- 1College of Acupuncture and Massage, Henan University of Chinese Medicine, Zhengzhou, China
- 2Department of Tuina, The Third Affiliated Hospital of Henan University of Chinese Medicine, Zhengzhou, China
- 3Central Hospital of Jiaozuo, Jiaozuo, China
- 4College of Computer Science, Xidian University, Xian, China
- 5College of Acupuncture and Massage, Shanghai University of Chinese Medicine, Shanghai, China
Background: The annual incidence of insomnia continues to increase owing to changes in lifestyle habits, increased work pressure, and increased environmental pollution. In recent years, an increasing number of external therapies have been proven effective in treating insomnia and have been widely used. However, the relative benefits and harms of external therapies remain uncertain, and an optimal treatment strategy has not yet been determined.
Objectives: A network meta-analysis was performed to evaluate and compare the efficacy and safety of multiple external therapies for patients with insomnia.
Methods: Eight electronic databases were comprehensively searched from their inception to June 2023 for relevant literature. We also searched the grey literature and reviewed the reference lists of related systematic reviews. Two independent reviewers performed the study selection, data extraction, and bias assessment of the included randomized controlled trials (RCTs) using the Cochrane Reviewers’ Handbook, and a network meta-analysis was conducted using Stata and RevMan software.
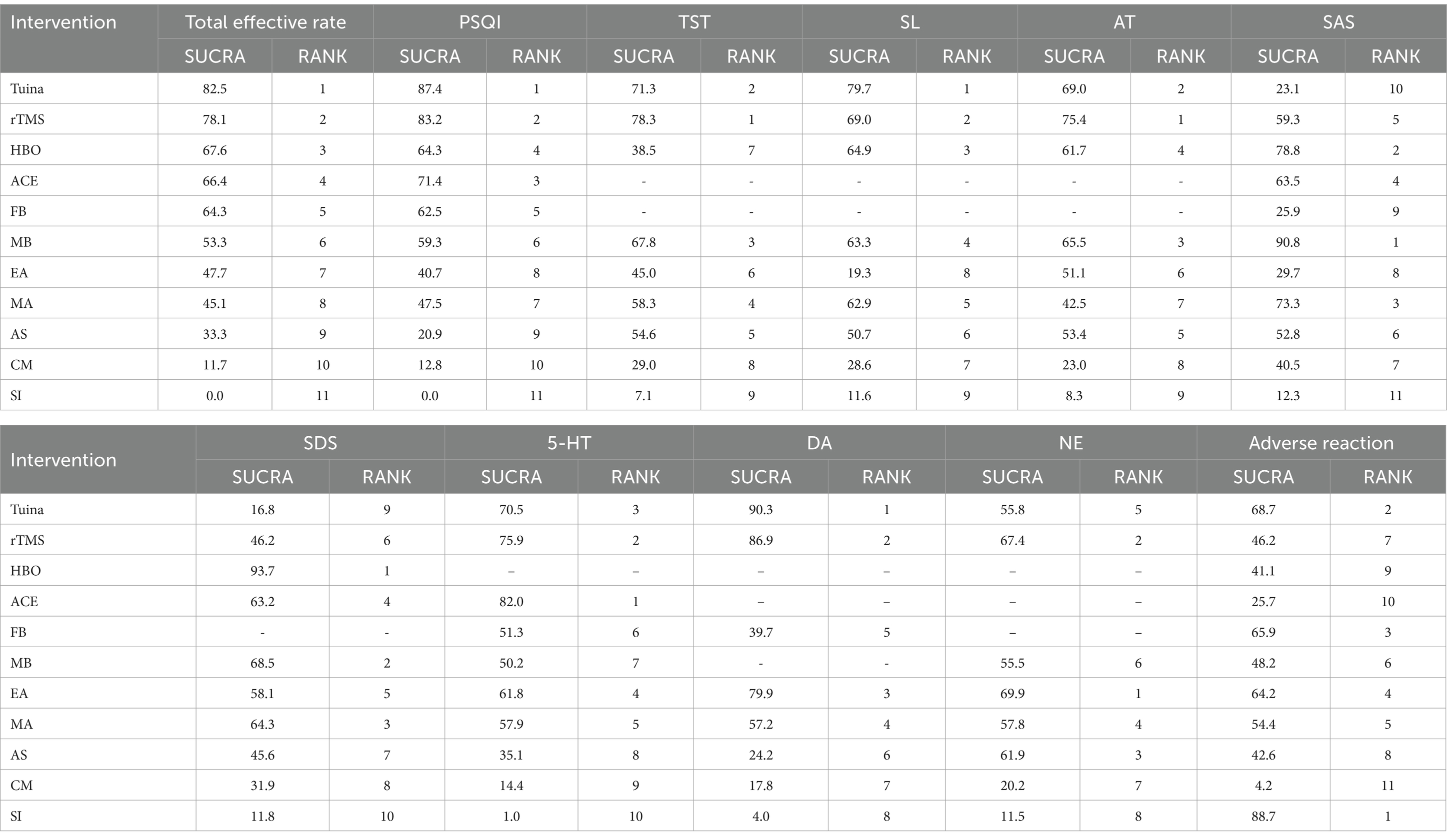
Results: In total, 14,826 studies were identified. Of these, 83 studies, including 9 external therapies and 6,100 patients, were deemed eligible for the present network meta-analysis. Except for the SL outcome, each external therapy was better than conventional medicine and the sham intervention (SI) in improving sleep quality. In terms of improving the psychological state indices of insomnia patients, each external therapy was superior to the SI; each external therapy had a better effect on the regulation of monoamine neurotransmitters. Tuina may be the most effective intervention in improving the total effective rate, Pittsburgh sleep quality index score, and SL. Repetitive transcranial magnetic stimulation (rTMS) perhaps resulted in the best improvement in total sleep time and awakening time (surface under the cumulative ranking curve [SUCRA] = 78.3 and 75.4%, respectively); and moxibustion (MB) and hyperbaric oxygen (HBO) were the most effective in reducing Self-rating Anxiety Scale and Self-rating Depression Scale scores. In terms of improving the monoamine neurotransmitters 5-hydroxytryptamine, norepinephrine, and dopamine, the best interventions were acupoint catgut embedding, electroacupuncture, and Tuina (SUCRA = 82.0, 69.9 and 90.3%, respectively). Safety results showed that the three safest interventions were the SI, Tuina, and foot bath. No serious adverse events were reported across the studies, and the most common minor adverse events included drowsiness, pain, excessive thirst, and hematoma.
Conclusion: Both Tuina and rTMS have significant effects on improving sleep quality, but the safety of rTMS is low. Therefore, Tuina can be recommended as the first line of treatment to improve sleep quality. If a patient’s anxiety and depression symptoms are evident, MB or HBO can be selected for treatment based on the actual situation. External therapy to improve sleep quality may be related to the regulation of monoamine neurotransmitters, which may be a potential mechanism of action.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=440882.
1 Introduction
Insomnia is a sleep disorder characterized by difficulty falling asleep, easy awakening, and early waking, and is a common clinical condition (1, 2). With the increasing work pressure and the accelerated pace of life, the incidence of insomnia is increasing annually and the disease can last for more than 10 years in severe cases (3, 4). A chronic lack of sleep can lead to emotional and mental problems such as anxiety and depression (5). Recent studies have shown that the severity of anxiety and depression positively correlates with the occurrence of insomnia (6, 7). The mechanisms of insomnia are complex and related to a variety of neurotransmitters (8). It is widely recognized that abnormal levels or reduced function of neurotransmitters underly the pathophysiology of insomnia (9, 10). Drug treatments for insomnia are commonly used and have the advantages of being easy to take, fast-acting, and long-lasting. However, the incidence of adverse effects is high, and it is more difficult for patients to adhere to treatment (11–13). Therefore, it is necessary to explore alternative therapies with significant, curative, stable, and safe effects.
Attention to non-pharmacological therapies is increasing because of concerns about the safety of pharmaceutical treatments. Non-pharmacological therapies mainly include external therapy, exercise and cognitive behavioral therapy. Because exercise and cognitive behavioral therapy make it difficult for patients to adhere, more and more patients choose external therapy for treatment. External therapy is a method of treatment from outside the body using instruments, needles and human fingers, which is greener and safer than drug therapy. Relevant studies (14, 15) have found that external therapies for insomnia have the advantages of significant efficacy, good safety profiles, and few adverse effects, and have become a popular topic in recent years. Several guidelines and consensuses (16, 17) list external treatments as the recommended intervention for the clinical treatment of insomnia. External therapies include modern medical and traditional Chinese medicine (TCM) treatments (18). Modern medical treatments include repetitive transcranial magnetic stimulation (rTMS), hyperbaric oxygen, electroencephalography (EEG) biofeedback, and laser therapy, whereas TCM treatments primarily include acupuncture, Tiuna, auricular stimulation, and moxibustion (19).
Different types of external therapies have different effects and advantages. Several traditional meta-analysis (20–22) have proven that external treatment of insomnia has advantages, but they are more focused on the comparisons of a single external therapy with drugs or another external therapy and did not compare multiple external therapies simultaneously. As the number of alternative treatment options increases, comparative effectiveness and safety studies are necessary (23). To date, no meta-analyses have comprehensively compared and evaluated the efficacy and safety of multiple types of external therapies. Thus, it is unknown which intervention measures have the best effects. Moreover, most systematic reviews focus only on the changes in insomnia-related indicators, mostly using subjective scale evaluations, and fail to explore the changes in the psychological state and neurotransmitter levels of insomnia patients under the intervention of external therapy. Therefore, a network meta-analysis was performed to simultaneously analyze both direct and indirect evidence from different studies, estimate the relative effectiveness and safety of all interventions, and rank the order of the interventions (24, 25). The aim of this study was to systematically evaluate the effects of external therapies on the psychological state and neurotransmitters of patients with insomnia based on the evaluation of insomnia-related indicators.
2 Methods
2.1 Inclusion criteria
2.1.1 Participants
All studies met the recognized diagnostic criteria for insomnia (26–29), regardless of age, sex, or race.
2.1.2 Interventions
The trial group received external therapy alone, in which drug involvement was excluded, including acupoint catgut embedding (ACE), rTMS, tuina, hyperbaric oxygen (HBO), electroacupuncture (EA), moxibustion (MB), foot bath (FB), manual acupuncture (MA), and auricular stimulation (AS).
2.1.3 Controls
The control group included patients receiving conventional medicine (CM), sham intervention (SI), or any of the external therapies mentioned above (e.g., HBO vs. MB). To reduce heterogeneity, only benzodiazepines were used in CM.
