
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Neurol. , 15 September 2023
Sec. Neurotrauma
Volume 14 - 2023 | https://doi.org/10.3389/fneur.2023.1220598
This article is part of the Research Topic Myelopathies and spinal cord injuries: advances and controversies in pathophysiology, diagnosis, and treatment View all 7 articles
 Mary Solou1*
Mary Solou1* Anastasios A. Politis1
Anastasios A. Politis1 Ιoannis Ydreos1
Ιoannis Ydreos1 Evangelos K. Papadopoulos1
Evangelos K. Papadopoulos1 Stamatios Banos1
Stamatios Banos1 Georgios Savvanis1
Georgios Savvanis1 Maria M. Gavra2
Maria M. Gavra2 Efstathios J. Boviatsis1
Efstathios J. Boviatsis1 Lampis C. Stavrinou1
Lampis C. Stavrinou1Background: Spinal cord injury (SCI) can be caused by a variety of factors and its severity can range from a mild concussion to a complete severing of the spinal cord. Τreatment depends on the type and severity of injury, the patient’s age and overall health. Reduction of dislocated or fractured vertebrae via closed manipulation or surgical procedures, fixation and removal of bony fragments and debris that compromise the spinal canal are indicated for decompression of the spinal cord and stabilization of the spine. However, when there is no obvious traumatic obstruction of spinal canal, the question arises as to whether laminectomy is needed to be performed to improve neurological outcome.
Methods: A literature review covering all indexed studies published between 2013 and 2023 was performed using keywords to identify the patient group of interest (spinal cord injury, SCI, spinal cord trauma, cervical, thoracic, lumbar, thoracolumbar),central cord syndrome (CCS) and the interventions (laminectomy, laminoplasty, decompression, duroplasty).
Results: This review includes6 observational studies investigating the outcome of posterior spinal decompression in patients suffering from spinal cord injury without traumatic spinal cord stenosis. Most patients already had degenerative stenosis. From a total of 202, 151 patients (74.7%) improved neurologically by at least one grade at ASIA scale, after being treated with either laminectomy, laminoplasty, duroplasty or a combination of these techniques.
Conclusion: Early decompression in SCI patients remains a reasonable practice option and can be performed safely, but no specific evidence supports the use of laminectomy alone. There is emerging evidence that intended durotomy followed by extended meningoplasty may improve the neurological outcome in patients suffering from SCI when meta-traumatic edema is apparent. However, the lack of high-quality evidence and results support the need for further research.
Spinal cord injury (SCI) can be caused by a variety of mechanisms, such as falls from height, car accidents, sports injuries, or violence, and has a devastating impact on the quality of life of the affected patients and their caregivers. The severity of the injury can range from a mild concussion to a complete severing of the spinal cord with an increased risk of permanent disability and considerable socio-economic impact (1). Studies have shown that timely and safe transport and diagnosis by healthcare professionals in the acute post-traumatic phase can reduce morbidity and mortality significantly (2). Improving the neurological and clinical outcome remains a challenge and timely treatment seems to be critical (3). Critical care management is based on intensive hemodynamic monitoring and spine immobilization (1). It seems logical and apparent to recommend surgery in cases of spinal instability or persistent spinal cord compression (4). Reduction to restore the spinal alignment may be performed via closed manipulation or surgically, depending on the type of injury. Additional decompression to relieve the pressure on the spinal cord may be needed, by removing any bony fragments and debris that have entered the spinal canal. On the other hand, there are cases of spinal cord injury without fracture or dislocation apparent in imaging scans. This is usually seen in young and middle-aged trauma patients (1, 5). In cases of cervical SCI, this kind of population accounts for about 45% of all cases. Central cord syndrome (CCS) is the most common type of incomplete spinal cord injury. The common setting of CCS without apparent osteoligamentous injury appears to be the closest analog of SCI without compromise of the spinal canal in adults (6). After the primary insult, a plethora of secondary events occur, with progressive edema and hemorrhage predominating and possibly being the cause of spinal cord compression (5, 6). Treatment of such patients may be surgical or conservative depending on the type, the severity of injury, and the clinical status of the patient (7, 8). For instance, in cervical spine injury without bone or disk involvement, some advocate conservative treatment while others feel a more aggressive approach is warranted (9). Consensus on the management of SCI-free of fractures and spine dislocation has not been established yet.
The majority of studies examine the importance of early decompression after traumatic spinal cord injury, comparing surgical intervention in different time frames in an attempt to identify the optimal time for surgical intervention. Early decompression and stabilization seem to yield the best results, but the decision should be individualized (3, 7). While there are various studies examining the effect of decompression after SCI in different animal models that have shown promising neurological results, little evidence exists on the management of patients with SCI without obvious obstruction of the spinal canal.
