
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Neurol. , 10 April 2024
Sec. Epilepsy
Volume 15 - 2024 | https://doi.org/10.3389/fneur.2024.1337960
Poststroke seizure is a potential complication of stroke, which is the most frequent acute symptomatic seizure in adults. Patients with stroke may present with an abnormal or aggressive behavior accompanied by altered mental status and symptoms, such as hemiparesis, dysarthria, and sensory deficits. Although stroke manifestations that mimic seizures are rare, diagnosing poststroke seizures can be challenging when accompanied with negative postictal symptoms. Differential diagnoses of poststroke seizures include movement disorders, syncope, and functional (nonepileptic) seizures, which may present with symptoms similar to seizures. Furthermore, it is important to determine whether poststroke seizures occur early or late. Seizures occurring within and after 7 d of stroke onset were classified as early and late seizures, respectively. Early seizures have the same clinical course as acute symptomatic seizures; they rarely recur or require long-term antiseizure medication. Conversely, late seizures are associated with a risk of recurrence similar to that of unprovoked seizures in a patient with a focal lesion, thereby requiring long-term administration of antiseizure medication. After diagnosis, concerns regarding treatment strategies, treatment duration, and administration of primary and secondary prophylaxis often arise. Antiseizure medication decisions for the initiation of short-term primary and long-term secondary seizure prophylaxis should be considered for patients with stroke. Antiseizure drugs such as lamotrigine, carbamazepine, lacosamide, levetiracetam, phenytoin, and valproate may be administered. Poststroke seizures should be diagnosed systematically through history with differential diagnosis; in addition, classifying them as early or late seizures can help to determine treatment strategies.
The incidence of stroke has increased by 50% over the past two decades, with a 70% increased incidence from 1990 to 2019 (1). Poststroke seizures are important complications of stroke, as the risks of mortality and morbidity are higher in stroke patients who experience seizure than in those who do not (2). In the past, poststroke seizures accounted for approximately 16% of all seizures; however, with the increasing incidence of stroke, a recent study indicated that 73% of acute symptomatic seizures in individuals >18 years of age are associated with stroke (3, 4). Late poststroke seizures tend to progress to poststroke epilepsy, with a recurrence rate of 71.5% within 10 years, necessitating the administration of antiseizure medications (5). The incidence of poststroke epilepsy was 6.4 and 12.4% in ischemic and hemorrhagic strokes, respectively, based on the analysis of over 100,000 stroke cases in the United Kingdom and Sweden (6, 7). However, the predictive factors for poststroke seizures are not well-established, and elucidating them is difficult owing to other causes of seizures besides stroke.
Differential diagnosis is crucial because patients with stroke often have comorbidities and may present with symptoms similar to poststroke seizures. This could be attributed to the aggressive or abnormal behavior observed in patients with stroke, accompanied with altered mental status and delirious conditions, abnormal movement disorders, and autonomic dysfunction, as well as relatively well-known neurological deficits, such as unilateral weakness, dysarthria, and sensory deficits, which depend on disease severity and stroke location. Epileptic seizures accompanied with negative postictal symptoms may mimic stroke, making diagnosis difficult (3). After diagnosis of poststroke seizures, concerns exist regarding the type of antiseizure medication (ASM) to be administered, duration of administration, and use of ASM to prevent recurrent seizures.
Stroke incidence has risen over the last few decades, and with post-stroke seizures being a complication with impacts on morbidity, mortality, and treatment, an understanding of the definition, diagnostic evaluation, treatment, and future study directions of post-stroke seizures and epilepsy is warranted.
Acute symptomatic seizures due to stroke are closely related to the location and severity of brain damage; therefore, a causal relationship should be inferred if the brain lesion causing the seizures is clearly identified and the seizure occurs with close temporal continuity (8). Some previous studies set 7 d after stroke as the threshold for distinguishing between early and late seizures, whereas others determined 14 d after stroke as the threshold (Table 1). The International League against Epilepsy (ILAE) classifies poststroke seizures into early and late seizures using a 7-d threshold; under this classification, seizures occurring within and after 7 d of stroke onset are classified as early and late seizures, respectively (Table 1) (16). Accordingly, the incidences of early and late seizures were 3–6 and 12%, respectively (9, 17, 18). Early seizures are characterized by increased inflammatory responses, changes in neuronal signaling related to protein synthesis, and increased excitatory neurotransmitter (glutamate) release, ionic imbalance, blood–brain barrier (BBB) permeability, breakdown of membrane phospholipids, release of free fatty acids, and oxidative stress (19, 20). Therefore, metabolic disturbances, such as electrolyte imbalances, acid–base disturbances, and glucose instability, may develop; however, most cases are transient and reversible (21). Late seizures are characterized by irreversible changes, such as gliosis, selective neuronal loss, chronic inflammation, angiogenesis, neurodegeneration, collateral synaptic sprouting, and synaptic plasticity (19). Thus, early seizures follow the course of acute symptomatic seizures, whereas late seizures follow the course of unprovoked seizures (5, 22, 23). Moreover, mortality and disability rates were higher in late seizures than in early seizures. In clinical practice, an evidence-based approach showed that the criteria for a situation that could stipulate the seizure recurrence risk as ≥60% (24). Classifying poststroke seizures into the early and late types is useful for distinguishing acute symptomatic and unprovoked seizures. According to the European guidelines, a poststroke seizure occurring after 1 week on stroke onset is considered a late seizure (i.e., an unprovoked seizure) (25).
Stroke is a common cause of epileptic seizures in older adults (19). However, there is no international consensus on a poststroke seizure risk prediction model. Systematic reviews and meta-analyses on comparative tests of poststroke seizure multivariate risk prediction models were limited by the potential risk for bias and the clinical heterogeneity of patients (26). Several factors may be useful to establish predictors by considering the risk factors for seizures and the poststroke condition.
