Standards of Reporting Trials (CONSORT) to ascertain the literature quality (147). (3) The absence of any analgesic regimen during the perioperative period for patients undergoing TKA contradicts the principles of ERAS. Consequently, a majority of the studies included in this analysis were semi-randomized controlled trials, which lacked placebo control groups. There exist variations in the parameters of EA and TEAS across different studies. Acupuncture therapy has many differences in the acupoint selection, manipulation, and frequency, which could cause heterogeneity. Well-designed subgroup analysis should have been conducted. (4) Furthermore, a majority of the studies included in the analysis were small-scale randomized controlled trials, which may introduce selection bias and implementation bias, consequently resulting in low quality of literature. (5) Due to limitations within the original literature, intervention measures were categorized into ACU + MA, EA + MA, TEAS+MA, AAT + MA, and MA interventions. The results suggest that combined therapies have better performance in improving the outcome indicators. However, there are many combinations of combined therapies, which will be further elaborated in subsequent studies. (6) The assessment of PPT was conducted using a restricted number of studies, potentially leading to biased outcomes. (7) The studies included in the analysis primarily emphasized the short-term effectiveness of acupuncture therapy in terms of alleviating postoperative pain and rehabilitating joint function after TKA surgery. However, the evaluation of long-term efficacy for acupuncture therapy remains inconclusive. Therefore, the overall effectiveness of acupuncture therapy in treating post-TKA pain warrants further scrutiny. (8) The majority of the studies included in this review were published in Chinese journals, which introduce a potential publication bias associated with Chinese culture.
In future research, a more detailed examination of various acupuncture therapies should be prioritized by researchers. While numerous studies have examined the mechanism and clinical outcomes of acupuncture in treating postoperative pain following TKA, there is a lack of exploration regarding the efficacy of varying acupoint selection, acupuncture depth, needle retention time, and treatment frequency. Future clinical research should prioritize investigating the regularity of acupoint selection and acupuncture methods in effectively managing postoperative pain in TKA patients and provide theoretical basis of acupuncture for the clinical treatment of postoperative pain. Furthermore, a variety of studies have explored the mechanisms of acupuncture, particularly focusing on signaling pathways and cytokines. However, the majority of studies examining signaling pathways have primarily utilized nodal signaling pathways as their subjects, resulting in a lack of coherence and comprehensiveness. Moreover, the precise signaling pathways underlying the effectiveness of acupuncture in managing postoperative pain following TKA remain inadequately understood, highlighting the necessity for expanded and comprehensive research efforts. Future investigations should integrate proteomics and genomics principles and methodologies to elucidate the specific regulatory mechanisms and distinctive features of acupuncture in TKA postoperative pain management, as well as find new clues for the treatment of TKA postoperative pain through animal studies of acupuncture.
5 Conclusion
The limitations of this study underscore the necessity for future clinical practice to address the following aspects: achieving consensus among clinicians and researchers to harmonize inclusion criteria for patient recruitment, designing study protocols and reporting results in strict adherence to the CONSORT principle, and registering study protocols on reputable registration platforms prior to trial commencement. Additional well-designed, large-sample, multi-centric clinical trials and comprehensive meta-analyses are necessary to further substantiate and enhance the validity of our results.
In general, different acupuncture therapies have advantages in terms of efficacy, safety, and patient compliance. EA + MA and TEAS+MA may be considered as optimal choices for mitigating postoperative pain in patients undergoing TKA, while ACU + MA may be preferable for enhancing postoperative knee function. AAT + MA could be regarded as an effective option for preventing postoperative nausea and vomiting, as well as dizziness and drowsiness. Moreover, the combination of acupuncture-related therapies with multimodal analgesia demonstrates significant overall benefits and safety, thus suggesting the utilization of these therapies in clinical settings.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
NL: Conceptualization, Data curation, Formal analysis, Resources, Software, Writing – original draft, Writing – review & editing. GL: Data curation, Visualization, Writing – review & editing. XC: Data curation, Formal analysis, Funding acquisition, Supervision, Writing – review & editing. YX: Investigation, Resources, Writing – review & editing. YH: Conceptualization, Data curation, Formal analysis, Software, Writing – review & editing. DZ: Methodology, Software, Writing – review & editing. LW: Resources, Supervision, Writing – review & editing. SC: Conceptualization, Funding acquisition, Methodology, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Major Basic research of Natural Science Foundation of Shandong Province (ZR2020ZD17) and Youth Project of Natural Science Foundation of Shandong Province (ZR2023QH041). The funding recipient SC was involved in conceptualizing, reviewing, and revising the manuscript. The funding recipient XC was also involved in the study design and data analysis.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2024.1361037/full#supplementary-material
References
1. Yebin, H, Kun, H, Jun, S, Xinchun, C, Zhenfa, L, Tingyong, L, et al. Epidemiological survey of rheumatoid arthritis among rural minority residents aged 20-79 years in Qiannan Prefecture, Guizhou Province. Mod Preven Med. (2020) 47:5.