2.1.4 Outcomes
2.1.4.1 Sleep quality
The following outcome measures were used to assess sleep quality: (1) The total effective rate, referring to efficacy standards formulated by the State Administration of Traditional Chinese Medicine and American Psychiatric Association (27, 28). The total effective rate is calculated as follows: [(Cure + marked effect + effective) number of cases ÷ total number of cases] × 100%; (2) Pittsburgh sleep quality index (PSQI); and (3) Data from polysomnography (PSG) including total sleep time (TST), sleep onset latency (SOL), and awakening time (AT).
2.1.4.2 Psychological state
The Self-rating Anxiety Scale (SAS) and Self-rating Depression Scale (SDS) were used to assess the patients’ psychological status.
2.1.4.3 Neurotransmitter level
The levels of 5-hydroxytryptamine (5-HT), dopamine (DA), and norepinephrine (NE) were analyzed.
2.1.4.4 Adverse reaction
The incidence of adverse reactions was used to evaluate the safety of the intervention.
All RCTs that contained at least one outcome indicator were eligible for inclusion in the network meta-analysis (NMA).
2.1.5 Study design and registration
This study followed the Preferred Reporting Items for Systematic Reviews and Meta-analysis network meta-analysis (PRISMA-NMA) guidelines (30) and was registered with PROSPERO (registration number: CRD42023440882).
2.2 Exclusion criteria
Exclusion criteria included: (1) Non-RCTs; (2) repeated publications; (3) inconsistent interventions; (4) no reference or homemade diagnostic criteria; (5) inability to obtain full text and outcomes; and (6) serious complications.
2.3 Information sources
The Cochrane Library, Embase, PubMed, Web of Science, Chinese Biomedical Databases, VIP, Chinese National Knowledge Infrastructure, and Wanfang databases were searched for relevant studies. We also searched the grey literature and reviewed the reference lists of the included studies and related systematic reviews. There were no restrictions regarding language, study type, date of publication, or status of publication. The retrieval strategy used a combination of subject headings and free words, and the databases were searched from inception until June 30, 2023. Each database search strategy is shown in Supplementary Figure S1 and Supplementary Table S1.
2.4 Study selection
Two researchers independently screened the studies based on the inclusion criteria. After extracting the data, they crosschecked each other’s results. Disagreements were resolved through consultation with a third party. EndNote software was used to check for duplicate publications. The investigators then screened the titles and abstracts of each study and excluded studies that did not meet the inclusion criteria. Subsequently, the investigators read the full texts of the remaining studies to decide whether to include them. If the literature was incomplete, the authors of the original studies were contacted to obtain detailed data.
2.5 Data collection
Two reviewers independently extracted the data from each eligible RCT using a standardized form. Disagreements were resolved through consultation with a third party. The extracted data included study characteristics (author, country, and publication date), patient characteristics (sample size, disease duration, sex, and age), intervention measures, treatment course, and outcome indicators.
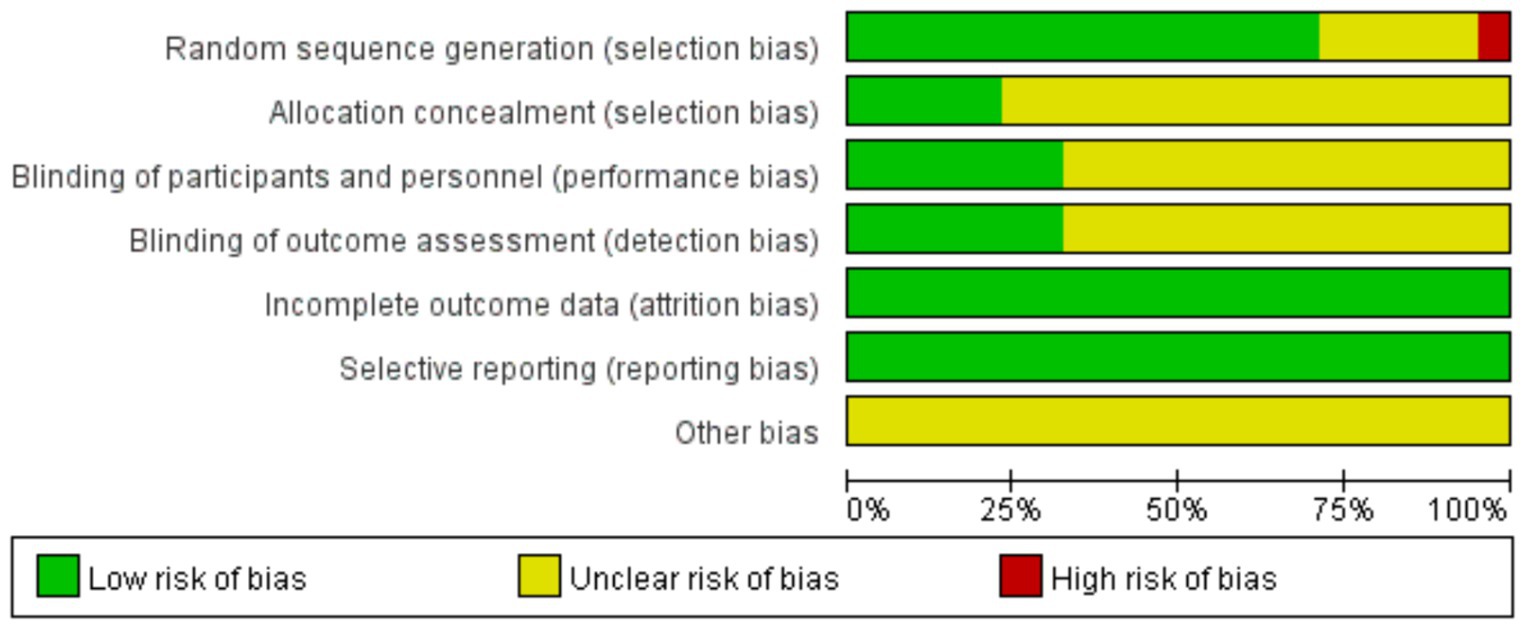
2.6 Risk of bias assessment
The risk of bias in the literature was evaluated by two independent investigators using the risk of bias assessment tool in the Cochrane Reviewers Handbook (31). The following seven aspects were evaluated to determine the risk of bias: random sequence generation, allocation concealment, implementation of a blind method for patients and trial personnel, implementation of a blind method for outcome assessors, incomplete result data, selective reporting, and other biases (such as potential bias related to special study designs and false statements). Eventually, a judgment on “low risk,” “high risk,” and “unclear risk” in the selected literatures was made.
2.7 Data synthesis and analysis
All outcome indicators were analyzed using random- or fixed-effects models based on the level of heterogeneity. The p values of the chi-square test and the I2 index in the heterogeneity test were used to indicate the level of statistical heterogeneity. When the level of heterogeneity was low, the data was analyzed using the fixed effects model (p ≥ 0.1 and I2 < 50%); otherwise, the random effects model (p < 0.1 or I2 > 50%) was used (32, 33). Relative risk (RR) was used as the effect size for dichotomous variables and the standardized mean difference (SMD) was used as the effect size for continuous variables to calculate the 95% confidence interval (CI).
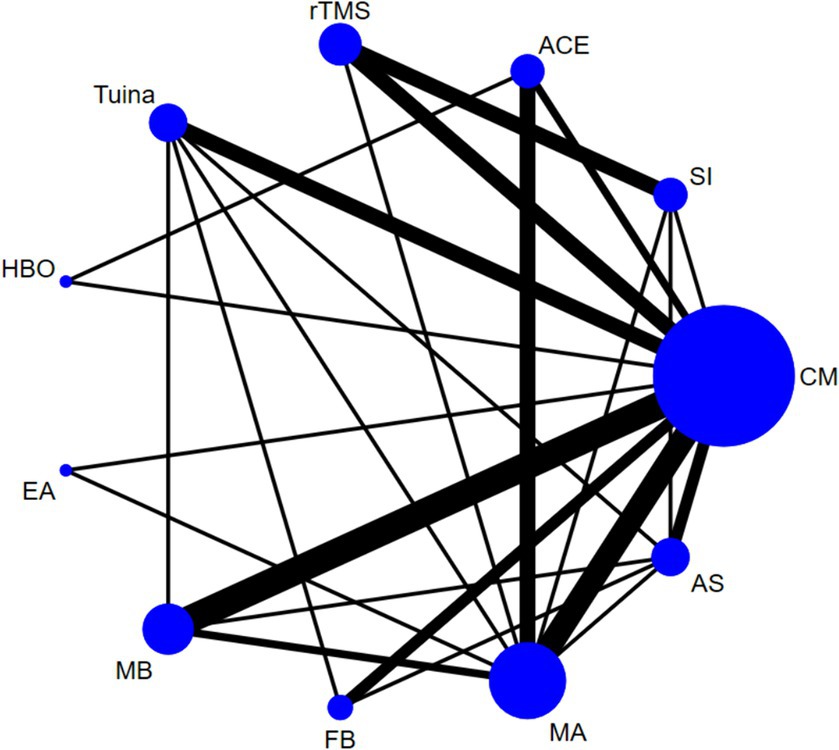
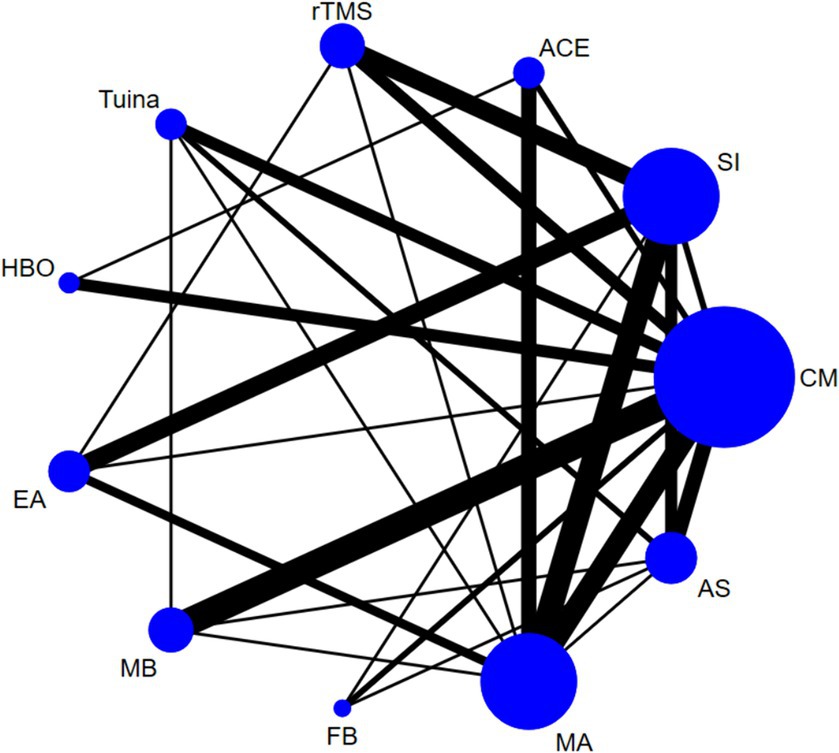
Based on the Bayesian model, Stata software (version 16.0) was used for network meta-analysis. The data was preprocessed using the network group command, and an evidence network diagram for each indicator was drawn. The curative effect of the indicators was sorted to obtain the surface under the cumulative ranking curve (SUCRA), and probability sorting was plotted. The dots in the evidence network diagram represent an intervention; the larger the area, the greater the number of patients with the intervention. The line connecting the two dots indicates a direct comparison between the two interventions, and the thickness of the line represents the number of included studies (34, 35). SUCRA is expressed as a percentage. A larger percentage indicates that the intervention has the highest probability of becoming the preferred option, and a value of zero indicates that the intervention may be completely ineffective (36, 37). When a closed loop exists, the node-splitting method is used to check for inconsistencies. When the number of studies on the outcome indicator was >10, a funnel plot was drawn to determine the possibility of a small sample effect. To test the robustness of the main findings, some factors that might influence the level of precision of the main outcome were removed, a sensitivity analysis was performed, and the quality of the literature was evaluated using Review Manager 5.4 software.
