- 1School of Basic Medical Sciences, Shanghai University of Medicine and Health Sciences, Shanghai, China
- 2Institute of Wound Prevention and Treatment, Shanghai University of Medicine and Health Sciences, Shanghai, China
- 3Chongming Hospital Affiliated to Shanghai University of Medicine and Health Sciences, Shanghai, China
- 4Department of Adult Internal Medicine, Hubei Maternity and Child Health Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
The mechanism of sudden unexpected death in epilepsy (SUDEP) is elusive and many questions remain unanswered. Autopsy is generally unhelpful in providing evidence for the cause of death, as pathological changes may be on the molecular level. Although histopathological examination occasionally demonstrates pathology such as vascular malformation, old traumatic injury, and tumor, in most cases of SUDEP, the examination is negative. We examined the current status of SUDEP research by performing a bibliometric analysis of studies in the Web of Science Core Collection database published between 2002 and 2022. Our aim was to demonstrate areas of interest and frontiers of SUDEP research. A total of 1803 papers were included in the analysis. The number of published papers focused on SUDEP has been increasing since 2002. Main areas of interest include clinical manifestations, prevalence, treatment, and underlying mechanisms. Research teams from the United States and Europe are leading the way in SUDEP research, while Asia trails behind. Future studies regarding the mechanism and neuropathology of SUDEP are warranted.
1. Introduction
Public interest in sudden unexpected death in epilepsy (SUDEP) has increased in recent years (1). Autopsy findings do not distinguish SUDEP from non-SUDEP deaths in individuals with epilepsy (2). Although pathologic brain examination can occasionally identify epilepsy-related pathology such as vascular malformation, old traumatic brain injury, and brain tumor, most SUDEP cases have negative findings.
The annual incidence of SUDEP is ~1.2 in 1,000 adult patients with epilepsy (3). Previously, the incidence in children was estimated to be 0.22 per 1,000 patient-years (4, 5); however, the latest data suggests the rate is similar to that in adults (6). In a study of 1,086 SUDEP cases in the United States, males comprised 63.2% of cases and the median age at death was 39 years. Death was unwitnessed in 83.2% of cases and 77.1% occurred at home. Interestingly, ~50% of victims were found in bed and 42.4% were in the prone position (3). The incidence of epilepsy in children, adolescents and young adults has decreased over the last few decades because of improvements in medical care, sanitation, and control of infectious diseases (7). In contrast, incidence of epilepsy is increasing in the elderly because of its association with age-related diseases such as stroke and neurodegenerative disorders and recent increases in life expectancy (7). Approximately 10 million people are suffering from epilepsy in China (8), however, the detection rate of SUDEP is rarely reported.
Known mechanisms of SUDEP include persistent seizures, brain stem dysfunction, and cardiorespiratory inhibition; however, the cause of death in most cases is unexplained (9, 10). Underlying disease, fever, traumatic brain injury, drug withdrawal, infection, and metabolic insults have been reported as factors related to SUDEP. Convulsive seizure is thought to be a common risk factor. Progressive bradycardia occurs at the onset of convulsive seizure, followed by terminal apnea along with terminal asystole (11). In a mouse model of epilepsy, lesions in the ventrolateral medulla were associated with respiratory suppression in fatal seizure (12).
The diagnosis of SUDEP is challenging because no clear diagnostic criteria have been established. In the practice of legal medicine, SUDEP is a diagnosis of exclusion. Toxicology testing should be performed (2). Other potential causes of sudden death including coronary heart disease and stroke must be also eliminated. In many cases, SUDEP does not directly lead to death, however, it can give rise to accidental falls and trauma as well as drowning. The prevalence of SUDEP is underestimated (13). Previous studies have demonstrated that only ~30% of SUDEP cases are reported as SUDEP, seizure, or epilepsy (4, 14). Prevention of SUDEP-related death is imperative and has attracted worldwide concern. Primary care physicians can act to decrease epilepsy-related risks, most of which are non-neurological and preventable (1, 15).
Questions regarding the pathology, etiology, and mechanisms of SUDEP warrant further study. Here, we present a bibliometric analysis of the SUDEP literature published over the last two decades.
2. Materials and methods
2.1. Database and search strategy
We searched the Web of Science Core Collection databases, including the Science Citation Index and Social Science Citation Index, on October 1, 2022 to identify studies regarding SUDEP published from 2002 to 2022. The search strategy was (TS=sudden unexpected death in epilepsy OR TS=SUDEP) OR (TS=sudden unexpected death AND TS=epilepsy).
2.2. Eligibility criteria
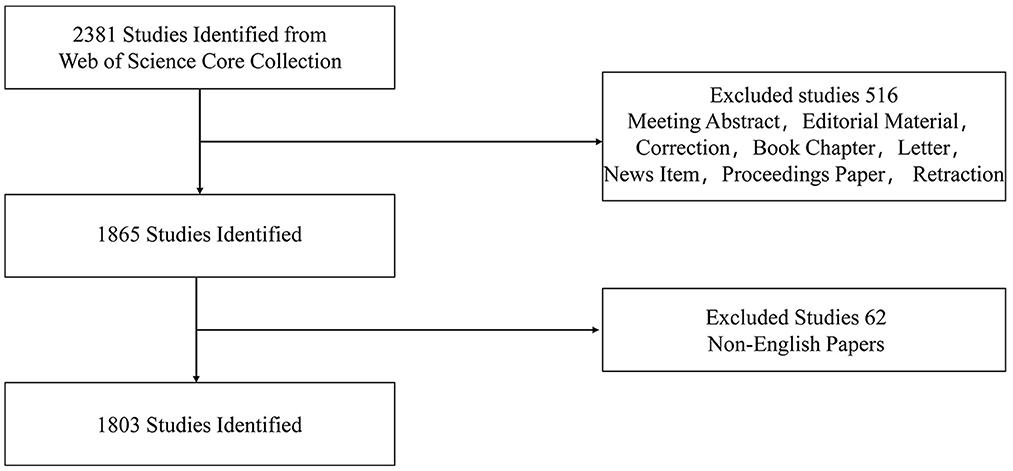
Mechanism and cohort studies associated with SUDEP and published in the English language were eligible for inclusion. Publication types included original articles, reviews, meeting papers, and online publications. Meeting abstracts, editorial materials, corrections, book chapters, letters, news items, proceedings papers, and retractions were excluded. The selection process is shown in Figure 1.
