
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Neurol. , 20 April 2023
Sec. Neurotrauma
Volume 14 - 2023 | https://doi.org/10.3389/fneur.2023.1160204
This article is part of the Research Topic Neurological and Neuropsychiatric Disorders Affecting Military Personnel and Veterans View all 17 articles
 Alec Giakas1
Alec Giakas1 Kiersten Mangold2
Kiersten Mangold2 Anthony Androulakis3
Anthony Androulakis3 Noah Hyduke4
Noah Hyduke4 Igor Galynker5
Igor Galynker5 Melinda Thiam6
Melinda Thiam6 Guoshuai Cai7
Guoshuai Cai7 X. Michelle Androulakis8,9*
X. Michelle Androulakis8,9*Objective: To conduct a systematic review and meta-analysis on suicidal ideation, attempts, and death in patients with head, neck, and back pain.
Method: Search was performed using PubMed, Embase, and Web of Science from the date of the first available article through September 31, 2021. A random effects model was used to estimate the pooled odds ratios (ORs) and 95% confidence intervals (95% CI) for the association between suicidal ideation and/or attempt and head, back/neck pain conditions. Articles describing non-migraine headache disorders and death by suicide were also reviewed but not included in the meta-analysis due to an insufficient number of studies.
Results: A total of 20 studies met criteria for systemic review. A total of 186,123 migraine patients and 135,790 of neck/back pain patients from 11 studies were included in the meta-analysis. The meta-analysis showed that the estimated risk of combined suicidal ideation and attempt in migraine [OR 2.49; 95% CI: 2.15–2.89] is greater than that in back/neck pain pain [OR 2.00; 95% CI: 1.63–2.45] compared to non-pain control groups. Risk of suicide ideation/planning is 2 folds higher [OR: 2.03; 95% CI: 1.92–2.16] and risk of suicide attempt is more than 3 folds higher [OR: 3.47; 95% CI: 2.68–4.49] in migraine as compared to healthy controls.
Conclusion: There is an elevated risk of suicidal ideation and attempt in both migraine and neck/back pain patients in comparison to healthy controls, and this risk is particularly higher among migraine patients. This study underscores the critical need for suicide prevention in migraine patients.
Chronic pain is a leading cause of disability worldwide and affects upwards of 20.4% of adults in the United States (1). Headache disorders, especially migraine, are among the most common types of chronic pain conditions encountered by neurologists and psychiatrists. Migraine has a global negative impact on overall quality of life, cognitive, emotional health, and contributes to isolation, frustration, guilt, fear, avoidance behavior, and stigma (2). Individuals with migraine thus often learn to internalize symptoms with strict concealment, as the manifestations of migraine, as well as its degree of severity and disability, are invisible: pain, cognitive impairment, nausea, vertigo, hypersensitivity to the environment, aura, etc. (3). Despite the prevalence and impact of migraines, 70% of migraine patients do not seek medical advice (4, 5).
Migraine has significant association with multiple mental health disorders. For example, bidirectional association exists between migraine and psychiatric disorders such as anxiety disorder, bipolar disorder, and depression (6–8). This is especially true for the military and Veteran population. In 2020, the suicide rate for Veterans was 57.3% greater than for non-Veteran U.S. adults when adjusted for demographic differences (9). Traumatic brain injury (TBI), PTSD, and depression are significant risk factors for chronic headache in Veterans (10). Veterans with chronic headache, especially those with comorbid TBI, PTSD, and depression, are at increased risk for suicidal behavior (10, 11). As such, there is a need to better understand the relationship between suicidality and head, neck, and back pain, and establishing interdisciplinary collaboration when caring for Veterans with migraine, which often go undiagnosed or not coded (12).
One cannot “split the brain”; therefore, improved understanding of increased suicide risk among headache disorders affords a unique opportunity for clinicians of various disciplines to proactively engage in dialogue to collaborate and advocate for better treatment. Currently, most of headache management is done by specialty care or primary care separately. We hope to bring awareness to the increased risk of suicide among headache disorders, which serves as an invitation for neurologists, psychiatrists, psychologists, and others involved in patient care to join the interdisciplinary care team.
Previous research has indeed associated migraines with an increased suicide risk (13, 14), but previous review and meta-analysis are lacking regarding the potential risk for suicide in both migraine and other pain disorders. There is also a lack of comprehensive review between different types of headache disorders and a spectrum of suicidal behaviors. As such, authors conducted a systematic review and meta-analysis to examine the risk of different types of suicidal behavior (i.e., ideation, attempts, and death) in patients with migraine, non-migraine headache conditions, and back/neck pain compared to healthy controls.