Surgical decompression aims to relieve the cause of the compression, thereby reducing secondary hypoxia and ischemia, potentially resulting in a better neurological outcome (3, 5). While arguing on the safety and effectiveness of decompression surgery, a specific question arises as to whether laminectomy is needed to improve neurological outcome in such SCI patients free of spinal obstruction. The purpose of this study is to review the literature on studies investigating the management of adult SCI patients without apparent traumatic stenosis of the spinal canal and to evaluate whether laminectomy is beneficial for improving the neurological outcome in such cases.
To examine the effect of laminectomy on neurological outcome following spinal cord injury after closed or surgical reduction and without any obvious traumatic obstruction of the spinal canal, a literature review was performed. This manuscript was structured in accordance with “The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines” [Supplementary material 1, (10)].
Articles published between January 2013 and March 2023 regarding decompression of the spinal canal in patients with SCI without traumatic compromise of the spinal canal were reviewed using the Pubmed search engine. The following keywords were used to identify this patient group (Supplementary material 2): spinal cord injury, SCI, spinal cord trauma, cervical, thoracic, lumbar, thoracolumbar, central cord syndrome, SCIWORA (Spinal Cord Injury without Radiographic Abnormality), and the interventions (laminectomy, laminoplasty, decompression, duroplasty/meningoplasty, and durotomy). The reference lists of the selected articles were also reviewed.
Included were studies (i) written in English, (ii) had an abstract and full text available, (iii) with a specific study design (meta-analysis, systematic review, randomized controlled study, prospective, and retrospective cohort study, and review-type studies) and referring to a (iv) population of adults (defined as age ≥ 18 years old), (v) undergoing decompression of spinal cord for SCI after being treated with closed or surgical reduction, and (vi) without any obvious traumatic stenosis of the spinal canal -no vertebrae fracture or dislocation compressing the spinal cord. Patients with prior degenerative spinal canal stenosis were included. From the study were excluded studies (i) referring to spine injury with traumatic canal stenosis, (ii) with only abstract available, (iii) animal and lab studies, (iv) case reports, (v) pediatric population studies, (vi) papers published in other than English language, and (vii) published prior to 2013.
The selection of study items followed a double-reviewer process. The records identified in Pubmed using date filters (01/2013–03/2023) and the foretold keywords were checked for duplicates. Then, articles were screened according to the selection criteria mentioned above using Rayyan online platform (11). The retrieved papers were examined in full for eligibility. The final list of articles included some studies from the respective reference lists. After articles were selected for inclusion, we reviewed the characteristics of each study and collected the relevant data.
Laminectomy is a surgical procedure that creates space in the spinal canal by removing part or all of the lamina of one or more spine vertebrae. Laminoplasty describes the surgical technique of enlarging the spinal canal by reconstructing the lamina arch and thus propping open the spinal canal. In the context of this review, durotomy is used in conjunction with duroplasty and describes the process of expanding the spinal intradural space by placing or stitching an (autologous or artificial) patch to an opened dura. SCIWORA is the short form of “Spinal Cord Injury without Radiographic Abnormality,” defining the patients experiencing symptoms of posttraumatic spinal cord injury without radiological evidence of fracture or spine malalignment. By referring to traumatic compromise of the spinal cord, we mean a spinal cord injury that causes compression to the spinal cord.
The neurological outcome measured in the ASIA scale after decompression of the spinal canal for SCI was considered as the primary outcome (12). Secondary outcomes included morbidity, mortality, and postoperative complications. All included studies were assessed for the level of evidence and quality, then conflicts were discussed and resolved.
The literature review was structured by analyzing the data from the included studies, comparing the homogenous data between them, and using the online statistics calculator “DATATab” [DATAtab Team (2023). DATAtab: Online Statistics Calculator. DATAtabe.U. Graz, Austria. URL https://datatab.net] for data analysis (13). Tables were created to illustrate more specifically the results of this systematic review. Microsoft® Excel was used for chart making (Microsoft Corporation. Microsoft Excel, 2018. Available from: https://office.microsoft.com/excel).
The search identified 10,506 studies, of which 2,563 were duplicates. From the 7,943 records screened on a title-abstract basis, 2 reports could not be retrieved and 7,213 studies were excluded due to inconsistent research content. From 728 full-text studies being left for eligibility assessment, 722 records not following the inclusion criteria were excluded after a double-reviewer process. In total, this systematic review included 6 observational retrospective or prospective studies (Figure 1).