2.3. Data analysis
CiteSpace version 5.8.2 (https://sourceforge.net/projects/citespace/postdownload) and Graphpad Prism 9 were used for data analysis after initial screening. If we did not assure the article classification of subtopics based on the metadata, the full text was read in detail for manual classification. The following indicators were chosen for analyzing research trends in SUDEP: top 10 countries and institutions for publishing SUDEP articles, top 10 journals for publishing SUDEP articles, top 10 funding sources for SUDEP studies, top 10 most cited papers and authors, and top 25 keywords. Visual maps and tables related to these indicators were created using CiteSpace.
3. Results
Two thousand three hundred eighty-one studies were identified and evaluated. Five hundred sixteen papers which did not meet criteria were excluded. Sixty-two non-English papers were also removed. Finally, 1,803 were included in the bibliometric analysis. Original articles (1,384, 76.761%) were most common, followed by review papers (n = 389, 21.575%), meeting papers (n = 65, 3.605%), and online publications (n = 5, 0.277%).
3.1. Growth trends of annual publication and citation number
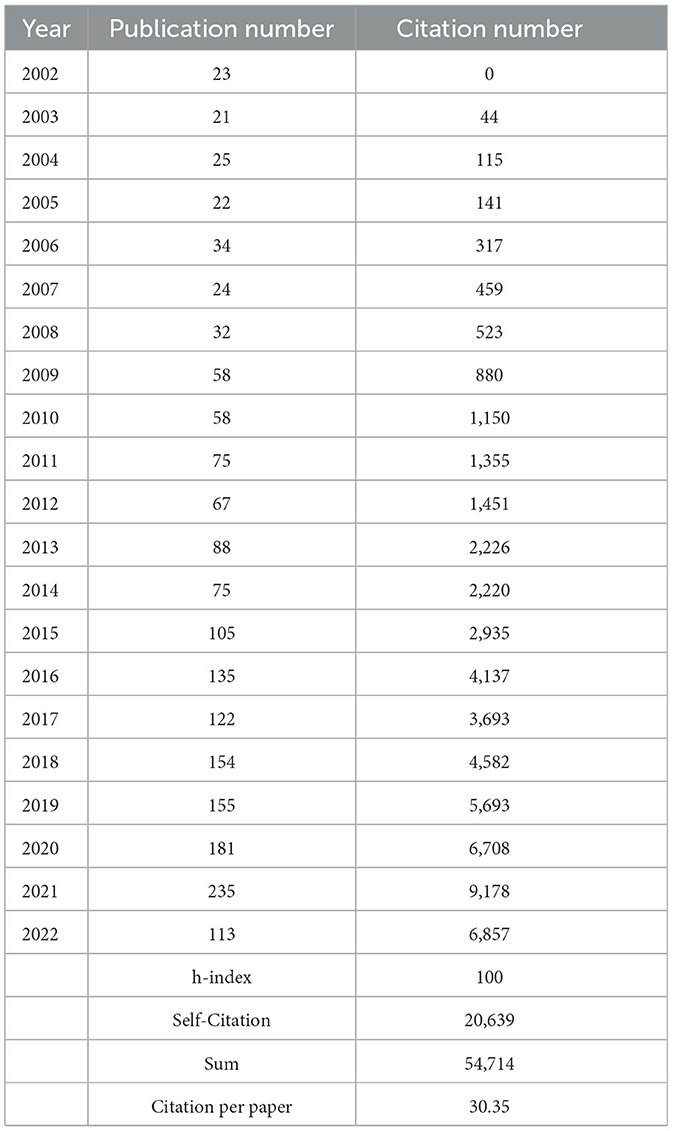
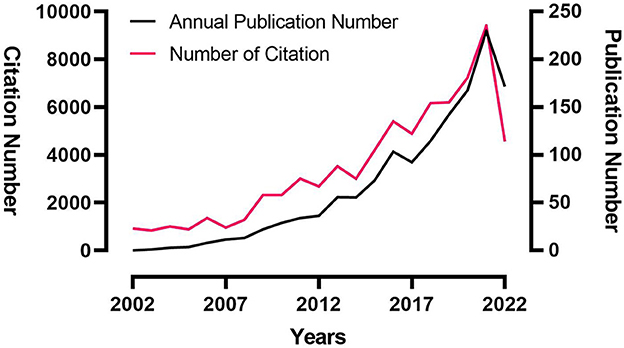
The growth trends of annual publication and citation numbers are shown in Table 1 and Figure 2. The number of annual publications related to SUDEP drastically increased with slight fluctuation over the last 20 years. Only 23 SUDEP papers were published in 2002, while 235 were published in 2021. One hundred fourteen articles had been published in 2022 prior to October 1. The citation number also increased from 0 in 2002 to 9178 in 2021, which paralleled the annual publication growth trend.
