- Rehabilitation Medicine Department, First Hospital of Jilin University, Changchun, China
Stroke and spinal cord injury are common neurological disorders that can cause various dysfunctions. Motor dysfunction is a common dysfunction that easily leads to complications such as joint stiffness and muscle contracture and markedly impairs the daily living activities and long-term prognosis of patients. Orthotic devices can prevent or compensate for motor dysfunctions. Using orthotic devices early can help prevent and correct deformities and treat muscle and joint problems. An orthotic device is also an effective rehabilitation tool for improving motor function and compensatory abilities. In this study, we reviewed the epidemiological characteristics of stroke and spinal cord injury, provided the therapeutic effect and recent advances in the application of conventional and new types of orthotic devices used in stroke and spinal cord injury in different joints of the upper and lower limbs, identified the shortcomings with these orthotics, and suggested directions for future research.
1. Introduction
Stroke and spinal cord injury (SCI) are common neurological disorders that can cause neurological dysfunctions (1, 2). Motor dysfunction is a common complication often accompanied by low muscle strength, muscular hypertonia, and limited joint activities. Serious complications, such as joint stiffness and muscle contracture, can easily occur if left untreated, significantly impacting the activities of daily living (ADL) and the long-term prognosis of patients (3).
Orthotic devices are special or general products developed using rehabilitation engineering technology that can prevent or compensate for the dysfunction in motor activities caused by neurological disorders. Orthotic devices can effectively reduce or overcome motor dysfunction and support rehabilitation training to improve movement and participation (4). Early use of orthotic devices with rehabilitation skills can rectify limb deformities and avoid secondary damage. The ADL and self-care ability of patients can be improved by improving their motor function and compensatory ability. Functional improvement may ease the burden on family and society and shorten rehabilitation (5, 6).
2. Methods
The first part briefly summarizes the epidemiological characteristics of stroke and SCI and shows the necessity for orthosis. The second section reviews progress with the clinical application of orthotic devices in stroke and SCI. In the second section, a literature search was conducted in November 2022, based on a selective search in the PubMed/MEDLINE databases to search the literature from January 1, 2013, up to September 30, 2022. We used search terms related to “stroke”, “spinal cord injury”, “orthosis”, “orthoses”, “orthotics”, “orthotic device”, “brace”, “splint”, and “arm sling”. The literature search was limited to articles published in English in which the full text was available. This manuscript mainly included prospective and retrospective research articles of upper or lower limb orthotic devices for patients with stroke and SCI. Studies that involved spinal orthoses, devices implanted in the body, orthoses with electrical/electronic components (or involving electrical stimulation devices), robotic devices, and orthoses unrelated to limb joints were not included. Studies not related to the improvement of motor function or ADL were also excluded. Fifty seven articles were selected to be included in this study.
3. Discussion
3.1. Epidemiological characteristics of stroke and spinal cord injury and the need for orthotic devices
Stroke is a common cause of hemiplegia. It is a group of acute cerebrovascular diseases that can induce many complications, including motor and cognitive dysfunction, aphasia/dysarthria, and psychological problems, which affect survivors' social activities and quality of life (7, 8). Motor dysfunction was the most common complication associated with stroke (9). It often has manifestations, such as low muscle strength, dystonia, and limited joint activities, which seriously affect the patient's balance, walking ability, and ADL (8). Stroke is characterized by a high prevalence in disability, recurrence, and mortality and is the second leading cause of death worldwide (10). In the United States, ~795,000 people experience a new or recurrent stroke each year. Approximately 7.0 million people over 20 years of age have experienced a stroke. The overall prevalence of stroke was ~2.5%. It is estimated that by 2030, there will be an increase of 3.4 million people with stroke in people over 18 years, and the prevalence will increase by 20.5% compared to 2012(11).
SCI is also a common central nervous system injury caused by traffic crashes, falls, and violence. SCI usually results in severe disruption of sensorimotor and autonomic nerve functions and may lead to severe physical and psychological problems in survivors. Tetraplegia and paraplegia are the most common sequelae of SCI (12), indicating that motor dysfunction occurs in the injury plane and is accompanied by abnormal muscle tension and pathological reflexes. Survivors may face permanent impairments, and only a few have completed neurological recovery. This can impose a heavy burden on individuals, families, and society. SCI can lead to severe morbidity and mortality and is estimated to affect 250,000–500,000 people annually (13). In Western Europe, the incidence of new cases of SCI is ~16–19.4 per million people annually (14).
In these neurological disorders, if spasticity, joint range of motion, and motor dysfunction are not reduced and corrected early, complications such as limited joint movement and stiffness, and muscle contracture will occur that can affect patients' quality of life. It is estimated that the global population of people with disabilities may exceed one billion, and more than half of them live in low- and middle-income countries (15). Although assistive devices may improve the function of people with disabilities, only 5–15% of people in need currently have access to assistive devices (16). Orthotics and prosthetics are important assistive devices. The orthotic device is an external application device used to restore and maintain anatomical and functional position and to assist the functions of the human body (17, 18). Common orthoses include upper limb orthosis, lower limb orthosis, and spinal orthosis according to the part of the body it is used. In addition, the main function of compression/containment orthosis is to improve limb stability by stabilizing the joints, and functional orthosis can control limb activities by stabilizing, supporting, strengthening, and protecting limbs based on joint stabilization and can also correct deformities and relieve pain (17, 19). Studies indicate that orthotics can effectively improve patients' function and prognoses and should be widely popularized (4–6).
