
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Neurol. , 13 July 2023
Sec. Endovascular and Interventional Neurology
Volume 14 - 2023 | https://doi.org/10.3389/fneur.2023.1218154
This article is part of the Research Topic Case Reports in Endovascular and Interventional Neurology, volume III - 2023 View all 14 articles
A 64-year-old man presented with headache and dizziness. A vertebrobasilar dissecting aneurysm was identified via computed tomography angiography and high resolution magnetic resonance imaging. Perioperatively, standard oral dual antiplatelet drugs were given. Two flow diverters were telespcoped for endovascular treatment of the aneurysm. Postoperatively, there were no signs of cerebral infarction and no new symptoms. At the 6-month follow-up, digital subtraction angiography showed that the aneurysm was almost completely occluded, with no other complications. This case serves as a reference for using the multiple telescoping flow diverter technique to treat vertebrobasilar dissecting aneurysm.
Surgical treatment of complex intracranial aneurysm is problematic, and endovascular treatment has high rates of complications and recurrence. Using a flow diverter (FD) makes treating this kind of aneurysm simpler and safer (1). The advantages of a flow diverter include low porosity and high metal coverage rates. Some studies, however, report that overlapping flow diverters increase the risks of the endovascular treatment and do not benefit the aneurysm cure rate (2).
It remains inevitable that in cases with large or giant aneurysms with extremely wide necks, or longer spindle-shaped aneurysms, two or more flow diverters must be inserted, through a telescoping technique. Studies that have reported the efficacy and safety of telescoping flow diverters in complex intracranial aneurysms treatment are limited (3, 4).
Here we report the case of a vertebrobasilar dissecting aneurysm treated with a multiple telescoping flow diverter technique, which may serve as a reference for the procedure.
A 64-year-old man visited a local hospital due to headache and dizziness. The head computed tomography angiogram (CTA) showed an aneurysm, and he was referred to our hospital in February 2022.
The patient had a family history of subarachnoid hemorrhage. Digital subtraction angiography revealed a fusiform aneurysm at the left vertebral artery V4 segment to the proximal segment of the basilar artery, with a maximum diameter and length of about 10 and 60 mm, respectively; the right vertebral artery was slender, and the right vertebral artery V4 segment was occluded (Figure 1). High resolution magnetic resonance imaging confirmed that the lesion was vertebrobasilar dissecting aneurysm (Figure 2). Considering the characteristics of the aneurysm, we decided to use a flow diverter for the treatment. Because of the large area of the lesion, a single flow diverter could not completely cover the aneurysm, so two flow diverters were implanted via a telescoping technique.
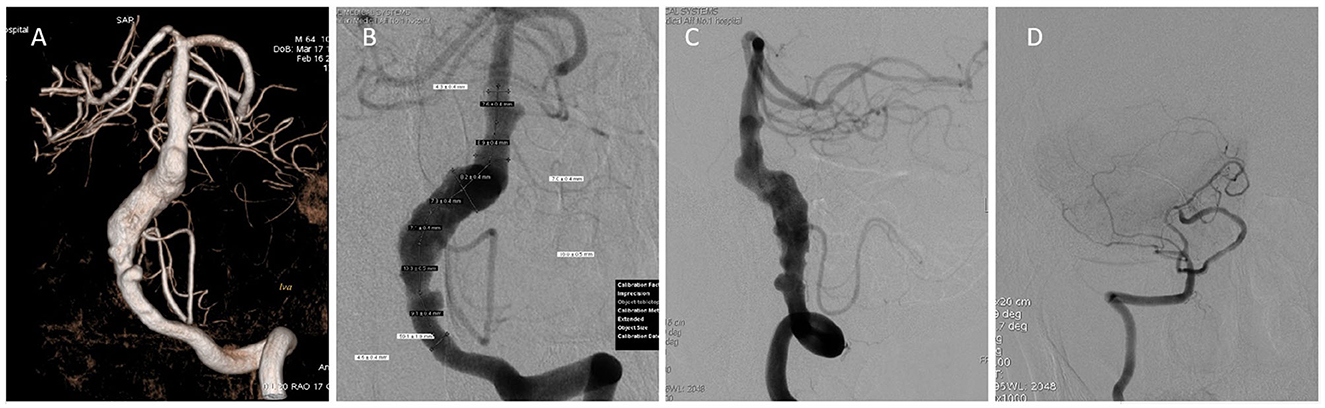
Figure 1. Preoperative angiography. (A) Three-dimensional angiography reveals a vertebrobasilar aneurysm. (B) Anteroposterior angiography measurement data shows the maximum outer diameter and the length of the aneurysm. (C) Lateral angiography reveals a vertebrobasilar aneurysm. (D) Anteroposterior angiography shows a slender right vertebral artery and occulded V4 segment.
