- 1Department of Neurology, Tianjin Huanhu Hospital, Tianjin, China
- 2Key Laboratory of Cerebral Vascular and Neurodegenerative Diseases, Tianjin Neurosurgical Institute, Tianjin, China
- 3Clinical College of Neurology, Neurosurgery and Neurorehabilitation, Tianjin Medical University, Tianjin, China
- 4Department of Neurosurgery, Tianjin Huanhu Hospital, Tianjin, China
- 5Department of Neurosurgery, The Second Hospital of Tianjin Medical University, Tianjin, China
- 6Department of Neurosurgery (Cerebrovascular Disease), The Third Hospital of Hebei Medical University, Shijiazhuang, China
- 7Department of Academy of Medical Engineering and Translational Medicine, Tianjin University, Tianjin, China
Background: The retrograde semi-retrieval technique (RESET) has been described as a modified technique for endovascular thrombectomy (EVT) whose safety and efficacy for intracranial atherosclerosis stenosis (ICAS) patients remain uncertain. This article presents our single-center experience, comparing RESET vs. non-RESET in ICAS patients.
Materials and methods: We analyzed 327 consecutive ICAS patients who underwent EVT at Tianjin Huanhu Hospital from January 2018 and December 2022. Patients were categorized into two groups: RESET and non-RESET. The primary outcome was the first-pass effect (FPE). Secondary outcomes included successful reperfusion, functional independence at 90 days, mortality, and symptomatic intracranial hemorrhage (sICH).
Results: RESET was significantly associated with FPE [adjusted odds ratio (aOR) 2.00, 95% confidence interval (CI) 1.03–3.87, p = 0.040]. RESET was not significantly associated with successful reperfusion (aOR 1.5, CI 0.55–4.06, p = 0.425), an mRS of 0–2 at 90 days (aOR 1.36, CI 0.83–2.21, p = 0.223), sICH (aOR 0.39, CI 0.12–1.23, p = 0.108), and mortality (aOR 0.49, CI 0.16–1.44, p = 0.193). After propensity score matching, the results were consistent with the primary analysis.
Conclusion: Compared to non-RESET, patients treated with RESET showed increased FPE incidence and significantly decreased puncture-to-reperfusion time. RESET was proven to be safe and effective in enhancing reperfusion for LVO patients receiving EVT with underlying ICAS.
1 Introduction
In recent years, numerous randomized controlled trials (RCTs) have provided Class I evidence for the safety and efficacy of endovascular treatment (EVT) in acute ischemic stroke (AIS) caused by large vessel occlusion (LVO) (1). Rapid, complete recanalization of these occluded vessels is critical in acute stroke settings, leading to beneficial clinical outcomes especially when successful recanalization is attained in a single or few thrombectomy attempts (2, 3). Since their inception, EVT devices have significantly advanced. Increasing evidence suggests the effectiveness and safety of stent-retrievers, used in combination with other devices, for managing AIS using various techniques (4–12).
Distal intracranial catheters (DICs) are widely utilized for continuous clot aspiration, owing to their exceptional efficacy in attaining high recanalization rates and reducing incidences of thrombi dislodgement (13). Previous studies have predominantly concentrated on advancing the DIC's distal end to the carotid siphon level to achieve thrombus proximity. Nevertheless, the optimal and accurate positioning of DICs prior to EVT has not been the focus of these studies. Previous thrombectomy techniques have been associated with thrombus fragmentation (4, 5) likely due to the substantial distance between the clot's proximal section and the DIC's distal end, through which the stent retriever navigates. Positioning the DIC nearer to the thrombus and concurrently performing stent retrieval and aspiration could offer benefits. Modified techniques such as stent retriever-assisted vacuum-locked extraction (SAVE) and stent-retrieving into an aspiration catheter with proximal balloon (ASAP) technique (6, 12) have been utilized for complete and rapid recanalization. However, these techniques need to be considered and applied in the context of intracranial atherosclerotic stenosis (ICAS), which demonstrates a prevalence of 46.6% in the Asian population (14) and has emerged as a predominant cause of AIS. Additionally, ICAS lesions exhibit a propensity for reocclusion (14), and no prior techniques have been specifically adapted for patients with underlying ICAS. As a result, we developed a modified retrieval method involving complete unfolding of the stent retriever, followed by advancing the DIC or microcatheter to partially re-sheath the stent retriever, creating a tapered configuration. This technique shortens the travel distance for the thrombi-embedded stent retriever and embeds the thrombi more tightly within the strut, preventing clot escape. Herein, we present our experience employing the retrograde semi-retrieval technique (RESET) for EVT in ICAS patients compared to those treated without RESET.
2 Materials and methods
2.1 Study population
We conducted a retrospective analysis of consecutive patients admitted to Tianjin Huanhu Hospital from January 2018 to December 2022, who underwent EVT with underlying ICAS. All patient data were extracted from the triage of patients with acute ischemic stroke due to large vessel occlusions (TRACK-LVO) registry. A certified neurologist evaluated the National Institute of Health Stroke Scale (NIHSS), modified Rankin scale (mRS), and Alberta Stroke Program Early Computed Tomography (ASPECT) scores during the hospitalization. The diagnosis of ischemic stroke was confirmed using non-contrast computed tomography (NCCT) or magnetic resonance imaging (MRI). The inclusion criteria were as follows: ICAS patients with LVO in the anterior circulation; patients presenting within 24 h from the last known well (LKW) time; patients with a baseline NIHSS score ≥ 6; and patients aged 18 years and above. Patients matching the following criteria were excluded: detection of any form of intracranial hemorrhage on CT or MRI; presence of tandem lesions; and loss to follow-up. Patients were categorized into two groups—those treated with RESET and those without—based on the treating physicians' discretion.
2.2 Study data
We examined the following variables: (1) preoperative characteristics such as age, gender, occlusion site, CT/diffusion-weighted imaging (DWI) ASPECT score, NIHSS score, onset-to-door time, onset-to-puncture time, and cardiovascular risk factors; (2) procedure-specific attributes including puncture-to-reperfusion time, number of thrombectomy pass, rescue therapy used in EVT (for example, angioplasty, stenting, intra-arterial thrombolysis, intra-arterial IIb/IIIa inhibitor or some combination), and modified thrombolysis in the cerebral infarction (mTICI) score. Patients with truncal-type occlusions were classified as having underlying ICAS. The diagnosis of truncal-type occlusion was primarily based on evaluations using computed tomography angiography (CTA). If the bifurcation site was distinctly visible on the CTA, it was categorized as truncal-type occlusion. The occlusion type was further confirmed with DSA during EVT. In instances where digital subtraction angiography (DSA) revealed all major branches and their bifurcation site to be clearly observable beyond the occlusion site, the LVO was classified as truncal-type occlusion. Distal confirmation could be achieved either through the collateral flow of the anterior communicating artery, observed on the contralateral internal cerebral artery angiogram or subsequent to minimal recanalization of the occlusion site post the placement of the stent retriever across the site of occlusion (15, 16). The level of intracranial arterial stenosis was determined using the Warfarin–Aspirin Symptomatic Intracranial Disease criteria (17).
