
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol. , 07 February 2024
Sec. Stroke
Volume 15 - 2024 | https://doi.org/10.3389/fneur.2024.1302298
 Yahia Z. Imam1,2,3*
Yahia Z. Imam1,2,3* Prem Chandra4
Prem Chandra4 Rajvir Singh5
Rajvir Singh5 Ishrat Hakeem1
Ishrat Hakeem1 Sally Al Sirhan3
Sally Al Sirhan3 Mona Kotob3
Mona Kotob3 Naveed Akhtar1,2,3
Naveed Akhtar1,2,3 Saadat Kamran1,2
Saadat Kamran1,2 Salman Al Jerdi2
Salman Al Jerdi2 Ahmad Muhammad1,2
Ahmad Muhammad1,2 Khawaja Hasan Haroon1
Khawaja Hasan Haroon1 Suhail Hussain1
Suhail Hussain1 Jon D. Perkins1
Jon D. Perkins1 Osama Elalamy1,2
Osama Elalamy1,2 Mohamed Alhatou1
Mohamed Alhatou1 Liaquat Ali1
Liaquat Ali1 Mohamed S. Abdelmoneim1
Mohamed S. Abdelmoneim1 Sujatha Joseph1
Sujatha Joseph1 Deborah Morgan1
Deborah Morgan1 Ryan Ty Uy1
Ryan Ty Uy1 Zain Bhutta6
Zain Bhutta6 Aftab Azad3,6
Aftab Azad3,6 Ali Ayyad1
Ali Ayyad1 Ahmed Elsotouhy1
Ahmed Elsotouhy1 Ahmed Own1
Ahmed Own1 Dirk Deleu1,2
Dirk Deleu1,2Background: Posterior cerebral circulation ischemic stroke (PCS) comprises up to 25% of all strokes. It is characterized by variable presentation, leading to misdiagnosis and morbidity and mortality. We aim to describe PCS in large multiethnic cohorts.
Methods: A retrospective review of a large national stroke database from its inception on the 1st of January 2014 till 31 December 2020. Incidence per 100,000 adult population/year, demographics, clinical features, stroke location, and outcomes were retrieved. We divided the cohort into patients from MENA (Middle East and North Africa) and others.
Results: In total, 1,571 patients were identified. The incidence of PCS was observed to be rising and ranged from 6.3 to 13.2/100,000 adult population over the study period. Men were 82.4% of the total. The mean age was 54.9 ± 12.7 years (median 54 years, IQR 46, 63). MENA patients comprised 616 (39.2%) while others were 954 (60.7%); of these, the majority (80.5%) were from South Asia. Vascular risk factors were prevalent with 1,230 (78.3%) having hypertension, 970 (61.7%) with diabetes, and 872 (55.5%) having dyslipidemia. Weakness (944, 58.8%), dizziness (801, 50.5%), and slurred speech (584, 36.2%) were the most commonly presenting symptoms. The mean National Institute of Health Stroke Score (NIHSS) score was 3.8 ± 4.6 (median 3, IQR 1, 5). The overall most frequent stroke location was the distal location (568, 36.2%). The non-MENA cohort was younger, less vascularly burdened, and had more frequent proximal stroke location (p < 0.05). Dependency or death at discharge was seen in 39.5% and was associated with increasing age, and proximal and multilocation involvement; while at 90 days it was 27.4% and was associated with age, male sex, and having a MENA nationality (p < 0.05).
Conclusion: In a multiethnic cohort of posterior circulation stroke patients from the MENA region and South Asia, we noted a rising incidence over time, high prevalence of vascular risk factors, and poor outcomes in older men from the MENA region. We also uncovered considerable disparities between the MENA and non-MENA groups in stroke location and outcome. These disparities are crucial factors to consider when tailoring individualized patient care plans. Further research is needed to thoroughly investigate the underlying reasons for these variations.
Posterior cerebral circulation ischemic stroke constitutes approximately 20%–25% of all ischemic stroke (1). It poses unique challenges to treating clinicians in that it has variable, nonspecific presentation owing to the vast area of supply, the complexity of the structures supplied, and the significant anatomical variations observed (2). Furthermore, even a score of zero on the National Institute of Health Stroke Scale (NIHSS) is not synonymous with “no stroke” given that it is heavily biased to detect anterior circulation stroke (3, 4). In addition, plain CT head scans are not sensitive enough which can lead to a false sense of security leading it to be frequently missed (5). This predisposes PCS patients to significant morbidity and mortality with basilar thrombosis in particular a feared presentation.