Authors conducted the literature search using three databases (PubMed, EMBASE, and Web of Science) from the date of the first available article through September 31, 2021. Studies related to headache, back pain, or neck pain and suicide were identified using keywords “migraine AND suicide,” “cluster headache AND suicide,” “trigeminal autonomic cephalgia AND suicide,” “post-traumatic headache AND suicide,” “tension headache AND suicide,” “trigeminal neuralgia AND suicide,” “hemicrania continua AND suicide,” “chronic back pain AND suicide,” “back pain AND suicide,” “lumbar pain AND suicide,” “cervicalgia AND suicide,” “chronic neck pain AND suicide,” and “neck pain AND suicide.” No other filters were used. The principles of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses was used to further screen and filter studies. One reviewer screened studies to determine whether they meet the eligibility criteria as outlined below, and one independent reviewer confirmed that only papers that fully met these criteria were included in this study. The full text of all included studies was then examined by a third reviewer to ensure that data had been recorded accurately.
To be included in the analysis, studies were required to meet all of the following criteria: (A) participants were adults 18 years of age or older; (B) the study defined the type of suicidal behavior being examined; (C) the study used healthy controls or controls without chronic pain conditions; (D) the study assessed the association of an individual headache disorder (migraine, cluster headache, tension headache, trigeminal autonomic cephalgia, and trigeminal neuralgia) or chronic back or neck pain with suicidal behavior or death by suicide as compared to healthy controls; (E) the study was published in the English language.
Studies were excluded if they met the following criteria: (A) inclusion of participants under 18 years of age; (B) published in the form of conference abstracts/posters, editorials, guidelines, or reviews; (C) insufficient data, such as raw data, mean or p-value; (D) lack of a healthy control group; (E) patients with chronic pain included in the control group.
Data were extracted by the same researcher from each article and included the following items: year, population of interest, ICD codes and/or method of defining chronic pain, statistical method, sample size of the chronic pain and healthy control groups, odds ratio of risk of suicide in pain group compared to healthy control group, and confidence intervals. Unadjusted ORs were used due to inter-study variance in controlled factors. Authors used Comprehensive Meta-Analysis (CMA) V3 software (Biostat, NJ, USA) to generate summary statistics and pooled adjusted ORs using a random effects model, as stratified by the suicidal behavior (suicide ideation, suicide attempt) and pain types (migraine, chronic neck/back pain).