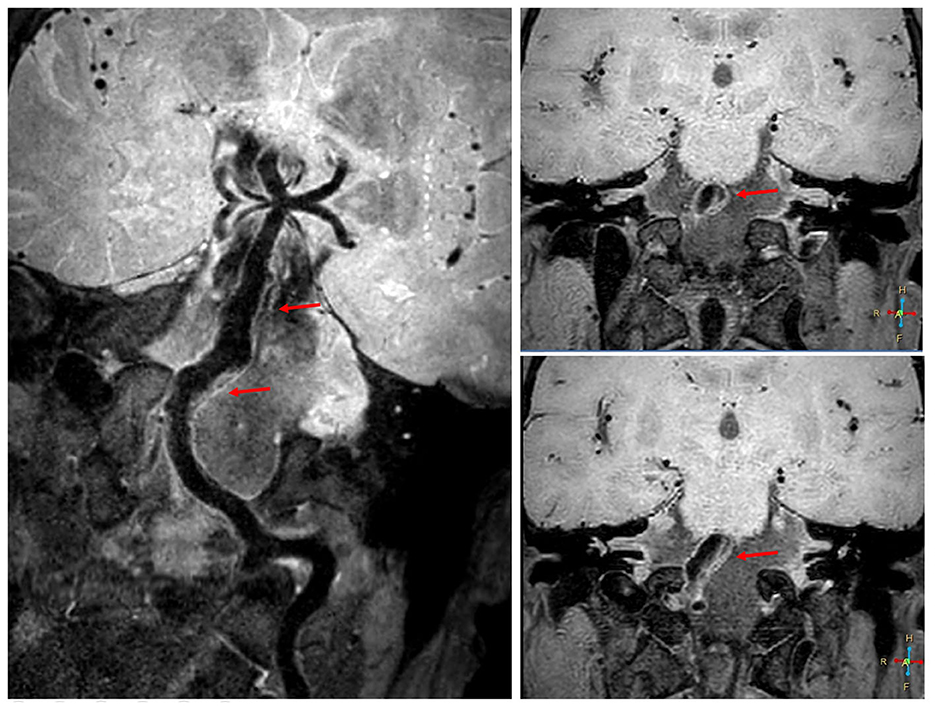
Figure 2. High resolution magnetic resonance imaging before the operation. High resolution magnetic resonance imaging reveals a vertebrobasilar dissecting aneurysm (red arrow).
The patient was administered oral antiplatelet drugs (aspirin 100 mg, and clopidogrel 75 mg, 1×/d) 5 days before the procedure. After 5 days, thromboelastography was performed. The arachidonic acid and adenosine diphosphate inhibition rates were 82 and 48%, respectively. Under general anesthesia, a 6F 90-cm long sheath (Cook, USA) was placed in the left subclavian artery, a 5F 115-cm Navien catheter (Medtronic, USA) was placed in the V3 segment of the left vertebral artery, and a microcatheter (Shanghai MicroPort, China) was inserted into the parent artery.