2. Zhang, Z, Xing, Q, Zhong, D, Pan, Y, He, T, Hu, Y, et al. The impact of psychological health on patient recovery after arthroplasty front. Psychiatry. (2022) 13:817716. doi: 10.3389/fpsyt.2022.817716
3. Breivik, H. International Association for the Study of Pain: update on WHO-IASP activities. J Pain Symptom Manag. (2002) 24:97–101. doi: 10.1016/s0885-3924(02)00465-7
4. Hudson, TJ, Painter, JT, Martin, BC, Austen, MA, Williams, JS, Fortney, JC, et al. Pharmacoepidemiologic analyses of opioid use among OEF/OIF/OND veterans. Pain. (2017) 158:1039–45. doi: 10.1097/j.pain.0000000000000874
5. Eymir, M, Unver, B, and Karatosun, V. Relaxation exercise therapy improves pain, muscle strength, and kinesiophobia following total knee arthroplasty in the short term: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. (2022) 30:2776–85. doi: 10.1007/s00167-021-06657-x
6. Nanavati, AJ, and Prabhakar, S. Fast-track surgery: toward comprehensive peri-operative care. Anesth Essays Res. (2014) 8:127–33. doi: 10.4103/0259-1162.134474
7. Webber, SC, Strachan, SM, and Pachu, NS. Sedentary behavior, cadence, and physical activity outcomes after knee arthroplasty. Med Sci Sports Exerc. (2017) 49:1057–65. doi: 10.1249/MSS.0000000000001207
8. Longhini, J, Marzaro, C, Bargeri, S, Palese, A, Dell’Isola, A, Turolla, A, et al. Wearable devices to improve physical activity and reduce sedentary behaviour: an umbrella review. Sports Med Open. (2024) 10:9. doi: 10.1186/s40798-024-00678-9
9. World Health Organization. Global action plan on physical activity 2018–2030: more active people for a healthier world. Geneva: World Health Organization (2018).
10. Garcia-Labbé, D, Ruka, E, Bertrand, OF, Voisine, P, Costerousse, O, and Poirier, P. Obesity and coronary artery disease: evaluation and treatment. Can J Cardiol. (2015) 31:184–94. doi: 10.1016/j.cjca.2014.12.008
11. Kahn, TL, and Schwarzkopf, R. Does Total knee arthroplasty affect physical activity levels? Data from the osteoarthritis initiative. J Arthroplast. (2015) 30:1521–5. doi: 10.1016/j.arth.2015.03.016
12. Pischon, T, and Nimptsch, K. Obesity and risk of cancer: an introductory overview. Recent Results Cancer Res. (2016) 208:1–15. doi: 10.1007/978-3-319-42542-9_1
13. Taniguchi, M, Sawano, S, Kugo, M, Maegawa, S, Kawasaki, T, and Ichihashi, N. Physical activity promotes gait improvement in patients with Total knee arthroplasty. J Arthroplast. (2016) 31:984–8. doi: 10.1016/j.arth.2015.11.012
14. Chandrasekaran, S, Ariaretnam, SK, Tsung, J, and Dickison, D. Early mobilization after total knee replacement reduces the incidence of deep venous thrombosis. ANZ J Surg. (2009) 79:526–9. doi: 10.1111/j.1445-2197.2009.04982.x
15. YaDeau, JT, Lin, Y, Mayman, DJ, Goytizolo, EA, Alexiades, MM, Padgett, DE, et al. Pregabalin and pain after total knee arthroplasty: a double-blind, randomized, placebo-controlled, multidose trial. Br J Anaesth. (2015) 115:285–93. doi: 10.1093/bja/aev217
16. Nielsen, NI, Kehlet, H, Gromov, K, Troelsen, A, Husted, H, Varnum, C, et al. High-dose steroids in high pain responders undergoing total knee arthroplasty: a randomised double-blind trial. Br J Anaesth. (2022) 128:150–8. doi: 10.1016/j.bja.2021.10.001
17. Schreiber, KL, Belfer, I, Miaskowski, C, Schumacher, M, Stacey, BR, and van de Ven, T. AAAPT diagnostic criteria for acute pain following breast surgery. J Pain. (2020) 21:294–305. doi: 10.1016/j.jpain.2019.08.008
18. Kehlet, H, and Dahl, JB. The value of “multimodal” or “balanced analgesia” in postoperative pain treatment. Anesth Analg. (1993) 77:1048–56. doi: 10.1213/00000539-199311000-00030
19. Mudumbai, SC, Ganaway, T, Kim, TE, Howard, SK, Giori, NJ, Shum, C, et al. Can bedside patient-reported numbness predict postoperative ambulation ability for total knee arthroplasty patients with nerve block catheters? Korean J Anesthesiol. (2016) 69:32–6. doi: 10.4097/kjae.2016.69.1.32
20. Remeniuk, B, Sukhtankar, D, Okun, A, Navratilova, E, Xie, JY, King, T, et al. Behavioral and neurochemical analysis of ongoing bone cancer pain in rats. Pain. (2015) 156:1864–73. doi: 10.1097/j.pain.0000000000000218
21. Wu, TC, Hsu, CH, Sun, WZ, Chen, HM, Lin, CP, and Shao, YY. Impact of expanded strong opioid availability on opioid prescription patterns in patients with cancer: A population-wide cohort study in Taiwan. Lancet Reg Health West Pac. (2021) 16:100255. doi: 10.1016/j.lanwpc.2021.100255
22. Young, A, and Buvanendran, A. Recent advances in multimodal analgesia. Anesthesiol Clin. (2012) 30:91–100. doi: 10.1016/j.anclin.2011.12.002
23. Váradi, A, Marrone, GF, Palmer, TC, Narayan, A, Szabó, MR, le Rouzic, V, et al. Mitragynine/corynantheidine pseudoindoxyls as opioid analgesics with mu agonism and delta antagonism, which do not recruit β-Arrestin-2. J Med Chem. (2016) 59:8381–97. doi: 10.1021/acs.jmedchem.6b00748
24. Wang, L, Song, L, and Han, WF. Comparison of posterior cruciate ligament retention and resection in total knee arthroplasty. J Capital Med Univ. (2017) 38:4. doi: 10.3969/j.issn.1006-7795.2017.06.026
25. Wang, CL. Comparative study of total knee arthroplasty with and without preservation of posterior cruciate ligament. Jilin: Jilin University. (2019).