Initial search yielded 1,763 results, which were then screened for inclusion in the review and meta-analysis (Figure 1). Twenty studies met the criteria to be included in the systematic review. Two of these studies examined cluster headache disorder (15, 16) and two examined tension-type headache (17, 18) so meta-analysis was not conducted for these specific headache disorders due to limited study numbers. Similarly, only two studies examined death by suicide as an outcome, they were not included in the meta-analysis (19, 20). The meta-analysis was therefore conducted for migraine and back/neck pain with suicidal ideation/planning or suicide attempts as outcome measures. Three additional studies were lacking specific statistics and thus were not eligible for the meta-analysis (21–23). Therefore, a total of 11 studies were included in the meta-analysis.
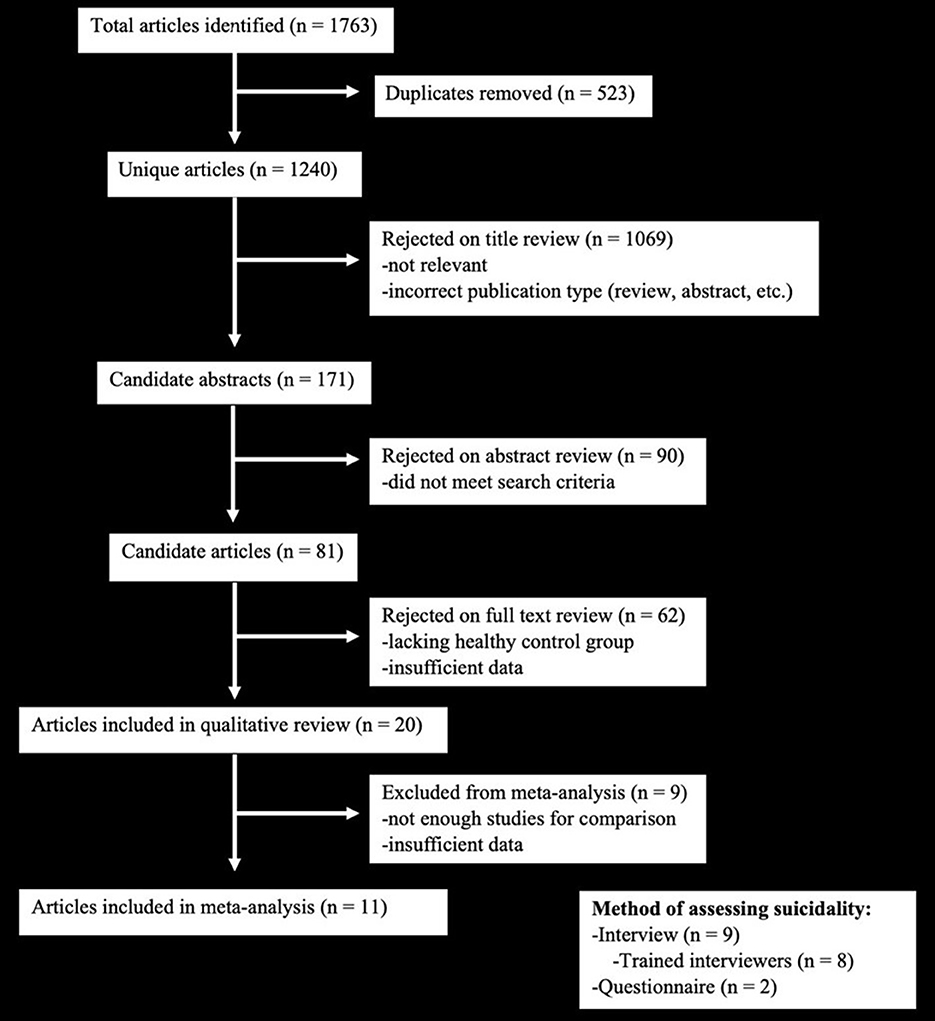
Figure 1. PRISMA inclusion diagram for meta-analysis, which demonstrates the process through which the studies used in the manuscript were selected from the total number of studies identified.
A total of 186,123 migraine patients and 135,790 of back/neck pain patients were included in the meta-analysis. The meta-analysis showed that the estimated risk of suicidal ideation and/or attempt both in patients with migraine (OR 2.49; 95% CI: 2.15–2.89) (Figure 2) and in those with back/neck pain (OR 2.00; 95% CI: 1.63–2.45) (Figure 3) was significantly elevated when compared to healthy controls. Migraine was associated with a 2-fold higher risk of suicidal ideation/planning (OR: 2.03; 95% CI: 1.92–2.16) (Figure 4) and over three times higher risk of suicide attempt (OR: 3.47; 95% CI: 2.68–4.49) (Figure 5) when compared to controls. The odds of suicidal ideation/planning in back/neck pain were just under two times that of healthy controls (OR: 1.81; 95% CI: 1.39–2.36) (Figure 6). Chronic back/neck pain was associated with a 2.53 (95% CI: 2.05–3.12) times increased odds of suicide attempts (Figure 7), which was lower than that associated with migraine (z test, p = 0.04).
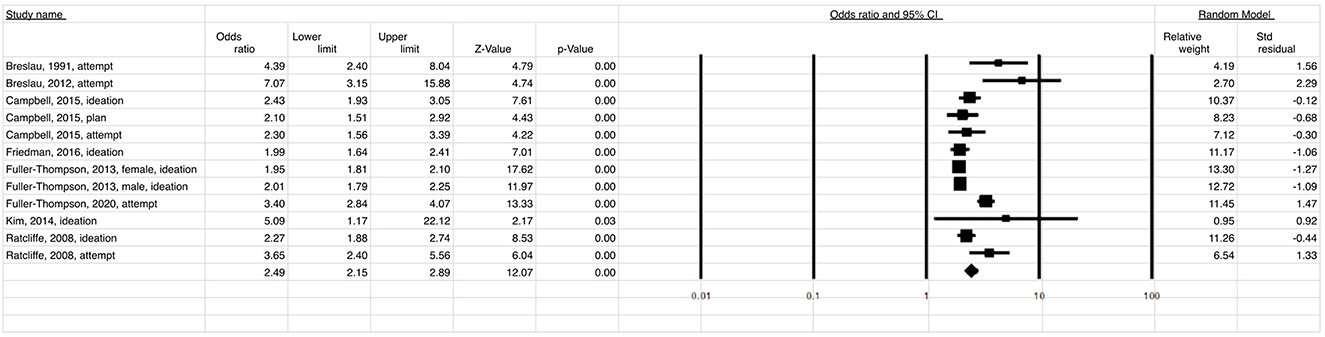
Figure 2. Relationship between suicide ideation and attempt (OR = 2.49) in patients with migraine when compared to healthy controls.
