
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol. , 13 November 2023
Sec. Stroke
Volume 14 - 2023 | https://doi.org/10.3389/fneur.2023.1285947
Introduction: Gait impairment is a common symptom among individuals with cerebral small vessel disease (CSVD). However, performance differences between single-task walking (STW) and dual-task walking (DTW) among individuals with CSVD remain unclear. Therefore, we aimed to examine differences in gait characteristics during STW and DTW as well as the association between gait performance and neuroimaging markers.
Methods: We enrolled 126 older individuals with CSVD. The speed, cadence, stride length, stride time, and their dual-task cost (DTC) or variability were measured under the STW, motor-cognitive DTW (cognitive DTW), and motor-motor DTW (motor DTW) conditions. We examined neuroimaging features such as white matter hyperintensities (WMHs), lacunes, microbleeds, and total burden. Further, we analysed the association of neuroimaging markers with gait performance, including gait variability and DTC.
Results: Almost all spatiotemporal characteristics, as well as their DTCs or variabilities, showed significant among-group differences according to disease severity in the cognitive DTW condition; however, relatively lesser differences were observed in the STW and motor DTW conditions. The total CSVD burden score was moderately correlated with all the spatial parameters, as well as their DTCs or variabilities, in the cognitive DTW condition. Moreover, WMHs showed a correlation with speed, stride time, and cadence, as well as their DTCs, in the cognitive DTW condition. Furthermore, lacunes showed a moderate correlation with speed, stride length, and the DTC of speed, whilst microbleeds were only related to the DTC of stride length in the cognitive DTW condition. Neuroimaging biomarkers were not correlated with spatiotemporal parameters in STW and motor DTW conditions after Bonferroni correction. Moreover, the correlation coefficient between the total CSVD burden score and gait parameters was greater than those of other biomarkers.
Discussion: Parameters in the cognitive DTW condition are more appropriate than those in the motor DTW condition for the evaluation of gait abnormalities in patients with CSVD. Moreover, the total CSVD burden score might have better predictive utility than any single neuroimaging marker. Patients with CSVD, especially those with moderate-to-severe disease, should concentrate more on their gait patterns and reduce the load of secondary cognitive tasks whilst walking in daily life.
Dual-task walking (DTW) is defined as walking whilst performing a secondary task, including a cognitive task (motor-cognitive DTW) or motor task (motor-motor DTW) (1). In daily life, people perform various tasks, including speaking or picking up a coffee mug, whilst walking. Therefore, DTW offers an appropriate method for assessing gait characteristics in daily life (2). Healthy individuals can simultaneously complete several tasks; however, this can be difficult for patients with neurological disorders. Accordingly, patients with vascular or neurodegenerative diseases are more likely to present deteriorated walking patterns during DTW than during single-task walking (STW) (3, 4). However, the gait characteristics of DTW among individuals with cerebral small vessel disease (CSVD) remain unclear (5, 6). Walking (which involves the planning and execution of movements, postural control, and motor coordination) and the secondary task would simultaneously compete for similar neural resources. Patients with diseases might have a reduced total of neural resources available, and this loss may be compensated during STW; however, this compensatory mechanism is limited by the secondary task during DTW. Motor-cognitive DTW (cognitive DTW) and motor-motor DTW (motor DTW) can be achieved by asking participants to perform arithmetic calculations (7–9) and carry a tray of empty glasses (8, 10), respectively, whilst walking.
In CSVD, structural abnormalities or dysfunction of cerebral microvessels often results in clinical, imaging, or pathological changes (11). Generally, CSVD affects the integrity of white matter connectivity (12) and is detected via brain computed tomography or magnetic resonance imaging (MRI). Imaging-based biomarkers for CSVD include recent small subcortical infarcts, white matter hyperintensities (WMHs), lacunar infarctions, enlarged perivascular spaces, cerebral microbleeds, and atrophy (13). The clinical characters of CSVD are gait abnormalities and cognitive deficits, which increase the risk of falls and mortality (14). Further, CSVD and gait disorders have several potential common mechanisms. For example, WMHs may influence gait posture through alterations in motion pathways and cortical thickness, changes in cognition and motion pathways induced by lacunar infarctions may exacerbate gait disorders, and damage to motion pathways induced by cerebral microbleeds may affect gait (15). Furthermore, the primary cognitive impairment observed in CSVD is related to executive function (14). This is also supported by the documented correlation between gait speed and executive function performance in the elderly (16). Consequently, the lack of executive function leads to gait deterioration in patients with CSVD. Moreover, brain regions involved in gait control and cognitive tasks appear to be interlinked (17). Specifically, the sensorimotor network, frontoparietal network, and auxiliary motor areas might influence gait control and cognitive tasks simultaneously (18). Gait might be interfered when the concurrent tasks compete for these shared neural networks which is limited in CSVD patients (19). Furthermore, Coleman's work verified a 1:1 integer ratio between heart and gait rates in normal individuals (20). Coupling between cardiac and locomotor rhythms is present at faster speeds but not at slow or comfortable speeds in healthy individuals. This suggests that the two rhythms must couple when there is a need to compensate for cognitive difficulties, such as during a subtraction task (21). However, this compensatory mechanism may be limited in certain diseases. Additionally, heart rate variability is related to executive function and prefrontal neural function, which play a critical role in the performance of DTW (19, 22). Therefore, the change in cardiac rhythm might be another reason for the deterioration in DTW performance. As a systemic disease, CSVD can impair the function of multiple organs, particularly the heart. The study indicates that decreased heart rate variability may be a potential risk factor for CSVD (23). Additionally, in most cases, individuals with CSVD do not often present with clinical abnormalities; instead, they show atypical neurological symptoms that are difficult to detect using traditional methods. DTW can exacerbate gait disorders and provide vital information regarding changes in walking patterns. Therefore, patients with CSVD may be particularly affected by DTW. Moreover, digital gait analysis can provide accurate parameters for assessing gait disorders (24).
Motor and cognitive DTW conditions have been widely used in studies on neurological diseases, including CSVD (5, 6, 9). However, there remains no consensus on which secondary task should be paired with walking to detect changes in gait. Accordingly, we aimed to investigate differences in walking patterns between motor and cognitive DTW. Further, we assessed the association of neuroimaging biomarkers with gait characteristics during STW and DTW. According to previously observation in our hospital, the hypotheses were as follows: (1) the total CSVD burden score may have superior predictive validity and (2) cognitive DTW may play an important role in detecting gait deterioration.
This study was conducted in accordance with the Declaration of Helsinki and approved by the Academic Ethics Committee of the Biological Sciences Division of the Seventh Medical Centre of the People's Liberation Army General Hospital (Beijing, China). All participants provided informed consent.
This cross-sectional study included 126 patients with CSVD from the Department of Neurology at the Seventh Medical Centre of People's Liberation Army General Hospital (Beijing, China) from September 1, 2020, to September 1, 2021. All patients were screened and interviewed by research personnel. Most participants were willing to undergo MRI owing to complaints such as mild dizziness, mild headache, mood disturbances, cognitive disorders, and motor dysfunction. The inclusion criteria were as follows: (1) ability to independently walk 31 steps; (2) sufficient ability to comprehend and adhere to instructions; and (3) having at least one of the following imaging manifestations of CSVD: WMH, lacunar infarction, or microbleeds. The exclusion criteria were as follows: (1) inability to independently walk 31 steps with or without a tray in their hands or (2) inability to comprehend and adhere to instructions. Further, we excluded individuals with any of the following characteristics: acute cerebral ischaemic or bleeding episodes; leukoencephalopathy with immune, demyelinating, or genetic causes; major psychiatric diseases; gait and balance disorders caused by non-vascular factors such as degenerative or musculoskeletal diseases; dementia based on the Mini-Mental State Examination (MMSE) score (25), and the optimal cut-off points for dementia were 17 for illiterate, 20 for individuals with 1–6 years of education, and 24 for individuals with seven or more years of education (26); communication barriers, including language, vision, or hearing impairment that could impede assessment efforts; and MRI contraindications. The age, sex, years of education, and MMSE scores were recorded. Additionally, the number of comorbid conditions (hypertension, angina, myocardial infarction, hyperlipidaemia, diabetes, migraine, and arthritis), as well as medical and treatment histories, were recorded during in-person interviews.