2.3 Study outcomes
The primary outcome was the first pass effect (FPE), which is defined as the successful removal of a thrombus in a single thrombectomy device pass, which leads to near-complete or complete revascularization. Secondary outcomes included successful reperfusion (mTICI score ≥ 2b at the end of the procedure), functional independence at 90 days follow-up [modified Rankin Scale (mRS) 0–2], all-cause mortality, and symptomatic intracerebral hemorrhage (sICH). The mRS score was assessed by a stroke neurologist during a 3-month follow-up visit or, in the event a clinical visit was impossible, via a telephone interview. sICH was classified according to the European Collaborative Acute Stroke Study (ECASS) II criteria, defined as any intracranial hemorrhage with an increase in the NIHSS score of ≥4 within 24 h or resultant death (18).
2.4 Endovascular intervention protocol
Endovascular treatment procedures were executed by two interventional neuroradiologists, each with over 5 years of neurovascular intervention experience. Written informed consent was procured from the patient's family members prior to the initiation of the procedure.
Upon placement of the guiding and intermediate catheters in the cervical segment of the internal carotid artery, the microguidewire was used to traverse the occlusion site, and the microcatheter, under the guidance of the microguidewire, reached the distal end of the occluded vessel for intraluminal angiography. This procedure confirmed the presence of the microcatheter in the true lumen of the distal occlusion vessel, enabling the deployment of the thrombectomy stent. Subsequent angiography was performed to identify the site of occlusion, the thrombus burden, and the potential stroke etiology.
If the presence of ICAS was confirmed, a semi-retrieval stent technique was employed. The stent retriever was initially semi-deployed by advancing the DIC. Nonetheless, in certain scenarios, significant stenosis might impede the re-sheathing of the stent retriever by the DIC. In cases of significant resistance encountered while advancing the DIC due to underlying ICAS, a microcatheter was used to re-sheath the stent. Subsequently, the DIC was held in place, and the stent was withdrawn under negative pressure. The DIC was retained in a distal position to facilitate potential rescue therapy.
If the distal thrombus could not be removed due to vascular stenosis, a balloon, guided by a microwire, was used to dilate the stenotic region before next thrombectomy. To prevent downstream thrombus displacement following post-dilation stenosis relief, the DIC maintained continuous negative pressure. After thrombectomy, if residual severe stenosis (≥70%), a mTICI score of <2b or a tendency for re-occlusion were observed, rescue measures such as balloon angioplasty, the preferred option, or stent implantation as an alternative under specific conditions (such as blood vessel dissection or elastic recoiling of the ICAS lesion), were undertaken.
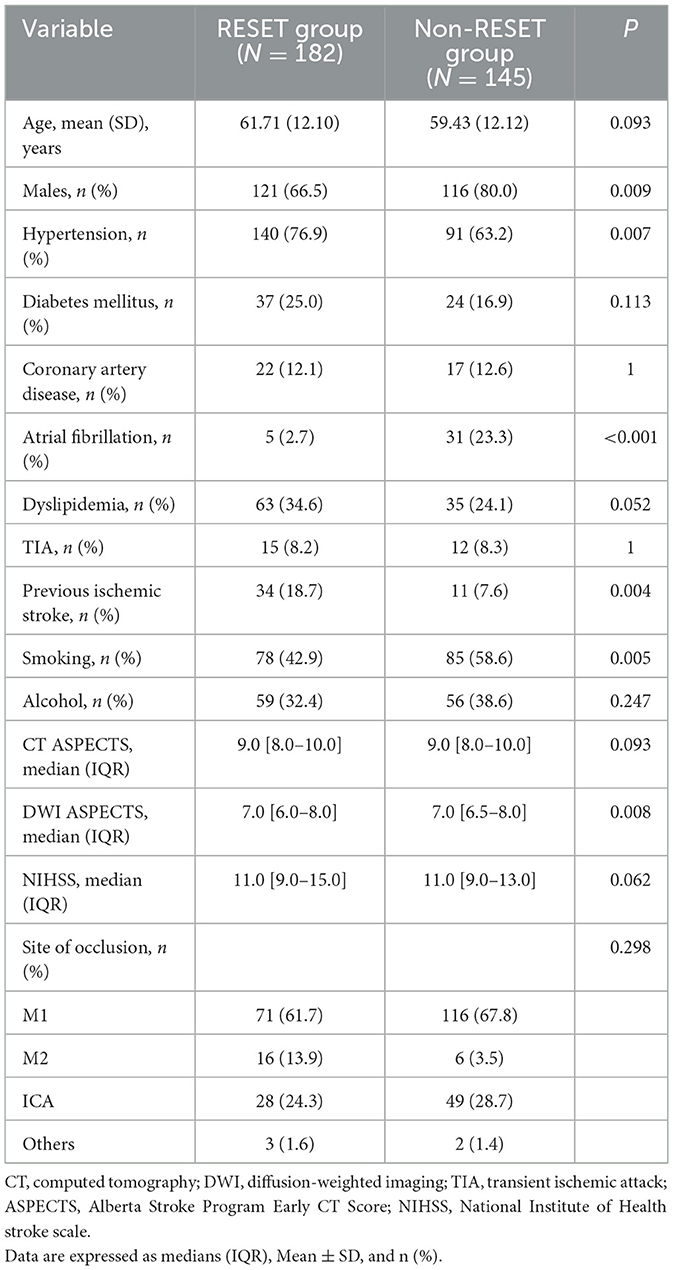
Following each rescue therapy, manual aspiration via the DIC was applied for 30 s under negative pressure. If preoperative chronic stenosis, intraoperative endothelial injury, or in-situ thrombosis leading to vascular re-occlusion were detected, intraoperative administration of tirofiban was performed. A comprehensive overview of the aforementioned technique is shown in Figures 1, 2.