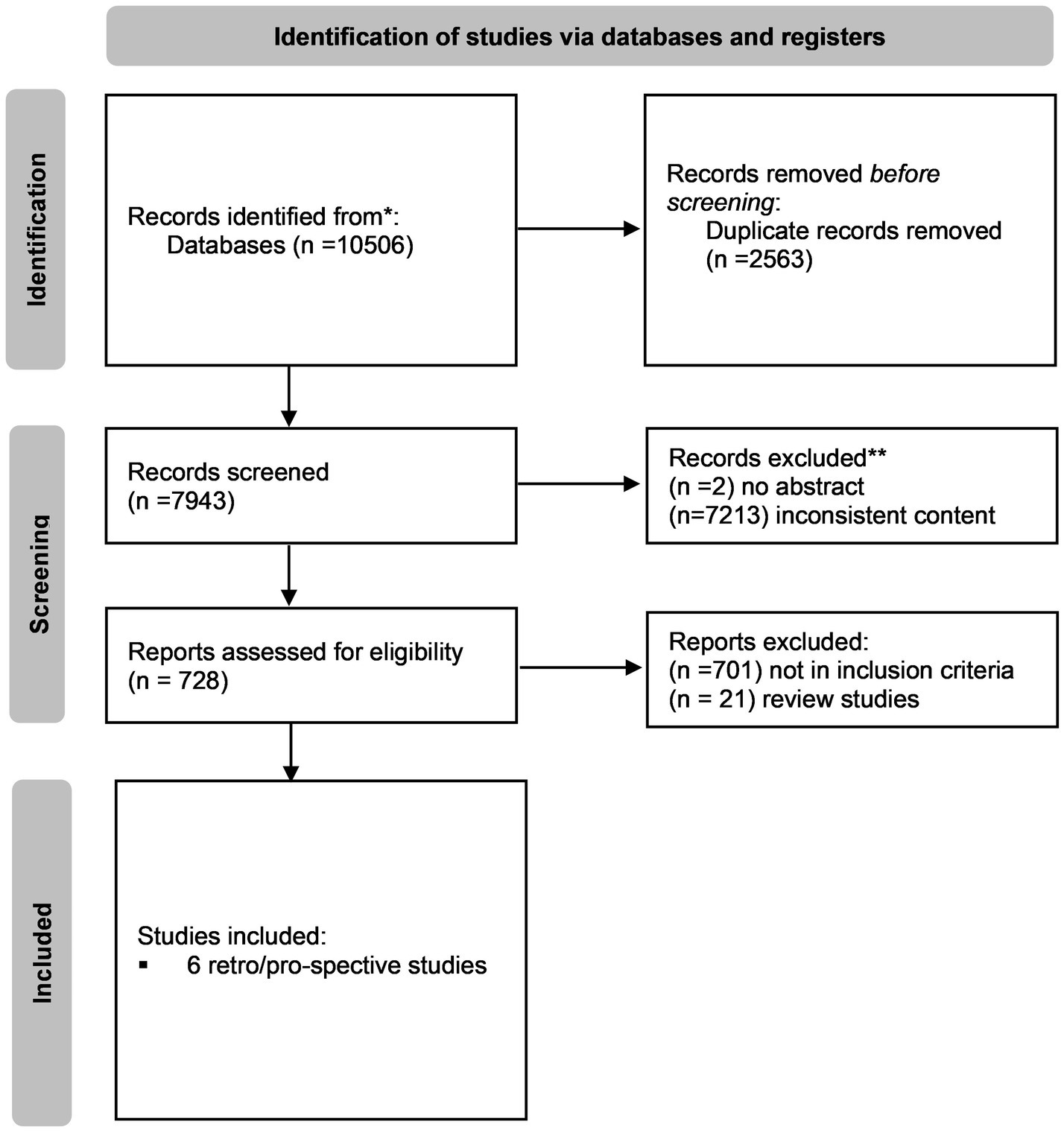
Figure 1. “PRISMA flowchart of selection process” (10).
In this study, data were derived from 6 observational studies investigating the neurological outcome after decompression of the spinal cord in patients with SCI without obvious traumatic spinal canal stenosis – be it fracture, vertebrae dislocation, or disk rupture. The main demographics of the included studies are shown in Table 1. The included studies either investigate the outcome in patients with SCI after laminectomy/laminoplasty/durotomy/duroplasty, or compare such treatment methods between them or to conservative management. In one study, Phang et al., which compares laminectomy alone (intervention arm) to laminectomy with duroplasty (control arm), both patient groups were eligible for our study and therefore we have added both intervention and control arms as separate groups in our study (14). Therefore, Table 1 consists of 7 groups of patients with SCI without traumatic spinal canal stenosis who underwent decompression. While none of the patients included in the studies had obvious traumatic spinal canal stenosis, the majority of the studied population had some degree of degenerative-type spinal stenosis (degenerative intervertebral disk protrusion, spondylosis, ossified posterior longitudinal ligament, etc.).
Our review included 202 patients from 6 observational studies. Regarding the level of injury, 5 out of 6 studies are investigating decompression techniques in cervical SCI, while one of them also incorporates patients with trauma of the thoracic spine. One study did not define the level of injury of its population. The included patients were aged 19 to 82 years old, with an average age of 47.83 ± 10.5 years. The preoperative neurological status graded in the ASIA scale was allocated as follows: 40 patients in the ASIA-A group and 55 cases in ASIA-B. The majority of patients (74 cases) belonged to the ASIA-C group and 32 patients to ASIA D or E (Figure 2). As mentioned before, most patients had degenerative stenosis, accounting for at least 176 out of 202 cases. The follow-up time varied from 3 months to 25.8 months, with an average time to be almost a year after surgery, at 12.31 months.