The first 5.5 × 45 mm Tubridge flow diverter (Shanghai MicroPort, China) was delivered to the head of the aneurysm via the microcatheter. The distal end of the first flow diverter was opened by pulling out the microcatheter, and the location of the distal end of the first flow diverter was determined. The first flow diverter was then slowly released in a push-based manner. After the first flow diverter was totally released, the microcatheter was conveyed to the distal end of the first flow diverter under the guidance of the flow diverter push guidewire. The second Tubridge flow diverter (6.0 × 45 mm) was delivered and opened inside the first, and then released slowly by combining a push and tension-reduction technique. The two flow diverters overlapped by ~25 mm (Figures 3A, B).
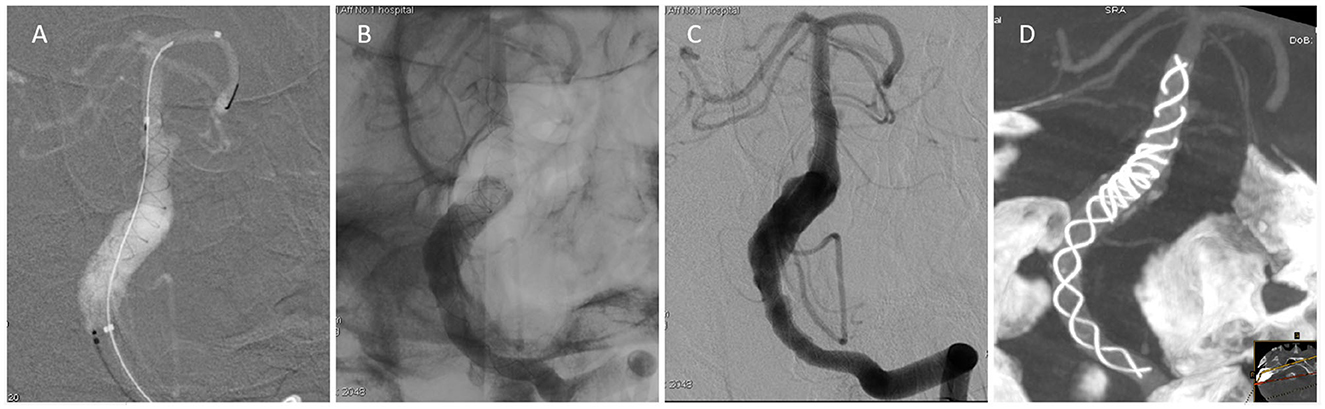
Figure 3. Angiography during the operation. (A) The first flow diverter was released in the distal end of the aneurysm. (B) The second flow diverter was telescoped from the distal to the proximal. (C) Angiography after release of the two flow diverters showed retention of contrast agent in the aneurysm. The parent artery was patent. (D) Postoperative Dyna-CT showed that the two flow diverters were satisfactorily open.
The angiography performed after the release of the flow diverter showed that the contrast agent was obviously retained in the aneurysm and the parent artery was patent [O'Kelly-Marotta (OKM)] grade B (5) (Figure 3C). Dyna computed tomography showed that the patency of the two flow diverters was satisfactory, in good agreement with the parent artery, and the entire lesion was covered (Figure 3D).
There were no signs of cerebral infarction after the operation, and the patient recovered well. He had no new symptoms after discharge and continued to receive dual antiplatelet aggregation therapy for 6 months. Six months after the operation, the follow-up digital subtraction angiography showed that the aneurysm was almost completely occluded, with OKM grade C (Figure 4). The antiplatelet strategy was then changed to aspirin (100 mg, 1×/d) with clinical follow-up.
