
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol. , 11 April 2023
Sec. Neuromuscular Disorders and Peripheral Neuropathies
Volume 14 - 2023 | https://doi.org/10.3389/fneur.2023.1100641
This article is part of the Research Topic Surgical Treatment of Peripheral Neuropathic Pain, Peripheral Nerve Tumors, and Peripheral Nerve Injury View all 25 articles
Objective: Unilateral biportal endoscopy (UBE) represents a relatively recent development in minimally invasive spine surgery. This study aimed to evaluate the efficacy and safety of UBE foraminotomy and diskectomy combined with piezosurgery for treating cervical spondylotic radiculopathy (CSR) with neuropathic radicular pain.
Methods: We retrospectively analyzed the outcomes in 12 patients with CSR who underwent UBE foraminotomy and diskectomy combined with piezosurgery. The intraoperative blood loss, operative time, visual analog scale (VAS) scores for the neck and arm, neck disability index (NDI) scores, and complications were recorded.
Results: Postoperative VAS scores of the neck and arm and NDI scores were significantly improved. Additionally, a postoperative CT scan revealed adequate enlargement of the cervical canal and nerve root. No specific complications occurred during surgery and the immediate postoperative period.
Conclusions: This primary study indicated that the UBE foraminotomy and diskectomy with piezosurgery is a promising technique for treating cervical spondylotic radiculopathy with neuropathic radicular pain.
With the arrival of an aging society, the number of patients with cervical spondylotic radiculopathy (CSR), which is one of the degenerative spinal diseases, is increasing rapidly (1). CSR is the most common form of cervical spondylosis, mainly due to cervical nerve root compression caused by disc degeneration, herniation, segmental instability, or other conditions, mainly manifested as neuropathic radicular pain. CSR, the most prevalent form of cervical spondylosis, is caused by cervical nerve root compression due to disc degeneration, herniation, segmental instability, or other conditions, mainly manifested as neuropathic radicular pain (2). Although anterior cervical discectomy and fusion (ACDF) is the gold standard surgical strategy for the treatment of CSR, it has several disadvantages, including adjacent segment degeneration, incision and implant-related complications, and high hospitalization costs (3). In addition, it is reported that anterior open surgery is closely associated with a high risk of postoperative dysphagia (4). Consequently, minimally invasive spinal surgeries have emerged with similar clinical outcomes, which have several advantages, including less injury, shorter hospital stay, and fewer postoperative complications (5).
Unilateral biportal endoscopy (UBE) is a minimally invasive spinal surgery with minimal injury to the surrounding structures, thereby greatly increasing the stability of the operated segment (6). Currently, UBE has gradually been applied for cervical disorders with remarkable efficiency and conveniency (6, 7).
However, whether piezosurgery can be used in UBE surgery has not been reported. This study aimed to evaluate the efficacy and safety of UBE foraminotomy and diskectomy combined with piezosurgery for treating CSR with neuropathic radicular pain
We retrospectively followed a group of 12 patients suffering from CSR and received UBE foraminotomy and diskectomy with piezosurgery between May 2020 and June 2021. The average age of patients was 50.2 ± 9.5 years, seven of them were men and five were women. The demographic and clinical characteristics of patients were shown in Table 1. This research was approved by the Ethics Committee of Affiliated Hangzhou Chest Hospital, Zhejiang University School of Medicine. Each patient provided written informed consent before being administered any treatment.
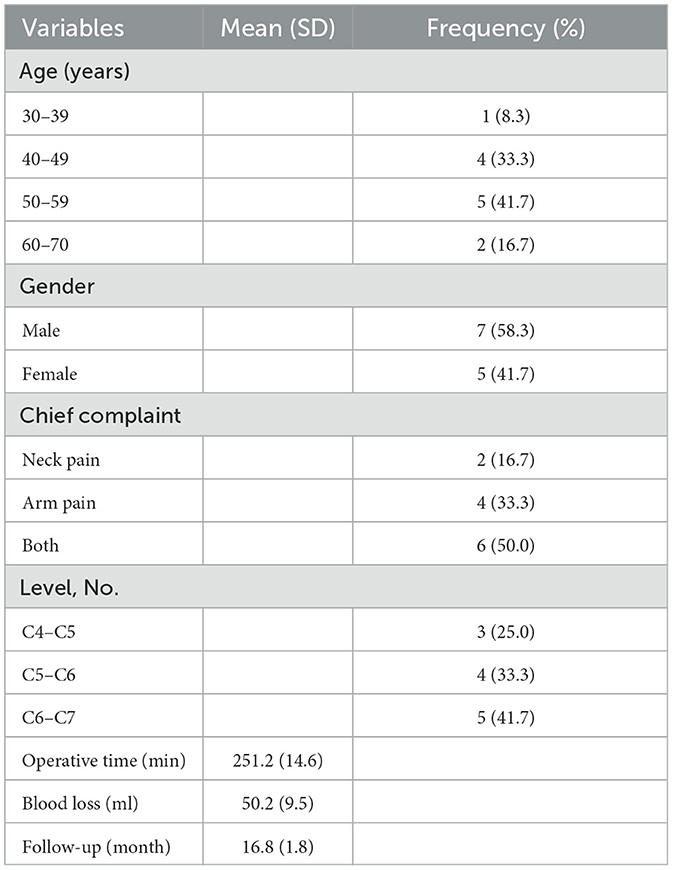
Table 1. Biodemographic data of patients with CSR who underwent UBE foraminotomy and diskectomy combined with piezosurgery.
