
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Neurol. , 27 July 2023
Sec. Endovascular and Interventional Neurology
Volume 14 - 2023 | https://doi.org/10.3389/fneur.2023.1200539
This article is part of the Research Topic Case Reports in Endovascular and Interventional Neurology, volume III - 2023 View all 14 articles
 Xin Zhang1,2,3,4,5†
Xin Zhang1,2,3,4,5† Jiaxiong Wang1,6†
Jiaxiong Wang1,6† Zhipeng Cao2,7
Zhipeng Cao2,7 Yingtao Liu2,8
Yingtao Liu2,8 Yi Dong2,7
Yi Dong2,7 Xin Cheng2,7
Xin Cheng2,7 Chao Gao1,2,3,4,5*
Chao Gao1,2,3,4,5* Yuxiang Gu1,2,3,4,5
Yuxiang Gu1,2,3,4,5Persistent hypoglossal artery (PHA) is a rare carotid-vertebrobasilar anastomosis in adults. Here, we report a case of mechanical thrombectomy for acute basilar artery occlusion via the PHA. A 44-year-old man was admitted to our stroke unit with an unstable gait and aphasia for 2 h. The baseline National Institutes of Health Stroke Scale (NIHSS) score was 4, but the clinical symptoms continued to worsen. Computed tomography angiography showed the absence of the basilar artery and an abnormal anastomosis between the anterior and posterior circulation. Clinical symptoms continued to worsen, and endovascular treatment was scheduled. PHA was demonstrated and basilar artery occlusion was confirmed using digital subtraction angiography. Mechanical thrombectomy with a stent retriever and aspiration was performed via the PHA, and modified thrombolysis in cerebral infarction level 3 was achieved. The patient underwent intravenous antiplatelet therapy after the operation, and follow-up neuroimaging revealed multiple small infarcts in the cerebellum and medulla oblongata. The patient was discharged after 10 days for further rehabilitation, with an NIHSS score of 25. At 10 months follow-up, the NIHSS score decreased to 18. Recognition of this rare variation is particularly important for interventional strategy determination and rapid recanalization of basilar artery occlusion.
Basilar artery occlusion (BAO) is the most serious type of acute ischemic stroke. Failure to achieve rapid recanalization can lead to high mortality and disability rates and poor clinical prognosis (1). The safety and efficacy of mechanical thrombectomy (MT) for the treatment of acute large-vessel occlusion in the anterior circulation have been confirmed in many studies (2). Multiple randomized controlled trials (3–6) have shown promising results for MT for acute BAO, with better clinical outcomes and reduced mortality.
Persistent hypoglossal artery (PHA) is a rare carotid-vertebrobasilar anastomosis in adults. Few studies have reported BAO accompanied by PHA. In this case, the patient with BAO received MT, and PHA was confirmed during the operation. Such variation is of great importance in the determination of an endovascular treatment (EVT) strategy for BAO, which includes the establishment of MT access with sufficient supporting strength and the evaluation of compensatory situations.
A 44-year-old man was admitted to our stroke unit with unstable gait and dysarthria for 2 h. The baseline National Institutes of Health Stroke Scale (NIHSS) score was 4 and the Modified Rankin Scale (mRS) score was 1. As the clinical symptoms progressively worsened, the NIHSS score increased to 33 and the mRS score to 4 within 95 min. The patient had a heavy smoking history and primary hypertension treated with nifedipine. In addition, the patient had a history of undefined intracranial hemorrhage; therefore, thrombolytic therapy was a contraindication.
Multimodal computed tomography (CT) was performed, and intracranial hemorrhage was excluded (Figure 1A). CT angiography (CTA) showed the absence of the basilar artery (BA) and an abnormal anastomosis between the internal carotid artery (ICA) and the intracranial segment of the vertebral artery (VA) located in the hypoglossal canal (Figures 1B, C). The size of the area with cerebral blood flow >30% and delay time < 3 s were determined using CT perfusion. The mismatch volume was 104 mL (Figure 1D), determined using MIStar software (Apollo Medical Imaging Technology, Melbourne, Australia). Digital subtraction angiography was performed via the right radial access and showed complete BAO with a modified Thrombolysis in Cerebral Infarction (mTICI) level of 0. PHA originated from the right ICA and anastomosed to the right VA. Right subclavian artery angiography revealed hypoplasia of VA origin. Left middle cerebral artery occlusion with collateral vessel formation and a slender left VA were also observed (Figures 1E–H).