Most of the descriptions of PCS have come from registry data and selections of posterior circulation patients from large clinical trials or multicenter cohorts (6–8), however, PCS is largely overshadowed by the more common anterior circulation stroke (ACS). Zhang et al. (8) reported on 690 patients from 22 Chinese centers with noncardiogenic PCS due to intracranial atherosclerotic disease (ICAD) and provided insights indicating that PCS due to non-vertebral ICAD was more common than vertebral ICAD in the Chinese population. However, the latter had more serious clinical-radiologic patterns and worse outcomes.
A large Iranian cohort study (9) on stroke compared ACS to PCS. It is noteworthy that the cohort had only 76 patients with PCS. It concluded that there was no difference in mortality and functional outcome between the two groups.
Another important registry is the New England Medical Center Posterior Circulation Registry (NEMC-PCR) (6). It is a multiethnic, predominantly white database that has provided a widely used neuroimaging-based PCS classification. However, non-white patients have been underrepresented.
Different populations have different demographics and psychosocial and economic connotations that impact how disease is diagnosed and treated (10). Furthermore, there is mounting evidence of the presence of ethnic disparity in stroke incidence (11), stroke care, and outcome (12). The Middle East and North Africa plus region (MENA+) is known to have a high stroke burden and, more worryingly, at a younger age (13). Emerging reports suggest existing disparity in the region itself in terms of stroke facilities, access to care, and availability of acute therapies (14), therefore, it is important to shed light on such data to help inform future research.
In this current descriptive study, we aim to mainly describe PCS demographics, risk factors, clinical features, and outcomes in a large multiethnic database with a predominance of patients from the Middle East, North Africa, and South and Southeast Asia.
This is a retrospective descriptive review of a large national stroke database from its inception on 1st January 2014 until 31 December 2020. Posterior cerebral circulation ischemic stroke (PCS) refers to a clinical syndrome resulting from ischemia caused by stenosis, in-situ thrombosis, or embolic occlusion affecting arteries in the posterior circulation. These arteries include the vertebral arteries in the neck, the intracranial vertebral, basilar, and posterior cerebral arteries, as well as their branches (15).
Patient inclusion criteria were adapted from Akhtar et al. (16) as:
1. Acute neurologic deficit attributable to posterior circulation and basilar artery occlusion, proven by computed tomographic angiogram (CTA), MRA, or conventional angiogram.
2. Acute neurologic deficit causing alternating hemi/tetraplegia with brain stem signs, visual loss, locked in state, coma, or death.
3. Coma or loss of consciousness and acute posterior circulation infarction on CT or MRI.
The Qatar Stroke database has a unique setup as Qatar has only one accredited comprehensive stroke center (Hamad General Hospital) and >90% of cases are either admitted, referred, or followed up here and are referenced in this prospective registry (17). Incidence per 100,000 adult population/year is calculated using the number of PCS/years divided by the total population from census data as previously described (18) or derived from the mid-year population estimates provided by the Planning and Statistics Authority (19).
The patients were grouped according to their nationality as follows. The Middle East and North Africa (MENA) region was defined as per the United Nations International Children’s Emergency Fund (UNICEF) definition (20). Whereas geographic regions within Asia were subdivided into East Asia, South Asia, and Southeast Asia according to United Nations Geoscheme (21). However, Iran was included in MENA as per the UNICEF definition as it shares tight geosocial ties with the rest of the MENA region. All other nationalities were included in the others.
Diabetes mellitus (DM) was defined as per American Diabetes Association criteria (22), and dyslipidemia (23), hypertension (24), coronary artery disease (25), and atrial fibrillation (26) were defined as per these respective guidelines.
This was described previously (16) and includes brain-imaging studies with CT and/or MRI (at least one), along with vascular imaging CTA or MRA or conventional angiogram.
Presenting symptoms and signs were described. Stroke severity was assessed by the National Institute of Health Stroke Scale (NIHSS) (27) and the stroke location on neuroimaging was described using the New England Medical Center Posterior Circulation registry classification (6) as illustrated in Figure 1 (adapted from Frank Netter’s Atlas of Human Anatomy) (28). Stroke etiology was classified according to the TOAST classification (29). Outcomes were assessed at discharge and 90 days using the Modified Rankin Score (mRS) (30). It was dichotomized to show independence (mRS 0–2) or dependence/death (mRS 3–6).