3 Results
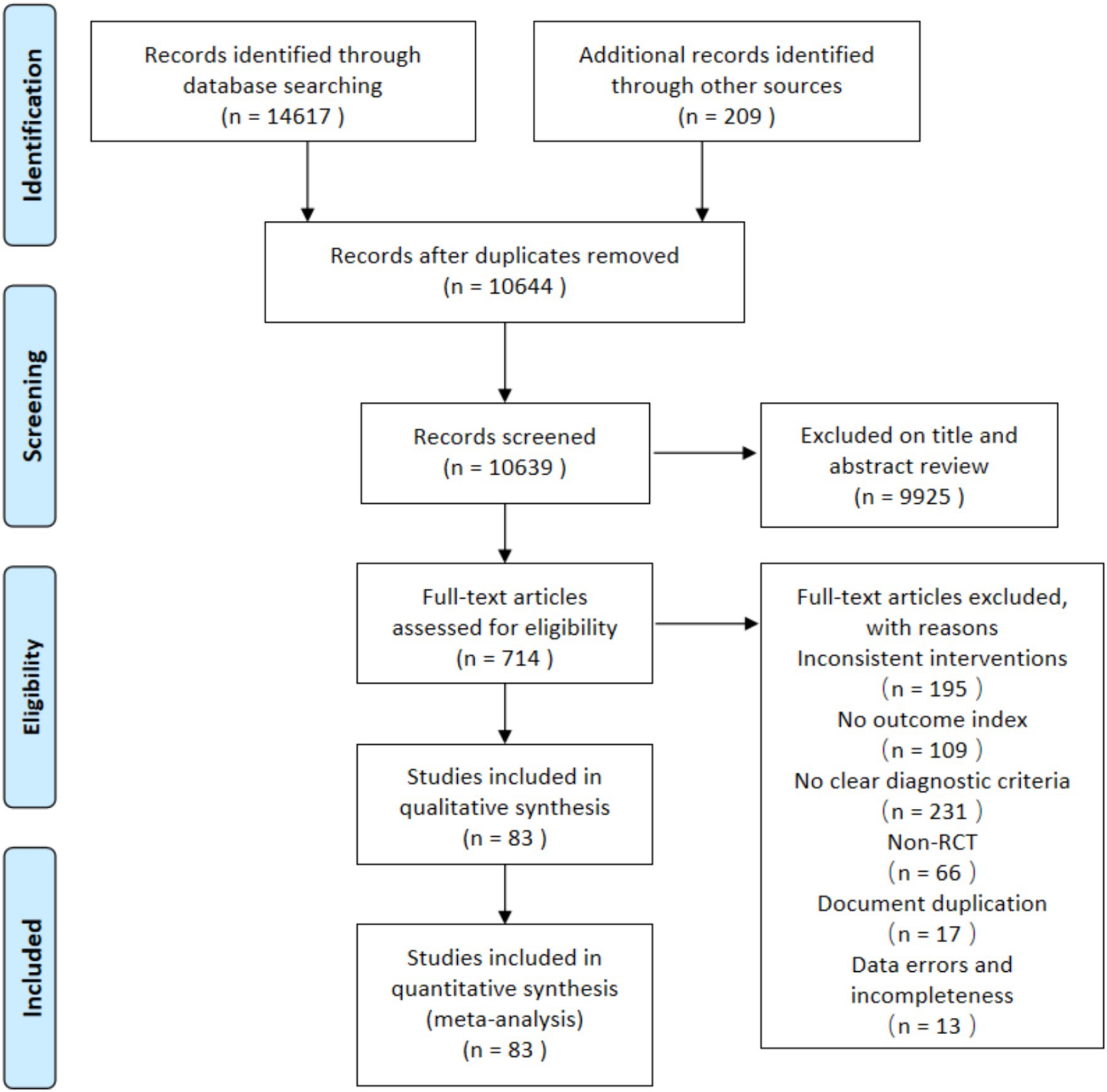
A total of 14,826 articles were retrieved from the initial search, of which 14,617 were from databases and 209 were from other sources. Among the literatures retrieved in the database, 4,239 were from CNKI, 2611 VIP, 3846 Wanfang, 2,973 CBM, 97 Embase, 205 Cochrane Library, 382 PubMed, and 264 Web of Science. Then, 714 were moved to full-text screening after title and abstract screening. Finally, we included 83 RCTs (38–120) in our meta-analysis, of which eight studies (38, 41, 54, 73, 77, 95, 112, 120) were three-arm trials and the remaining studies were two-arm trials. The screening flowchart is shown in Figure 1.
3.1 Study characteristics
Supplementary Table S2 summarizes the characteristics of the 83 RCTs, with sample sizes ranging from 32 to 153, involving 6,100 participants with a mean age of 18–68 years; nine external therapies, including ACE, rTMS, Tuina, HBO, EA, MB, FB, MA, and AS. Descriptions of each intervention are presented in Supplementary Table S3.
3.2 Risk of bias
Of the 83 included RCTs, 18 (57, 58, 73–77, 82, 98, 104–109, 113, 114, 119) were published in English, and the remainder were published in Chinese. The studies had comparable general information between the control and trial groups. Seventy-nine studies reported specific schemes for random sequence generation, with 41 (38, 42, 44, 46, 47, 50, 51, 53, 56, 60, 62, 64–66, 68, 70, 71, 73, 74, 80–86, 88, 90, 91, 96, 98–103, 110, 112, 114, 119, 120) using the random number table method and 17 (40, 43, 61, 72, 75–78, 89, 97, 104–109, 113) using the envelope method. One study (45) was rated as low risk using the coin-toss method for random allocation, two (39, 63) were rated as high risk according to the order of consultation, two (67, 87) were randomized according to different treatments, and the remaining 20 studies mentioned randomization only. Twenty-seven studies mentioned the implementation of blinding: 21 (40, 43, 59, 61, 64, 72–76, 78, 97, 99, 104, 106–109, 112, 113, 115) were single-blinded, six (58, 77, 89, 92, 105, 114) were double-blinded, 19 (40, 43, 61, 64, 72, 75–78, 89, 97, 104–109, 113, 114) used allocation concealment rated as low risk, and the remaining studies did not mention blinding or allocation concealment. All 83 studies reported on the outcome indicators used in this study, and the studies did not identify falsified or incomplete data, with incomplete reporting and early discontinuation of trials rated as low risk. No other biases were mentioned in any of the studies. The results are shown in Figure 2, and a summary of the risk of bias is shown in Supplementary Figure S2.
3.3 Network meta-analysis
The results of the heterogeneity test showed high heterogeneity for all outcome indicators (p < 0.05, I2 > 50%). Therefore, a random-effects model was used for all the meta-analyses in this study. The heterogeneity results are presented in Supplementary Table S4. Except for 5-HT, NE, and DA, the evidence network diagrams of the outcome indicators were closed loops. The node-splitting method showed good consistency with no heterogeneity emerging between the studies (p > 0.05). The results of the node-splitting tests are listed in Supplementary Tables S5–S12.
3.3.1 Sleep quality
3.3.1.1 Total effective rate
Forty-four studies (38–43, 45, 46, 48, 50, 51, 54–56, 62–65, 68, 71, 78–81, 83–88, 90, 92, 94–96, 99, 101–103, 110, 113, 115, 116, 119, 120) reported the total effective rate, involving 3,223 participants and 11 interventions. Thus, 55 two-by-two comparisons were formed, and the evidence network was generally centered on the CM, thereby forming 19 closed loops (see Figure 3). Compared to SI, all external therapies and CM showed a better effect on the total effective rate (p < 0.05). Except for EA and AS, external therapies were superior to CM in improving the total effective rate (p < 0.05). There were no significant differences in most comparisons between the external treatments (p > 0.05) (Figure 4).
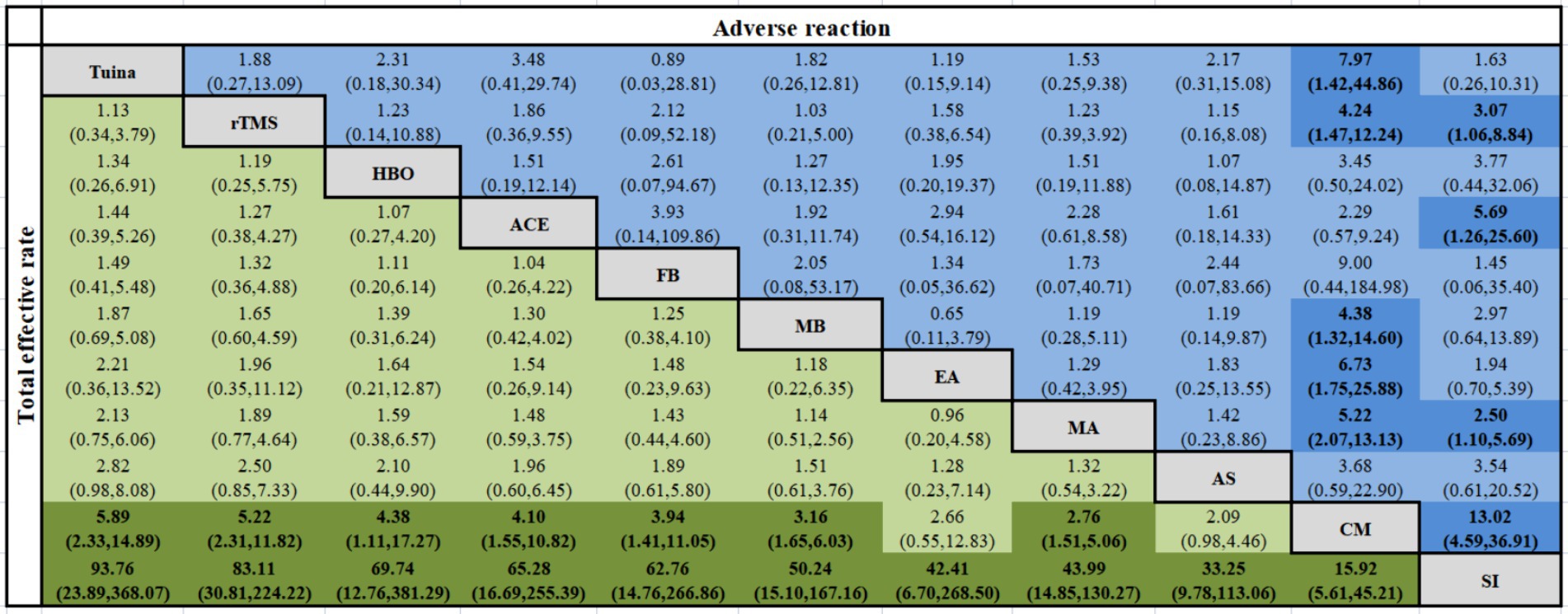
Figure 4. Network meta-analysis of the total effective rate and adverse reaction rate [RR (95% CI)].