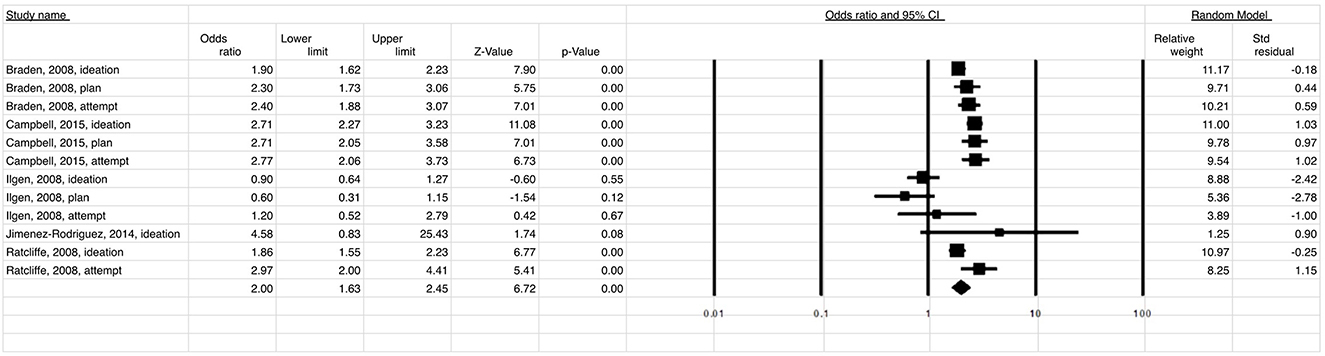
Figure 3. Relationship between suicide ideation and attempt (OR = 2.00) in patients with back/neck pain when compared to healthy controls.
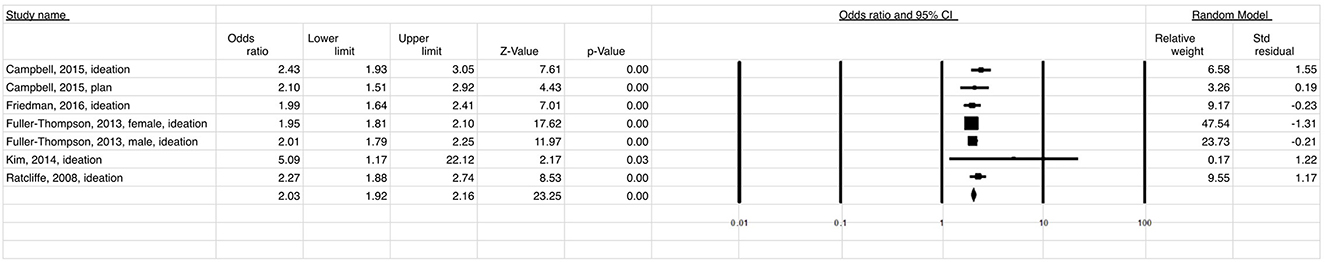
Figure 4. Relationship between the risk of suicide ideation/planning (OR = 2.03) in patients with migraine when compared to healthy controls.

Figure 5. Relationship between suicide attempt (OR = 3.47) in patients with migraine when compared to healthy controls.
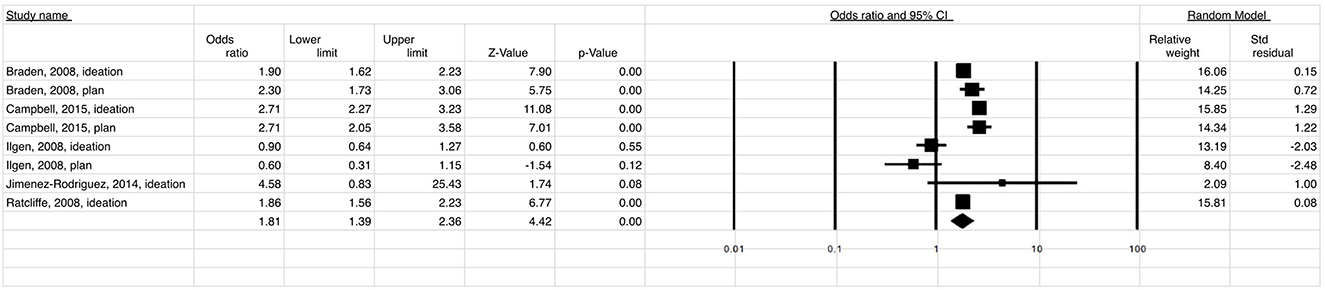
Figure 6. Relationship between risk of suicide ideation/planning (OR=1.81) in patients with back/neck pain when compared to healthy controls.