3.2. Main countries/regions and institutions
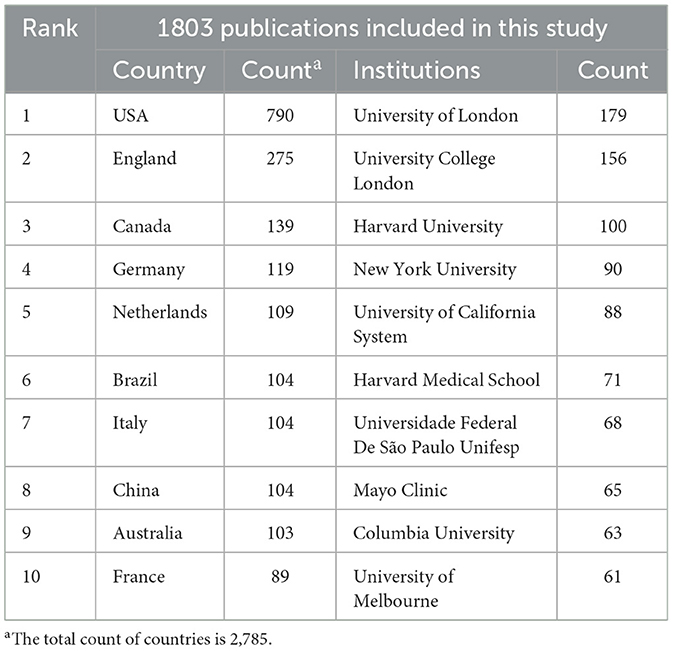
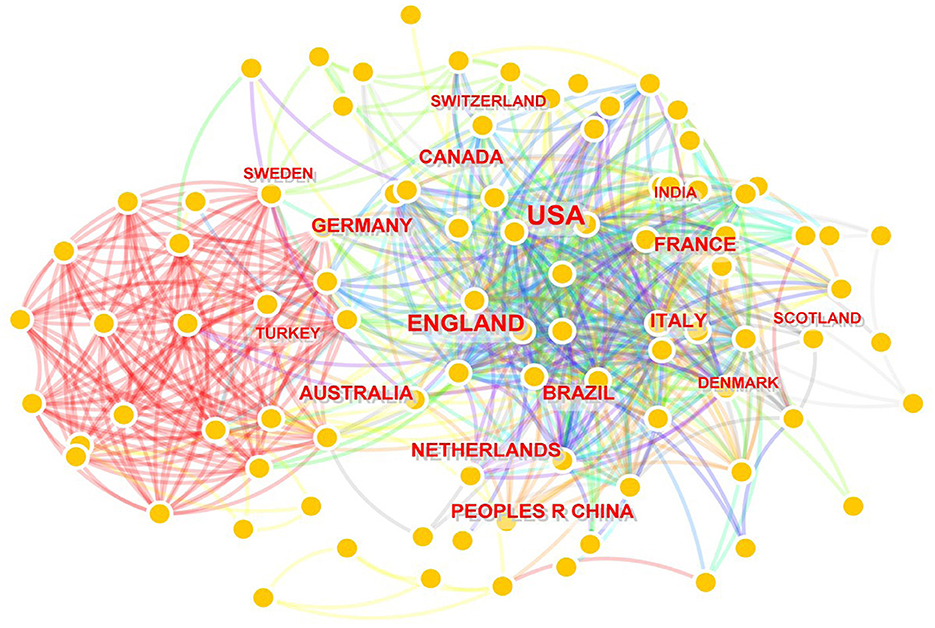
A total of 95 countries/regions and 2,198 institutions contributed to 1,803 scientific articles. The countries and institutions which published the highest number of SUDEP articles from 2002 to 2022 are shown in Table 2. The United States and England were the top two countries with 790 and 275 articles, respectively. Canada, Germany, the Netherlands, Brazil, Italy, China, Australia, and France contributed 119, 109, 104, 104, 104, 103, and 89 papers, respectively during the 20 years. The top two institutions, the University of London (n = 179) and University College London (n = 156), were both in England. Most of the other institutions in the list were from the United States, including Harvard University (n = 100), New York University (n = 90), University of California System (n = 88), Harvard Medical School (n = 71), Mayo Clinic (n = 65), and Columbia University (n = 63). Network maps of countries and institutions are shown in Figures 3, 4. The top 10 countries and institutions had considerable cross-references to each other.
3.3. Primary funding agencies
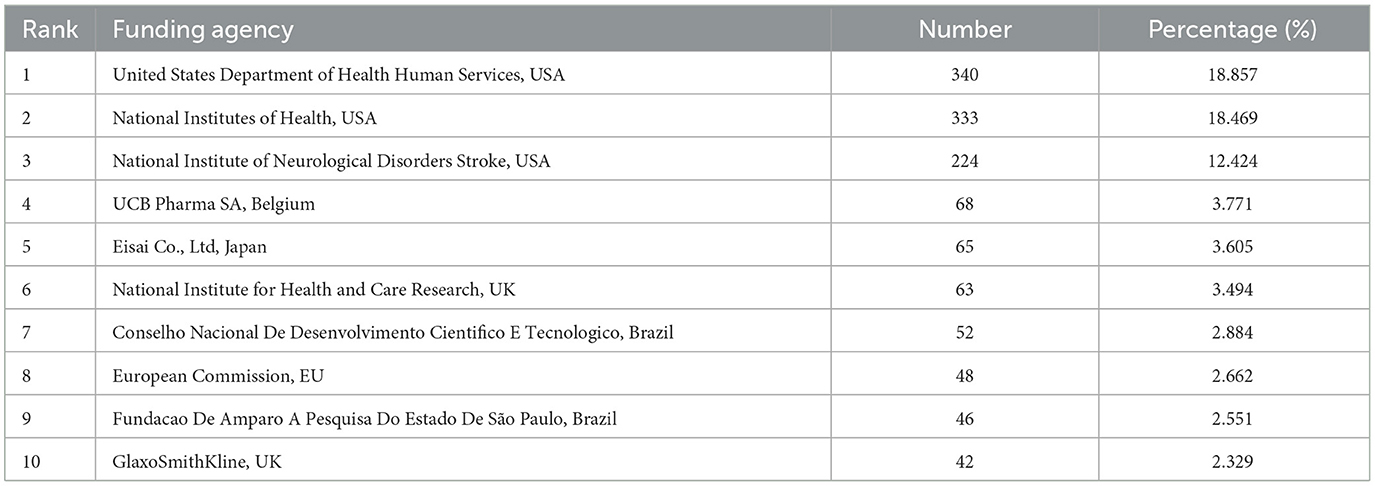
Among the 1,803 analyzed papers, 340 (18.875%) were funded by the United States Department of Health and Human Services. Three hundred thirty-three (18.469%) and 224 (12.424%) were supported by the National Institutes of Health and National Institute of Neurological Disorders and Stroke of the United States. The top three funding agencies supported approximately half of the SUDEP studies. Other studies were sponsored by UCB Pharma SA (Belgium), Eisai Co., Ltd (Japan), National Institute for Health and Care Research (UK), Conselho Nacional De Desenvolvimento Cientifico E Tecnologico (Brazil), European Commission (EU), Fundacao De Amparo A Pesquisa Do Estado De São Paulo (Brazil), and GlaxoSmithKline (UK). Further details are presented in Table 3.