The prevalence of acute symptomatic seizures with intracranial hemorrhage is higher than that of ischemic stroke (10–16% vs. 2–4%) (27, 28). Ischemic strokes with hemorrhagic transformation have a higher seizure risk compared to ischemic strokes alone (29).
There is an increased incidence of poststroke seizures in cases with cortical involvement, total anterior circulation infarction, severe stroke with larger lesions, and functional deficits (25, 30). Reperfusion injury can manifest as blood brain barrier disruption, cortical irritation, and epileptic seizures (31). In late poststroke seizures, upregulation in endostatin and NCAM, and downregulation in S100B, Hsc70, and TNF-R1 in acute phase blood samples of stroke showed a high correlation (32). However the seizure risk for cerebral venous thrombosis is debatable, as some studies suggest an increase of up to 34%, whereas other studies indicate no association (33–35).
Acute symptomatic or provoked seizures can be induced by direct and immediate causes (27), including metabolic conditions, central nervous system (CNS) infections, sepsis, trauma, drugs, and alcohol consumption (36).
Determining the causes of acute symptomatic seizures other than stroke lesions is important. Acute symptomatic seizures due to metabolic disturbances are associated with the metabolic condition’s rate of deterioration; the faster the deterioration rate, the higher the risk of seizure (37). Metabolic conditions are usually determined by electrolyte tests conducted within 24 h of seizure. However, no absolute cutoff values for seizure prediction have been established, and only few studies have proposed cutoff values as references (Table 2) (27, 36, 37). Seizures in metabolic disturbances with an electrolyte value below the cutoff should be classified into an unknown category and follow-up should be conducted (8). Acute symptomatic seizures due to CNS infection can be considered acute symptomatic seizures even after 7 d, depending on the clinical course or laboratory findings, as the criteria remain unclear (8). Sepsis can induce encephalopathy, which leads to convulsive or nonconvulsive seizures by triggering the electric circuits that promote seizures (42). Alcohol-withdrawal acute symptomatic seizures should be considered in a patient with a history of excessive alcohol use who develops generalized tonic–clonic seizures after alcohol abstinence for 7–48 h (8). As alcohol-induced acute symptomatic seizures may occur, it is very rare and should exclude other etiologies such as metabolic disturbance, trauma, and drug abuse (36). Drug-related acute symptomatic seizures may occur following the administration of meperidine, methaqualone, glutarimide, theophylline, isoniazid, imipenem, cefepime, and chlorpromazine (36, 41). Furthermore, breakthrough seizures can develop when drugs, such as barbiturates and benzodiazepines, are discontinued (41). If any of these factors are determined, correction and treatment are essential.
Poststroke seizures reflect the extent of excessive neuronal discharge and consequent clinical symptomatology. Tonic, clonic, and myoclonic seizures with other semiological findings, such as lip-smacking and motionless staring, may be observed in clinical practice. Nonconvulsive seizures should be confirmed using electroencephalography (EEG).
Clinical signs and symptoms of seizures occur when symptomatic zones of the brain are involved. This may differ from the seizure onset zone or brain lesion, and clinical features may vary according to the seizure propagation pattern. Therefore, even if brain lesions can be accurately localized on brain imaging, semiology may develop in diverse and complex ways when seizure propagation is rapid (43, 44). Furthermore, when seizure semiology and stroke lesions are correlated, the diagnostic accuracy increases significantly through lateralization and localization. Many studies have reported the characteristics of seizure semiology, depending on the location of the brain lesions (Table 3).
Poststroke seizures primarily manifest localization-related seizure semiology, depending on the location of the brain lesion. One-third of all seizures are generalized tonic–clonic seizures (GTCS), whereas two-thirds present as focal seizures, with status epilepticus observed in 9% of cases (47, 48). Focal seizures are common in early seizures, whereas generalized seizures are common in late seizures (47). In patients with ischemic stroke due to large vessel occlusion, seizures occurring within 24 h were predominantly focal seizures or GTCS, whereas seizures with impaired awareness were more common after 24 h (49).
Video-EEG monitoring of all patients with stroke is practically impossible because of time and cost limitations and legislations in different countries. Epileptic seizures are commonly missed by the witness, as most poststroke seizures end within 5 min. Consequently, history taking is the simplest and most vital step in diagnosing poststroke seizures. Although clinicians should carefully listen to patients’ subjective complaints, they should also be familiar with seizure semiology and auras. During interviews, clinicians should ask relevant questions to ensure a correct diagnosis because many patients cannot describe their symptoms concretely and objectively. To ensure an accurate diagnosis, history taking should be divided into preictal, ictal (seizure), and postictal phases. In the preictal phase, determining the various auras of the patient in different environments is important. For example, symptoms appearing while eating, talking, walking, or waking up at night to use the bathroom may be helpful in differential diagnoses. Regarding aura history, confirming the presence of a specific and detailed aura, such as an epigastric rising sensation, hallucinatory taste or smell, ambiguous feelings of fear, anxiety, familiarity, or panorama-like scenes, can help diagnose seizures more accurately than nonspecific symptoms such as headache, dizziness, and nausea (50).
However, the symptoms that develop in the ictal phase cannot be described clearly unless the witness is a clinician. It is therefore crucial to determine the patient’s ability to communicate during a seizure, head version, uneven pupils, patient’s posture, and whether the seizure is tonic or flaccid. Furthermore, abnormal movements, tremulous or myoclonic, such as repetitive, regular muscle contractions, should be determined to ensure accurate diagnosis. In the postictal phase, investigating the presence of confusion, one-sided weakness (Todd’s paresis), or dysphagia is crucial to enable localization or lateralization (50).