3.2. Advances in the use of common orthotic devices
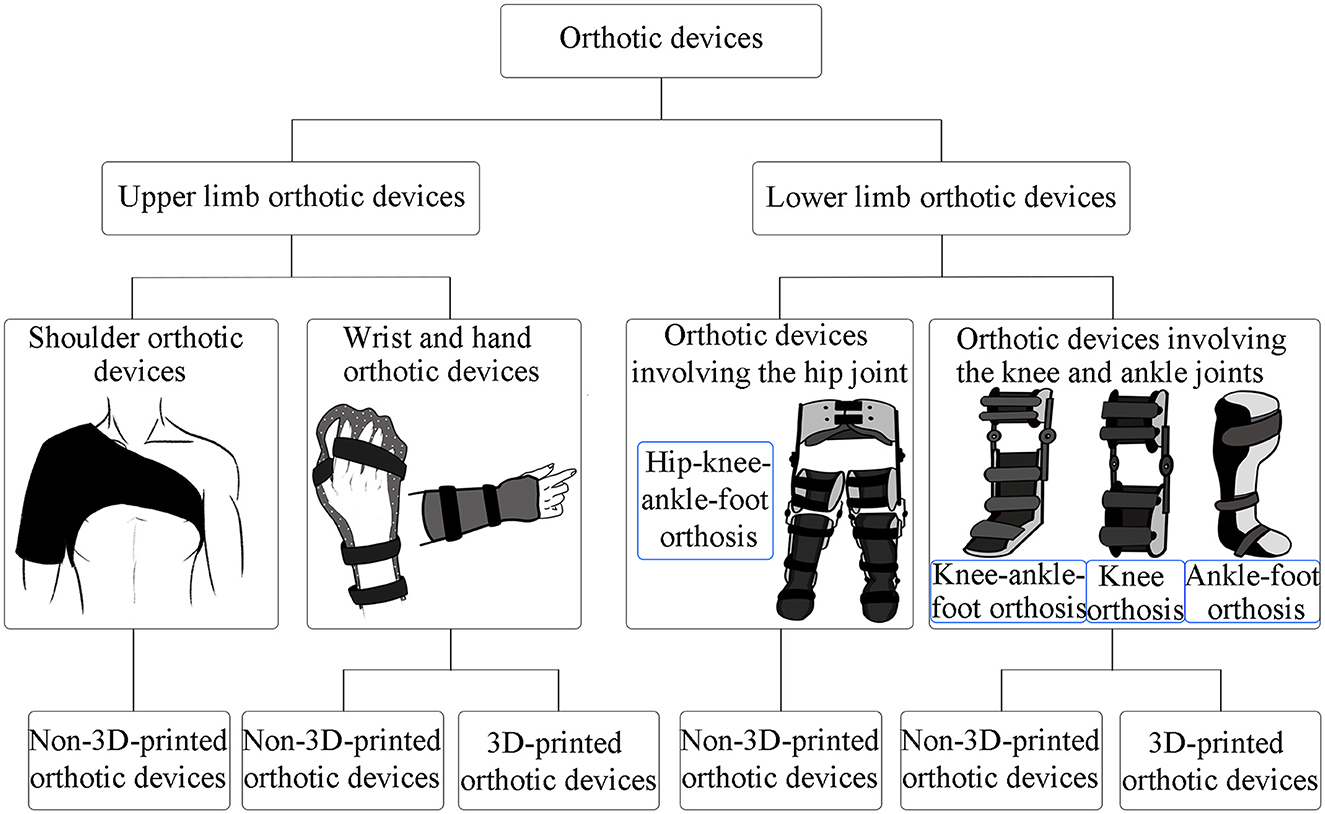
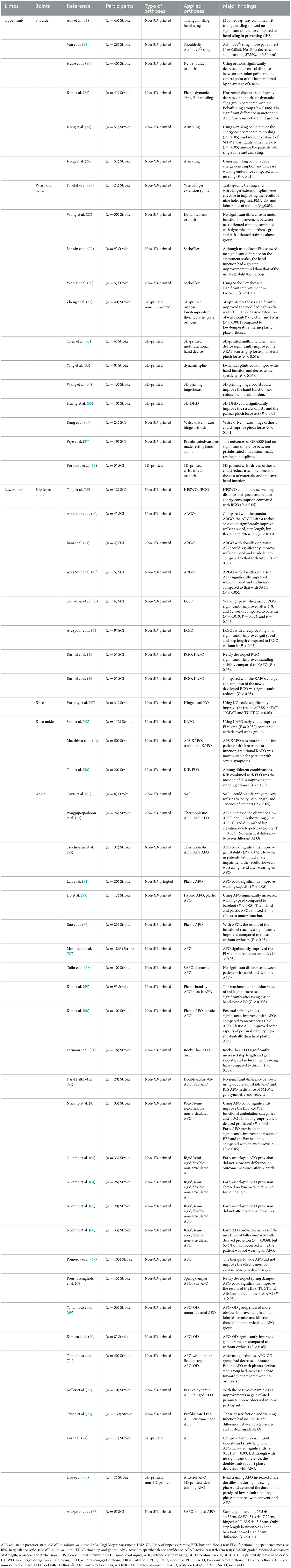
To prevent contracture, limbs with motor dysfunction must maintain a joint range of motion. Methods to maintain the joint range of motion of limbs include normal limb position, stretching and standing training, and the use of orthotic devices. Early use of orthotic devices can play a role in early prevention, improve therapeutic effect, lay a stable foundation for later rehabilitation, and prevent joint deformities. It also helps control muscle tension, improve joint range of motion, prevent muscle contracture, and maintain physical alignment of the limbs. The classification of orthotic devices reviewed in this article is shown in Figure 1. The characteristics of the articles are summarized in Table 1.
3.2.1. Upper limb orthotic devices
Hemiplegia due to stroke and quadriplegia due to SCI can cause upper limb motor dysfunction. Upper-limb orthotic devices are widely used in stroke and SCI. They can prevent and correct upper limb deformities, keep the limbs in functional position, provide traction to prevent joint contracture, partially compensate for the function of disabled muscles, and help to treat upper limb motor dysfunction.
3.2.1.1. Shoulder orthotic devices
Shoulder orthotic devices are commonly used to treat glenohumeral subluxation (GHS). GHS, also known as shoulder subluxation, is a common complication in hemiplegia. GHS can cause loss of range of motion due to the instability of the shoulder joint. Approximately 80% of stroke patients with hemiplegia may experience GHS (20), and if left untreated may cause shoulder pain, upper extremity edema, and limited shoulder joint movement. A study compared the efficacy of hemi-sling to a lap-tray combined with a triangle sling in GHS among acute stroke survivors. The result showed no significant difference between the two groups in preventing subluxation, pain, contracture, or movement limitation (21). This suggests that further studies may be needed to find effective shoulder support devices for patients with GHS. Van et al. (22) also compared different arm slings and found that the shoulderlift that directly supports the shoulder joint was more efficient than the Actimove® sling in reducing pain. However, subluxation was reduced only in the control group without slings, suggesting that orthoses may affect active correction. Although studies have shown that wearing orthoses is helpful for recovery in GHS, they should be removed promptly if necessary. The selection of orthotics and the appropriate time for wearing them may require further research.
X-ray findings suggest an improvement in GHS in some studies (23, 24). In a study, radiography revealed that wearing an orthosis reduced the vertical displacement of the glenohumeral joint in stroke patients (23). In another study using an elastic dynamic shoulder sling in stroke patients with GHS, radiography showed that the horizontal distance from the humeral head to the glenoid fossa improved compared to the control group (Bobath sling) (24). Considering that orthoses provide immediate improvement of GHS, and different orthoses have different effects on GHS recovery, it is necessary to adapt the best orthotic devices. Meanwhile, the results showed that the improvement in motor function was more pronounced after 8 weeks than after 4 weeks in the group (24). This suggests that the length of wearing time affects the functional improvement. However, the results also indicated no significant difference in motor and ADL functions between the groups (24). Studies suggest that improving motor function is an important method to recover from GHS, and further studies may be needed to consider suitable orthoses and GHS improvement methods for patients.
Interestingly, wearing shoulder orthotics also affected gait efficiency. Some studies have shown that patients with GHS after stroke wore shoulder support arm slings, which could reduce energy consumption and increase walking distance (25, 26). This suggests that posture correction may improve motor function. Dysfunction of different parts may affect each other, and rehabilitation after stroke should be comprehensive.