26. de Oliveira Silva, D, Webster, KE, Feller, JA, and McClelland, JA. Anterior knee pain following primary unilateral total knee arthroplasty with posterior-stabilized prosthesis and patellar resurfacing: prevalence and clinical implications. J Arthroplast. (2023) 38:281–5. doi: 10.1016/j.arth.2022.08.042
27. White, PB, Turcan, S, Satalich, JR, Ranawat, AS, and Ranawat, CS. Clinical outcomes of a modern Total knee arthroplasty prosthesis compared to its predecessor at 5-year follow-up: matched pair analysis. J Arthroplast. (2020) 35:3150–5. doi: 10.1016/j.arth.2020.06.024
28. Maistrello, LF, Rossettini, G, and Zambito, A. Clinical and functional results of Optetrack™ Total knee arthroplasty after 6 to 13 years: findings from a retrospective study. Adv Rehabil. (2023) 37:40–8. doi: 10.5114/areh.2023.126056
29. Qiao, L, Guo, M, Qian, J, Xu, B, Gu, C, and Yang, Y. Research advances on acupuncture analgesia. Am J Chin Med. (2020) 48:245–58. doi: 10.1142/S0192415X20500135. Epub 2020 Mar 5
30. Cai, M, Lee, JH, and Yang, EJ. Electroacupuncture attenuates cognition impairment via anti-neuroinflammation in an Alzheimer’s disease animal model. J Neuroinflammation. (2019) 16:264. doi: 10.1186/s12974-019-1665-3
31. da Silva, MD, Bobinski, F, Sato, KL, Kolker, SJ, Sluka, KA, and Santos, ARS. IL−10 cytokine released from M2 macrophages is crucial for analgesic and anti-inflammatory effects of acupuncture in a model of inflammatory muscle pain. Mol Neurobiol. (2015) 51:19–31. doi: 10.1007/s12035-014-8790-x
32. Nielsen, A, Gereau, S, and Tick, H. Risks and safety of extended auricular therapy: a review of reviews and case reports of adverse events. Pain Med. (2020) 21:1276–93. doi: 10.1093/pm/pnz379
33. Hong, Z, Lihua, S, and Xuhong, J. Therapeutic effect of auricular point pressing combined with oral Jiawei Tongqiao Huoxue decoction on headache after traumatic brain injury. Zhejiang J Integr Tradit Western Med. (2020) 30:3.
34. Rui, L, Yan, L, Mengmeng, W, Dianhui, Y, et al. Treatment of qi stagnation and blood stasis type menstrual migraine with auricular point sticking and pressure and its effect on serum E2 and 5-HT. Chinese Acupunct. (2023) 43:427–431+436. doi: 10.13703/j.0255-2930.20221008-k0009
35. Lu, W, Giobbie-Hurder, A, Freedman, RA, Shin, IH, Lin, NU, Partridge, AH, et al. Acupuncture for chemotherapy-induced peripheral neuropathy in breast Cancer survivors: a randomized controlled pilot trial. Oncologist. (2020) 25:310–8. doi: 10.1634/theoncologist.2019-0489
36. Li, YY, Yin, CY, Li, XJ, Liu, B, Wang, J, Zheng, X, et al. Electroacupuncture alleviates paclitaxel-induced peripheral neuropathic pain in rats via suppressing TLR4 signaling and TRPV1 upregulation in sensory neurons. Int J Mol Sci. (2019) 20:5917. doi: 10.3390/ijms20235917
37. Songpo, S, Xisheng, W, and Bin, F. Research progress in the analysis of pain causes and pain prediction models after total knee arthroplasty. Chin J Orthop. (2018) 38:7. doi: 10.3760/cma.j.issn.0253-2352.2018.17.008
38. Han, JS. Acupuncture: neuropeptide release produced by electrical stimulation of different frequencies. Trends Neurosci. (2003) 26:17–22. doi: 10.1016/s0166-2236(02)00006-1
39. Li, X, Zhu, Y, Sun, H, Shen, Z, Sun, J, Xiao, S, et al. Electroacupuncture inhibits pain memory and related anxiety-like behaviors by blockading the GABAB receptor function in the midcingulate cortex. Mol Neurobiol. (2023) 60:6613–26. doi: 10.1007/s12035-023-03467-9
40. Yan, L, Pei, W, Donghuan, D, Wei, Y, Lei, L, Hongjiang, J, et al. Meta-analysis of Electroacupuncture intervention for pain after Total knee arthroplasty. Chinese J Tissue Eng Res. (2021) 25:957–63.
41. Petersen, T, Hautopp, H, Duus, B, and Juhl, C. No effect of acupuncture as adjunctive therapy for patients with total knee replacement: a randomized controlled trial. Pain Med. (2018) 19:1280–9. doi: 10.1093/pm/pnx317
42. Hutton, B, Salanti, G, Caldwell, D, Chaimani, A, Schmid, CH, Cameron, C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. (2015) 162:777–84. doi: 10.7326/m14-2385
43. Wang, X, Chen, Y, Liu, Y, Yao, L, Estill, J, Bian, Z, et al. Reporting items for systematic reviews and meta-analyses of acupuncture: the PRISMA for acupuncture checklist. BMC Complement Altern Med. (2019) 19:208. doi: 10.1186/s12906-019-2624-3
44. Chinese Orthopaedic Association. Guideline for the diagnosis and treatment of osteoarthritis (2007 edition). Chin J Orthop Surg. (2014) 22:2. doi: 10.3760/j.issn:0253-2352.2007.10.016
45. Leung, K, Zhang, B, Tan, J, Shen, Y, Geras, KJ, Babb, JS, et al. Prediction of total knee replacement and diagnosis of osteoarthritis by using deep learning on knee radiographs: data from the osteoarthritis initiative. Radiology. (2020) 296:584–93. doi: 10.1148/radiol.2020192091
46. Madry, H. Surgical therapy in osteoarthritis. Osteoarthr Cartil. (2022) 30:1019–34. doi: 10.1016/j.joca.2022.01.012
47. Yan, T, Chen, W, Feng, Z, Jin, DM, Shi, XE, He, XK, et al. Rehabilitation treatment guide. Beijing: People’s Medical Publishing House (2011). 468 p.