Although clinicians may witness poststroke seizures directly in some cases, many cases rely on witness statements. Hence, semiological assessment is important for determining epileptic seizures. Moreover, even if a clinician witnesses the seizure, diagnosis may be difficult in cases with nonconvulsive seizures, unusual seizure semiology, or seizure-related sensory symptoms. In such cases, additional tests, such as EEG, magnetic resonance imaging, and laboratory tests, can aid in the diagnosis. In addition, it is necessary to check for an altered mental state, corporeal localization or lateralization, and somatosensory symptoms and autonomic changes and analyze seizure-like activities (51). If the semiology does not indicate a tangible expression of epileptic seizures, another disease should be suspected.
EEG can aid in the effective evaluation of the brain condition of patients, as it provides real-time and dynamic information on brain function in a simple and noninvasive manner. It effectively distinguishes non-convulsive seizures from autonomic syncope, movement disorders, and pseudo-seizures. EEG has a high sensitivity for the immediate detection of brain ischemia and particularly helpful in cases of large acute infarct volumes (52, 53). In cerebral ischemia, the amplitude and frequency of the EEG waves decrease (54). Acute cerebral infarction may show lateralized or focal slowing patterns on EEG (54). Continuous polymorphic delta with suppressed alpha or beta activity observed in the ischemic hemisphere indicates a poor prognosis (54). Good prognosis is indicated with only delta-to-theta slowing, with no or minor slow activity, and a relatively well-maintained background frequency are observed (54). A recent prospective study investigated whether early (within the initial 72 h) EEG abnormalities could predict poststroke epilepsy during the first year after stroke; the study reported that background asymmetry and interictal epileptiform discharge were independent predictors (55). Another study suggested that there was a 3.2-fold increase in the risk of unprovoked seizures when background asymmetry was observed in the first EEG poststroke and a 3.8-fold increase when interictal epileptiform discharge was observed (55).
Antiseizure medications should be administered when clinical seizures are observed in poststroke patients. However, ASM administration in asymptomatic patients with abnormal EEG findings (e.g., sharp waves or sharply contoured lateralized periodic discharge [LPD]) is debatable in critically ill patients of stroke. The ictal-interictal continuum pattern on EEG can be used as a reference for clinical management, as it suggests possible electrographic seizures (Table 4) (56). A brief, potentially ictal, rhythmic discharge pattern on EEG indicates a seizure onset zone; critically ill patients with this pattern may develop refractory seizures (Table 4) (57). In cases where the EEG pattern satisfies the electrographic seizure or ictal-interictal continuum criteria according to the 2021 American Clinical Neurophysiology Society guidelines, ASM should be considered (Table 4) (56). Furthermore, time-locked LPD is clinically correlated with focal motor jerks, strongly suggesting that epileptic seizures require ASM administration. However, if the discharge frequency does not satisfy the ictal-interictal continuum (<1 Hz) criterion and the shape is less sharply contoured (>200 ms) with LPD, ASM prescription may be suspended. This is due to the possibility of a bystander epiphenomenon, resulting from brain injury without an ongoing insult resulting from a simple structural lesion (58, 59). Generally, one unprovoked seizure with EEG showing prominent epileptiform discharge should be considered an epilepsy based on a seizure recurrence rate ≥ 60% (59, 60). However, applying this in poststroke seizures is difficult because a spike or sharp wave may be observed on EEG due to an epiphenomenon induced by a current acute structural lesion during stroke. In this case, EEG changes induced by the structural lesion (epiphenomenon) disappeared over time when the stroke was properly managed. The 2017 European guidelines do not overlook paroxysmal EEG phenomena as a clinical basis for predicting the recurrence of poststroke seizures (25).
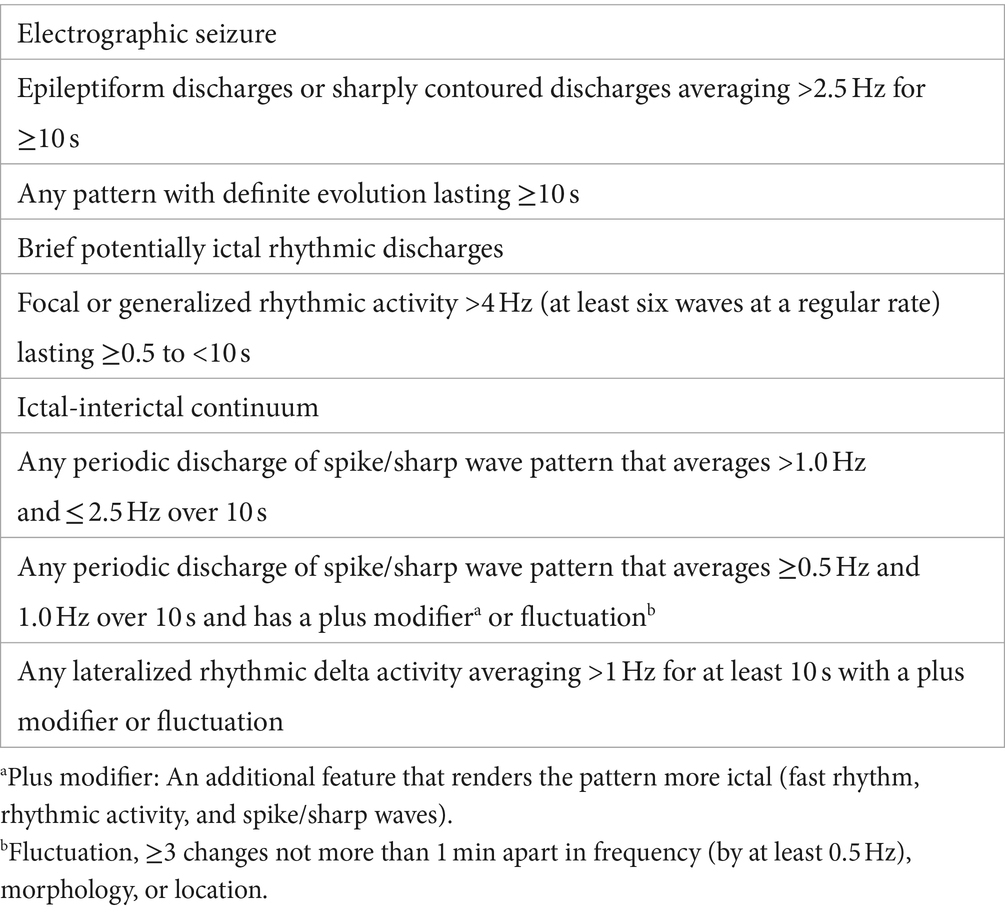
Table 4. American Clinical Neurophysiology Society terminologies and definitions for electroencephalography (2021) (56).
