- 1Center for Rehabilitation Medicine, Department of Neurology, Zhejiang Provincial People’s Hospital (Affiliated People’s Hospital), Hangzhou Medical College, Hangzhou, Zhejiang, China
- 2Center for Rehabilitation Medicine, Department of Radiology, Zhejiang Provincial People’s Hospital (Affiliated People’s Hospital), Hangzhou Medical College, Hangzhou, Zhejiang, China
- 3Department of Neurology, Barrow Neurological Institute (BNI), Phoenix, AZ, United States
- 4Department of Neurology, Huashan Hospital, Fudan University, Shanghai, Shanghai Municipality, China
Objective: The present study aimed to investigate the impact of angiographic thrombus surface morphology on the angiographic and clinical outcomes of basilar artery occlusion (BAO).
Methods: This retrospective study included 141 patients with acute BAO who underwent mechanical thrombectomy (MT). We categorized thrombus surface phenotypes as either regular (smooth and straight, either convex or concave) or irregular. Patients with BAO were grouped based on the presence of a regular or irregular phenotype, and we compared their angiographic and clinical outcomes.
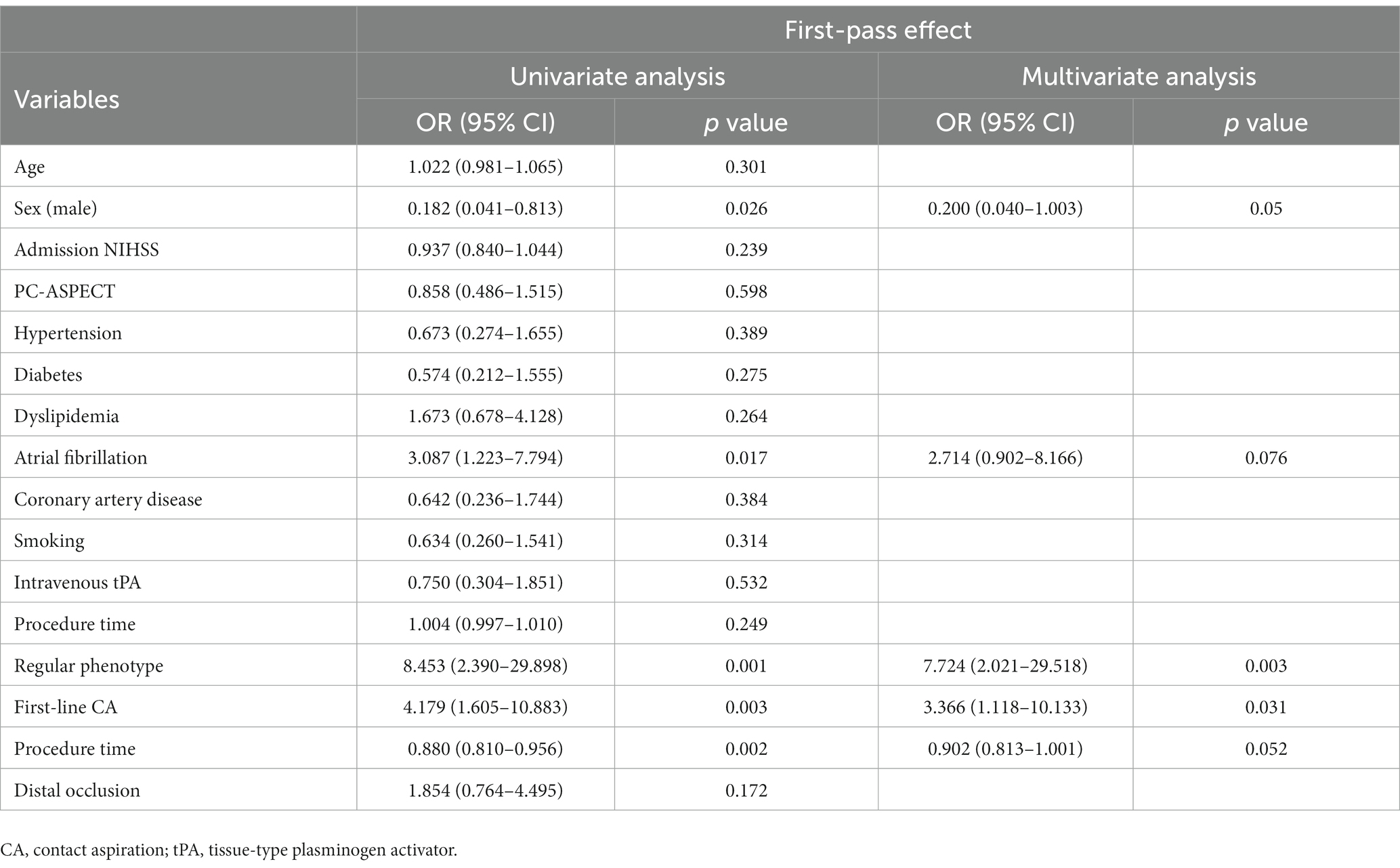
Results: In total, 52.5% (74/141) of acute BAO patients exhibited a regular thrombus morphology. These patients had a higher rate of first-pass effect (28.4% vs. 4.5%, p = 0.0002) and fewer retrieval attempts (2 vs. 2; p = 0.0198) compared to those with irregular morphology. Among patients treated with contact aspiration (CA), the regular thrombus morphology showed a higher first-pass success rate (45.7% vs. 12.8%; p = 0.0017), a shorter procedural duration (46 vs. 50 min; p = 0.0159), and fewer retrieval attempts (1 vs. 2; p = 0.0338) compared to stent retriever (SR) thrombectomy. Both the regular thrombus morphology (OR 7.72, 95% CI 2.02–29.52; p = 0.003) and using CA as the first-line treatment (OR 3.37, 95% CI 1.12–10.13; p = 0.031) independently predicted first-pass success.