48. Li, L, Liu, X, and Herr, K. Postoperative pain intensity assessment: a comparison of four scales in Chinese adults. Pain Med. (2007) 8:223–34. doi: 10.1111/j.1526-4637.2007.00296.x
49. Ip, D. Orthopedic rehabilitation, assessment, and enablement. Berlin, Heidelberg: Springer. (2007).
50. Meng, Z, Liu, J, and Zhou, N. Comparison between Jadad scale and Cochrane collaboration’s tool for assessing risk of bias on the quality and risk of bias evaluation in randomized controlled trials. Arch Orthop Trauma Surg. (2023) 143:409–21. doi: 10.1007/s00402-021-04326-9
51. Higgins, J, and Green, S. Cochrane handbook for systematic reviews of interventions: the cochrane collaboration. (2008). Available at: http://www.cochrane.org/training/cochrane-handbook
52. Zhang, C, Yan, JZ, Sun, F, Liu, Q, Guo, Y, Zeng, XT, et al. Differentiation and handling of homogeneity in network meta-analysis. Chin J Evid Based Med. (2014) 14:884–8. doi: 10.7507/1672-2531.20140146
53. Chaimani, A, Higgins, J, Mavridis, D, Spyridonos, P, and Salanti, G. Graphical tools for network meta-analysis in STATA. PLoS One. (2013) 8:e76654. doi: 10.1371/journal.pone.0076654
54. Salanti, G, Ades, A, and Ioannidis, J. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. (2011) 64:163–71. doi: 10.1016/j.jclinepi.2010.03.016
55. Chen, CC, Yang, CC, Hu, CC, Shih, HN, Chang, YH, and Hsieh, PH. Acupuncture for pain relief after total knee arthroplasty: a randomized controlled trial. Reg Anesth Pain Med. (2015) 40:31–6. doi: 10.1097/AAP.0000000000000138
56. Tsang, RC, Tsang, PL, Ko, CY, Kong, BCH, Lee, WY, and Yip, HT. Effects of acupuncture and sham acupuncture in addition to physiotherapy in patients undergoing bilateral total knee arthroplasty--a randomized controlled trial. Clin Rehabil. (2007) 21:719–28. doi: 10.1177/0269215507077362
57. Tzeng, CY, Chang, SL, Wu, CC, Chang, CL, Chen, WG, Tong, KM, et al. Single-blinded, randomised preliminary study evaluating the effects of 2 Hz electroacupuncture for postoperative pain in patients with total knee arthroplasty. Acupunct Med. (2015) 33:284–8. doi: 10.1136/acupmed-2014-010722
58. Peijian, T, Haidong, W, Zhenchuan, M, Weifeng, J, Ju, L, Tao, P, et al. Application and curative effect observation of auricular point therapy in perioperative analgesia of total knee arthroplasty. Chinese J Integ Tradit Western Med. (2010) 30:931–4.
59. Zhihua, Y. Effect of auricular point sticking on postoperative subjective experience in patients with total knee arthroplasty. Clin Res Tradit Chinese Med. (2015) 34:134–6. doi: 10.3969/j.issn.1674-7860.2015.34.071
60. Shengjuan, Z. Application of auricular point sticking combined with celecoxib for preemptive analgesia in total knee arthroplasty. Shanghai J Acupuncture Moxibust. (2015) 34:3. doi: 10.13460/j.issn.1005-0957.2015.02.0134
61. Weiwei, K, Julan, L, Fan, L, Leilei, A, Junhong, Z, Junqiang, T, et al. Study on the efficacy of auricular point sticking in acute pain and early rehabilitation after total knee arthroplasty. West China J Tradit Chinese Med. (2020). doi: 10.12174/j.issn.1004-6852.2020.12.30
62. Guiju, D, Wenying, Z, and Yiqin, Y. Clinical study on the efficacy of auricular point application in the treatment of pain after total knee arthroplasty. Inner Mongolia J Tradit Chinese Med. (2020) 39:108–10.
63. Liang, Y, Yongqiang, S, and Xiaoze, S. Clinical study on auricular point pressing for preventing pain sensitivity after knee arthroplasty. J Clin Tradit Chinese Med. (2014) 12:2.
64. Weihua, Z, Lingyun, G, Mingjun, L, Yong, Z, Kaihao, M, Yonglin, Z, et al. Effect of auricular point application assisted analgesia on lower limb pain and knee function after primary total knee arthroplasty. Asia Pac J Tradit Med. (2023) 19:88–93.
65. Yang, F. Clinical efficacy observation of auricular point application in postoperative analgesia after total knee arthroplasty. Fuzhou: Fujian University of Traditional Chinese Medicine (2017).
66. He, BJ, Tong, PJ, Li, J, Jing, HT, and Yao, XM. Auricular acupressure for analgesia in perioperative period of total knee arthroplasty. Pain Med. (2013) 14:1608–13. doi: 10.1111/pme.12197
67. Jinfa, W, Hangxing, B, Yunhuo, C, Jianhua, Z, and Peijian, T. Clinical application of ear acupuncture analgesia during perioperative period of total knee arthroplasty. J TCM Bonesetting. (2012) 24:4.