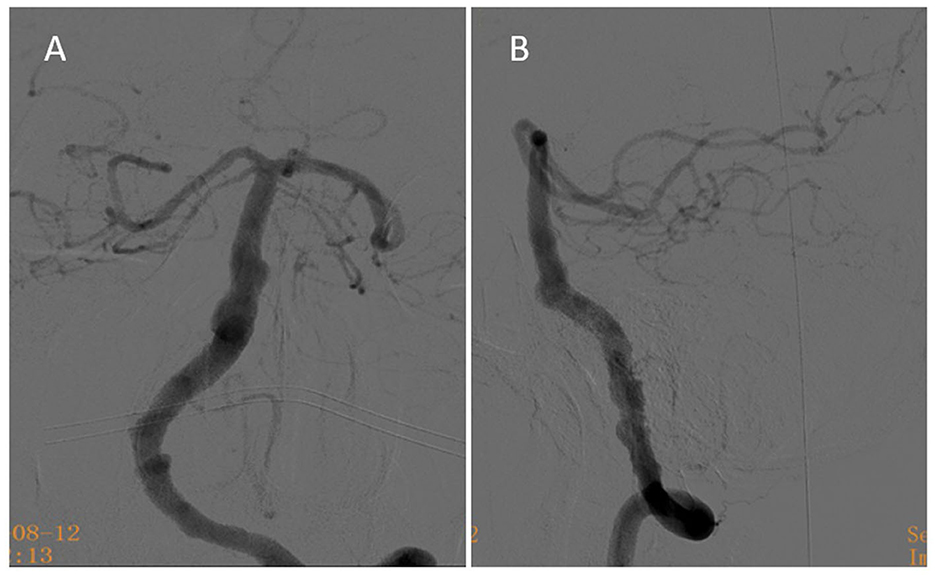
Figure 4. Six-month follow-up angiography. (A) At the 6-month follow-up, anteroposterior angiography showed that the aneurysm was nearly completely occluded. (B) At the 6-month follow-up, lateral angiography reveals the aneurysm was nearly completely occluded.
Numerous clinical studies have reported the safety and efficacy of flow diversion in treating large intracranial and dissecting aneurysms (1, 6, 7). In recent years, flow diversion to treat vertebrobasilar aneurysms has also been applied, although off-label (8, 9). Few studies have evaluated flow diverter telescoping techniques for treating vertebrobasilar aneurysms. Yet, these techniques offer two advantages. First, multiple telescoping flow diverters to treat aneurysm of the neck effect significantly benefit blood flow changes, and promote thrombopoiesis in the aneurysm. Secondly, for large or dissected aneurysms, a single flow diverter is insufficient to cover the diseased vessels; for long-term efficacy, telescoping is required to completely cover the proximal and distal ends of the aneurysm (10).
The flow diverters now commonly used in China include the pipeline embolization device (PED) and Tubridge. The latter is longer; the maximum length is 45 mm. However, the Tubridge is weaker radially and more highly porous compared with the PED, larger aperture in design can reduce the incidence of perforator occlusion events. This is why the Tubridge flow diverter was chosen for the present case.
Dissecting aneurysms in the vertebrobasilar artery have a complex neurovascular anatomy (11). Placement of flow diverters inevitably results in coverage of basilar artery branches and perforators, the occlusion of perforator may be the most common cause of ischemia events (12). Having a perforators of the basilar artery occluded after FD implantation may occur by 2 mechanisms: the profile of the FD mechanically blocks the orifice of the perforators; or tiny thrombi form on the surface of the FD, which are then carried downstream by flowing blood causing perforators embolism. The smallest branching arteries of the basilar trunk are the perforators, which tend to have a diameter in the range of 80 to 940 μm, with a mean value of 400 μm (13). The Tubridge FD is a self-expanding device, it is composed of 46–62 nickel–titanium alloy microfilaments of 35 μm, and the pore size varies between 1,100 and 2,500 μm, depending on the final FD morphology and selection of the proper size adapted to the vessel diameter. The large-size Tubridge (>3.5 mm), which was mostly used in the posterior circulation, has less decreases the shortening rate after its full opening and offers lower pore attenuation (14). Tubridge FD has larger aperture in design, thus decreases the risk of mechanically blocks the perforators. In addition, in the present case, the overlapping area of the two FDs was selected at the proximal segment of the basilar artery with relatively few perforators to increased security.
