- 1Acupuncture and Tuina School, Chengdu University of Traditional Chinese Medicine, Chengdu, China
- 2Acupuncture and Brain Research Center, Chengdu University of Traditional Chinese Medicine, Chengdu, China
- 3Hospital of Chengdu University of Traditional Chinese Medicine, Chengdu, China
Introduction: Acupuncture is an effective and safe therapy for patients with migraine without aura (MwoA), but only 41–59% of patients show improvement with this treatment. Screening positive responders to acupuncture treatment for MwoA can ensure that healthcare resources can be appropriately targeted to specific patients who would most benefit. The objective of this study is to determine whether the structure and functional activity in certain brain regions can predict analgesia response in patients with MwoA who receive acupuncture treatment.
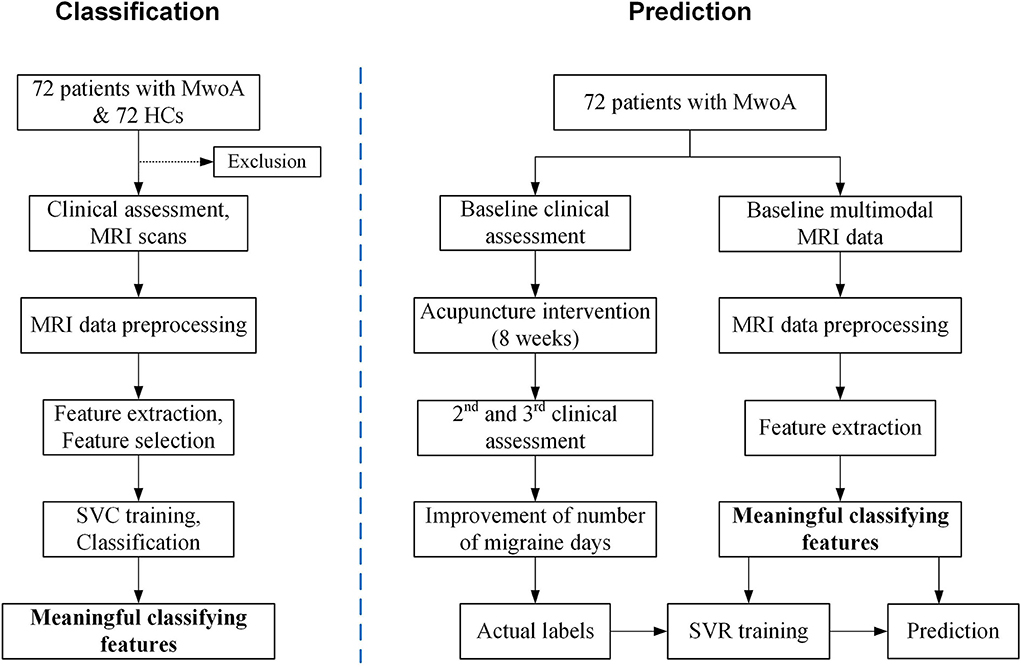
Methods and analysis: A total of 72 patients with MwoA and 72 healthy controls (HCs) will be enrolled in this study. Resting-state structural and functional magnetic resonance imaging (MRI) data will be collected from each participant at baseline. Patients with MwoA will undergo 12 sessions of acupuncture treatment for 8 weeks, twice per week in the first 4 weeks and once per week for the last 4 weeks. The follow-up will be 12 weeks. The number of days with migraine, frequency of migraine attacks, and average visual analog scale scores will be recorded in detail at weeks 0, 4, 8, 12, and 16 and at the end of follow-up (week 20). The positive response rate will be calculated as the proportion of patients with ≥50% reduction in the number of migraine days during follow-up compared with baseline. Machine learning methods will be applied to classify patients with MwoA and HCs and predict patients with response or non-response to acupuncture treatment based on multimodal MRI parameters, such as gray matter volume, regional homogeneity, amplitude of low-frequency fluctuation, fractional anisotropy, and mean diffusivity.
Discussion: This study aims to establish brain structural and functional characteristics that can identify patients with MwoA who will derive analgesia benefits from acupuncture treatment.
Trial registration number: http://www.chictr.org.cn/showproj.aspx?proj=65443, identifier: ChiCTR2100042915.
Introduction
Migraine is a common neurologic disorder characterized by recurrent attacks of disabling headaches that are often accompanied by nausea, vomiting, photophobia, and phonophobia (1). Migraine is the 7th leading cause of time spent disabled worldwide (2), with an estimated 1-year prevalence of 15% in the general population (3). At present, there are no satisfactory treatments for migraine (4–6). Acupuncture, an important component of traditional Chinese medicine, is recommended by the World Health Organization as an alternative and complementary therapy for migraine. Many randomized controlled trials and systematic reviews have demonstrated that acupuncture is safe and cost-effective with comparable efficacy to prophylactic drugs for migraine and can reduce headache intensity, frequency of migraine attacks, and number of migraine days (7–10).