68. Penghui, Z, Peng, L, Huizhou, L, Wang Mingjie, W, Shuang, Z, Zhao, L, et al. Effects of transcutaneous electrical acupoint stimulationon patient-controlled intravenous analgesia in elderly patients after total knee arthroplasty. J Clin Anesthesiol. (2019) 3:4.
69. Yuliu, C, Peiwen, L, Xinxiao, L, Yifei, W, Weidong, S, Ying, C, et al. Clinical study on the efficacy of percutaneous electricalacupoint stimulation for postoperative analgesia and plasma β-endorphin levels in patients after total knee arthroplasty. Modern Chinese Med Clin. (2021) 28:14–8.
70. Tianyu, B, Jiaming, Q, Zige, L, Yifei, W, Guannan, W, Peiwen, L, et al. Effects of transcutaneous electrical acupoint stimulation on the efficacy of adjuvant analgesia and plasma β-endorphin in patients after total knee arthroplasty. Chinese J Tradit Chinese Med Inform. (2023) 30:141–5. doi: 10.19879/j.cnki.1005-5304.202206544
71. Xu, YL, Sun, YS, Wei, YF, Bai, TY, Wang, HJ, Zeng, LQ, et al. Effects of transcutaneous electrical acupoint stimulation on early response after total knee arthroplasty. Chinese Journal of Orthopaedic Surgery. (2023) 31:2104–8.
72. Cong-rui, W, Jian-xin, Y, Zi-jian, C, Zhi-shou, M, Lei, G, Sun, Q, et al. Effects of percutaneous acupoint electrical stimulation assisted multimodal analgesia on postoperative rehabilitation in elderly patients undergoing total knee arthroplasty. Chinese J Pharm Clin. (2021) 21:3507–10. doi: 10.11655/zgywylc2021.21.002
73. Zhongqing, W, Kanna, X, Jingjun, X, Song Junyang, S, Guofeng, Y, Dan, W, et al. Clinical study on the improvement of pain after total knee arthroplasty by percutaneous electrical acupoint stimulation. J Shandong Univ Tradit Chinese Med. (2017) 41:244–6. doi: 10.16294/j.cnki.1007-659x.2017.03.015
74. Gang, C, Ruixin, G, and Dandan, X. Application of electroacupuncture therapy in rehabilitation after total knee arthroplasty. Chinese Acupunct. (2012) 32:309–12. doi: 10.3969/j.issn.1672-7002.2006.07.017
75. Wenxing, L. Therapeutic effect observation of electroacupuncture on analgesia after total knee arthroplasty. Guangzhou: Guangzhou University of Chinese Medicine (2013).
76. Dong, S. Clinical efficacy analysis and experimental study of electroacupuncture on analgesia after total knee arthroplasty. Guangzhou: Guangzhou University of Chinese Medicine (2018).
77. Sheng, Z. Clinical efficacy and supraspinal mechanism of electroacupuncture for acute pain after total knee arthroplasty Shanghai University of Traditional Chinese Medicine (2021).
78. Chao, G. Clinical observation of electroacupuncture for pain after total knee arthroplasty. Jinan: Shandong University of Traditional Chinese Medicine (2023).
79. Yong, Y, Jiheng, Y, and Li, H. Effect of electroacupuncture at affected limb acupoints on postoperative pain and rehabilitation after TKA. World Latest Med Inform Digest. (2017) 17:3.
80. Da, C, Dong, S, Jingli, X, Yangyue, Z, Tianye, L, Qingwen, Z, et al. Effect of electroacupuncture on postoperative pain and activity limitation after total knee arthroplasty. Chinese J Acupunct Moxibustion. (2019) 39:247–50. doi: 10.13703/j.0255-2930.2019.03.006
81. Junteng, Z. Study on the effect of electroacupuncture on pain and activity limitation after total knee arthroplasty. Fuzhou: Fujian University of Traditional Chinese Medicine (2014).
82. Bingxin, K, Lianbo, X, Chi, Z, Hui, X, Sheng, Z, Chenxin, G, et al. Effect of electroacupuncture combined with celecoxib on pain after total knee arthroplasty. Chinese J Integr Tradit Western Med. (2022) 42:1169–74.
83. Xiang, J, Zhang, Y, Wu, J, Shui, Y, and Zhu, Y. Electroacupuncture combined with continuous adductor canal block for postoperative analgesia in patients undergoing total knee arthroplasty. Zhongguo Zhen Jiu. (2023) 44:57–61. doi: 10.13703/j.0255-2930.20230418-0003
84. Zequan, L, Yang, L, Yong, H, and Xinglong, W. Clinical study of Dong’s special acupoint combined with cheek acupuncture for perioperative multimodal analgesia after total knee arthroplasty. J Acupunct Moxibust. (2023) 39:29–33. doi: 10.19917/j.cnki.1005-0779.023173
85. Yi, Z, Yuchan, Z, and Xuemei, X. Therapeutic effect of Feijing-Zhuyu acupuncture on lower limb swelling after total knee arthroplasty. Liaoning J Tradit Chinese Med. (2019) 46:1045–8. doi: 10.13192/j.issn.1000-1719.2019.05.049
86. Piaopiao, C, Wenpeng, X, Wenxue, L, Bing, Y, and Hongming, Q. Clinical study of transcutaneous electrical acupoint stimulation in improving pain after artificial total knee arthroplasty. J Mod Integr Tradit Western Med. (2020) 29:5. doi: 10.3969/j.issn.1008-8849.2020.31.009
87. Chenghao, M, Hai, H, Ruonan, L, Zuohai, T, Hao, W, Zhixing, N, et al. Clinical study of electroacupuncture at the same name of hand and foot for pain after total knee arthroplasty. Chinese J Tissue Eng Res. (2021) 25:5798–803.