Neuroimaging parameters were obtained using a 3.0 T MRI scanner (SIEMENS AG, Munich, Germany). The imaging protocols were as follows: T1-weighted imaging, T2-weighted imaging, fluid-attenuated inversion recovery, and susceptibility-weighted imaging. The findings were interpreted by two experienced clinical neurologists who were blinded to information regarding the participants.
Lacunar infarcts are often defined as round or ovoid, subcortical, fluid-filled cavities (signal similar to that of cerebrospinal fluid) with a diameter of 3–15 mm and are consistent with a previous acute small subcortical infarct or haemorrhage (13). Contrastingly, microbleeds are defined as small (generally 2–5 mm in diameter but sometimes up to 10 mm) signal-void areas with associated blooming observed on T2-weighted or susceptibility-weighted imaging (13). WMH were assessed using the Fazekas scale (27). The highest grade observed in either the periventricular or subcortical area (grades 1–3) was documented (9, 27). The Fazekas scale is a simple tool that is widely used in studies on CSVD and Alzheimer's disease; moreover, the number of lacunar infarcts and microbleeds was calculated. These parameters were used to determine the total CSVD burden score, which may better reflect the overall CSVD-induced damage than a single neuroimaging biomarker (28). Specifically, the total CSVD burden score was calculated by counting the number of MRI features, including lacunar infarcts, cerebral microbleeds, and WMHs (score range: 0–3), as previously described (28).
Here, one point was assigned if the participant had three or more lacunar infarctions. Another point was assigned if the participant had any number of cerebral microbleeds. Finally, another point was added if the participant showed confluent or deep WMHs (Fazekas score: 2 or 3). As only a few participants attained the highest total CSVD burden scores, the participants were divided into the following three subgroups: high burden (score: 2 or 3), medium burden (score: 1), and low burden (score: 0). Additionally, when lacunes or microbleeds were calculated separately, the existence of lacunes or microbleeds was defined as the presence of two or more lacunes or any microbleeds.
Gait parameters were obtained from patients under different conditions: (1) only walking (STW), (2) walking whilst performing three serial subtractions from a randomly selected starting number (90, 95, 100, or 105; cognitive DTW). For example, 95-3,−3, and−3; and (3) walking whilst holding a tray with four empty glasses placed on the corners (motor DTW).
A meta-analysis indicated that cognitive tasks that involve internal interfering factors (mental tracking) seem to disturb gait performance more than those involving external interfering factors (reaction time) (29). Another literature review of Parkinson′s disease showed that secondary tasks which mainly involved executive functions, including arithmetic, language, or motor functions, considerably affected gait parameters; however, tasks that involved memory and visual-spatial function only had a small effect on gait characteristics (4). Moreover, although studies used different secondary tasks for DTW, there was strong evidence suggesting that velocity was affected in DTW across all the secondary tasks (4). Given the simplicity and accessibility of arithmetic tasks, we applied it to the cognitive DTW tasks.
In both STW and DTW conditions, the participants comfortably walked 31 strides in a passageway. According to the regulations, participants are required to commence walking 6 steps before the starting line and conclude six steps after the 25th stride. To prevent the impact of acceleration and deceleration on gait, we only analysed 25 strides in the middle part of the test. In the DTW condition, the participants were required to perform both the walking and secondary tasks to the best of their ability without prioritising either activity. The starting and end points of each trial were marked and recorded.
Gait parameters were recorded using a MiniSun Intelligent Device for Energy Expenditure and Activity System (MiniSun, Fresno, CA, USA), which is a wearable gait analyser that provides temporal (time) and spatial (distance) information via a movable sensor connected to a computer. It comprises a recorder and five acceleration sensors. The position of the acceleration sensors is fixed on the posterior edge of the fourth metatarsal head on both soles, the anterior and middle positions of the thighs on both sides, and 4 cm below the midpoint of the sternoclavicular joint connexion on both sides. This device has been shown to obtain extremely accurate spatiotemporal parameters at different conditions (walking, running, or climbing up and down stairs) (24, 30–32). Additionally, this device has been used to assess gait disorders in patients with CSVD (9, 33).
We measured the average values of velocity, cadence, stride length, and stride time. Stride time (s) was defined as the time taken to complete a walking cycle, i.e., the time elapsed from the heel of one lower limb leaving the ground to the same heel returning to the ground. Stride length (m) was defined as the distance between the heel of one lower limb leaving the ground to the same heel landing again. Velocity (m/s) was calculated as the velocity of two successive strides. Cadence (steps/min) was calculated as the number of steps/stairs per minute (8).
Gait variability (%) was determined as the coefficient of variation (CV) calculated using the four aforementioned indicators (2). As the ratio of both legs was related, we calculated the CV for one side as follows:
A high CV value indicated large variability. Further, we calculated the dual-task cost (DTC) as follows (34):
A positive DTC value indicated lower dual-task ability, whilst a negative value indicated higher dual-task ability in velocity, cadence, and stride length. On the contrary, a negative DTC value indicated lower dual-task ability in stride time.
All individuals completed a set of neuropsychological assessments, including the MMSE, verbal fluency test, clock drawing test, and the trail-making test part B (TMT-B). The verbal fluency test was used to assess language skills. Here, the number of animals which could be named by participants within 1 min was counted. The higher the number of names, the less severe the damage to word fluency. Visual search speed and cognitive flexibility were assessed using the TMT-B. Here, the participant connected a trail through symbols (numbers 1, 2, 3, … 9 and corresponding Chinese characters 壹, 贰, 叁, …玖) in the correct order. The time from the instruction to start until trial completion was recorded. The longer the time, the more severe the damage to performing function. Visual-spatial skills were assessed using the transformed score of the clock drawing test. Here, the participants were asked to draw the face of a clock with all the numbers and set the time to 10 min past 11 o'clock. The drawing score system was assessed using 13-point criteria (35, 36). General cognitive function was assessed using the MMSE. A low score indicated limited cognitive function.
Normality was assessed using the Shapiro–Wilk test. Variables with normal and skewed distributions are presented as the mean ± standard deviation (SD) and median with interquartile range (IQR), respectively. Categorical variables are represented as frequencies. Normally distributed variables were assessed using a one-way analysis of variance test. Parameters with skewed distributions were analysed using the nonparametric Kruskal–Wallis test. Categorical variables were analysed using the chi-square test. Spatiotemporal parameters and their DTCs or variability were analysed using generalised estimating equations, with three groups (low, medium, and high burden) and two or three conditions in STW and DTW. In the case of interaction between group and condition, we performed the post-hoc analysis with Bonferroni correction to detect discrepancies. Spearman's rank correlation was performed to determine the association of neuroimaging markers (ordered categorical variables) with spatiotemporal parameters in different conditions. All statistical analyses were performed using SPSS version 26.0 (IBM, Armonk, NY, USA), all the figures were created with GraphPad Prism 9. Statistical significance was set at P < 0.05.
