
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol. , 25 October 2022
Sec. Endovascular and Interventional Neurology
Volume 13 - 2022 | https://doi.org/10.3389/fneur.2022.990722
 Neeharika Krothapalli1
Neeharika Krothapalli1 Mohamad Fayad2
Mohamad Fayad2 Smit Patel2
Smit Patel2 Ahmed Elmashad1
Ahmed Elmashad1 Eric Sussman3
Eric Sussman3 Charles Bruno2
Charles Bruno2 Andrew Grande4
Andrew Grande4 Bharathi Jagadeesan4
Bharathi Jagadeesan4 Brendan Killory3
Brendan Killory3 Mark Alberts5
Mark Alberts5 Inam Kureshi3
Inam Kureshi3 Martin Ollenschleger2
Martin Ollenschleger2 Ramachandra Tummala4
Ramachandra Tummala4 Tapan Mehta2*
Tapan Mehta2*Background: Trans-radial access (TRA) for MMA embolization has grown due to lower access site complications and greater patient satisfaction. Here, we describe the feasibility of utilizing a 6F Envoy Simmons 2 (6F-SIM2) as a guide catheter with TRA and compare outcomes with trans-femoral approach (TFA) in a single center case series.
Methods: We performed a retrospective review of patients who underwent MMA embolization for management of chronic subdural hematoma (cSDH). TRA was performed by utilizing a combination of 6F 90cm Envoy (Codman & Shurtleff, Inc., Rayham, MA) Simmons 2 guide catheter and 5F 125cm Sofia (Microvention, Aliso Viejo, CA) intermediate catheter. Outcomes measured are Modified Rankin Score (mRS) at 90 days, inpatient mortality, post-embolization recurrence, fluoroscopy time and radiation exposure.
Results: A total of 71 patients underwent 97 MMA embolization overall with 65 (67%) in trans-femoral access group, 11 (11.3%) in trans-radial access without use of Simmons 2 Guide catheter group and 21 (21.6%) in trans-radial access with use of Simmons 2 Guide catheter group. There were no direct access-related complications in either group. One patient had thromboembolic stroke in trans-femoral group. There was no difference in average procedure-related total fluro time or radiation dose among all three groups.
Conclusion: Trans-radial approach using 6F-SIM2 guide catheter coupled with 5F Sofia intermediate catheter is safe and effective. It provides an alternative approach to access distal branches of bilateral anterior circulation in elderly patients with difficult anatomy undergoing MMA embolization.
The feasibility of trans-radial approach has been demonstrated in a variety of endovascular procedures including flow diversion, aneurysm coiling, carotid stenting, acute ischemic stroke and MMA embolization (1, 2) for its lower rate of access complications and reduced cost (3, 4). Most importantly, trans-radial approach (TRA) has a much higher patient satisfaction due to earlier ambulation, shorter hospital stay, and avoidance of groin shaving and exposure. Several studies did directly elucidate the differences in the angiographic and clinical outcomes of TRA and trans-femoral approach (TFA) (5, 6). In patients with a bovine aortic arch and common carotid innominate trunk, TRA with a 6F larger system for intracranial embolization is less challenging compared to the more common non-bovine aortic arch as there is lesser likelihood of requiring a Simmons shape catheter for shape formation within the aortic arch. Moreover, catheterization of the left middle meningeal artery through trans-radial approach can be challenging especially in non-bovine Type II/III aortic arches. The risk of guide catheter herniation remains higher in Type II/III arches with pre-existing tortuosity in great vessels. Unstable access does theoretically increase the risk of complications during intracranial embolization. This can be averted by utilizing a guide catheter with Simmons2 shape, which can redirect intermediate and microcatheter force during advancement into the carotid artery as the curvature point of a Simmons catheter is supported by the ventral wall of an aortic arch. Previous studies have described use of reverse angled guide catheter use for trans-femoral and trans-radial approach for treatment of carotid artery stenting (7–9).
In our study, we describe the feasibility of tri-axial trans-radial approach using 6F Envoy Simmons 2 (6F-SIM2) guide catheter coupled with a 5F Sofia intermediate catheter to perform bilateral MMA embolization.
