
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol. , 27 November 2023
Sec. Headache and Neurogenic Pain
Volume 14 - 2023 | https://doi.org/10.3389/fneur.2023.1231351
Purpose: The study aimed to validate and compare coding algorithms for identifying people with migraine within the Japanese claims database.
Methods: This study used the administrative claim database provided by DeSC Healthcare, Inc., that was linked to the results of an online survey administered to adult users of the health app “kencom®.” The ability of the 12 algorithms to detect migraines using diagnostic records alone or with prescription records was evaluated based on sensitivity, specificity, positive predictive values (PPVs), and negative predictive values (NPVs). We used a migraine diagnosis judged based on respondents' self-reported symptoms according to the diagnostic criteria of the International Classification of Headache Disorders, version 3 (ICHD-3), as true.
Results: Of the 21,480 individuals, 691 had migraine according to the ICHD-3 criteria. The 12 algorithms had a sensitivity of 5.4–8.8%, specificity of 98.8–99.6%, PPVs of 19.2–32.5%, and NPVs of 96.9–97.0%. Algorithm 9 (migraine diagnostic records more than once AND at least one prescription record for migraine prophylaxis or triptans in the same month as diagnosis) produced the highest PPV, whereas Algorithm 2 (at least one diagnostic record of migraine or tension-type headache) had the highest sensitivity. Similar trends were observed when using the ID-Migraine or 4-item migraine screener, instead of the ICHD-3 criteria, for case ascertainment.
Conclusion: Strict algorithms, such as Algorithm 9, yielded a higher PPV but a lower sensitivity, and such algorithms may be suitable for studies estimating the relative risk. Conversely, algorithms based on a single diagnostic record, such as Algorithm 2, had a higher sensitivity and may be suitable for studies estimating the prevalence/incidence of disease. Our findings will help select a desirable algorithm for migraine studies using a Japanese claim database.
Migraine is a highly disabling neurological disorder, with a prevalence exceeding that of diabetes, epilepsy, and asthma combined (1). It is more common in women than in men, with a global age-standardized prevalence of 18.9% in women and 9.8% in men (2). Estimates of the prevalence of migraine in Japan are slightly lower, ranging from 6.0 to 8.6% (3, 4). According to the Global Burden of Disease 2016 survey, it is the second leading cause of disability worldwide (1), particularly in women under the age of 50 years (2).
Despite its prevalence, migraines have only recently been recognized as an important public health concern (5). It was not included in the Global Burden of Diseases, Injuries, and Risk Factors studies before 2000 (2). Migraine research has historically been underfunded (6, 7) partially because it is an “invisible” disorder (8) and there are no obvious physical manifestations or clinical laboratory results associated with migraine. Consequently, this condition is often underestimated, underdiagnosed, and undertreated (9–12). However, its impact on productivity and quality of life is substantial (13). According to an employee population survey in Japan, the estimated annual economic loss due to presenteeism was USD 2,217 per person (5). Therefore, further research on migraine should be conducted in Japan to reduce this large patient burden.
The diagnosis of migraine is based on the symptoms reported by the patients. The diagnostic criteria for migraine, according to the International Classification of Headache Disorders, version 3 (ICHD-3), are attacks lasting for 4–72 h with any two of the following attributes: unilateral location, pulsating quality, moderate to severe pain intensity, and aggravation by physical activity (14). In addition, attacks must be accompanied by either nausea and/or vomiting or photophobia and phonophobia (14). Questionnaires such as the ID-Migraine (15) and 4-item migraine screener (16) have been developed and used as diagnostic screeners to aid in the diagnosis of migraine.
Medical claims databases, which generally store anonymized, individual-level, and standardized data on patients (e.g., age and sex) and claims (e.g., diagnosis, prescriptions, and treatments) in both inpatient and outpatient settings, are used in studies on many diseases in Japan; however, these data are not primarily generated for research purposes. Therefore, the use of validated algorithms to identify patients with a disease of interest is crucial to avoid misclassification of outcomes and exposures (17, 18), which can introduce bias (19). In validation studies, the accuracy of claims-based algorithms is usually compared to a gold-standard source of information such as clinical laboratory values, medical chart reviews, or registry data (20, 21). However, for migraine, which is diagnosed based on patients' descriptions of their symptoms, information obtained from a self-report questionnaire may help detect it. Indeed, a previous validation study conducted in the U.S. developed algorithms to identify patients who had not been diagnosed with chronic migraine using claims data. The study evaluated its performance using a questionnaire survey in combination with semi-structured interviews as the gold standard method for diagnosing chronic migraine (22).
In Japan, no studies have assessed claim-based algorithms for migraine detection. Therefore, in the present study, we compared 12 coding algorithms to identify people with migraines within a Japanese claim database based on four measures: sensitivity, specificity, positive predictive values (PPVs), and negative predictive values (NPVs). Given the diagnostic nature of migraine, which depends on patients' self-description of their symptoms, we used patient responses to an online survey asking about their symptoms, which incorporated questions in line with the diagnostic criteria of the ICHD-3. We considered migraine cases classified according to the survey responses as true migraine cases. Additionally, we have also examined the four measures considering individuals classified as having migraine according to the ID-Migraine and 4-item migraine screeners as true cases. Our findings could provide useful information to define and validate migraine cases in future database studies.
This study used a combination of administrative claims data and the linked results of an online survey. The combined data were obtained from DeSC Healthcare, Inc. (DeSC). The details of the conduct of this study were provided in an earlier publication (23).
The claims data, covering the period from 1 December 2017 to 30 November 2020, were provided by the society-managed employment-based health insurance associations that had contracts with DeSC for subscribers who agreed to the secondary use of their medical data by DeSC (~600,000 subscribers). Data included patient information (e.g., age and sex), diagnoses, prescriptions, and treatments in both inpatient and outpatient settings.