The CSR patients were initially diagnosed according to a combination of the patient's clinical history, radicular symptoms, and radiographic scan. Inclusion criteria were as follow: no improvement in radicular symptoms after at least 3 months of conservative treatments with oral NSAIDs and neurotrophy drugs, no previous cervical surgery, 1-level disk herniation, no large disk repress cervical myelopathy, and the patient refused conventional open surgeries. Exclusion criteria included: disc herniation with no radicular symptoms, accompanying spinal instability, and coexisting spinal infection or malignancy.
Following general anesthesia, the patient underwent surgery in a prone position on a chest pad, and the neck was placed in slight flexion using a horseshoe-shaped headrest. With the guidance of a C-arm fluoroscope, the target interlaminar space was identified and marked. Two 1.5 cm skin incisions about 1 to 1.5 cm ipsilateral to the spinous process line were created at 1 cm above and below the marker line. Next, a series of dilators were used to split the paraspinal muscle and created the two viewing and working portals. The viewing portal was used to provide surgical vision, while the working portal was used for instrument handling.
Under endoscopic guidance, the soft tissue was removed from the bone surface with a bipolar radiofrequency probe until the “V” point is exposed. Thereafter, foraminotomy was carefully performed on the inferior lamina, superior lamina, interlaminar spaces, and the medial portion of the facet joint. An oval hole about 2 cm in the bone was made with a high-speed spherical drill and Piezosurgery device (XD880A, SMTP Technology Co., Ltd.) (Figure 1). The use of Piezosurgery device can safely and efficiently remove the bone around the nerve root, thereby fully releasing the nerve root.