Table 1 presents the basic characteristics of the included participants. We observed no significant among-group differences in age, sex, years of education, or comorbidity (low-, medium-, and high-burden groups; P > 0.05). Further, Table 1 summarises the results of traditional cognitive assessment. The total CSVD burden score was negatively correlated with the TMT-B scores. However, there were no among-group differences in the MMSE, clock drawing test, and verbal fluency test scores.
Additionally, the average number of participants was 2.37 for lacunar infarctions and 1.55 for cerebral microbleeds. Approximately 40 participants exhibited three or more lacunar infarctions, while 60 participants displayed one or more cerebral microbleeds. Furthermore, there were 38 participants with a Fazekas grade of 2 and 20 participants with a grade of 3. Therefore, in accordance with regulations, the participants were divided into groups based on burden level: 30 in the low burden group, 34 in the medium burden group, and 62 in the high burden group.
Tables 2, 3 present the main effects and interactions in spatiotemporal measures and their DTCs or variabilities. The outcomes presented in Table 2 show that there were significant interactions between the group and condition for stride time, stride length, and their variabilities. Moreover, speed and cadence had a significant interaction; however, only significant main effects were observed for the variabilities in speed and cadence. Therefore, we included all variables in the post-hoc analysis, except for the variabilities in speed and cadence. In the STW condition, only speed and stride length (P = 0.034 and P = 0.014, respectively) differed between the low-burden and high-burden groups. Similarly, in the motor DTW condition, there were differences in stride length (P = 0.021) between the low-burden and high-burden groups. Notably, almost all parameters showed among-group differences in the cognitive DTW condition (0.026 < P < 9.078 × 10−10). In the high-burden group, deterioration of spatial parameters during the motor DTW condition was seen compared with those in the STW condition (speed, P = 0.005; stride length, P = 0.014). Contrastingly, almost all spatiotemporal parameters of cognitive DTW significantly deteriorated compared with those in the STW condition in the low-burden (speed, P = 0.024; cadence, P = 0.001; stride length, P = 0.044; stride time, P = 0.086), medium-burden (speed, P < 0.001; cadence, P < 0.001; stride length, P = 0.155; stride time, P < 0.001), and high-burden (speed, P < 0.001; cadence, P < 0.001; stride length, P < 0.001; stride time, P < 0.001) groups. In addition, we observed significant differences in the CV of stride time (P = 0.002) and length (P = 0.002) between the STW and cognitive DTW conditions only in the high-burden group.
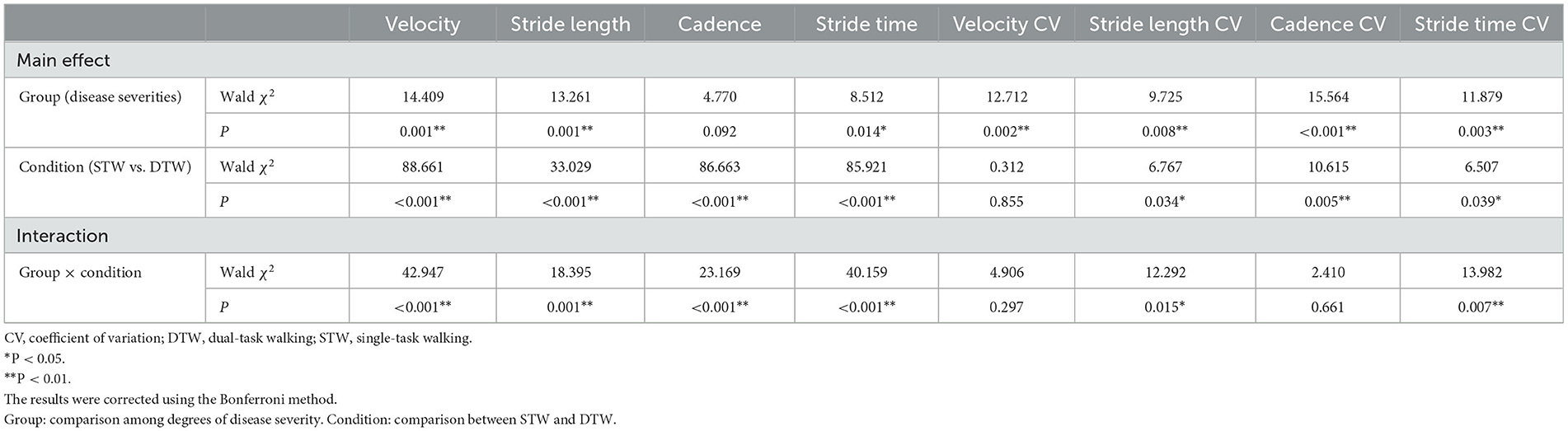
Table 2. Differences in gait parameters in generalised estimation equation among patients with cerebral small vessel disease.
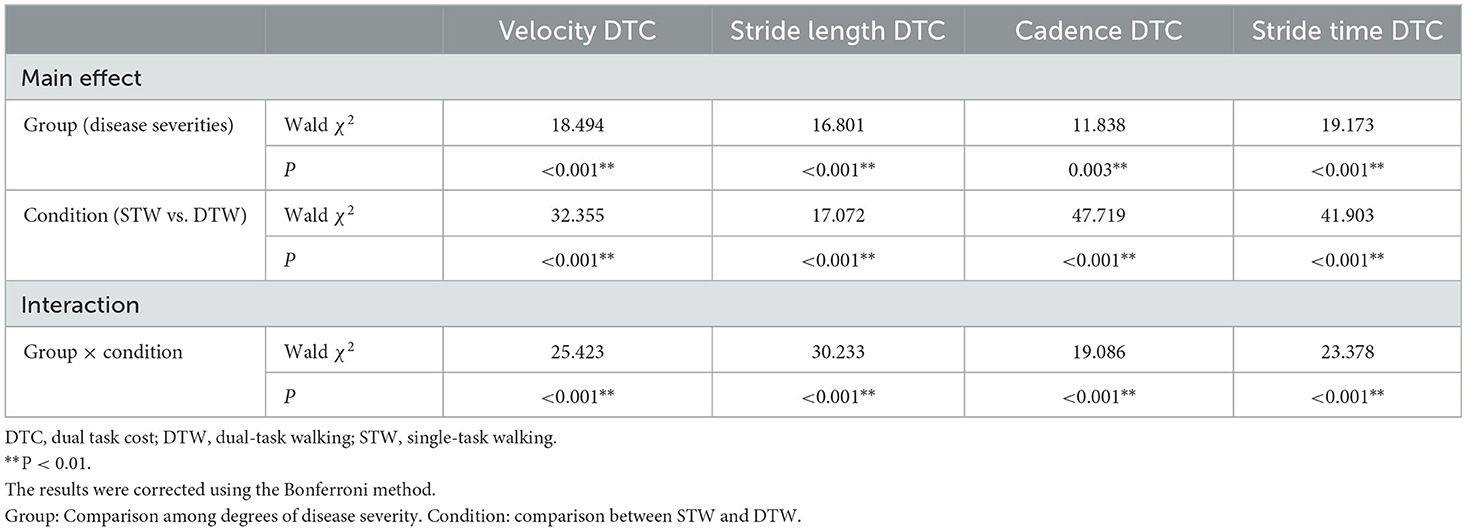
Table 3. Differences in gait DTC in the generalised estimation equation among patients with cerebral small vessel disease.