3.3.1.2 PSQI
Seventy studies (38–43, 45, 47–50, 53–69, 71–86, 88–91, 93, 94, 97–104, 106–108, 110, 112–120) reported the PSQI score, involving 5,224 participants and 11 interventions; thus, 55 two-by-two comparisons were formed, with an overall network of evidence centered on CM, thereby forming 24 closed loops (see Figure 5). The results of the NMA showed that Tuina, rTMS, ACE, and MB significantly reduced the PSQI score compared with AS, and Tuina, rTMS, ACE, HBO, FB, MB, and MA were better than CM. Compared with SI, all external treatments and CM showed a better effect on decreasing the PSQI total scores. All the above-mentioned differences were statistically significant (p < 0.05), as shown in Supplementary Figure S12.
3.3.1.3 TST
Twenty-three studies (46, 48, 51, 52, 57, 60, 61, 66, 67, 73–77, 81, 101, 104–106, 109, 110, 112, 118) reported the TST, involving 1,814 participants and 9 interventions. Thus, 36 two-by-two comparisons were formed, and the evidence network was generally centered on the SI, leading to eight closed loops (see Supplementary Figure S3). Compared with SIs, rTMS (MD = 51.23, 95% CI [15.57, 86.89]), MA (MD = 36.43, 95% CI [13.49, 59.38]), and EA (MD = 28.55, 95% CI [3.57, 53.54]) significantly improved the TST (p < 0.05), as shown in Supplementary Figure S12.
3.3.1.4 SL
Twenty-one studies (46, 48, 51–53, 56, 57, 60, 61, 66, 67, 73, 74, 76, 81, 101, 104–106, 110, 118) reported SL, involving 1,631 participants and 9 interventions. Thus, 36 two-by-two comparisons were formed with an overall network of evidence centered on CM, thereby forming six closed loops (see Supplementary Figure S4). Compared with SI, rTMS (MD = −12.48, 95% CI [−22.95, −2.01]) and MA (MD = −11.34, 95% CI [−20.06, −2.62]) significantly reduced SL. rTMS (MD = −10.88, 95% CI [−21.56, −0.19]) was a superior intervention to CM. All the abovementioned differences were statistically significant (p < 0.05), as shown in Supplementary Figure 13.
3.3.1.5 AT
Fourteen studies (6, 48, 51–53, 60, 61, 66, 67, 75, 77, 81, 101, 112) reported SL, involving 1,089 participants and 9 interventions. Thus, 36 two-by-two comparisons were formed, and the evidence network was generally centered on CM, thereby forming five closed loops (see Supplementary Figure S5). The results of the NMA showed that rTMS was a better intervention than CM and SI [MD = −1.31, 95% CI (−2.42, −0.20); MD = −2.01, 95% CI (−3.56, −0.46)], respectively; p < 0.05) (Supplementary Figure S13).
3.3.2 Psychological state
3.3.2.1 SAS
Eighteen studies (42, 45, 47, 56, 63, 70, 75, 82, 83, 87, 93, 96, 101, 103, 108, 109, 115, 116) reported SL, involving 1,462 participants and 11 interventions. Thus, 55 two-by-two comparisons were formed, with an overall network of evidence centered on CM, thereby forming only one closed loop (see Supplementary Figure S6). The results of the NMA showed that MB, HBO, MA, and rTMS significantly reduced the SAS score compared to SI. MA (MD = −5.52, 95% CI [−10.96, −0.08]) was a better intervention than CM. Compared with Tuina, MB (MD = -14.68, 95% CI [−27.90, −1.47]) was more effective at reducing SAS scores. All the abovementioned differences were statistically significant (p < 0.05), as shown in Supplementary Figure S14.
3.3.2.2 SDS
Nineteen studies (42, 45, 47, 56, 63, 70, 73, 75, 77, 82, 87, 89, 99, 101, 103, 108, 109, 115, 116) reported SL, involving 1,555 participants and 10 interventions. Thus, 45 two-by-two comparisons were formed, and the evidence network was generally centered on the MA, thereby forming two closed loops (see Supplementary Figure S7). Compared to SI, MB, HBO, MA, and EA significantly reduced the SDS score. HBO was a better intervention than CM (MD = −17.39, 95% CI [−32.19, −2.59]) and Tuina (MD = −23.02, 95% CI [−43.73, −2.31]). All the abovementioned differences were statistically significant (p < 0.05), as shown in Supplementary Figure S14.
3.3.3 Neurotransmitters
3.3.3.1 5-HT
Twenty studies (43, 44, 46, 51, 55, 59, 65, 66, 71, 81, 84, 88, 92, 94, 96, 100, 102, 107, 111, 117) reported 5-HT as an outcome measure, involving 1,339 participants and 10 interventions. Thus, 45 two-by-two comparisons were performed, with an overall network of evidence centered on CM (Supplementary Figure S8). The results of the NMA demonstrated that with the exception of CM, most of the external therapies showed a better effect on 5-HT levels than SI (p < 0.05). Compared to CM, ACE, rTMS, Tuina, MA, and MB significantly reduced 5-HT levels (p < 0.05). No significant differences were found among the different external treatments (p > 0.05), as shown in Supplementary Figure S15.
3.3.3.2 DA
Nine studies (44, 46, 51, 55, 59, 72, 94, 98, 117) reported DA as an outcome measure, involving 572 participants and eight interventions. Thus, 28 two-by-two comparisons were made, with an overall network of evidence centered on the CM and SI (see Supplementary Figure S9). The results of the NMA showed that rTMS, Tuina, EA, MA, and FB significantly improved DA levels compared with SI and CM. Compared with FB and AS, rTMS, Tuina, EA, and MA were more effective in increasing DA concentrations. rTMS, Tuina and EA were superior in performance to MA. All the abovementioned differences were statistically significant (p < 0.05; Supplementary Figure S15).
3.3.3.3 NE
Ten studies (44, 51, 55, 56, 65, 71, 88, 98, 102, 111) reported NE outcome measures involving 679 participants and eight interventions; thus, 28 two-by-two comparisons were performed and the evidence network was generally centered on CM (see Supplementary Figure S10). Compared with SI, rTMS [MD = −18.55, 95% CI (−28.71, −8.38)] and AS [MD = −17.23, 95% CI (−31.26, −3.20)] significantly reduced the NE levels. rTMS and MA were more effective than CM in reducing NE levels. All the abovementioned differences were statistically significant (p < 0.05; Supplementary Figure S16).
3.3.4 Adverse reactions
Of the 83 included articles, 46 reported adverse reactions. Among them, seven (43, 44, 64, 71, 72, 79, 104) reported no adverse events and 39 studies (38–42, 45–47, 49, 54, 56, 58, 59, 61, 68, 73–77, 80, 83–85, 89, 92, 97, 99–101, 103, 105, 107–109, 113–115) reported minor adverse reactions or no serious adverse reactions. Owing to the limited number of included studies and the broad range of definitions, adverse reactions could not be specifically subdivided, and only the total number of adverse reactions triggered directly by the interventions was analyzed. Specific adverse reactions are detailed in Supplementary Table S13. Forty-six studies involving 3,400 participants and 11 interventions reported adverse reactions. Thus, 55 two-by-two comparisons were formed, and the evidence network was generally centered on the MA, thereby forming 14 closed loops (see Supplementary Figure S11). The results of the NMA showed that Tuina, rTMS, MB, EA, and MA significantly improved adverse reactions when compared with CM. SI was safer than rTMS, ACE, MA, or CM. All the abovementioned differences were statistically significant (p < 0.05), as shown in Figure 4.
3.4 SUCRA probability ranking
3.4.1 Sleep quality
3.4.1.1 Total effective rate
Tuina was the most effective intervention in improving the total efficacy rate (82.5%), followed by rTMS (78.1%), HBO (67.6%), ACE (66.4%), FB (64.3%), EA (47.7%), MA (45.1%), AS (33.3%), CM (11.7%), SI (10.3%) and SI (0.0%).
3.4.1.2 PSQI
Tuina was the most effective intervention (87.4%), followed by rTMS (83.2%), ACE (71.4%), HBO (64.3%), FB (62.5%), MB (59.3%), MA (47.5%), EA (40.7%), AS (20.9%), CM (12.8%), and SI (0.0%).
3.4.1.3 TST
rTMS was the most effective therapy for improving the TST (78.3%), followed by Tuina (71.3%), MB (67.8%), MA (58.3%), AS (54.6%), EA (45.0%), HBO (38.5%), CM (29.0%), and SI (7.1%).
3.4.1.4 SL
Tuina had the greatest effect on SL reduction (79.7%), followed by rTMS (69.0%), HBO (64.9%), MB (63.3%), MA (62.9%), AS (50.7%), CM (28.6%), EA (19.3%), and SI (11.6%).
3.4.1.5 AT
rTMS was the most effective intervention for reducing AT (75.4%), followed by Tuina (69.0%), MB (65.5%), HBO (61.7%), AS (53.4%), EA (51.1%), MA (42.5%), CM (23.0%), and SI (8.3%).
3.4.2 Psychological states
3.4.2.1 SAS scores
Regarding SAS score reduction, MB was the most effective therapy (90.8%), followed by HBO (78.8%), MA (73.3%), ACE (63.5%), rTMS (59.3%), AS (52.8%), CM (40.5%), EA (29.7%), FB (25.9%), Tuina (23.1%), and SI (12.3%).