Conclusion: For BAO patients treated with CA as the primary strategy, the presence of a regular thrombus surface might predict higher first-pass success and shorter procedural duration. A diligent assessment of thrombus morphology within the MT workflow could improve the feasibility of procedural techniques.
Introduction
Treatment outcomes for patients with basilar artery occlusion (BAO) have been less than optimal, despite recent advancements in mechanical thrombectomy (MT) techniques (1–3). When compared to anterior circulation cases, some BAO patients continue to exhibit poorer clinical results (4). This discrepancy may be attributed to distinct anatomical variations in the posterior circulation, including vessel caliber, vessel tortuosity, perforators, and collateral patterns (5, 6). Additionally, intracranial atherosclerotic stenosis (ICAS) is a more frequent cause of posterior circulation artery occlusion compared to the anterior circulation (6). Nevertheless, achieving timely and successful recanalization remains crucial for optimal outcomes in BAO patients (7, 8).
Recent attention has focused on predictive radiological features, such as the meniscus sign, cut-off sign, and tapered sign, which may enhance the likelihood of rapid and successful recanalization (9). Prior research has suggested that when the initial digital subtraction angiography (DSA) reveals a regular thrombus surface in anterior circulation large vessel occlusion (LVO), it is associated with higher recanalization rates, particularly when using contact aspiration (CA) as the first-line thrombectomy device (9–13). However, it remains uncertain whether the impact of this thrombus surface characteristic also applies to BAO patients undergoing MT. Therefore, our study aims to validate these findings by assessing the influence of a regular thrombus surface on the success rate and the selection of the first-line device in BAO patients treated with MT.
Methods
Patient and study design
The data were obtained from the prospective registry of our stroke database. All consecutive patients with BAO treated with MT between January 2018 and June 2022 were enrolled if they met the following inclusion criteria: (1) acute symptomatic patients with BAO identified on computed tomographic (CT) or magnetic resonance (MR) angiography; (2) patients with a pre-stroke modified Rankin Scale (mRS) 0–2 (14); (3) patients treated with stent retriever or contact aspiration as the primary treatment; and (4) time from onset of symptoms to groin puncture of ≤12 h. They were excluded if the following was true: (1) SR or CA was not the first-line thrombectomy strategy; (2) the target vascular occlusion could not be reached with thrombectomy devices; (3) LVO was caused by arterial dissection, vasculitis, or moyamoya disease; and (4) angiography images were of poor quality. The patient selection process is shown in Figure 1.