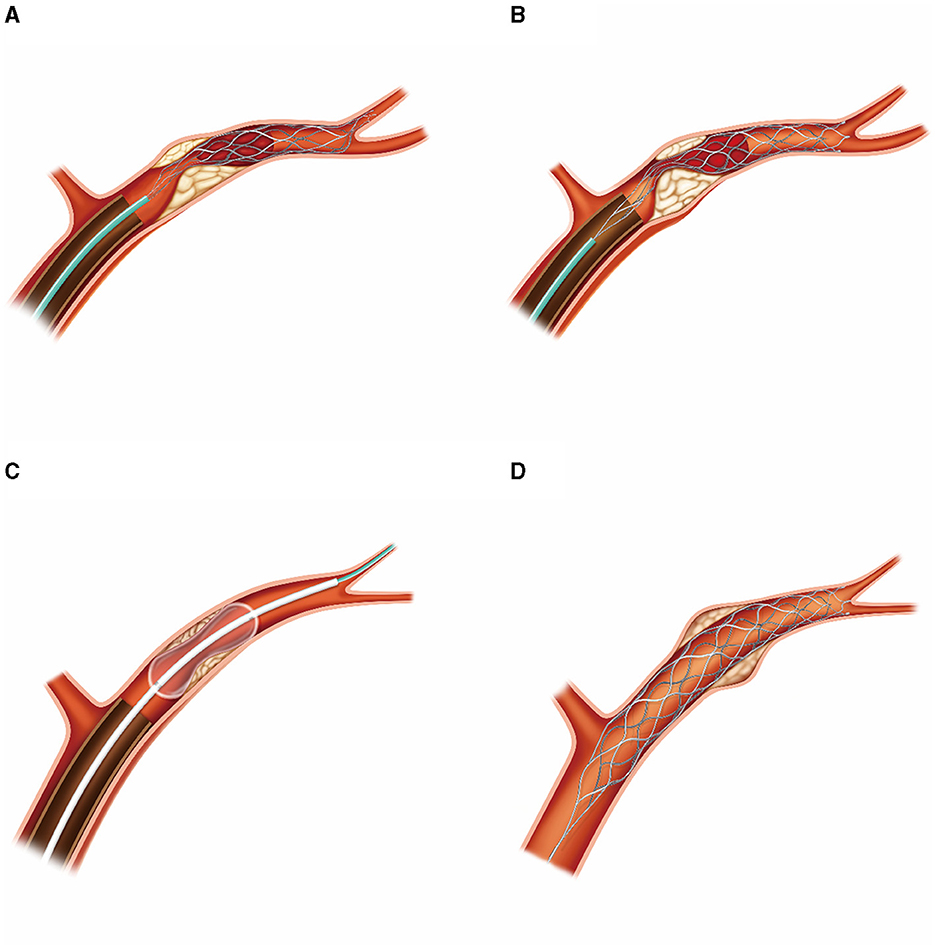
Figure 1. Hand-drawn illustration of the retrograde semi-retrieval technique in patients with ICAS. (A) Stent-retriever was fully deployed across the thrombus, with the DIC advanced until its tip was over the ACA's orifice. (B) Microcatheter was maintained in position to re-sheath the stent retriever in case of failure of re-sheath process by DIC. The DIC was advanced to attain proximity to the thrombus and held in place to generate maximum negative pressure during stent retriever withdrawal. (C) Rescue therapy, such as stent-retriever implantation or balloon dilation, was carried out on residual stenosis as required through the DIC. (D) In cases where compromised blood flow persisted, or vascular dissection occurred post-balloon dilation, a Solitaire stent was implanted. ACA, anterior cerebral artery.
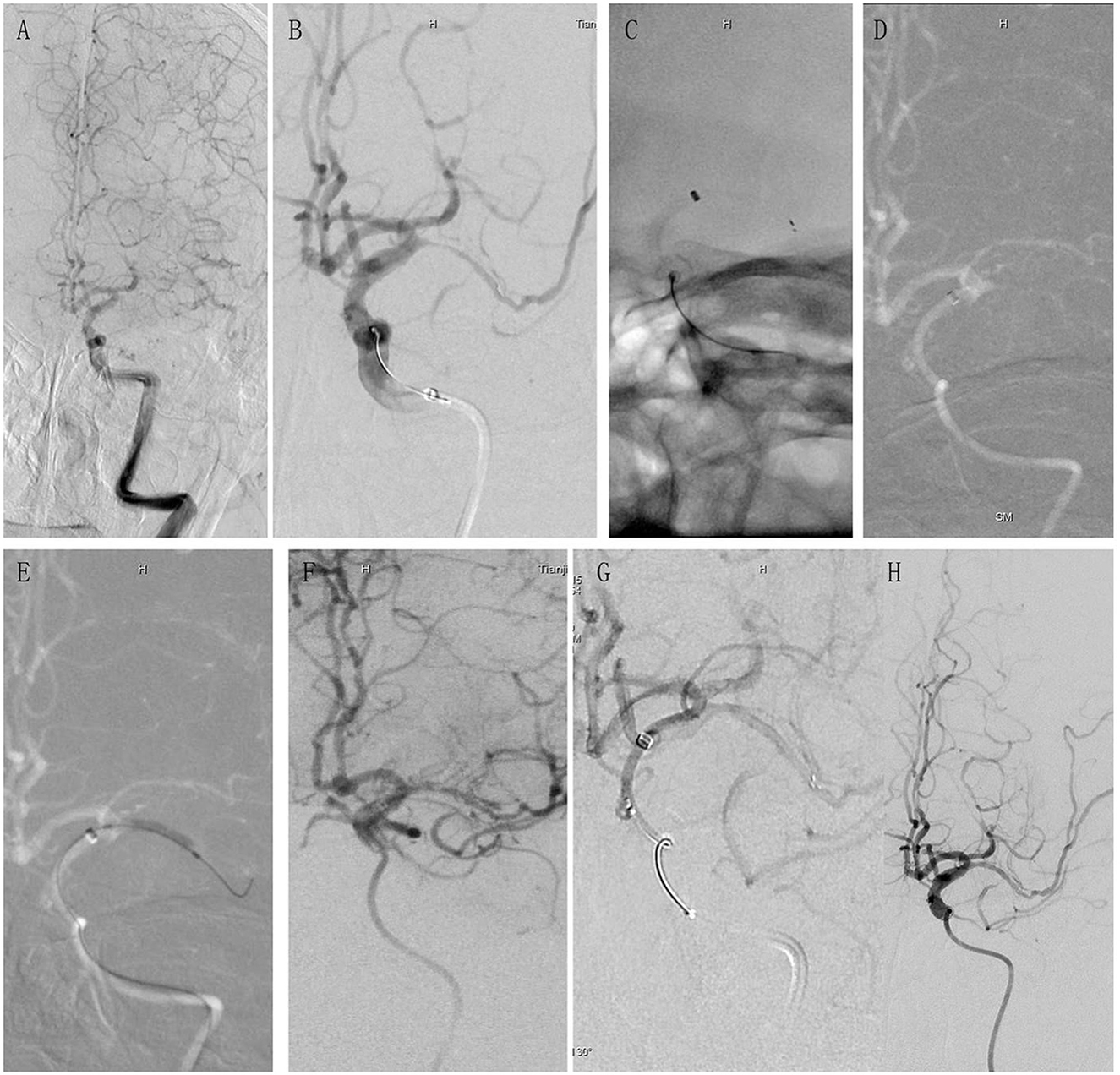
Figure 2. A case presentation showcasing the application of the retrograde semi-retrieval technique in a real-world clinical setting for a patient with ICAS. A 67-year-old male with a medical history of hypertension and diabetes, and no indication of atrial fibrillation, presented to the emergency room with sudden right limb numbness and hemiplegia, which had started 10 h before admission. His NIHSS score upon admission was 9, clinically suggestive of AIS due to LVO with underlying ICAS. (A) Preoperative angiography revealed occlusion in the left MCA. The bilateral tissue regions supplied by the ACA were sustained by one dominant ACA, and the ICA was tortuous. (B) DIC was advanced to the petrous portion of the ICA and a Solitaire FR stent was deployed. Severe stenosis observed in the MCA on angiography further substantiated the ICAS diagnosis. (C) DIC was advanced beyond the ophthalmic artery (OA) origin, up to the C7 segment of the ICA. However, it was unable to progress further into the MCA. The stent was semi-retrieved using the microcatheter, following which the microcatheter and Solitaire FR stent were withdrawn as a single unit. (D) Angiography postretrieval of the Solitaire FR demonstrated unrecanalized MCA. (E) Rescue balloon angioplasty was initiated via the unwithdrawn DIC. (F) Although the MCA recanalized following angioplasty, potential indicators of vascular dissection were discerned. (G) The Solitaire FR stent was redeployed, and subsequent angiography