Patients with stroke may show impaired autonomic function, such as a high incidence of orthostatic hypotension, arrythmias, and syncope, owing to their decreased ability to maintain cerebral blood flow. Although the precise underlying mechanisms remains unknown, several studies have proposed possible mechanisms. For example, damage in ischemic stroke can affect nuclear tractus solitarius signaling, resulting in a constant sympathetic activity that increases the resistance of adrenergic beta receptors to stimulation (30). Meanwhile, other studies have postulated that impaired autonomic function occurs when cerebral perfusion decreases in response to a significant decrease in central blood pressure, potentially due to the withdrawal of excessive sympathetic tone (25). A heart rate variability test was conducted to check for reduced cardiac baroreceptor reflex sensitivity and vagal inhibitory outflow (50). Because autonomic dysfunction symptoms may resemble epileptic seizures, unnecessary ASM use should be avoided in the differential diagnosis.
Abnormal poststroke movements are not necessarily the manifestations in epileptic seizures. Therefore, understanding semiology is crucial. Poststroke movement disorder (PSMD) is a poststroke abnormal movement that affects 1–4% of all stroke patients (55). A study analyzing 284 published cases revealed that ischemic stroke accounted for 75% of all PSMD cases. Common sites of the stroke lesions included the posterolateral thalamus (23%), putamen (19%), and caudate nucleus (14%) (61). Because approximately 46% of PSMD cases develop within 7 d poststroke, they overlap with early seizures; therefore, differential diagnosis is vital (61). PSMD after an ischemic stroke can appear quickly, usually within 1 month (61, 62). The frequencies of abnormal movements were as follows: dystonia (23%), chorea (16%), and myoclonus (15%) (61, 62). Chorea and myoclonus often occur within 7 d (61, 62). Movement disorders after a hemorrhagic stroke, commonly including dystonia and tremor, appear more frequently after 6 months (61, 62). In PSMD, owing to stroke lesions, the onset time of caudate lesions is relatively long (approximately 6 months). When the lesion is located in the posterolateral thalamus or putamen, PSMD commonly occurs within 7 d (63); therefore, differentiating it from early seizures is important (63). Because 84% of myoclonus cases induced by PSMD improve naturally when appropriately diagnosed, unnecessary use of ASM can be avoided (61).
Primary ASM prophylaxis is not recommended, as it has not been sufficiently proven to reduce acute symptomatic or unprovoked seizures or to improve functional outcomes or mortality (25). Short-term ASM treatment for 1–4 weeks is used for acute symptomatic or early seizures, as the risk of recurrence is generally low (25). European guidelines do not recommend secondary prophylactic ASM for poststroke seizures. Patients experiencing one acute symptomatic seizure within 7 d have a 10–20% chance of experiencing recurrent acute symptomatic seizures; therefore, secondary ASM prophylaxis is not required (25, 64). Despite the relatively low recurrence rate, short-term ASM is used in patients with a pathophysiological background. ASM may decrease neuronal excitotoxicity, peri-infarct depolarization, and inflammatory responses (65). Some studies recommend short-term ASM treatment in early seizures to reduce the tendency of clinical worsening in the acute phase. This approach relies on pathophysiological considerations, including reduced brain perfusion conditions such as stroke with hemodynamically relevant stenosis, brain edema, and vasospasm after subarachnoid hemorrhage (66, 67). However, guidelines recommend tapering of ASM after the acute phase because the low 10-year risk of unprovoked seizure incidence after one poststroke acute symptomatic seizure (30%) (25). The risk of recurrence of unprovoked poststroke seizures within 10 years is high (70%); therefore, secondary ASM prophylaxis is recommended (5, 25). Long-term ASM use is recommended for poststroke unprovoked seizures because the high risk of seizure recurrence when ASM is discontinued (≥50%) (5, 25).
In summary, long-term ASM use is not recommended, except for poststroke unprovoked seizures. However, it can only be used briefly in the acute phase, depending on the patient’s condition, consistent with the definition and treatment strategy for epilepsy provided by the ILAE (8, 41). ASMs, such as lamotrigine, carbamazepine, lacosamide, levetiracetam, phenytoin, and valproate, may be used (68). A multicenter randomized controlled study suggested lamotrigine is more effective as a first-line treatment for patients with focal epilepsy than levetiracetam or zonisamide (69). Regarding poststroke seizure treatment, the efficacies among lamotrigine, levetiracetam, and sustained-release carbamazepine did not differ; however, lamotrigine and levetiracetam were more tolerable than carbamazepine (70, 71).
Administration of an intensive statin dose in patients with stroke reportedly decreases early or late poststroke seizures. Moreover, when statins were administered for ≥2 years, the risk of poststroke epilepsy decreased, regardless of whether statins were administered before or after stroke (72–74). The precise antiseizure mechanism of statins is unknown; however, several theories have been proposed. First, neuroinflammation caused by stroke increases nerve excitability, inducing the secretion of abnormal neurotransmitters by increasing BBB permeability, and leading to seizures by exacerbation of cerebral hypoxia. Statins prevent seizures by exerting anti-inflammatory actions, including regulating blood brain barrier permeability (75), modulating endothelial nitric oxide (76), controlling proinflammatory genes, pro-inflammatory cytokines, and free radicals, and inhibiting lipid peroxidation. While acute ischemia elevates glutamate levels (77, 78), statins inhibit the excitatory toxicity of glutamate by reducing the activity and absorption of N-methyl-d-aspartate receptors and regulating intracellular calcium levels (75, 79, 80). Bax induces apoptosis, whereas Bcl inhibits apoptosis (19). Statins affect apoptotic pathways associated with these genes and increase neuronal survival, thereby preventing epilepsy (19).