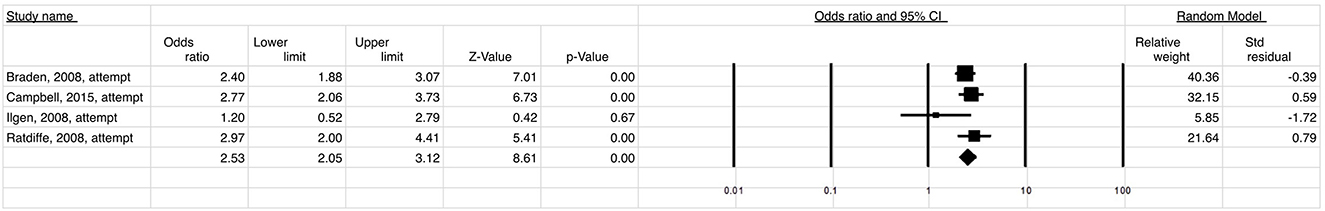
Figure 7. Relationship between risk of suicide attempt (OR = 2.53) in patients with chronic back/neck pain when compared to healthy controls.
Two studies identified in the present review examined death by suicide as an outcome measure. One study examined the association between migraine and both self-harm and suicide mortality. The authors reported an increased odds (hazard ratio = 2.18) of self-harm for those diagnosed with migraine but did not find an association between migraine and death by suicide (19). However, another study reported an increased risk of death by suicide associated with migraine (hazard ratio = 1.68), which persisted when controlling for psychiatric comorbidities (hazard ratio = 1.34) (17).
Three studies identified in our search examined suicidality in relation to headache disorders distinct from migraine, specifically cluster headache and tension headache. Cluster headache was reported to increase the risk of suicidal ideation by 2.5 times [OR: 2.49, 95% CI: 1.91–3.25] (16) and around 2-fold [OR: 2.04, 95% CI: 1.08–3.85] (15) when compared to controls in two separate studies, even after accounting for depression and demoralization. A similar pattern was reported for tension headaches, which were associated with 2.39 times higher odds of suicidal ideation or attempt, defined as suicidal ideation and/or attempts (18). One study also reported an increased risk of death by suicide associated with headache or tension headache (hazard ratio = 1.38) (17). When distinguishing between chronic and episodic tension headache, only chronic tension headache was associated with increased suicidal ideation or attempt (18). In further comparison of headache conditions, another study reported an increased odds of suicide attempt for both migraine [OR: 7.21, 95% CI: 3.21–16.2] and non-migraine headache [OR: 8.38, 95% CI: 3.35–21.0] when compared to controls with no history of severe headache; however, there were no differences between migraine and non-migraine type headaches for odds of suicide attempts (24).
This study sought to examine the risk of suicidality among patients suffering from migraine, non-migraine headache disorders, and back/neck pain. This meta-analysis demonstrates that suicidal ideation and attempts are both significantly increased among patients with migraine or back/neck pain compared to healthy controls, whereas systematic review demonstrates an increased risk of suicidality in patients with non-migraine headache disorders as well. Of note, the risk of suicide attempt in patients with migraine is statistically higher than in those with back/neck pain. The odds associated with suicide attempts in migraine were over 3-fold—the highest for any of the pain conditions and suicidal behaviors investigated in this study.
Previous literature reviews have described an increase in suicidal ideation and attempts associated with non-specific chronic pain (25–28). Our study provides additional evidence for increased risk of suicidality in patients with migraine and non-migraine headache disorders. Most importantly, our results shed light on a potentially higher risk of suicide attempt in patients with migraine than in those with back/neck pain.
It is worth noting that studies examining the association between mental health disorder diagnosis as it relates to chronic pain and suicidality reveal inconsistent results. Some studies suggested that the relationship between migraine or back/neck pain and suicidality persists when accounting for psychiatric comorbidities (24, 29–31) while others didn't find significant associations (21, 32, 33). Further discrepancies are present based on the type of suicidal behavior examined. For example, one study reported that, when controlling for mental health disorders, migraine remained associated with suicidal ideation but not planning or attempts (30), whereas another study noted a consistent association with suicidal ideation and planning but not attempts, which may be due to under diagnosis of mental health disorders (34). Regardless of the intensity of pain of migraine attacks, the frequency and duration have been found to have a strong association with the burden of psychiatric comorbidity [OR: 7.21, 95% CI: 3.21–16.2] (6).
It is imperative to note while migraine is strongly associated with elevated suicide risk, physicians should also be familiar with increased suicide risk in patients with cluster and chronic tension headaches. Very few studies examined non-migraine type headache disorders, and thus were not included in the meta-analysis. However, upon systematic review, the odds of self-inflicted injury, suicidal ideation and attempt, or death by suicide for cluster headache and chronic tension headache were similar to that of migraine (15–18). Cluster headaches have been linked with increased suicidal ideation, planning and attempts during attacks, which was found to predict increased suicidality in the interictal phase of cluster headache. In addition, longer disease burden, even with episodic cluster headaches, was associated with a similar increase in suicidality, prompting the need for preventative treatment (35). These results further parallel those of another study showing the risk of suicide attempts in migraine patients was equivalent to that in non-migraine type headaches (24).