Regarding the survey data, an online survey was administered by DeSC to the registered users of the health app “kencom®” aged 19–74 years (~150,000 users), irrespective of the presence of headache, from 1 to 30 November 2020. This health monitoring app was designed by DeSC and is freely available to users in Japan who are members of an affiliated society-managed, employment-based health insurance association (24). The survey questionnaire included items on sociodemographic characteristics (e.g., age, sex, residential area, occupation, and annual household income) and questions related to headache (the clinical features that include headache in the past 3 months, headache frequency, symptoms of headache, types of headache medicines used, impact of headache on daily activities, and questions to measure migraine-specific quality of life, work productivity, and activity impairment) (23). The questions also included items in line with the diagnostic criteria of the ICHD-3 (14) or common screening tools for migraine [e.g., ID-Migraine (15) and 4-item migraine screener (16)]. The study included all individuals who responded to the online survey regardless of whether they had headaches.
This study was approved by the independent ethics committee of Otsuka Pharmaceutical Co., Ltd. (approval no. 220617). The study used anonymized data, and no new individual-level consent was obtained for data use. The survey was conducted in accordance with the ethical guidelines for medical and biological research involving human subjects in Japan and the Declaration of Helsinki (revised in October 2013) of the World Medical Association.
The present study assessed the ability of 12 algorithms to detect people with migraines within the database (Table 1). These 12 algorithms were selected, through consultation with headache specialists and epidemiologists, from the combinations of the following disease and prescription codes identified in the claims data: diagnostic records of migraine [International Classification of Diseases-10 (ICD-10) code G43], tension-type headache (ICD-10 code G44.2), or premenstrual migraine (Japanese disease/injury code 8833260, under ICD-10 code N94.3) alone, or in combination with prescription records of acute medications [i.e., triptans, acetaminophen, and nonsteroidal anti-inflammatory drugs (NSAIDs)] or prophylactic medications (i.e., valproic acid, topiramate, propranolol, lomerizine, and candesartan). These medications were chosen from those listed in the Clinical Practice Guidelines for Headache 2021, according to the clinician's judgment on their use in migraine treatment in clinical practice (25). We constructed algorithms that included a diagnostic record of tension-type headache (G44.2), in addition to migraines, because chronic or frequent migraines can transform into tension-type headache (transformed migraines) and vice versa.
As the database was not linked to patient medical records, we were unable to conduct a chart review, which is the gold standard for case ascertainment. Instead, the present study judged migraine cases based on respondents' self-reported symptoms according to the diagnostic criteria of the ICHD-3 (14). Additionally, we defined the cases according to two valid diagnostic screeners for migraine: (1) ID-Migraine, consisting of three items on disability, nausea, and photophobia (15); and (2) 4-item migraine screener, with four questions on the aggravation by daily activities, nausea/stomach discomfort, photophobia, and osmophobia (16). Conditions to meet the definitions of migraine according to each of these three criteria are provided in Supplementary Table S1.
The demographic and disease characteristics of the respondents are descriptively summarized. For each algorithm, a confusion matrix was constructed using a diagnosis based on survey responses as true (Table 2). The ability of each algorithm to detect people with migraine was evaluated primarily using PPV. The PPV was calculated as the proportion of migraine cases based on survey responses, i.e., true positives (= a), among migraine patients detected using the algorithm (= a + b) (Table 2). Additionally, sensitivity [proportion of true positives (a) among migraine cases based on survey responses (= a + c)], specificity [proportion of false positives (b) among non-migraine individuals based on survey responses (= b + d)], and NPV [proportion of true negatives (d) among non-migraine individuals based on the algorithm (= c + d)] were also calculated. For exploratory purposes, stratification by sex and age group (19–29, 30–39, 40–49, 50–59, and ≥60 years) was also performed. In addition to the analysis that meets the definition of migraine according to each of the three criteria, we have also performed analyses based on migraine cases that met all three criteria as well as those that met one of them. All statistical analyses were performed in SAS Release 9.4 (SAS Institute, Inc., NC, USA). Missing data were treated as they were, and no imputation was performed.
A total of 604,102 members of the health insurance association consented to the secondary use of their medical data (Figure 1). After excluding 765 members aged <19 or >74 years, 603,337 (99.9%) aged 19–74 years met the age criteria. Of these, 153,545 (25.4%) were registered with Kencom®. Of the 21,704 individuals who responded to the survey, 224 were excluded because their age and/or sex did not match the medical claims data, resulting in an analysis population of 21,480 (99.0%) respondents (Figure 1).
Of the 21,480 individuals included in the study population, 15,802 (73.6%) were men and 5,678 (26.4%) were women, with a mean (standard deviation) age of 48.8 (10.5) years (Table 3). Among the overall study population, 7,311 (34.0%) reported having headaches; of these, 735 (10.1%) responded that they had visited a physician for headaches, and 2,859 (39.1%) reported that they only used over-the-counter (OTC) drugs for headaches.

Table 3. Demographics and disease characteristics of the study population irrespective of the presence of headache.
Of the 21,480 respondents, 691 (3.2%) had migraine according to the ICHD-3 criteria, 616 (2.9%) according to the ID-Migraine, and 653 (3.0%) according to the 4-item migraine screener (Figure 1). Using these results as the “true” diagnosis, we evaluated the ability of each algorithm to identify people with migraine.
The assessment indices calculated for each of the 12 algorithms using the ICHD-3 criteria for case ascertainment are summarized in Table 4. PPVs ranged from 19.2% for Algorithm 2 (at least one diagnostic record of migraine or tension-type headache) to 32.5% for Algorithm 9 [migraine diagnostic records more than once AND at least one prescription record for migraine prophylaxis or triptans in the same month as the diagnostic record of migraine (Algorithm 5)]. The overall sensitivity was low, with the highest value of 8.8% for Algorithm 2. In contrast, the specificity was excellent (~99%) for all algorithms, with high NPVs of ~97%.
