- 1Department of Neurosurgery, The First Hospital of Jilin University, Changchun, China
- 2Department of Neurosurgery, Sichuan Provincial People’s Hospital, University of Electronic Science and Technology of China, Chengdu, China
- 3Department of Hepatobiliary Surgery, Zhijin County People's Hospital, Bijie, China
Hypertensive cerebral hemorrhage, the most common prevalent of spontaneous cerebral hemorrhage, poses a significant threat to patient mortality and morbidity, while therapeutic options remain limited, making the disease a burden not only for patients’ families but also a major challenge for national healthcare systems. The elevation of intracranial pressure subsequent to hypertensive cerebral hemorrhage is a critical contributor to mortality. However, it often manifests before the onset of clinical symptoms, which are typically atypical, leading to delayed treatment and irreversible consequences for the patient. Hence, early detection of intracranial pressure variations can aid in timely, efficient, and precise treatment, reducing patient mortality. Invasive intracranial pressure monitoring enables real-time, accurate monitoring of intracranial pressure changes, providing clinicians with therapeutic guidance and overcoming the limitations of empirical treatment. This article aims to review the use of invasive intracranial pressure monitoring in postoperative hypertensive cerebral hemorrhage and hopes to contribute to clinical and scientific research.
Introduction
Cerebral hemorrhage represents a significant acute disease with a high rate of mortality and disability rate, comprising 10–15% of all stroke subtypes (1, 2). Hypertensive cerebral hemorrhage, accounting for the majority of spontaneous cerebral hemorrhages, is frequently associated with a history of hypertension in up to 70% of cases (3, 4). After hypertension-induced rupture of a cerebral blood vessel, blood penetrates the brain parenchyma, resulting in hematoma formation. On the one hand, this is the main cause of brain injury, as the hematoma occupies and compresses surrounding healthy brain tissue, causing destruction. On the other hand, the formation and retraction of the hematoma, as well as the extravasation of plasma proteins, can cause cerebral edema around the hematoma, which leads to a decrease in hydrostatic pressure around the hematoma space (5), The interaction between these factors can cause a pathological increase in intracranial pressure, ultimately leading to perihematomal edema (6, 7). Intracranial hypertension is common after cerebral hemorrhage, particularly in young and supratentorial cerebral hemorrhage patients (8). Intracranial hypertension is independently associated with patient clinical prognosis and mortality (9), Changes in intracranial pressure precede the onset of clinical signs and symptoms, emphasizing the critical importance of accurate and real-time monitoring of intracranial pressure to guide clinical treatment. This article reviews invasive intracranial pressure monitoring, which is widely utilized in clinical practice and has a high degree of accuracy.
Literature search
PubMed, Medline, and Embase were utilized as search tools to identify relevant studies and articles, with the final search conducted on April 1st, 2023. The following search terms were employed: “intracerebral hemorrhage,” “cerebral hemorrhage,” “hypertensive intracerebral hemorrhage,” “hypertensive cerebral hemorrhage,” “intracranial pressure,” “ICP,” “intracranial pressure monitoring,” and “invasive intracranial pressure monitoring.” The exclusion criteria comprised all article types not written in the English language and/or without a full-text publication, single case reports, and those that included pediatric patients.