3.4. Predominant journals
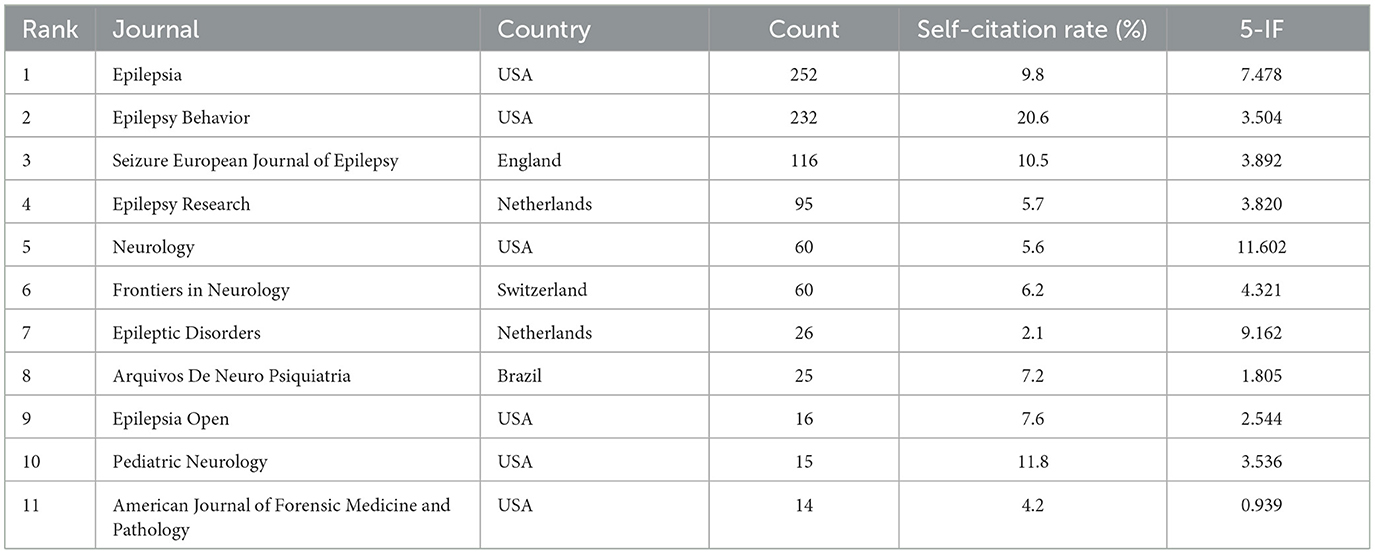
The SUDEP articles analyzed were published in 436 journals. Six journals published more than 50 papers during the 20-year period, and three published more than 100. According to Bradford's Law, 11 journals were considered core journals in the field of SUDEP (Table 4). Eight hundred and eleven papers were published in the top 11 journals, accounting for 50.5% of all. Among all the core journals, American Journal of Forensic Medicine and Pathology was the only one associated with forensic medicine. While the top 10 journals in the list were all specialized journals of neurology and the top three were epilepsy-specific. The impact factor of the listed journals ranged from 0.939 to 11.802.
3.5. Impactful articles and authors
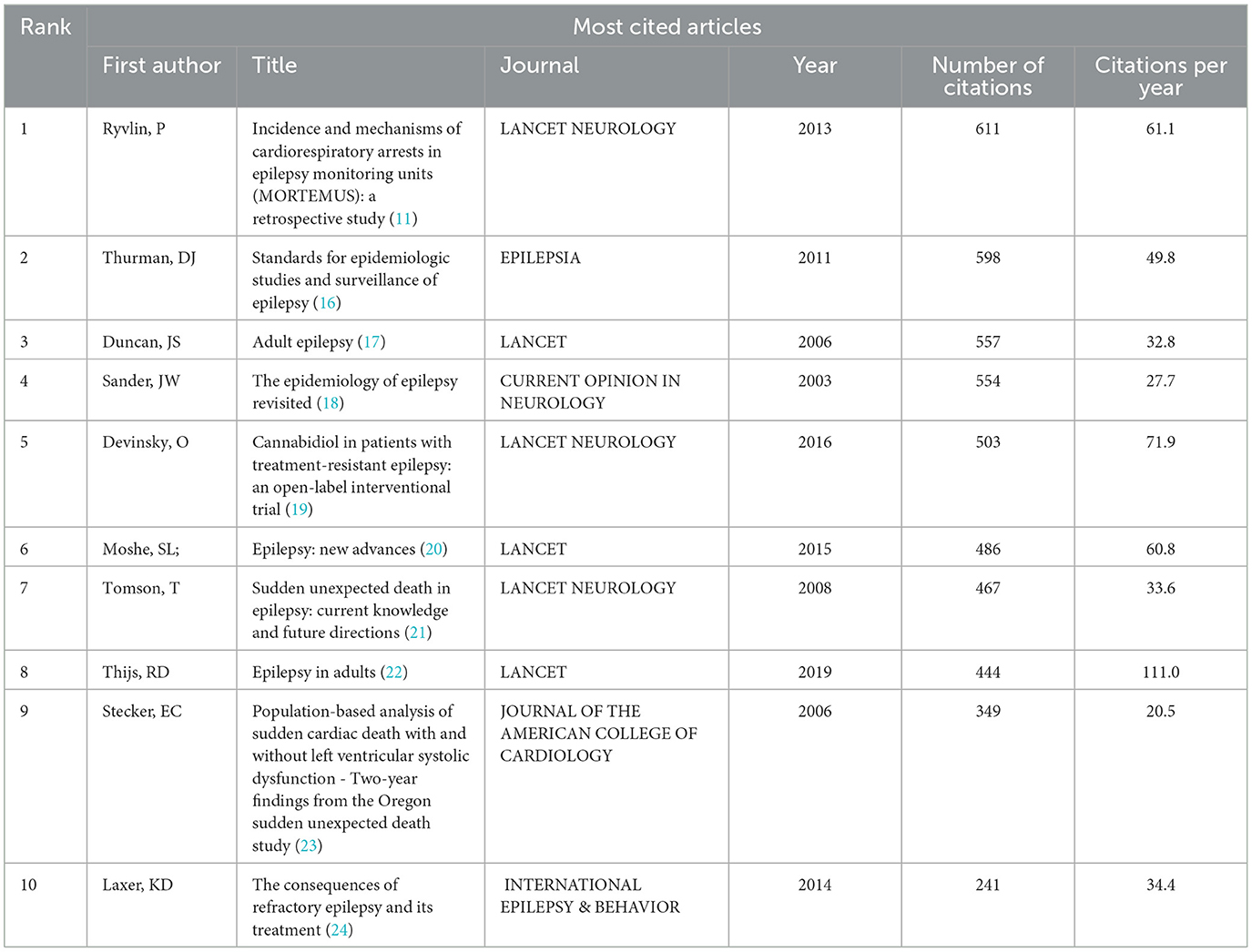
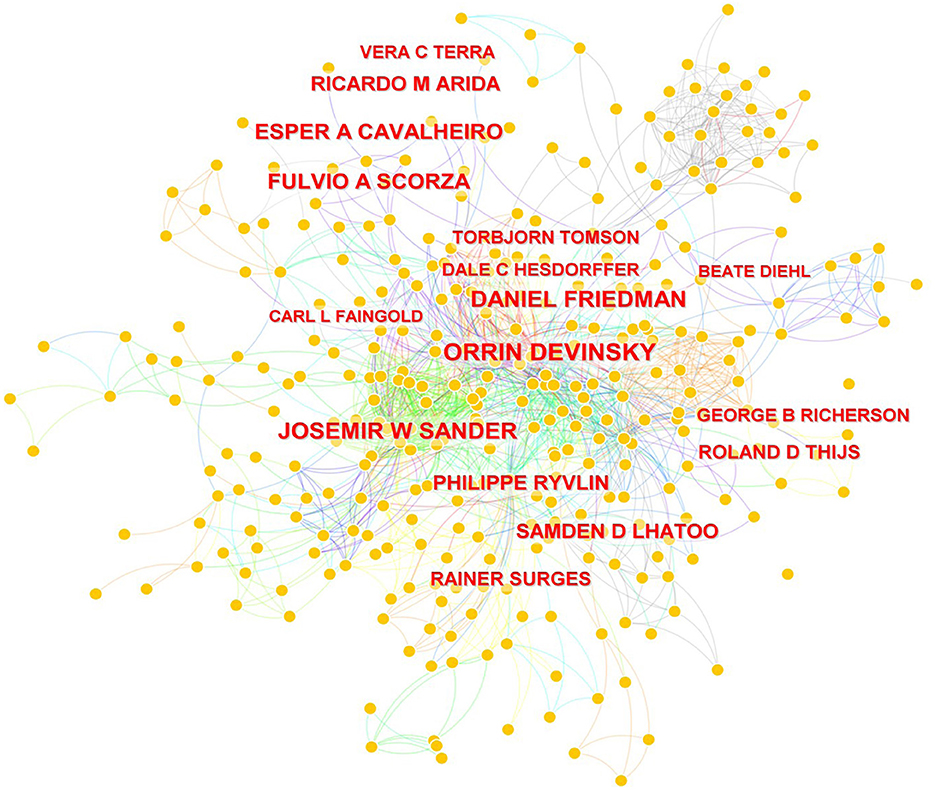
Eight papers were cited more than 400 times and three more than 500. The most-cited paper was “Incidence and mechanisms of cardiorespiratory arrest in epilepsy monitoring units (MORTEMUS): a retrospective study,” which was published in Lancet Neurology in 2013 and cited 611 times. The journals