Rigorous adequate standardized antiplatelet therapy (with reference to the thromboelastogram) can effectively reduce perforators thrombi embolic events. In the present case, the patient had no ischemic events occurred perioperatively. Rigorous testing of platelet function and subsequent regimen adjustments were crucial to minimize the risk of ischemic complications. Despite this, implantation of multiple FDs should be prudent in vertebrobasilar dissecting aneurysm, which helped to reduce thromboembolic complications.
In our patient, the flow diverter was deployed from the aneurysmal distal to the proximal, which is preferable to proximal-to-distal. Firstly, after the release of the first flow diverter, the re-superselection of the microcatheter can be conducted more easily in the channel of the first flow diverter. Secondly, when telescoping from the distal to the proximal aneurism (with reference to the heart), the first flow diverter and the pushing guidewire can be used to support the microcatheter. Compared with telescoping from proximal to distal, the guidewire support is longer, which can support the microcatheter more stably for re-superselection. In addition, it is necessary to ensure that the first flow diverter is firmly anchored in the distal parent artery through distal-to-proximal telescoping.
In this patient, the first flow diverter was anchored about 10 mm in the distal parent artery. A sufficient anchoring length at the distal end is especially important to ensure the stability of the distal flow diverter (15). Studies have confirmed that healing of the aneurysm is promoted when the flow diverter is attached to the wall of the tube after it is implanted. However, attachment is also associated with thrombosis and long-term stenosis and occlusion in the flow diverter itself (16). The telescoping technique may lead to poor adhesion of the flow diverter wall, requiring further treatment.
In the present case, a J-tip guidewire dilation in the flow diverter was performed after the Tubrige implantation to promote adherence of the flow diverter. The present case shows that vertebrobasilar dissecting aneurysm can be treated using telescoping flow diverters. However, we await the long-term results.
This report is evidence that vertebrobasilar dissecting aneurysm can be successfully treated with a telescoping flow diverter technique with two flow diverters, and the treatment is feasible for this type of aneurysm. A prospective randomized study is needed to strengthen the evidence and determine the best conditions for applying flow diverter technology.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by First Affiliated Hospital of Dalian Medical University. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the participant/patient(s) for the publication of this case report.
M-YW and FW performed most of the investigation, data analysis, and wrote the manuscript. Y-SL, X-BA, and TP contributed to interpretation of the data and analyses. All authors have read and approved the manuscript.
We thank Medjaden Inc. for scientific editing of this manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
FD, flow diverter; CTA, Computed tomography angiography; HR-MRI, High resolution magnetic resonance imaging; DSA, Digital subtraction angiography; OKM, O'kelly-Marotta.
1. Becske T, Potts MB, Shapiro M, Kallmes DF, Brinjikji W, Saatci I, et al. Pipeline for uncoilable or failed aneurysms: 3-year follow-up results. J Neurosurg. (2017) 127:81–8. doi: 10.3171/2015.6.JNS15311
2. Chalouhi N, Tjoumakaris S, Phillips JL, Starke RM, Hasan D, Wu C, et al. A single pipeline embolization device is sufficient for treatment of intracranial aneurysms. AJNR Am J Neuroradiol. (2014) 35:1562–6. doi: 10.3174/ajnr.A3957