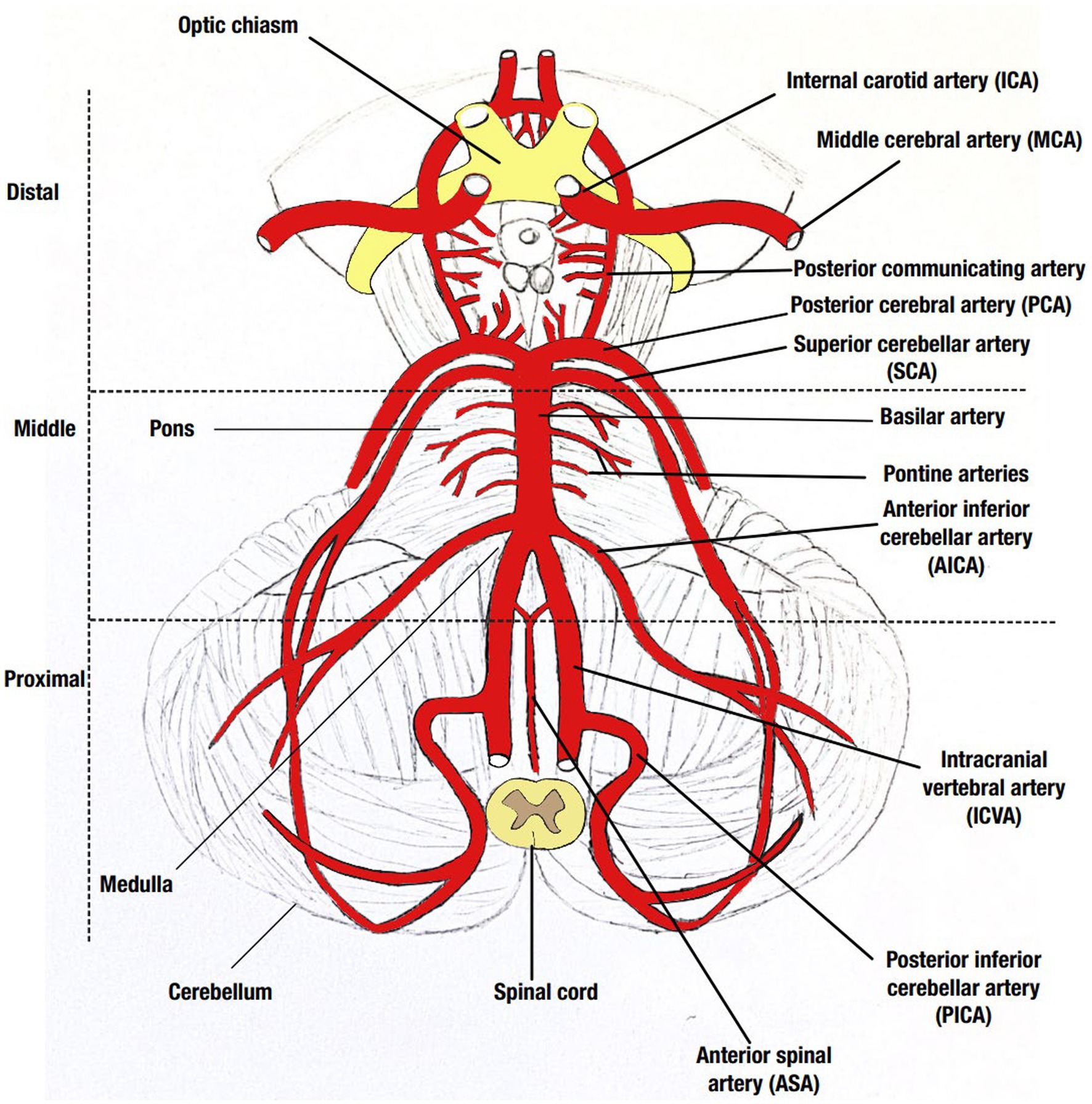
Figure 1. Illustration of the posterior circulation including the three distinct locations described in the New England Medical Center Posterior Circulation registry classification. Drawing by Sally Al-Sirhan adopted from Netter (28).
Descriptive statistics were used to summarize demographics, clinical features, neuroimaging findings, and outcomes of posterior circulation ischemic stroke cases and related risk factors. Quantitative results were reported with the mean and the standard deviation (SD), while the median and the interquartile range (IQR) were used for skewed/non-normal data distribution. Quantitative data (such as age, NIHSS, and mRS score) between MENA vs. Others were analyzed using an independent t test or the Mann–Whitney U test as appropriate. Incidence rates of PCS per 100,000 adult population by year were estimated and presented with respective 95% confidence intervals (CI). Confidence intervals for incidence rates were calculated using the OpenEpi software (31). Categorical data were summarized using frequencies and percentages. Associations between two or more categorical data were assessed using Chi-square (χ2) and/or Fisher Exact test as appropriate. Box plots were constructed to depict the distribution of age across outcome categories. All p-values presented were two-tailed, and values <0.05 were considered statistically significant. Statistical data analyses were performed using statistical software packages SPSS version 28.0 (Armonk, NY: IBM Corp) and Epi-info (Centers for Disease Control and Prevention, Atlanta, GA).
This study was approved by the Institutional Review Board at the Medical Research Center, research protocol 03-SI-17-075.