This is a single center retrospective observational study of patients age ≥18 with cSDH who presented to our comprehensive stroke center between 01/01/2020 to 12/01/2021 and underwent MMA embolization procedures for cSDH. MMA embolization was performed on cSDH patients with CT head demonstrating iso-density or hypodensity of ≥50% of the volume of blood products in the subdural space. Patients also had to have evidence of mass effect with or without midline shift. They required a 24-h follow-up head CT indicating stability of the SDH. Patients with neurological symptoms such as headaches, cognitive decline, speech difficulties, gait impairment or imbalance, weakness, paresthesia, and seizures who were not surgical candidates were not excluded from an MMA embolization. Patients were excluded from MMA embolization if they required urgent neurosurgical evacuation, had focal SDH within frontal, temporal base or interhemispheric space without involvement of the cerebral convexity, demonstrated secondary SDH due to vascular lesion such as dural arteriovenous fistula or arterial venous malformation, brain tumor, spontaneous intracranial hypotension or in setting of craniotomy not performed for subdural evacuation. Patients with comorbidities such as cardiopulmonary instability, severe carotid artery disease resulting in occlusion, near occlusion of the external carotid artery or increasing risk of stroke, mRS of 4–6 or life expectancy < 1-year, end stage renal disease and significant coagulopathy were excluded. Pregnant patients or patients with contralateral blindness were also excluded. Access approach was determined by the proceduralist. Study variables included age, gender, vessel anatomy (aortic arch type, left common carotid artery loop, brachiocephalic trunk tortuosity), side of SDH, catheter system used, type of embolic material, fluoroscopy time, radiation dose, etiology of hematoma, anticoagulants or antiplatelets used, history of coagulopathy, presence of midline shift and size of pre-embolization SDH on initial head CT as reported by the radiologist. Focused procedure-related outcomes measured failed access, guide catheter herniation events, access site complications and peri-procedural ischemic stroke.
A descriptive analysis was performed for all patients with MMA embolization of cSDH and compared TFA vs. TRA without use of Simmons 2 Guide catheter vs. TRA with use of Simmons 2 Guide catheter groups. Wilcoxon Rank-Sum test and Student's t-test for continuous variables and categorical variables were compared using Chi-square tests of proportion as cell frequencies permitted and Fisher's exact test when frequencies were ≤ 5. Comparison was univariate as small sample size was insufficient for multivariate analysis. Data analysis was performed with statistical package SAS 9.4. This study was approved by the Institutional Review Board of our hospital with total waiver of consent since it does not contain direct enrollment of patients.
All procedures were performed under general anesthesia. Access to right radial artery was obtained under ultrasound guidance and a 6F slender Terumo radial sheath was placed and connected to continuous flush of heparinized saline at a concentration of 5iu/ml. A 6F Envoy Simmons 2 guide catheter as well as a 5F Sofia intermediate catheter were flushed, prepped on a sterile table and connected to continuous flush of heparinized saline. The intermediate catheter was introduced into the guide catheter followed by a baby J Glide wire into the intermediate catheter. The system was then placed into the radial sheath and baby J Glide wire was introduced about 30 cm followed by 10 cm of the intermediate catheter. Subsequently, the entire system was advanced together under fluoroscopy guidance into the descending aortic arch. The Glide wire was then retrieved and intermediate catheter was pulled back proximal to the Simmons 2 shape. In select cases with Type III anatomy, it can be difficult to navigate the glide wire over the aortic arch. In these situations, we typically used a 5F 120 cm Angled tip catheter to facilitate ascent of the glide wire over the lesser curve of the aortic arch. Next, the guide catheter was slowly rotated in a counterclockwise maneuver until the Simmons knot is formed and advanced into the ascending arch. After the common carotid artery was selected, the Sofia intermediate catheter was advanced over a glide wire under roadmap guidance to properly select the internal carotid artery for orbital blood supply confirmation. The external carotid artery was then selected. A variety of microcatheters were used for embolization based on compatibility with the form of embolization. Figure 1 is an anterior-posterior view of head and neck demonstrating 6F Envoy Simmons2 access (hollow arrow) with 5F Sofia intermediate catheter (solid arrow) with a left common carotid artery run. Figure 2 is an anterior-posterior view of head and neck without digital subtraction angiography and shows catheterization of the left common carotid artery.

Figure 1. Anterior-posterior view of head and neck demonstrating 6F Envoy Simmons2 access with 5F Sofia intermediate catheter with left common carotid artery run.
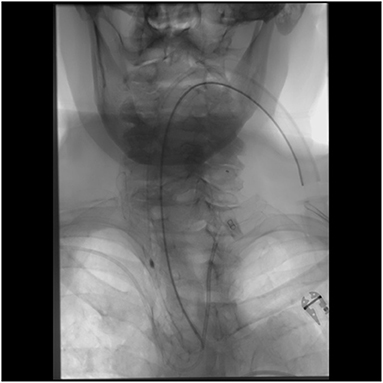
Figure 2. Anterior-posterior view of head and neck showing catheterization of left common carotid artery.