Neurological improvement as measured by the change in the ASIA grade from the preoperative assessment to the final follow-up visit for the entire patient cohort is presented in Table 1. From a total of 202, 151 patients (74.7%) improved neurologically (at least one grade change in ASIA scale) after being decompressed with one of the techniques of either laminectomy, laminoplasty or duroplasty. In Figure 3, the percentage of neurologically improved patients is illustrated in relation to the studied groups. In 2 out of 7 studies less than 50% of the patients improved neurologically. These are the group of Mazaki et al., treated with laminoplasty and being compared to conservative management, and the group of laminectomy alone of Phang et al. which was compared to a group receiving laminectomy and duroplasty. All other studies show improvement of 50% and more in their included patients. Moreover, Figure 4 presents the ratio of patient improvement based on the operation type as it is categorized into three groups regarding the type of decompression: (1) surgical techniques involving the opening of both lamina and dura, (2) decompression via laminoplasty, and (3) when surgical decompression was limited to laminectomy. Greater improvement is seen when bone decompression is followed by dura opening. The main outcomes of the 6 included studies are presented in Table 2.
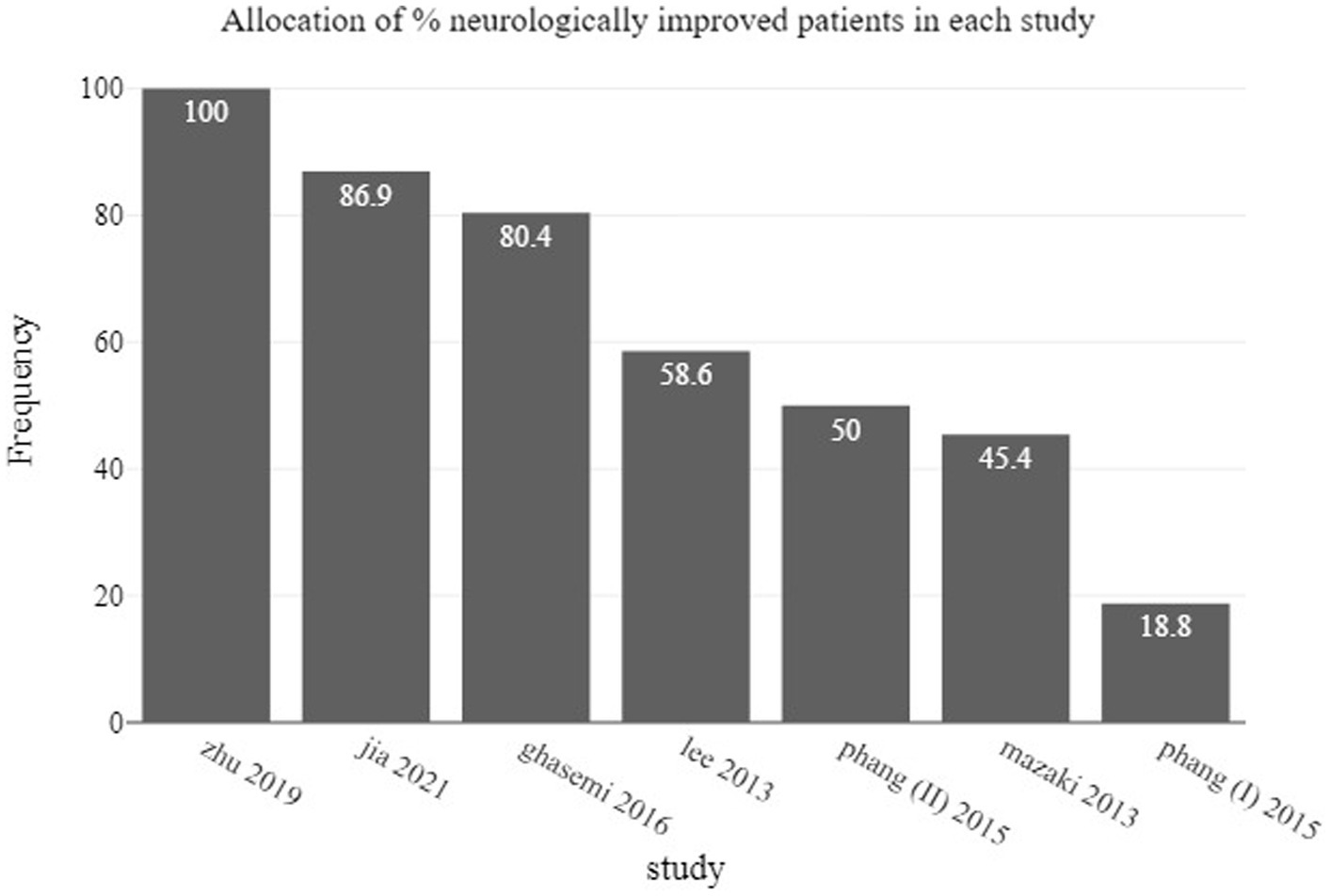
Figure 3. Barchart showing the percentage of neurologically improved patients as allocated in studied groups.