Suicide Crisis Syndrome, or SCS, is a recently described acute suicidal mental state which may link migraines and suicidal behavior (36). Several SCS criteria have symptoms overlapping with migraine (36, 37). Of note, CDC report demonstrated that only a fraction of deaths by suicide expressed ideation before their death; >75% explicitly denied suicidal ideation prior to their death (38). One of the reasons for non-disclosure of suicidal ideation is that explicit suicidal intent may last less than 10 min preceding a suicide attempt, a very short period which is likely to occur outside the clinical setting. Another reason is that suicidal individuals would not admit to their suicidal intent out of fear of being hospitalized and losing their autonomy; this is potentially more likely to occur among military personnel and Veterans. SCS, on the other hand, is diagnosed indirectly, without asking about suicidal ideation or intent, and has consistently outperformed suicidal ideation for prediction of future suicidal behavior (13–16, 39). It is worth noting that all studies reviewed used a simple yes/no question to elicit suicidal behavior (Table 1). This represents a significant void in clinical research studying associations between migraine and suicidal behavior. Using SCS checklist may be an exceedingly useful tool for identifying individuals with migraine headaches who are at imminent risk for suicide.
Despite the novelty of this study, there are some limitations. As discussed above, there were very few studies that included patients with headache disorders other than migraine, thus we were only able to include patients with migraine and back/neck pain in the meta-analysis. This lack of existing literature limits the conclusions we are able to draw pertaining to non-migraine type headache disorders and highlights an important direction for future research to allow for broader and more detailed analysis of suicidality in headache disorders. Additionally, our meta-analysis pooled results were uncontrolled for different variables, such as psychiatric comorbidities. We chose to analyze uncontrolled results because of the variability between studies in their adjusted analyses. For example, some studies controlled for diagnosed psychiatric disorders (24, 33, 40), while others controlled for self-reported depression or anxiety scores (32) and adverse childhood experiences (42).
A national cohort study in the Veterans Health Administration for fiscal year 2008–2019 found that Veterans with headache were being seen at the emergency department at the same rate as at neurology clinics and at a larger rate than headache specialists (12). In patients who died by suicide, it has been elucidated that one-third had contact with mental health services within a year and one-fifth had contact within a month of their suicide. Additionally, about three-quarters of patients were seen by their primary care physician within a year, and about one-half of patients were seen within the month, of their suicide (39). This further demonstrates the need for increasing awareness of suicide risks among Veterans with different types of pain conditions and for collaboration between specialties within VHA.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
XMA contributed to the design, interpretation of results, and drafting of the study. All authors contributed to the interpretation of results, drafting, and the revision of the final manuscript.
XMA received support from the VA Headache Center of Excellence Program.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Saylor D, Steiner TJ. The Global Burden of Headache. Semin Neurol. (2018) 38:182–90. doi: 10.1055/s-0038-1646946
2. Estave PM, Beeghly S, Anderson R, Margol C, Shakir M, George G, et al. Learning the full impact of migraine through patient voices: A qualitative study. Headache. (2021) 61:1004–20. doi: 10.1111/head.14151
3. Lipton RB, Nicholson RA, Reed ML, Araujo AB, Jaffe DH, Faries DE, et al. Diagnosis, consultation, treatment, and impact of migraine in the US: Results of the OVERCOME (US) study. Headache. (2022) 62:122–40. doi: 10.1111/head.14259
4. MacGregor EA. The doctor and the migraine patient: improving compliance. Neurology. (1997) 48:S16–20. doi: 10.1212/WNL.48.3_Suppl_3.16S
5. Monteith TS. Advocacy for migraine relief: strategic planning to eliminate the burden. Curr Pain Headache Rep. (2022) 26:567–74. doi: 10.1007/s11916-022-01059-1
6. Pistoia F, Salfi F, Saporito G, Ornello R, Frattale I, D'Aurizio G, et al. Behavioral and psychological factors in individuals with migraine without psychiatric comorbidities. J Headache Pain. (2022) 23:1–9. doi: 10.1186/s10194-022-01485-x
7. Bergman-Bock S. Associations between migraine and the most common psychiatric co-morbidities. Headache. (2018) 58:346–53. doi: 10.1111/head.13146
8. Leo RJ, Singh J. Migraine headache and bipolar disorder comorbidity: A systematic review of the literature and clinical implications. Scand J Pain. (2016) 11:136–45. doi: 10.1016/j.sjpain.2015.12.002
9. Prevention VS. National Veteran Suicide Prevention Annual Report 2022. Office of Mental Health and Suicide Prevention. (2022).