A total of 1,571 PCS patients were identified. Of these 1,295 (82.4%) were men. The mean age of the PCS cohort was 54.9 ± 12.7 years (median 54 years, IQR 46, 63). Patients from South Asia constituted 768 (48.9%), followed by the MENA region with 616 (39.2%), then Southeast and East Asia with 145 (9.2%), and 42 from other regions (2.7%). The incidence of PCS ranged from 6.3 to 13.2/100,000 adult population as seen in Table 1.
Vascular risk factors were prevalent, with 1,230 (78.3%) having hypertension, 970 (61.7%) with DM, 872 (55.5%) with dyslipidemia, 179 (11.4%) with coronary artery disease (CAD), 69 (4.4%) with atrial fibrillation (AF), and 184 (11.7%) had a prior history of Stroke/TIA.
The most prevalent presenting complaint was weakness (any of the face, arm, or leg or clumsiness) with 944 (58.8%), followed by 801 (50.5%) with dizziness, 584 (36.2%) with slurred speech, 207 (13.1%) with vertigo, 598 (28.8%) with nausea/vomiting, 450 (28.5%) with numbness, 428 (26.5%) with headache, and 365 (23.2%) with eye complaints including double vision, blurring of vision or field cut, as well as 196 (12.5%) with decreased sensorium and 164 (10.4%) with imbalance.
The NIHSS mean score was 3.8 ± 4.6 (median 3, IQR 1, 5). The most frequent location of stroke was the distal location with 568 (36.2%), followed by the proximal location with 464 (29.5%) and the least frequent was the middle location with 352 (22.4%). Multiple locations were observed in 187 (11.9%).
Demographics, stroke risk factors, stroke locations, and outcomes are illustrated in Table 2 and grouped into MENA vs. Others (non-MENA).

Table 2. Demographics, risk factors, stroke location, and outcomes in Middle East and North Africa (MENA) cohort vs non-MENA.
The non-MENA cohort was significantly younger and had significantly lower body weight, diabetes, hypertension, coronary artery disease, and atrial fibrillation (p < 0.05) than the MENA cohort.
The TOAST classification was available for 87.3% of patients. Small vessel disease (SVD, 50.7%) was the most frequent stroke etiology, followed by large artery atherosclerosis (LAA, 19.8%), and cardioembolic (CE, 17.1%). There was no significant difference observed (p > 0.05) in stroke etiology between the MENA and non-MENA contingents (Table 2).
The most prevalent locations among the proximal location were isolated PICA cerebellum involvement in 376 (62%) patients, whereas the pontine branches were the most prevalent in the middle location in 394 (82.9%) patients and PCA involvement in the distal location in 563 (78.4%) patients.
Over the study period (7 years) there were 49 recurrent events documented at the rate of 3.1%.
Outcome data was available for 100% of patients at discharge and 87.8% of the MENA cohort and 77% of the non-MENA group at 90 days. There were 120 fatalities at 90 days, yielding a mortality rate of 7.6% with a significant discrepancy between the non-MENA and MENA cohorts:45 (4.7%) vs. 75 (12.2%; p < 0.001) respectively.
Dependency or death (mRS > 2) at discharge was seen in 621 (39.5%) patients and was significantly associated with increasing age (Figure 2), and proximal and multilocation involvement (p < 0.05).
At 90 days, dependency or death was seen in 349/1,276 (27.4%) and was significantly associated with increasing age (Figure 2), male sex, and having a MENA nationality (p < 0.05; Figure 3).
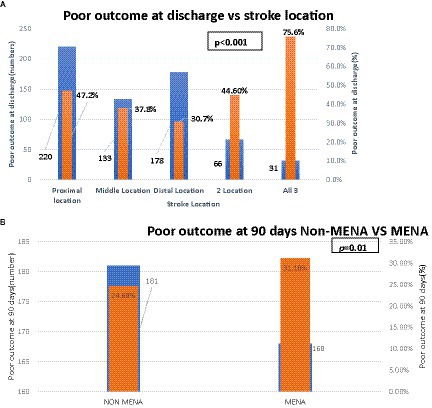
Figure 3. (A) Shows relationship between stroke location and poor outcomes at discharge. (B) Nationality and poor outcome at 90 days.
In a large multiethnic group encompassing individuals from the Middle East and North Africa (MENA) and South Asia, noteworthy distinctions were noted between the younger non-MENA subgroup and the older MENA subgroup concerning the prevalence of vascular risk factors, stroke localization, mortality rates, and outcomes at 90 days. Our research aligns with prior studies indicating a high prevalence of vascular risk factors and favorable outcomes in PCS patients (32). Notably, we observed increased dependency or mortality rates in the older male MENA cohort. This contributes more insights into the non-white population data, thereby enhancing the existing literature that has traditionally been predominantly focused on white populations or characterized by limited ethnic diversity.