which published the top 10 most-cited articles included Lancet Neurology, Epilepsia, Lancet, Current Opinion in Neurology, Journal of the American College of Cardiology, and International Epilepsy & Behavior. The most-cited papers are listed in Table 5. The impact of the 742 authors who published SUDEP research is visualized in Figure 5, which demonstrates the co-occurrence among authors. The impact of an author is positively associated with the name size exhibited in the figure. Orrin Devinsky, Josmir W Sander, Daniel Friedman, Fulvio A Scozar, and Esper A Cavalheiro, were the top impactful authors.
3.6. Top keywords and analysis
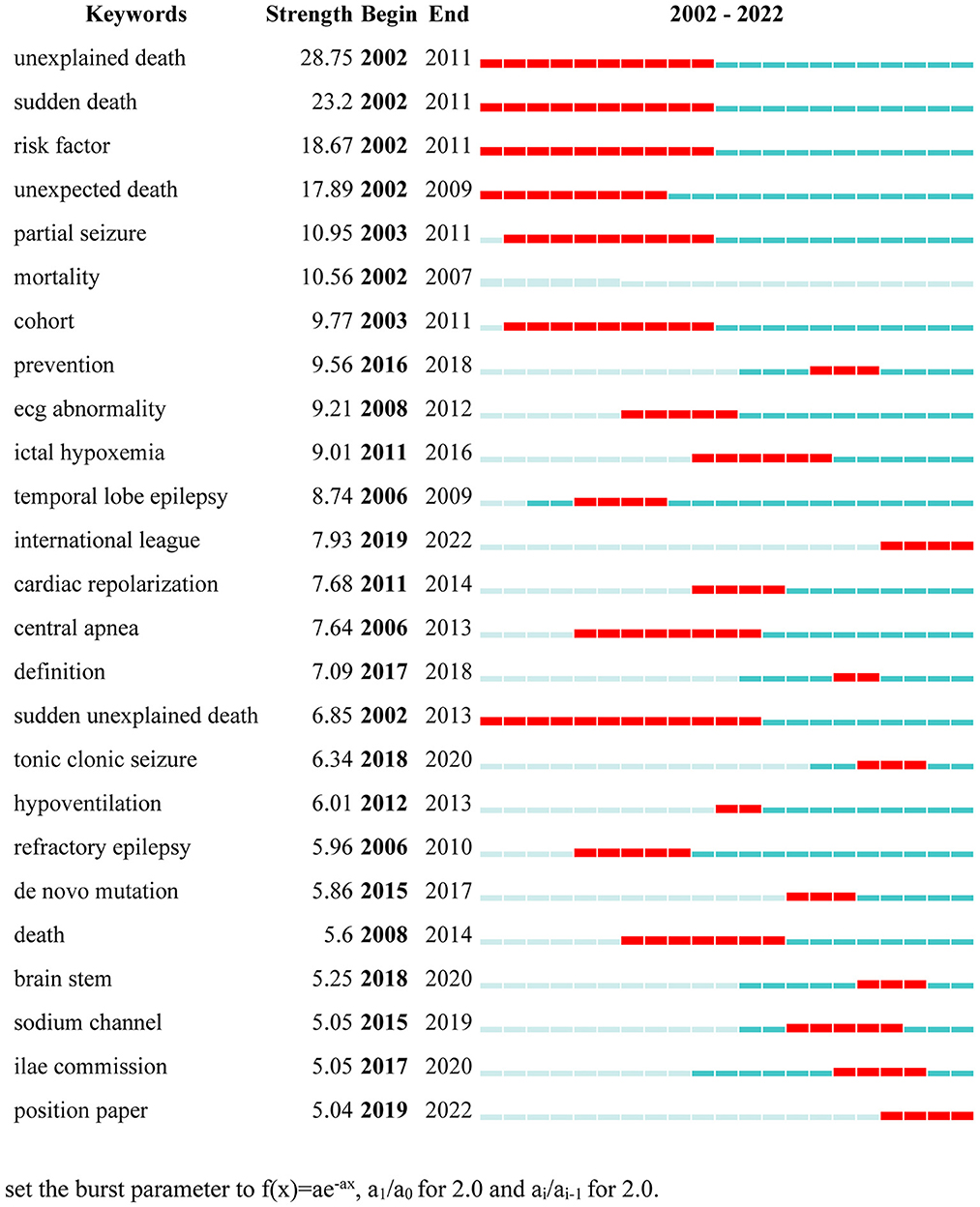
Keywords were extracted from the SUDEP articles and 25 burst words were exported after CiteSpace analysis. Keywords with the strongest citation burst are listed in Figure 6. Burst words significantly changed over the 20-year period. “Unexplained death” and “sudden death” were the top two strongest keywords in the list, emerging from 2002 to 2010 and 2002 to 2011, respectively, with burst intensities of 28.75 and 23.2. The third-ranked keyword was “risk factor” with a strength of 18.67.