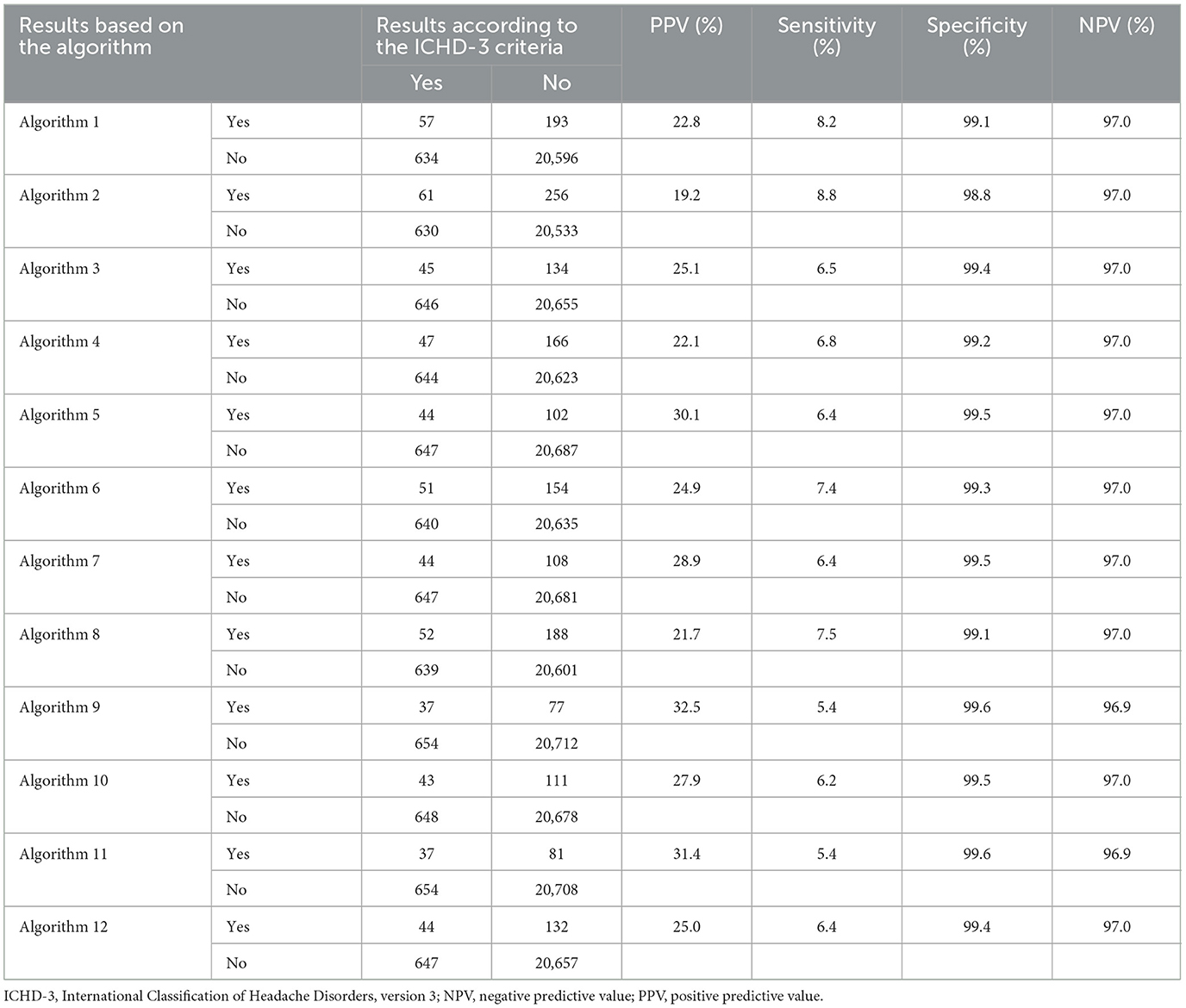
Table 4. PPV, sensitivity, specificity, and NPV for each algorithm, using diagnosis according to the ICHD-3 criteria as true.
The evaluation results of each algorithm using the ID-Migraine for case ascertainment are summarized in Table 5. PPVs ranged from 26.2% for Algorithm 2 to 39.7% for Algorithm 5. The sensitivity ranged from 7.3% for Algorithms 9 and 11 (the same diagnostic records of migraine or tension-type headache more than once AND at least one prescription record for migraine prophylaxis or triptans in the same month as the diagnostic record of migraine or tension-type headache) to 13.5% for Algorithm 2. The specificity was high at ~99% for all algorithms, with high NPVs of ~97%.