As summarised in Table 3, the DTCs in the motor and cognitive DTW conditions showed significant main effects and interactions for all parameters. Post-hoc analyses revealed similar findings as those mentioned above. We observed significant among-group differences in the DTCs for all parameters in the cognitive DTW condition (0.046 < P < 2.883 × 10−12) but not in the motor DTW condition (P > 0.050). Furthermore, compared with the motor DTW condition, the cognitive DTW condition showed significantly higher DTCs in the medium-burden (speed, P < 0.001; cadence, P < 0.001; stride length, P = 0.040; stride time, P < 0.001) and high-burden (speed, P < 0.001; cadence, P < 0.001; stride length, P < 0.001; stride time, P < 0.001) groups.
The values of spatiotemporal gait parameters measured in both STW and DTW conditions showed in Tables 4, 5. The significant differences of post-hoc analysis showed in Figures 1–4.
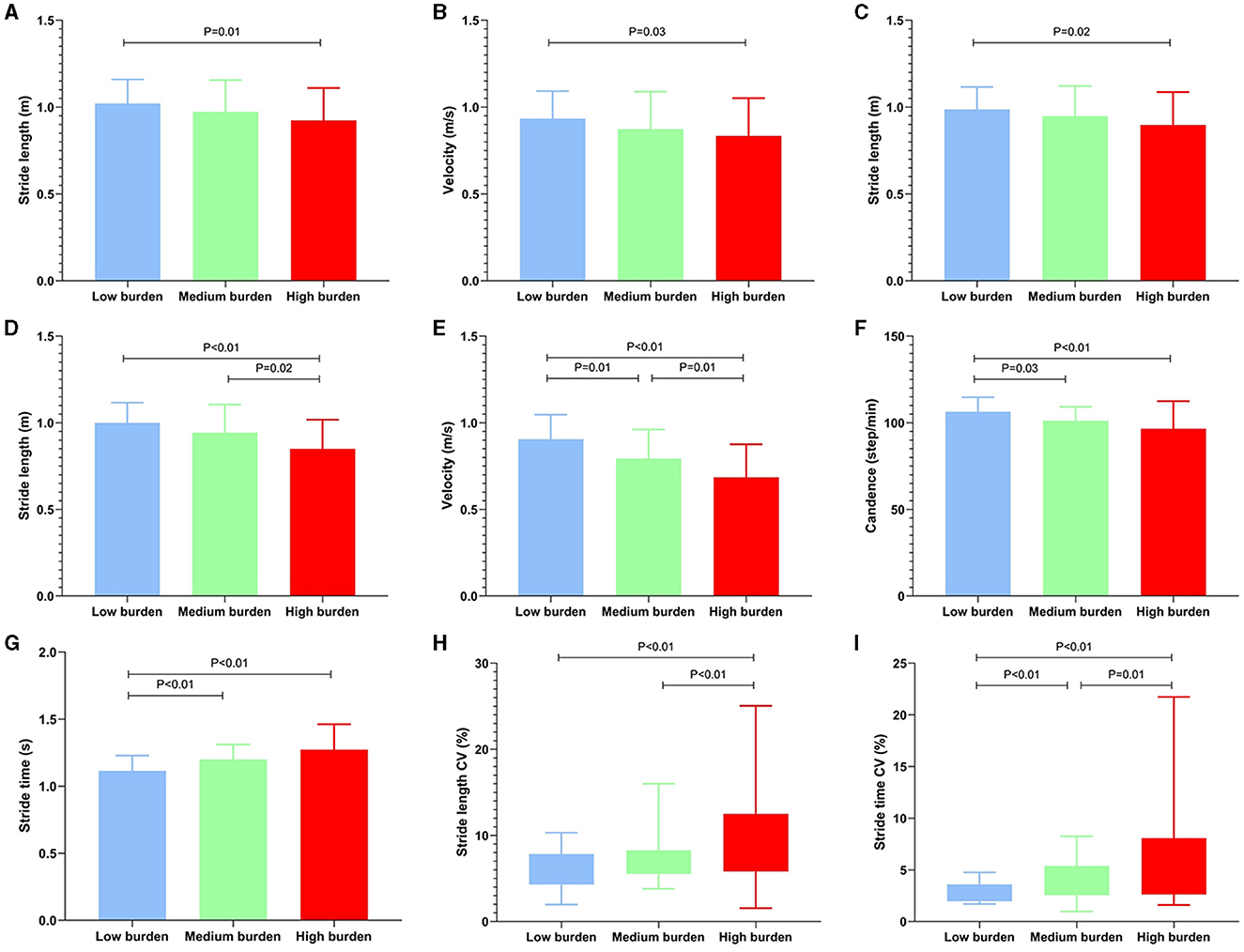
Figure 1. Significant differences among the total CSVD burden in basic parameters and its CV. The basic parameter values were represented by medians, while the CV was represented by the interquartile range. CSVD, cerebral small vessel disease; STW, single-task walking; DTW, dual-task walking; CV, coefficient of variation. (A, B) Differences of basic parameters among the groups during STW; (C) Differences of basic parameters among the groups during motor DTW; (D–G) Differences of basic parameters among the groups during cognitive DTW; (H, I) Differences of CV among the groups during cognitive DTW. The criterion for statistical significance was set at P < 0.05.

Figure 2. Significant intergroup differences in basic parameters and its CV during different walking patterns. The basic parameter values were represented by medians, while the CV was represented by the interquartile range. STW, single-task walking; DTW, dual-task walking; CV, coefficient of variation. (A–C) Discrepancy of basic parameters during different walking patterns in low burden group; (D, H) Discrepancy of CV during different walking patterns in high burden group; (E–G) Discrepancy of basic parameters during different walking patterns in medium burden group; (I–L) Discrepancy of basic parameters during different walking patterns in high burden group. The criterion for statistical significance was set at P < 0.05.