revealed no signs of dissection. (H) The removal of the Solitaire FR stent resulted in good vascular patency, as per the angiography. NIHSS, National Institute of Health Stroke Scale; AIS, acute ischemic stroke; LVO, large vessel occlusion; ICAS, intracranial atherosclerotic stenosis; ACA, anterior cerebral artery; MCA, middle cerebral artery; ICA, internal carotid artery.
2.5 Statistical analysis
The comparative analysis involved the baseline characteristics and clinical outcomes between the two groups. Appropriate statistical tests were utilized to analyze the data: categorical and binary variables were examined using the chi-square test or Fisher's exact test as necessary, while continuous variables were analyzed with the Mann–Whitney U-test. Continuous variables are represented as mean ± SD for a normal distribution and as a median with IQR for a skewed distribution. Percentages along with their corresponding 95% CIs were used to present categorical variables. Statistical comparisons of baseline characteristics and study outcomes were performed for patients treated with and without RESET. Multivariable regression analysis was subsequently performed, with adjustments made for clinically relevant variables: age, gender, baseline stroke severity (as per the NIHSS), clot location, and presentation time from LKW. Sensitivity analysis was conducted through propensity score matching (PSM), for which the propensity score was computed based on logistic regression models while controlling for the aforementioned covariates. R software (version 4.3.2 for Windows) was employed for all statistical analyses. A p-value of <0.05 was considered as statistically significant.
3 Results
3.1 Baseline characteristics of study population
Our study period analysis involved a total of 2,812 AIS patients registered in the TRACK-LVO registry. Among these, we included 327 patients with underlying ICAS (182 treated with the RESET technique and 145 with non-RESET) meeting the requisite inclusion and exclusion criteria for the final analysis (see Figure 3).
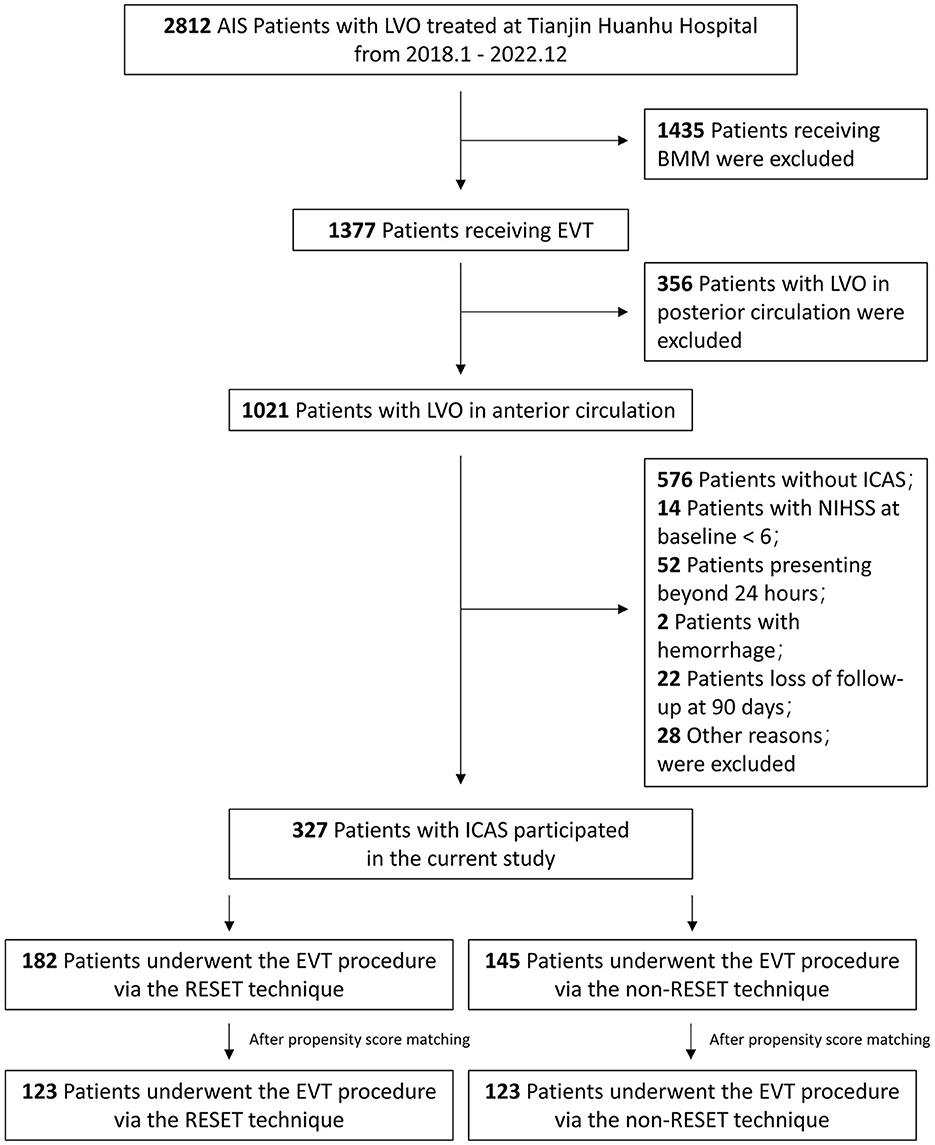
Figure 3. Study flow chart. AIS, acute ischemic stroke; BMM, best medical management; EVT, endovascular thrombectomy; ICAS, intracranial atherosclerotic stenosis; LVO, large vessel occlusion; NIHSS, National Institute of Health stroke scale; RESET, Retrograde Semi-Retrieval Technique.