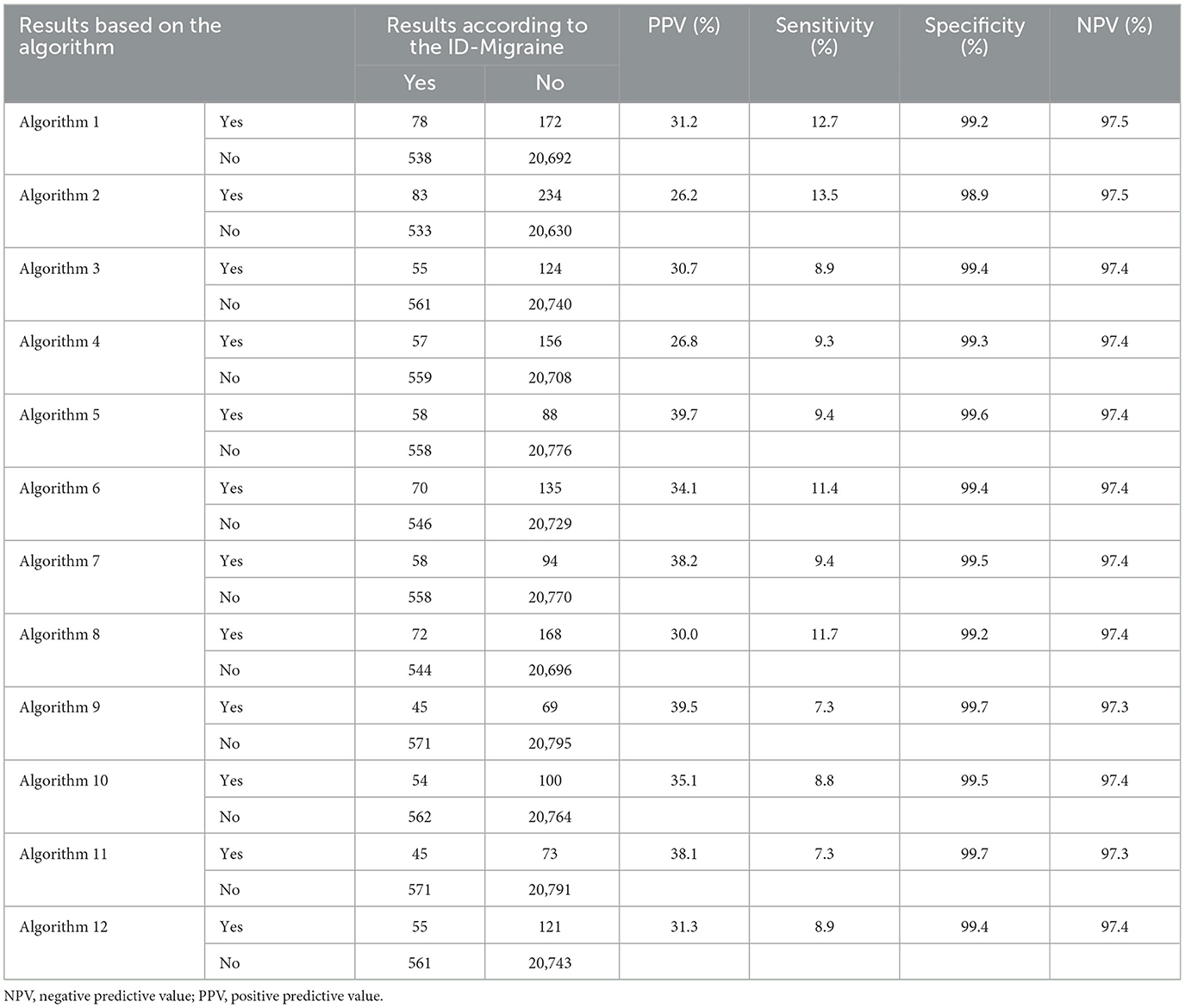
Table 5. PPV, sensitivity, specificity, and NPV for each algorithm, using diagnosis according to the ID-Migraine as true.
The results of using the 4-item migraine screener for case ascertainment are summarized in Table 6. PPVs ranged from 27.1% for Algorithm 2 to 42.1% for Algorithm 9. The sensitivity was the lowest at 7.4% for Algorithms 9 and 11, whereas the highest was 13.2% for Algorithm 2. The specificity was ~99%, and the NPVs were ~97% for all algorithms.
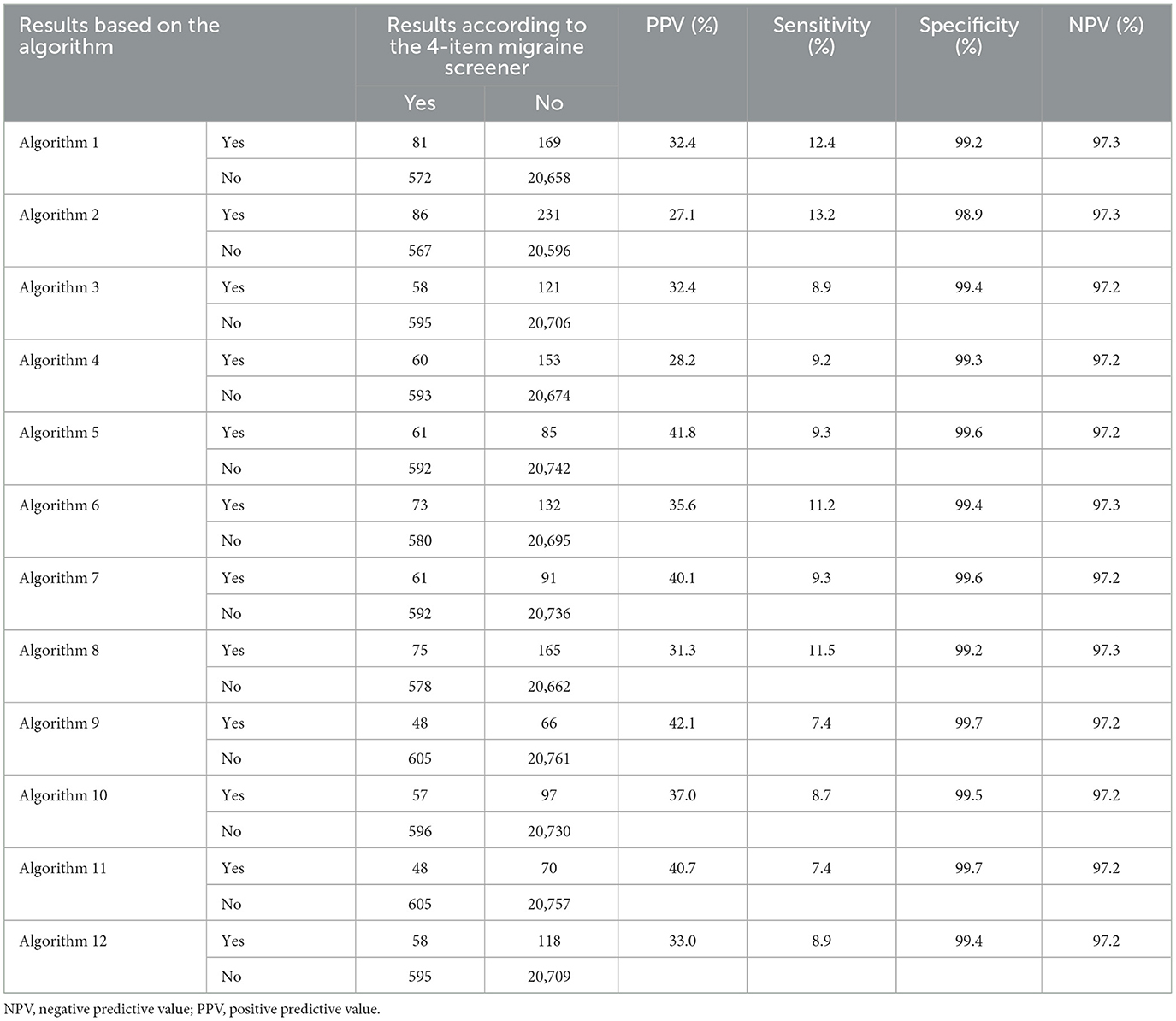
Table 6. PPV, sensitivity, specificity, and NPV for each algorithm, using diagnosis according to the 4-item migraine screener as true.