A total of 71 patients underwent a total of 97 MMA embolization with 65 (67%) in trans-femoral access group, 11 (11.3%) in trans-radial access without use of Simmons 2 Guide catheter group and 21 (21.6%) in trans-radial access with use of Simmons 2 Guide catheter group. Table 1 demonstrates baseline clinical characteristics and outcomes of the case series. There was no difference observed in anatomical factors contributing to difficult access like tortuosity of left common carotid artery [TFA (41.5%), TRwoSim2 (45.5%); p = 0.098 vs. TRwSim2 (57.1%); p = 0.20], tortuous right subclavian-brachiocephalic trunk [TFA (75.4%), TRwoSim2 (72.7%); p = 0.85 vs. TRwSim2 (71.4%); p = 0.72], Type II/III arch [TFA (Type II 95.4%, Type III 1.5%), TRwoSim2 (100%); p = 0.54 vs. TRwSim2 (Type II 90.5%, Type III 9.5%); p = 0.40 and 0.08], or aortic arch diameter > 28 mm [TFA (40%), TRwoSim2 (36.3%), TRwSim2 (42.8%); p = 0.82]. We also did not observe any difference among the three groups for radiation dose [TFA (723 mGy), TRwoSim2 (557 mGy); p = 0.74 vs. TRwSim2 (672 mGy); p = 0.76] or fluoroscopy time [TFA (40.5 min), TRwoSim2 (29 min); p = 0.33 vs. TRwSim2 (33.1 min); p = 0.22].
There was no difference observed in anticoagulation use at time of index event [TFA (29.2%), TRwoSim2 (18.1%), TRwSim2 (42.9%)]. Antiplatelet use at time of index event was higher in TRwoSim2 group compared to TFA group (63.6 vs. 29.2%; p = 0.026). A significant variability was noted in resumption of antiplatelet or anticoagulant medications (as reported in Table 1). The projected time for antiplatelet or anticoagulation hold was not available due to variations in decision making in individual clinician plans and complexity of individual patient case. Determining the role of antiplatelet or anticoagulation use contributing to recurrence of subdural hematoma is beyond the scope of this study.
Mortality unrelated to procedure occurred in 3 (3.9%) patients overall with 1 (3.6%) in TRA and 2 (4.17%) in TFA group within 90 days. There was no mortality related to procedure in either group. There were no failed cases that necessitated a different set-up. There were no access site complications in either group but one patient had thromboembolic stroke in trans-femoral group. Two patients in trans-femoral group had guide catheter herniation at the time of MMA catheterization.
Trans-radial access (TRA) for coronary interventions demonstrated >60% reduction in access site complications (10–12). Utilization of TRA for neuro-interventional procedures provides certain advantages over trans-femoral approach (TFA) including immediate ambulation, greater patient satisfaction, reduced postprocedural hospital stay and cost saving (13–15). This strategy has now been employed in a variety of neuro-interventions including diagnostic angiograms, flow diversion, mechanical thrombectomy, aneurysm coiling, AVM embolization and carotid artery stenting (5, 6, 16, 17).
Superiority of radial vs. femoral vascular access can be difficult to assess in patients with ischemic stroke, intracranial aneurysm embolization or high flow vascular malformation embolization. The variation in selection of ideal access approach is significantly influenced by necessity of a larger size guide catheter and/or speed to approach the target lesion (i.e., in mechanical thrombectomy cases with ischemic stroke). One of the major strengths of our study is that we have compared the outcomes of access approaches for only elective MMA embolization cases, which usually does not require larger than 6F access. The patient population is also more uniform as the majority of MMA embolizations are common in elderly patients (median age of 73 years) with higher incidence of arch complexities. At our organizations, individual operators had different access route preferences. However, those who used radial first as the MMA embolization approach prefer to use 6F Envoy transradial access set up as primary approach as long as radial artery anatomy is favorable. For trans-radial approach, the only exception for not using reverse angle guide catheter was bovine arch anatomy as it can be easily accessed with straight tip or angled tip catheters and does not require additional support. Traditionally we have also avoided transradial approach with heavy calcifications involving aortic arch or right subclavian-brachiocephalic complex as the risk of plaque disruption would be theoretically higher with manipulation of reverse angle guide catheters.