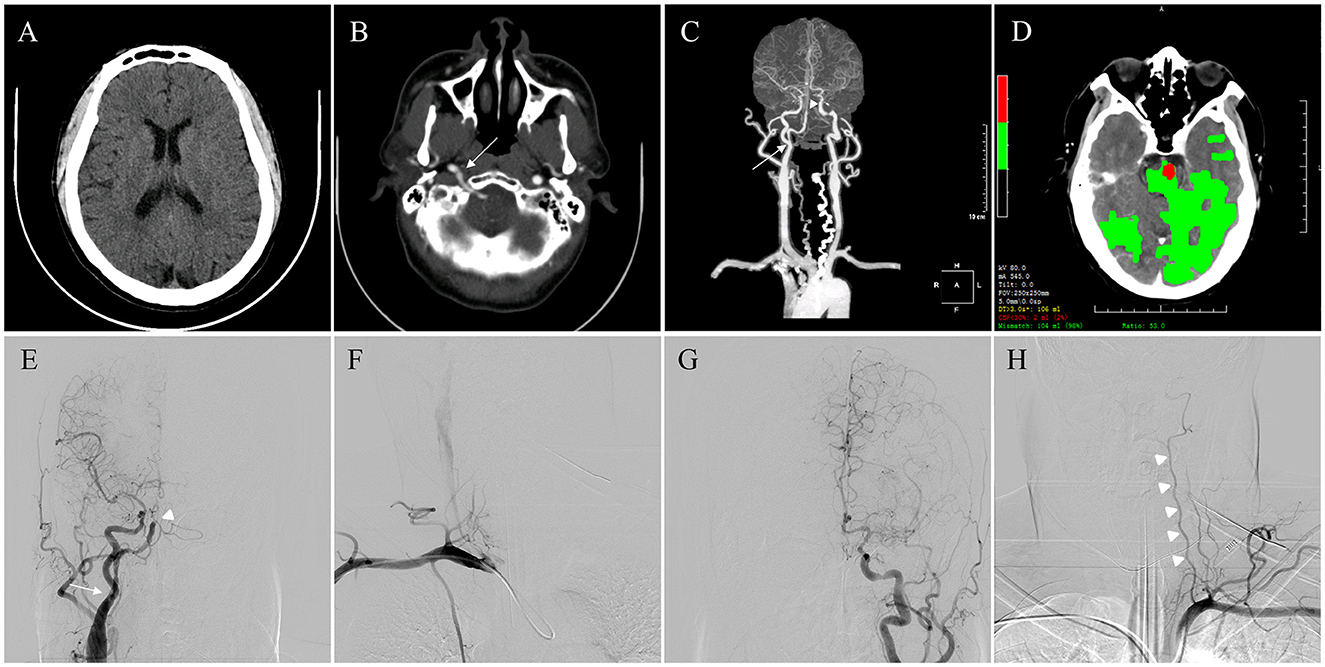
Figure 1. Preoperative multimodal neuroimaging evaluation. (A) Intracranial hemorrhage was excluded through computed tomography (CT). (B) Cross-sectional contrast CT revealed abnormal anastomosis (arrow) between the internal carotid artery (ICA) and the intracranial segment of the vertical artery (VA) located in the atlantooccipital space. (C) CT angiography (anterior-posterior view) showed basilar artery occlusion (arrowhead) and that right VA (arrow) originated from the ICA. (D) Volumes of infarct core (red area) and penumbra (green area) were evaluated automatically from CT perfusion to calculate the mismatch volume. (E) Right hemispheric angiography showed complete occlusion of the middle segment of the basilar artery (arrowhead) and that persistent hypoglossal artery (PHA) (arrow) originated from the right ICA. (F) Right subclavian artery angiography showed the absence of VA origin. (G) Left middle cerebral artery occlusion was observed with collateral vessel formation. (H) Slender left VA (arrowheads) demonstrated in left hemispheric angiography.