Poststroke seizures are common complications of stroke. It is pivotal to systematically approach, evaluate, classify, and manage them (Figure 1) and differentiate them from abnormal movement disorders, syncope, and psychogenic nonepileptic seizures based on semiology. A systematic approach and identification of factors other than stroke-related structural lesions that can cause acute symptomatic seizures are important (Figure 1). Once a poststroke seizure is confirmed, we can effectively treat patients, improve their prognosis by determining whether it is an early or late seizure, and plan a treatment strategy appropriate for their condition.
HR: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. HKi: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – original draft. B-SS: Data curation, Formal analysis, Investigation, Project administration, Supervision, Writing – review & editing. HKa: Conceptualization, Investigation, Resources, Supervision, Validation, Visualization, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Fund of Biomedical Research Institute, Jeonbuk National University Hospital.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Feigin, VL, Brainin, M, Norrving, B, Martins, S, Sacco, RL, Hacke, W, et al. World stroke organization (WSO): global stroke fact sheet 2022. Int J Stroke. (2022) 17:18–29. doi: 10.1177/17474930211065917
2. Mishra, NK, Engel, J Jr, Liebeskind, DS, Sharma, VK, Hirsch, LJ, Kasner, SE, et al. International post stroke epilepsy research consortium (IPSERC): a consortium to accelerate discoveries in preventing epileptogenesis after stroke. Epilepsy Behav. (2022) 127:108502. doi: 10.1016/j.yebeh.2021.108502
3. Annegers, JF, Hauser, WA, Lee, JR, and Rocca, WA. Incidence of acute symptomatic seizures in Rochester, Minnesota, 1935-1984. Epilepsia. (1995) 36:327–33. doi: 10.1111/j.1528-1157.1995.tb01005.x
4. Herzig-Nichtweiß, J, Salih, F, Berning, S, Malter, MP, Pelz, JO, Lochner, P, et al. Prognosis and management of acute symptomatic seizures: a prospective, multicenter, observational study. Ann Intensive Care. (2023) 13:85. doi: 10.1186/s13613-023-01183-0
5. Hesdorffer, DC, Benn, EK, Cascino, GD, and Hauser, WA. Is a first acute symptomatic seizure epilepsy? Mortality and risk for recurrent seizure. Epilepsia. (2009) 50:1102–8. doi: 10.1111/j.1528-1167.2008.01945.x
6. Graham, NSN, Crichton, S, Koutroumanidis, M, Wolfe, CDA, and Rudd, AG. Incidence and associations of poststroke epilepsy: the prospective South London stroke register. Stroke. (2013) 44:605–11. doi: 10.1161/STROKEAHA.111.000220
7. Zelano, J. Poststroke epilepsy: update and future directions. Ther Adv Neurol Disord. (2016) 9:424–35. doi: 10.1177/1756285616654423
8. Mauritz, M, Hirsch, LJ, Camfield, P, Chin, R, Nardone, R, Lattanzi, S, et al. Acute symptomatic seizures: an educational, evidence-based review. Epileptic Disord. (2022) 24:26–49. doi: 10.1684/epd.2021.1376
9. Lamy, C, Domigo, V, Semah, F, Arquizan, C, Trystram, D, Coste, J, et al. Patent foramen ovale and atrial septal aneurysm study group. Early and late seizures after cryptogenic ischemic stroke in young adults. Neurology. (2003) 60:400–4. doi: 10.1212/wnl.60.3.400
10. Arntz, R, Rutten-Jacobs, L, Maaijwee, N, Schoonderwaldt, H, Dorresteijn, L, van Dijk, E, et al. Post-stroke epilepsy in young adults: a long-term follow-up study. PLoS One. (2013) 8:e55498. doi: 10.1371/journal.pone.0055498
11. Naess, H, Nyland, HI, Thomassen, L, Aarseth, J, and Myhr, KM. Long-term outcome of cerebral infarction in young adults. Acta Neurol Scand. (2004) 110:107–12. doi: 10.1111/j.1600-0404.2004.00273.x
12. Bladin, CF, Alexandrov, AV, Bellavance, A, Bornstein, N, Chambers, B, Coté, R, et al. Seizures after stroke: a prospective multicenter study. Arch Neurol. (2000) 57:1617–22. doi: 10.1001/archneur.57.11.1617
13. Olafsson, E, Gudmundsson, G, and Hauser, WA. Risk of epilepsy in long-term survivors of surgery for aneurysmal subarachnoid hemorrhage: a population-based study in Iceland. Epilepsia. (2000) 41:1201–125. doi: 10.1111/j.1528-1157.2000.tb00326.x
14. Sung, CY, and Chu, NS. Epileptic seizures in intracerebral haemorrhage. J Neurol Neurosurg Psychiatry. (1989) 52:1273–6. doi: 10.1136/jnnp.52.11.1273
15. Qian, C, Löppönen, P, Tetri, S, Huhtakangas, J, Juvela, S, Turtiainen, HME, et al. Immediate, early and late seizures after primary intracerebral hemorrhage. Epilepsy Res. (2014) 108:732–9. doi: 10.1016/j.eplepsyres.2014.02.020