This study included 202 patients from 6 observational studies divided in 7 groups and showed a trend towards a beneficial effect of decompression of the spinal cord in patients suffering from SCI, especially in cervical spine, even in the setting of an uncompromised spinal canal. Nevertheless, the literature is still inconclusive and one should be cautious before formulating practice recommendations.
The role of the spinal meninges in spinal cord trauma is not fully understood. Certain assumptions derive from the management of traumatic brain injury (TBI): the composition of cell types in the brain parenchyma and the spinal cord is similar and thus they share common pathogenetic mechanisms in an injury. It is well known that after brain injury, the brain swells against the non-expansile dura and skull, with ICP to be increased when the compensatory mechanisms fail. Spinal cord swelling against the dura after SCI may be blamed for the compression by raising the intra-spinal pressure (ISP) and reducing the perfusion of spinal cord (15). Many describe the compression of spinal cord in SCI without bone involvement as a “compartment-like” syndrome caused by the restriction of the cord within the dura. Therefore, removing bony and dural restrictions through laminectomy/laminoplasty and expansion duroplasty in cases of SCI is regarded as the decompressive craniectomy for TBI (15, 16). Along the same line, monitoring has been evolved significantly lately and thus the intra-spinal pressure may be recorded by implanting an intradural extramedullary pressure transducer at the injury site. This seems to be of use in the decision-making for the management of SCI (15).
Ghasemi et al. and Lee et al. studied the effect of laminoplasty and both studies concluded that laminoplasty offers neurological improvement in patients with SCI with uncompromised spinal canal (1, 8). The authors report that better outcome is observed in patients having less than 50% compression of the spinal cord due to degenerative causes (8). In their review, Zhu et al. state that adequate decompression of the spinal cord in reasonable timing can eliminate the associated secondary injury, especially in patients with incomplete injury (3). Additionally, in cases of acute traumatic central cord syndrome (ATCCS), previous studies advocated management similar to cervical myelopathy, with emergent surgery to be proposed in cases of progressive neurological deficits or moderate–severe ATCCS (17). Adequately decompressed patients with ATCCS are reported to have a better prognosis (18). Surgical decompression acts also beneficially to prevent repetitive trauma to the spinal cord by secondary mechanisms which may have led to the deterioration (19). Malliqaj et al. state that there is class III evidence suggesting no difference in outcome between anterior or posterior approach. Similarly, laminoplasty and laminectomy appear equivalent as far as neurological outcome is concerned (17). In the study of Jia et al. comparing 164 patients with acute central cord syndrome who underwent either the anterior cervical discectomy or posterior cervical laminectomy, the authors found similar results between the two approaches, with a slight superiority of the laminectomy technique (6). A more recent retrospective study by Yang et al. regarding the management of patients with SCI also suggests that traumatic edema of the spinal cord is better resolved when an early laminoplasty is performed (20). Lastly, thoracic and lumbar spinal cord injury has not been adequately discussed in the literature and the relation between laminectomy/laminoplasty and neurological outcome is unknown (21).
Literature suggests that in many cases of spinal cord injury, the compression cause involves the dura, hence decompression of the bony spinal canal alone may not alleviate the pressure on the injured spinal cord (22). Saadoun et al. suggest that this happens in more than a quarter of patients. They investigated 21 patients and concluded that compared to laminectomy alone, bony decompression followed by duroplasty adequately widens the dural tube, relieves the intraspinal pressure, and improves cord perfusion, thus improving neurological outcome (22). This could offer a possible explanation as to why studies with only bony decompression have not convincingly benefited the outcome (14). Similarly, the study of Phang et al., with the privilege of comparing laminectomy-alone versus laminectomy followed by duroplasty, showed that both methods can improve the ASIA score in SCI patients, but duroplasty gives better results in radiological and physiological parameters by expanding the space around the injured spinal cord, reducing ISP (intra-spinal pressure) and increasing SCPP (spinal cord perfusion pressure) (14). Being one of the few studies which included patients with thoracic SCI, it is important to mention that in complete thoracic injury cases (ASIA A), the decompression did not result in any improvement, while some of the patients with complete cervical injury appeared to recover substantially after decompression of spinal cord (14). In their review article, Grassner et al. recommend early surgical decompression and blood pressure augmentation after traumatic SCI. The authors argue that increased intraspinal pressure should be estimated as well, in line with the most recent studies that support a beneficial effect of intentional durotomy in elevating the perfusion pressure of the spinal cord (23). Grassner et al. also note that in small duroplasties, the swollen spinal cord can be restricted at the dural edges while the edema expands, similar to an inadequate craniectomy. On the other hand, larger duroplasties are more commonly associated with complications and require wider laminectomies and potentially fusion procedures (23). Complications may be CSF leakage, pseudomeningoceles, and increased hospitalization time (23). Αcurrently running RCT termed DISCUS (Duroplasty for Injured cervical Spinal Cord with Uncontrolled Swelling) aims to test whether expansion duroplasty after bony decompression improves outcome compared with bony decompression alone in patients with cervical SCI (15).