Great difficulties were encountered in the establishment of MT access with sufficient supporting strength via transradial access; therefore, transfemoral access was selected. A triaxial system, including a five French aspiration catheter (Navien, Medtronic, Irvine, CA, USA), microcatheter (Prowler Select Plus, Cerenovus, Bridgewater, NJ, USA), and stent retriever (Solitaire AB, Medtronic), was chosen for MT. A 4 × 20 mm Solitaire AB stent was deployed from the P1 segment of the left posterior cerebral artery (PCA) via the PHA for thrombectomy. Angiography showed thrombotic migration to the tip of the BA and severe stenosis in the BA trunk. After angioplasty with a 3 × 9 mm noncompliant balloon (Gateway, Stryker Neurovascular, Kalamazoo, Michigan), thrombectomy was performed again from the right PCA with proximal aspiration via a 5 French distal access catheter (Silver Snake, TonBridge Medical, Zhuhai, China). Complete recanalization of BA flow was achieved at an mTICI level of 3. Postoperative CT revealed no obvious intracranial hemorrhage, and a loading dose of tirofiban was administered (Figures 2A–H).
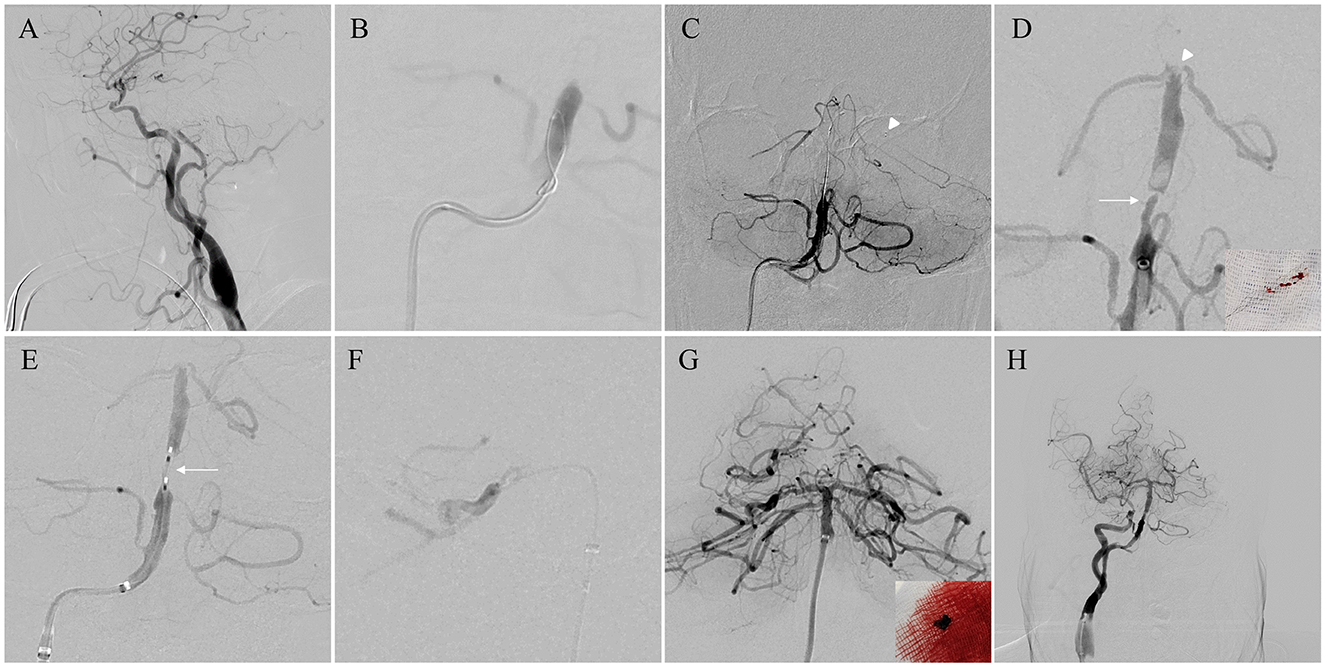
Figure 2. Surgical process. (A) Lateral view as a working projection for the establishment of access for thrombectomy. (B) Angiography via the microcatheter to confirm the real lumen of the distal basilar artery (BA). (C) The distal part of the stent retriever (arrowhead) was deployed from the left posterior cerebral artery. (D) After the first thrombectomy, part of the clot was removed with the stent (right corner), and cerebral angiography showed the migration of residual thrombosis to the tip of the BA (arrowhead) and severe stenosis in the BA trunk (arrow). (E) Angioplasty with a 3 × 9 mm balloon (arrow) in the stenotic portion of the BA. (F) The second thrombectomy was performed from the right persistent hypoglossal artery (PCA) with proximal aspiration. (G) Complete recanalization of the BA and the clot from the aspiration catheter (right corner). (H) Modified Thrombolysis in Cerebral Infarction (mTICI) level 3 forward flow was confirmed after 20 min.