3.2.1.2. Wrist and hand orthotic devices
Depending on the disorders, the wrist and hand orthotic devices can take various forms, such as wrist stabilization, wrist-hand stabilization, and wrist-finger stabilization. The biomechanical principle is to assist in the extension of the wrist and finger joints (77). Hemiplegic spasm is a common complication; the incidence of hemiplegic spasm in the 1st year after stroke is between 33 and 78%, and the incidence of contracture is at least 50% (78). Early prevention and treatment, such as passive stretching, can increase muscle extensibility and effectively reduce muscle spasms to improve the recovery of upper limb function. Wrist and hand orthotic devices assist in the stabilization of the wrist and hand in a functional position and may be considered an effective method of passive stretching to reduce wrist flexor spasticity. Wrist and hand orthotic devices often prevent wrist and finger contractures in hemiplegic survivors, but their effectiveness is unclear (79). A study using task-specific training combined with wrist-finger extension splints in hemiplegic patients, showed effective improvements in finger dexterity, upper limb motor function, and range of motion of the wrist and hand joints (27). However, another study suggested that task-oriented training combined with dynamic hand orthosis did not significantly improve motor function compared to task-oriented training alone in patients with subacute stroke (28). Further studies are needed to determine the timing and circumstances of wearing orthoses, considering that not all cases using orthotic devices had beneficial effects on motor function improvement compared with no orthotics. However, sample size and other factors may have influenced the results.
Patients with cervical SCI are prone to quadriplegia, and after rehabilitation treatment, the recovery of motor function is often incomplete, and orthotic assistance is needed. The wrist-driven flexor hinge orthosis, a device designed to restore hand function by providing three-point prehension, has been used in patients with SCI and has shown a significant increase in pinch force (36). Using orthoses can improve the patient's hand function, which is helpful for ADL, such as eating. A study comparing prefabricated and custom-made resting hand splints among SCI patients showed no statistical difference (37). Although custom-made orthotic devices are generally recommended in clinical practice, sometimes their advantages are minimal, and they have the disadvantages of being time-consuming and expensive. In some cases, prefabricated orthotics can also be used. However, the custom-made orthotic devices require further improvement.
There are some special orthoses for the recovery of motor function in patients. One study showed that SaeboFlex, a spring-assisted orthosis, helped improve hand dexterity in patients with almost complete loss of hand function after stroke (29). Additionally, a study showed that SaeboFlex significantly improved upper limb motor function in patients with stroke (30). Considering that if static hand orthoses cannot effectively improve distal upper-limb motor function, it is necessary to use appropriate orthoses to improve hand function effectively.
Currently, conventional wrist and hand orthotic devices have certain disadvantages. Some of them are bulky, and their customization is time-consuming. With technological advances, numerous new orthotic devices have emerged, including custom-made three-dimensional (3D) printed orthoses. With 3D printing technology, orthoses can be accurately designed using computer graphics program, which can solve the problems of time-consuming manufacturing and difficult customization of conventional orthotic devices. The materials used for 3D printing are also readily available (80), and 3D-printed orthoses can be made of lightweight, ventilating, and biodegradable materials (81). A study compared two different types of wrist-hand orthoses, and the results showed that the therapeutic effect of 3D-printed orthoses was better than that of low-temperature thermoplastic plate orthoses. Compared with the other orthosis, 3D-printed orthosis could better reduce the spasticity of stroke patients and had an important effect on improving the motor function of the wrist joint (31). Since 3D-printed orthoses can be customized more accurately through software and are more adaptable to patients than conventional orthoses, they may provide better support. Some studies have shown that 3D-printed orthotic devices can effectively improve patients' hand function (32–34) and compared the effects of wearing time (3 weeks vs. 3 months). The results showed that the grip strength and hand function of stroke patients tended to improve with an increase in wearing time, although the difference was insignificant (34). Considering that 3D-printed orthotics can effectively improve patients' hand function, prolonging wearing time will not cause adverse reactions but will further improve the motor function of the patients. Furthermore, a 3D-printed dynamic hand device (3D-DHD) was used to supplement task-oriented training in stroke survivors. The results showed that the improvement in hand function in the 3D-DHD group was greater than that in the task-oriented training alone group (35). This suggests that 3D-printed orthoses combined with appropriate rehabilitation methods can more effectively improve the motor function of patients.
3D-printed orthoses can also be used in patients with SCI. A study has shown that using 3D printing technology to make wrist-driven orthoses could reduce hands-on assembly time and the cost of the material. In addition, hand function in patients with SCI could improve (38). Considering with 3D printing technology, we developed an orthosis that can accurately adapt to a user, and its function is not inferior to that of conventional technology. Although 3D printing technology may require more conditions, it is worth promoting and can compensate for the many defects of conventional orthoses.
3.2.2. Lower limb orthotic devices
Hemiplegia and SCI-induced tetraplegia/paraplegia are common causes of lower limb motor dysfunction. Lower-limb orthotic devices can support body weight, prevent and correct lower-limb deformities, effectively compensate for the function of paralyzed muscles, and limit unnecessary activities of the lower-limb joints. They can improve posture while standing and walking and help treat lower limb motor dysfunction. Moreover, lower-limb orthotic devices may help improve patients' ADL (82).
3.2.2.1. Orthotic devices involving the hip joint
The hip-knee-ankle-foot orthosis (HKAFO) is the most common hip joint orthotic device according to the literature search results and is the main hip joint orthotic device reviewed in this paper. The HKAFO was used to stabilize the hip, knee, and ankle joints. It is suitable for patients with extensive lower limb muscle paralysis and assists patients in standing and walking. A reciprocating gait orthosis (RGO) is a type of HKAFO. Different types of HKAFOs have different effects on lower limb motor function. A study comparing the newly designed hip energy storage walking orthosis (HESWO) and RGO, suggested that SCI patients wearing HESWO had more significant gait improvement and lower energy consumption than those wearing RGO, considering that HESWO can provide a more energy-efficient gait (39). Arazpour et al. added a rocker sole to advanced RGO (ARGO) and found improvements in walking function compared to ARGO with a flat sole among patients with SCI (40). Two studies compared two kinds of ARGOs; and the results suggested that ARGO with dorsiflexion-assisted ankle-foot orthosis (AFO) was better than that with solid AFO in improving gait function in patients with SCI (41, 42). These studies suggest that the influence of different orthotic components on motor function improvement should be considered. Through continuous research with orthotic components, appropriate orthotic devices should be adapted according to the functional status of the patients.
One study showed that using isocentric RGO (IRGO) in patients with SCI could significantly improve walking capacity (43). Another study compared IRGO with and without the reciprocating link, and the results showed that the reciprocating link was useful in improving the walking ability of patients (44). IRGO is effective in improving walking parameters in patients with SCI. However, the sample sizes of these studies were small. To determine which orthotic devices are suitable for users, we need to increase the sample size for further studies to identify appropriate orthoses in clinical practice.
Two studies investigated whether controlling the hip joint improves motor function. They compared the standing stability between RGO and a knee-ankle-foot orthosis (KAFO) (45, 46). The results showed that compared with the KAFO group, patients with SCI wearing the newly developed RGO were more stable in standing at rest and performing tasks, especially when standing at rest (45). Meanwhile, the energy cost decreased significantly and walking style improved (46). Considering that hip joint control is helpful for standing stability, for paraplegic patients with SCI, orthotics with hip control may help improve motor function.