16. Guidelines for Epidemiologic Studies on Epilepsy. Commission on epidemiology and prognosis, international league against epilepsy. Epilepsia. (1993) 34:592–6. doi: 10.1111/j.1528-1157.1993.tb00433.x
17. So, EL, Annegers, JF, Hauser, WA, O’Brien, PC, and Whisnant, JP. Population-based study of seizure disorders after cerebral infarction. Neurology. (1996) 46:350–5. doi: 10.1212/wnl.46.2.350
18. Serafini, A, Gigli, GL, Gregoraci, G, Janes, F, Cancelli, I, Novello, S, et al. Are early seizures predictive of epilepsy after a stroke? Results of a population-based study. Neuroepidemiology. (2015) 45:50–8. doi: 10.1159/000382078
19. Feyissa, AM, Hasan, TF, and Meschia, JF. Stroke-related epilepsy. Eur J Neurol. (2019) 26:18–e3. doi: 10.1111/ene.13813
20. Karhunen, H, Jolkkonen, J, Sivenius, J, and Pitkänen, A. Epileptogenesis after experimental focal cerebral ischemia. Neurochem Res. (2005) 30:1529–42. doi: 10.1007/s11064-005-8831-y
21. Barker-Haliski, M, and Steve White, H. Glutamatergic mechanisms associated with seizures and epilepsy. Cold Spring Harb Perspect Med. (2015) 5:a022863. doi: 10.1101/cshperspect.a022863
22. Alberti, A, Paciaroni, M, Caso, V, Venti, M, Palmerini, F, and Agnelli, G. Early seizures in patients with acute stroke: frequency, predictive factors, and effect on clinical outcome. Vasc Health Risk Manag. (2008) 4:715–20. doi: 10.2147/VHRM.S2445
23. Lee, JC, Lin, KL, Wang, HS, Chou, ML, Hung, PC, Hsieh, MY, et al. Seizures in childhood ischemic stroke in Taiwan. Brain and Development. (2009) 31:294–9. doi: 10.1016/j.braindev.2008.05.006
24. Fisher, RS, Acevedo, C, Arzimanoglou, A, Bogacz, A, Cross, JH, Elger, CE, et al. (ILAE) official report: a practical clinical definition of epilepsy. Epilepsia. (2014) 55:475–82. doi: 10.1111/epi.12550
25. Holtkamp, M, Beghi, E, Benninger, F, Kälviäinen, R, Rocamora, R, Christensen, H, et al. European stroke organisation guidelines for the management of post-stroke seizures and epilepsy. Eur Stroke J. (2017) 2:103–15. doi: 10.1177/2396987317705536
26. Lee, SH, Aw, KL, Banik, S, and Myint, PK. Post=stroke seizure risk prediction models: a systematic review and meta-analysis. Epileptic Disord. (2022) 24:302–14. doi: 10.1684/epd.2021.1391
27. Beghi, E, Carpio, A, Forsgren, L, Hesdorffer, DC, Malmgren, K, Sander, JW, et al. Recommendation for a definition of acute symptomatic seizure. Epilepsia. (2010) 51:671–5. doi: 10.1111/j.1528-1167.2009.02285.x
28. Procaccianti, G, Zaniboni, A, Rondelli, F, Crisci, M, and Sacquegna, T. Seizures in acute stroke: incidence, risk factors and prognosis. Neuroepidemiology. (2012) 39:45–50. doi: 10.1159/0003383748
29. Beghi, E, D’Alessandro, R, Beretta, S, Consoli, D, Crespi, V, Delaj, L, et al. Incidence and predictors of acute symptomatic seizures after stroke. Neurology. (2011) 77:1785–93. doi: 10.1212/WNL.0b013e3182364878
30. Pitkänen, A, Roivainen, R, and Lukasiuk, K. Development of epilepsy after ischemic stroke. Lancet Neurol. (2016) 15:185–97. doi: 10.1016/S1474-4422(15)00248-3
31. Hafeez, F, Razzaq, MA, Levine, RL, and Ramirez, MAN. Reperfusion seizures: a manifestation of cerebral reperfusion injury after administration of recombinant tissue plasminogen activator for acute ischemic stroke. J Stroke Cerebrovasc Dis. (2007) 16:273–7. doi: 10.1016/j.jstrokecerebrovasdis.2007.07.007
32. Abraira, L, Santamarina, E, Cazorla, S, Bustamante, A, Quintana, M, Toledo, M, et al. Blood biomarkers predictive of epilepsy after an acute stroke event. Epilepsia. (2020) 61:2244–53. doi: 10.1111/epi.16648
33. Lindgren, E, Silvis, SM, Hiltunen, S, Heldner, MR, Serrano, F, de Scisco, M, et al. Acute symptomatic seizures in cerebral venous thrombosis. Neurology. (2020) 95:e1706–15. doi: 10.1212/WNL.0000000000010577
34. Sánchez van Kammen, M, Lindgren, E, Silvis, SM, Hiltunen, S, Heldner, MR, Serrano, F, et al. Late seizures in cerebral venous thrombosis. Neurology. (2020) 95:e1716–23. doi: 10.1212/WNL.0000000000010576
35. Phan, J, Ramos, M, Soares, T, and Parmar, MS. Poststroke seizure and epilepsy: a review of incidence, risk factors, diagnosis, pathophysiology, and pharmacological therapies. Oxidative Med Cell Longev. (2022) 2022:7692215–5. doi: 10.1155/2022/7692215
36. McLauchlan, DJ, and Powell, R. Acute symptomatic seizures. Pract Neurol. (2012) 12:154–65. doi: 10.1136/practneurol-2012-000244
37. Nardone, R, Brigo, F, and Trinka, E. Acute symptomatic seizures caused by electrolyte disturbances. J Clin Neurol. (2016) 12:21–33. doi: 10.3988/jcn.2016.12.1.21
38. Delanty, N, Vaughan, CJ, and French, JA. Medical causes of seizures. Lancet. (1998) 352:383–90. doi: 10.1016/S0140-6736(98)02158-8