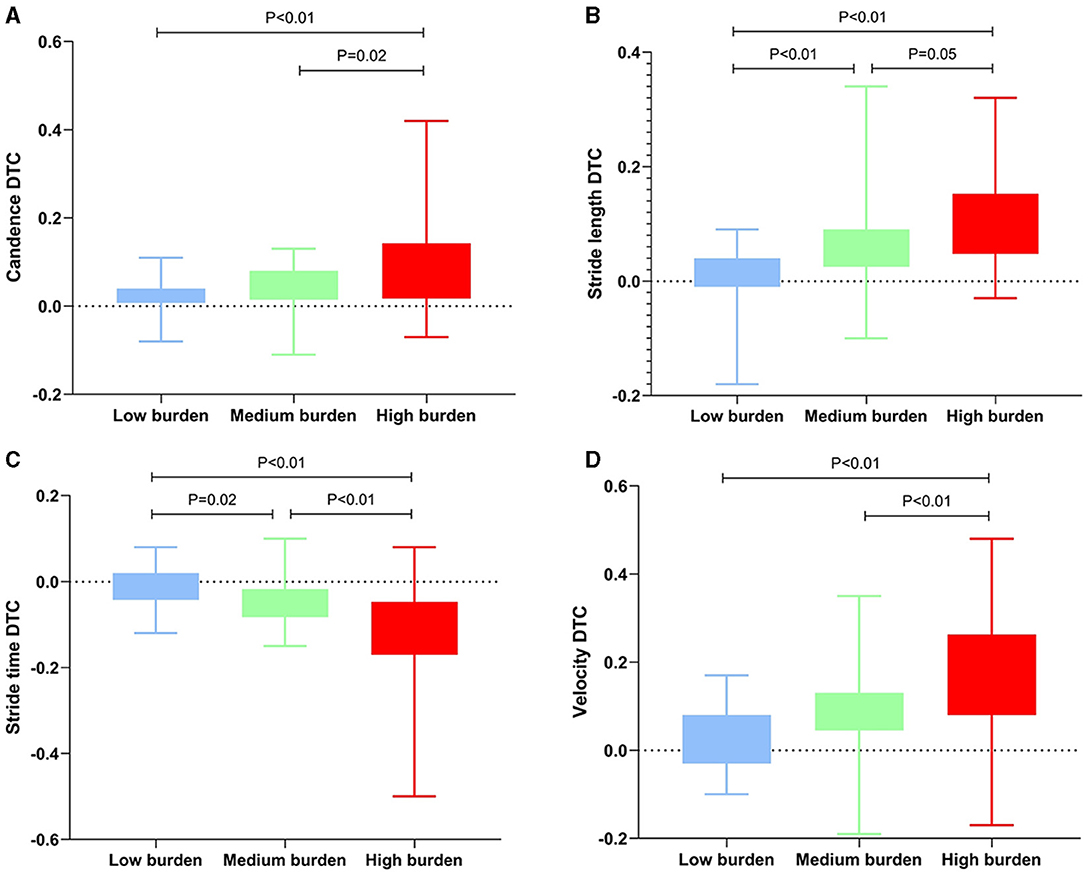
Figure 3. Significant differences among the total CSVD burden in DTC. The DTC was represented by the interquartile range. CSVD, cerebral small vessel disease; DTW, dual-task walking; DTC, dual task cost. (A–D) Differences of DTC among the groups during cognitive DTW. The criterion for statistical significance was set at P < 0.05.
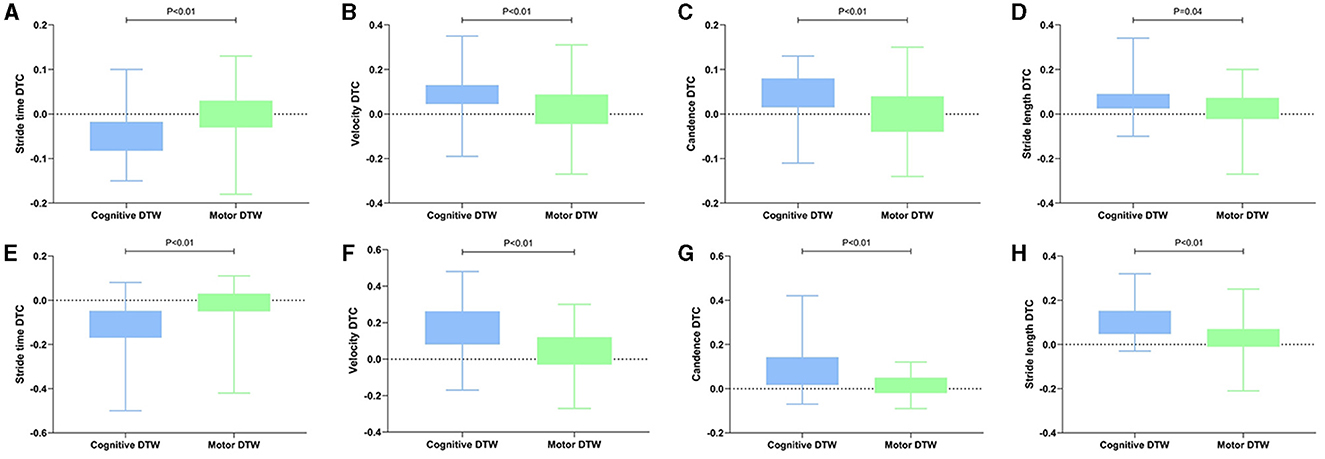
Figure 4. Significant intergroup differences in DTC during different walking patterns. The DTC was represented by the interquartile range. DTW, dual-task walking; DTC, dual task cost. (A–D) Discrepancy of DTC during different walking patterns in medium burden group; (E–H) Discrepancy of DTC during different walking patterns in high burden group. The criterion for statistical significance was set at P < 0.05.
As shown in Table 6, there was a relationship between spatiotemporal gait measures and the CSVD burden. Regarding gait velocity, the total CSVD burden score showed a moderate negative relationship with speed and a positive correlation with its variability or DTC in the cognitive DTW condition; however, it was not correlated with any of the parameters in the STW or motor DTW condition. Similar results were observed for WMHs; however, they had a relatively smaller correlation coefficient. Lacune infarctions were moderately correlated with cognitive DTW velocity and its DTC; moreover, the correlation coefficient was similar to that for WMHs. However, there was no relation with the variability. Additionally, microbleeds were not correlated with any of the spatiotemporal measures.
Regarding cadence, the total CSVD burden score and WMHs showed a moderate negative relationship with the cadence in the cognitive DTW condition and a positive relationship with its DTC. The correlation coefficients were similar. Contrastingly, only the total CSVD burden score was significantly related to the variability of cadence. Microbleeds and lacune infarctions were not correlated with cadence parameters.
Regarding stride length, the total CSVD burden had a moderate correlation with stride length and its DTC or variability in the cognitive DTW condition but not in the STW and motor DTW conditions. However, WMHs were not correlated with stride length and its DTC or variability. Contrastingly, lacune infarctions showed a moderate negative correlation with stride length, whilst microbleeds showed a positive correlation with the DTC of stride length in the cognitive DTW condition.
Finally, the total CSVD burden had a moderate correlation with stride time and its DTC or variability in the cognitive DTW condition. Similar to that in speed, WMHs were correlated with stride time and its DTC, but not its variability, in the cognitive DTW condition. WMHs had a smaller correlation coefficient than that of the total CSVD burden score. Similarly, lacune infarctions and microbleeds were not correlated with any of the parameters for stride time.
We observed among-group differences in all gait parameters during cognitive DTW. However, for STW and motor DTW, only some parameters showed differences between the low-burden and high-burden groups. In addition, the total CSVD burden had the strongest relationship with gait parameters in the cognitive DTW condition compared with any single neuroimaging index.
Previous studies on older patients with Alzheimer's disease have discussed the correlation between WMH and gait characteristics during STW. They indicated that only among-group stride length differences were detected according to the degree of WMH (37). Another study revealed that CSVD-related white matter alterations were significantly correlated with reduced stride length in individuals with pure CSVD (8). Similarly, another study showed that spatial, but not temporal, gait features were correlated with the WMH degree in the STW condition (38). A Chinese cross-sectional study on patients with CSVD showed that Fazekas scores were associated with gait parameters, including the step speed and length, but not frequency, in the STW condition (39). These findings could be attributed to the fact that CSVD commonly damages the integrity of subcortical connexions (40). Spatial gait parameters are primarily controlled by cortical and subcortical areas, specifically neurons connecting in the frontal cortex and basal ganglia. Contrastingly, temporal features might be more dependent on mechanisms in the brainstem and spinal cord (41, 42).
Our findings are inconsistent with those of the previous reports. Although speed and stride length differed between the low-burden and high-burden groups, the total CSVD burden or WMH was not significantly correlated with spatial gait parameters following the Bonferroni correction. This indicates that gait parameters obtained in the STW condition are not sensitive indicators for the severity of CSVD.
DTW is a complex task requiring normal cognitive functions; accordingly, performance deterioration in DTW is indicative of competition for attentional resources (43). CSVD severity is negatively correlated with the availability of attentional resources (44). To this end, gait performance deteriorates when more demanding tasks are simultaneously implemented. However, the specific associations between CSVD biomarkers and gait performance in the DTW condition remain unclear.