When compared to patients treated with EVT using the non-RESET method, those treated with EVT using the RESET technique displayed a lower likelihood of being male (66.5% in RESET vs. 80.0% in non-RESET, p = 0.009), and a trend toward older age (mean age 61.71 ± 12.10 years vs. 59.43 ± 12.12 years, p = 0.093) and a higher baseline stroke severity as measured by NIHSS [median score 11.0 (9.0–15.0) vs. 11.0 (9.0–13.0), p = 0.062]. The baseline CT ASPECTS [median score 9.0 (8.0–10.0) in both groups, p = 0.093] was not significantly different between the two groups. However, the DWI-ASPECTS score was significantly lower in the non-RESET group compared to the RESET group [median 7.0 (6.0–8.0) vs. 7.0 (6.5–8.0), p = 0.008]. No significant differences were noted in the remaining clinically relevant baseline characteristics.
In terms of cardiovascular risk factors, RESET-treated patients were more likely to have hypertension (76.9% in RESET vs. 63.2% in non-RESET, p = 0.007) and previous ischemic stroke events (18.7% in RESET vs. 7.6% in non-RESET, p = 0.004), but a significantly reduced incidence of atrial fibrillation (2.7% in RESET vs. 23.3% in non-RESET, p < 0.001). Table 1 summarizes baseline information of the two groups.
3.2 Primary outcome of study population
FPE occurred in 38 (20.9%) patients in the RESET group as compared to 17 (11.7%) patients in the non-RESET group (p = 0.037). After adjustment, RESET was significantly associated with FPE [adjusted odds ratio (aOR) 2.00, 95% confidence interval (CI) 1.03–3.87, p = 0.040] (see Table 2).
3.3 Secondary outcomes of study population
In the RESET cohort, successful reperfusion was achieved in 173 patients (95.1%) compared to 135 patients (93.1%) in the non-RESET cohort (p = 0.483). At the 3-month follow-up, an mRS of 0–2 was observed in 102 patients (56.0%) in the RESET group and in 76 patients (52.4%) in the non-RESET group (p = 0.576). The occurrence of sICH was noted in 6 patients (3.3%) from the RESET group and in 9 patients (6.2%) from the non-RESET group (p = 0.288). Mortality was less frequently observed in the RESET group, with seven deaths (3.8%) as compared to the non-RESET group which recorded nine deaths (6.2%) (p = 0.440). Upon adjustment, there was no significant association between the RESET group and the successful reperfusion (aOR 1.5, CI 0.55–4.06, p = 0.425), mRS of 0–2 at 90 days (aOR 1.36, CI 0.83–2.21, p = 0.223), incidence of sICH (adjusted OR 0.39, CI 0.12–1.23, p = 0.108), and mortality rate (adjusted OR 0.49, CI 0.16–1.44, p = 0.193) (see Table 2).
3.4 Study outcomes in the PSM population
Following propensity score matching, the cohort was refined to include 123 patients each in the RESET and non-RESET groups. These results were consistent with the primary analysis. Specifically, the RESET technique exhibited a significant association with FPE (aOR 2.85, CI 1.45–5.63, p = 0.002) when compared to the non-RESET group. However, no significant differences were observed in successful reperfusion (aOR 2.06, CI 0.59–7.19, p = 0.256), mRS of 0–2 at 90 days (aOR 1.34, CI 0.77–2.34, p = 0.297), incidence of sICH (aOR 0.46, CI 0.14–1.51, p = 0.198), and mortality rate (aOR 0.5, CI 0.15–1.68, p = 0.264).
4 Discussion
EVT has been demonstrated to be both safe and effective in the treatment of AIS caused by LVO. However, it is imperative to acknowledge that, while efficacious, EVT does not wholly eradicate the risks of morbidity and mortality (1). Prior research studies have suggested that successful recanalization achieved in a single or minimal thrombectomy attempt correlates with improved patient outcomes (2, 3). Nevertheless, complete reperfusion with a single pass is accomplished in <50% of patients, often necessitating multiple thrombectomy endeavors or even supplementary rescue therapy (19, 20). Multiple passes of thrombectomy devices might also extend the procedure duration, inflict harm to arterial endothelial tissue, and potentially impact clinical outcomes negatively (21, 22).
In the context of ongoing innovations in thrombectomy devices, the primary objective of thrombectomy should be to achieve complete revascularization with as few passes as possible. Nevertheless, an optimal EVT technique consensus, particularly in ICAS patients, is yet to be established (23). A prior report suggested the use of ADAPT for the initial attempt due to its association with higher reperfusion rates, increased positive outcomes, and reduced hemorrhagic complications. However, it still results in failed ADAPT in approximately one-third of cases, necessitating rescue therapy (24). Given that previous studies on aspiration techniques rarely included Asian populations (25), which display a substantial prevalence of ICAS, ADAPT may not be an appropriate treatment for severe atherosclerotic stenosis under such conditions. Other techniques, such as the Solumbra technique, continuous aspiration prior to intracranial vascular embolectomy (CAPTIVE) (8), SAVE, ASAP, Aspiration-Retriever technique for stroke (ARTS) (7), guide sheath advancement and aspiration in the distal petrocavernous ICA (GUARD) (26), balloon guide with large bore distal access catheter with dual aspiration with stent-retriever as standard (BADDASS) (11), and proximal balloon occlusion together with direct thrombus aspiration (PROTECT) (9, 10) involve a hybrid approach of aspiration and stent retrieval. However, these techniques' efficacy and safety remain untested in ICAS patients.