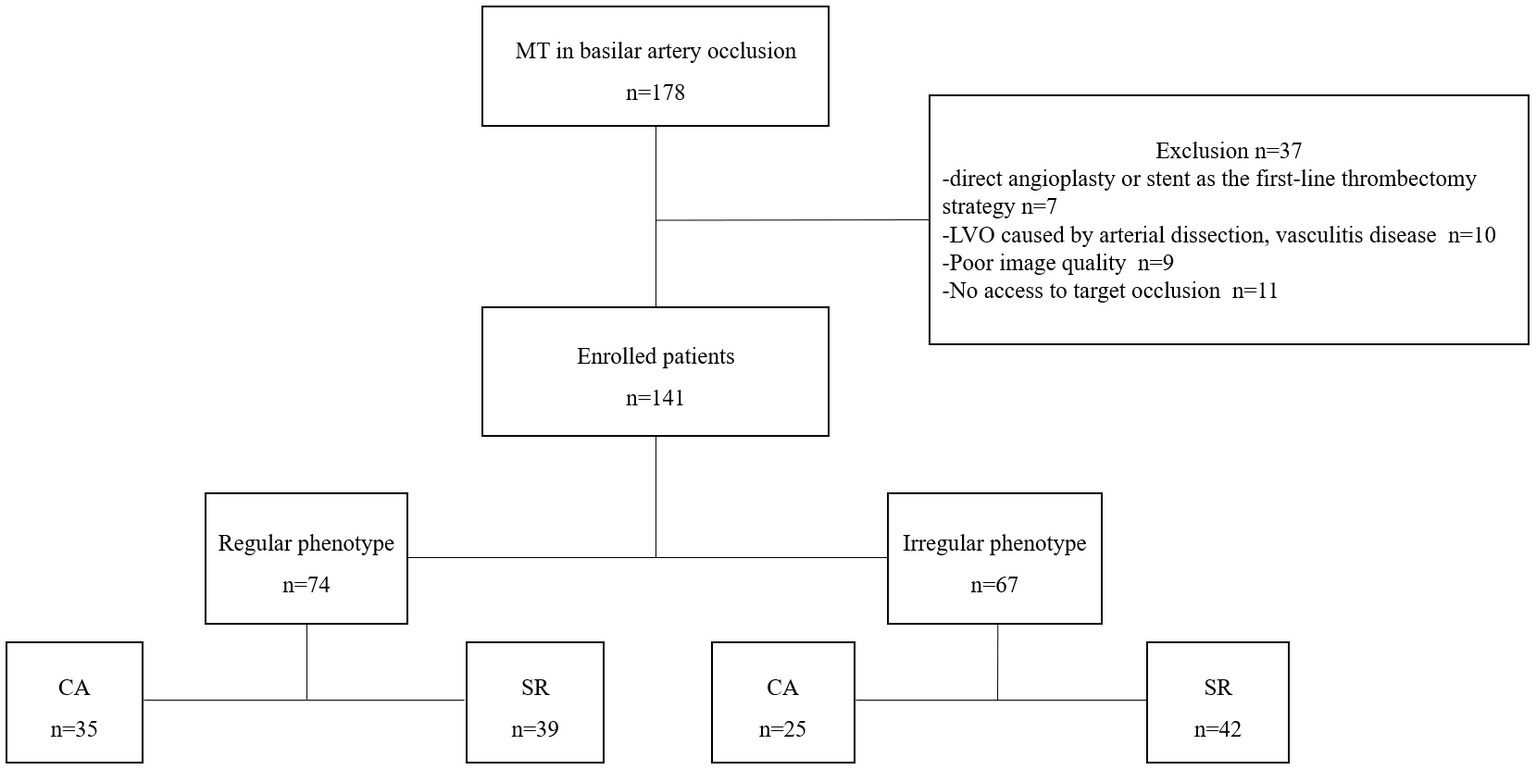
Figure 1. Flow chart of patient selection. MT, mechanical thrombectomy; LVO, large vessel occlusion; CA, contact aspiration; SR, stent retriever.
The following data were also collected: patient’s demographics, comorbidities, vascular risk factors, symptom onset, and severity of stroke: National Institutes of Health Stroke Scale (NIHSS) and Posterior Circulation Alberta Stroke Program Early CT Score (PC-ASPECTS), treatment with intravenous thrombolysis (IVT), the degree of collateral circulation(good or poor) (15), endovascular devices, total attempts, times, and recanalization results [modified treatment in cerebral ischemia (mTICI), clinical outcomes such as mRS after 90 days, and symptomatic intracerebral hemorrhage (ICH)]. This retrospective study was approved by the local ethics committee of Zhejiang Provincial People’s Hospital. (NO.KY2017019). The need for written informed consent was waived given the retrospective nature of this study.
Assessment of thrombus surface phenotype
The thrombus surface phenotype of the target vessel occlusion was classified as “regular” if the profile of the occlusion was smooth and straight with a linear interruption of flow in the artery that appeared to be abruptly cut off; an irregular pattern was classified as any type of obvious change in the linearity of the occlusion, such as concave or convex shapes or the presence of multiple contrast filling defects on the profile of the occlusion (Figure 2). Two experienced neuroradiologists (W.P, D.Y.) with >10 years’ experience in cerebrovascular imaging evaluated the thrombus surface phenotypes. During imaging analysis, the reviewers were blinded to the device usage, angiographic data, and clinical outcome. Any controversy was resolved by the consensus of two reviewers.