3. Tonetti DA, Casillo SM, Jankowitz BT. Telescoping flow diverters for a pediatric fusiform distal anterior cerebral artery aneurysm: technical case report. Childs Nerv Syst. (2021) 37:999–1002. doi: 10.1007/s00381-020-04797-y
4. Sun L, Ren J, Ye M, Zhang H. Multiple telescoping flow diverter technique in endovascular treatment of a giant petrous and cavernous carotid aneurysm. World Neurosurg. (2022) 167:7. doi: 10.1016/j.wneu.2022.08.012
5. O'Kelly C J, Krings T, Fiorella D, Marotta TR. A novel grading scale for the angiographic assessment of intracranial aneurysms treated using flow diverting stents. Interv Neuroradiol. (2010) 16:133–7. doi: 10.1177/159101991001600204
6. Griessenauer CJ, Ogilvy CS, Adeeb N, Dmytriw AA, Foreman PM, Shallwani H, et al. Pipeline embolization of posterior circulation aneurysms: a multicenter study of 131 aneurysms. J Neurosurg. (2018) 130:923–35. doi: 10.3171/2017.9.JNS171376
7. Liu JM, Zhou Y, Li Y, Li T, Leng B, Zhang P, et al. Parent artery reconstruction for large or giant cerebral aneurysms using the tubridge flow diverter: a multicenter, randomized, controlled clinical trial (parat). AJNR Am J Neuroradiol. (2018) 39:807–16. doi: 10.3174/ajnr.A5619
8. Bender MT, Colby GP, Jiang B, Lin LM, Campos JK, Xu R, et al. Flow diversion of posterior circulation cerebral aneurysms: a single-institution series of 59 cases. Neurosurgery. (2019) 84:206–16. doi: 10.1093/neuros/nyy076
9. Wallace AN, Madaelil TP, Kamran M, Miller TR, Delgado Almandoz JE, Grossberg JA, et al. Pipeline embolization of vertebrobasilar aneurysms-a multicenter case series. World Neurosurg. (2019) 124:e460–9. doi: 10.1016/j.wneu.2018.12.116
10. Tang H, Shang C, Hua W, Lu Z, Pan J, Wang S, et al. The 8-year single-center experience of telescoping flow diverter for complex intracranial aneurysms treatment. J Clin Neurosci. (2022) 100:131–7. doi: 10.1016/j.jocn.2022.04.014
11. Church EW, Bigder MG, Sussman ES, Gummidipundi SE, Han SS, Heit JJ, et al. Treatment of posterior circulation fusiform aneurysms. J Neurosurg. (2020) 134:1894–900. doi: 10.3171/2020.4.JNS192838
12. Griessenauer CJ, Enriquez-Marulanda A, Taussky P, Biswas A, Grandhi R, Xiang S, et al. Experience with the pipeline embolization device for posterior circulations aneurysms: a multicenter cohort study. Neurosurgery. (2020) 87:1252–61. doi: 10.1093/neuros/nyaa277
13. Marinkovic SV, Gibo H. The surgical anatomy of the perforating branches of the basilar artery. Neurosurgery. (1993) 33:80–7. doi: 10.1227/00006123-199307000-00012
14. Zhou Y, Yang PF, Fang YB, Xu Y, Hong B, Zhao WY, et al. Parent artery reconstruction for large or giant cerebral aneurysms using a Tubridge flow diverter (PARAT): study protocol for a multicenter, randomized, controlled clinical trial. BMC Neurol. (2014) 14:97. doi: 10.1186/1471-2377-14-97
15. Srinivasan VM, Carlson AP, Mokin M, Cherian J, Chen SR, Puri A, et al. Prolapse of the pipeline embolization device in aneurysms: incidence, management, and outcomes. Neurosurg Focus. (2017) 42:E16. doi: 10.3171/2017.3.FOCUS1738
Keywords: flow diverter, telescoping technique, vertebrobasilar, dissecting, aneurysm
Citation: Wang M-Y, Liu Y-S, An X-B, Pan T and Wang F (2023) Multiple telescoping flow diverter technique in endovascular treatment of a vertebrobasilar dissecting aneurysm: case report. Front. Neurol. 14:1218154. doi: 10.3389/fneur.2023.1218154
Received: 06 May 2023; Accepted: 26 June 2023;
Published: 13 July 2023.
Edited by:
Tianxiao Li, Henan Provincial People's Hospital, ChinaReviewed by:
Yueqi Zhu, Shanghai Jiao Tong University, ChinaCopyright © 2023 Wang, Liu, An, Pan and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Feng Wang, Mjc3OTUzMDE1OEBxcS5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.