A previous study (38) showed that WMH volume had a negative association with velocity and stride length in the motor DTW condition, which is inconsistent with our findings. In our study, although stride length differed between the low-burden and high-burden groups in the motor DTW condition, total CSVD burden and WMH were not correlated with spatial gait parameters after Bonferroni correction.
These findings are consistent with the task prioritisation model (45), which suggests that individuals prioritise complex tasks in case of competition for attentional resources. Walking requires mainly somatosensory central processing and somatosensory responses; moreover, secondary motor tasks also require additional manual responses (46). Therefore, both tasks have similar complexities, and the secondary motor task does not take up extensive neural resources. Accordingly, gait parameters in the motor DTW condition are not affected in the early disease stage.
Additionally, the correlation coefficients of the total CSVD burden score or WMH were similar between the motor DTW and STW conditions. Taken together, gait parameters in the motor DTW condition cannot effectively distinguish the severity stratification of disease among patients with CSVD.
Hairu et al. (38) discovered that temporal and parietal WMH volumes were negatively correlated with stride length during cognitive DTW. Another study indicated that deep WMHs were significantly correlated with gait speed in the DTW condition (5, 47), and executive function mediated this relationship. Patients with pure CSVD have shown deficits in all spatiotemporal gait parameters in the semantic DTW condition (8). Additionally, compared with healthy individual, CSVD patients showed significant deteriorate in stride time CV during cognitive DTW (9, 48). In our study, almost all gait parameters showed differences among groups that were stratified according to total CSVD burden score. These findings were consistent with those in the correlation analysis. The total CSVD burden score was correlated with temporal and spatial parameters and their variabilities in the DTW condition. Moreover, the DTCs of basic gait parameters showed an identical performance with basic parameters. This can be attributed to the interlinking between brain networks responsible for pace control and those responsible for cognitive task performance (9), leading to competition for the same resources and, thus, impairment of all gait characteristics (8).
Pantoni reported that among several neuroimaging biomarkers, WMHs in specific brain regions had the strongest correlation with gait disturbance (12). Contrastingly, we found that the total CSVD burden but not WMHs had the strongest correlation with gait disturbance. Specifically, the variability of spatiotemporal parameters was associated with total CSVD burden but not WMHs; moreover, the correlation coefficient of WMHs was lower than that of the total CSVD burden score for all gait parameters except cadence. This indicates that the total CSVD burden score is a stronger predictor of gait performance than any single biomarker. Notably, only a few gait parameters were associated with microbleeds and lacunar infarcts, indicating the poor predictive utility of these biomarkers for gait abnormalities.
Hairu et al. (38) reported that in patients with Alzheimer's disease, motor DTW resulted in greater deterioration of gait characteristics (velocity, cadence, and stride length) than cognitive DTW. Similarly, Cherng et al. (46, 49) found that in children with developmental coordination disorder, motor DTW resulted in greater interference of gait parameters than cognitive DTW, as indicated by decreased velocity, cadence, stride length, and double limb support. Contrastingly, we found that gait parameters in the cognitive, but not motor, DTW condition were significantly correlated with the disease severity.
According to Wickens, attentional resources are not unitary but are divided into various pools, which are “defined by a three-dimensional metric consisting of the stages of processing, codes of perceptual and central processing, and modalities of input and response” (50). Walking requires mainly somatosensory central processing and somatosensory responses. In addition, the secondary motor task also requires additional manual responses. Contrastingly, a cognitive secondary task will require further executive functional and verbal central processing as well as vocal responses (46), with limited opportunities for compensatory mechanisms. Therefore, in cognitive DTW, more brain regions may be active, and the remaining resources do not meet the demands of gait control. Accordingly, a cognitive task greatly interferes with walking, leading to obvious gait abnormalities in the early disease stage.
In our study, the DTC in the cognitive DTW condition was significantly higher than that in the motor DTW condition, suggesting that parameters in the cognitive DTW condition could better predict abnormal gait in individuals with CSVD. This finding is inconsistent with previous literature (38, 46, 49), which could be attributed to differences in the examined diseases. Specifically, Alzheimer's disease mainly causes grey matter damage, whilst CSVD mainly affects cortical and subcortical connecting fibres (38). Furthermore, developmental coordination disorder is a movement disorder; accordingly, the motor DTW condition yields more obvious differences (46).
Taken together, patients with CSVD showed significant gait deterioration, especially in the cognitive DTW condition. Our conclusion has been substantiated by an increasing body of evidence. A literature review spanning from 1997 to 2017 revealed that gait changes associated with cognitive DTW may serve as a potential marker for nervous system diseases (51). Therefore, in daily life, patients should reduce the load of secondary tasks while walking, especially cognitive tasks. However, the underlying brain network mechanisms during DTW remain unclear. Future studies should use diffusion tensor imaging to observe changes in white matter fibre during DTW.
Furthermore, despite the prevalence of gait disorders and falls among patients with CSVD (11, 12, 15), a definitive cure remains elusive. Previous studies have indicated that cognitive dual-task training is both safe and effective in improving various spatiotemporal gait parameters (52). Additionally, another systematic review confirmed that cognitive DTW training improves balance and reduces the incidence of falls in older adults (53). Against this backdrop, we have substantiated the significance of cognitive DTW for patients with CSVD. We speculate that CSVD patients would also derive benefits from dual-task training, including improved exercise performance and reduced fall incidence. However, as no studies have investigated the impact of dual-task training in CSVD patients, a prospective cohort study is necessary to explore the implications of dual-task training in the future.
This study has some limitations. First, the sample size was relatively small; accordingly, a large-scale multicentre longitudinal study is warranted to verify our findings. Second, the patients with CSVD had different clinical features. Therefore, there was heterogeneity in the participants of our study, which might have caused bias in the results. Third, the neuroimaging assessment was not extensively comprehensive and accurate. Specifically, neuroimaging findings were semi-quantitatively evaluated, which could have introduced systematic errors. The use of quantitative technology could better demonstrate among-group differences and correlations, especially during cognitive DTW. Fourth, although the sample entropy, asymmetry and phase coordination index might be good indicators, we did not include it in our study. In the future, our intention is to increase the sample size to further investigate the role of these parameters in the early diagnosis and management of CSVD.
Parameters in the cognitive DTW condition may be more appropriate than those in the motor DTW condition for the evaluation of gait abnormalities in patients with CSVD. Moreover, the total CSVD burden score might have a better predictive utility than any single neuroimaging marker. Patients with CSVD, especially those with moderate-to-severe disease, should reduce the load of secondary tasks while walking in daily life, especially cognitive tasks.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Academic Ethics Committee of the Biological Sciences Division of the Seventh Medical Centre of the People's Liberation Army General Hospital (Beijing, China). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
CX: Writing—original draft. HX: Writing—original draft. TL: Writing—review & editing. YD: Writing—review & editing. HZ: Writing—review & editing. YH: Writing—review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Wu Jieping Foundation (Grant No.: 320.6750.18456).
The authors thank Dr. Wei Wei for the magnetic resonance imaging support and Miss Jiajia Gao for her assistance in data processing.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
CMB, cerebral microbleeds; CSVD, cerebral small vessel disease; DTC, dual-task cost; DTW, dual-task walking; IQR, interquartile range; LI, lacunar infarction; MMSE, mini-mental state examination; MRI, magnetic resonance imaging; SD, standard deviation; STW, Single-task walking; TMT-B, trail-making test-part B; WMH, white matter hyperintensity.