3.4.2.2 SDS scores
HBO therapy had the best effect in terms of reducing SDS scores (93.7%), followed by MB (68.5%), MA (64.3%), ACE (63.2%), EA (58.1%), rTMS (46.2%), AS (45.6%), CM (31.9%), Tuina (16.8%), and SI (11.8%).
3.4.3 Neurotransmitters
3.4.3.1 5-HT
ACE had superior efficacy in increasing 5-HT levels (82.0%), followed by rTMS (75.9%), Tuina (70.5%), EA (61.8%), MA (57.9%), FB (51.3%), MB (50.2%), AS (35.1%), CM (14.4%), and SI (1.0%).
3.4.3.2 DA
Tuina was the most effective intervention in improving DA levels (90.3%), followed by rTMS (86.9%), EA (79.9%), MA (57.2%), FB (39.7%), AS (24.2%), CM (17.8%), and SI (4.0%).
3.4.3.3 NE
In terms of NE reduction, EA had the best effect (69.9%), followed by rTMS (67.4%), AS (61.9%), MA (57.8%), Tuina (55.8%), MB (55.5%), CM (20.2%), and SI (11.5%).
3.4.4 Adverse reactions
SI was the safest intervention (88.7%), followed by Tuina (68.7%), FB (65.9%), EA (64.2%), MA (54.4%), MB (48.2%), rTMS (46.2%), AS (42.6%), HBO (41.1%), ACE (25.7%), and CM (4.2%). The SUCRA values and ranking results for each outcome indicator are shown in Table 1. Higher SUCRA values indicate more effective and safer interventions.
3.5 Publication bias
Stata 16.0 was used to test for small-sample effects for each outcome indicator except for DA. Stata was also used to produce funnel plots. The funnel plots for AT, NE, SAS scores, and adverse events showed good symmetry, suggesting that the quality of the included studies was high and the possibility of publication bias was low. In terms of the total effective rate, there was a pronounced outlier on the left side. The exclusion of this outlier had no significant effect on the study results. Therefore, the probability of publication bias was considered low. The funnel plots for the remaining outcome indicators had poor symmetry, suggesting that there may have been some publication bias (Supplementary Figures S17–26).
3.6 Sensitivity analysis
To test the reliability and stability of this network meta-analysis, two sensitivity analyses were performed using Stata 16.0. First, four papers (39, 63, 67, 87) that were evaluated as high-risk in terms of literature quality were excluded, and sensitivity analyses were performed before and after exclusion. Second, considering that RCTs with small sample sizes may have affected the accuracy of the results, 14 studies (40, 54, 58, 61, 67, 72, 78, 80, 88, 92, 97, 107, 111, 117) with a sample size of less than 60 were excluded from the sensitivity analysis. Sensitivity analyses were only performed for some indicators (total effective rate, PSQI, SAS scores, and adverse reactions). The results show that there is little difference between the results before and after the exclusion of the two sensitivity analyses, indicating that the quality of the literature is good and that this network meta-analysis is reliable and stable.
4 Discussion
To the best of our knowledge, neither a systematic review nor a network meta-analysis of the efficacy and safety of external therapies in the treatment of insomnia has been reported. This is the first study to use a network meta-analysis to evaluate the effects of external therapies on sleep quality, psychological status, and neurotransmitters in patients with insomnia. In this network meta-analysis, we pooled evidence from 83 studies with 6,100 patients in total.
The total effective rate, PSQI as a subjective scale, and PSG indices (TST, SL, and AT) as objective indicators were used to assess the effectiveness of the external treatments in improving sleep quality. An in-depth analysis of the indicators revealed that the external therapies included in this study were superior to SI in terms of improving sleep quality, with Tuina therapy and rTMS consistently ranking highly. Tuina was the best intervention for improving the total effective rate, PSQI, and SL. The reason for the better effect of Tuina may be due to the activation of the corticotropin-releasing hormone (CRH)/CRH receptor type 1 (CRH/CRHR1) pathway and modulation of monoamine neurotransmitters (121, 122). rTMS was effective in increasing TST and reducing AT. Studies have shown that rTMS can reduce cortical excitability and increase melatonin secretion in the pineal gland, thereby restoring brain activity to a normal state (123). Although both Tuina and rTMS have good efficacy, after considering their safety, we found that rTMS was less safe, while Tuina was second only to SI in terms of safety. Therefore, the use of Tuina is a good choice when symptoms of sleep disorders are observed in patients.
Insomnia is also associated with many emotional and psychological changes, and prolonged poor-quality sleep not only affects quality of life, but also has many negative psychological effects on patients (124). Some studies have shown that the relationship between insomnia and depression and anxiety is bidirectional and that improvements in poor psychological states can also affect the effectiveness of insomnia treatment (125, 126). After analysis of relevant indicators, it was found that Tuina and rTMS, which were more effective in improving sleep disorder symptoms, were less effective in improving patients’ anxiety and depressive states. MB and HBO were the most effective in reducing SAS and SDS scores, second only to Tuina and rTMS in improving insomnia symptoms, and were found to be the most effective interventions for improving anxiety. Studies have shown that MB can promote blood circulation through warm stimulation, increase melatonin synthesis, improve mood, and promote sleep by regulating monoamine neurotransmitters, inhibitory neurotransmitters, and cytokines (127). HBO was effective in reducing depressive symptoms, which may be related to its ability to increase blood oxygen levels, improve blood supply to the brain, and restore neurological function (128, 129).
Monoamine neurotransmitters are important factors in the maintenance of the sleep–wake balance. The representative monoamine neurotransmitters 5-HT, DA, and NE are involved in the regulation of sleep activities and are closely related to the occurrence and development of insomnia (130, 131). We analyzed three outcome indicators, 5-HT, DA, and NE levels, and the results showed that Tuina and rTMS, which ranked high in the effectiveness index, also improved 5-HT, DA, and NE concentrations more effectively, with some positive correlations, which may underly their mechanisms of action. However, there is also a certain negative correlation; for example, EA is the most effective at reducing NE, but all of them are poorly ranked in terms of sleep quality and thus still need to be validated in a large number of clinical trials.
When we assessed the literature quality, we found that most studies used low-risk random assignment methods. The literature included in previous studies rarely mentioned blinding and allocation concealment or described them inaccurately. In this study, nearly half of the studies explicitly proposed the blind method and allocation concealment and described the specific implementation methods. The funnel plot showed some heterogeneity in some outcome indicators. Therefore, in order to identify the source of heterogeneity and improve the persuasiveness of the evidence, we conducted two sensitivity analyses of the total efficacy rate (as indicated by PSQI scores, SAS scores, and adverse reactions). After high-risk literature and small-sample studies were excluded, the overall results were still robust, indicating that the quality of the literature included in this study was acceptable.
However, this study had some limitations. First, owing to the relatively strict inclusion and exclusion criteria, RCTs with vagus nerve stimulation, transcranial direct current stimulation, and transcranial alternating current stimulation were not included; therefore, no statistical analysis of these therapies was conducted. Second, we only performed sensitivity analyses and not subgroup analyses because of limited evidence. Third, network diagrams may oversimplify complex relationships or overlook certain nuances in the NMA. Furthermore, Some objective indicators, such as slow wave sleep, REM sleep percentage, spindle and slow wave power and number, were not included in the analysis because external therapy reported less, which could not satisfy the statistical analysis. Finally, most included studies lacked follow-up data.
5 Conclusion
Altogether, most types of external treatments showed improvements in both subjective and objective sleep indices. External treatments are also highly effective in improving the psychological state and monoamine neurotransmitter levels in patients with insomnia. Tuina improves sleep disorder symptoms, and HBO and MB can be prioritized for insomnia treatment when patients have depression or anxiety as their main symptoms. The mechanism of action of external therapy for insomnia may be positively correlated with the regulation of monoamine neurotransmitters. However, this is not a one-to-one correlation. Limited by the quality of the included studies, the obtained conclusions must be verified.
Data availability statement
The original contributions presented in this study are included in the article/Supplementary material. Further inquiries can be directed at the corresponding author.
Author contributions
ZhenW: Methodology, Writing – original draft, Writing – review & editing. HX: Data curation, Software, Visualization, Writing – review & editing. ZhengW: Funding acquisition, Methodology, Software, Supervision, Writing – review & editing. HZ: Formal analysis, Investigation, Resources, Writing – review & editing. LZ: Conceptualization, Methodology, Supervision, Writing – review & editing. YW: Data curation, Formal analysis, Investigation, Writing – review & editing. ML: Conceptualization, Data curation, Validation, Writing – review & editing. YZ: Conceptualization, Funding acquisition, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the National Natural Science Foundation of China (No. 8187151703), the Central Plains Thousand Talents Program-Central Plains Famous Doctors (No. ZYQR201912120), the Henan Science and Technology R&D Program Joint Fund (Cultivation of Superior Disciplines) Cultivation Project the (No. 222301420061), Henan Province Science and Technology Tackling Program Project (No. 232102311203), the 2022 Central Plains Talent Plan (Talent Education Series)-Central Plains Youth Top Talent Project (No. Yu Talent Office [2022] No. 5), Henan University of Chinese Medicine graduate research innovation ability improvement plan project (2023KYCX071), and Henan Province “Double First-class” establishment Discipline of Chinese Medical Science Research Project (HSRP-DFCTCM-2023-8-11).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2024.1297767/full#supplementary-material
Abbreviations
NMA, Network meta-analysis; RCTs, Randomized controlled trial; PSQI, Pittsburgh sleep quality index; PSG, Polysomnography; TST, Total sleep time; SOL, Sleep onset latency; AT, Awakening time; SAS, Self-rating anxiety scale; SDS, Self-rating depression scale; 5-HT, 5-hydroxytryptamine; ACE, Acupoint catgut embedding; rTMS, Repetitive transcranial magnetic stimulation; HBO, Hyperbaric oxygen; EA, Electroacupuncture; MB, Moxibustion; FB, Foot bath; MA, Manual acupuncture; AS, Auricular stimulation.