The incidence of PCS almost doubled from 2014 to 2019, coinciding with the establishment of organized stroke services, the launch of the stroke database, better case ascertainment with increased utilization of magnetic resonance imaging (MRI), and an increase in the population. The dip in 2020 coincides with the COVID-19 pandemic where stroke admissions were observed to have diminished (33).
Compared to the historical NEMC-PCR study (6), our cohort showed similar age (average 61 years) and stroke location in the MENA group. In contrast, the South Asian non-MENA group was notably younger by a margin of 10 years, had a higher male-to-female ratio, and had a greater occurrence of proximal strokes. The higher representation of men in our cohort mirrors Qatar’s demographic skew toward men, primarily influenced by a significant presence of able-bodied South Asian blue-collar workers in the construction and gas sectors (34).
Both MENA and non-MENA groups in our study had high rates of vascular risk factors such as diabetes, hypertension, and dyslipidemia, aligning with findings from prior stroke cohorts in this region (17, 18) However, the older MENA group showed a higher incidence of CAD and AF. This emphasizes the necessity for effective screening and prevention programs at the primary health level.
Interestingly, the NEMC-PCR reported double the prevalence of CAD (35%) compared to our older MENA cohort. However, the incidence of AF was similar in both cohorts (34/407, 8.5%). It is noteworthy that the NEMC-PCR data was collected during a time when prolonged cardiac monitoring was not commonplace. As a result, there is a possibility that the prevalence of AF may have been underestimated, considering the significance of extended monitoring in identifying paroxysmal AF (35). Additionally, if taken at face value, the finding might suggest a lower prevalence of AF in the posterior circulation, as reported by Frid et al. (36).
The NIHSS scores were low in both the MENA and non-MENA cohorts, with a mean score of 3.8. This finding aligns with a large multicenter study conducted in Europe and North America (36) but is considerably lower than the scores reported in two Chinese cohorts (32, 37), 6.6 and 6.5, respectively. Low NIHSS scores in posterior circulation strokes are now widely recognized as a consequence of the scale’s limitations, primarily due to its focus on anterior circulation components (4).
Significant differences emerged between the MENA and non-MENA cohorts in stroke locations. The MENA group predominantly experienced distal strokes, followed by middle and proximal locations. Conversely, the non-MENA group had a higher frequency of proximal strokes, followed by distal and less frequently, middle locations (17, 18, 38).
This variation in stroke locations aligns with prior reports. Reports from predominantly white NEMC-PCR and a Chinese study (32) showed a similar prevalence of distal location strokes, whereas a Korean registry (38) highlighted middle PCS strokes as the most common. These differences in stroke locations might signal different underlying causes and potentially impact outcomes.
The predominance of distal location strokes in our population is likely due to small penetrating vessel disease (such as isolated thalamic lacunes) or artery-to-artery embolization from intracranial atherosclerosis, both prevalent stroke etiologies in our region, rather than cardioembolic strokes, as seen in reports from NEMC-PCR (17, 18, 20).
Limited data exists on the overall prognosis of PCS, although it is believed to be similar to anterior circulation strokes when typical prognostic factors are accounted for (39).
The 90-day fatality rate in our report was influenced by the lower fatality rate in the non-MENA cohort that comprised 60% of the total cohort (4.7%), aligning with the low stroke mortality seen in Qatar. This was similarly reported in the NEMC-PCR (16, 40). Possible explanations would include younger age, the prevalence of small vessel etiology, and advanced stroke care in Qatar (41). Conversely, the MENA subgroup demonstrated nearly triple the mortality rate compared to both the non-MENA cohort and the NEMC-PCR, exceeding previously reported stroke mortality rates in Qatari patients (18). This dichotomy in mortality and dependence between the older, more vascularly burdened MENA cohort and the younger, less vascularly burdened non-MENA group underscores age as a consistent factor linked to poorer outcomes at both early and 90-day intervals.
Moreover, the MENA group, despite matching the NEMC-PCR in age, sex distribution, and prevalence of distal stroke location, showed higher fatality rates, suggesting the presence of other critical prognostic factors warranting further investigation.
Involvement of the proximal segment corresponds to worse short-term outcomes, echoing earlier findings associating cerebellar infarction and significant brainstem lesions with heightened mortality and morbidity (42). Similarly, multi-segmental involvement, likely linked to cardioembolic and vertebrobasilar thromboembolism, correlates with poorer outcomes (6, 32).
The strength of this study lies in its origins as a prospective, extensive, and diverse dataset, uniquely established as a national database, thereby circumventing the constraints of conventional hospital-based registries. However, limitations of our research encompass the retrospective nature of data extraction and the presence of incomplete data at 90-day follow-up. Moreover, reliance on hospital-based registries is associated with potential errors in interpretation, documentation, and coding (43).