Additional analyses based on cases that meet all three criteria of ICHD-3, ID-Migraine, and 4-item screener and those that meet one of them are provided in Supplementary Tables S2, S3. Both results showed that Algorithm 9 yielded the highest PPV, and Algorithm 2 yielded the highest sensitivity. This pattern remained consistent with that found among the migraine cases identified using each of the three methods.
As Algorithm 9 yielded the highest (or the second highest) PPV regardless of the criteria used to judge “true” migraine cases, we additionally evaluated its performance, stratifying by sex and age groups (Tables 7–9). According to the ICHD-3 criteria, the PPVs were 17.3% for men and 45.2% for women when stratified by sex (Table 7). PPVs were the highest at 66.7% for people aged 19–29 years, followed by 42.1% for 30–39 years and 41.3% for 40–49 years, and they decreased to18.4% for those aged 50–59 years and 12.5% for those aged ≥60 years. Similar trends were observed with the ID-Migraine (Table 8) and the 4-item migraine screener (Table 9).
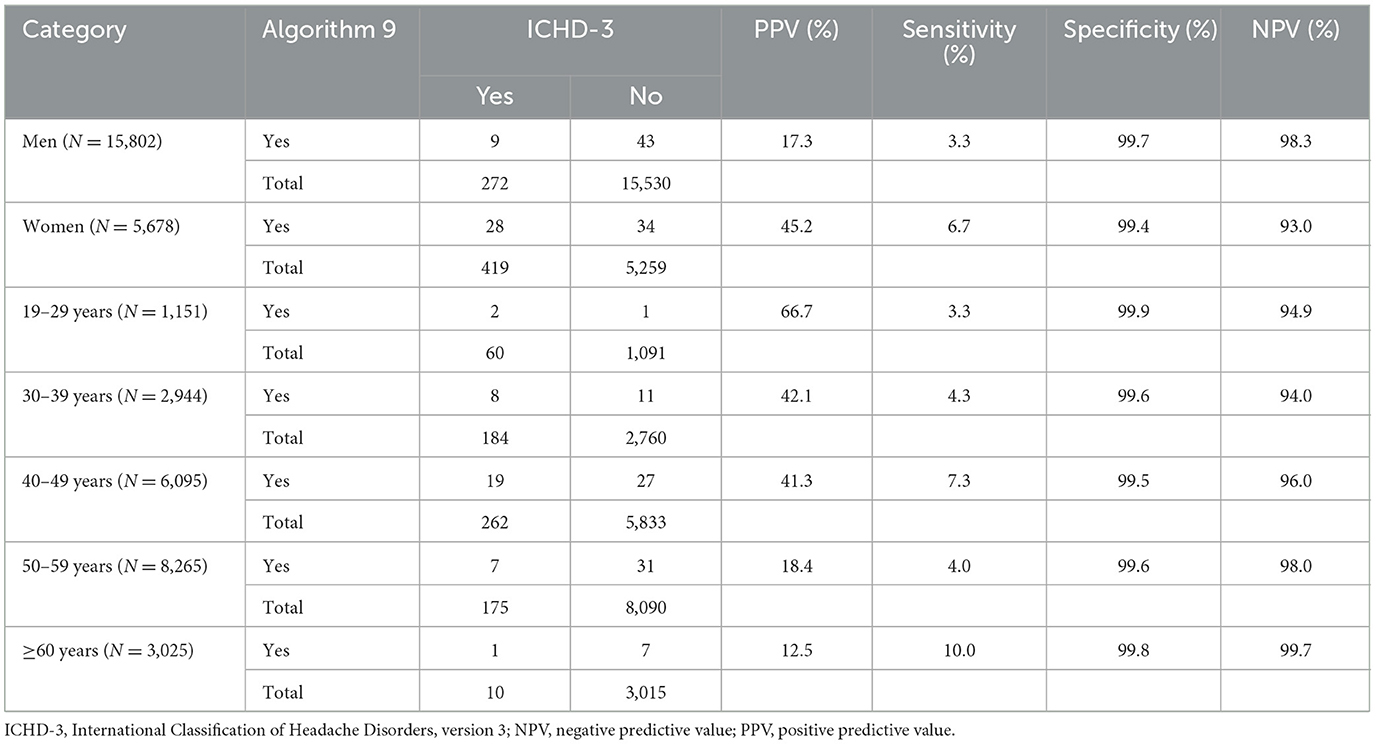
Table 7. Assessment results of algorithm 9, using diagnosis according to the ICHD-3 criteria as true.