Although one study showed no significant difference in gait speed between powered gait orthosis and IRGO (83), orthotics with electrical/electronic components have been widely used in recent years to improve walking capacity in patients with SCI (84). However, this paper focused on orthotics without electrical/electronic components. Therefore, these orthotic devices were not reviewed in detail.
3.2.2.2. Orthotic devices involving the knee and ankle joints
KAFO and AFO are the most common orthotic devices involving the knee and ankle joints. The KAFO is used in hemiplegic patients with unstable knee and ankle joints and lumbar paraplegia. It can support, stabilize, and limit the movement of the joints and is suitable for knee and ankle joints rehabilitation. Of course, there is also a knee orthosis (KO) for simple knee joint stabilization (47). AFO is widely used for foot and ankle deformities, such as strephenopodia, strephexopodia, and foot drop.
KAFO is widely used to stabilize lower limb segments during walking. However, only a few paraplegic patients discharged from the hospital continue to use KAFO. KAFO gait requires upper limb muscle strength, increases gait fatigue and may lead to upper limb musculoskeletal injury. Consequently, the KAFO is often used for standing posture or gait training rather than functional gait (85). However, some studies have shown that KAFO may positively affect patient recovery. A previous study showed that using a KAFO early could significantly improve the ADL in stroke patients (48). Another study showed that in hemiplegic patients, the adjustable posterior strut KAFO was more suitable for patients with better motor function, whereas traditional KAFO was suitable for patients with severe symptoms and difficulty obtaining practical walking ability (49). It is beneficial for patients to wear orthoses early, and different orthoses are suitable for patients with different functional statuses.
One study used three different applications: knee immobilization brace (KIB), KIB combined with Foot Lifter Orthosis® (FLO), and KIB combined with rigid taping, suggesting that KIB combined with FLO was the most helpful strategy for improving the balance of hemiplegic patients (50). Considering that simultaneous control of the knee and ankle joints is helpful for the balance of hemiplegic patients, the effect of FLO on ankle joint stabilization is better than that of rigid taping. Therefore, the KAFO, which covers both the knee and ankle joints, is most widely used for patients who need to stabilize the knee joint. However, an orthotic device that stabilizes the knee joint can also positively improve motor function. Moreover, a study using hinged soft KO among stroke patients showed that KO prevented knee hyperextension, significantly improved balance and walking distance, and reduced walking time (47). Patients can improve their walking ability by controlling the knee joint and preventing knee hyperextension.
Some studies conducted gait analysis for stroke patients with and without AFO, and the results indicated that AFO effectively improved walking ability, gait stability (51–55), balance (56), and might improve ADL (57). Furthermore, AFO reduces compensatory strategies during walking (52). However, in some patients with mild ankle impairment, the results showed a worsening trend after wearing an AFO (53). Stabilizing the ankle joint can stabilize the lower limb, effectively regulate the posture, and help improve walking capacity. However, different effects may occur depending on the severity of the patient's condition, which requires further study.
Foot drop is a common complication in hemiplegic patients. One study showed that the solid and dynamic AFO had no significant difference in controlling foot drop (58). Some studies have compared elastic AFO and hard plastic AFO with no AFO. The results showed that compared with patients without orthoses, those with orthotic devices had improved motor function (59, 60). Furthermore, elastic band-type AFO could improve foot drop better than hard plastic AFO (59), and postural stability tended to improve (60). Research has shown that plastic materials may limit the ankle joint, resulting in insufficient ankle dorsiflexion (59). Foot drop may require ankle joint stabilization; however, a stiffer material might not provide the best support. Soft materials can also provide good ankle joint stabilization and improve user comfort.
Some studies have compared the different types of AFOs. A study comparing solid AFO with hinged AFO during treadmill training in patients with SCI showed that solid AFO could improve step length compared to hinged AFO, although with no statistical difference (76). Another study suggested that a rocker bar AFO might improve walking capacity better than a solid AFO (61). Considering that different orthotic devices have different effects on patient function, further studies are needed to adapt the best orthosis under different conditions. Moreover, Do et al. showed that wearing a hybrid AFO was similar to a plastic AFO in motor function, but the hybrid AFO was lighter and more satisfactory (55). Another study compared a double-adjustable AFO with a posterior leaf spring AFO (PLS AFO) and found no significant differences in walking capacity (62). The results suggest that the selection of orthoses requires many considerations. When there is no significant difference in functional improvement, the appropriate orthosis should be selected according to factors such as wearing comfort and patient satisfaction.
Some studies have compared the duration of use of orthotic devices. A study comparing the early provision of AFOs with delayed provision showed that both groups had significant improvement in walking function after wearing AFO, and the improvement of balance was more pronounced in the early provision group (4). This suggests that using an AFO early significantly affects the recovery of lower limb motor function. However, the effectiveness of early AFO use in patients with stroke paralysis with foot drops is controversial. Some studies have shown that early or delayed AFO provision after stroke did not affect outcomes (63–65), However, providing AFO had a positive short-term effect on ankle kinematics in the early phase after stroke (65). In addition, another study showed that using an AFO early increased the risk of falls in hemiplegic patients, but it was important to note that 63.6% of falls occurred while the patient was not wearing an AFO (66). Considering that patients who have adapted to AFO gait may be more prone to falls when they do not wear orthoses, attention should be paid to the use of orthoses when motor function has not sufficiently improved. Notwithstanding, wearing an AFO is still necessary for stroke patients, and the most appropriate time to wear orthoses may require further study. A study suggested that using quick-made AFOs by therapists did not improve the effectiveness of conventional physical therapy (67). However, quick-made orthotics are an option for patients to have custom-made orthotics at an early stage of the disease (67). While the effectiveness of early or delayed wearing of orthotics remains controversial, further exploration and improvement with orthotic devices are needed.
Some AFOs have dampers. A study has shown that the newly developed AFO with spring damper is superior to the PLS AFO in improving balance (68). Studies of AFO with an oil damper (AFO-OD) have suggested that AFO-OD might significantly improve ankle joint motor function and gait parameters in stroke patients (69, 70). Another study conducted a gait analysis after rehabilitation with different AFOs. The results showed that the AFO-OD group had decreased thoracic tilt, but the AFO with plantar flexion stop group had increased pelvic forward tilt (71) after wearing orthotics. Adding dampers may optimize the function of AFO and improve motor function. Meanwhile, AFO-OD can better avoid dislocation of thorax and pelvis when walking, and can guide a more stable and natural gait.
With the development of orthotics, custom-made orthotics have become increasingly common and sophisticated. In a study that personalized the passive-dynamic AFO, improvements in parameters related to walking function were observed in some participants (72). However, another study showed that compared with prefabricated orthotics, customized orthotic devices showed no improvement in walking function and user satisfaction (73). Considering that custom-made orthoses may improve patients function from a new perspective through different components, they need further research and are actively promoted in clinical practice.