Search results
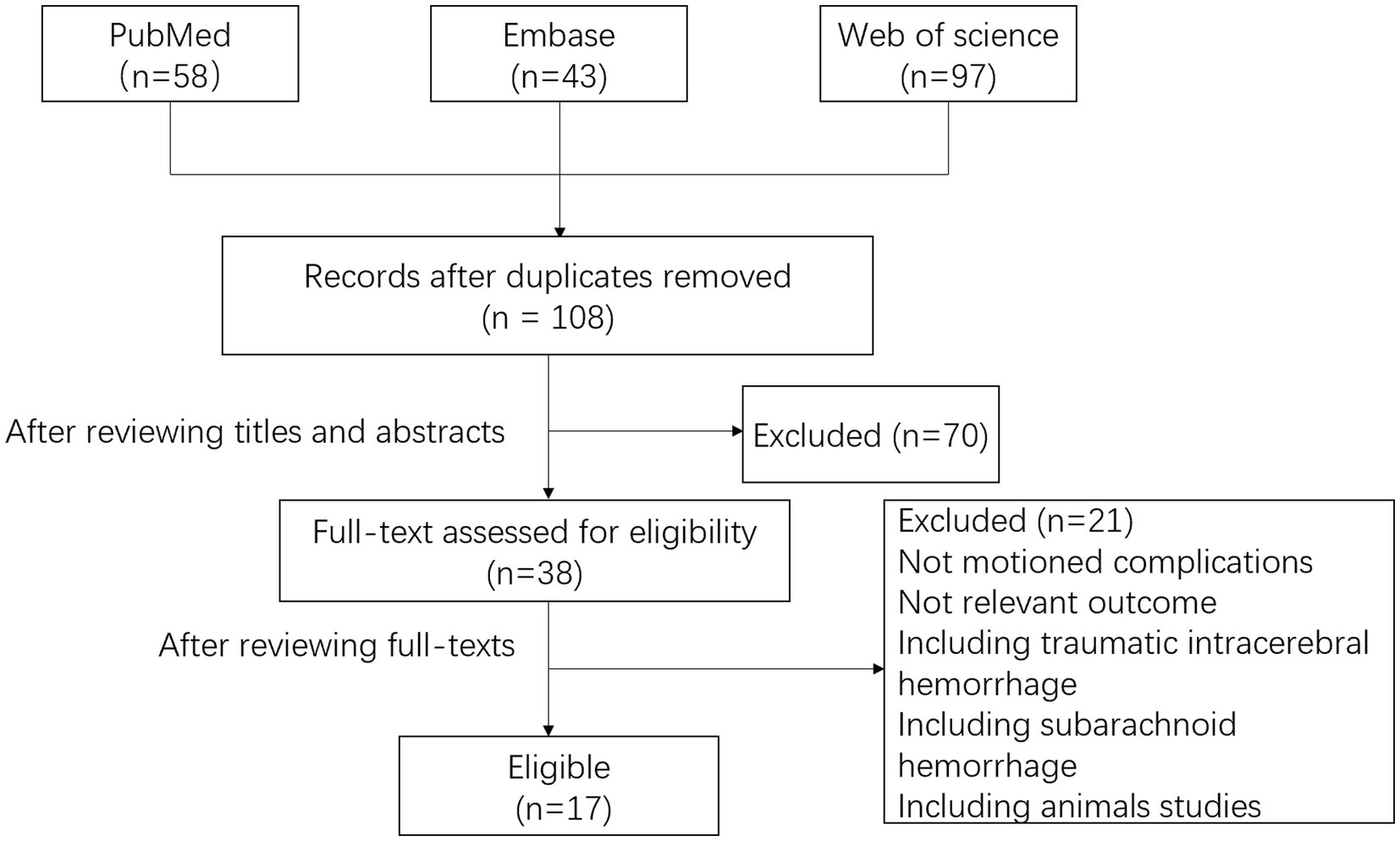
From the aforementioned search parameters, Figure 1 shows the study screening and selection process. The systematic database search yielded 58, 97, and 43 records from the PubMed, Web of Science, and Embase databases, respectively. After excluding duplicates and reviewing titles and abstracts, 38 articles were considered potential studies on invasive intracranial pressure monitoring following surgery for hypertensive cerebral hemorrhage. After reviewing the full-text, we have identified 17 primary studies that conform to the inclusion criteria and provide a comprehensive analysis of the monitoring techniques, monitoring duration, associated complications, and study conclusions. This data has been succinctly summarized in Table 1.
The significance of intracranial pressure for the patient
Intracranial pressure refers to the force exerted by the contents of the cranial cavity on the surrounding lining. The cerebrospinal fluid plays a crucial role in maintaining a stable intracranial pressure, and any disruptions between its production and absorption can affect the pressure (10). For patients suffering from cerebral hemorrhage, analyzing and measuring intracranial pressure can be essential for determining the most effective therapeutic management measures (11). By measuring the intracranial pressure, the patient’s cerebral perfusion pressure can be estimated using the formula: cerebral perfusion pressure = mean arterial pressure−mean intracranial pressure. An increase in intracranial pressure may hinder blood flow, leading to ischemia, while an increase in cerebrovascular perfusion pressure may result in overperfusion, vasogenic edema, and secondary effects due to increased intracranial pressure (12). Intracranial hypertension is a significant cause of secondary brain injury and is also closely related to poor prognosis. Regular monitoring of intracranial pressure and cerebral perfusion pressure may therefore alter the prognosis of patients with brain injury (13–15). However, assessing changes in intracranial pressure and cerebral perfusion pressure from clinical observations of the patient’s state of consciousness and radiological changes can be challenging (8).