A number of studies advocate conservative treatment, reserving surgery for cases with instability and obvious compression of the spinal cord (24–26). Atesok et al. support that cases of SCI with normal MRI scans or intraneural findings like edema or contusion -but without compression- should be managed conservatively (27). Surgery is reserved for patients with ligamentous injury, instability, or spinal cord compression in MRI images, along with deterioration or not-improving neurological status (27). Similarly, Rouanet et al. highlight that operative management is only indicated in substantial compression of the spinal cord with deterioration of neurological deficits (7). A2018 study by Wagner et al. favored surgery for patients with spinal column instability or persistent compression of the spinal cord after traumatic CCS without any neurologic improvement (Level B of recommendation) (4). Some studies claim that in patients with intact spinal canal, conservative treatment is preferred, regardless of the neurologic status, and only in neurologic deterioration cases isa prompt decompression warranted (4, 28). However, in a study by Qin et al. comparing conservative treatment and early and delayed surgery in patients with acute traumatic central cord syndrome without fracture or dislocation, no significant difference in neurological recovery was reported among the therapeutic approaches (29). Only when early decompression is performed, patients were found to experience faster motor function recovery (29). Similarly, another study by Khorasanizadeh et al. showed that neurologic deficit improvement is independent of the treatment choice-conservative versus surgical-but noted that the mechanism and characteristics of injury may affect the outcome (30). Some studies support that even in cases where patients were treated conservatively at first with continuous neurological improvement, delayed surgery may still be beneficial (4). In any case, the improvement of neurologic deficits post-operatively seems unpredictable (4).
Studies arguing against surgery focus not only on negative outcome results but also on the inherent risks of surgery. Mazaki et al. state that there is no significant difference in outcome comparing laminoplasty to conservative treatment, with surgery being associated with a higher frequency of complications (9). In their review, Atesok et al. refer that for SCIWORA patients with normal or pure intraneural MRI findings surgery is not recommended, no matter their neurological status (27). Possible complications of spinal canal decompression may be dural tear and subsequent CSF-leakage, nerve root palsy, wound infection, CNS infection, pneumonia and respiratory failure, thromboembolic events, cardiac arrest, or death (4, 20, 31). The complication and morbidity rates should be taken into account together with the previously mentioned negative results (i.e., results showing no benefit of surgery over conservative treatment) when choosing the optimal treatment for a patient, especially when treating older patients or patients with comorbidities.
Although we did include SCWIORA in our search algorithm, we tried to avoid the term in our manuscript for several reasons: Firstly, we feel that the term itself is rather outdated; it refers mainly to the absence of radiographic abnormality (no radiographic or computed tomographic features of spinal fracture or instability as per the original paper by Paul and Wilberger) and in the modern era of widespread MRI-availability it is rather unusual to have clinical signs of spinal cord trauma without any radiographic evidence of injury. Secondly, the term has a strong connotation to spinal injuries in children (32). Adults who have spinal cord injury without computed tomographic evidence of trauma have CT-scans showing canal stenosis and significant degenerative changes in the cervical spine; thus, it is not accurate to state that they have SCIWORA (33).
A limitation of this study is the limited number of eligible studies included and thus the restricted sample size for data extraction and result forming. This limits our ability to detect potential associations that may be statistically significant in our analysis. Moreover, the various types of surgical treatments used in each individual study were categorized into techniques of lamina- or dura- decompression in order to summarize our results. Most papers investigate cervical spinal cord injury and thus, studies for patients with thoracic or lumbar spine injuries are missing. Finally, it should be noted that the majority of the studied population consists of patients having additionally some degree of degenerative-type spinal stenosis (intervertebral disk, spondylosis, ossified posterior longitudinal ligament etc.), and thus there are no formal results regarding cases with fully uncompressed spinal canal.
In our review, the majority of studies found that decompression of the spinal canal improves post-operative ASIA grade. The amount of data, however, is scarce and one should be cautious to interpret these results as more than a trend favoring decompression after spinal cord injury, even in the absence of traumatic compromise of the spinal canal. Ultimately, the type of surgical approach may not be the defining factor, provided that the approach itself generates an environment within the spinal canal able to mitigate or alleviate secondary injury to the spinal cord.