3D printing technology can also be used to fabricate lower limb orthotic devices. A study showed that after stroke patients wore 3D-printed AFO, their gait speed and stride length improved, and the double limb support phase decreased (74). Motion feedback can also be used for orthotics. A study suggested that a 3D-printed AFO with motion feedback in stroke patients improved walking function better than conventional AFO (75). This suggests that 3D-printed orthoses exhibit good performance and are comparable to conventional orthoses. 3D printing technology has potential benefits in design and production and can be actively promoted.
4. Conclusion
In this article, we reviewed conventional and new types of orthotic devices for stroke and SCI according to the different joints of the upper and lower limbs. Conventional orthotic devices are widely used and can effectively improve motor function. Custom-made orthoses are generally recommended; however, sometimes, there are no significant differences in efficacy or user preference between prefabricated and customized orthotic devices. In addition, custom-made conventional orthotic devices are sometimes time-consuming. Nowadays, new orthotics and various components are constantly being developed, which tend to be durable, lightweight, ventilating, and intelligent, and the kinematics of these devices are very close to the anatomy of the human limb, sometimes even in the form of human-computer interactions. However, some devices are still in development stages and cannot be widely and immediately used in clinical practice. The direction of future research on orthotic devices is to improve the functions of conventional orthotic devices and develop new types of devices. Further research is needed to make them more consistent with clinical practice, help patients improve motor function, rebuild their confidence, and enable them to return to their families and society faster.
Author contributions
YC drafted the manuscript. SC and XC performed the literature search and extracted the articles. GX, NM, HL, and HZ assisted with drafting and revising the manuscript. ZL conceived and designed the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was financially supported by the Science and Technology Department of Jilin Province, China [No. 20200404209YY].
Acknowledgments
The authors thank the financial support of the Department of Science and Technology of Jilin Province of China (No. 20200404209YY). We thank the editors and the reviewers for their useful feedback that improved this paper.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
GHS, glenohumeral subluxation; SCI, spinal cord injury; ADL, activities of daily living; 3D, three-dimensional; 3D-DHD, 3D printed dynamic hand device; HKAFO, hip-knee-ankle-foot orthosis; HESWO, hip energy storage walking orthosis; RGO, reciprocating-gait orthosis; ARGO, advanced RGO; IRGO, isocentric RGO; KAFO, knee-ankle-foot orthosis; KO, knee orthosis; KIB, knee immobilization brace; FLO, Foot Lifter Orthosis®; AFO, ankle-foot orthosis; AFO-OD, AFO with oil damper; PLS AFO, posterior leaf spring AFO.
References
1. Kumar R, Lim J, Mekary RA, Rattani A, Dewan MC, Sharif SY, et al. Traumatic spinal injury: global epidemiology and worldwide volume. World Neurosurg. (2018) 113:e345–e63. doi: 10.1016/j.wneu.2018.02.033
2. Ma VY, Chan L, Carruthers KJ. Incidence, prevalence, costs, and impact on disability of common conditions requiring rehabilitation in the United States: stroke, spinal cord injury, traumatic brain injury, multiple sclerosis, osteoarthritis, rheumatoid arthritis, limb loss, and back pain. Arch Phys Med Rehabil. (2014) 95:986–95. doi: 10.1016/j.apmr.2013.10.032
3. Hornby TG, Reisman DS, Ward IG, Scheets PL, Miller A, Haddad D, et al. Clinical practice guideline to improve locomotor function following chronic stroke, incomplete spinal cord injury, and brain injury. J Neurol Phys Ther. (2020) 44:49–100. doi: 10.1097/NPT.0000000000000303
4. Nikamp CDM, Buurke JH, van der Palen J, Hermens HJ, Rietman JS. Early or delayed provision of an ankle-foot orthosis in patients with acute and subacute stroke: a randomized controlled trial. Clin Rehabil. (2017) 31:798–808. doi: 10.1177/0269215516658337
5. Nadler M, Pauls M. Shoulder orthoses for the prevention and reduction of hemiplegic shoulder pain and subluxation: systematic review. Clin Rehabil. (2017) 31:444–53. doi: 10.1177/0269215516648753
6. Yeung LF, Ockenfeld C, Pang MK, Wai HW, Soo OY Li SW, et al. Randomized controlled trial of robot-assisted gait training with dorsiflexion assistance on chronic stroke patients wearing ankle-foot-orthosis. J Neuroeng Rehabil. (2018) 15:51. doi: 10.1186/s12984-018-0394-7
7. Mayo NE, Aburub A, Brouillette MJ, Kuspinar A, Moriello C, Rodriguez AM, et al. In support of an individualized approach to assessing quality of life: comparison between Patient Generated Index and standardized measures across four health conditions. Qual Life Res. (2017) 26:601–9. doi: 10.1007/s11136-016-1480-6
8. Han P, Zhang W, Kang L, Ma Y, Fu L, Jia L, et al. Clinical evidence of exercise benefits for stroke. Adv Exp Med Biol. (2017) 1000:131–51. doi: 10.1007/978-981-10-4304-8_9
9. Stinear CM, Lang CE, Zeiler S, Byblow WD. Advances and challenges in stroke rehabilitation. Lancet Neurol. (2020) 19:348–60. doi: 10.1016/S1474-4422(19)30415-6
10. Donkor ES. Stroke in the 21(st) century: a snapshot of the burden, epidemiology, and quality of life. Stroke Res Treat. (2018) 2018:3238165. doi: 10.1155/2018/3238165
11. Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation. (2020) 141:e139–596. doi: 10.1161/CIR.0000000000000746