10. Androulakis XM, Guo S, Zhang J, Sico J, Warren P, Giakas A, et al. Suicide attempts in US veterans with chronic headache disorders: a 10-year retrospective cohort study. J Pain Res. (2021) 14:2629–39. doi: 10.2147/JPR.S322432
11. Allan NP, Holm-Denoma J, Conner KR, Zuromski KL, Saulnier KG, Stecker T. Profiles of risk for suicidal behavior in past and current united states military personnel: latent profile analysis of current risk factors. Arch Suicide Res. (2020) 24:1–17. doi: 10.1080/13811118.2018.1506843
12. Sico JJ, Seng E, Wang K, Skanderson M, Schindler EA, Ney JP, et al. Characteristics and gender differences of headache in the veterans health administration: a national cohort study, fiscal year 2008–2019. Neurology. (2022) 99:e1993–2005. doi: 10.1212/WNL.0000000000200905
13. Karimi L, Dimi H, Christine B, Melissa B, Tissa W, Sheila GC. Recent evidence regarding the association between migraine and suicidal behaviors: a systematic review. Front Neurol. (2020) 11:490. doi: 10.3389/fneur.2020.00490
14. Nović A, Kõlves K, O'Dwyer S, De Leo D. Migraine and suicidal behaviors: a systematic literature review. Clin J Pain. (2016) 32:351–64. doi: 10.1097/AJP.0000000000000256
15. Koo BB, Bayoumi A, Albanna A, Abusuliman M, Burrone L, Sico JJ, et al. Demoralization predicts suicidality in patients with cluster headache. J Headache Pain. (2021) 22:28. doi: 10.1186/s10194-021-01241-7
16. Choong CK, Ford JH, Nyhuis AW, Joshi SG, Robinson RL, Aurora SK, et al. Clinical characteristics and treatment patterns among patients diagnosed with cluster headache in US Healthcare Claims Data. Headache. (2017) 57:1359–74. doi: 10.1111/head.13127
17. Ilgen MA, Kleinberg F, Ignacio RV, Bohnert AS, Valenstein M, McCarthy JF, et al. Noncancer pain conditions and risk of suicide. JAMA Psychiatry. (2013) 70:692–7. doi: 10.1001/jamapsychiatry.2013.908
18. Seo JG, Kim KT, Moon HJ, Kuk Do J, Kim SY, Park SP. Suicidality and its risk factors in tension-type headache patients: A multicenter case-control study. J Clin Neurosci. (2019) 69:21–5. doi: 10.1016/j.jocn.2019.08.084
19. Colman I, Kingsbury M, Sareen J, Bolton J, van Walraven C. Migraine headache and risk of self-harm and suicide: A population-based study in Ontario, Canada. Headache. (2016) 56:132–40. doi: 10.1111/head.12710
20. Singhal A, Ross J, Seminog O, Hawton K, Goldacre MJ. Risk of self-harm and suicide in people with specific psychiatric and physical disorders: comparisons between disorders using English national record linkage. J R Soc Med. (2014) 107:194–204. doi: 10.1177/0141076814522033
21. Berhane HY, Jamerson-Dowlen B, Friedman LE, Berhane Y, Williams MA, Gelaye B. Association between migraine and suicidal behavior among Ethiopian adults. BMC Psychiatry. (2018) 18:1–9. doi: 10.1186/s12888-018-1629-7
22. Friedman LE, Zhong Q-Y, Gelaye B, Williams MA, Peterlin BL. Association Between Migraine and Suicidal Behaviors: A Nationwide Study in the USA. Headache. (2018) 58:371–80. doi: 10.1111/head.13235
23. Harnod T, Lin CL, Kao CH. Risk and predisposing factors for suicide attempts in patients with migraine and status migrainosus: a nationwide population-based study. J Clin Med. (2018) 7:268. doi: 10.3390/jcm7090269
24. Breslau N, Schultz L, Lipton R, Peterson E, Welch KMA. Migraine Headaches and Suicide Attempt. Headache. (2012) 52:723–31. doi: 10.1111/j.1526-4610.2012.02117.x