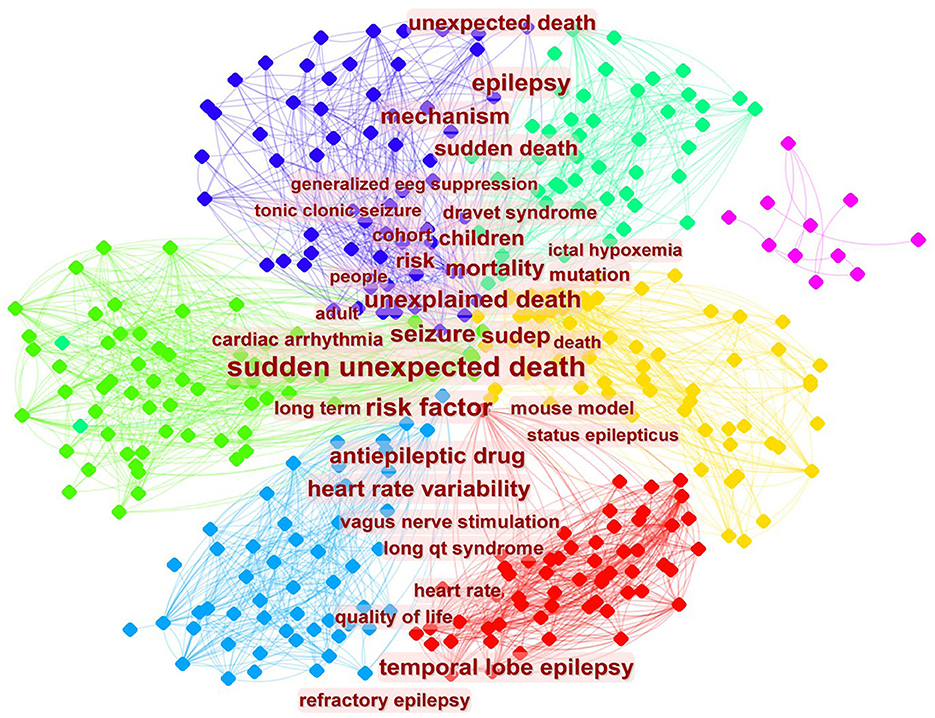
Clustering analysis on the co-occurrence of keywords is shown in Figure 7. The figure demonstrates many important issues of co-occurrence such as sudden unexpected death, seizure, unexplained death, children, risk factor, heart rate variability, temporal lobe epilepsy, and mechanism.
4. Discussion
The results from this bibliometric analysis demonstrate that SUDEP attracted growing research attention from 2002 to 2022. The number of SUDEP articles published in 2021 was 10 times higher than that published in 2002. The burst of papers is partly related to increasing support from official agencies. National Institutes of Health funding for SUDEP increased by 10,000-fold between 2009 and 2016 (3), and the number has increased by 2.5-fold from 2016 to 2022 (25). United States funding agencies supported the most SUDEP research, followed by the United Kingdom, Japan, European Union, and Brazil. Chinese funding agencies did not make it into the top 10, which is unparallel to their greater support for other fields of research (26).
From 2002 to 2022, the United States and European countries were the predominant drivers in SUDEP research. However, developing countries including China and Brazil also participate. Both countries contributed 104 articles over the 20-year period examined and rank in the top 10. Although institutions from the United States published the highest number of articles in the period, the top two institutions are located in the United Kingdom and three institutions from the top 10 are in London. Institutions from the United States account for six positions in the top 10. An institution from Brazil, Universida de Federal de São Paulo, published 68 papers in the 20-year period and is ranked seventh; this was the only developing country institution in the top 10. Surprisingly, institutions from the European Union were absent from the top 10.
Our results also demonstrate that the most important journals publishing SUDEP research are Epilepsia and Epilepsy Behavior. Epilepsia published the highest number of articles, accounting for 14%. The top 10 journals combined published 49.7% of all SUDEP papers. Most journals publishing SUDEP articles focus on neurology and some specialize in epilepsy or seizure. Diagnosis of SUDEP is extremely difficult in the practice of forensic medicine and should be paid great attention. American Journal of Forensic Medicine and Pathology is one of the core journals of SUDEP according to the Bradford's Law, publishing 14 papers regarding SUDEP in the two decades. We hope that more practitioners in forensic medicine can take part in the research of SUDEP.