12. Khorasanizadeh M, Yousefifard M, Eskian M, Lu Y, Chalangari M, Harrop JS, et al. Neurological recovery following traumatic spinal cord injury: a systematic review and meta-analysis. J Neurosurg Spine. (2019) 2019:1–17. doi: 10.3171/2018.10.SPINE18802
13. Quadri SA, Farooqui M, Ikram A, Zafar A, Khan MA, Suriya SS, et al. Recent update on basic mechanisms of spinal cord injury. Neurosurg Rev. (2020) 43:425–41. doi: 10.1007/s10143-018-1008-3
14. Scivoletto G, Miscusi M, Forcato S, Ricciardi L, Serrao M, Bellitti R, et al. The rehabilitation of spinal cord injury patients in Europe. Acta Neurochirurgica Supplement. (2017) 124:203–10. doi: 10.1007/978-3-319-39546-3_31
15. Martin Ginis KA, van der Ploeg HP, Foster C, Lai B, McBride CB, Ng K, et al. Participation of people living with disabilities in physical activity: a global perspective. Lancet (London, England). (2021) 398:443–55. doi: 10.1016/S0140-6736(21)01164-8
16. Khasnabis C, Mirza Z, MacLachlan M. Opening the GATE to inclusion for people with disabilities. Lancet (London, England). (2015) 386:2229–30. doi: 10.1016/S0140-6736(15)01093-4
17. Shroff G, Thakur D, Dhingra V, Baroli DS, Khatri D, Gautam RD. Role of physiotherapy in the mobilization of patients with spinal cord injury undergoing human embryonic stem cells transplantation. Clin Transl Med. (2016) 5:41. doi: 10.1186/s40169-016-0122-5
18. Choo YJ, Boudier-Revéret M, Chang MC. 3D printing technology applied to orthosis manufacturing: narrative review. Ann Palliat Med. (2020) 9:4262–70. doi: 10.21037/apm-20-1185
19. Hadadi M, Haghighat F, Mohammadpour N, Sobhani S. Effects of kinesiotape vs soft and semirigid ankle orthoses on balance in patients with chronic ankle instability: a randomized controlled trial. Foot Ankle Int. (2020) 41:793–802. doi: 10.1177/1071100720917181
20. Arya KN, Pandian S, Puri V. Rehabilitation methods for reducing shoulder subluxation in post-stroke hemiparesis: a systematic review. Top Stroke Rehabil. (2018) 25:68–81. doi: 10.1080/10749357.2017.1383712
21. Ada L, Foongchomcheay A, Langhammer B, Preston E, Stanton R, Robinson J, et al. Lap-tray and triangular sling are no more effective than a hemi-sling in preventing shoulder subluxation in those at risk early after stroke: a randomized trial. Eur J Phys Rehabil Med. (2017) 53:41–8. doi: 10.23736/S1973-9087.16.04209-X
22. Van BA, Lambrecht G, Oostra KM, Vanderstraeten G, Cambier D, A. randomized controlled trial on the immediate and long-term effects of arm slings on shoulder subluxation in stroke patients. Eur J Phys Rehabil Med. (2017) 53:400–9. doi: 10.23736/S1973-9087.17.04368-4
23. Hesse S, Herrmann C, Bardeleben A, Holzgraefe M, Werner C, Wingendorf I, et al. A new orthosis for subluxed, flaccid shoulder after stroke facilitates gait symmetry: a preliminary study. J Rehabil Med. (2013) 45:623–9. doi: 10.2340/16501977-1172
24. Kim MG, Lee SA, Park EJ, Choi MK, Kim JM, Sohn MK, et al. Elastic dynamic sling on subluxation of hemiplegic shoulder in patients with subacute stroke: a multicenter randomized controlled trial. Int J Environ Res Public Health. 2022; 19:9975. doi: 10.3390/ijerph19169975
25. Jeong YG, Jeong YJ, Koo JW. The effect of an arm sling used for shoulder support on gait efficiency in hemiplegic patients with stroke using walking aids. Eur J Phys Rehabil Med. (2017) 53:410–5. doi: 10.23736/S1973-9087.17.04425-2
26. Jeong YG, Jeong YJ, Kim HS, Lee KH. Predictors of the effect of an arm sling on gait efficiency in stroke patients with shoulder subluxation: a pre-post design clinical trial. Physiother Theory Pract. (2022) 38:729–36. doi: 10.1080/09593985.2020.1799458
27. Khallaf ME, Ameer MA, Fayed EE. Effect of task specific training and wrist-fingers extension splint on hand joints range of motion and function after stroke. NeuroRehabilitation. (2017) 41:437–44. doi: 10.3233/NRE-162128
28. Wong Y, Li CJ, Ada L, Zhang T, Månum G, Langhammer B. Upper limb training with a dynamic hand orthosis in early subacute stroke: a pilot randomized trial. J Rehabil Med. (2022) 54:jrm00279. doi: 10.2340/jrm.v54.2231
29. Lannin NA, Cusick A, Hills C, Kinnear B, Vogel K, Matthews K, et al. Upper limb motor training using a Saebo(™) orthosis is feasible for increasing task-specific practice in hospital after stroke. Aust Occup Ther J. (2016) 63:364–72. doi: 10.1111/1440-1630.12330
30. Woo Y, Jeon H, Hwang S, Choi B, Lee J. Kinematics variations after spring-assisted orthosis training in persons with stroke. Prosthet Orthot Int. (2013) 37:311–6. doi: 10.1177/0309364612461050
31. Zheng Y, Liu G, Yu L, Wang Y, Fang Y, Shen Y, et al. Effects of a 3D-printed orthosis compared to a low-temperature thermoplastic plate orthosis on wrist flexor spasticity in chronic hemiparetic stroke patients: a randomized controlled trial. Clin Rehabil. (2020) 34:194–204. doi: 10.1177/0269215519885174
32. Chen ZH, Yang YL, Lin KW, Sun PC, Chen CS. Functional assessment of 3D-printed multifunction assistive hand device for chronic stroke patients. IEEE Trans Neural Syst Rehabil Eng. (2022) 30:1261–6. doi: 10.1109/TNSRE.2022.3173034
33. Yang YS, Emzain ZF, Huang SC. Biomechanical evaluation of dynamic splint based on pulley rotation design for management of hand spasticity. IEEE Trans Neural Syst Rehabil Eng. (2021) 29:683–9. doi: 10.1109/TNSRE.2021.3068453
34. Wang K, Shi Y, He W, Yuan J, Li Y, Pan X, et al. The research on 3D printing fingerboard and the initial application on cerebral stroke patient's hand spasm. Biomed Eng Online. (2018) 17:92. doi: 10.1186/s12938-018-0522-4
35. Huang TY, Pan LH, Yang WW, Huang LY, Sun PC, Chen CS. Biomechanical evaluation of three-dimensional printed dynamic hand device for patients with chronic stroke. IEEE Trans Neural Syst Rehabil Eng. (2019) 27:1246–52. doi: 10.1109/TNSRE.2019.2915260