After the cervical nerve root and herniated disc were seen under the endoscope, a diskectomy was performed to remove the herniated nucleus pulposus tissue, thus releasing the nerve root. Subsequently, complete decompression of the spinal cord and nerve root was confirmed. Finally, the endoscopy and instrument were withdrawn, a drainage tube was placed, and then the wound was closed. The surgical procedure is shown in Figure 2.
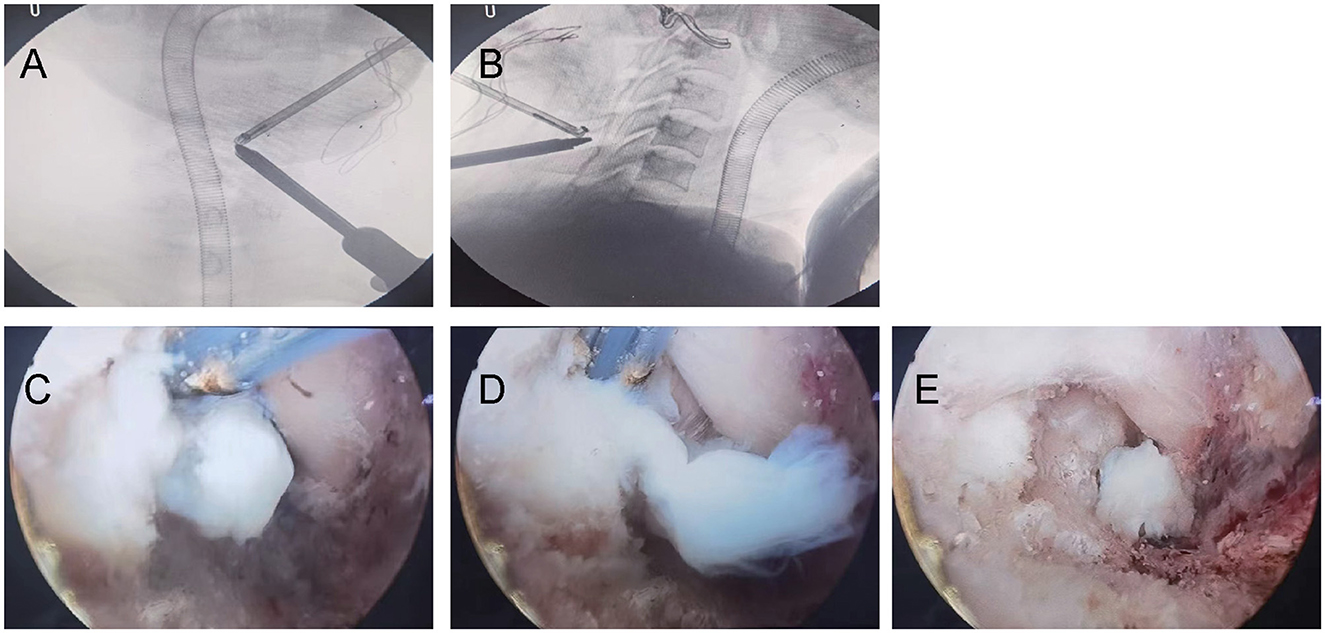
Figure 2. (A, B) Radiographic anteroposterior represented the locations of viewing and working portals. (C–E) Diskectomy was performed.
Intraoperative blood loss, operative time, visual analog scale (VAS) score for the neck and arm, Neck Disability Index (NDI) scores and complications were documented. Radiographic examinations including MRI and CT were performed to access the extent of disc herniation, the status of the spinal cord and nerve root, and relevant bony structures preoperatively and at the follow-up periods.
Statistical analyses were conducted on all data employing SPSS 16.0 (IBM, USA). Results were presented as mean ± standard deviation (SD). Herein, Fisher's exact probability test, independent-samples t-test, and one-way ANOVA analysis were conducted employing SPSS. p < 0.05 was judged significant.
Table 1 shows the mean operation time and intraoperative blood loss. Postoperative CT scan revealed adequate enlargement of the cervical canal and nerve root (Figure 3). At the final follow-up, VAS scores of the neck and arm and NDI scores were significantly improved compared to the pre-operation (Figure 4).
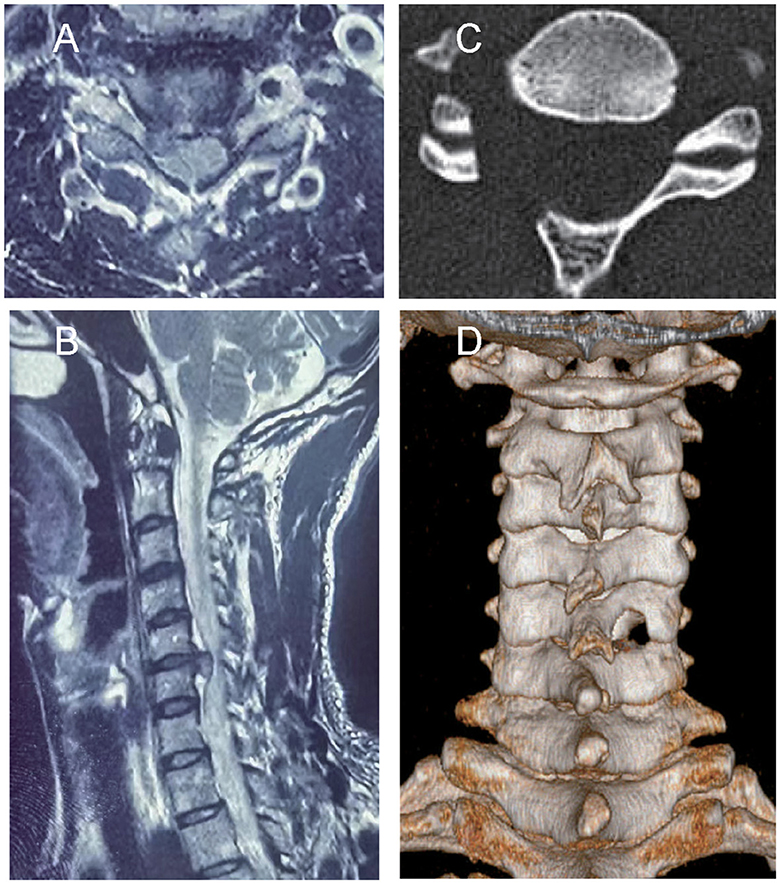
Figure 3. A 40-year-old man had cervical 5–6 intervertebral disc herniation, presenting with neck pain and numbness in the right upper limb. (A, B) Preoperative axial and sagittal magnetic resonance images showed C5/6 disk protrusion on the right subarticular zone. (C) Postoperative axial computed tomography scan showed the location of the unilateral foraminotomy. (D) Postoperative 3-dimensional computed tomography scan showed widening of the spinal canal after surgery.