Optimal duration of invasive intracranial pressure monitoring and the most common complications
There are no established guidelines or expert consensus regarding the optimal duration of intracranial pressure monitoring. A retrospective study conducted by Julien Dimitriou et al. revealed that the use of intracranial pressure monitoring for more than 5 days increased the risk of infection (16). It has also been suggested that the risk of infection associated with intracerebroventricular pressure monitoring increases after 5 days, with an overall infection rate of approximately 5%. However, the risk of infection with parenchymal monitoring is lower than that of intracerebroventricular monitoring (12). Therefore, the five-day mark may be an optimal time point for intracranial pressure monitor placement, but further studies are necessary to validate this conclusion. Infection is the most frequent complication associated with invasive intracranial pressure monitoring. In a study of 123 patients who underwent parenchymal intracranial pressure monitoring, only one case of infection was reported, compared to 16 out of 173 patients who underwent extra-ventricular drainage, and the duration of catheterization was found to be associated with the infection rate (16). Moreover, a meta-analysis indicated that the use of intracranial pressure monitoring was linked to a reduced rate of infection and an improved prognosis compared to the group without intracranial pressure monitoring (17). In a retrospective study of 213 patients with traumatic brain injury who had undergone invasive intracranial pressure monitoring, Alexander Bumberger et al. concluded that although there may be some complications associated with this method, they are acceptable. Furthermore, invasive intracranial pressure monitoring reduces the number of cranial CT scans performed on patients with increased intracranial pressure or those with a declining level of consciousness. This, in turn, lowers the number of patient evacuations and the hazards associated with transportation (18). A meta-analysis demonstrated that aggressive intracranial pressure monitoring and treatment resulted in a better prognosis for patients (19).
The need for intracranial pressure monitoring in patients with hypertensive cerebral hemorrhage
Hypertensive cerebral hemorrhage results from the rupture of a blood vessel in the brain due to hypertension, leading to the accumulation of blood in brain tissue and the formation of a hematoma. This, in turn, causes distortion and deformation of the brain tissue (20). Regardless of whether conservative medication or surgery is used for treatment, hematoma formation is inevitable following cerebral hemorrhage. On the one hand, the hematoma compresses the healthy brain tissue surrounding it, leading to tissue death, while, on the other hand, the secondary damage caused by the mechanical effect of the expanding hematoma and the toxic effect of its degradation products on the surrounding brain tissue leads to the formation of peri-hematoma edema (21, 22). Furthermore, hypertensive cerebral hemorrhage usually affects deep brain structures such as the basal ganglia and thalamus (23). This poor functional prognosis is due to the presence of crucial neural nuclei in the deep brain. Hematomas after cerebral hemorrhage may compress the circulatory pathways of the cerebrospinal fluid, leading to obstructive hydrocephalus (24). The growth of the acute hematoma, the enlargement of the ventricles, and the edema of the tissue surrounding the hematoma all contribute to the deterioration of the patient’s neurological function (25). The occupying effect of the hematoma, progressive perihematomal edema, and hematoma widening can cause a reduction in cerebral perfusion pressure, an increase in intracranial pressure, and even cerebral herniation (26). Recurrence of hemorrhage, edema and hydrocephalus after hypertensive cerebral hemorrhage can all causes an increase in intracranial pressure and a deterioration in the patient’s level of consciousness. However, changes in intracranial pressure occur prior to the onset of clinical signs and symptoms in patients. For patients undergoing intracranial pressure monitoring, a quick review of cranial Computed Tomography can be performed at the time of intracranial pressure elevation so that patients can receive treatment before their condition worsens.