However, only 41–59% of patients with migraine without aura (MwoA) experience symptom improvement with acupuncture treatment (9). This is associated not only with clinical but also with socioeconomic challenges. Therefore, identifying characteristics that can be used to predict migraineurs' response to acupuncture is important to improve the efficacy of the treatment and provide individualized therapy to patients who would most benefit.
Personalized medicine can be achieved by conducting clinical trials, assessing clinical outcomes, analyzing numerous characteristics, and identifying common and unique predictors of treatment outcomes. Previous studies have reported that patients' expectations, educational background, and treatment preferences influence the clinical efficacy of acupuncture for diseases characterized by pain (11–15). However, the questionnaires used in these studies were subjective and qualitative. Recently, with the development of neuroimaging techniques and artificial intelligence, magnetic resonance imaging (MRI) data have been used to predict the clinical efficacy of various interventions, including pharmacologic treatments (16), cognitive behavioral therapy (17), and placebo treatments (18), among others. These studies often provide more objective and reliable predictions than questionnaires.
Patients with MwoA show widespread structural and functional changes in cortical and subcortical brain regions (19, 20). Acupuncture can potentially alleviate brain dysfunction in migraineurs in a specific way (21–24). Some studies have used either structural or functional parameters of different brain regions to predict the efficacy of verum or sham acupuncture treatment for chronic pain diseases (18, 25–27), demonstrating that objective neuroimaging parameters can be used to predict the analgesic efficacy of acupuncture treatment in patients with migraine.
The aim of this study is to identify brain features detected by multimodal MRI that can be used to predict the response to acupuncture treatment. To this end, multimodal MRI indicators from patients with MwoA and healthy controls (HCs) will be analyzed, then an advanced multivariate pattern analysis (MVPA) based on support vector classification (SVC) will be conducted through training, validation, and testing approach to classify migraineurs and HCs. Responders and non-responders of acupuncture treatment for patients with MwoA will be identified by the clinical outcomes obtained before vs. after treatment. The efficacy of acupuncture will be predicted by support vector regression (SVR) based on multimodal MRI data detected at baseline.
Methods and analysis
Study design
This non-randomized clinical trial will enroll 72 patients with MwoA and 72 with HCs. The study will last 24 weeks including a 4-week baseline period; for migraineurs, this will be followed by an 8-week treatment period and a 12-week follow-up period (Table 1). Structural and functional MRI scans will be performed at baseline. Clinical outcomes will be evaluated after treatment and during the follow-up. Figure 1 shows a flow diagram of the study. This protocol is reported in accordance with Consolidated Standards of Reporting Trials and Standards for Reporting Interventions in Clinical Trials of Acupuncture. The protocol was approved by the Institutional Review Board and Ethics Committee of the Hospital of Chengdu University of Traditional Chinese Medicine (approval no. 2020KL-058) and is registered with the Chinese Clinical Trial Registry (registration no. ChiCTR2100042915).