1. Montero-Odasso M, Verghese J, Beauchet O, Hausdorff JM. Gait and cognition: a complementary approach to understanding brain function and the risk of falling. J Am Geriatr Soc. (2012) 60:2127–36. doi: 10.1111/j.1532-5415.2012.04209.x
2. Wollesen B, Voelcker-Rehage C, Regenbrecht T, Mattes K. Influence of a visual–verbal Stroop test on standing and walking performance of older adults. Neuroscience. (2016) 318:166–77. doi: 10.1016/j.neuroscience.2016.01.031
3. Gonzales JU, James CR, Yang HS, Jensen D, Atkins L, Al-Khalil K, et al. Carotid flow pulsatility is higher in women with greater decrement in gait speed during multi-tasking. Gait Posture. (2017) 54:271–6. doi: 10.1016/j.gaitpost.2017.03.024
4. Raffegeau TE, Krehbiel LM, Kang N, Thijs FJ, Altmann LJP, Cauraugh JH, et al. A meta-analysis: Parkinson's disease and dual-task walking. Parkinsonism Relat Disord. (2019) 62:28–35. doi: 10.1016/j.parkreldis.2018.12.012
5. Ghanavati T, Smitt MS, Lord SR, Sachdev P, Wen W, Kochan NA, et al. Deep white matter hyperintensities, microstructural integrity and dual task walking in older people. Brain Imaging Behav. (2018) 12:1488–96. doi: 10.1007/s11682-017-9787-7
6. Hashimoto M, Takashima Y, Uchino A, Yuzuriha T, Yao H. Dual task walking reveals cognitive dysfunction in community-dwelling elderly subjects: the Sefuri brain MRI study. J Stroke Cerebrovasc Dis. (2014) 23:1770–5. doi: 10.1016/j.jstrokecerebrovasdis.2014.05.008
7. Radovanović S, Perić S, Savić-Pavićević D, Dobričić V, Pešović J, Kostić V, et al. Comparison of temporal and stride characteristics in myotonic dystrophies type 1 and 2 during dual-task walking. Gait Posture. (2016) 44:194–9. doi: 10.1016/j.gaitpost.2015.12.020
8. Finsterwalder S, Wuehr M, Gesierich B, Dietze A, Konieczny MJ, Schmidt R, et al. Minor gait impairment despite white matter damage in pure small vessel disease. Ann Clin Transl Neurol. (2019) 6:2026–36. doi: 10.1002/acn3.50891
9. Ma R, Zhào H, Wei W, Liu Y, Huang Y. Gait characteristics under single-/dual-task walking conditions in elderly patients with cerebral small vessel disease: analysis of gait variability, gait asymmetry and bilateral coordination of gait. Gait Posture. (2022) 92:65–70. doi: 10.1016/j.gaitpost.2021.11.007
10. Monticone M, Ambrosini E, Fiorentini R, Rocca B, Liquori V, Pedrocchi A, et al. Reliability of spatial–temporal gait parameters during dual-task interference in people with multiple sclerosis. A cross-sectional study. Gait Posture. (2014) 40:715–8. doi: 10.1016/j.gaitpost.2014.06.015
11. Hu W, Huang Y, Wang Y. Consensus of Chinese experts in diagnosis and treatment of cerebral small vessel diseases. Chin J Stroke. (2021) 16:716–26. doi: 10.3969/j.issn.1673-5765.2021.07.013
12. Pantoni L. Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol. (2010) 9:689–701. doi: 10.1016/S1474-4422(10)70104-6
13. Wardlaw JM, Smith EE, Biessels GJ, Cordonnier C, Fazekas F, Frayne R, et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol. (2013) 12:822–38. doi: 10.1016/S1474-4422(13)70124-8
14. Siejka TP, Srikanth VK, Hubbard RE, Moran C, Beare R, Wood A, et al. Frailty and cerebral small vessel disease: a cross-sectional analysis of the Tasmanian study of cognition and gait (TASCOG). J Gerontol A Biol Sci Med Sci. (2018) 73:255–60. doi: 10.1093/gerona/glx145
15. Su C, Yang X, Wei S, Zhao R. Association of cerebral small vessel disease with gait and balance disorders. Front Aging Neurosci. (2022) 14:834496. doi: 10.3389/fnagi.2022.834496
16. Holtzer R, Verghese J, Xue X, Lipton RB. Cognitive processes related to gait velocity: results from the Einstein Aging Study. Neuropsychology. (2006) 20:215–23. doi: 10.1037/0894-4105.20.2.215
17. Smith E, Cusack T, Blake C. The effect of a dual task on gait speed in community dwelling older adults: a systematic review and meta-analysis. Gait Posture. (2016) 44:250–8. doi: 10.1016/j.gaitpost.2015.12.017
18. Zhou X, Zhang C, Li L, Zhang Y, Zhang W, Yin W, et al. Altered brain function in cerebral small vessel disease patients with gait disorders: a resting-state functional MRI study. Front Aging Neurosci. (2020) 12:234. doi: 10.3389/fnagi.2020.00234
19. Klingberg T. Limitations in information processing in the human brain: neuroimaging of dual task performance and working memory tasks. Prog Brain Res. (2000) 126:95–102. doi: 10.1016/S0079-6123(00)26009-3
20. Coleman WM. On the correlation of the rate of heart beat, breathing, bodily movement and sensory stimuli. J Physiol. (1920) 54:213–7. doi: 10.1113/jphysiol.1920.sp001920
21. De Bartolo D, De Giorgi C, Compagnucci L, Betti V, Antonucci G, Morone G, et al. Effects of cognitive workload on heart and locomotor rhythms coupling. Neurosci Lett. (2021) 762:136140. doi: 10.1016/j.neulet.2021.136140
22. Thayer JF, Hansen AL, Saus-Rose E, Johnsen BH. Heart rate variability, prefrontal neural function, and cognitive performance: the neurovisceral integration perspective on self-regulation, adaptation, and health. Ann Behav Med. (2009) 37:141–53. doi: 10.1007/s12160-009-9101-z
23. Tian Y, Yao D, Pan Y, Wang M, Meng X, Zhao X, et al. Implication of heart rate variability on cerebral small vessel disease: a potential therapeutic target. CNS Neurosci Ther. (2023) 29:1379–91. doi: 10.1111/cns.14111
24. Gardner MJ, Barker JU, Briggs SM, Backus SI, Helfet DL, Lane JM, et al. An evaluation of accuracy and repeatability of a novel gait analysis device. Arch Orthop Trauma Surg. (2007) 127:223–7. doi: 10.1007/s00402-006-0279-2
25. Folstein MF, Folstein SE, McHugh PR. ‘Mini-mental state'. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. (1975) 12:189–98. doi: 10.1016/0022-3956(75)90026-6
26. Li H, Jia J, Yang Z. Mini-mental state examination in elderly Chinese: a population-based normative study. J Alzheimers Dis. (2016) 53:487–96. doi: 10.3233/JAD-160119
27. Fazekas F, Chawluk JB, Alavi A, Hurtig HI. Zimmerman RA. MR signal abnormalities at 15 T in Alzheimer's dementia and normal aging. AJR Am J Roentgenol. (1987) 149:351–6. doi: 10.2214/ajr.149.2.351
28. Amin Al Olama AAA, Wason JMS, Tuladhar AM, van Leijsen EMC, Koini M, Hofer E, et al. Simple MRI score aids prediction of dementia in cerebral small vessel disease. Neurology. (2020) 94:e1294–302. doi: 10.1212/WNL.0000000000009141
29. Al-Yahya E, Dawes H, Smith L, Dennis A, Howells K, Cockburn J. Cognitive motor interference while walking: a systematic review and meta-analysis. Neurosci Biobehav Rev. (2011) 35:715–28. doi: 10.1016/j.neubiorev.2010.08.008
30. Zhang K, Werner P, Sun M, Pi-Sunyer FX, Boozer CN. Measurement of human daily physical activity. Obes Res. (2003) 11:33–40. doi: 10.1038/oby.2003.7
31. Gorelick ML, Bizzini M, Maffiuletti NA, Munzinger JP, Munzinger U. Test–retest reliability of the IDEEA system in the quantification of step parameters during walking and stair climbing. Clin Physiol Funct Imaging. (2009) 29:271–6. doi: 10.1111/j.1475-097X.2009.00864.x
32. Li YG, Li LP, Li ZJ, Li H, Li Y, Li Q, et al. Gait analysis in the elderly patients with lumbar spinal stenosis. Int Orthop. (2021) 45:673–9. doi: 10.1007/s00264-020-04935-w
33. Zhào H, Wei W, Liu Y, Gao J, Huang Y. Cognitive frailty among elderly Chinese patients with cerebral small vessel disease: a structural MRI study. Front Med. (2020) 7:397. doi: 10.3389/fmed.2020.00397
34. Kelly VE, Janke AA, Shumway-Cook A. Effects of instructed focus and task difficulty on concurrent walking and cognitive task performance in healthy young adults. Exp Brain Res. (2010) 207:65–73. doi: 10.1007/s00221-010-2429-6
35. Freedman M, Leach M, Kaplan E, Winocur G, Shulman K, Delis DC. Clock Drawing: A Neuropsychological Analysis, 1st ed. New York, NY: Oxford University Press (1994).