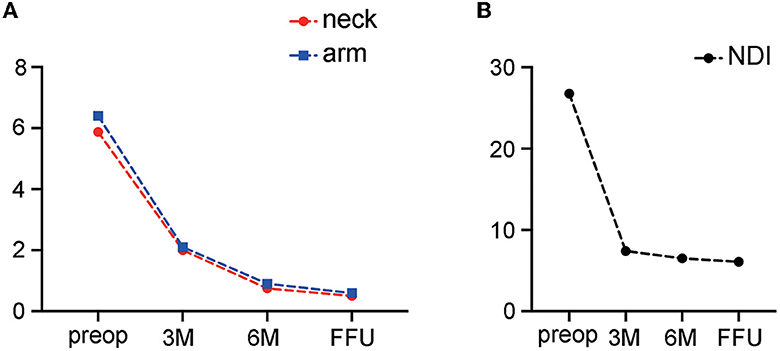
Figure 4. At the final follow-up, VAS scores of the neck and arm (A) and the Neck Disability Index (NDI) scores (B) were significantly improved compared to the pre-operation (P < 0.05). preop, preoperative; M, month; FFU, final follow-up.
No specific complications occurred during surgery and the immediate postoperative period. No patient required additional surgery for sustained or aggravated symptoms during postoperative hospitalization. No patient had the nerve or vascular injury during surgery, and no patient experienced persistent or aggravated symptoms during the postoperative hospitalization.
CSR, mainly manifested as neuropathic radicular pain, is one of the common spinal disorders and usually requires only conservative treatment. However, when conservative treatment fails, surgery is necessary to relieve the symptoms by removing the compression (8). Generally, ACDF is the primary surgical strategy for CSR with good outcomes, however, it is accompanied by several limitations, including limited neck mobility, adjacent segment degeneration, and high reoperation rate (9–11). In addition, there is conflicting evidence regarding the efficacy of anterior foraminotomy, with reported success rates of 52–99%, but recurrence of radicular symptoms is as high as 30% (12).
With the development of new technology and devices, the application of minimally invasive endoscopic surgery to treat CSR is gradually increasing, with better outcomes and fewer complications compared to ACDF (13–15). A decade ago, percutaneous endoscopic cervical diskectomy using a small-sized single portal was introduced, which was reported to not only minimize surgical trauma but also effectively relieve compression (16, 17). However, working and viewing in the same narrow portal manifested several difficulties, such as disorientation and difficulty in maneuvering (18, 19).
Currently, UBE technology represents a relatively recent development in minimally invasive spine surgery (20, 21). Compared with uniportal endoscopic surgery, UBE with two portals has important advantages in improving the scope of the surgical field and the freedom of working devices. Through independent viewing and working portals, the operator can maneuver comfortably with working devices, such as piezosurgery and drills, to expand the range of exploration and decompression. Moreover, independent control of the 30-degree endoscope can enlarge the surgical field of view, which is conducive to the observation of tiny blood vessels and ligaments, thereby reducing iatrogenic blood vessels and neurological injuries. At the same time, the use of continuous irrigation not only provides a clearer view to preventing intraoperative complications but also flushes away inflammatory factors to reduce postoperative pain and the risk of infection (22).
As we all know, the vessels and nerves around the spine are dense and complex. During foraminotomy and diskectomy, there is a risk of unintended injury to the nerve root, blood vessel, and dura. In particular, rotary drills are commonly used to remove bone tissue, however, they undoubtedly increase the risk of neurovascular structures due to their rotational power and limited operating space (23). Piezosurgery technique is based on micro-vibrations, which selectively cuts bone tissue and preserve surrounding soft tissue structures (24). Piezosurgery device performs bone cutting by controlled scraping motion without rotational power, which provides precise and safe bone removal procedures with reduced risk to adjacent soft tissue (25). To our knowledge, the present study first combined Piezosurgery device and UBE for cervical foraminotomy and discectomy to optimize surgical precision and reduce surgical risks. A series of foraminotomy and diskectomy in 12 patients with CSR was performed, which showed that the postoperative VSA and NDI scores were significantly improved at the final follow-up. No nerve or vascular injury occurred during surgery and the immediate postoperative period. Meanwhile, no patient experienced persistent or aggravated symptoms during the postoperative hospitalization.