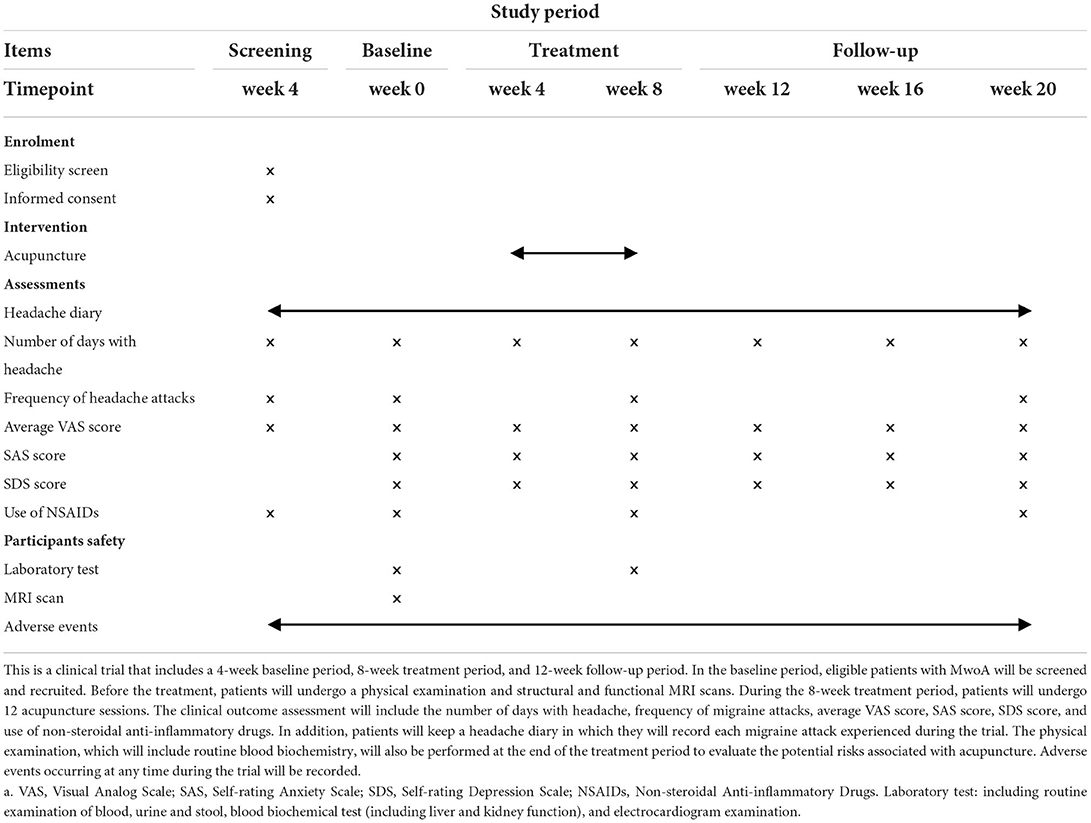
Table 1. Standard protocol items: recommendations for interventional trials (SPIRIT) schedule of the trial.
Participants
Seventy-two patients with MwoA and 72 with HCs will be recruited for this study. Inclusion criteria for patients with MwoA are as follows: (1) aged 18–60 years; (2) right handed; (3) diagnosed with MwoA according to the 2018 International Classification of Headache Disorders (ICHD-3) (1); (4) have a history of migraine for over 6 months; (5) have had migraine attacks 3–15 times per month in the past 3 months; (6) did not take prophylactic headache medicine or receiving acupuncture treatment in the previous 3 months; and (7) signed the informed consent form.
Exclusion criteria were as follows: (1) suffering from psychiatric, neurologic, cardiovascular, respiratory, or renal illness; (2) suffering from any other chronic pain conditions or have a history of head trauma with loss of consciousness; (3) alcohol or drug abusers; (4) are pregnant or lactating; (5) have acupuncture contraindications such as bleeding tendency; and (6) have MRI contraindications such as claustrophobia.
Inclusion criteria for HCs are as follows: (1) aged 18–60 years; (2) right handed; and (3) free of any diseases. HCs will be excluded if they meet the following criteria: (1) have drug or alcohol addiction; (2) have contraindications for MRI; and (3) pregnant or lactating.
Participant recruitment
All MwoA patients and HCs will be recruited as outpatients and inpatients of the Neurology Department of the Hospital of Chengdu University of Traditional Chinese Medicine or from the community through advertising from March 2021 to December 2023.
Blinding
This trial follows the principle of separation of researchers, evaluators, and statistical analysts.
Interventions
HCs will not receive any treatment during the trial. All patients with MwoA will receive the same acupuncture treatment procedure. Baihui (GV20), bilateral Fengchi (GB20), bilateral Touwei (ST8), bilateral Shuaigu (GB8), bilateral Taiyang (EX-HN5), bilateral Hegu (LI4), and bilateral Taichong (LR3) will be targeted by the acupuncture treatment (Figure 2).