The most impactful article was “Incidence and mechanisms of cardiorespiratory arrests in epilepsy monitoring units (MORTEMUS): a retrospective study,” written by Ryvlin et.al. They retrospectively collected and analyzed data from all cardiorespiratory arrests associated with SUDEP in numerous epilepsy monitoring units in Europe, Israel, Australia, and New Zealand (11). They proposed improving supervision at night to prevent immediate cardiorespiratory dysfunction induced by unpredictable seizures (11). The second most-cited paper was a guideline, ‘Standards for epidemiologic studies and surveillance of epilepsy' published in Epilepsia. In this article (16), Thurman et.al. discussed the following issues: (1) conceptual and operational definitions of epilepsy, (2) data resources and recommended data elements, and (3) methods and analyses appropriate for epidemiologic studies or epilepsy surveillance. The paper is instructional for designing studies with different purposes and provides variant methods for data retrieval based on the particular needs of different study teams.
Keyword frequency can reflect study interests within a particular research field. According to our results, the hotspots in SUDEP research predominantly focus on mortality, epidemiology, and clinical manifestations. The results demonstrated in the list of burst keywords are in accordance with the hotspots figure. Most research did not pay attention to the etiology of SUDEP. Issues such as disease mechanism and neuropathology were not sufficiently studied during the period, which hinders a deeper understanding of the disease. Although postmortem examinations are likely to be unhelpful in SUDEP cases, occasionally they can provide interesting findings. In one case report (27), a capillary telangiectasia was observed in the hippocampus in a patient who died of unexplained seizures, implying that hippocampal pathology could induce fatal epilepsy. Some study teams start to study SUDEP at the molecular level in the near 10 years. Indeed, keywords of de novo mutation and sodium channel emerged in 2015, which suggests that research on SUDEP is reaching the deep-water zone. Overall, the etiology of SUDEP includes a series of different factors and cannot be explained by a single theory. Despite the low detection rate, we still recommend performing systematic pathological examination in all suspected cases of SUDEP. Furthermore, brain tissue, cerebrospinal fluid, and serum should be stored in a special SUDEP tissue bank to enable further studies at the molecular level.
We also propose that the Chinese government increase SUDEP funding and increase the autopsy rate in SUDEP cases. A better understanding of SUDEP can prolong life expectancy and enhance quality of life. The low autopsy rate is hindering China from making progress in SUDEP as well as other fields of research. Developed countries pay greater attention to autopsies for all deaths: in 2019, the autopsy rate in the Commonwealth of Nations and the World Health Organization European Region was 43.4 and 25.9%, respectively (28). In the United States, the autopsy rate was 50% in the 1940s but drastically declined to 8% in 2018 (29). Only 1.6% of all deaths in Japan were autopsied in 2014, the lowest among developed countries (30). Unfortunately, the percentage in China is even lower—from 1990 to 2011, the autopsy rate in large teaching hospitals in China was <1% and some hospitals performed no autopsies (31). Therefore, we can speculate that the overall autopsy rate in China is extremely low. If China increased the national autopsy rate to 10%, they would be able to make considerable contributions to SUDEP research.
5. Conclusion
The number of published papers focused on SUDEP has been increasing since 2002. Current study interests involve clinical manifestations, prevalence, treatment, and underlying mechanisms. Research teams from the United States and Europe are leading the way in SUDEP research, while Asia trails behind. Systematic pathological examination could increase the understanding of SUDEP. Tissue banks of SUDEP could be established to enable further studies at the molecular level. Studies which focus on mechanisms and neuropathology are warranted to improve our understanding of this disease.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
FT, YL, and ZY designed the framework of the review and drafted the manuscript. FT, ZZ, JL, ZY, YL, and QW provided supervision and contributed to manuscript writing and editing. All authors have read and approved the latest version of the manuscript.
Funding
This work was funded by the Shanghai Sailing Plan (21YF1418800), Innovative Foundation Project for Students of Shanghai University of Medicine and Health Sciences (202210262058 and A3-0200-22-309009-190), and Discipline Construction Projects of Institute of Wound Prevention and Treatment, Shanghai University of Medicine and Health Sciences (HXXM-22-08-004).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer YZ declared a shared affiliation with the author QW to the handling editor at the time of review.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Panelli RJ. SUDEP: A global perspective. Epilepsy Behav. (2020) 103:106417. doi: 10.1016/j.yebeh.2019.07.018
2. Nashef L, So EL, Ryvlin P, Tomson T. Unifying the definitions of sudden unexpected death in epilepsy. Epilepsia. (2012) 53:227–33. doi: 10.1111/j.1528-1167.2011.03358.x
3. Cihan E, Devinsky O, Hesdorffer DC, Brandsoy M, Li L, Fowler DR, et al. Temporal trends and autopsy findings of SUDEP based on medico-legal investigations in the United States. Neurology. (2020) 95:e867–77. doi: 10.1212/WNL.0000000000009996
4. Sveinsson O, Andersson T, Carlsson S, Tomson T. The incidence of SUDEP: A nationwide population-based cohort study. Neurology. (2017) 89:170–7. doi: 10.1212/WNL.0000000000004094