36. Zhào H, Chi L, Zhang Y, Huang Y, Tian H. Spatial navigation is impaired in elderly patients with cerebral small vessel disease. Front Neurol. (2021) 12:608797. doi: 10.3389/fneur.2021.608797
37. Nadkarni NK, McIlroy WE, Mawji E, Black SE. Gait and subcortical hyperintensities in mild Alzheimer's disease and aging. Dement Geriatr Cogn Disord. (2009) 28:295–301. doi: 10.1159/000245158
38. Hairu R, Close JCT, Lord SR, Delbaere K, Wen W, Jiang J, et al. The association between white matter hyperintensity volume and gait performance under single and dual task conditions in older people with dementia: a cross-sectional study. Arch Gerontol Geriatr. (2021) 95:104427. doi: 10.1016/j.archger.2021.104427
39. Jiang M, Wu S, Zhang Y, Li Y, Lin B, Pan Q, et al. Impact of white matter hyperintensity and age on gait parameters in patients with cerebral small vessel disease. J Am Med Dir Assoc. (2023) 24:672–8. doi: 10.1016/j.jamda.2022.12.001
40. Wardlaw JM, Smith C, Dichgans M. Small vessel disease: mechanisms and clinical implications. Lancet Neurol. (2019) 18:684–96. doi: 10.1016/S1474-4422(19)30079-1
41. Verwer JH, Biessels GJ, Heinen R, Exalto LG, Emmelot-Vonk MH, Koek HL, et al. Occurrence of impaired physical performance in memory clinic patients with cerebral small vessel disease. Alzheimer Dis Assoc Disord. (2018) 32:214–9. doi: 10.1097/WAD.0000000000000233
42. Martin KL, Blizzard L, Wood AG, Srikanth V, Thomson R, Sanders LM, et al. Cognitive function, gait, and gait variability in older people: a population-based study. J Gerontol A Biol Sci Med Sci. (2013) 68:726–32. doi: 10.1093/gerona/gls224
43. Clark DJ. Automaticity of walking: functional significance, mechanisms, measurement and rehabilitation strategies. Front Hum Neurosci. (2015) 9:246. doi: 10.3389/fnhum.2015.00246
44. Salvadori E, Poggesi A, Valenti R, Della Rocca E, Diciotti S, Mascalchi M, et al. The rehabilitation of attention in patients with mild cognitive impairment and brain subcortical vascular changes using the Attention Process Training-II. The RehAtt Study: rationale, design and methodology. Neurol Sci. (2016) 37:1653–62. doi: 10.1007/s10072-016-2649-z
45. Yang L, Lam FM, Huang M, He C, Pang MY. Dual-task mobility among individuals with chronic stroke: changes in cognitive-motor interference patterns and relationship to difficulty level of mobility and cognitive tasks. Eur J Phys Rehabil Med. (2018) 54:526–35. doi: 10.23736/S1973-9087.17.04773-6
46. Cherng RJ, Liang LY, Hwang IS, Chen JY. The effect of a concurrent task on the walking performance of preschool children. Gait Posture. (2007) 26:231–7. doi: 10.1016/j.gaitpost.2006.09.004
47. Alzaid H, Ethofer T, Kardatzki B, Erb M, Scheffler K, Berg D, et al. Gait decline while dual-tasking is an early sign of white matter deterioration in middle-aged and older adults. Front Aging Neurosci. (2022) 14:934241. doi: 10.3389/fnagi.2022.934241
48. Mukli P, Detwiler S, Owens CD, Csipo T, Lipecz A, Pinto CB, et al. Gait variability predicts cognitive impairment in older adults with subclinical cerebral small vessel disease. Front Aging Neurosci. (2022) 14:1052451. doi: 10.3389/fnagi.2022.1052451
49. Cherng RJ, Liang LY, Chen YJ, Chen JY. The effects of a motor and a cognitive concurrent task on walking in children with developmental coordination disorder. Gait Posture. (2009) 29:204–7. doi: 10.1016/j.gaitpost.2008.08.003
50. Wickens CD. Processing resources in attention. In:Parasuraman R, Davies DR, editors. Varieties of Attention. New York, NY: Academic Press (1984), p. 63–102.
51. Belghali M, Chastan N, Cignetti F, Davenne D, Decker LM. Loss of gait control assessed by cognitive-motor dual-tasks: pros and cons in detecting people at risk of developing Alzheimer's and Parkinson's diseases. GeroScience. (2017) 39:305–29. doi: 10.1007/s11357-017-9977-7
52. Geroin C, Nonnekes J, de Vries NM, Strouwen C, Smania N, Tinazzi M, et al. Does dual-task training improve spatiotemporal gait parameters in Parkinson's disease? Parkinsonism Relat Disord. (2018) 55:86–91. doi: 10.1016/j.parkreldis.2018.05.018
Keywords: cerebral small vessel disease, gait, dual-task walking, white matter hyperintensity, neuroimaging biomarkers
Citation: Xia C, Xie H, Li T, Ding Y, Zhào H and Huang Y (2023) Spatiotemporal gait characteristics during single- and dual-task walking are associated with the burden of cerebral small vessel disease. Front. Neurol. 14:1285947. doi: 10.3389/fneur.2023.1285947
Received: 30 August 2023; Accepted: 30 October 2023;
Published: 13 November 2023.
Edited by:
Gary Kui Kai Lau, The University of Hong Kong, Hong Kong SAR, ChinaReviewed by:
Daniela De Bartolo, Vrije Universiteit Amsterdam, NetherlandsCopyright © 2023 Xia, Xie, Li, Ding, Zhào and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yonghua Huang, aHVhbmd5aEAxNjMuY29t
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.