36. Kang YS, Park YG, Lee BS, Park HS. Biomechanical evaluation of wrist-driven flexor hinge orthosis in persons with spinal cord injury. J Rehabil Res Dev. (2013) 50:1129–38. doi: 10.1682/JRRD.2012.10.0189
37. Frye SK, Geigle PR, A. comparison of prefabricated and custom made resting hand splints for individuals with cervical spinal cord injury: A randomized controlled trial. Clin Rehabil. (2021) 35:861–9. doi: 10.1177/0269215520983486
38. Portnova AA, Mukherjee G, Peters KM, Yamane A, Steele KM. Design of a 3D-printed, open-source wrist-driven orthosis for individuals with spinal cord injury. PLoS One. (2018) 13:e0193106. doi: 10.1371/journal.pone.0193106
39. Yang M, Li J, Guan X, Gao L, Gao F, Du L, et al. Effectiveness of an innovative hip energy storage walking orthosis for improving paraplegic walking: A pilot randomized controlled study. Gait Posture. (2017) 57:91–6. doi: 10.1016/j.gaitpost.2017.05.022
40. Arazpour M, Hutchins SW, Ahmadi Bani M, Curran S, Bahramizadeh M, Saberi H, et al. The influence of a rocker sole adaptation on gait parameters in spinal cord injury patients ambulating with the advanced reciprocating gait orthosis - a pilot study. Disabil Rehabil Assist Technol. (2015) 10:89–92. doi: 10.3109/17483107.2013.838805
41. Bani MA, Arazpour M, Ghomshe FT, Mousavi ME, Hutchins SW. Gait evaluation of the advanced reciprocating gait orthosis with solid versus dorsi flexion assist ankle foot orthoses in paraplegic patients. Prosthet Orthot Int. (2013) 37:161–7. doi: 10.1177/0309364612457704
42. Arazpour M, Bani MA, Hutchins SW, Curran S, Javanshir MA. The influence of ankle joint mobility when using an orthosis on stability in patients with spinal cord injury: a pilot study. Spinal Cord. (2013) 51:750–4. doi: 10.1038/sc.2013.78
43. Samadian M, Arazpour M, Ahmadi Bani M, Pouyan A, Bahramizadeh M, Hutchins SW. The influence of orthotic gait training with an isocentric reciprocating gait orthosis on the walking ability of paraplegic patients: a pilot study. Spinal Cord. (2015) 53:754–7. doi: 10.1038/sc.2015.60
44. Arazpour M, Gholami M, Bahramizadeh M, Sharifi G, Bani MA. Influence of Reciprocating Link When Using an Isocentric Reciprocating Gait Orthosis (IRGO) on Walking in Patients with Spinal Cord Injury: A Pilot Study. Top Spinal Cord Inj Rehabil. (2017) 23:256–62. doi: 10.1310/sci16-00016
45. Karimi MT, Amiri P, Esrafilian A, Sedigh J, Fatoye F. Performance of spinal cord injury individuals while standing with the Mohammad Taghi Karimi reciprocal gait orthosis (MTK-RGO). Australas Phys Eng Sci Med. (2013) 36:35–42. doi: 10.1007/s13246-013-0183-3
46. Karimi MT, Fatoye F. Evaluation of the performance of paraplegic subjects during walking with a new design of reciprocal gait orthosis. Disabil Rehabil Assist Technol. (2016) 11:72–9. doi: 10.3109/17483107.2014.921247
47. Portnoy S, Frechtel A, Raveh E, Schwartz I. Prevention of genu recurvatum in poststroke patients using a hinged soft knee orthosis. PMR. (2015) 7:1042–51. doi: 10.1016/j.pmrj.2015.04.007
48. Sato K, Inoue T, Maeda K, Shimizu A, Murotani K, Ueshima J, et al. Early wearing of knee-ankle-foot orthosis improves functional prognosis in patients after stroke. J Stroke Cerebrovasc Dis. (2022) 31:106261. doi: 10.1016/j.jstrokecerebrovasdis.2021.106261
49. Maeshima S, Okazaki H, Okamoto S, Mizuno S, Asano N, Maeda H, et al. A comparison of knee-ankle-foot orthoses with either metal struts or an adjustable posterior strut in hemiplegic stroke patients. J Stroke Cerebrovasc Dis. (2015) 24:1312–6. doi: 10.1016/j.jstrokecerebrovasdis.2015.02.003
50. Talu B, Bazancir Z. The effect of different ankle and knee supports on balance in early ambulation of post-stroke hemiplegic patients. Neurol Sci. (2017) 38:1811–6. doi: 10.1007/s10072-017-3065-8
51. Carse B, Bowers R, Meadows BC, Rowe P. The immediate effects of fitting and tuning solid ankle-foot orthoses in early stroke rehabilitation. Prosthet Orthot Int. (2015) 39:454–62. doi: 10.1177/0309364614538090
52. Pongpipatpaiboon K, Mukaino M, Matsuda F, Ohtsuka K, Tanikawa H, Yamada J, et al. The impact of ankle-foot orthoses on toe clearance strategy in hemiparetic gait: a cross-sectional study. J Neuroeng Rehabil. (2018) 15:41. doi: 10.1186/s12984-018-0382-y
53. Tsuchiyama K, Mukaino M, Ohtsuka K, Matsuda F, Tanikawa H, Yamada J, et al. Effects of ankle-foot orthoses on the stability of post-stroke hemiparetic gait. Eur J Phys Rehabil Med. (2022) 58:352–62. doi: 10.23736/S1973-9087.21.07048-9
54. Lan Y, Xu GQ, Huang DF, Mao YR, Chen SZ, Pei Z, et al. Association between improved trunk stability and walking capacity using ankle-foot orthosis in hemiparetic patients with stroke: evidence from three-dimensional gait analysis. Chin Med J (Engl). (2013) 126:3869–73. doi: 10.3760/cma.j.issn.0366-6999.20130921
55. Do KH, Song JC, Kim JH, Jung GS, Seo SW, Kim YK, et al. Effect of a hybrid ankle foot orthosis made of polypropylene and fabric in chronic hemiparetic stroke patients. Am J Phys Med Rehabil. (2014) 93:130–7. doi: 10.1097/PHM.0b013e3182a92f85
56. Rao N, Aruin AS. Role of ankle foot orthoses in functional stability of individuals with stroke. Disabil Rehabil Assist Technol. (2016) 11:595–8. doi: 10.3109/17483107.2015.1027300
57. Momosaki R, Abo M, Watanabe S, Kakuda W, Yamada N, Kinoshita S. Effects of ankle-foot orthoses on functional recovery after stroke: a propensity score analysis based on Japan rehabilitation database. PLoS ONE. (2015) 10:e0122688. doi: 10.1371/journal.pone.0122688
58. Zollo L, Zaccheddu N, Ciancio AL, Morrone M, Bravi M, Santacaterina F, et al. Comparative analysis and quantitative evaluation of ankle-foot orthoses for foot drop in chronic hemiparetic patients. Eur J Phys Rehabil Med. (2015) 51:185–96.