39. Karceski, S. Acute symptomatic seizures and systemic illness. CONTIN Lifelong Learn Neurol. (2014) 20:614–23. doi: 10.1212/01.CON.0000450969.61204.6f
40. Gschwind, M, and Seeck, M. Modern management of seizures and epilepsy. Swiss Med Wkly. (2016) 146:w14310. doi: 10.4414/smw.2016.14310
41. Beleza, P. Acute symptomatic seizures: a clinically oriented review. Neurologist. (2012) 18:109–19. doi: 10.1097/NRL.0b013e318251e6c3
42. Alessandri, F, Badenes, R, and Bilotta, F. Seizures and sepsis: a narrative review. J Clin Med. (2021) 10:1041. doi: 10.3390/jcm10051041
43. Jehi, L. The epileptogenic zone: concept and definition. Epilepsy Curr. (2018) 18:12–6. doi: 10.5698/1535-7597.18.1.12
44. Tufenkjian, K, and Lüders, HO. Seizure semiology: its value and limitations in localizing the epileptogenic zone. J Clin Neurol. (2012) 8:243–50. doi: 10.3988/jcn.2012.8.4.243
45. Jan, MMS, and Girvin, JP. Seizure semiology: value in identifying seizure origin. Can J Neurol Sci. (2008) 35:22–30. doi: 10.1017/s0317167100007526
46. Turek, G, and Skjei, K. Seizure semiology, localization, and the 2017 ILAE seizure classification. Epilepsy Behav. (2022) 126:108455. doi: 10.1016/j.yebeh.2021.108455
47. Myint, PK, Staufenberg, EF, and Sabanathan, K. Post-stroke seizure and post-stroke epilepsy. Postgrad Med J. (2006) 82:568–72. doi: 10.1136/pgmj.2005.041426
48. Rumbach, L, Sablot, D, Berger, E, Tatu, L, Vuillier, F, and Moulin, T. Status epilepticus in stroke: report on a hospital-based stroke cohort. Neurology. (2000) 54:350–4. doi: 10.1212/wnl.54.2.350
49. Tako, LM, Strzelczyk, A, Rosenow, F, Pfeilschifter, W, Steinmetz, H, Golbach, R, et al. Predictive factors of acute symptomatic seizures in patients with ischemic stroke due to large vessel occlusion. Front Neurol. (2022) 13:894173. doi: 10.3389/fneur.2022.894173
50. Rodriguez, J, Blaber, AP, Kneihsl, M, Trozic, I, Ruedl, R, Green, DA, et al. Poststroke alterations in heart rate variability during orthostatic challenge. Medicine (Baltimore). (2017) 96:e5989. doi: 10.1097/MD.0000000000005989
51. Jan, MM. The value of seizure semiology in lateralizing and localizing partially originating seizures. Neurosciences (Riyadh). (2007) 12:185–90.
52. Shreve, L, Kaur, A, Vo, C, Wu, J, Cassidy, JM, Nguyen, A, et al. Electroencephalography measures are useful for identifying large acute ischemic stroke in the emergency department. J Stroke Cerebrovasc Dis. (2019) 28:2280–6. doi: 10.1016/j.jstrokecerebrovasdis.2019.05.019
53. Erani, F, Zolotova, N, Vanderschelden, B, Khoshab, N, Sarian, H, Nazarzai, L, et al. Electroencephalography might improve diagnosis of acute stroke and large vessel occlusion. Stroke. (2020) 51:3361–5. doi: 10.1161/STROKEAHA.120.030150
54. Jordan, KG. Emergency EEG and continuous EEG monitoring in acute ischemic stroke. J Clin Neurophysiol. (2004) 21:341–52.
55. Bentes, C, Martins, H, Peralta, AR, Morgado, C, Casimiro, C, Franco, AC, et al. Early EEG predicts poststroke epilepsy. Epilepsia. (2018) 3:203–12. doi: 10.1002/epi4.12103
56. Hirsch, LJ, Fong, MWK, Leitinger, M, LaRoche, SM, Beniczky, S, Abend, NS, et al. American clinical neurophysiology society’s standardized critical care EEG terminology: 2021 version. J Clin Neurophysiol. (2021) 38:1–29. doi: 10.1097/WNP.0000000000000806
57. Yoo, JY, Jetté, N, Kwon, CS, Young, J, Marcuse, LV, Fields, MC, et al. Brief potentially ictal rhythmic discharges and paroxysmal fast activity as scalp electroencephalographic biomarkers of seizure activity and seizure onset zone. Epilepsia. (2021) 62:742–51. doi: 10.1111/epi.16822
58. Appavu, B, and Riviello, JJ. Electroencephalographic patterns in neurocritical care: pathologic contributors or epiphenomena? Neurocrit Care. (2018) 29:9–19. doi: 10.1007/s12028-017-0424-5
59. Husari, KS, and Johnson, EL. Periodic discharges: how to approach, when to treat. J Clin Neurophysiol. (2020) 37:411–21. doi: 10.1097/WNP.0000000000000647
60. Lin, L, and Drislane, FW. Lateralized periodic discharges: a literature review. J Clin Neurophysiol. (2018) 35:189–98. doi: 10.1097/WNP.0000000000000448
61. Suri, R, Rodriguez-Porcel, F, Donohue, K, Jesse, E, Lovera, L, Dwivedi, AK, et al. Post-stroke movement disorders: the clinical, neuroanatomic, and demographic portrait of 284 published cases. J Stroke Cerebrovasc Dis. (2018) 27:2388–97. doi: 10.1016/j.jstrokecerebrovasdis.2018.04.028
62. Bansil, S, Prakash, N, Kaye, J, Wrigley, S, Manata, C, Stevens-Haas, C, et al. Movement disorders after stroke in adults: a review. Tremor Other Hyperkinet Mov. (2012) 2:tre-02–42-195-1. doi: 10.7916/D86W98TB