Methods of invasive intracranial pressure monitoring
In current clinical practice, methods for measuring intracranial pressure include both invasive and non-invasive techniques. Although non-invasive intracranial pressure monitoring has the advantage of not causing trauma or complications to patients due to the placement of monitor sensors, its inaccuracy and unreliability have limited its widespread use (27). The potential for inaccurate intracranial pressure readings to mask a patient’s critical condition and mislead clinicians underscores the importance of using invasive intracranial pressure monitoring as the main method for dynamic, real-time clinical monitoring of intracranial pressure changes. Despite the availability of various non-invasive intracranial pressure measurement methods, none of them can provide the same level of accuracy as invasive intracranial pressure monitoring (28). Therefore, invasive intracranial pressure monitoring continues to be the preferred method, requiring the insertion of a sensor probe into the brain parenchyma or ventricles using a cranial drill.
Intracerebroventricular pressure monitoring: invasive intracranial pressure monitoring, combined with extra-ventricular drainage, is considered the gold standard for monitoring intracranial pressure (29, 30). This technique involves inserting a catheter into one of the lateral ventricles, with the external transducer placed at the same level as the Monro foramen (31). This method has various advantages. Firstly, the measurement of pressure can be used as a therapeutic tool by opening the drainage tube when the intracranial pressure is elevated. Secondly, the intracerebroventricular pressure monitoring catheter and the ICP probe share the same device, meaning that even if the catheter becomes blocked, the pressure can still be measured normally (30). Furthermore, the intracerebroventricular pressure monitoring method has the ability to be zeroed in vivo (32). However, there are limitations to this technique. For instance, in cases of congenital small ventricles or where the ventricles are deformed by pressure due to severe cerebral edema, the placement of an external ventricular drainage can be technically challenging (27). In addition, this method is mainly prone to high infection rates and is not suitable for long-term monitoring as data show that the risk of intracranial infection begins to increase five days after the placement of an extra-ventricular drain (27, 29). Of the 155 patients who received extra-ventricular drainage included by Fabrizio Ortolano’study, 33 experienced minor bleeding associated with extra-ventricular drain placement, but none of these cases caused deterioration in neurological function or required surgical intervention to remove the hematoma (33).
Intracerebral parenchymal pressure monitoring: In patients who undergo surgical treatment for cerebral hemorrhage, whether through minimally invasive drilling and drainage or decompressive craniectomy, intracerebral parenchymal pressure measurement necessitates the placement of transducers without additional boreholes, allowing the transducer probe to be placed using surgical access to avoid unnecessary patient harm. However, there is a zero point drift, and the parenchymal probe cannot be recalibrated after placement (27). Studies on traumatic brain injury have shown that parenchymal intracranial pressure monitoring is equally accurate as intracerebroventricular pressure measurement, and that intracerebroventricular pressure measurement results in a worse prognosis and higher mortality compared to intracerebroventricular pressure measurement devices, with one of the drawbacks being the inability to drain cerebrospinal fluid (34). Moreover, intracranial pressure measured by ventricular drains is considered the gold standard for measuring overall pressure, whereas for intracerebral parenchymal pressure monitoring, when there is an intracranial pressure gradient, the measurement cannot substitute for the overall intracranial pressure (35).
The intracranial pressure monitoring methods of epidural and subdural monitoring are infrequently used in clinical practice due to their low accuracy and unreliability (36, 37). In contrast, non-invasive methods of intracranial pressure monitoring have gained popularity due to their practicality, reproducibility, safety, and lack of known side effects. An increase in intracranial pressure can cause the optic nerve sheath diameter in the retrobulbar chamber to expand, and ultrasound can be used as a non-invasive tool for assessing intracranial pressure by measuring the optic nerve sheath diameter (38). However, ocular ultrasound lacks a clear- cut-off value as an indicator of elevated intracranial pressure when using the optic nerve sheath diameter as an indirect assessment (39), and it is a difficult test that requires a high level of knowledge and a trained operator, which is one of its drawbacks (40, 41).