References
1. Bragg, S, Benich, JJ, Christian, N, Visserman, J, and Freedy, J. Updates in insomnia diagnosis and treatment. Int J Psychiatry Med. (2019) 54:275–89. doi: 10.1177/0091217419860716
2. Riemann, D, Baglioni, C, Bassetti, C, Bjorvatn, B, Dolenc Groselj, L, Ellis, JG, et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. (2017) 26:675–700. doi: 10.1111/jsr.12594
3. Dopheide, JA. Insomnia overview: epidemiology, pathophysiology, diagnosis and monitoring, and nonpharmacologic therapy. Am J Manag Care. (2020) 26:S76–84. doi: 10.37765/ajmc.2020.42769
4. Cunnington, D, Junge, MF, and Fernando, AT. Insomnia: prevalence, consequences and effective treatment. Med J Aust. (2013) 199:S36–40. doi: 10.5694/mja13.10718
5. Zhou, F, Li, S, and Xu, H. Insomnia, sleep duration, and risk of anxiety: a two-sample Mendelian randomization study. J Psychiatr Res. (2022) 155:219–25. doi: 10.1016/j.jpsychires.2022.08.012
6. Glidewell, RN, McPherson Botts, E, and Orr, WC. Insomnia and anxiety: diagnostic and management implications of complex interactions. Sleep Med Clin. (2015) 10:93–9. doi: 10.1016/j.jsmc.2014.11.008
7. Gebara, MA, Siripong, N, DiNapoli, EA, Maree, RD, Germain, A, Reynolds, CF, et al. Effect of insomnia treatments on depression: a systematic review and meta-analysis. Depress Anxiety. (2018) 35:717–31. doi: 10.1002/da.22776
8. Porwal, A, Yadav, YC, Pathak, K, and Yadav, R. An update on assessment, therapeutic management, and patents on insomnia. Biomed Res Int. (2021) 2021:6068952–19. doi: 10.1155/2021/6068952
9. Li, ZW, Zhu, YH, Song, XJ, et al. Research progress on the neurotransmitter mechanism of acupuncture in improving insomnia by regulating sleep structure. Acupuncture Res. (2023) 48:618–24. doi: 10.13702/j.1000-0607.20220531
10. Wang, T, Su, S, Zhang, X, et al. Effects of “heart and gall bladder” mai-grain moxibustion on hippocampal monoamine neurotransmitter levels in depressed co-morbid insomnia rats. World Sci. Technol. Moderniz. Chinese Med. (2023) 25:235–42.
11. Taylor, DJ, and Roane, BM. Treatment of insomnia in adults and children: a practice-friendly review of research. J Clin Psychol. (2010) 66:1137–47. doi: 10.1002/jclp.20733
12. Mayer, G, Jennum, P, Riemann, D, and Dauvilliers, Y. Insomnia in central neurologic diseases-occurrence and management. Sleep Med Rev. (2011) 15:369–78. doi: 10.1016/j.smrv.2011.01.005
13. Feng, TY, and Xu, XW. Progress of drug therapy for insomnia. World J Sleep Med. (2019) 10:691–6.
14. Lei, HL, and Deng, YH. The research progress of external treatment to treat insomnia. J Yunnan J Trad Chin Med. (2024) 5:85–9.
15. Zheng, XY, Geng, S, Hong, J, et al. Clinical research progress of convenient external treatment for insomnia. Chin Folk Ther. (2020) 28:98–100. doi: 10.19621/j.cnki.11-3555/r.2020.0250
16. Gu, P. Interpretation of domestic and foreign guidelines for diagnosis and treatment of insomnia: external therapy and insomnia. J Sleep Med. (2015) 9:83–8.
17. Sleep disorders group, Chinese Society of Neurology. Guidelines for diagnosis and external treatment of insomnia in Chinese adults. Chin J Evid Based Med. (2015) 24:1–14.
18. Zhang, TY, Yang, YY, and Cui, SK. Advances in Chinese and Western medicine research on insomnia. Mod Dist Educ Chinese Trad Med. (2023) 21:196–9.
19. Gou, YP, Zhang, XW, and Sun, SW. A review of advances in Chinese and Western medical treatment of insomnia. Chinese convalescent medicine. (2022) 31:483–491. doi: 10.13517/j.cnki.ccm.2022.05.007
20. Wang, Z, Xu, H, Zhou, H, Lei, Y, Yang, L, Guo, J, et al. A systematic review with meta-analysis: traditional Chinese tuina therapy for insomnia. Front Neurosci. (2023) 16:1096003. doi: 10.3389/fnins.2022.1096003
21. Sun, N, He, Y, Wang, Z, Zou, W, and Liu, X. The effect of repetitive transcranial magnetic stimulation for insomnia: a systematic review and meta-analysis. Sleep Med. (2021) 77:226–37. doi: 10.1016/j.sleep.2020.05.020
22. Li, W, Li, Z, Zhang, H, Wang, Y, Chen, H, and Xiong, L. Acupoint catgut embedding for insomnia: a Meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med. (2020) 2020:5450824–14. doi: 10.1155/2020/5450824
23. Li, T, Puhan, MA, Vedula, SS, Singh, S, and Dickersin, K The Ad Hoc Network Meta-analysis Methods Meeting Working Group. Ad hoc network Meta-analysis methods meeting working group. Network meta-analysis-highly attractive but more methodological research is needed. BMC Med. (2011) 9:79. doi: 10.1186/1741-7015-9-79
24. Shim, S, Yoon, BH, Shin, IS, and Bae, JM. Network meta-analysis: application and practice using Stata. Epidemiol Health. (2017) 39:e2017047. doi: 10.4178/epih.e2017047
25. Seitidis, G, Nikolakopoulos, S, Hennessy, EA, Tanner-Smith, EE, and Mavridis, D. Network Meta-analysis techniques for synthesizing prevention science evidence. Prev Sci. (2022) 23:415–24. doi: 10.1007/s11121-021-01289-6
26. Chinese Society of Neurology, Chinese Society of Neurology, Sleep Disorders Group. Guidelines for the diagnosis and treatment of insomnia in adults in China. Chin J Neurol. (2018) 51:324–35.
27. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th Edn. Washington, DC: American Psychiatric Press, (1999). 240–241.
28. State Administration of Traditional Chinese Medicine. The diagnosis and curative effect standard of traditional Chinese medicine disease and syndrome. Beijing: China Medical Science and Technology Press. (2012). 135–138.
29. Zheng, Y. Guiding principles for clinical research of new traditional Chinese medicines (trial). Beijing: China Medical Science and Technology Press. (2002). 168–172.
30. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
31. Higgins, JP, Altman, DG, Gotzsche, PC, Juni, P, Moher, D, Oxman, AD, et al. Cochrane Bias methods group; Cochrane statistical methods group. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928
32. Watt, J, Tricco, AC, Straus, S, Veroniki, AA, Naglie, G, and Drucker, AM. Research techniques made simple: network Meta-analysis. J Invest Dermatol. (2019) 139:4–12.e1. doi: 10.1016/j.jid.2018.10.028
33. Bowden, J, Tierney, JF, Copas, AJ, and Burdett, S. Quantifying, displaying and accounting for heterogeneity in the meta-analysis of RCTs using standard and generalised Q statistics. BMC Med Res Methodol. (2011) 11:41. doi: 10.1186/1471-2288-11-41
34. Wang, Z, Zhou, Z, Zhang, L, Li, X, Li, M, Pan, Y, et al. Efficacy and safety of nonpharmacological strategies for the treatment of oligoasthenospermia: a systematic review and Bayesian network meta-analysis. Eur J Med Res. (2023) 28:6. doi: 10.1186/s40001-022-00968-6
35. Uhlmann, L, Jensen, K, and Kieser, M. Hypothesis testing in Bayesian network meta-analysis. BMC Med Res Methodol. (2018) 18:128. doi: 10.1186/s12874-018-0574-y
36. Higgins, JP, Thompson, SG, Deeks, JJ, and Altman, DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
37. Watt, J, and Del Giovane, C. Network Meta-analysis. Methods Mol Biol. (2022) 2345:187–201. doi: 10.1007/978-1-0716-1566-9_12
38. Cao, XL, Ma, Y, and Wang, Y. Clinical efficacy of injected acupuncture point buried thread in the treatment of insomnia[J]. Sichuan Trad Chin Med. (2014) 32:161–5.
39. Guo, AS, Li, AH, Feng, LF, et al. Clinical study on the treatment of primary insomnia with buried acupuncture points. J Nanjing Univ Trad Chin Med. (2013) 29:331–4. doi: 10.14148/j.issn.1672-0482.2013.04.012
40. Li, PZ. Clinical efficacy of acupuncture point burial combined with hyperbaric oxygen in the treatment of insomnia after stroke. Guangzhou Univ Chin Med. (2021). doi: 10.27044/d.cnki.ggzzu.2021.000359
41. Xu, F, Xuan, LH, Zheng, ZG, et al. Clinical study on the treatment of insomnia of the stomach-medium disharmony type by the acupuncture point buried thread method. Zhejiang J Trad Chin Med. (2013) 48:791–3.
42. Li, XR, Hou, X, Ye, YJ, Bu, XM, An, CL, and Yan, XK. Comparison of the efficacy of the buried thread method and acupuncture based on the formula of “dredging the liver and regulating the spirit” in the treatment of insomnia with liver stagnation and qi stagnation. Chinese acupuncture. (2020) 40:1277–1280+1285. doi: 10.13703/j.0255-2930.20200614-k0002
43. Chen, AY. Clinical efficacy of abdominal needle burial therapy based on the theory of “brain and intestine communion” on insomnia of heart and spleen deficiency. Fujian Univ Chin Med. (2020). doi: 10.27021/d.cnki.gfjzc.2020.000034
44. Yu, WW, Li, ZG, Sun, HR, et al. Clinical study of repetitive transcranial magnetic stimulation for the treatment of depression and sleep disorders in patients with early Parkinson’s disease. J Clin Neurol. (2017) 30:341–5.
45. Feng, XJ, Gai, N, and Wang, XY. Efficacy observation of repetitive transcranial magnetic stimulation for primary insomnia. J Clin Psychiatry. (2017) 27:415–7.
46. Yu, XL, and Chen, HL. Clinical effect and prognosis analysis of repetitive transcranial magnetic stimulation for insomnia patients with Parkinson’s disease. Chinese and foreign medical treatment. (2022) 41:20–24. doi: 10.16662/j.cnki.1674-0742.2022.04.020
47. Qi, WY, Qi, GQ, Liang, Y, et al. Effect of repetitive transcranial magnetic stimulation on insomnia after stroke and the effect on patients’ anxiety and depression status. China Mod Phys. (2022) 60:100–3.
48. Buydina, A, Nurbiya, B, Wang, QY, et al. Clinical efficacy of repetitive transcranial magnetic stimulation for non-organic insomnia in 30 cases. World J Sleep Med. (2016) 3:275–9.
49. Ding, L, Tang, X, Chen, X, et al. Effects of repetitive transcranial magnetic stimulation on plasma Glu and GABA levels in patients with Parkinson’s sleep disorder. Chinese and foreign. Med Care. (2018) 37:7–22. doi: 10.16662/j.cnki.1674-0742.2018.26.007
50. Kou, XL, Chen, L, Dai, FY, et al. Clinical correlation study of acupuncture combined with repetitive transcranial magnetic stimulation technique on the prognosis of patients with insomnia. Mod Pract Med. (2019) 31:1321–2.