88. Haiping, Z. Effect of knee acupuncture on patients after total knee arthroplasty. China Minkang Med. (2022) 34:109–12.
89. Yonghui, Z, Lin, Z, and Min, L. Intervention of meridian-guided acupuncture combined with femoral nerve block on analgesia and functional rehabilitation after knee arthroplasty: a randomized controlled study. Chinese J Acupunct Moxibust. (2018) 38:251–5. doi: 10.13703/j.0255-2930.2018.03.006
90. Wanlu, L, Xinrong, G, Yang, G, Xu, Q, Zhenyu, L, Wei, Z, et al. Effects of acupuncture combined with CPM machine on joint function rehabilitation after total knee arthroplasty. J Mod Integr Tradit Western Med. (2021). doi: 10.3969/j.issn.1008-8849.2021.22.007
91. Dejin, W. Effects of acupuncture combined with femoral nerve block on knee joint function in patients after knee arthroplasty. J Zhejiang Integr Tradit Western Med. (2019) 29:2.
92. Jiaqun, Z, Bo, C, and Jinquan, X. Effects of acupuncture combined with nerve block on analgesic effect and early joint functional recovery in patients with knee arthroplasty. New Chinese Med. (2022) 54:192–5. doi: 10.13457/j.cnki.jncm.2022.07.045
93. Rongzhen, L, Danchun, L, and Shichang, H. Effect of acupuncture at Siguan combined with celecoxib on perioperative preemptive analgesia in patients undergoing total knee arthroplasty. Chinese J Geriatr. (2019) 39:3688–90. doi: 10.3969/j.issn.1005-9202.2019.15.028
94. Zongwen, L, Li, H, Xinyan, T, and Shangxian, S. Clinical study on the analgesic effect of acupuncture at Siguan point combined with xi-cleft point after total knee arthroplasty. Rheumatol Arthritis. (2021) 10:13–6.
95. Tedesco, D, Gori, D, Desai, KR, Asch, S, Carroll, IR, Curtin, C, et al. Drug-free interventions to reduce pain or opioid consumption after total knee arthroplasty: a systematic review and meta-analysis. JAMA Surg. (2017) 152:e172872. doi: 10.1001/jamasurg.2017.2872
96. Wulf, G. Attentional focus and motor learning: a review of 15 years. Int Rev Sport Exerc Psychol. (2013) 6:77–104. doi: 10.1080/1750984X.2012.723728
97. Jazaeri, SZ, Azad, A, Mehdizadeh, H, Habibi, SA, Mandehgary Najafabadi, M, Saberi, ZS, et al. The effects of anxiety and external attentional focus on postural control in patients with Parkinson’s disease. PLoS One. (2018) 13:e0192168. doi: 10.1371/journal.pone.0192168
98. Piccoli, A, Rossettini, G, Cecchetto, S, Viceconti, A, Ristori, D, Turolla, A, et al. Effect of attentional focus instructions on motor learning and performance of patients with central nervous system and musculoskeletal disorders: a systematic review. J Funct Morphol Kinesiol. (2018) 3:40. doi: 10.3390/jfmk3030040
99. Yanchun, S. Analysis of the impact of early rehabilitation training on joint function recovery after total knee replacement. Chinese Med Guide. (2017) 15:124–5. doi: 10.15912/j.cnki.gocm.2017.28.099
100. Ruiting, W, Li, J, Jinhua, Z, Shaowei, C, Cuicui, G, Qing, C, et al. Effect of perioperative rehabilitation after artificial knee replacement. Qilu Med J. (2009) 24:253–5.
101. Rossettini, G, Testa, M, Vicentini, M, and Manganotti, P. The effect of different attentional focus instructions during finger movement tasks in healthy subjects: an exploratory study. Biomed Res Int. (2017) 2017:2946465–7. doi: 10.1155/2017/2946465
102. Pinto, PR, McIntyre, T, Ferrero, R, Almeida, A, and Araújo-Soares, V. Predictors of acute postsurgical pain and anxiety following primary total hip and knee arthroplasty. J Pain. (2013) 14:502–15. doi: 10.1016/j.jpain.2012.12.020
103. Xiaowei, X, Chen, Y, Pengde, K, Zongke, Z, Jing, Y, Bin, S, et al. Analysis of related factors for acute pain after primary total knee arthroplasty under enhanced recovery after surgery mode. Chinese J Orthopaed Arthrit Surg. (2016) 9:4. doi: 10.3969/j.issn.2095-9958.2016.06-10
104. Caixia, G, and Li, G. Analysis of the causes of long-term joint pain after artificial total knee arthroplasty. Chinese Med Clin. (2020) 20:2. doi: 10.11655/zgywylc2020.02.027
105. Zhou, YF, Ying, XM, He, XF, Shou, SY, Wei, JJ, Tai, ZX, et al. Suppressing PKC-dependentmembrane P2X3 receptor upregulation in dorsal root gangliamediated electroacupuncture analgesia in rat painful diabeticneuropathy. PurinergicSignal. (2018) 14:359–69. doi: 10.1007/s11302-018-9617-4
106. Zhang, XH, Feng, CC, Pei, LJ, Zhang, YN, Chen, L, Wei, XQ, et al. Electroacupuncture attenuates neuropathic pain and comorbid negative behavior: the involvement of the dopamine system in the amygdala. Front Neurosci. (2021) 15:657507. doi: 10.3389/fnins.2021.657507
107. Fang, JQ, du, JY, Fang, JF, Xiao, T, Le, XQ, Pan, NF, et al. Parameter-specific analgesic effects of electroacupuncture mediated by degree of regulation TRPV1 and P2X3 in inflammatory pain in rats. Life Sci. (2018) 200:69–80. doi: 10.1016/j.lfs.2018.03.028
108. Xiao, J, Wei, W, Yaqi, W, Xueqin, L, Ying, Z, Xiaohui, L, et al. Research progress on analgesic mechanism of auricular point pressing with beans. Guangming Chinese Med. (2022) 37:3306–8.