59. Kim JH, Won BH. Kinematic on ankle and knee joint of post-stroke elderly patients by wearing newly elastic band-type ankle-foot orthosis in gait. Clin Interv Aging. (2019) 14:2097–104. doi: 10.2147/CIA.S222087
60. Kim JH, Sim WS, Won BH. Effectiveness of elastic band-type ankle-foot orthoses on postural control in poststroke elderly patients as determined using combined measurement of the stability index and body weight-bearing ratio. Clin Interv Aging. (2015) 10:1839–47. doi: 10.2147/CIA.S92888
61. Farmani F, Mohseni-Bandpei MA, Bahramizadeh M, Aminian G, Abdoli A, Sadeghi-Goghari M. The influence of rocker bar ankle foot orthosis on gait in patients with chronic hemiplegia. J Stroke Cerebrovasc Dis. (2016) 25:2078–82. doi: 10.1016/j.jstrokecerebrovasdis.2016.02.021
62. Karakkattil PS, Trudelle-Jackson E, Medley A, Swank C. Effects of two different types of ankle-foot orthoses on gait outcomes in patients with subacute stroke: a randomized crossover trial. Clin Rehabil. (2020) 34:1094–102. doi: 10.1177/0269215520927738
63. Nikamp CDM, Buurke JH, van der Palen J, Hermens HJ, Rietman JS. Six-month effects of early or delayed provision of an ankle-foot orthosis in patients with (sub)acute stroke: a randomized controlled trial. Clin Rehabil. (2017) 31:1616–24. doi: 10.1177/0269215517709052
64. Nikamp CDM, van der Palen J, Hermens HJ, Rietman JS, Buurke JH. The influence of early or delayed provision of ankle-foot orthoses on pelvis, hip and knee kinematics in patients with sub-acute stroke: A randomized controlled trial. Gait Posture. (2018) 63:260–7. doi: 10.1016/j.gaitpost.2018.05.012
65. Nikamp CDM, Hobbelink MSH, van der Palen J, Hermens HJ, Rietman JS, Buurke JH, et al. Randomized controlled trial on providing ankle-foot orthoses in patients with (sub-)acute stroke: Short-term kinematic and spatiotemporal effects and effects of timing. Gait Posture. (2017) 55:15–22. doi: 10.1016/j.gaitpost.2017.03.028
66. Nikamp CDM, Hobbelink MSH, van der Palen J, Hermens HJ, Rietman JS, Buurke JH. The effect of ankle-foot orthoses on fall/near fall incidence in patients with (sub-)acute stroke: A randomized controlled trial. PLoS ONE. (2019) 14:e0213538. doi: 10.1371/journal.pone.0213538
67. Pomeroy VM, Rowe P, Clark A, Walker A, Kerr A, Chandler E, et al. A randomized controlled evaluation of the efficacy of an ankle-foot cast on walking recovery early after stroke: SWIFT cast trial. Neurorehabil Neural Repair. (2016) 30:40–8. doi: 10.1177/1545968315583724
68. Pourhoseingholi E, Saeedi H. Role of the newly designed Ankle Foot Orthosis on balance related parametersin drop foot post stroke patients. J Bodyw Mov Ther. (2021) 26:501–4. doi: 10.1016/j.jbmt.2020.11.022
69. Yamamoto S, Motojima N, Kobayashi Y, Osada Y, Tanaka S, Daryabor A. Ankle-foot orthosis with an oil damper versus nonarticulated ankle-foot orthosis in the gait of patients with subacute stroke: a randomized controlled trial. J Neuroeng Rehabil. (2022) 19:50. doi: 10.1186/s12984-022-01027-1
70. Kimura N, Ohata K, Kawasaki S, Nogi S, Tsuruda A, Yamada S. Influencing kinetic energy using ankle-foot orthoses to help improve walking after stroke: a pilot study. Prosthet Orthot Int. (2021) 45:513–20. doi: 10.1097/PXR.0000000000000041
71. Yamamoto S, Tanaka S, Motojima N. Comparison of ankle-foot orthoses with plantar flexion stop and plantar flexion resistance in the gait of stroke patients: A randomized controlled trial. Prosthet Orthot Int. (2018) 42:544–53. doi: 10.1177/0309364618774055
72. Koller C, Reisman D, Richards J, Arch E. Understanding the effects of quantitatively prescribing passive-dynamic ankle-foot orthosis bending stiffness for individuals after stroke. Prosthet Orthot Int. (2021) 45:313–21. doi: 10.1097/PXR.0000000000000012
73. Tyson SF, Vail A, Thomas N, Woodward-Nutt K, Plant S, Tyrrell PJ. Bespoke versus off-the-shelf ankle-foot orthosis for people with stroke: randomized controlled trial. Clin Rehabil. (2018) 32:367–76. doi: 10.1177/0269215517728764
74. Liu Z, Zhang P, Yan M, Xie YM, Huang GZ. Additive manufacturing of specific ankle-foot orthoses for persons after stroke: A preliminary study based on gait analysis data. Math Biosci Eng. (2019) 16:8134–43. doi: 10.3934/mbe.2019410
75. Hsu CC, Huang YK, Kang JH, Ko YF, Liu CW, Jaw FS, et al. Novel design for a dynamic ankle foot orthosis with motion feedback used for training in patients with hemiplegic gait: a pilot study. J Neuroeng Rehabil. (2020) 17:112. doi: 10.1186/s12984-020-00734-x
76. Arazpour M, Tajik HR, Aminian G, Bani MA, Ghomshe FT, Hutchins SW. Comparison of the effects of solid versus hinged ankle foot orthoses on select temporal gait parameters in patients with incomplete spinal cord injury during treadmill walking. Prosthet Orthot Int. (2013) 37:70–5. doi: 10.1177/0309364612448511
77. Andringa AS, Van de Port IG, Meijer JW. Tolerance and effectiveness of a new dynamic hand-wrist orthosis in chronic stroke patients. NeuroRehabilitation. (2013) 33:225–31. doi: 10.3233/NRE-130949
78. Allison R, Shenton L, Bamforth K, Kilbride C, Richards D. Incidence, time course and predictors of impairments relating to caring for the profoundly affected arm after stroke: a systematic review. Physiother Res Int. (2016) 21:210–27. doi: 10.1002/pri.1634
79. Winstein CJ, Stein J, Arena R, Bates B, Cherney LR, Cramer SC, et al. Guidelines for adult stroke rehabilitation and recovery: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. (2016) 47:e98–169. doi: 10.1161/STR.0000000000000098
80. Meng X, Ren M, Zhuang Y, Qu Y, Jiang L, Li Z. Application experience and patient feedback analysis of 3D printed AFO with different materials: a random crossover study. Biomed Res Int. (2021) 2021:8493505. doi: 10.1155/2021/8493505
81. Yoo HJ, Lee S, Kim J, Park C. Lee B. Development of 3D-printed myoelectric hand orthosis for patients with spinal cord injury. J Neuroeng Rehabil. (2019) 16:162. doi: 10.1186/s12984-019-0633-6
82. Hada T, Momosaki R, Abo M. Impact of orthotic therapy for improving activities of daily living in individuals with spinal cord injury: a retrospective cohort study. Spinal Cord. (2018) 56:790–5. doi: 10.1038/s41393-018-0088-9
83. Arazpour M, Ahmadi Bani M, Kashani RV, Tabatabai Ghomshe F, Mousavi ME, Hutchins SW. Effect of powered gait orthosis on walking in individuals with paraplegia. Prosthet Orthot Int. (2013) 37:261–7. doi: 10.1177/0309364612463164
84. Kandilakis C, Sasso-Lance E. Exoskeletons for Personal Use After Spinal Cord Injury. Arch Phys Med Rehabil. (2021) 102:331–7. doi: 10.1016/j.apmr.2019.05.028
Keywords: orthotics, 3D-printing, motor dysfunction, stroke, spinal cord injury
Citation: Cui Y, Cheng S, Chen X, Xu G, Ma N, Li H, Zhang H and Li Z (2023) Advances in the clinical application of orthotic devices for stroke and spinal cord injury since 2013. Front. Neurol. 14:1108320. doi: 10.3389/fneur.2023.1108320
Received: 25 November 2022; Accepted: 27 January 2023;
Published: 17 February 2023.
Edited by:
Filippo Camerota, Sapienza University of Rome, ItalyReviewed by:
Claudia Celletti, Umberto 1 Hospital, ItalyFan Gao, University of Kentucky, United States
Copyright © 2023 Cui, Cheng, Chen, Xu, Ma, Li, Zhang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhenlan Li,  emhlbmxhbkBqbHUuZWR1LmNu
emhlbmxhbkBqbHUuZWR1LmNu
 Yinxing Cui
Yinxing Cui Shihuan Cheng
Shihuan Cheng Xiaowei Chen
Xiaowei Chen Guoxing Xu
Guoxing Xu Ningyi Ma
Ningyi Ma He Li
He Li Hong Zhang
Hong Zhang Zhenlan Li
Zhenlan Li