The current study has several limitations: (1) It was a retrospective non-randomized comparative study; (2) Need a larger number of patients and a longer follow-up period to further confirm the outcomes; (3) The disadvantage of UBE surgery is that it is relatively difficult and requires a long learning curve for the surgeon to gain proficiency.
In summary, UBE foraminotomy and diskectomy with piezosurgery is a promising technique for the treatment of cervical spondylotic radiculopathy, which has several advantages, including improvement of pain and functional disability, less blood loss, low hospitalization cost, and preservation of spinal tissue.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethics Committee of Affiliated Hangzhou Chest Hospital, Zhejiang University School of Medicine. The patients/participants provided their written informed consent to participate in this study.
Conceptualization: YJ. Methodology: BZ. Validation: MZ. Writing original draft preparation: PZ. Writing-review and editing: XY. Project administration: QZ. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer HQ declared a shared affiliation with the authors at the time of review.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Cook C, Roman M, Stewart KM, Leithe LG, Isaacs R. Reliability and diagnostic accuracy of clinical special tests for myelopathy in patients seen for cervical dysfunction. J Orthop Sports Phys Ther. (2009) 39:172–8. doi: 10.2519/jospt.2009.2938
2. Hu JH, Chen F, Qiu GX, Sun TS, Yang HL, Shen HY, et al. Jingshu Keli for treating cervical spondylotic radiculopathy: the first multicenter, randomized, controlled clinical trial. J Orthop Translat. (2020) 27:44–56. doi: 10.1016/j.jot.2020.10.010
3. Jung SB, Kim N. Biportal endoscopic spine surgery for cervical disk herniation a technical notes and preliminary report. Medicine. (2022) 101:e29751. doi: 10.1097/MD.0000000000029751
4. Puvanesarajah V, Jain A, Shimer AL, Singla A, Shen F, Hassanzadeh H. Complications and mortality following one to two-level anterior cervical fusion for cervical spondylosis in patients above 80 years of age. Spine. (2017) 42:E509–14. doi: 10.1097/BRS.0000000000001876
5. Yuan H, Zhang XF, Zhang L M, Yan YQ, Liu YK, Lewandrowski KU. Comparative study of curative effect of spinal endoscopic surgery and anterior cervical decompression for cervical spondylotic myelopathy. J Spine Surg. (2020) 6:S186–96. doi: 10.21037/jss.2019.11.15
6. Kim J, Heo DH, Lee DC, Chung HT. Biportal endoscopic unilateral laminotomy with bilateral decompression for the treatment of cervical spondylotic myelopathy. Acta Neurochir. (2021) 163:2537–43. doi: 10.1007/s00701-021-04921-0
7. Zhu CY, Deng XQ, Pan H, Zhang W. Unilateral biportal endoscopic laminectomy with lateral mass screw fixation for treating cervical spinal stenosis. Acta Neurochir. (2022) 164:1529–33. doi: 10.1007/s00701-022-05212-y
8. Park JH, Jun SG, Jung JT, Lee SJ. Posterior percutaneous endoscopic cervical foraminotomy and diskectomy with unilateral biportal endoscopy. Orthopedics. (2017) 40:e779–83. doi: 10.3928/01477447-20170531-02
9. Epstein NE, A. review of complication rates for anterior cervical Diskectomy and fusion (ACDF). Surg Neurol Int. (2019) 10:100. doi: 10.25259/SNI-191-2019
10. Chung JY, Kim SK, Jung ST, Lee KB. Clinical adjacent-segment pathology after anterior cervical discectomy and fusion: results after a minimum of 10-year follow-up. Spine J. (2014) 14:2290–8. doi: 10.1016/j.spinee.2014.01.027
11. Shousha M, Alhashash M, Allouch H, Boehm H. Reoperation rate after anterior cervical discectomy and fusion using standalone cages indegenerative disease: a study of 2,078 cases. Spine J. (2019) 19:2007–12. doi: 10.1016/j.spinee.2019.08.003
12. Tong Y, Huang Z, Hu C, Fan Z, Bian F, Yang F, et al. A comparison study of posterior cervical percutaneous endoscopic ventral bony decompression and simple dorsal decompression treatment in cervical spondylotic radiculopathy caused by cervical foraminal and/or lateral spinal stenosis: a clinical retrospective study. BMC Musculoskelet Disord. (2020) 21:290. doi: 10.1186/s12891-020-03313-2
13. Bonaldi G, Minonzio G, Belloni G, Dorizzi A, Fachinetti P, Marra A, et al. Percutaneous cervical diskectomy: preliminary experience. Neuroradiology. (1994) 36:483–6. doi: 10.1007/BF00593690
14. Chiu JC, Hansraj KK, Akiyama C, Greenspan M. Percutaneous (endoscopic) decompression discectomy for non-extruded cervical herniated nucleus pulposus. Surg Technol Int. (1997) 6:405–11.