Discussion
Monitoring intracranial pressure provides a crucial reference point for diagnosing and treating neurosurgical diseases, as well as determining intracranial diseases (42), Increased intracranial pressure is a frequent complication of cerebral hemorrhage and can be attributed to various factors such as the hematoma’s occupying effect, peri-hematoma edema, hematoma enlargement, altered cerebrospinal fluid hemodynamics, and subsequent hydrocephalus formation. Intracranial hypertension is independently related to clinical prognosis and patient mortality (43–45). Daniel Agustín Godoy et al.’s meta-analysis revealed that up to 67% of patients had intracranial hypertension after cerebral hemorrhage. This figure was obtained after excluding patients who had abandoned further treatment or had been externally drained from the ventricles. The mortality rate associated with increased intracranial pressure was 50% in four studies involving 239 patients (45). The value of intracranial pressure monitoring lies in its ability to intervene before irreversible brain damage occurs, thus allowing clinicians to make informed treatment decisions (46).
Published studies have largely demonstrated that intracranial pressure monitoring has a positive effect on patient prognosis. In a retrospective study involving 196 patients, Junwei Ren et al. concluded that patients who received intracranial pressure monitoring had better clinical outcomes and lower mortality rates at 6 months post-discharge (44). However, a retrospective study by Che et al. (46) found that invasive intracranial pressure monitoring did not prolong hospital stays, reduce patient mortality, or improve functional recovery and prognosis 6 months after hypertensive cerebral hemorrhage. Furthermore, some patients may be treated using less invasive methods with the assistance of intracranial pressure monitoring (47). On the one hand, this method avoids unnecessary major trauma for the patient, and on the other hand, having a reference for intracranial pressure values provides assurance for the clinician’s management. Additionally, monitoring and normalizing intracranial pressure can reduce secondary neurological injury and its associated morbidity and mortality (48). These facts highlight the value of intracranial pressure monitoring after cerebral hemorrhage, which is often considered life-saving (31). In clinical practice, patients’ intracranial pressure values often precedes changes in clinical symptoms and signs (49). Moreover, early symptoms may be atypical and overlooked, but once the obvious symptoms appear, the patient’s optimal window of treatment may be have passed.
Conclusion
Currently, invasive intracranial pressure monitoring is deemed the most dependable method for monitoring intracranial pressure in real-time and with precision. However, further prospective, multi-center and multi-data research is still necessary to fully comprehend its impact on patient outcomes. As society develops, there is a growing demand for minimally invasive or even non-invasive techniques. With advancements in technology, non-invasive intracranial pressure monitoring is expected to become the primary method for monitoring intracranial pressure in the future, provided that technical challenges related to accuracy, stability, and real-time monitoring are overcome. As such, non-invasive intracranial pressure monitoring is currently an active area of research.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. de Oliveira Manoel, AL. Surgery for spontaneous intracerebral hemorrhage. Crit Care. (2020) 24:45. doi: 10.1186/s13054-020-2749-2
2. Kang, M, and Yao, Y. Oligodendrocytes in intracerebral hemorrhage. CNS Neurosci Ther. (2019) 25:1075–84. doi: 10.1111/cns.13193