25. Fishbain DA. The association of chronic pain and suicide. Semin Clin Neuropsychiatry. (1999) 4:221–7.
26. Tang NK, Crane C. Suicidality in chronic pain: a review of the prevalence, risk factors and psychological links. Psychol Med. (2006) 36:575–86. doi: 10.1017/S0033291705006859
27. Fishbain DA, Lewis JE, Gao J. The pain suicidality association: a narrative review. Pain Med. (2014) 15:1835–49. doi: 10.1111/pme.12463
28. Calati R, Laglaoui Bakhiyi C, Artero S, Ilgen M, Courtet P. The impact of physical pain on suicidal thoughts and behaviors: Meta-analyses. J Psychiatr Res. (2015) 71:16–32. doi: 10.1016/j.jpsychires.2015.09.004
29. Ratcliffe GE. Chronic pain conditions and suicidal ideation and suicide attempts: An epidemiologic perspective. Clin J Pain. (2008). 24:204–10. doi: 10.1097/AJP.0b013e31815ca2a3
30. Campbell G, Darke S, Bruno R, Degenhardt L. The prevalence and correlates of chronic pain and suicidality in a nationally representative sample. Aust N Z J Psychiatry. (2015) 49:803–11. doi: 10.1177/0004867415569795
31. Friedman LE, Gelaye B, Rondon MB, Sanchez SE, Peterlin BL, Williams MA. Association of migraine headaches with suicidal ideation among pregnant women in Lima, Peru. Headache. (2016) 56:741–9. doi: 10.1111/head.12793
32. Kim SY, Park SP. Suicidal ideation and risk factors in Korean migraine patients. J Clin Neurosci. (2014) 21:1699–704. doi: 10.1016/j.jocn.2014.03.016
33. Braden JB, Sullivan MD. Suicidal thoughts and behavior among adults with self-reported pain conditions in the national comorbidity survey replication. J Pain. (2008) 9:1106–15. doi: 10.1016/j.jpain.2008.06.004
34. Braden JB, Zhang L, Zimmerman FJ, Sullivan MD. Employment outcomes of persons with a mental disorder and comorbid chronic pain. Psychiatr Serv. (2008) 59:878–85. doi: 10.1176/ps.2008.59.8.878
35. Ji Lee M, Cho SJ, Wook Park J, Kyung Chu M, Moon HS, Chung PW, et al. Increased suicidality in patients with cluster headache. Cephalalgia. (2019) 39:1249–56. doi: 10.1177/0333102419845660
36. Galynker I, Yaseen ZS, Cohen A, Benhamou O, Hawes M, Briggs J. Prediction of suicidal behavior in high risk psychiatric patients using an assessment of acute suicidal state: The suicide crisis inventory. Depress Anxiety. (2017) 34:147–58. doi: 10.1002/da.22559
37. Bloch-Elkouby S, Gorman B, Schuck A, Barzilay S, Calati R, Cohen LJ, et al. The suicide crisis syndrome: A network analysis. J Couns Psychol. (2020) 67:595–607. doi: 10.1037/cou0000423
38. Schuck A, Calati R, Barzilay S, Bloch-Elkouby S, Galynker I. Suicide Crisis Syndrome: A review of supporting evidence for a new suicide-specific diagnosis. Behav Sci Law. (2019) 37:223–39. doi: 10.1002/bsl.2397
39. Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry. (2002) 159:909–16. doi: 10.1176/appi.ajp.159.6.909
40. Breslau N, Davis GC, Andreski P. Migraine, psychiatric disorders, and suicide attempts: an epidemiologic study of young adults. Psychiatry Res. (1991) 37:11–23. doi: 10.1016/0165-1781(91)90102-U
41. Fuller-Thomson E, Schrumm M, Brennenstuhl S. Migraine and despair: Factors associated with depression and suicidal ideation among canadian migraineurs in a population-based study. Depress Res Treat. (2013) 2013:401487. doi: 10.1155/2013/401487
42. Fuller-Thomson E, Hodgins GA. Suicide attempts among those with migraine: findings from a nationally representative canadian study. Arch Suicide Res. (2020) 24:360–79. doi: 10.1080/13811118.2019.1578710
43. Jimenez-Rodríguez I, Garcia-Leiva JM, Jimenez-Rodriguez BM, Condés-Moreno E, Rico-Villademoros F, Calandre EP. Suicidal ideation and the risk of suicide in patients with fibromyalgia: a comparison with non-pain controls and patients suffering from low-back pain. Neuropsychiatr Dis Treat. (2014) 10:625–30. doi: 10.2147/NDT.S57596
Keywords: suicide, chronic back pain, chronic neck pain, migraine, headache
Citation: Giakas A, Mangold K, Androulakis A, Hyduke N, Galynker I, Thiam M, Cai G and Androulakis XM (2023) Risks of suicide in migraine, non-migraine headache, back, and neck pain: a systematic review and meta-analysis. Front. Neurol. 14:1160204. doi: 10.3389/fneur.2023.1160204
Received: 06 February 2023; Accepted: 30 March 2023;
Published: 20 April 2023.
Edited by:
Lisa C. Krishnamurthy, United States Department of Veterans Affairs, United StatesReviewed by:
Christofer Lundqvist, University of Oslo, NorwayCopyright © 2023 Giakas, Mangold, Androulakis, Hyduke, Galynker, Thiam, Cai and Androulakis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: X. Michelle Androulakis, eGlhby5hbmRyb3VsYWtpc0B2YS5nb3Y=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.