Our retrograde semi-retrieval technique offers several advantages over previously mentioned methods. First, it is a straightforward procedure that does not necessitate the use of complex devices such as balloon-guiding catheters or aspiration pumps, which can be financially burdensome for hospitals in many developing nations. Prior methods have employed an 8–9 Fr balloon-guiding catheter to achieve flow arrest; however, in situations with tortuous aortic arches, utilizing a larger balloon-guiding catheter poses a significant challenge. Additionally, the complication rate at the groin puncture site is estimated to be as high as 0.8% (27). Catheters with sheath sizes >8F have been associated with extended hospital stays and elevated mortality rates (28). Second, this method offers greater flexibility, with strategies varying based on whether the patient has an underlying ICAS. It has also been employed for patients without ICAS, as previously reported (29). The aspiration impact can be fine-tuned by adjusting the manual aspiration force and the retraction of the microcatheter (in cases where DIC could semi-retrieve the stent-retriever) (Figure 1). The aspiration catheter remains stationary at the location where the stent-retriever was withdrawn, applying a constant aspiration force to eliminate any potential thrombus fragments. This technique is similar to the ASAP method (12) but does not involve inflating a balloon guide catheter in the cervical ICA. Third, a DIC provides stability in the M1 segment, thereby enabling the swift execution of rescue therapy. This makes RESET an optimal thrombectomy procedure for ICAS patients as most ICAS patients require rescue therapy. In the majority of MCA occlusion cases, the DIC can be easily advanced to the MCA (13), facilitating the rapid exchange of the balloon or stent deployment. Fourth, the DIC is advanced close to the clot or the residual stenotic lesion, maximizing the aspiration force, reducing the clot-retrieval distance, and inhibiting thrombus migration. This simplifies the treatment and subsequent rescue therapies for atherosclerotic stenosis.
A potential concern about the RESET technique is its potential suboptimality when handling high-load thrombus due to the risk of fragment detachment and subsequent distal embolization, despite continuous aspiration. Nonetheless, in patients with ICAS, thrombi are typically smaller in size (30), making the blend of stent retrieval and aspiration generally adequate for successful clot removal. In cases of MCA occlusion, most stenosis typically localizes in the middle of the M1 segment as opposed to the bifurcation, a scenario more commonly observed in embolic strokes. This location is conducive for DIC advancement, facilitating more intimate contact with ICAS lesions, and potentially enabling even high-load thrombus management. In our routine practice, we seldom resort to alternative thrombectomy techniques and infrequently encounter thrombus distal embolization. Therefore, this strategy may serve well in treating patients presenting with ICAS.
In the propensity score-matched population, the FPE rate was achieved in 35 (28.5%) patients using the RESET technique, which is commendable considering the complexity of thrombectomy procedures in ICAS patients. In a single-center study comparing the efficacy of ADAPT and Solumbra techniques in ICAS patients, FPE was observed in 9 (16.1%) patients using ADAPT and 12 (25.0%) patients using the Solumbra technique (24). This discrepancy in FPE attainment can be attributed to several factors. First, inherent characteristics of RESET, such as the more distal positioning of the DIC, may account for some of this difference. The distal end of the DIC is closer to the ICAS lesion, which maximizes the aspiration force. Second, the aspiration starts while advancing the DIC to semi-retrieve the stent-retriever. Third, the semi-retrieval process brings the stent and the embedded thrombus into close contact, causing the thrombus to compact, which aids the retrieval process. The combined effect of a robust aspiration force, adequate aspiration during the stent semi-retrieval process and increased contact between the stent and thrombus collectively contribute to an enhanced FPE.
A significant reduction in the time from puncture to reperfusion was also noticed in patients treated with RESET. Previous research has established a link between decreased puncture-to-reperfusion time and improved functional outcomes (31, 32). The use of RESET for ICAS patients may enhance functional independence, as indicated by our findings showing a numerically higher proportion of patients achieving functional independence with RESET as the primary thrombectomy technique (RESET 56.0% vs. non-RESET 52.4%). The reduction in puncture-to-reperfusion time may be attributed to this technique's ability to swiftly facilitate rescue therapy. Prior research has demonstrated that both non-compliant balloons and intracranial stents are effective and safe for mechanical thrombectomy in acute ischemic stroke patients with ICAS and emergent LVO (33). However, in earlier studies, the rescue therapy procedure was complex and time-consuming. In this study, to rapidly reach the thrombus, the DIC was advanced as far as possible to improve access for balloon or stent delivery (Figure 2). Given that ICAS patients often present with severe stenotic lesions or tortuous intracranial blood vessels, making DIC advancement challenging, we utilize coaxial techniques and the stent's anchoring force to quickly deliver the DIC.
In our propensity score-matched population, we reported a sICH rate of 4.1% and a mortality rate of 4.1%. When compared to a previous meta-analysis that reported pooled rates of sICH and mortality at 5.5 and 20.2%, respectively, our study suggests that the RESET technique may be relatively safer (34). Numerous studies have indicated that more than three thrombectomy passes can be associated with intracerebral hemorrhage (35). In our study, upon confirmation of ICAS, we typically proceed directly to rescue therapy. Consequently, the number of thrombectomy passes is often limited to no more than two passes, assisted by aspiration. Furthermore, following each rescue therapy, we initiate aspiration to prevent the dispersion of emboli during the procedure. Finally, the semi-retrieval of the stent leads to a denser thrombus and a more secure adhesion between the stent and thrombus, further reducing the risk of thrombus embolization. These factors could potentially decrease the likelihood of thrombus migration and may elucidate the safety profile of the RESET technique.
The most effective thrombectomy technique for ICAS patients remains a subject of ongoing debate. While some neurointerventionists posit that stent thrombectomy surpasses aspiration in efficacy, the RESET method merges the strong suits of both techniques, thereby offering improved efficiency and safety. Therefore, the retrograde semi-retrieval technique merits consideration as a first-line treatment for patients with LVO and concomitant underlying ICAS.
This study has several limitations, including its retrospective design, single-center scope, and the exclusive enrollment of Chinese patients. Furthermore, selection bias may be present since patients with atrial fibrillation, who are presumed to have large-load thrombus, led treating physicians to favor non-RESET techniques. Future prospective multicenter studies are necessary to more comprehensively assess the potential advantages of the RESET technique over other methods in patients with AIS due to LVO with underlying ICAS.