3. Wilkinson, DA, Pandey, AS, Thompson, BG, Keep, RF, Hua, Y, and Xi, G. Injury mechanisms in acute intracerebral hemorrhage. Neuropharmacology. (2018) 134:240–8. doi: 10.1016/j.neuropharm.2017.09.033
4. Zille, M, Farr, TD, Keep, RF, Romer, C, Xi, G, and Boltze, J. Novel targets, treatments, and advanced models for intracerebral haemorrhage. EBioMedicine. (2022) 76:103880. doi: 10.1016/j.ebiom.2022.103880
5. Zheng, H, Chen, C, Zhang, J, and Hu, Z. Mechanism and therapy of brain edema after intracerebral hemorrhage. Cerebrovasc Dis. (2016) 42:155–69. doi: 10.1159/000445170
6. Chen, CJ, Ding, D, Ironside, N, Buell, TJ, Southerland, AM, Testai, FD, et al. Intracranial pressure monitoring in patients with spontaneous intracerebral hemorrhage. J Neurosurg. (2019) 132:1854–64. doi: 10.3171/2019.3.JNS19545
7. Keep, RF, Hua, Y, and Xi, G. Intracerebral haemorrhage: mechanisms of injury and therapeutic targets. Lancet Neurol. (2012) 11:720–31. doi: 10.1016/S1474-4422(12)70104-7
8. Kamel, H, and Hemphill, JC 3rd. Characteristics and sequelae of intracranial hypertension after intracerebral hemorrhage. Neurocrit Care. (2012) 17:172–6. doi: 10.1007/s12028-012-9744-7
9. Yang, Y, Pan, Y, Chen, C, Zhao, P, and Hang, C. Clinical significance of multiparameter intracranial pressure monitoring in the prognosis prediction of hypertensive intracerebral hemorrhage. J Clin Med. (2022) 11:671. doi: 10.3390/jcm11030671
10. Bothwell, SW, Janigro, D, and Patabendige, A. Cerebrospinal fluid dynamics and intracranial pressure elevation in neurological diseases. Fluids Barriers CNS. (2019) 16:9. doi: 10.1186/s12987-019-0129-6
11. Norager, NH, Olsen, MH, Pedersen, SH, Riedel, CS, Czosnyka, M, and Juhler, M. Reference values for intracranial pressure and lumbar cerebrospinal fluid pressure: a systematic review. Fluids Barriers CNS. (2021) 18:19. doi: 10.1186/s12987-021-00253-4
12. Czosnyka, M, and Pickard, JD. Monitoring and interpretation of intracranial pressure. J Neurol Neurosurg Psychiatry. (2004) 75:813–21. doi: 10.1136/jnnp.2003.033126
13. Patel, HC, Menon, DK, Tebbs, S, Hawker, R, Hutchinson, PJ, and Kirkpatrick, PJ. Specialist neurocritical care and outcome from head injury. Intensive Care Med. (2002) 28:547–53. doi: 10.1007/s00134-002-1235-4
14. Robba, C, Bacigaluppi, S, Cardim, D, Donnelly, J, Bertuccio, A, and Czosnyka, M. Non-invasive assessment of intracranial pressure. Acta Neurol Scand. (2016) 134:4–21. doi: 10.1111/ane.12527
15. Aiolfi, A, Khor, D, Cho, J, Benjamin, E, Inaba, K, and Demetriades, D. Intracranial pressure monitoring in severe blunt head trauma: does the type of monitoring device matter? J Neurosurg. (2018) 128:828–33. doi: 10.3171/2016.11.JNS162198
16. Dimitriou, J, Levivier, M, and Gugliotta, M. Comparison of complications in patients receiving different types of intracranial pressure monitoring: a retrospective study in a single Center in Switzerland. World Neurosurg. (2016) 89:641–6. doi: 10.1016/j.wneu.2015.11.037
17. Wang, H, He, Y, Liang, R, Wu, X, Zhao, L, Yang, J, et al. A meta-analysis and systematic review of intracranial pressure monitoring on severe craniocerebral injury. Ann Palliat Med. (2021) 10:5380–90. doi: 10.21037/apm-21-897
18. Bumberger, A, Braunsteiner, T, Leitgeb, J, and Haider, T. Intracranial pressure monitoring following traumatic brain injury: evaluation of indications, complications, and significance of follow-up imaging-an exploratory, retrospective study of consecutive patients at a level I trauma center. Eur J Trauma Emerg Surg. (2022) 48:863–70. doi: 10.1007/s00068-020-01570-3
19. Stein, SC, Georgoff, P, Meghan, S, Mirza, KL, and El Falaky, OM. Relationship of aggressive monitoring and treatment to improved outcomes in severe traumatic brain injury. J Neurosurg. (2010) 112:1105–12. doi: 10.3171/2009.8.JNS09738