109. Yujie, G, Haifa, Q, Qiang, W, Jie, L, Gang, L, Yuan, W, et al. To explore the clinical significance of acupuncture at distant acupoints for meridian tendon diseases based on body surface-body surface correlation. Chinese J Tradit Chinese Med. (2022) 37:5730–4.
110. Shuyi, C, Junhui, W, and Jiaxin, Z. Observation on the rehabilitation efficacy of acupuncture exercise therapy and isokinetic muscle strength training after arthroscopic meniscectomy. Chinese Acupunct. (2023) 43:1118–22. doi: 10.13703/j.0255-2930.20221228-0002
111. Kean, CO, Hinman, RS, Wrigley, TV, Lim, BW, and Bennell, KL. Impact loading following quadriceps strength training in individuals with medial knee osteoarthritis and varus alignment. Clin Biomech. (2017) 42:20–4. doi: 10.1016/j.clinbiomech.2017.01.002
112. Haggard, P, Iannetti, GD, and Longo, MR. Spatial sensory organization and body representation in pain perception. Curr Biol. (2013) 23:R164–76. doi: 10.1016/j.cub.2013.01.047
113. Viceconti, A, Camerone, EM, Luzzi, D, Pentassuglia, D, Pardini, M, Ristori, D, et al. Explicit and implicit own’s body and space perception in painful musculoskeletal disorders and rheumatic diseases: a systematic scoping review. Front Hum Neurosci. (2020) 14:83. doi: 10.3389/fnhum.2020.00083
114. Gu, L, Gong, W, Zhang, J, Chen, W, and Guo, J. The impact of the illusion of body ownership on pain and its mechanism. Prog Psychol Sci. (2022) 30:2518–28. doi: 10.3724/SP.J.1042.2022.02518
115. Park, JY, Park, JJ, Jeon, S, Doo, AR, Kim, SN, Lee, H, et al. From peripheral to central: the role of ERK signaling pathway in acupuncture analgesia. J Pain. (2014) 15:535–49. doi: 10.1016/j.jpain.2014.01.498
116. Jung, WM, Lee, IS, Wallraven, C, Ryu, YH, Park, HJ, and Chae, Y. Cortical activation patterns of bodily attention triggered by acupuncture stimulation. Sci Rep. (2015) 5:12455. doi: 10.1038/srep12455
117. Menon, V, and Uddin, LQ. Saliency, switching, attention and control: a network model of insula function. Brain Struct Funct. (2010) 214:655–67. doi: 10.1007/s00429-010-0262-0
118. Craig, AD. Significance of the insula for the evolution of human awareness of feelings from the body. Ann N Y Acad Sci. (2011) 1225:72–82. doi: 10.1111/j.1749-6632.2011.05990.x
119. Petrovic, P, Kalso, E, Petersson, KM, and Ingvar, M. Placebo and opioid analgesia-- imaging a shared neuronal network. Science. (2002) 295:1737–40. doi: 10.1126/science.1067176
120. Zeng, X, Wang, H, and Li, L. Research on the efficacy of acupuncture combined with proprioception training on knee osteoarthritis. Massage Rehabil Med. (2022) 13:17–21. doi: 10.19787/j.issn.1008-1879.2022.21.005
121. Jeong, HS, Lee, SC, Jee, H, Song, JB, Chang, HS, and Lee, SY. Proprioceptive training and outcomes of patients with knee osteoarthritis: a meta-analysis of randomized controlled trials. J Athl Train. (2019) 54:418–28. doi: 10.4085/1062-6050-329-17
122. Wang, Y, Chen, Y, Meng, L, Wu, B, Ouyang, L, Peng, R, et al. Electro-acupuncture treatment inhibits the inflammatory response by regulating γδ T and Treg cells in ischemic stroke. Exp Neurol. (2023) 362:114324. doi: 10.1016/j.expneurol.2023.114324
123. Koog, YH. Effect of placebo acupuncture over no-treatment: a simple model incorporating the placebo and nocebo effects. Complement Ther Med. (2016) 24:69–72. doi: 10.1016/j.ctim.2015.12.007
124. Wand, BM, Abbaszadeh, S, Smith, AJ, Catley, MJ, and Moseley, GL. Acupuncture applied as a sensory discrimination training tool decreases movement-related pain in patients with chronic low back pain more than acupuncture alone: a randomised cross-over experiment. Br J Sports Med. (2013) 47:1085–9. doi: 10.1136/bjsports-2013-092949
126. Zhang, Q, Zhou, M, Huo, M, Si, Y, Zhang, Y, Fang, Y, et al. Mechanisms of acupuncture-electroacupuncture on inflammatory pain. Mol Pain. (2023) 19:17448069231202882. doi: 10.1177/17448069231202882
127. Bingel, U, and Tracey, I. Imaging CNS modulation of pain in humans. Physiology. (2008) 23:371–80. doi: 10.1152/physiol.00024.2008
128. Wager, TD, Rilling, JK, Smith, EE, Sokolik, A, Casey, KL, Davidson, RJ, et al. Placebo-induced changes in FMRI in the anticipation and experience of pain. Science. (2004) 303:1162–7. doi: 10.1126/science.1093065
129. Zou, K, Wong, J, Abdullah, N, Chen, X, Smith, T, Doherty, M, et al. Examination of overall treatment effect and the proportion attributable to contextual effect in osteoarthritis: meta-analysis of randomised controlled trials. Ann Rheum Dis. (2016) 75:1964–70. doi: 10.1136/annrheumdis-2015-208387