The patient received half loading-dose of intravenous antiplatelet therapy (Tirofiban) and the systolic blood pressure was strictly maintained between 130 and 140 mmHg after the operation. Postoperative neuroimaging follow-up revealed multiple small, newly developed infarcts in the cerebellum and medulla oblongata (Figures 3A–E). CTA performed 3 days after the operation showed good patency of the BA trunk (Figure 3F). The patient was discharged after 10 days for further rehabilitation, with an NIHSS score of 25 and a mRS score of 5. At 10 months follow-up, the NIHSS score decreased to 18 and the mRS score decreased to 4.
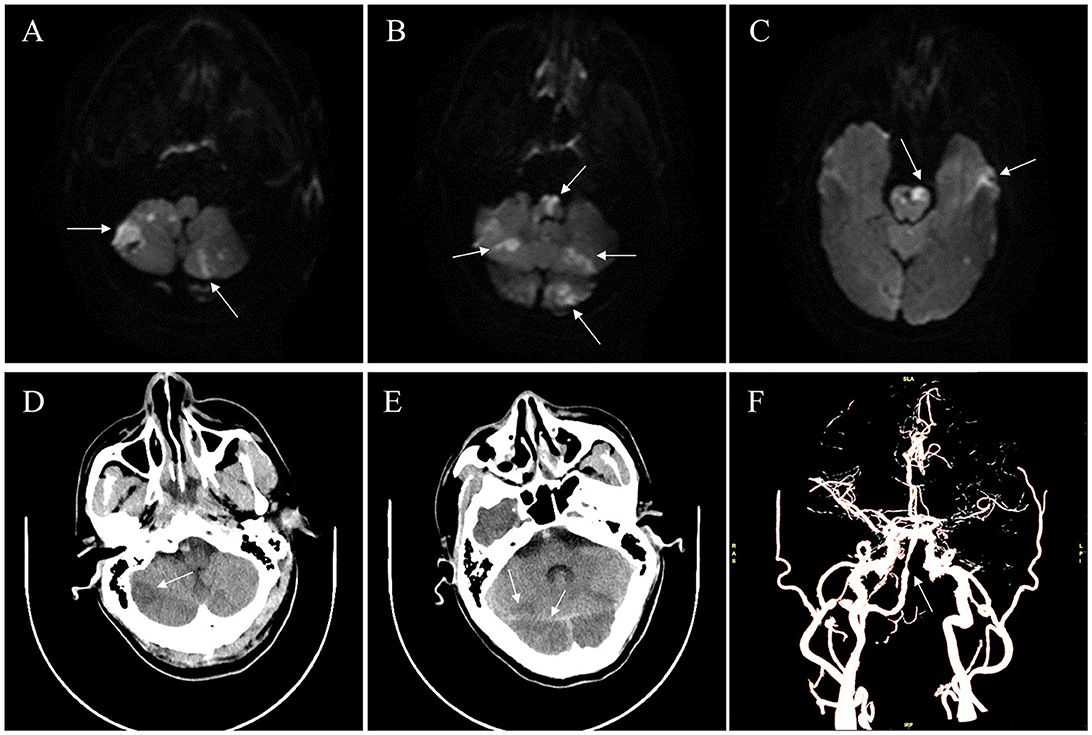
Figure 3. Neuroimaging follow-up. (A–E) Postoperative follow-up revealed multiple small newly developed infarcts (arrows) in the cerebellum and medulla oblongata on diffusion weighted imaging and computed tomography (CT). (F) Postoperative CT angiography confirmed the general patency of the BA trunk, with slight stenosis (arrow).