In literature, TRA has demonstrated maximal benefit in patients with bovine arch, large body habitus, occlusive aorto-iliac disease, approach to posterior circulation and concurrent use of anticoagulation or antiplatelet agents during procedure (18). Despite the plethora of benefits with a trans-radial approach, there are some hurdles to overcome. Some unfavorable factors for radial artery access include Type II or III arch while selecting intracranial segments of left internal or external carotid artery branches, marked subclavian or innominate tortuosity, small size of radial artery and other uncommon arch variants. Jo et al reported 82.6% success rates of selective catheterization to the left internal carotid artery through radial access (19). A prospective review by Sattur et al demonstrated that procedural success was achieved in 92.3% of patients who underwent TRA and crossover to femoral route occurred in 6.5% of cases (20). In our series, there were no access-site complications or TRA-to-TFA conversion.
Our study has several limitations. The retrospective design of our study may have led to selection bias, limiting the generalizability of results. In this analysis, there is data for patients treated with MMA embolization but not for proportions of patients excluded by the initial triage process. Small sample size and individual operator bias for procedural methods are significant confounders. Determining the role of antiplatelet or anticoagulation use contributing to recurrence of subdural hematoma is beyond the scope of this study.
In summary, our study demonstrates that utilizing a reverse angle guide catheter like 6F 90 cm Envoy (Simmons 2 shape) along with soft 5F Sofia intermediate catheter in type II/III arches may be a relatively safe and proficient approach to access distal left anterior circulation branches through TRA. The 5F Sofia distal access catheter is soft enough that it does not disrupt the Simmons 2 shape of 6F Envoy guide catheter. This approach may be superior to TFA in select procedures like MMA embolization, where TFA with tortuous aortic arch may prove more time consuming, difficult and demonstrate higher embolic risk in atherosclerotic vessels (21).
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Hartford Hospital, HHC-2021-0088. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
NK and TM: substantial contribution to conception, design, analysis and interpretation of data, drafted and reviewed the work. MF and SP: drafted and reviewed the work. AE, ES, CB, AG, BJ, BK, MA, IK, MO, and RT: reviewed the work. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Rajah GB, Waqas M, Dossani RH, Vakharia K, Gong AD, Rho K, et al. Transradial middle meningeal artery embolization for chronic subdural hematoma using Onyx: case series. J Neurointerv Surg. (2020) 12:1214–8. doi: 10.1136/neurintsurg-2019-015493
2. Siddiqui AH, Waqas M, Neumaier J, Zhang JF, Dossani RH, Cappuzzo JM, et al. Radial first or patient first: a case series and meta-analysis of transradial versus transfemoral access for acute ischemic stroke intervention. J Neurointerv Surg. (2021) 13:687–92. doi: 10.1136/neurintsurg-2020-017225
3. Mitchell MD, Hong JA, Lee BY, Umscheid CA, Bartsch SM, Don CW. Systematic review and cost-benefit analysis of radial artery access for coronary angiography and intervention. Circ Cardiovasc Qual Outcomes. (2012) 5:454–62. doi: 10.1161/CIRCOUTCOMES.112.965269
4. Mann JT III, Cubeddu MG, Schneider JE, Arrowood M. Right radial access for PTCA: a prospective study demonstrates reduced complications and hospital charges. J Invasive Cardiol. (1996) 8:40D−4D.
5. Chen SH, Snelling BM, Sur S, Shah SS, McCarthy DJ, Luther E, et al. Transradial versus transfemoral access for anterior circulation mechanical thrombectomy: comparison of technical and clinical outcomes. J Neurointerv Surg. (2019) 11:874–8. doi: 10.1136/neurintsurg-2018-014485
6. Snelling BM, Sur S, Shah SS, Caplan J, Khandelwal P, Yavagal DR, et al. Transradial approach for complex anterior and posterior circulation interventions: technical nuances and feasibility of using current devices. Oper Neurosurg (Hagerstown). (2019) 17:293–302. doi: 10.1093/ons/opy352
7. Tummala RP. Carotid angioplasty and stenting: complication avoidance and management. In:Khatri R, Rodriguez GJ, Raymond J, Qureshi AI, , eds. Complications of Neuroendovascular Procedures and Bailout Techniques. Cambridge: Cambridge University Press (2016), 84–104.