We described the incidence, clinical features, and outcomes of PCS in a multiethnic cohort. Our study highlights the increase in incidence over time and the high prevalence of vascular risk factors and relatively poor outcomes in older male MENA patients which stresses the need for effective prevention and management of these patients. Further studies are needed to investigate potential genetic or environmental risk factors for PCS and their impact on outcomes in different populations.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the Hamad Medical Corporation, Medical Research Center Institutional Review Board (research protocol 03-SI-17-075). The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants' legal guardians/next of kin due to the retrospective nature of the study.
YI: Conceptualization, Funding acquisition, Visualization, Writing – original draft, Writing – review & editing. PC: Formal analysis, Software, Validation, Writing – review & editing. RS: Formal analysis, Software, Validation, Writing – review & editing. IH: Data curation, Methodology, Project administration, Resources, Writing – review & editing. SAS: Methodology, Resources, Visualization, Writing – review & editing. MK: Resources, Writing – review & editing. NA: Investigation, Supervision, Writing – review & editing. SK: Investigation, Supervision, Writing – review & editing. SAJ: Investigation, Supervision, Writing – review & editing. AM: Investigation, Supervision, Writing – review & editing. KH: Investigation, Writing – review & editing. SH: Investigation, Writing – review & editing. JP: Formal analysis, Writing – review & editing. OE: Writing – review & editing. MAl: Writing – review & editing. LA: Investigation, Writing – review & editing. MAb: Writing – review & editing. SJ: Data curation, Writing – review & editing. DM: Data curation, Writing – review & editing. RU: Data curation, Writing – review & editing. ZB: Writing – review & editing. AAz: Writing – review & editing. AAy: Writing – review & editing. AE: Writing – review & editing. AO: Writing – review & editing. DD: Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
2. Hoyer, C, and Szabo, K. Pitfalls in the diagnosis of posterior circulation stroke in the emergency setting. Front Neurol. (2021) 12:682827. doi: 10.3389/fneur.2021.682827
3. Martin-Schild, S, Albright, KC, Tanksley, J, Pandav, V, Jones, EB, Grotta, JC, et al. Zero on the NIHSS does not equal the absence of stroke. Ann Emerg Med. (2011) 57:42–5. doi: 10.1016/j.annemergmed.2010.06.564
4. Alemseged, F, Rocco, A, Arba, F, Schwabova, JP, Wu, T, Cavicchia, L, et al. Posterior National Institutes of Health stroke scale improves prognostic accuracy in posterior circulation stroke. Stroke. (2022) 53:1247–55. doi: 10.1161/STROKEAHA.120.034019
5. Grewal, K, Austin, PC, Kapral, MK, Lu, H, and Atzema, CL. Missed strokes using computed tomography imaging in patients with vertigo: population-based cohort study. Stroke. (2015) 46:108–13. doi: 10.1161/STROKEAHA.114.007087
6. Caplan, LR, Wityk, RJ, Glass, TA, Tapia, J, Pazdera, L, Chang, HM, et al. New England Medical Center posterior circulation registry. Ann Neurol. (2004) 56:389–98. doi: 10.1002/ana.20204
7. Pirson, FAV, Boodt, N, Brouwer, J, Bruggeman, AAE, Hinsenveld, WH, Staals, J, et al. Etiology of large vessel occlusion posterior circulation stroke: results of the MR CLEAN registry. Stroke. (2022) 53:2468–77. doi: 10.1161/STROKEAHA.121.038054
8. Zhang, C, Li, Z, Liu, L, Pu, Y, Zou, X, Yan, H, et al. Posterior circulation stroke due to intracranial artery disease in the Chinese population. Brain Behav. (2022) 12:e2717. doi: 10.1002/brb3.2717
9. Jalali, N, Sadeghi Hokmabadi, E, Ghoreishi, A, Sariaslan, P, Rafie, S, Borhani-Haghighi, A, et al. Outcome predictors in anterior and posterior ischemic strokes: a study based on the Iranian SITS registry. Sci Rep. (2023) 13:1231. doi: 10.1038/s41598-023-28465-8