5. Harden C, Tomson T, Gloss D, Buchhalter J, Cross JH, Donner E, et al. Practice guideline summary: Sudden unexpected death in epilepsy incidence rates and risk factors: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Neurology. (2017) 88:1674–80. doi: 10.1212/WNL.0000000000003685
6. Keller AE, Whitney R, Li SA, Pollanen MS, Donner EJ. Incidence of sudden unexpected death in epilepsy in children is similar to adults. Neurology. (2018) 91:e107–11. doi: 10.1212/WNL.0000000000005762
7. Feigin VL, Roth GA, Naghavi M, Parmar P, Krishnamurthi R, Chugh S, et al. Global burden of stroke and risk factors in 188 countries, during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet Neurol. (2016) 15:913–24. doi: 10.1016/S1474-4422(16)30073-4
8. Ding D, Zhou D, Sander JW, Wang W, Li S, Hong Z, et al. Epilepsy in China: major progress in the past two decades. Lancet Neurol. (2021) 20:316–26. doi: 10.1016/S1474-4422(21)00023-5
9. Thurman DJ, Logroscino G, Beghi E, Hauser WA, Hesdorffer DC, Newton CR, et al. The burden of premature mortality of epilepsy in high-income countries: A systematic review from the Mortality Task Force of the International League Against Epilepsy. Epilepsia. (2017) 58:17–26. doi: 10.1111/epi.13604
10. Levira F, Thurman DJ, Sander JW, Hauser WA, Hesdorffer DC, Masanja H, et al. Premature mortality of epilepsy in low- and middle-income countries: A systematic review from the Mortality Task Force of the International League Against Epilepsy. Epilepsia. (2017) 58:6–16. doi: 10.1111/epi.13603
11. Ryvlin P, Nashef L, Lhatoo SD, Bateman LM, Bird J, Bleasel A, et al. Incidence and mechanisms of cardiorespiratory arrests in epilepsy monitoring units (MORTEMUS): a retrospective study. Lancet Neurol. (2013) 12:966–77. doi: 10.1016/S1474-4422(13)70214-X
12. Jansen NA, Schenke M, Voskuyl RA, Thijs RD, van den Maagdenberg A, Tolner EA, et al. Apnea associated with brainstem seizures in Cacna1a(S218L) mice is caused by medullary spreading depolarization. J Neurosci. (2019) 39:9633–44. doi: 10.1523/JNEUROSCI.1713-19.2019
13. Keller AE, Ho J, Whitney R, Li SA, Williams AS, Pollanen MS, et al. Autopsy-reported cause of death in a population-based cohort of sudden unexpected death in epilepsy. Epilepsia. (2021) 62:472–80. doi: 10.1111/epi.16793
14. Chen S, Joodi G, Devinsky O, Sadaf MI, Pursell IW, Simpson RJ, et al. Under-reporting of sudden unexpected death in epilepsy. Epileptic Disord. (2018) 20:270–8. doi: 10.1684/epd.2018.0979
16. Thurman DJ, Beghi E, Begley CE, Berg AT, Buchhalter JR, Ding D, et al. Standards for epidemiologic studies and surveillance of epilepsy. Epilepsia. (2011) 52 Suppl 7:2–26. doi: 10.1111/j.1528-1167.2011.03121.x
18. Sander JW. The epidemiology of epilepsy revisited. Curr Opin Neurol. (2003) 16:165–70. doi: 10.1097/00019052-200304000-00008
19. Devinsky O, Marsh E, Friedman D, Thiele E, Laux L, Sullivan J, et al. Cannabidiol in patients with treatment-resistant epilepsy: an open-label interventional trial. Lancet Neurol. (2016) 15:270–8. doi: 10.1016/S1474-4422(15)00379-8
20. Moshé SL, Perucca E, Ryvlin P, Tomson T. Epilepsy: new advances. Lancet (London, England). (2015) 385:884–98. doi: 10.1016/S0140-6736(14)60456-6
21. Tomson T, Nashef L, Ryvlin P. Sudden unexpected death in epilepsy: current knowledge and future directions. Lancet Neurol. (2008) 7:1021–31. doi: 10.1016/S1474-4422(08)70202-3
22. Thijs RD, Surges R, O'Brien TJ, Sander JW. Epilepsy in adults. Lancet (London, England). (2019) 393:689–701. doi: 10.1016/S0140-6736(18)32596-0
23. Stecker EC, Vickers C, Waltz J, Socoteanu C, John BT, Mariani R, et al. Population-based analysis of sudden cardiac death with and without left ventricular systolic dysfunction: two-year findings from the Oregon Sudden Unexpected Death Study. J Am Coll Cardiol. (2006) 47:1161–6. doi: 10.1016/j.jacc.2005.11.045
24. Laxer KD, Trinka E, Hirsch LJ, Cendes F, Langfitt J, Delanty N, et al. The consequences of refractory epilepsy and its treatment. Epilepsy Behav. (2014) 37:59–70. doi: 10.1016/j.yebeh.2014.05.031
25. Research Portfolio Online Reporting Tools,. US Department of Health Human Services. (2015). Available online at: projectreporter.nih.gov (accessed on December 16, 2022).
26. Granting Status of National Natural Science Foundation of China. National Natural Science Foundation of China. (2022). Available online at: https://www.nsfc.gov.cn/publish/portal0/tab505/ (accessed on December 29, 2022).
27. Liu Y, Liang Y, Tong F, Huang W, Tinzing L, Le Grange JM, et al. Sudden death from an epileptic seizure due to capillary telangiectasias in the hippocampus. Forensic Sci Med Pathol. (2019) 15:243–8. doi: 10.1007/s12024-018-0075-7
28. Autopsy Rate (%) for all Deaths (2022),. World Health Organization European Region. Available online at: https://gateway.euro.who.int/en/indicators/hfa_545-6410-autopsy-rate-for-all-deaths/ (accessed on December 30, 2022).
29. Goldman L. Autopsy 2018: still necessary, even if occasionally not sufficient. Circulation. (2018) 137:2686–8. doi: 10.1161/CIRCULATIONAHA.118.033236
30. Ikegaya H. Criminology: Update forensics for deaths in Japan. Nature. (2014) 507:306. doi: 10.1038/507306e
Keywords: SUDEP, epilepsy, bibliometric analysis, research interest, English literature, autopsy rate
Citation: Tong F, Lin J, Zeng Z, Wang Q, Yang Z and Lv Y (2023) Sudden unexpected death in epilepsy: A bibliometric overview. Front. Neurol. 14:1139521. doi: 10.3389/fneur.2023.1139521
Received: 07 January 2023; Accepted: 30 January 2023;
Published: 23 February 2023.
Edited by:
Beixu Li, Shanghai University of Political Science and Law, ChinaReviewed by:
Kang Wang, Nanjing Medical University, ChinaYiwu Zhou, Huazhong University of Science and Technology, China
Zhengdong Li, Academy of Forensic Science, China
Copyright © 2023 Tong, Lin, Zeng, Wang, Yang and Lv. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhifang Yang,  eWFuZ3pmQHN1bWhzLmVkdS5jbg==; Yehui Lv,
eWFuZ3pmQHN1bWhzLmVkdS5jbg==; Yehui Lv,  bHZ5aF8xNUBzdW1ocy5lZHUuY24=
bHZ5aF8xNUBzdW1ocy5lZHUuY24=
 Fang Tong
Fang Tong Jian Lin
Jian Lin Zixuan Zeng1
Zixuan Zeng1 Yehui Lv
Yehui Lv