8. Chang FC, Tummala RP, Jahromi BS, Samuelson RM, Siddiqui AH, Levy EI, et al. Use of the 8 French Simmons-2 guide catheter for carotid artery stent placement in patients with difficult aortic arch anatomy. J Neurosurg. (2009) 110:437–41. doi: 10.3171/2008.7.17627
9. Heck D, Jost A, Howard G. Stenting the carotid artery from radial access using a Simmons guide catheter. J Neurointerv Surg. (2022) 14:169–73. doi: 10.1136/neurintsurg-2020-017143
10. Mason PJ, Shah B, Tamis-Holland JE, Bittl JA, Cohen MG, Safirstein J, et al. American Heart Association Interventional Cardiovascular Care Committee of the Council on Clinical Cardiology; Council on Cardiovascular and Stroke Nursing; Council on Peripheral Vascular Disease; and Council on Genomic and Precision Medicine. An Update on Radial Artery Access and Best Practices for Transradial Coronary Angiography and Intervention in Acute Coronary Syndrome: A Scientific Statement From the American Heart Association. Circ Cardiovasc Interv. (2018) 11:e000035. doi: 10.1161/HCV.0000000000000035
11. Brueck M, Bandorski D, Kramer W, Wieczorek M, Höltgen R, Tillmanns H, et al. randomized comparison of transradial versus transfemoral approach for coronary angiography and angioplasty. JACC Cardiovasc Interv. (2009) 2:1047–54. doi: 10.1016/j.jcin.2009.07.016
12. Sinha SK, Jha MJ, Mishra V, Thakur R, Goel A, Kumar A, et al. Radial artery occlusion—incidence, predictors and long-term outcome after TRAnsradial Catheterization: clinico-Doppler ultrasound-based study (RAIL-TRAC study). Acta Cardiol. (2017) 72:318–27. doi: 10.1080/00015385.2017.1305158
13. Khanna O, Sweid A, Mouchtouris N, Shivashankar K, Xu V, Velagapudi L, et al. Radial artery catheterization for neuroendovascular procedures. Stroke. (2019) 50:2587–90. doi: 10.1161/STROKEAHA.119.025811
14. Narsinh KH, Mirza MH, Caton MT Jr, Baker A, Winkler E, Higashida RT, et al. Radial artery access for neuroendovascular procedures: safety review and complications. J Neurointerv Surg. (2021) 13:1132–8. doi: 10.1136/neurintsurg-2021-017325
15. Pancholy SB, Bernat I, Bertrand OF, Patel TM. Prevention of radial artery occlusion after transradial catheterization: the PROPHET-II randomized trial. JACC Cardiovasc Interv. (2016) 9:1992–9. doi: 10.1016/j.jcin.2016.07.020
16. Chen SH, Snelling BM, Shah SS, Sur S, Brunet MC, Starke RM, et al. Transradial approach for flow diversion treatment of cerebral aneurysms: a multicenter study. J Neurointerv Surg. (2019) 11:796–800. doi: 10.1136/neurintsurg-2018-014620
17. Brunet MC, Chen SH, Sur S, McCarthy DJ, Snelling B, Yavagal DR, et al. Distal transradial access in the anatomical snuffbox for diagnostic cerebral angiography. J Neurointerv Surg. (2019) 11:710–3. doi: 10.1136/neurintsurg-2019-014718
18. Brunet MC, Chen SH, Peterson EC. Transradial access for neurointerventions: management of access challenges and complications. J Neurointerv Surg. (2020) 12:82–6. doi: 10.1136/neurintsurg-2019-015145
19. Jo KW, Park SM, Kim SD, Kim SR, Baik MW, Kim YW. Is transradial cerebral angiography feasible and safe? A single center's experience. J Korean Neurosurg Soc. (2010) 47:332–7. doi: 10.3340/jkns.2010.47.5.332
20. Sattur MG, Almallouhi E, Lena JR, Spiotta AM. Illustrated guide to the transradial approach for neuroendovascular surgery: a step-by-step description gleaned from over 500 cases at an early adopter single center. Oper Neurosurg (Hagerstown). (2020) 19:181–9. doi: 10.1093/ons/opaa153
Keywords: reverse angle guide catheter, trans-radial approach, middle meningeal artery, embolization, subdural hematoma
Citation: Krothapalli N, Fayad M, Patel S, Elmashad A, Sussman E, Bruno C, Grande A, Jagadeesan B, Killory B, Alberts M, Kureshi I, Ollenschleger M, Tummala R and Mehta T (2022) Use of reverse angle guide catheter with trans-radial approach in patients undergoing middle meningeal artery embolization. Front. Neurol. 13:990722. doi: 10.3389/fneur.2022.990722
Received: 10 July 2022; Accepted: 10 October 2022;
Published: 25 October 2022.
Edited by:
Osama O. Zaidat, Northeast Ohio Medical University, United StatesReviewed by:
Philipp Taussky, Beth Israel Deaconess Medical Center and Harvard Medical School, United StatesCopyright © 2022 Krothapalli, Fayad, Patel, Elmashad, Sussman, Bruno, Grande, Jagadeesan, Killory, Alberts, Kureshi, Ollenschleger, Tummala and Mehta. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tapan Mehta, dGFwYW4ubWVodGFAaGhjaGVhbHRoLm9yZw==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.