In conclusion, the RESET technique is safe, effective, and applicable for patients with acute LVO caused by ICAS.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients/participants or patients/participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
WW: Data curation, Project administration, Writing—original draft. YX: Data curation, Formal analysis, Writing—original draft. BZ: Methodology, Project administration, Writing—review & editing. SL: Writing—review & editing, Data curation. ZM: Writing—original draft & editing, Visualization, Resources. SW: Writing—original draft, Validation, Investigation. PZ: Writing—review & editing, Methodology, Conceptualization, Formal analysis. MW: Methodology, Conceptualization, Writing—review & editing.
Funding
This study was funded by the National Health Commission Capacity Building and Continuing Education Center Nervous System and Minimally Invasive Intervention (Program No.GWJJ2022100106), the Tianjin Health Science and Technology (Project No. MS20015), the Beijing-Tianjin-Hebei Basic Research Cooperation Project (Grant number: 22JCZXJC00190), the Tianjin Key Medical Discipline (Specialty) Construction Project, Tianjin Key Research and Development Program in Science and Technology, No.19YFZCSY00260, and the Beijing Postdoctoral Research Foundation (Grant/Award Number: 2021-ZZ-029).
Acknowledgments
The authors extend our gratitude to the patients and their families for their participation. Moreover, we appreciate the support and assistance offered by our hospital leadership, thrombectomy teams, operating room colleagues, and collaborative departmental teams.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. (2019) 50:e344–418. doi: 10.1161/STR.0000000000000211
2. Flottmann F, Brekenfeld C, Broocks G, Leischner H, Mcdonough R, Faizy TD, et al. Good clinical outcome decreases with number of retrieval attempts in stroke thrombectomy. Stroke. (2021) 52:482–90. doi: 10.1161/STROKEAHA.120.029830
3. Seker F, Pfaff J, Wolf M, Ringleb PA, Nagel S, Schönenberger S, et al. Correlation of thrombectomy maneuver count with recanalization success and clinical outcome in patients with ischemic stroke. AJNR. (2017) 38:1368–71. doi: 10.3174/ajnr.A5212
4. Deshaies EM. Tri-axial system using the Solitaire-FR and Penumbra Aspiration Microcatheter for acute mechanical thrombectomy. J Clin Neurosci. (2013) 20:1303–5. doi: 10.1016/j.jocn.2012.10.037
5. Chen L, Shen R, Zhang X, Chen Z, Lu H, Zhou X, et al. A single-center comparative study of the SWIM technique in the treatment of acute ischemic stroke due to anterior circulation occlusion. Thromb Res. (2020) 192:131–3. doi: 10.1016/j.thromres.2020.05.011
6. Maus V, Henkel S, Riabikin A, Riedel C, Behme D, Tsogkas I, et al. The SAVE technique: large-scale experience for treatment of intracranial large vessel occlusions. Clin Neuroradiol. (2019) 29:669–76. doi: 10.1007/s00062-018-0702-4
7. Massari F, Henninger N, Lozano JD, Patel A, Kuhn AL, Howk M, et al. ARTS (aspiration-retriever technique for stroke): initial clinical experience. Interv Neuroradiol. (2016) 22:325–32. doi: 10.1177/1591019916632369
8. Mctaggart RA, Tung EL, Yaghi S, Cutting SM, Hemendinger M, Gale HI, et al. Continuous aspiration prior to intracranial vascular embolectomy (CAPTIVE): a technique which improves outcomes. J Neurointerv Surg. (2017) 9:1154–9. doi: 10.1136/neurintsurg-2016-012838
9. Maegerlein C, Berndt MT, Mönch S, Kreiser K, Boeckh-Behrens T, Lehm M, et al. Further development of combined techniques using stent retrievers, aspiration catheters and BGC: The PROTECT(PLUS) technique. Clin Neuroradiol. (2020) 30:59–65. doi: 10.1007/s00062-018-0742-9
10. Maegerlein C, Mönch S, Boeckh-Behrens T, Lehm M, Hedderich DM, Berndt MT, et al. PROTECT: PRoximal balloon Occlusion TogEther with direCt Thrombus aspiration during stent retriever thrombectomy - evaluation of a double embolic protection approach in endovascular stroke treatment. J Neurointerv Surg. (2018) 10:751–5. doi: 10.1136/neurintsurg-2017-013558
11. Ospel JM, Volny O, Jayaraman M, Mctaggart R, Goyal M. Optimizing fast first pass complete reperfusion in acute ischemic stroke - the BADDASS approach (BAlloon guiDe with large bore Distal Access catheter with dual aspiration with Stent-retriever as Standard approach). Expert Rev Med Devices. (2019) 16:955–63. doi: 10.1080/17434440.2019.1684263
12. Goto S, Ohshima T, Ishikawa K, Yamamoto T, Shimato S, Nishizawa T, et al. A stent-retrieving into an aspiration catheter with proximal balloon (ASAP) technique: a technique of mechanical thrombectomy. World Neurosurg. (2018) 109:e468–75. doi: 10.1016/j.wneu.2017.10.004
13. Nayak S. Mechanical thrombectomy using distal access catheters: current status and future prospects. J Neuroimaging. (2020) 30:754–61. doi: 10.1111/jon.12793
14. Wang Y, Zhao X, Liu L, Soo YO, Pu Y, Pan Y, et al. Prevalence and outcomes of symptomatic intracranial large artery stenoses and occlusions in China: the Chinese Intracranial Atherosclerosis (CICAS) Study. Stroke. (2014) 45:663–9. doi: 10.1161/STROKEAHA.113.003508
15. Baek JH, Kim BM, Kim DJ, Heo JH, Nam HS, Song D, et al. Importance of truncal-type occlusion in stentriever-based thrombectomy for acute stroke. Neurology. (2016) 87:1542–50. doi: 10.1212/WNL.0000000000003202
16. Baek JH, Kim BM, Yoo J, Nam HS, Kim YD, Kim DJ, et al. Predictive value of computed tomography angiography-determined occlusion type in stent retriever thrombectomy. Stroke. (2017) 48:2746–52. doi: 10.1161/STROKEAHA.117.018096
17. Samuels OB, Joseph GJ, Lynn MJ, Smith HA, Chimowitz MI. A standardized method for measuring intracranial arterial stenosis. AJNR Am J Neuroradiol. (2000) 21:643–6.