20. Schrag, M, and Kirshner, H. Management of Intracerebral Hemorrhage: JACC focus seminar. J Am Coll Cardiol. (2020) 75:1819–31. doi: 10.1016/j.jacc.2019.10.066
21. Kearns, KN, Ironside, N, Park, MS, Worrall, BB, Southerland, AM, Chen, CJ, et al. Neuroprotective therapies for spontaneous intracerebral hemorrhage. Neurocrit Care. (2021) 35:862–86. doi: 10.1007/s12028-021-01311-3
22. Selim, M, and Norton, C. Perihematomal edema: implications for intracerebral hemorrhage research and therapeutic advances. J Neurosci Res. (2020) 98:212–8. doi: 10.1002/jnr.24372
23. Gross, BA, Jankowitz, BT, and Friedlander, RM. Cerebral Intraparenchymal hemorrhage: a review. JAMA. (2019) 321:1295–303. doi: 10.1001/jama.2019.2413
24. Owen, B, Akbik, O, Torbey, M, Davis, H, and Carlson, AP. Incidence and outcomes of intracerebral haemorrhage with mechanical compression hydrocephalus. Stroke Vasc Neurol. (2021) 6:328–36. doi: 10.1136/svn-2020-000401
25. Al-Kawaz, MN, Hanley, DF, and Ziai, W. Advances in therapeutic approaches for spontaneous intracerebral hemorrhage. Neurotherapeutics. (2020) 17:1757–67. doi: 10.1007/s13311-020-00902-w
26. Al-Kawaz, MN, Li, Y, Thompson, RE, Avadhani, R, de Havenon, A, Gruber, J, et al. Intracranial pressure and cerebral perfusion pressure in large spontaneous intracranial hemorrhage and impact of minimally invasive surgery. Front Neurol. (2021) 12:729831. doi: 10.3389/fneur.2021.729831
27. Canac, N, Jalaleddini, K, Thorpe, SG, Thibeault, CM, and Hamilton, RB. Review: pathophysiology of intracranial hypertension and noninvasive intracranial pressure monitoring. Fluids Barriers CNS. (2020) 17:40. doi: 10.1186/s12987-020-00201-8
28. Robba, C, Pozzebon, S, Moro, B, Vincent, JL, Creteur, J, and Taccone, FS. Multimodal non-invasive assessment of intracranial hypertension: an observational study. Crit Care. (2020) 24:379. doi: 10.1186/s13054-020-03105-z
29. Ganslandt, O, Mourtzoukos, S, Stadlbauer, A, Sommer, B, and Rammensee, R. Evaluation of a novel noninvasive ICP monitoring device in patients undergoing invasive ICP monitoring: preliminary results. J Neurosurg. (2018) 128:1653–60. doi: 10.3171/2016.11.JNS152268
30. Zhang, X, Medow, JE, Iskandar, BJ, Wang, F, Shokoueinejad, M, Koueik, J, et al. Invasive and noninvasive means of measuring intracranial pressure: a review. Physiol Meas. (2017) 38:R143–r182. doi: 10.1088/1361-6579/aa7256
31. Kawoos, U, McCarron, RM, Auker, CR, and Chavko, M. Advances in intracranial pressure monitoring and its significance in managing traumatic brain injury. Int J Mol Sci. (2015) 16:28979–97. doi: 10.3390/ijms161226146
32. Tavakoli, S, Peitz, G, Ares, W, Hafeez, S, and Grandhi, R. Complications of invasive intracranial pressure monitoring devices in neurocritical care. Neurosurg Focus. (2017) 43:E6. doi: 10.3171/2017.8.FOCUS17450
33. Ortolano, F, Carbonara, M, Stanco, A, Civelli, V, Carrabba, G, Zoerle, T, et al. External ventricular drain causes brain tissue damage: an imaging study. Acta Neurochir. (2017) 159:1981–9. doi: 10.1007/s00701-017-3291-0
34. Bales, JW, Bonow, RH, Buckley, RT, Barber, J, Temkin, N, and Chesnut, RM. Primary external ventricular drainage catheter versus Intraparenchymal ICP monitoring: outcome analysis. Neurocrit Care. (2019) 31:11–21. doi: 10.1007/s12028-019-00712-9
35. Kirkman, MA, and Smith, M. Intracranial pressure monitoring, cerebral perfusion pressure estimation, and ICP/CPP-guided therapy: a standard of care or optional extra after brain injury? Br J Anaesth. (2014) 112:35–46. doi: 10.1093/bja/aet418
36. Heldt, T, Zoerle, T, Teichmann, D, and Stocchetti, N. Intracranial pressure and intracranial Elastance monitoring in Neurocritical care. Annu Rev Biomed Eng. (2019) 21:523–49. doi: 10.1146/annurev-bioeng-060418-052257