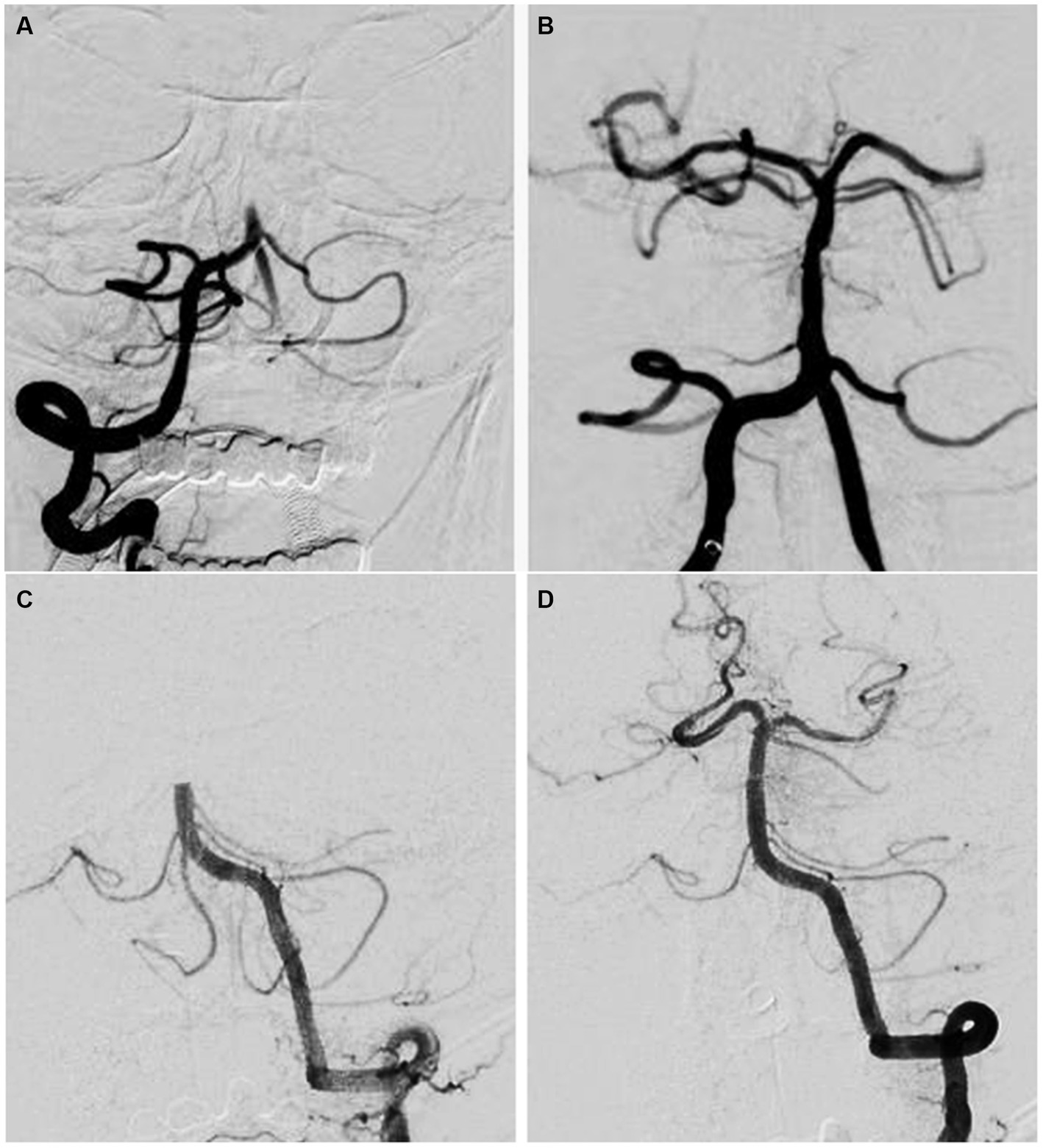
Figure 2. Pre-treatment digital subtraction angiography images of basilar artery occlusion with different thrombus surface phenotypes of the occlusion site. (A,B) Pre-treatment digital subtraction angiogram shows the irregular phenotype of an occlusion at the proximal segment of the basilar artery. After multiple attempts of mechanical thrombectomy, complete recanalization of the basilar artery with residual stenosis is seen. (C,D) Pre-treatment digital subtraction angiogram shows the regular phenotype of an occlusion at the middle segment of the basilar artery. After a single attempt of contact aspiration, complete recanalization of the basilar artery without residual stenosis is seen.
Outcome measures
Recanalization status was classified according to the modified Thrombolysis in Cerebral Infarction (TICI) scale. The angiographic outcomes of the present study included the first pass effect (FPE), successful recanalization (mTICI 2b-3) after procedure, number of passes, rescues treatment, and procedure time. The first pass effect was defined as achieving complete recanalization (mTICI 3) with a single thrombectomy device and without any rescue treatment (16, 17). The procedure time was defined as the time from puncture to final recanalization in those with successful recanalization or time of the last angiographic series in those with unsuccessful recanalization (18). Clinical outcomes were measured with mRS after 90 days and post-procedure ICH. Favorable clinical outcome was defined as a 90-day mRS score of 0–2.