15. Knight MT, Goswami A, Patko JT. Cervical percutaneous laser disc decompression: preliminary results of an ongoing prospective outcome study. J Clin Laser Med Surg. (2001) 19:3–8. doi: 10.1089/104454701750066875
16. Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic cervical posterior foraminotomy for the operation of lateral disc herniations using 59-mm endoscopes: a prospective, randomized, controlled study. Spine. (2008) 33:940–8. doi: 10.1097/BRS.0b013e31816c8b67
17. Ruetten S, Komp M, Merk H, Godolias G. A new full-endoscopic technique for cervical posterior foraminotomy in the treatment of lateral disc herniations using 69-mm endoscopes: prospective 2-year results of 87 patients. Minim Invasive Neurosurg. (2007) 50:219–26. doi: 10.1055/s-2007-985860
18. Ahn Y. Percutaneous endoscopic decompression for lumbar spinal stenosis. Expert Rev Med Devices. (2014) 11:605–16. doi: 10.1586/17434440.2014.940314
19. Minamide A, Yoshida M, Yamada H, Nakagawa Y, Maio K, Kawai M, et al. Clinical outcomes of microendoscopic decompression surgery for cervical myelopathy. Eur Spine J. (2010) 19:487–93. doi: 10.1007/s00586-009-1233-0
20. Choi CM, Chung JT, Lee SJ, Choi DJ. How i do it? biportal endoscopic spinal surgery (BESS) for treatment of lumbar spinal stenosis. Acta Neurochir. (2016) 158:459–63. doi: 10.1007/s00701-015-2670-7
21. Ahn JS, Lee HJ, Choi DJ, Lee KY, Hwang SJ. Extraforaminal approach of biportal endoscopic spinal surgery: a new endoscopic technique for transforaminal decompression and discectomy. J Neurosurg Spine. (2018) 28:492–8. doi: 10.3171/2017.8.SPINE17771
22. Soliman HM. Irrigation endoscopic discectomy: a novel percutaneous approach for lumbar disc prolapse. Eur Spine J. (2013) 22:1037–44. doi: 10.1007/s00586-013-2701-0
23. Chanda A, Nanda A. Retrosigmoid intradural suprameatal approach: advantages and disadvantages from an anatomical perspective. Neurosurgery. (2006) 59:ONS1–6. doi: 10.1227/01.NEU.0000220673.79877.30
24. Vercellotti T. Technological characteristics and clinical indications of piezoelectric bone surgery. Minerva Stomatol. (2004) 53:207–14.
Keywords: cervical spondylotic radiculopathy, neuropathic radicular pain, unilateral biportal endoscopy, piezosurgery, foraminotomy and diskectomy
Citation: Zhang P, Jin Y, Zhu B, Zheng M, Ying X and Zheng Q (2023) Unilateral biportal endoscopic foraminotomy and diskectomy combined with piezosurgery for treating cervical spondylotic radiculopathy with neuropathic radicular pain. Front. Neurol. 14:1100641. doi: 10.3389/fneur.2023.1100641
Received: 17 November 2022; Accepted: 14 February 2023;
Published: 11 April 2023.
Edited by:
Shizhang Ling, The First Affiliated Hospital of Wannan Medical College, ChinaReviewed by:
Viktor Aleinikov, National Center for Neurosurgery, KazakhstanCopyright © 2023 Zhang, Jin, Zhu, Zheng, Ying and Zheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaozhang Ying, eXh6OTkxMDEwQHpjbXUuZWR1LmNu; Qi Zheng, MTM2NTY2NDIwMDhAMTYzLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.