Few studies have reported the occurrence of BAO accompanied by PHA (Table 1). During early development of the human embryo, various anastomotic channels exist between the carotid artery and vertebrobasilar system, which play critical roles in irrigating the posterior circulatory bed before it fully develops (7). PHA is usually involved in the 12 to 14 mm embryonic stage. Rarely, it fails to regress and persists into adult life, with an incidence of 0.03–0.09% (8). PHA is generally accompanied by other anomalies such as hypoplasia of the VA or PCA. Due to its unique anatomical and hemodynamic characteristics, PHA is a potential risk factor of posterior circulation ischemic events (9). However, cases of PHA combined with acute BAO have rarely been reported.
Earlier recanalization has been correlated with a better prognosis for acute BAO. Owing to its various clinical symptoms, advanced CT evaluations are essential to select suitable cases for patients with BAO (10). Based on the MIStar software, the ischemic penumbra and core infarction could be identified, even though the diagnostic value may be limited because of the influence of the blood flow velocity and the bony structure of the posterior fossa. In addition, CTA is helpful in distinguishing potential variations so that appropriate access catheters can be selected effectively to shorten recanalization time. Hence, the application of advanced CT evaluations is particularly important in surgical decision-making for BAO combined with PHA.
Previous studies (11–13) on BAO accompanied by PHA have mostly attributed it to cardioembolic stroke, and aspiration alone has a high rate of recanalization (Table 1). In this case, the mechanism of BAO was considered to be ischemic stroke based on intracranial atherosclerotic stenosis (ICAS), which is highly prevalent in East Asian populations. Although bridging intravenous treatment may confer benefits for ICAS, the patient had a history of intracranial hemorrhage; therefore, direct MT was selected. To the best of our knowledge, this is the first report of the treatment of BAO via PHA using a stent retriever with aspiration. Similar to the pathogenesis of ICAS, rescue angioplasty after MT is essential for maintaining forward blood flow. More importantly, although the BA was completely recanalized with an mTICI level of 3, embolic debris migration and limited collateral circulation may have resulted in a very poor prognosis. Despite the aforementioned methods, flow control in the proximal part of the ICA with a balloon-guiding catheter may also be more effective and should be seriously considered in subsequent clinical practice (14).
BAO accompanied by PHA is extremely rare, and relevant literature is lacking. Preoperative multimodal CT evaluations are helpful in identifying such vascular variations to determine an interventional strategy for earlier recanalization. Proximal flow control, aspiration with a balloon-guiding catheter, and the use of intra-arterial alteplase or tirofiban may improve the clinical outcomes of ischemic stroke based on ICAS.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Institutional Review Board (IRB) of Huashan Hospital, Fudan University, China (approval number KY2015-256). The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) and/or minor(s)' legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
XZ, JW, ZC, YL, YD, XC, CG, and YG contributed to the conception and design, acquisition and interpretation of the case data, drafting and revision of the article, particularly for important intellectual content, final approval of the published version, and agreement to be accountable for the accuracy or integrity of the article. All authors contributed to the manuscript and approved the submitted version.
This study was supported by the National Natural Science Foundation of China (Grant Number 82171313) and the Shanghai Hospital Development Center (Grant Number SHDC2022CRD032).