Statistical analysis
The baseline characteristics, angiographic outcome, clinical outcomes, and complications were compared hierarchically based on ‘regular’ or ‘irregular’ thrombus surface phenotype. The results were reported as frequency, mean ± standard deviation (SD), or median (interquartile range, IQR). The overall sample used Pearson’s χ2-test or Fisher’s exact test for categorical variables. In contrast, the Student’s t-test or Mann–Whitney U test (for non-Gaussian distributions) is used for continuous variables comparison. Univariate and Multivariable logistic regression were performed to evaluate the independent variables of first-pass effect. The inter-rater reliability of occlusion type rating was calculated using Cohen’s kappa coefficient (k) with its 95% confidence interval (CI). Kappa values of 0–0.2 indicate slight, 0.21–0.4 fair, 0.41–0.6 moderate, 0.61–0.8 substantial, and 0.81–1.00 almost perfect agreement, respectively17. A p < 0.05 was considered statistically significant. SPSS Statistics (Version 25) and R software (version 3.5.3) were used for all statistical analyses.
Results
During the study period, 178 consecutive patients underwent MT due to BAO. Among them, 37 patients were excluded due to the following reasons: direct angioplasty or stent as the first-line treatment (n = 7), occluded BA due to dissection or vasculitis (n = 10), poor image quality (n = 9), and no access to target occlusion (n = 11). Finally, 141 patients were included in the present study. Baseline characteristics including comorbidities and vascular risk factors are shown in Table 1. The median age was 65 (IQR 37–87), and 68.8% (97/141) were male. The baseline NIHSS and ASPECT on admission were 15 (IQR 8–27) and 8 (IQR 7–9), respectively. IVT was administered to 61 patients (43.3%) before EVT. The average time from symptom onset to groin puncture was 290 ± 74 min. A regular thrombus surface was diagnosed in 52.5% (74/141). For the regular or irregular thrombus surface, we found an excellent inter-reader and intra-reader agreement (κ values, 0.87, 95% CI 0.74 to 1.0, and 0.92, 95% CI 0.87 to 0.95, respectively). The baseline characteristics between regular and irregular groups did not differ significantly.

Table 1. Comparison of baseline characteristics, treatment, and outcomes of basilar artery occlusion patients according to regular/irregular phenotype.
Of all patients, 17.0% (n = 24/141) presented with the first pass effect. Patients with regular thrombus surface had a higher rate of first pass effect compared to those with irregular thrombus surface (28.4% vs. 4.5%; p = 0.0002). There were no significant differences in this cohort with either regular or irregular thrombus surface morphology in their rate of successful recanalization (mTICI 2b-3) after the procedure (93.2% vs. 85.1%; p = 0.1162), the procedure time (48 vs. 49 min; p = 0.2361), and number of rescue treatment (18.9% vs. 25.4%; p = 0.3554). The mean procedure time was 48 ± 7 min, and the median number of passes was 2 (IQR 1–4). Patients with a regular thrombus surface had a significantly lower median number of passe than irregular thrombus surface [2 (IQR 1–3) vs. 2 (IQR 1–4), p = 0.0198]. Rescue treatment was reported in 21.9% (n = 31) of all patients (Table 1).
In the group with regular thrombus surface, patients treated with CA had a higher rate of FPE (45.7% vs. 12.8%, p = 0.0017), lower number of passes (1 vs. 2, p = 0.0388) and shorter procedure time (46 vs. 50, p = 0.0159). In the group with irregular thrombus surface, patients treated with SR had a lower rate of rescue treatment (16.7% vs. 40.0%; p = 0.0338). However, there was no significant difference in successful recanalization, favorable clinical outcome (90-day mRS 6), symptomatic ICH after the procedure, and occlusion site between the CA and SR groups in patients with a regular/irregular thrombus surface (Table 2).

Table 2. Treatment and clinical outcomes of the CA and SR groups according to regular/irregular phenotype.
Multivariate logistic regression analysis showed that the regular thrombus surface (OR 7.72, 95% CI 2.02–29.52; p = 0.003) and the first-line CA thrombectomy (OR 3.37, 95% CI 1.12–10.13; p = 0.031) were independent predictors of PFE when adjusting for sex (male), atrial fibrillation, and procedure time (Table 3).
Discussion
This study underscores the significant impact of angiographic thrombus surface morphology on the treatment outcomes of acute BAO patients undergoing MT. The presence of a regular thrombus surface is closely associated with several positive treatment outcomes, including a higher first-pass success rate, a reduced total number of passes, and shorter procedure times. BAO patients with regular thrombus surfaces, particularly those treated with CA as the primary thrombectomy method, demonstrate superior first-pass success rates, shorter procedural durations, and fewer passes compared to those treated with stent retriever SR thrombectomy. It is important to note that the regular thrombus surface and the choice of CA as the first-line thrombectomy are independent predictors of first-pass success in BAO cases.