10. Singh, K, Kondal, D, Mohan, S, Jaganathan, S, Deepa, M, Venkateshmurthy, NS, et al. Health, psychosocial, and economic impacts of the COVID-19 pandemic on people with chronic conditions in India: a mixed methods study. BMC Public Health. (2021) 21:685. doi: 10.1186/s12889-021-10708-w
11. Gardener, H, Sacco, RL, Rundek, T, Battistella, V, Cheung, YK, and Elkind, MSV. Race and ethnic disparities in stroke incidence in the northern Manhattan study. Stroke. (2020) 51:1064–9. doi: 10.1161/STROKEAHA.119.028806
12. Thompson, SG, Barber, PA, Gommans, JH, Cadilhac, DA, Davis, A, Fink, JN, et al. The impact of ethnicity on stroke care access and patient outcomes: a New Zealand nationwide observational study. Lancet Reg Health West Pac. (2022) 20:100358. doi: 10.1016/j.lanwpc.2021.100358
13. Tran, J, Mirzaei, M, Anderson, L, and Leeder, SR. The epidemiology of stroke in the Middle East and North Africa. J Neurol Sci. (2010) 295:38–40. doi: 10.1016/j.jns.2010.05.016
14. Al Hashmi, AM, Shuaib, A, Imam, Y, Amr, D, Humaidan, H, Al Nidawi, F, et al. Stroke services in the Middle East and adjacent region: a survey of 34 hospital-based stroke services. Front Neurol. (2022) 13:1016376. doi: 10.3389/fneur.2022.1016376
15. Merwick, Á, and Werring, D. Posterior circulation ischaemic stroke. BMJ. Br Med J. (2014) 348:g3175. doi: 10.1136/bmj.g3175
16. Akhtar, N, Kamran, SI, Deleu, D, D'Souza, A, Miyares, F, Elsotouhy, A, et al. Ischaemic posterior circulation stroke in State of Qatar. Eur J Neurol. (2009) 16:1004–9. doi: 10.1111/j.1468-1331.2009.02709.x
17. Imam, YZ, Kamran, S, Akhtar, N, Deleu, D, Singh, R, Malik, RA, et al. Incidence, clinical features and outcomes of atrial fibrillation and stroke in Qatar. Int J Stroke. (2020) 15:85–9. doi: 10.1177/1747493019830577
18. Imam, YZ, Kamran, S, Saqqur, M, Ibrahim, F, Chandra, P, Perkins, JD, et al. Stroke in the adult Qatari population (Q-stroke) a hospital-based retrospective cohort study. PLoS One. (2020) 15:e0238865. doi: 10.1371/journal.pone.0238865
19. Qatar Poulation Available at: https://www.psa.gov.qa/en/statistics1/statisticssite/pages/popmobile.aspx (Accessed July 12, 2023).
20. Imam, YZ, Akhtar, N, Kamran, S, Garcia-Bermejo, P, Al Jerdi, S, Zakaria, A, et al. Rescue stent placement for acute ischemic stroke with large vessel occlusion refractory to mechanical Thrombectomy: a multiethnic middle eastern/African/Asian cohort. J Vasc Interv Radiol. (2023) 34:1740–8. doi: 10.1016/j.jvir.2023.06.005
21. United Nations Geoscheme Available at: https://unstats.un.org/unsd/methodology/m49/United (n.d.)
22. American Diabetes Assoiation . Diagnosis and classification of diabetes mellitus. Diabetes Care. (2012) 35:S64–71. doi: 10.2337/dc12-s064
23. Catapano, AL, Graham, I, De Backer, G, Wiklund, O, Chapman, MJ, Drexel, H, et al. 2016 ESC/EAS guidelines for the Management of Dyslipidaemias. Eur Heart J. (2016) 37:2999–3058. doi: 10.1093/eurheartj/ehw272
24. Williams, B, Mancia, G, Spiering, W, Agabiti Rosei, E, Azizi, M, Burnier, M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur Heart J. (2018) 39:3021–104. doi: 10.1093/eurheartj/ehy339
25. Montalescot, G, Sechtem, U, Achenbach, S, Andreotti, F, Arden, C, Budaj, A, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the task force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J. (2013) 34:2949–3003. doi: 10.1093/eurheartj/eht296
26. January, CT, Wann, LS, Alpert, JS, Calkins, H, Cigarroa, JE, Cleveland, JCJr, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association task force on practice guidelines and the Heart Rhythm Society. Circulation. (2014) 130:2071–104. doi: 10.1161/CIR.0000000000000040
27. Kwah, LK, and Diong, J. National Institutes of Health stroke scale (NIHSS). J Physiother. (2014) 60:61. doi: 10.1016/j.jphys.2013.12.012
29. Adams, HP Jr, Bendixen, BH, Kappelle, LJ, Biller, J, Love, BB, Gordon, DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of org 10172 in acute stroke treatment. Stroke. (1993) 24:35–41. doi: 10.1161/01.STR.24.1.35
30. Banks, JL, and Marotta, CA. Outcomes validity and reliability of the modified Rankin scale: implications for stroke clinical trials: a literature review and synthesis. Stroke. (2007) 38:1091–6. doi: 10.1161/01.STR.0000258355.23810.c6