The authors wish to thank the patient for agreeing to the publication of this case report and all members of the multidisciplinary first aid team for cerebrovascular disease of Huashan Hospital, Fudan University for their continuous collaboration and support.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Liu X, Dai Q, Ye R, Zi W, Liu Y, Wang H, et al. Endovascular treatment versus standard medical treatment for vertebrobasilar artery occlusion (BEST): an open-label, randomised controlled trial. Lancet Neurol. (2020) 19:115–22. doi: 10.1016/S1474-4422(19)30395-3
2. Writing Group for the BASILAR Group Zi W Qiu Z Wu D Li F Liu H . Assessment of endovascular treatment for acute basilar artery occlusion via a nationwide prospective registry. JAMA Neurol. (2020) 77:561–73. doi: 10.1001/jamaneurol.2020.0156
3. Novakovic-White R, Corona JM, White JA. Posterior circulation ischemia in the endovascular era. Neurology. (2021) 97:S158–69. doi: 10.1212/WNL.0000000000012808
4. Langezaal LCM, van der Hoeven EJRJ, Mont'Alverne FJA, de Carvalho JJF, Lima FO, Dippel DWJ, et al. Endovascular therapy for stroke due to basilar-artery occlusion. N Engl J Med. (2021) 384:1910–20. doi: 10.1056/NEJMoa2030297
5. Tao C, Nogueira RG, Zhu Y, Sun J, Han H, Yuan G, et al. Trial of endovascular treatment of acute basilar-artery occlusion. N Engl J Med. (2022) 387:1361–72. doi: 10.1056/NEJMoa2206317
6. Jovin TG, Li C, Wu L, Wu C, Chen J, Jiang C, et al. Trial of thrombectomy 6 to 24 hours after stroke due to basilar-artery occlusion. N Engl J Med. (2022) 387:1373–84. doi: 10.1056/NEJMoa2207576
7. Johnson MD, Prestigiacomo CJ, Ferioli S, Flaherty ML. Persistent hypoglossal artery and concurrent carotid thrombus. Ann Neurol. (2020) 88:233–4. doi: 10.1002/ana.25795
8. See AP, Baranoski JF, Flores BC, Ducruet A, Albuquerque FC. Basilar stroke from a persistent hypoglossal artery. J Neurointerv Surg. (2017) 9:e30. doi: 10.1136/neurintsurg-2016-012859.rep
9. Jin X, Sun L, Feng Z, Li X, Zhang H, Meng K, et al. Persistent hypoglossal artery as a potential risk factor for simultaneous carotid and vertebrobasilar infarcts. Front Neurol. (2018) 9:837. doi: 10.3389/fneur.2018.00837
10. Gunasekera L, Churilov L, Mitchell P, Bivard A, Sharma G, Parsons MW, et al. Automated estimation of ischemic core prior to thrombectomy: comparison of two current algorithms. Neuroradiology. (2021) 63:1645–9. doi: 10.1007/s00234-021-02651-9
11. Kawano H, Inatomi Y, Hirano T, Yonehara T. Cerebral infarction in both carotid and vertebrobasilar territories associated with a persistent primitive hypoglossal artery with severe dilated cardiomyopathy. J Stroke Cerebrovasc Dis. (2014) 23:176–8. doi: 10.1016/j.jstrokecerebrovasdis.2012.07.020
12. Voronovich Z, Grandhi R, Zwagerman NT, Jadhav AP, Jovin TG. Manual aspiration thrombectomy for basilar infarction in the setting of a persistent primitive hypoglossal artery: case report and review of the literature. Surg Neurol Int. (2014) 5:182. doi: 10.4103/2152-7806.147412
13. Park JS, Shin BS, Kang HG. Endovascular treatment for acute basilar artery occlusion via persistent primitive hypoglossal artery: a case report. Medicine. (2021) 100:e27998. doi: 10.1097/MD.0000000000027998
14. Ospel JM, Volny O, Jayaraman M, McTaggart R, Goyal M. Optimizing fast first pass complete reperfusion in acute ischemic stroke - the BADDASS approach (BAlloon guiDe with large bore Distal Access catheter with dual aspiration with Stent-retriever as Standard approach). Expert Rev Med Devices. (2019) 16:955–63. doi: 10.1080/17434440.2019.1684263
Keywords: persistent hypoglossal artery, acute ischemic stroke, basilar artery occlusion, thrombectomy, case report
Citation: Zhang X, Wang J, Cao Z, Liu Y, Dong Y, Cheng X, Gao C and Gu Y (2023) Case report: Mechanical thrombectomy for acute basilar artery occlusion via persistent hypoglossal artery. Front. Neurol. 14:1200539. doi: 10.3389/fneur.2023.1200539
Received: 06 April 2023; Accepted: 10 July 2023;
Published: 27 July 2023.
Edited by:
Franklin Marden, Alexian Brothers Medical Center, United StatesReviewed by:
Luis Rafael Moscote-Salazar, Colombian Clinical Research Group in Neurocritical Care, ColombiaCopyright © 2023 Zhang, Wang, Cao, Liu, Dong, Cheng, Gao and Gu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chao Gao, Z2NfaHVhc2hhbm5ldXJvQHNpbmEuY29t
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.