In our study, we defined a regular thrombus surface as one exhibiting a smooth and straight profile with a linear interruption of flow, giving the appearance of an abrupt cutoff in the artery. This definition aligns with similar classification methods described in previous studies. For instance, the clot meniscus sign can be considered a subset of the regular thrombus surface. Furthermore, a more detailed subtyping of thrombus phenotypes, such as the meniscus sign, may inadvertently exclude patients who could benefit from a phenotype-based device selection. Therefore, our regular/irregular thrombus surface definition is likely more suitable for clinical application.
In the context of anterior circulation large vessel occlusion (LVO), prior studies have explored the morphological analysis of occlusive lesions in relation to MT efficacy (10–13). Two studies have demonstrated higher success rates and complete first-pass recanalization (mTICI 2b-3 and mTICI 3) when employing first-line CA in patients with regular thrombus surfaces (10, 12). In contrast, one study has suggested that irregular M1-MCA occlusive thrombus surfaces treated with SR as the first-line thrombectomy device were associated with higher success rates and complete first-pass recanalization (11).
Regarding complete recanalization, recent research has indicated that, in BAO patients with the clot meniscus sign or a regular thrombus phenotype, first-line CA thrombectomy may be more effective than SR (5). Interestingly, among patients with irregular thrombus surfaces, we observed a significant difference in the rate of rescue treatments between the CA and SR groups, which is consistent with previous findings that noted a higher rate of rescue treatments in CA thrombectomy for M1-MCA occlusions compared to SR (11). However, in patients with irregular thrombus surfaces, we found no differences in recanalization rates, procedural times, or the total number of retrievals attempts between the CA and SR groups.
The existing literature on the association between thrombus surface phenotype and treatment outcomes in BAO patients is limited. Previous studies have indicated that meniscoid-like thrombus surfaces or the claw sign are associated with higher recanalization (18, 19). A recent study suggested that the regular thrombus surface may independently predict complete recanalization with first-line CA in BAO patients (20). However, these studies did not further investigate the impact of thrombus surface phenotypes on recanalization efficacy with different first-line thrombectomy devices (CA or SR). Our study validated the results of the previous study in a relatively larger cohort and further demonstrated the relationship between the success of the first pass using two different recanalization techniques and thrombus surface phenotypes in BAO patients.
Achieving early complete recanalization is a primary goal in BAO and is pivotal for better clinical outcomes (7, 8). In this regard, first-line CA thrombectomy may be associated with higher rates of complete recanalization compared to SR (8). Our findings, including the independent prediction of complete recanalization after the first pass by the regular thrombus surface and first-line CA thrombectomy in BAO patients, align with our initial hypothesis and prior research (20). Nevertheless, our study did not reveal a significant difference in favorable clinical outcomes between patients with regular and irregular thrombus surfaces regardless of the technique employed (CA or SR). This finding is consistent with previous studies that found no significant difference in clinical outcomes based on thrombus surface morphology in BAO patients. (20)The lack of significant differences in clinical outcomes may be attributed to the current sample size, which may not yet balance the multitude of factors influencing clinical outcomes.
The association between recanalization efficacy and the regular/irregular thrombus surfaces of large vessel occlusions remains an area of ongoing exploration. While most studies have reported no significant difference in the rate of complete first-pass recanalization between thrombus surfaces (10, 11), recent literature has highlighted a potential link between the rate of complete first-pass recanalization and angiographic thrombus surfaces of occlusive lesions and found that patients with an anterior circulation LVO from a thrombus of regular surface had a higher rate of complete first-pass recanalization than those with an irregular thrombus surface (46.3% vs. 20.7%; p = 0.0004). Similarly, our study showed that BAO patients with regular thrombus surfaces had a higher rate of complete first-pass recanalization than those with an irregular thrombus surface (28.4% vs. 4.5%; p = 0.0002).
Our results indicate that the use of CA is associated with higher rates of FPE in patients with BAO who exhibit the regular thrombus phenotype. Several potential mechanisms may explain the superiority of CA over stent retriever (SR) thrombectomy in BAO patients with a regular thrombus surface: (1) During CA, a large-bore aspiration/intermediate catheter can occupy a higher percentage of the cross-sectional area of the vessel lumen. This effective vessel lumen occupation may reduce the impact force on the thrombus, resulting in more efficient retrieval and a decreased risk of thrombus distal migration (5, 18). (2) Enhanced “Contact”: Successful recanalization in CA thrombectomy relies on effective “contact” between the aspiration catheter and the proximal surface of the thrombus (21). The regular thrombus surface substantially increases the contact area of the aspiration catheter with the thrombus, potentially improving the catheter’s efficiency and increasing the revascularization rate (3). Erythrocyte-rich thrombus was associated with cardioembolic etiology (22). Our statistics and previous study showed that patients with atrial fibrillation had a higher proportion of regular thrombus surface than irregular thrombus surface. The characteristics of the erythrocyte-rich thrombus had a higher clot burden and higher density (23). The physiological characteristics may be increasing the catheter’s efficiency and decreased risk of thrombus distal migration. However, further studies are needed for revealing the precise association of histological thrombus composition with different surface phenotypes.