130. Sellmeijer, J, Mathis, V, Hugel, S, Li, XH, Song, Q, Chen, QY, et al. Hyperactivity of anterior cingulate cortex areas 24a/24b drives chronic pain-induced Anxiodepressive-like consequences. J Neurosci. (2018) 38:3102–15. doi: 10.1523/JNEUROSCI.3195-17.2018
131. Zou, X, Zhang, J, and Wang, G. Role of NR2B in rostal anterior cingulate cortex in development of pain-related aversion in a rat model of bone cancer pain: siRNA technique. Chinese J Anesthesiol. (2018) 12:1086–9. doi: 10.3760/cma.j.issn.0254-1416.2018.09.016
132. Tang, Y, and Zhang, Y. The molecular mechanism of the NMDA receptor-MAPK-CREB pathway in the anterior cingulate cortex involved in pain aversion. Acta Physiol Sin. (2017) 69:637–46. doi: 10.13294/j.aps.2017.0055
133. Cook, CE, Bailliard, A, Bent, JA, Bialosky, JE, Carlino, E, Colloca, L, et al. An international consensus definition for contextual factors: findings from a nominal group technique. Front Psychol. (2023) 14:1178560. doi: 10.3389/fpsyg.2023.1178560
134. Chae, Y, Lee, YS, and Enck, P. How placebo needles differ from placebo pills? Front Psych. (2018) 9:243. doi: 10.3389/fpsyt.2018.00243
135. Vickers, AJ, Vertosick, EA, Lewith, G, MacPherson, H, Foster, NE, Sherman, KJ, et al. Acupuncture for chronic pain: update of an individual patient data meta-analysis. J Pain. (2018) 19:455–74. doi: 10.1016/j.jpain.2017.11.005
136. Wager, TD, and Atlas, LY. The neuroscience of placebo effects: connecting context, learning and health. Nat Rev Neurosci. (2015) 16:403–18. doi: 10.1038/nrn3976
137. Geuter, S, Koban, L, and Wager, TD. The cognitive neuroscience of placebo effects: concepts, predictions, and physiology. Annu Rev Neurosci. (2017) 40:167–88. doi: 10.1146/annurev-neuro-072116-031132
138. Schafer, SM, Geuter, S, and Wager, TD. Mechanisms of placebo analgesia: a dual-process model informed by insights from cross-species comparisons. Prog Neurobiol. (2018) 160:101–22. doi: 10.1016/j.pneurobio.2017.10.008
139. Rossettini, G, Colombi, A, Carlino, E, Manoni, M, Mirandola, M, Polli, A, et al. Unraveling negative expectations and nocebo-related effects in musculoskeletal pain. Front Psychol. (2022) 13:789377. doi: 10.3389/fpsyg.2022.789377
140. Zhao, SS, Duffield, SJ, and Goodson, NJ. The prevalence and impact of comorbid fibromyalgia in inflammatory arthritis. Best Pract Res Clin Rheumatol. (2019) 33:101423. doi: 10.1016/j.berh.2019.06.005
141. Alciati, A, Nucera, V, Masala, IF, Giallanza, M, La Corte, L, Giorgi, V, et al. One year in review 2021: fibromyalgia. Clin Exp Rheumatol. (2021) 39:3–12. doi: 10.55563/clinexprheumatol/gz4i3i
142. Viceconti, A, Geri, T, De Luca, S, Maselli, F, Rossettini, G, Sulli, A, et al. Neuropathic pain and symptoms of potential small-fiber neuropathy in fibromyalgic patients: a national on-line survey. Joint Bone Spine. (2021) 88:105153. doi: 10.1016/j.jbspin.2021.105153
143. Li, D, Song, X, Li, Z, Liao, L, Zhu, Y, et al. Combination of Shenmen and Sanyinjiao acupoints improves anxiety and depression in patients with insomnia: a randomized controlled study. Chinese Acupunct. (2022) 42:13–7. doi: 10.13703/j.0255-2930.20210113-k0002
144. Liang, L, Yang, L, and Fan, X. Research on the molecular biological effect mechanism of acupuncture Zusanli. Int J Tradit Chinese Med. (2020) 42:5. doi: 10.3760/cma.j.cn115398-20190423-00155
145. Xiao, X, Chen, W, and Ansheng, Y. The mechanism of acupuncture anesthesia in thyroid surgery. Chinese J Tradit Chinese Med. (2022) 37:3.
146. Li, B. fMRI study on the brain effect mechanism of acupuncture at Taichong and Ligou groups Heilongjiang University of Traditional Chinese Medicine. (2021).
Keywords: acupuncture therapy, total knee arthroplasty (TKA), pain management, alternative therapies, network meta-analysis (NMA), randomized controlled trials
Citation: Liu N, Liu G, Chang X, Xu Y, Hou Y, Zhang D, Wang L and Chen S (2024) Combining various acupuncture therapies with multimodal analgesia to enhance postoperative pain management following total knee arthroplasty: a network meta-analysis of randomized controlled trials. Front. Neurol. 15:1361037. doi: 10.3389/fneur.2024.1361037
Edited by:
Guanhu Yang, Ohio University, United StatesReviewed by:
José Aparecido Da Silva, University of Brasilia, BrazilGiacomo Rossettini, University of Verona, Italy
Ke Xu, Chongqing University, China
Copyright © 2024 Liu, Liu, Chang, Xu, Hou, Zhang, Wang and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shaozong Chen, Y2NzejE5NjNAMTYzLmNvbQ==
 Ningning Liu
Ningning Liu Gaihong Liu1
Gaihong Liu1 Xiaoli Chang
Xiaoli Chang