51. Wang, JX, and Li, YH. Diagnostic value of neurotransmitter levels in the brain on sleep disorders and evaluation of the effect of repeated transcranial magnetic stimulation intervention. J Clin Psychos Disord. (2020) 26:64–67+117.
52. Sheng, W, Yang, X, Lv, L, et al. Clinical study of polysomnography observation of transcranial magnetic stimulation combined with music electroacupuncture for the treatment of sleep disorders after stroke. Clin J Acupunct Moxibust. (2019) 35:7–12.
53. Xu, L, Jiang, L, and He, F. Clinical study of 30 cases of chronic insomnia treated with electroacupuncture combined with low-frequency repetitive transcranial magnetic stimulation. Jiangsu Trad Chin Med. (2021) 53:60–2. doi: 10.19844/j.cnki.1672-397X.2021.03.022
54. Meng, F, Gao, SH, Bu, CHL, et al. Clinical control study of low-frequency repetitive transcranial magnetic stimulation for insomnia. J Qiqihar Med College. (2017) 38:895–7.
55. Tang, L. Effect of ultra-low frequency transcranial magnetic stimulation on EEG ultralow waves in patients with insomnia and its efficacy. Med Clin Research. (2014) 6:1201–3. doi: 10.3969/j.issn.1671-7171.2014.06.060
56. Ren, YX, Tang, SJ, and He, JJ. A single-center prospective randomized controlled study of eszopiclone combined with transcranial magnetic stimulation for the treatment of chronic insomnia in the elderly. Drug Eval Res. (2022) 45:938–45.
57. Jiang, CG, Zhang, T, Yue, FG, Yi, ML, and Gao, D. Efficacy of repetitive transcranial magnetic stimulation in the treatment of patients with chronic primary insomnia. Cell Biochem Biophys. (2013) 67:169–73. doi: 10.1007/s12013-013-9529-4
58. Huang, Z, Li, Y, Bianchi, MT, Zhan, S, Jiang, F, Li, N, et al. Repetitive transcranial magnetic stimulation of the right parietal cortex for comorbid generalized anxiety disorder and insomnia: a randomized, double-blind, sham-controlled pilot study. Brain Stimul. (2018) 11:1103–9. doi: 10.1016/j.brs.2018.05.016
59. Wang, J, Liu, XF, and Xue, WG. Clinical efficacy and safety observation of Tui Na therapy for insomnia in Chinese medicine. Guizhou Med. (2021) 45:432–3.
60. Yu, LW, Lin, L, Lu, XG, et al. Clinical efficacy of one-finger zen Tui na in the treatment of senile insomnia. Geriatric Med Health Care. (2017) 23:404–7.
61. Wei, M. Clinical observation on the treatment of chronic insomnia with taiji tuina and the effect on serum CRP and IL-6. Hubei Univ. Chin Med. (2020). doi: 10.27134/d.cnki.ghbzc.2020.000281
62. Tang, HL, Chen, Z, Pang, J, et al. Pivotal meridian Tui na for insomnia: a randomized controlled study. Chin Acupunct. (2015) 35:816–8. doi: 10.13703/j.0255-2930.2015.08.017
63. Pan, LK. 30 cases of primary insomnia treated with modified yang-into-yin tuina. J Trad Chin Med Ext Treat. (2018) 27:10–1.
64. Zhou, XB. A controlled study of massage techniques and milli-needle acupuncture for cervical insomnia. Beijing Trad Chin Med. (2010) 29:495–7. doi: 10.16025/j.1674-1307.2010.07.027
65. Tan, T, Wang, JG, and Zhao, HY. Effects of the “Jingu Tui Na” technique on blood pentraxin and norepinephrine in patients with psychophysiological insomnia of the heart and spleen deficiency type. Tianjin Chin Med. (2014) 31:529–33.
66. Zheng, HH, Bei, N, Tang, Q, et al. Effects of pramipexole hydrochloride with hyperbaric chamber therapy on γ-GABA and Glu in patients with Parkinson’s sleep disorder. J Hunan Normal Univ. (2022) 19:116–20.
67. Pan, Y, Luo, M, and Wang, XY. Efficacy of pramipexole combined with hyperbaric chamber in the treatment of Parkinson’s disease combined with sleep disorders. Chin J Geriatric Cardiovas Cerebrovas Dis. (2016) 18:125–8.
68. Liao, HY, Chen, WX, Chen, SR, et al. Efficacy of hyperbaric oxygen in the treatment of perimenopausal insomnia. Hebei Med. (2010) 16:1348–51.
69. Kuang, AH, Huang, H, Jia, SB, et al. Efficacy of hyperbaric oxygen in the treatment of insomnia. J Ningxia Med Univ. (2009) 31:83–4.
70. Zhu, Y. Study on the effects of hyperbaric oxygen adjuvant therapy on the psychological status, sleep quality and quality of life of patients with gastric cancer with insomnia. World J Sleep Med. (2020) 7:1868–9.
71. Sun, YZ, Liu, Y, and Yu, TY. Effect of toning electroacupuncture combined with transcranial repetitive needle stimulation in the treatment of patients with post-stroke sleep disorders of the heart and spleen type and the effects on HRV, 5-HT and NE. Shi-Zhen Guomao Guomao. (2021) 32:2699–702.
72. Wang, XQ, Qin, S, Wu, WZ, Liu, CY, Shang, HT, Wan, QY, et al. Electroacupuncture in the treatment of insomnia in the elderly and its effect on serum melatonin and dopamine. Chin Acupuncture. (2021) 41:501–4. doi: 10.13703/j.0255-2930.20200404-k0001
73. Yeung, WF, Chung, KF, Tso, KC, Zhang, SP, Zhang, ZJ, and Ho, LM. Electroacupuncture for residual insomnia associated with major depressive disorder: a randomized controlled trial. Sleep. (2011) 34:807–15. doi: 10.5665/SLEEP.1056
74. Yeung, WF, Chung, KF, Zhang, SP, Yap, TG, and Law, ACK. Electroacupuncture for primary insomnia: a randomized controlled trial. Sleep. (2009) 32:1039–47. doi: 10.1093/sleep/32.8.1039
75. Li, S, Wang, Z, Wu, H, Yue, H, Yin, P, Zhang, W, et al. Electroacupuncture versus sham acupuncture for Perimenopausal insomnia: a randomized controlled clinical trial. Nat Sci Sleep. (2020) 12:1201–13. doi: 10.2147/NSS.S282315
76. Lee, B, Kim, BK, Kim, HJ, Jung, IC, Kim, AR, Park, HJ, et al. Efficacy and safety of Electroacupuncture for insomnia disorder: a multicenter, randomized, Assessor-blinded. Controlled Trial Nat Sci Sleep. (2020) 12:1145–59. doi: 10.2147/NSS.S281231
77. Yin, X, Li, W, Wu, H, Dong, B, Ma, J, Li, S, et al. Efficacy of Electroacupuncture on treating depression-related insomnia: a randomized controlled trial. Nat Sci Sleep. (2020) 12:497–508. doi: 10.2147/NSS.S253320
78. Wu, WZ, Zheng, SY, Liu, CY, et al. Effects of “Tongdu Tiaoshen” acupuncture on the treatment of chronic insomnia and on serum GABA and CORT levels. (2021) 41:721–4.
79. Liu, H, Hu, XW, and Deng, CY. Clinical observation of long snake moxibustion in treating menopausal insomnia of liver-depression and qi stagnation type. Chin Trad Med Mod Distance Educ. (2022) 20:113–5.
80. Lu, XX, Wu, SM, Zhang, C, et al. Clinical observation on the treatment of insomnia in the elderly by warming the Yang and dispelling the cold with tian moxibustion. Inner Mongolia Trad Chin Med. (2020) 39:109–11. doi: 10.16040/j.cnki.cn15-1101.2020.04.066
81. Li, Q, Liu, LL, and Yang, HX. Exploring the effect of thermal moxibustion treatment on the improvement of sleep quality in patients with primary insomnia of the heart and spleen deficiency type. Sichuan Trad Chin Med. (2020) 38:181–4.
82. Li, LC, Liang, Y, Hu, YH, et al. Effect of thermal moxibustion on anxiety and depression in patients with liver-depression and qi-stagnation type insomnia. World. J Acupunct Moxibust. (2018) 28:15–75. doi: 10.1016/j.wjam.2018.03.012
83. Wu, S, Liu, ZZ, and Li, SY. Clinical effects of thunder fire moxibustion in treating liver-depression and yin-deficiency type of insomnia. China Med Herald. (2019) 16:149–53.
84. Wang, J, Tu, MX, Ma, FF, et al. Clinical study on the treatment of insomnia after cerebral infarction with Lei Huo moxibustion at Shen que point. New Chin Med. (2021) 53:193–6. doi: 10.13457/j.cnki.jncm.2021.19.044
85. Li, J. Study on the application of moxibustion with moxibustion and umbilical cord combined with meridian point massage in heart and spleen deficiency type insomnia. Huzhou Norm Univ. (2020). doi: 10.27946/d.cnki.ghzsf.2020.000043
86. Li, LC, Xing, HJ, Liang, Y, et al. Efficacy of thermal moxibustion of original points of liver and gallbladder meridian in the treatment of liver-depression and qi-stagnation type insomnia. Acupuncture Res. (2018) 43:573–5. doi: 10.13702/j.1000-0607.170765
87. Li, D, Xuan, X, and Liu, YH. Clinical observation on the treatment of insomnia of the heart and spleen deficiency type by interspersed ginger-garlic pavement moxibustion on the merging heart points of the directing vessel. Shaanxi Trad Chin Med. (2021) 42:159–60.
88. Chen, E, Wang, XD, Zhang, WD, et al. Clinical observation of 28 cases of stroke-related insomnia treated with moxibustion. J Gansu Univ Chin Med. (2021) 38:56–61. doi: 10.16841/j.issn1003-8450.2021.02.11
89. Chen, Q, Chen, XJ, Zhou, ZY, et al. Effect of moxibustion of dorsal points on insomnia in patients with deficiency of heart and spleen. J Zhejiang Univ Trad Chin Med. (2013) 37:1023–5. doi: 10.16466/j.issn1005-5509.2013.08.017
90. Li, SH. Efficacy observation of foot bath in the treatment of cervical insomnia of liver-depression and fire type and experience of evidence-based care. Chinese and foreign medical research. (2015) 13:153–5. doi: 10.14033/j.cnki.cfmr.2015.14.079
91. Cao, DF, Lai, WR, and Li, SM. Effect of Chinese herbal footbath therapy on the clinical efficacy of insomnia patients. Gen Pract Nurs. (2018) 16:2903–4.
92. Wang, XB, Huang, HG, and Yang, YJ. Analysis of the efficacy of Chinese herbal foot bath on elderly patients with insomnia. Clin Res Chin Med. (2021) 13:95–7.