Limitations
Our study has several limitations. Firstly, it employs a retrospective design, which warrants a cautious interpretation of the results. Secondly, the choice of the first-line thrombectomy device was determined by the interventionist’s experience, introducing potential bias. Thirdly, our study primarily involved Chinese populations, who exhibit a higher incidence of intracranial atherosclerotic stenosis (ICAS), which may influence the outcomes of endovascular treatment. Lastly, we did not conduct a histologic examination of the retrieved clots, leaving the relationship between thrombus composition and angiographic morphology as a potential avenue for future research.
Conclusion
For BAO patients treated with CA as the primary strategy, the presence of a regular thrombus surface might predict higher first-pass success and shorter procedural duration. Diligent assessment of thrombus morphology within the MT workflow could improve the feasibility of procedural techniques.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the local Ethics Committee of Zhejiang Provincial People’s Hospital. (No. KY2017019). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
XJ: Writing – original draft, Writing – review & editing. SY: Writing – review & editing. DW: Conceptualization, Writing – original draft. YD: Supervision, Writing – review & editing. PW: Funding acquisition, Resources, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Jovin, TG, Li, C, Wu, L, Wu, C, Chen, J, Jiang, C, et al. Trial of Thrombectomy 6 to 24 hours after stroke due to basilar-artery occlusion. N Engl J Med. (2022) 387:1373–84. doi: 10.1056/NEJMoa2207576
2. Tao, C, Nogueira, RG, Zhu, Y, Sun, J, Han, H, Yuan, G, et al. Trial of endovascular treatment of acute basilar-artery occlusion. N Engl J Med. (2022) 387:1361–72. doi: 10.1056/NEJMoa2206317
3. Langezaal, LCM, van der Hoeven, E, Mont’Alverne, FJA, de Carvalho, JJF, Lima, FO, Dippel, DWJ, et al. Endovascular therapy for stroke due to basilar-artery occlusion. N Engl J Med. (2021) 384:1910–20. doi: 10.1056/NEJMoa2030297
4. Writing Group for the BASILAR Group Zi, W, Qiu, Z, Wu, D, Li, F, Liu, W, et al. Assessment of endovascular treatment for acute basilar artery occlusion via a Nationwide prospective registry. JAMA Neurol. (2020) 77:561–73. doi: 10.1001/jamaneurol.2020.0156
5. Baik, SH, Jung, C, Kim, BM, Han, K, and Kim, DJ. Clot Meniscus sign: an angiographic clue for choosing between stent retriever and contact aspiration in acute basilar artery occlusion. AJNR Am J Neuroradiol. (2021) 42:732–7. doi: 10.3174/ajnr.A6988
6. Baik, SH, Park, HJ, Kim, JH, Jang, CK, Kim, BM, and Kim, DJ. Mechanical Thrombectomy in subtypes of basilar artery occlusion: relationship to recanalization rate and clinical outcome. Radiology. (2019) 291:730–7. doi: 10.1148/radiol.2019181924
7. Deb-Chatterji, M, Flottmann, F, Leischner, H, Alegiani, A, Brekenfeld, C, Fiehler, J, et al. Recanalization is the key for better outcome of Thrombectomy in basilar artery occlusion. Clin Neuroradiol. (2020) 30:769–75. doi: 10.1007/s00062-019-00850-9
8. Gory, B, Mazighi, M, Blanc, R, Labreuche, J, Piotin, M, Turjman, F, et al. Mechanical thrombectomy in basilar artery occlusion: influence of reperfusion on clinical outcome and impact of the first-line strategy (ADAPT vs stent retriever). J Neurosurg. (2018) 129:1482–91. doi: 10.3171/2017.7.JNS171043
9. Liang, W, Wang, Y, Du, Z, Mang, J, and Wang, J. Intraprocedural angiographic signs observed during endovascular Thrombectomy in patients with acute ischemic stroke: a systematic review. Neurology. (2021) 96:1080–90. doi: 10.1212/WNL.0000000000012069
10. Consoli, A, Rosi, A, Coskun, O, Nappini, S, di Maria, F, Renieri, L, et al. Thrombectomy for M1-middle cerebral artery occlusion: angiographic Aspect of the arterial occlusion and recanalization: a preliminary observation. Stroke. (2018) 49:1286–9. doi: 10.1161/STROKEAHA.117.018987