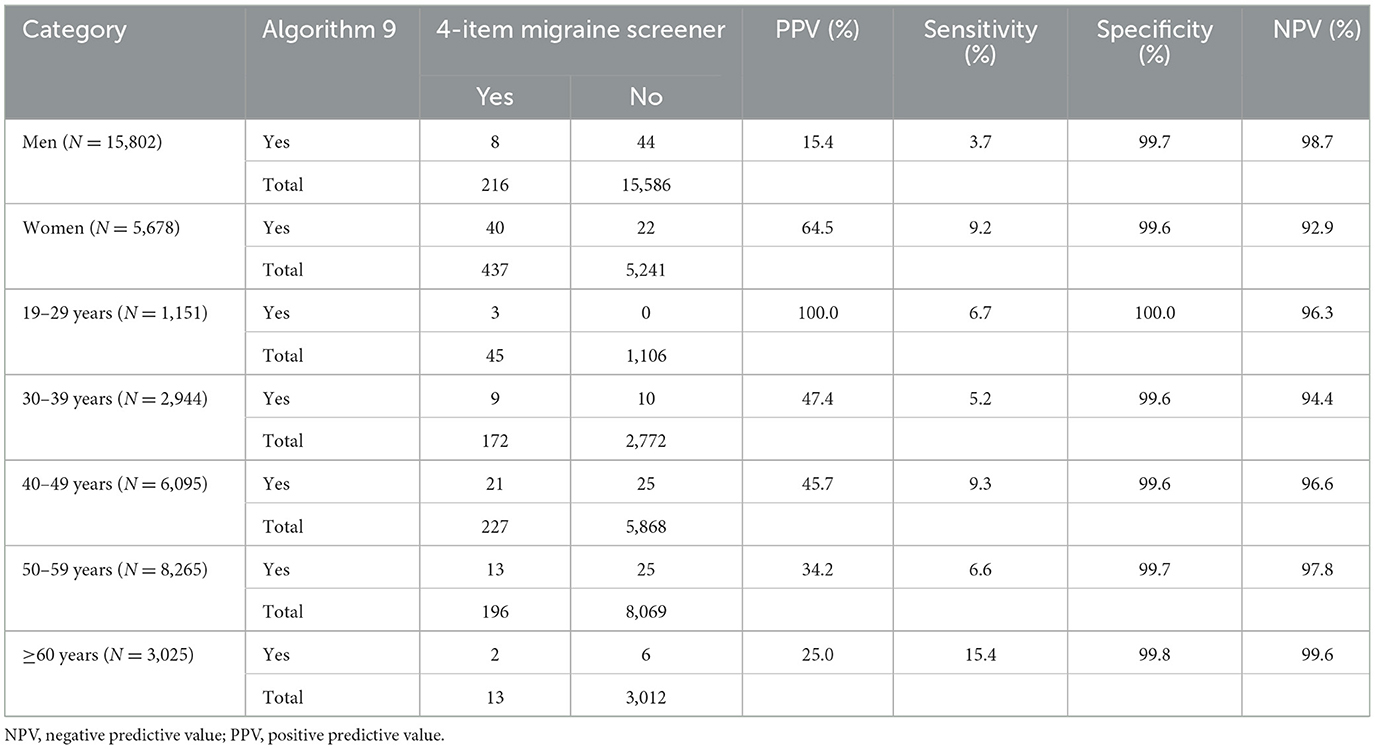
Table 9. Assessment results of algorithm 9, using diagnosis according to the 4-item migraine screener as true.
In this study, we explored the ability of 12 coding algorithms, based on diagnostic records alone or in combination with prescription records, to identify people with migraine within a large-scale Japanese claims database. As migraine is diagnosed based primarily on patients' descriptions of their symptoms, we judged the “true” migraine cases using self-reported information collected in the online survey. The non-use of semi-structured interviews limited the accuracy of “true” migraine cases in this study. However, we observed consistent trends in the assessment of our algorithms for the three criteria used for case ascertainment. These trends, which are discussed below, can provide useful information for considering an appropriate coding algorithm to define migraines in each claims database study.
The 12 algorithms had overall low PPVs of ~20–30% with the ICHD-3 criteria and 30–40% with the ID-Migraine or 4-item migraine screener. However, this result should be interpreted in light of the fact that PPV depends on disease prevalence (26). These values were influenced by the low prevalence of migraine in this population (2.9–3.2%), which was lower than the reported prevalence of 6.0–8.6% in Japan (3, 4). This low prevalence may be related to the fact that this study was based on a self-administered survey without semi-structured interviews, which may have underestimated the prevalence of migraine and PPV. Many people with migraine are reportedly undiagnosed (3, 5, 27). A previous study reported that 59.4–71.8% of people with migraine in Japan had never consulted a physician previously, and only 11.6% were aware of the condition (28). Low awareness of migraine and the common use of OTC drugs for headaches (3) may have underestimated the number of people with migraine in the claims database. Indeed, only 250 people had a migraine diagnostic record in this study, whereas the responses to the survey suggested that 616–691 people possibly had migraines. This may also be partially responsible for the overall low sensitivity of our algorithms (5.4–13.5%), given the possibility of misclassifying patients who had migraines as “false negatives” because there are no migraine records in their claim records.
Among the 12 algorithms, we found that Algorithms 9 and 5 yielded the highest PPVs (32.5–42.1%), and this trend was consistent regardless of the criteria used for case ascertainment. This was probably because the strict conditions that require single (Algorithm 5) or multiple (Algorithm 9) diagnostic records plus prescription records of migraine prophylaxis or triptans could reduce “false positives.” Interestingly, the addition of acetaminophen or NSAIDs to triptans lowered the PPVs (Algorithms 6 vs. 5, 8 vs. 7, 10 vs. 9, and 12 vs. 11). These analgesics have wider indications and can be used for other conditions, which may have increased “false positives.” In contrast, Algorithm 2, which relied on a single diagnostic record of migraine or tension-type headache had the lowest PPV (19.2–27.1%). The algorithm used in a study that aims to estimate the relative risk of an outcome should have a high PPV so that the relative risk can be correctly estimated (26). Therefore, a strict coding algorithm based on a combination of multiple diagnostic records and prescription records of specific treatments, such as Algorithm 9, may be the most suitable for a migraine study with such an aim because it can reduce “false positives” and increase PPV.
However, a high PPV has high specificity, possibly at the sacrifice of sensitivity, as a result of increasing “false negatives (26).” Accordingly, Algorithm 9, which had high PPVs, had the lowest sensitivity (5.4–7.4%), while Algorithm 2, which had low PPVs, had the highest sensitivity (8.8–13.5%). For an exploratory study or a study that aims to estimate the prevalence or incidence of an outcome, an algorithm with high sensitivity is desirable (26) because maximizing the inclusion of patients with the target disease is more important than purifying the population under strict conditions. Therefore, for such a study aim, an algorithm based solely on a simple diagnostic record of migraine or tension-type headaches, such as Algorithm 2, may be desirable. This algorithm had the highest sensitivity, although at low levels, yet had an excellent specificity of ~99%, indicating the high accuracy of the diagnostic records in the claims database.