37. Schizodimos, T, Soulountsi, V, Iasonidou, C, and Kapravelos, N. An overview of management of intracranial hypertension in the intensive care unit. J Anesth. (2020) 34:741–57. doi: 10.1007/s00540-020-02795-7
38. Vitiello, L, Salerno, G, De Bernardo, M, D'Aniello, O, Capasso, L, Marotta, G, et al. Ultrasound detection of intracranial hypertension in brain injuries. Front Med (Lausanne). (2022) 9:870808. doi: 10.3389/fmed.2022.870808
39. Vitiello, L, De Bernardo, M, Capasso, L, Cornetta, P, and Rosa, N. Optic nerve ultrasound evaluation in animals and Normal subjects. Front Med (Lausanne). (2021) 8:797018. doi: 10.3389/fmed.2021.797018
40. De Bernardo, M, Vitiello, L, De Pascale, I, Capasso, L, Cornetta, P, and Rosa, N. Optic nerve ultrasound evaluation in idiopathic intracranial hypertension. Front Med (Lausanne). (2022) 9:845554. doi: 10.3389/fmed.2022.845554
41. De Bernardo, M, Vitiello, L, De Luca, M, La Marca, A, and Rosa, N. Optic nerve changes detected with ocular ultrasonography during different surgical procedures: a narrative review. J Clin Med. (2022) 11:5467. doi: 10.3390/jcm11185467
42. Wang, G, Liu, W, Li, C, and Wang, H. Effect of minimally invasive surgery combined with intracranial pressure monitoring on neurological function recovery and quality of life in patients with hypertensive cerebral hemorrhage. Am J Transl Res. (2021) 13:8076–84.
43. Sykora, M, Steinmacher, S, Steiner, T, Poli, S, and Diedler, J. Association of intracranial pressure with outcome in comatose patients with intracerebral hemorrhage. J Neurol Sci. (2014) 342:141–5. doi: 10.1016/j.jns.2014.05.012
44. Ren, J, Wu, X, Huang, J, Cao, X, Yuan, Q, Zhang, D, et al. Intracranial pressure monitoring-aided management associated with favorable outcomes in patients with hypertension-related spontaneous intracerebral hemorrhage. Transl Stroke Res. (2020) 11:1253–63. doi: 10.1007/s12975-020-00798-w
45. Godoy, DA, Nunez-Patino, RA, Zorrilla-Vaca, A, Ziai, WC, and Hemphill, JC 3rd. Intracranial hypertension after spontaneous intracerebral hemorrhage: a systematic review and Meta-analysis of prevalence and mortality rate. Neurocrit Care. (2019) 31:176–87. doi: 10.1007/s12028-018-0658-x
46. Che, XR, Wang, YJ, and Zheng, HY. Prognostic value of intracranial pressure monitoring for the management of hypertensive intracerebral hemorrhage following minimally invasive surgery. World J Emerg Med. (2020) 11:169–73. doi: 10.5847/wjem.j.1920-8642.2020.03.007
47. Jin, T, Lian, W, Xu, K, Liu, Y, Xu, Z, Lu, R, et al. Effect of combination invasive intracranial pressure (ICP) monitoring and transcranial Doppler in the treatment of severe craniocerebral injury patients with decompressive craniectomy. Ann Palliat Med. (2021) 10:4472–8. doi: 10.21037/apm-21-504
48. Changa, AR, Czeisler, BM, and Lord, AS. Management of Elevated Intracranial Pressure: a review. Curr Neurol Neurosci Rep. (2019) 19:99. doi: 10.1007/s11910-019-1010-3
Keywords: invasive intracranial pressure monitoring, intracranial pressure, hypertensive cerebral hemorrhage, occupying effect, perihematomal edema
Citation: Chen F, Zhang S, Li B, Zhang J, Ran M and Qi B (2023) A review of invasive intracranial pressure monitoring following surgery for hypertensive cerebral hemorrhage. Front. Neurol. 14:1108722. doi: 10.3389/fneur.2023.1108722
Edited by:
Nicola Rosa, University of Salerno, ItalyReviewed by:
Livio Vitiello, University of Salerno, ItalyAbhijit Vijay Lele, University of Washington, United States
Copyright © 2023 Chen, Zhang, Li, Zhang, Ran and Qi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bin Qi, cWlfYmluQGpsdS5lZHUuY24=
 Fu Chen1
Fu Chen1 Bin Qi
Bin Qi