There is no clear consensus on the management of spinal cord injuries without apparent traumatic obstruction of spinal canal. Increasing evidence suggests that osseous decompression and restoration of the spinal alignment may not be sufficient to adequately address intraspinal pathogenetic cascades, thus leading surgeons to intervene by opening the dura and further releasing the spinal cord. The potential drawback of this approach is longer operative times and a higher complication rate. While in literature there seems to be a trend towards surgery, further research is necessary to more clearly define the surgical indications and evaluate the benefit of bony and dura decompression in neurological outcome.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
MS and LS: conceptualization and formal Analysis. MS, LS, and EB: methodology. MS, LS, IY, AP, MG, EP, SB, and GS: investigation. LS: supervision. LS and MG: manuscript editing. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2023.1220598/full#supplementary-material
1. Lee, HJ, Kim, HS, Nam, KH, Han, IH, Cho, WH, and Choi, BK. Neurologic outcome of laminoplasty for acute traumatic spinal cord injury without instability. Korean J Spine. (2013) 10:133–7. doi: 10.14245/kjs.2013.10.3.133
2. Wang, TY, Park, C, Zhang, H, Rahimpour, S, Murphy, KR, Goodwin, CR, et al. Management of acute traumatic spinal cord injury: a review of the literature. Front Surg. (2021) 8:698736. doi: 10.3389/fsurg.2021.698736
3. Zhu, YK, Lu, FT, Zhang, GD, and Liu, ZP. A review of strategies associated with surgical decompression in traumatic spinal cord injury. J Neurol Surg A Cent Eur Neurosurg. (2023). [Epub ahead of print]. doi: 10.1055/a-1811-8201
4. Wagner, PJ, CP, DP, Connolly, PJ, and Stauff, MP. Controversies in the management of central cord syndrome: the state of the art. J Bone Joint Surg AM. (2018) 100:618–26. doi: 10.2106/JBJS.17.00811
5. Zhu, F, Yao, S, Ren, Z, Telemacque, D, Qu, Y, Chen, K, et al. Early durotomy with duroplasty for severe adult spinal cord injury without radiographic abnormality: a novel concept and method of surgical decompression. Eur Spine. (2019) 28:2275–82. doi: 10.1007/s00586-019-06091-1
6. Jia, Y, Zuo, X, Zhang, Y, Yao, Y, Yin, Y, and Yang, X. Effectiveness of different surgical methods in the treatment of acute central cord syndrome without fractures and dislocations of the cervical spine. J Back Musculoskelet Rehabil. (2023) 36:71–7. doi: 10.3233/BMR-210377
7. Rouanet, C, Reges, D, Rocha, E, Gagliardi, V, and Silva, GS. Traumatic spinal cord injury: current concepts and treatment update. Arq Neuropsiquiatr. (2017) 75:387–93. doi: 10.1590/0004-282X20170048
8. Ghasemi, AA, and Behfar, B. Outcome of laminoplasty in cervical spinal cord injury with stable spine. Asian J Neurosurg. (2016) 11:282–6. doi: 10.4103/1793-5482.175638
9. Mazaki, T, Ito, Y, Sugimoto, Y, Koshimune, K, Tanaka, M, and Ozaki, T. Does laminoplasty really improve neurological status in patients with cervical spinal cord injury without bone and disc injury? A prospective study about neurological recovery and early complications. Arch Orthop Trauma Surg. (2013) 133:1401–5. doi: 10.1007/s00402-013-1810-x
10. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. Statement: an updated guideline for reporting systematic reviews. BMJ. (2020) 372:372. doi: 10.1136/bmj.n71
11. Mourad, O, Hammady, H, Fedorowicz, Z, and Elmagarmid, A. Rayyan — a web and mobile app for systematic reviews. Syst Rev. (2016) 5:5–210. doi: 10.1186/s13643-016-0384-4
12. Roberts, TT, Leonard, GR, and Cepela, DJ. Classifications in brief: American spinal injury association (ASIA) impairment scale. Clin Orthop Relat Res. (2017) 475:1499–504. doi: 10.1007/s11999-016-5133-4
14. Phang, I, Werndle, MC, Saadoun, S, Varsos, G, Czosnyka, M, Zoumprouli, A, et al. Expansion duroplasty improves intraspinal pressure, spinal cord perfusion pressure, and vascular pressure reactivity index in patients with traumatic spinal cord injury: injured spinal cord pressure evaluation study. J Neurotrauma. (2015) 32:865–74. doi: 10.1089/neu.2014.3668
15. Saadoun, S, and Papadopoulos, MC. Acute, severe traumatic spinal cord injury: monitoring from the injury site and expansion duraplasty. Neurosurg Clin N Am. (2021) 32:365–76. doi: 10.1016/j.nec.2021.03.008
16. Saadoun, S, and Jeffery, ND. Acute traumatic spinal cord injury in humans, dogs, and other mammals: the under-appreciated role of the dura. Front Neurol. (2021) 12:629445. doi: 10.3389/fneur.2021.629445