In stratified analyses, the PPV was higher in women and individuals aged 20 to 40 years, which is in line with the sex and age trends of migraine prevalence. The prevalence of migraine in women is 2 to 3.6 times higher than that in men (3, 29). Moreover, the prevalence is the highest between 30 and 39 years of age and decreases as age increases (30). Considering that the present study population was predominantly male (73.6%), the prevalence of migraine may have been lower than that in the general population, which may have affected the PPVs observed in our analysis of the overall study population. Therefore, our data stratified by sex and age group may be more useful as a reference when considering an appropriate claims-based algorithm in other studies, depending on the demographic characteristics of the population in these settings.
This study has some limitations, including those previously reported (23). For example, the study population may not represent the overall adult population of Japan since the database comprised data from employees and family members of large companies that are members of the health insurance associations, and survey respondents were limited to the Kencom® users, with a high proportion of men (73.6%) compared to the general population in Japan [the prevalence of migraine in women and men was however 7.4 and 1.7%, respectively (23)]. These background characteristics may have influenced the low number of PPVs identified in this study. Because the prevalence of migraine or the distribution of other factors in our data may differ from those of other settings, the absolute values of this study may not be applicable to other databases.
One major limitation was that the present study used self-reported information collected in the online survey to judge the “true” migraine cases. Although the survey questionnaire included all items necessary to classify migraine according to the ICHD-3 criteria, no consultations with healthcare providers restricted us from obtaining an accurate or more reliable “true” status of migraine. Moreover, the ID-Migraine and 4-item migraine screener are screening tools although their use is recommended to aid diagnosis in clinical practice (25). However, these screening tools were used for supplemental purposes, considering that the ICHD-3 criteria may be too strict and miss unknown “true” migraineurs. Therefore, the accuracy of the case ascertainment in this study was limited, and the absolute values obtained should not be overinterpreted. Nevertheless, it is noteworthy that consistent trends were observed in the performance of the 12 algorithms across the three criteria. These findings will help us understand the advantages and disadvantages of each claims-based algorithm for use in migraine studies using Japanese claims databases.
A claims-based algorithm based on both the diagnostic records and prescription records of specific migraine medications had the highest PPV among the 12 algorithms considered, suggesting that such strict conditions may be appropriate for a study aimed at estimating relative risks. However, for an exploratory study, an algorithm based on a single diagnostic record of migraine or tension-type headache may be more suitable because it has higher sensitivity while maintaining high specificity. Because a suitable algorithm differs depending on the purpose of the study, it is important to choose an appropriate algorithm to define migraine in each claims database study.
The data that support the findings of this study are available from DeSC Healthcare, Inc. (Tokyo, Japan), but restrictions apply to the availability of these data, which were used under license for the current study and are not publicly available. However, data are available from the authors upon reasonable request and with permission of DeSC Healthcare, Inc. Requests to access these datasets should be directed to KY, WWFtYXRvLktlbnRhcm9Ab3RzdWthLmpw.
The studies involving humans were approved by the Independent Ethics Committee of Otsuka Pharmaceutical Co., Ltd. (approval no. 220617). The study used anonymized data, and no new individual-level consent was obtained for data use. The survey was conducted in accordance with the Ethical Guidelines for Medical and Biological Research Involving Human Subjects in Japan and the Declaration of Helsinki (revised in October 2013) of the World Medical Association. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
KY and HS contributed to the study conception, design, and contributed to the manuscript drafting. KH and TN reviewed and revised it critically for important intellectual content. All authors approved the final version of the manuscript for publication and agreed to be accountable for all aspects of this study and made substantial contributions to the analysis or interpretation of data.
This study was sponsored and funded by the Otsuka Pharmaceutical Co., Ltd. The funder had the following involvement with the study: the study design, collection, analysis, interpretation of data, the writing of this article, and the decision to submit it for publication.
Otsuka Pharmaceutical Co., Ltd. contracted with DeSC Healthcare, Inc. for data management and extraction services, Clinical Study Support., Inc. for statistical analysis, and Clinical Study Support, Inc. in collaboration with Evidera-PPD for writing and editorial services. The authors thank Tatsuo Sakashita for statistical support and Michael Ossipov of Evidera-PPD and Yuri Haga of Clinical Study Support for their help with writing, editing, and formatting the manuscript.
KY and HS are employees of the Otsuka Pharmaceutical Co., Ltd. KH and TN have advisory role for Otsuka Pharmaceutical Co., Ltd.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2023.1231351/full#supplementary-material
1. GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet. (2017) 390:1211–59. doi: 10.1016/S0140-6736(17)32154-2
2. GBD 2016 Headache Collaborators. Global, regional, and national burden of migraine and tension-type headache, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. (2018) 17:954–76. doi: 10.1016/S1474-4422(18)30322-3
3. Sakai F, Igarashi H. Prevalence of migraine in Japan: a nationwide survey. Cephalalgia. (1997) 17:15–22. doi: 10.1046/j.1468-2982.1997.1701015.x
4. Hirata K, Ueda K, Komori M, Zagar AJ, Selzler KJ, Nelson AM, et al. Comprehensive population-based survey of migraine in Japan: results of the observational survey of the epidemiology, treatment, and care of migraine (overcome [Japan]) study. Curr Med Res Opin. (2021) 37:1945–55. doi: 10.1080/03007995.2021.1971179
5. Shimizu T, Sakai F, Miyake H, Sone T, Sato M, Tanabe S, et al. Disability, quality of life, productivity impairment and employer costs of migraine in the workplace. J Headache Pain. (2021) 22:29. doi: 10.1186/s10194-021-01243-5
6. National Institutes of Health. Estimates of Funding for Various Research, Condition, and Disease Categories (RCDC). (2023). Available online at: https://report.nih.gov/funding/categorical-spending#/ (accessed March 30, 2023).