31. Sullivan, KM, Dean, A, and Soe, MM. Open epi: a web-based epidemiologic and statistical calculator for public health. Public Health Rep. (2009) 124:471–4. doi: 10.1177/003335490912400320
32. Han, Y, Xu, M, Zhao, Y, and Zhang, Y. Long-term outcome and prognostic factors of posterior circulation ischemia patients: results from a single center retrospective study. Vascular. (2020) 28:25–30. doi: 10.1177/1708538119866604
33. Akhtar, N, Kamran, S, Al-Jerdi, S, Imam, Y, Joseph, S, Morgan, D, et al. Trends in stroke admissions before, during and post-peak of the COVID-19 pandemic: a one-year experience from the Qatar stroke database. PLoS One. (2022) 17:e0255185. doi: 10.1371/journal.pone.0255185
34. Imam, Y, Al-Salahat, A, Aljurdi, S, Mahfoud, Z, Reyes, CZ, Akhtar, N, et al. Stroke in airplane passengers: a study from a large international hub. J Stroke Cerebrovasc Dis. (2022) 31:106452. doi: 10.1016/j.jstrokecerebrovasdis.2022.106452
35. Imam, YZ, D'Souza, A, Malik, RA, and Shuaib, A. Secondary stroke prevention: improving diagnosis and management with newer technologies. Transl Stroke Res. (2016) 7:458–77. doi: 10.1007/s12975-016-0494-2
36. Frid, P, Drake, M, Giese, AK, Wasselius, J, Schirmer, MD, Donahue, KL, et al. Detailed phenotyping of posterior vs. anterior circulation ischemic stroke: a multi-center MRI study. J Neurol. (2020) 267:649–58. doi: 10.1007/s00415-019-09613-5
37. Tao, WD, Kong, FY, Hao, ZL, Lin, S, Wang, DR, Wu, B, et al. One-year case fatality and disability after posterior circulation infarction in a Chinese hospital-based stroke study. Cerebrovasc Dis. (2010) 29:376–81. doi: 10.1159/000281836
38. Lee, JH, Han, SJ, Yun, YH, Choi, HC, Jung, S, Cho, SJ, et al. Posterior circulation ischemic stroke in Korean population. Eur J Neurol. (2006) 13:742–8. doi: 10.1111/j.1468-1331.2006.01274.x
39. Markus, HS, and Michel, P. Treatment of posterior circulation stroke: acute management and secondary prevention. Int J Stroke. (2022) 17:723–32. doi: 10.1177/17474930221107500
40. Jallow, E, Al Hail, H, Han, TS, Sharma, S, Deleu, D, Ali, M, et al. Current status of stroke in Qatar: including data from the BRAINS study. JRSM Cardiovasc Dis. (2019) 8:204800401986916. doi: 10.1177/2048004019869160
41. Akhtar, N, Kamran, S, Singh, R, Cameron, P, D'Souza, A, Imam, Y, et al. Beneficial effects of implementing stroke protocols require establishment of a geographically distinct unit. Stroke. (2015) 46:3494–501. doi: 10.1161/STROKEAHA.115.010552
42. Salerno, A, Strambo, D, Nannoni, S, Dunet, V, and Michel, P. Patterns of ischemic posterior circulation strokes: a clinical, anatomical, and radiological review. Int J Stroke. (2022) 17:714–22. doi: 10.1177/17474930211046758
Keywords: observational, incidence, clinical features, posterior circulation stroke, multiethnic, outcomes
Citation: Imam YZ, Chandra P, Singh R, Hakeem I, Al Sirhan S, Kotob M, Akhtar N, Kamran S, Al Jerdi S, Muhammad A, Haroon KH, Hussain S, Perkins JD, Elalamy O, Alhatou M, Ali L, Abdelmoneim MS, Joseph S, Morgan D, Uy RT, Bhutta Z, Azad A, Ayyad A, Elsotouhy A, Own A and Deleu D (2024) Incidence, clinical features, and outcomes of posterior circulation ischemic stroke: insights from a large multiethnic stroke database. Front. Neurol. 15:1302298. doi: 10.3389/fneur.2024.1302298
Received: 26 September 2023; Accepted: 08 January 2024;
Published: 07 February 2024.
Edited by:
Sonu M. M. Bhaskar, Liverpool Hospital and South West Sydney Local Health District (SWSLHD), AustraliaReviewed by:
Sebastian F. Ameriso, Fundación Para la Lucha Contra las Enfermedades Neurológicas de la Infancia (FLENI), ArgentinaCopyright © 2024 Imam, Chandra, Singh, Hakeem, Al Sirhan, Kotob, Akhtar, Kamran, Al Jerdi, Muhammad, Haroon, Hussain, Perkins, Elalamy, Alhatou, Ali, Abdelmoneim, Joseph, Morgan, Uy, Bhutta, Azad, Ayyad, Elsotouhy, Own and Deleu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yahia Z. Imam, eWltYW1AaGFtYWQucWE=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.