17. Molliqaj, G, Payer, M, Schaller, K, and Tessitore, E. Acute traumatic central cord syndrome: a comprehensive review. Neurochirurgie. (2014) 60:5–11. doi: 10.1016/j.neuchi.2013.12.002
18. Tosic, L, Voglis, S, Bellut, D, Sprengel, K, Regli, L, and Stienen, MN. Acute traumatic central cord syndrome: etiology, pathophysiology, clinical manifestation, and treatment. Praxis. (2021) 110:324–35. doi: 10.1024/1661-8157/a003659
19. Lee, D-Y, Park, Y-J, Song, S-Y, Hwang, S-C, Kim, K-T, and Kim, D-H. The importance of early surgical decompression for acute traumatic spinal cord injury. Clin Orthop Surg. (2018) 10:448–54. doi: 10.4055/cios.2018.10.4.448
20. Yang, C, Wang, Q, Xu, S, Guan, C, Li, G, and Wang, G. Early expansive single sided laminoplasty decompression treatment severe traumatic cervical spinal cord injury. Front Surg. (2022) 9:984899. doi: 10.3389/fsurg.2022.984899
21. Charles, YP, and Steib, J-P. Management of thoracolumbar spine fractures with neurologic disorder. Orthop Traumatol Surg Res. (2015) 101:S31–40. doi: 10.1016/j.otsr.2014.06.024
22. Saadoun, S, Werndle, MC, Lopez de Heredia, L, and Papadopoulos, MC. The dura causes spinal cord compression after spinal cord injury. Br J Neurosurg. (2016) 30:582–4. doi: 10.3109/02688697.2016.1173191
23. Grassner, L, Grillhösl, A, Griessenauer, CJ, Thome, C, Bühren, V, Strowitzki, M, et al. Spinal meninges and their role in spinal cord injury: a neuroanatomical review. J Neurotrauma. (2018) 35:403–10. doi: 10.1089/neu.2017.5215
24. Martinez-Perez, R, Munarriz, PM, Paredes, I, Cotrina, J, and Lagares, A. Cervical spinal cord injury without computed tomography evidence of trauma in adults: magnetic resonance imaging prognostic factors. World Neurosurg. (2017) 99:192–9. doi: 10.1016/j.wneu.2016.12.005
25. Liu, Q, Liu, Q, Zhao, J, Yu, H, Ma, X, and Wang, L. Early MRI finding in adult spinal cord injury without radiologic abnormalities does not correlate with the neurological outcome: a retrospective study. Spinal Cord. (2015) 53:750–3. doi: 10.1038/sc.2015.45
26. Ouchida, J, Yukawa, Y, Ito, K, Katayama, Y, Matsumoto, T, Machino, M, et al. Delayed magnetic resonance imaging in patients with cervical spinal cord injury without radiographic abnormality. Spine (Phila Pa 1976). (2016) 41:E981–6. doi: 10.1097/BRS.0000000000001505
27. Atesok, K, Tanaka, N, O’Brien, A, Robinson, Y, Pang, D, Deinlein, D, et al. Posttraumatic spinal cord injury without radiographic abnormality. Adv Orthop. (2018) 2018:7060654–10. doi: 10.1155/2018/7060654
28. Jin, W, Sun, X, Shen, K, Wang, J, Liu, X, Shang, X, et al. Recurrent neurological deterioration after conservative treatment for acute traumatic central cord syndrome without bony injury: seventeen operative case reports. J Neurotrauma. (2017) 34:3051–7. doi: 10.1089/neu.2016.4706
29. Qin, C, Liu, B, Wang, Y, Su, J, and Zhang, Y. Impact of timing of surgery on traumatic central cord syndrome without fracture or dislocation. Interdiscip Neurosurg. (2022) 28:101507. doi: 10.1016/j.inat.2022.101507
30. Khorasanizadeh, M, Yousefifard, M, Eskian, M, Lu, Y, Chalangari, M, Harrop, JS, et al. Neurological recovery following traumatic spinal cord injury: a systematic review and meta-analysis. J Neurosurg Spine. (2019) 30:683–99. doi: 10.3171/2018.10.SPINE18802
31. Du, L, Gao, Y, Zhao, C, Zhou, T, Tian, H, Zhang, K, et al. Laminoplasty with selective fusion at unstable segment versus laminectomy with fusion for multilevel cervical myelopathy: a case-control study. BMC Musculoskelet Disord. (2021) 22:426. doi: 10.1186/s12891-021-04297-3
32. Szwedowski, D, and Walecki, J. Spinal cord injury without radiographic abnormality (SCIWORA) – clinical and radiological aspects. Pol J Radiol. (2014) 79:461–4. doi: 10.12659/PJR.890944
Keywords: spinal cord injury (SCI), SCI, laminectomy, laminoplasty, durotomy, duroplasty
Citation: Solou M, Politis AA, Ydreos &, Papadopoulos EK, Banos S, Savvanis G, Gavra MM, Boviatsis EJ and Stavrinou LC (2023) Posterior spinal decompression in adults with spinal cord injury without traumatic compromise of the spinal canal: what is the data? Front. Neurol. 14:1220598. doi: 10.3389/fneur.2023.1220598
Received: 11 May 2023; Accepted: 26 July 2023;
Published: 15 September 2023.
Edited by:
Colin Chalk, McGill University, CanadaReviewed by:
Lei Wang, Huazhong University of Science and Technology, ChinaCopyright © 2023 Solou, Politis, Ydreos, Papadopoulos, Banos, Savvanis, Gavra, Boviatsis and Stavrinou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mary Solou, bWFyeXNvbG91MDZAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.