18. Hacke W, Kaste M, Fieschi C, Von Kummer R, Davalos A, Meier D, et al. Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Second Eur-Austral Acute Stroke Study Invest Lancet. (1998) 352:1245–51. doi: 10.1016/S0140-6736(98)08020-9
19. Nikoubashman O, Dekeyzer S, Riabikin A, Keulers A, Reich A, Mpotsaris A, et al. True first-pass effect. Stroke. (2019) 50:2140–6. doi: 10.1161/STROKEAHA.119.025148
20. Linfante I, Starosciak AK, Walker GR, Dabus G, Castonguay AC, Gupta R, et al. Predictors of poor outcome despite recanalization: a multiple regression analysis of the NASA registry. J Neurointerv Surg. (2016) 8:224–9. doi: 10.1136/neurintsurg-2014-011525
21. Zaidat OO, Castonguay AC, Linfante I, Gupta R, Martin CO, Holloway WE, et al. First pass effect: a new measure for stroke thrombectomy devices. Stroke. (2018) 49:660–6. doi: 10.1161/STROKEAHA.117.020315
22. Dong S, Yu C, Wu Q, Xia H, Xu J, Gong K, et al. Predictors of symptomatic intracranial hemorrhage after endovascular thrombectomy in acute ischemic stroke: a systematic review and meta-analysis. Cerebrovasc Dis. (2023) 52:363–75. doi: 10.1159/000527193
23. Munoz A, Jabre R, Orenday-Barraza JM, Eldin MS, Chen C-J, Al-Saiegh F, et al. A review of mechanical thrombectomy techniques for acute ischemic stroke. Intervent Neuroradiol. (2022) 29:450–8. doi: 10.1177/15910199221084481
24. Li ZS, Zhou TF, Li Q, Guan M, Liu H, Zhu LF, et al. Endovascular management of intracranial atherosclerosis-related large vessel occlusion with the a direct aspiration first-pass thrombectomy compared with solumbra technique. Front Neurol. (2021) 12:643633. doi: 10.3389/fneur.2021.643633
25. Turk AS, Frei D, Fiorella D, Mocco J, Baxter B, Siddiqui A, et al. ADAPT FAST study: a direct aspiration first pass technique for acute stroke thrombectomy. J Neurointerv Surg. (2018) 10:i4–7. doi: 10.1136/neurintsurg-2014-011125.rep
26. Ansari SA, Darwish M, Abdalla RN, Cantrell DR, Shaibani A, Hurley MC, et al. GUide sheath advancement and aspiration in the distal petrocavernous internal carotid artery (GUARD) technique during thrombectomy improves reperfusion and clinical outcomes. AJNR. (2019) 40:1356–62. doi: 10.3174/ajnr.A6132
27. Shah VA, Martin CO, Hawkins AM, Holloway WE, Junna S, Akhtar N. Groin complications in endovascular mechanical thrombectomy for acute ischemic stroke: a 10-year single center experience. J Neurointerv Surg. (2016) 8:568–70. doi: 10.1136/neurintsurg-2015-011763
28. Trimarchi S, Smith DE, Share D, Jani SM, O'Donnell M, Mcnamara R, et al. Retroperitoneal hematoma after percutaneous coronary intervention: prevalence, risk factors, management, outcomes, and predictors of mortality: a report from the BMC2 (Blue Cross Blue Shield of Michigan Cardiovascular Consortium) registry. JACC Cardiovasc Interv. (2010) 3:845–50. doi: 10.1016/j.jcin.2010.05.013
29. Wei M, Wei Z, Li X, Li H. Retrograde semi-retrieval technique for combined stentriever plus aspiration thrombectomy in acute ischemic stroke. Interv Neuroradiol. (2017) 23:285–8. doi: 10.1177/1591019916689053
30. Kang DH, Yoon W, Baek BH, Kim SK, Lee YY, Kim JT, et al. Front-line thrombectomy for acute large-vessel occlusion with underlying severe intracranial stenosis: stent retriever versus contact aspiration. J Neurosurg. (2019) 132:1202–8. doi: 10.3171/2019.1.JNS182905
31. Bourcier R, Goyal M, Liebeskind DS, Muir KW, Desal H, Siddiqui AH, et al. Association of time from stroke onset to groin puncture with quality of reperfusion after mechanical thrombectomy: a meta-analysis of individual patient data from 7 randomized clinical trials. JAMA Neurol. (2019) 76:405–11. doi: 10.1001/jamaneurol.2018.4510
32. Sun CH, Zaidat OO, Castonguay AC, Veznedaroglu E, Budzik RF, English J, et al. A decade of improvement in door-to-puncture times for mechanical thrombectomy but ongoing stagnation in prehospital care. Stroke Vasc Intervent Neurol. (2023) 3:e000561. doi: 10.1161/SVIN.122.000561
33. Yoon W, Kim SK, Park MS, Kim BC, Kang HK. Endovascular treatment and the outcomes of atherosclerotic intracranial stenosis in patients with hyperacute stroke. Neurosurgery. (2015) 76:680–6; discussion 686. doi: 10.1227/NEU.0000000000000694
34. Almallouhi E, Murad MH, Chalhoub R, Kicielinski KP, Lena J, Brennan EA, et al. Rescue endovascular treatment of patients with emergent large vessel occlusion attributed to intracranial atherosclerosis: a systematic review and meta-analysis. Stroke Vasc Interven Neurol. (2023) 3:e000510. doi: 10.1161/SVIN.122.000510
Keywords: thrombectomy, acute ischemic stroke, large vessel occlusion, stent retriever, retrograde semi-retrieval technique
Citation: Wang W, Xu Y, Zhang B, Liu S, Ma Z, Wang S, Zhang P and Wei M (2024) Mechanical thrombectomy using the retrograde semi-retrieval technique for patients with underlying intracranial atherosclerotic stenosis. Front. Neurol. 14:1280181. doi: 10.3389/fneur.2023.1280181
Received: 19 August 2023; Accepted: 13 November 2023;
Published: 12 January 2024.
Edited by:
Takeshi Yoshimoto, National Cerebral and Cardiovascular Center, JapanCopyright © 2024 Wang, Xu, Zhang, Liu, Ma, Wang, Zhang and Wei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ming Wei, ZHJ3ZWltaW5nQDE2My5jb20=; Pinyuan Zhang, WmhweV83NkBzaW5hLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Wei Wang
Wei Wang Yongbo Xu3,4†
Yongbo Xu3,4† Bohao Zhang
Bohao Zhang