7. Schwedt TJ, Shapiro RE. Funding of research on headache disorders by the national institutes of health. Headache. (2009) 49:162–9. doi: 10.1111/j.1526-4610.2008.01323.x
8. Rutberg S, Öhrling K. Migraine–more than a headache: women's experiences of living with migraine. Disabil Rehabil. (2012) 34:329–36. doi: 10.3109/09638288.2011.607211
9. Dodick D, Edvinsson L, Makino T, Grisold W, Sakai F, Jensen R, et al. Vancouver declaration on global headache patient advocacy 2018. Cephalalgia. (2018) 12:333102418781644. doi: 10.1177/0333102418781644
10. Lipton RB, Silberstein SD. Episodic and chronic migraine headache: breaking down barriers to optimal treatment and prevention. Headache. (2015) 55:103–22. doi: 10.1111/head.12505_2
11. Tfelt-Hansen P, Olesen J. Taking the negative view of current migraine treatments: the unmet needs. CNS Drugs. (2012) 26:375–82. doi: 10.2165/11630590-000000000-00000
12. Buse DC, Rupnow MF, Lipton RB. Assessing and managing all aspects of migraine: migraine attacks, migraine-related functional impairment, common comorbidities, and quality of life. Mayo Clin Proc. (2009) 84:422–35. doi: 10.1016/S0025-6196(11)60561-2
13. Matsumori Y, Ueda K, Komori M, Zagar AJ, Kim Y, Jaffe DH, et al. Burden of migraine in Japan: results of the observational survey of the epidemiology, treatment, and care of migraine (overcome [Japan]) study. Neurol Ther. (2022) 11:205–22. doi: 10.1007/s40120-021-00305-9
14. Headache Classification Committee of the International Headache Society. (Ihs) The International Classification of Headache Disorders. Cephalalgia. (2018) 38:1–211. doi: 10.1177/0333102417738202
15. Lipton RB, Dodick D, Sadovsky R, Kolodner K, Endicott J, Hettiarachchi J, et al. A self-administered screener for migraine in primary care: the id migraine validation study. Neurology. (2003) 61:375–82. doi: 10.1212/01.WNL.0000078940.53438.83
16. Takeshima T. A simple migraine screening instrument: validation study in Japan. Jap J Headache. (2015) 42:134–43.
17. Benchimol EI, Manuel DG, To T, Griffiths AM, Rabeneck L, Guttmann A. Development and use of reporting guidelines for assessing the quality of validation studies of health administrative data. J Clin Epidemiol. (2011) 64:821–9. doi: 10.1016/j.jclinepi.2010.10.006
18. van Walraven C, Austin P. Administrative database research has unique characteristics that can risk biased results. J Clin Epidemiol. (2012) 65:126–31. doi: 10.1016/j.jclinepi.2011.08.002
19. Funk MJ, Landi SN. Misclassification in administrative claims data: quantifying the impact on treatment effect estimates. Curr Epidemiol Rep. (2014) 1:175–85. doi: 10.1007/s40471-014-0027-z
20. Khan NF, Harrison SE, Rose PW. Validity of diagnostic coding within the general practice research database: a systematic review. Br J Gen Pract. (2010) 60:e128–36. doi: 10.3399/bjgp10X483562
21. McBrien KA, Souri S, Symonds NE, Rouhi A, Lethebe BC, Williamson TS, et al. Identification of validated case definitions for medical conditions used in primary care electronic medical record databases: a systematic review. J Am Med Inform Assoc. (2018) 25:1567–78. doi: 10.1093/jamia/ocy094
22. Pavlovic JM Yu JS, Silberstein SD, Reed ML, Kawahara SH, Cowan RP, et al. Development of a claims-based algorithm to identify potentially undiagnosed chronic migraine patients. Cephalalgia. (2019) 39:465–76. doi: 10.1177/0333102418825373
23. Sakai F, Hirata K, Igarashi H, Takeshima T, Nakayama T, Sano H, et al. A study to investigate the prevalence of headache disorders and migraine among people registered in a health insurance association in Japan. J Headache Pain. (2022) 23:70. doi: 10.1186/s10194-022-01529-2
24. Hamaya R, Fukuda H, Takebayashi M, Mori M, Matsushima R, Nakano K, et al. Effects of an Mhealth App (Kencom) with integrated functions for healthy lifestyles on physical activity levels and cardiovascular risk biomarkers: observational study of 12,602 users. J Med Internet Res. (2021) 23:e21622. doi: 10.2196/21622
25. Headache Clinical Practice Guideline Development Committee. Clinical Practice Guideline for Headache. Tokyo: Igaku-Shoin (2021).
26. Iwagami M, Aoki K, Akazawa M, Ishiguro C, Imai S, Ooba N, et al. Task force report on the validation of diagnosis codes and other outcome definitions in the Japanese receipt data. Jap J Pharmacoepidemiol. (2018) 21:95–123. doi: 10.3820/jjpe.23.95
27. Takeshima T, Ishizaki K, Fukuhara Y, Ijiri T, Kusumi M, Wakutani Y, et al. Population-based door-to-door survey of migraine in Japan: the daisen study. Headache. (2004) 44:8–19. doi: 10.1111/j.1526-4610.2004.04004.x
28. Takeshima T, Wan Q, Zhang Y, Komori M, Stretton S, Rajan N, et al. Prevalence, burden, and clinical management of migraine in China, Japan, and South Korea: a comprehensive review of the literature. J Headache Pain. (2019) 20:111. doi: 10.1186/s10194-019-1062-4
29. Burch R, Rizzoli P, Loder E. The prevalence and impact of migraine and severe headache in the united states: figures and trends from government health studies. Headache. (2018) 58:496–505. doi: 10.1111/head.13281
Keywords: migraine, primary headache, predictive value, survey, claims data
Citation: Yamato K, Sano H, Hirata K and Nakayama T (2023) Validation and comparison of the coding algorithms to identify people with migraine using Japanese claims data. Front. Neurol. 14:1231351. doi: 10.3389/fneur.2023.1231351
Received: 30 May 2023; Accepted: 30 October 2023;
Published: 27 November 2023.
Edited by:
Raffaele Ornello, University of L'Aquila, ItalyReviewed by:
Edina Szabo, Beth Israel Deaconess Medical Center and Harvard Medical School, United StatesCopyright © 2023 Yamato, Sano, Hirata and Nakayama. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kentaro Yamato, WWFtYXRvLktlbnRhcm9Ab3RzdWthLmpw
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.