93. Zhang, H. Effect of Chinese herbal foot bath on sleep quality in patients with irritable bowel syndrome with insomnia. World J Sleep Med. (2019) 6:1068–9.
94. An, XM, and Gao, H. Exploring the effect of auricular acupressure combined with foot bath on 5-HT and DA levels and care in patients with liver fire disturbing insomnia. China Med Guide. (2016) 14:4+6. doi: 10.15912/j.cnki.gocm.2016.04.004
95. Li, M. Clinical observation of point therapy and Chinese herbal foot bath care to improve insomnia. Psychologist. (2018) 24:221.
96. Xie, C, and Xie, WN. Observation on the efficacy of acupuncture in the treatment of insomnia. Shanghai J Acupunct Moxibust. (2018) 37:503–6. doi: 10.13460/j.issn.1005-0957.2018.05.0503
97. Xi, HQ, Wu, WZ, Liu, CY, et al. The effect of acupuncture and tonifying formula on excessive wakefulness state in patients with chronic insomnia. Chin Acupunct. (2021) 41:263–7. doi: 10.13703/j.0255-2930.20200303-k0004
98. Pan, Y, Luo, Z, and Zhang, HL. Effects of acupuncture on serum amino acid neurotransmitters in insomnia patients with Sishencong and Baihui. World J Acupunct Moxibust. (2017) 27:23–7. doi: 10.1016/S1003-5257(17)30095-8
99. Zhang, LX, Hui, RT, Tang, Y, et al. Effect of acupuncture intervention on insomnia with depression. Chin J Trad Chin Med. (2020) 35:4271–4.
100. Liang, FJ, Hu, HX, Zhang, JB, et al. Effects of acupuncture on serum brain and intestinal peptides and sleep quality in patients with primary insomnia. J Integ Cardiovas Cerebrovas Dis Chinese West Med. (2020) 18:2042–5.
101. Liu, JX. Clinical study on the effect of acupuncture on the regulation of arousal state in post-stroke insomnia patients. J Chin Med. (2017) 32:2544–8. doi: 10.16368/j.issn.1674-8999.2017.12.661
102. Guo, Q. The effect of regulating Ren and Tongdu acupuncture treatment on sleep quality and neuroendocrine levels in perimenopausal insomnia patients. Chin Med Innov. (2021) 18:82–6.
103. Yu, L, Zhang, R, Tan, DH, et al. Clinical efficacy of sparing and balancing acupuncture in the treatment of chronic insomnia with anxiety and depression. Chin Med Inform. (2022) 39:55–9. doi: 10.19656/j.cnki.1002-2406.20220809
104. Wang, C, Xu, WL, Li, GW, Fu, C, Li, JJ, Wang, J, et al. Impact of acupuncture on sleep and comorbid symptoms for chronic insomnia: a randomized clinical trial. Nat Sci Sleep. (2021) 13:1807–22. doi: 10.2147/NSS.S326762
105. Yeung, WF, Yu, BY, Yuen, JW, et al. Semi-individualized acupuncture for insomnia disorder and oxidative stress: a randomized, double-blind. Sham-Control Trial Nat Sci Sleep. (2021) 13:1195–207. doi: 10.2147/NSS.S318874
106. Fu, C, Zhao, N, Liu, Z, Yuan, LH, Xie, C, Yang, WJ, et al. Acupuncture improves Peri-menopausal insomnia: a randomized controlled trial. Sleep. (2017) 40:153–158. doi: 10.1093/sleep/zsx153
107. Liu, C, Zhao, Y, Qin, S, Wang, X, Jiang, Y, and Wu, W. Randomized controlled trial of acupuncture for anxiety and depression in patients with chronic insomnia. Ann Transl Med. (2021) 9:1426. doi: 10.21037/atm-21-3845
108. Zhang, L, Tang, Y, Hui, R, Zheng, H, Deng, Y, Shi, Y, et al. The effects of active acupuncture and placebo acupuncture on insomnia patients: a randomized controlled trial. Psychol Health Med. (2020) 25:1201–15. doi: 10.1080/13548506.2020.1738015
109. Yin, X, Gou, M, Xu, J, Dong, B, Yin, P, Masquelin, F, et al. Efficacy and safety of acupuncture treatment on primary insomnia: a randomized controlled trial. Sleep Med. (2017) 37:193–200. doi: 10.1016/j.sleep.2017.02.012
110. Zhong, SQ, Zhang, GQ, Ding, MZ, et al. Effects of Ziwu Liujiao selective ear acupuncture points and sour jujube seeds on sleep quality in patients with heart and spleen deficiency type of hypochondriac with insomnia. World J Integ Chin West Med. (2022) 17:945–9. doi: 10.13935/j.cnki.sjzx.220520
111. Chen, XY. Effect of Chinese medicine auricular pressure bean care on the expression levels of NE, 5-HT and IL-1β in patients with type 2 diabetes mellitus with insomnia. Jilin Med. (2021) 42:1523–4.
112. Jiang, YB, Guan, L, and Bi, LL. Analysis of the efficacy of nimble and tranquilizing snap acupuncture combined with auricular acupuncture for the treatment of insomnia. Clin J Acupunct Moxibust. (2018) 34:6–10.
113. Chen, H, Zhang, MJ, Wu, JA, She, YF, Yuan, XR, Huo, YX, et al. Effect of auricular Acupoint bloodletting plus auricular acupressure on sleep quality and neuroendocrine level in college students with primary insomnia: a randomized controlled trial. Chin J Integr Med. (2022) 28:1096–104. doi: 10.1007/s11655-022-3581-0
114. Wu, Y, Yang, L, Zhong, Z, Wu, X, He, Z, Ma, H, et al. Auricular acupressure for hemodialysis patients with insomnia: a multicenter double-blind randomized sham-controlled trial. J Integr Complement Med. (2022) 28:339–48. doi: 10.1089/jicm.2021.0332
115. Xiang, Y. Clinical observation on the treatment of spleen and kidney deficiency type insomnia with the combination of solid capital and healthy brain liquid and ear acupressing beans. Hubei Univ National. (2022). doi: 10.27764/d.cnki.ghbmz.2022.000031
116. Zang, LL, and Hu, H. Efficacy of auricular acupressure in treating patients with insomnia. Chin Med Guide. (2014) 22:7–8.
117. Luo, MF. Clinical efficacy of auricular acupressure in the treatment of cervical insomnia of liver fire disturbing the heart type. Mod Diag Ther. (2015) 26:631–2.
118. Zhang, J, and Guan, L. Efficacy of auricular acupressure therapy in the treatment of sleep disorders in sea service personnel. J PLA Med College. (2022) 43:966–70.
119. GAO, J, YAO, M, DING, DG, XIANG, X, and XU, MT. Auricular intradermal acupuncture for insomnia:a randomized controlled trial. World J Acupunc Moxibust. (2020) 30:19–22. doi: 10.1016/j.wjam.2020.03.004
120. Guo, X, Zhang, XX, Zhang, Y, et al. Effects of ear acupressure combined with moxibustion on patients with sleep disorders after chemotherapy for lung cancer. Tianjin Nursing. (2019) 27:352–4.
121. Gao, JH, Cui, XF, Zhang, CF, et al. Effects of moist abdominal therapy on appetitin and related neurotransmitters in insomniac rats. Hebei TCM. (2022) 44:810–4.
122. Zhang, Y. Study on the metabolic mechanism of CRH/CRHR1 pathway mediated by vibration abdominal circular kneading for insomnia based on brain-gut interaction theory. Changchun Univ Trad Chin Med. (2022). doi: 10.26980/d.cnki.gcczc.2022.000024
123. Nardone, R, Sebastianelli, L, Versace, V, Brigo, F, Golaszewski, S, Pucks-Faes, E, et al. Effects of repetitive transcranial magnetic stimulation in subjects with sleep disorders. Sleep Med. (2020) 71:113–21. doi: 10.1016/j.sleep.2020.01.028
124. Fernandez-Mendoza, J, and Vgontzas, AN. Insomnia and its impact on physical and mental health. Curr Psychiatry Rep. (2013) 15:418. doi: 10.1007/s11920-013-0418-8
125. Baglioni, C, Spiegelhalder, K, Lombardo, C, and Riemann, D. Sleep and emotions: a focus on insomnia. Sleep Med Rev. (2010) 14:227–38. doi: 10.1016/j.smrv.2009.10.007
126. Chellappa, SL, and Aeschbach, D. Sleep and anxiety: from mechanisms to interventions. Sleep Med Rev. (2022) 61:101583. doi: 10.1016/j.smrv.2021.101583
127. Lin, RY, Wu, L, and Zhao, J. Efficacy of inducing qi and returning to yuan acupuncture combined with moxibustion at Yongquan point in the treatment of perimenopausal insomnia and the effects on patients’ serum interleukin-1β, 5-HT and FSH. Shaanxi TCM. (2020) 41:811–4.
128. Long, Y, Tan, J, Nie, Y, Lu, Y, Mei, X, and Tu, C. Hyperbaric oxygen therapy is safe and effective for the treatment of sleep disorders in children with cerebral palsy. Neurol Res. (2017) 39:239–47. doi: 10.1080/01616412.2016.1275454
129. Liu, Y, Huang, LP, Yuan, X, et al. The application of hyperbaric oxygen therapy in insomnia disorders. Int J Psychiatry. (2020) 47:894–909. doi: 10.13479/j.cnki.jip.2020.05.012
130. Atkin, T, Comai, S, and Gobbi, G. Drugs for insomnia beyond benzodiazepines: pharmacology, clinical applications, and discovery. Pharmacol Rev. (2018) 70:197–245. doi: 10.1124/pr.117.014381
Keywords: insomnia, external treatment, network meta-analysis, neurotransmitter, psychological state
Citation: Wang Z, Xu H, Wang Z, Zhou H, Zhang L, Wang Y, Li M and Zhou Y (2024) Efficacy and safety of multiple external therapies in patients with insomnia: a systematic review and network meta-analysis. Front. Neurol. 15:1297767. doi: 10.3389/fneur.2024.1297767
Edited by:
Jie Sun, Peking University, ChinaReviewed by:
Tianyuan Yu, Beijing University of Chinese Medicine, ChinaYulin Zou, China Three Gorges University, China
Yong-Bo Zheng, Peking University Sixth Hospital, China
Copyright © 2024 Wang, Xu, Wang, Zhou, Zhang, Wang, Li and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yunfeng Zhou, enlmNTY4MDE5OEAxMjYuY29t
†These authors have contributed equally to this work and share first authorship
 Zhen Wang
Zhen Wang Hui Xu
Hui Xu Zheng Wang
Zheng Wang Hang Zhou1
Hang Zhou1 Miaoxiu Li
Miaoxiu Li Yunfeng Zhou
Yunfeng Zhou