63. Gupta, N, and Pandey, S. Post-thalamic stroke movement disorders: a systematic review. Eur Neurol. (2018) 79:303–14. doi: 10.1159/000490070
64. Leung, T, Leung, H, Soo, YOY, Mok, VCT, and Wong, KS. The prognosis of acute symptomatic seizures after ischemic stroke. J Neurol Nerurosurg Psychiatry. (2017) 88:86–94. doi: 10.1136/jnnp-2015-311849
65. Dirnagl, U, Iadecola, C, and Moskowitz, MA. Pathobiology of ischaemic stroke: an integrated view. Trends Neurosci. (1999) 22:391–7. doi: 10.1016/s0166-2236(99)01401-0
66. Galovic, M, Ferreira-Atuesta, C, Abraira, L, Döhler, N, Sinka, L, Brigo, F, et al. Seizures and epilepsy after stroke: epidemiology, biomarkers and management. Drugs Aging. (2021) 38:285–99. doi: 10.1007/s40266-021-00837-7
67. Zelano, J, Holtkamp, M, Agarwal, N, Lattanzi, S, Trinka, E, and Brigo, F. How to diagnose and treat post-stroke seizures and epilepsy. Epileptic Disord. (2020) 22:252–63. doi: 10.1684/epd.2020.1159
68. Consoli, D, Bosco, D, Postorino, P, Galati, F, Plastino, M, Perticoni, GF, et al. EPIC study. Levetiracetam versus carbamazepine in patients with late poststroke seizures: a multicenter prospective randomized open-label study (EpIC project). Cerebrovasc Dis. (2012) 34:282–9. doi: 10.1159/000342669
69. Marson, A, Burnside, G, Appleton, R, Smith, D, Leach, JP, Sills, G, et al. The SANAD II study of the effectiveness and cost-effectiveness of levetiracetam, zonisamide, or lamotrigine for newly diagnosed focal epilepsy: an open-label, non-inferiority, multicentre, phase 4, randomised controlled trial. Lancet. (2021) 397:1363–74. doi: 10.1016/S0140-6736(21)00247-6
70. Bekelaar, K, van Tuijl, JH, van Raak, EPM, van Oostenbrugge, RJ, Aldenkamp, AP, and Rouhl, RPW. Medication use in poststroke epilepsy: a descriptive study on switching of antiepileptic drug treatment. Epilepsy Behav. (2020) 104:106434. doi: 10.1016/j.yebeh.2019.07.035
71. Xu, MY. Poststroke seizure: optimising its management. Stroke Vasc Neurol. (2019) 4:48–56. doi: 10.1136/svn-2018-000175
72. Li, Y, Zhang, B, Zhang, L, Xie, D, and Li, Y. Efficacy of statin therapy in post-stroke seizure prophylaxis: clues from an observational study of routine secondary prevention treatment. Seizure. (2019) 71:185–9. doi: 10.1016/j.seizure.2019.07.010
73. Matsubara, S, Tanaka, T, Tomari, S, Fukuma, K, Ishiyama, H, Abe, S, et al. Statin treatment can reduce incidence of early seizure in acute ischemic stroke: a propensity score analysis. Sci Rep. (2020) 10:1968. doi: 10.1038/s41598-020-58652-w
74. Xu, T, Wang, Y, Yuan, J, Chen, Y, and Luo, H. Statin use and the risk of post-stroke seizures: a meta-analysis. Seizure. (2020) 83:63–9. doi: 10.1016/j.seizure.2020.10.004
75. Ifergan, I, Wosik, K, Cayrol, R, Kébir, H, Auger, C, Bernard, M, et al. Statins reduce human blood-brain barrier permeability and restrict leukocyte migration: relevance to multiple sclerosis. Ann Neurol. (2006) 60:45–55. doi: 10.1002/ana.20875
76. Moezi, L, Shafaroodi, H, Hassanipour, M, Fakhrzad, A, Hassanpour, S, and Dehpour, AR. Chronic administration of atorvastatin induced anti-convulsant effects in mice: the role of nitric oxide. Epilepsy Behav. (2012) 23:399–404. doi: 10.1016/j.yebeh.2012.02.001
77. Quintana-Pájaro, LJ, Ramos-Villegas, Y, Cortecero-Sabalza, E, Joaquim, AF, Agrawal, A, Narvaez-Rojas, AR, et al. The effect of statins in epilepsy: a systematic review. J Neurosci Rural Prac. (2018) 9:478–86. doi: 10.4103/jnrp.jnrp_110_18
78. Jauch, EC, Saver, JL, Adams, HP, Bruno, A, Connors, JJB, Demaerschalk, BM, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. (2013) 44:870–947. doi: 10.1161/STR.0b013e318284056a
79. Bösel, J, Gandor, F, Harms, C, Synowitz, M, Harms, U, Djoufack, PC, et al. Neuroprotective effects of atorvastatin against glutamate-induced excitotoxicity in primary cortical neurones. J Neurochem. (2005) 92:1386–98. doi: 10.1111/j.1471-4159.2004.02980.x
Keywords: poststroke seizure, unilateral weakness, dysarthria, sensory deficit, stroke
Citation: Ryu HU, Kim HJ, Shin B-S and Kang HG (2024) Clinical approaches for poststroke seizure: a review. Front. Neurol. 15:1337960. doi: 10.3389/fneur.2024.1337960
Received: 13 November 2023; Accepted: 26 March 2024;
Published: 10 April 2024.
Edited by:
Sara Gasparini, Magna Græcia University, ItalyReviewed by:
Rossen Т. Rousseff, Medical University, BulgariaCopyright © 2024 Ryu, Kim, Shin and Kang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hyun Goo Kang, aGdrYW5nQGpibnUuYWMua3I=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.