11. Consoli, A, Zhu, F, Bourcier, R, Dargazanli, C, Marnat, G, Duhamel, A, et al. Effect of the phenotype of the M1-middle cerebral artery occlusion on the recanalization rates in the ASTER trial. J Neurointerv Surg. (2020) 12:7–12. doi: 10.1136/neurintsurg-2019-015002
12. Kaiser, D, Laske, K, Winzer, R, Hädrich, K, Wahl, H, Krukowski, P, et al. Impact of thrombus surface on first pass reperfusion in contact aspiration and stent retriever thrombectomy. J Neurointerv Surg. (2021) 13:221–5. doi: 10.1136/neurintsurg-2020-016194
13. Mönch, S, Boeckh-Behrens, T, Berndt, M, Maegerlein, C, Wunderlich, S, Zimmer, C, et al. Angiographic baseline proximal Thrombus appearance of M1/M2 occlusions in mechanical Thrombectomy. Clin Neuroradiol. (2021) 31:189–96. doi: 10.1007/s00062-019-00863-4
14. Huo, X, Ma, G, Tong, X, Zhang, X, Pan, Y, Nguyen, TN, et al. Trial of endovascular therapy for acute ischemic stroke with large infarct. N Engl J Med. (2023) 388:1272–83. doi: 10.1056/NEJMoa2213379
15. Goyal, N, Tsivgoulis, G, Nickele, C, Doss, VT, Hoit, D, Alexandrov, AV, et al. Posterior circulation CT angiography collaterals predict outcome of endovascular acute ischemic stroke therapy for basilar artery occlusion. J Neurointerv Surg. (2016) 8:783–6. doi: 10.1136/neurintsurg-2015-011883
16. Abdullayev, N, Maus, V, Behme, D, Barnikol, UB, Kutschke, S, Stockero, A, et al. True first-pass effect in basilar artery occlusions: first-pass complete reperfusion improves clinical outcome in stroke thrombectomy patients. J Clin Neurosci. (2021) 89:33–8. doi: 10.1016/j.jocn.2021.04.020
17. Huang, X, Chen, C, Li, M, Duan, Z, Ji, Y, Wu, K, et al. First-pass effect in patients with acute vertebrobasilar artery occlusion undergoing thrombectomy: insights from the PERSIST registry. Ther Adv Neurol Disord. (2022) 15:175628642211395. doi: 10.1177/17562864221139595
18. Baik, SH, Kim, JW, Kim, BM, and Kim, DJ. Significance of angiographic clot meniscus sign in mechanical thrombectomy of basilar artery stroke. J Neurointerv Surg. (2020) 12:477–82. doi: 10.1136/neurintsurg-2019-015321
19. Yamamoto, Y, Yamamoto, N, Kanematsu, Y, Korai, M, Shimada, K, Izumi, Y, et al. The claw sign: an angiographic predictor of recanalization after mechanical Thrombectomy for cerebral large vessel occlusion. J Stroke Cerebrovasc Dis. (2019) 28:1555–60. doi: 10.1016/j.jstrokecerebrovasdis.2019.03.007
20. Kaiser, D, Krukowski, P, Hädrich, K, Winzer, R, Pallesen, LP, Gawlitza, M, et al. Association of Regular Thrombus Surface Phenotype with Complete Recanalization in first-line contact aspiration Thrombectomy for basilar artery occlusion. Front Neurol. (2021) 12:666933. doi: 10.3389/fneur.2021.666933
21. Kang, DH, and Hwang, YH. Frontline contact aspiration treatment for emergent large vessel occlusion: a review focused on practical techniques. J Stroke. (2019) 21:10–22. doi: 10.5853/jos.2018.03076
22. Cho, KH, Kim, JS, Kwon, SU, Cho, AH, and Kang, DW. Significance of susceptibility vessel sign on T2*-weighted gradient echo imaging for identification of stroke subtypes. Stroke. (2005) 36:2379–83. doi: 10.1161/01.STR.0000185932.73486.7a
Keywords: thrombus morphology, basilar artery occlusion, mechanical thrombectomy, acute stroke, contact aspiration, stent retriever
Citation: Jiang X, Yu S, Wang D, Dong Y and Wang P (2023) The impact of thrombus surface morphology of the basilar artery on the successful rate of mechanical thrombectomy. Front. Neurol. 14:1280317. doi: 10.3389/fneur.2023.1280317
Edited by:
Markus Holtmannspötter, Klinikum Nürnberg, GermanyReviewed by:
Pengfei Wang, Weihai Municipal Hospital, ChinaWang Jiaxiong, South YunNan Central Hospital of YunNan Provience, China
Luis Rafael Moscote-Salazar, Colombian Clinical Research Group in Neurocritical Care, Colombia
Copyright © 2023 Jiang, Yu, Wang, Dong and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: YI Dong, ZHJkb25neWlAeWVhaC5uZXQ=; Peng Wang, MTk3OXd3d3dAMTYzLmNvbQ==
†These authors have contributed equally to this work
 Xinzhao Jiang
Xinzhao Jiang Shufeng Yu2
Shufeng Yu2 YI Dong
YI Dong