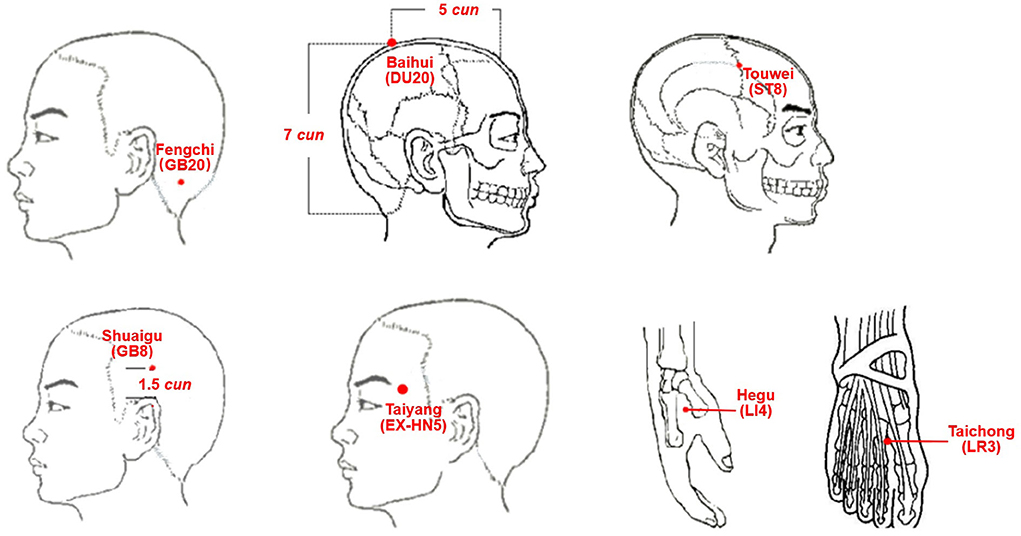
Figure 2. Location of Acupoints. DU20 (Baihui): on the head, five cun directly above the midpoint of the anterior hairline or at the midpoint of the line connecting the apexes of the two auricles. GB20 (Fengchi): on the nape, below the occiput in the depression between the upper portion of the trapezius and sternocleidomastoid. ST8 (Touwei): at the lateral side of the head, within 0.5 cun of the hairline at the corner of the forehead, and 4.5 cun lateral to the median line of the head. GB8 (Shuaigu): on the head above the apex of the auricle and SJ-20 (Jiaosun), within 1.5 cun of the hairline. EX-HN5 (Taiyang): in the region of the temples, in the depression about one finger-width posterior to the midpoint between the lateral end of the eyebrow and outer canthus. LI4 (Hegu): on the dorsum of the hand, between the 1st and 2nd metacarpal bones, at the midpoint of the 2nd metacarpal bone on the radial side. LR3 (Taichong): on the dorsum of the foot, in the depression proximal to the first metatarsal space.
The acupuncture procedure is as follows: after skin disinfection, needles (diameter, 0.25 mm and length, 15 or 40 mm; Hwatuo, Suzhou, China) will be inserted vertically or horizontally into each point. After eliciting deqi (28), the needles will be kept in place for 60 min with manipulation twice for 10–15 s every 20 min.
Patients will undergo 12 sessions of acupuncture treatment for a total of 8 weeks, twice per week in the first 4 weeks and once per week for the last 4 weeks. All acupuncture manipulations will be performed by two trained and licensed acupuncturists.
Medications
In cases of severe pain for migraineurs, ibuprofen will be allowed as rescue medication. The use of medication will be recorded in detail during the trial.
Outcome assessment
Clinical outcomes
Data acquisition will be performed by independent assessors who have received professional training before the start of the study. Clinical outcomes are as follows:
Number of days with migraine and frequency of migraine attacks
Each patient with MwoA will record the number of days with migraine, frequency of migraine attacks, onset time, accompanying symptoms, duration, and methods used to relieve the headache in a headache diary (29, 30) during the trial.
Response rate
Response rate is defined as the proportion of patients with ≥50% reduction in the number of migraine days (31), which will be calculated at the end of treatment (week 8) and end of follow-up (week 20).
Average visual analog scale (VAS)
Average visual analog scale scores for pain will be used to assess changes in headache intensity from the baseline to the end of follow-up (32). Scores will be recorded every 4 weeks to evaluate the severity of headache for the previous 4 weeks.
Evaluation of emotional state and usage of ibuprofen
The emotional state of patients will be assessed using the Zung Self-rating Anxiety Scale (SAS) and Self-rating Depression Scale (SDS) at weeks 0, 4, 8, 12, 16, and 20. The use of ibuprofen during the trial will be recorded every 4 weeks.
Multimodal MRI data acquisition
MRI data will be acquired at week 0 with a 3.0T magnetic resonance scanner (GE Discovery 750; Milwaukee, WI, USA) with a 16-channel phase-array head coil at the MRI Center of the University of Electronic Science and Technology in China. Participants will be asked to lie in the supine position on the examination bed, stay awake, keep their head still, with eyes closed and ears plugged during the scan.
Three-dimensional T1-weighted (3D-T1) imaging will be performed to obtain high-resolution structural images for each participant with a voxel size of 1 mm3, using a spoiled gradient-recalled sequence (repetition time [TR], 6.008 ms; echo time [TE], 1.7 ms; field of view [FOV], 256 × 256 mm2; data matrix: 256 × 256). Resting-state blood oxygenation level-dependent (BOLD) signals will be obtained by gradient-recalled echo planar imaging (31 contiguous slices; slice thickness, 5 mm; TR, 2000 ms; TE, 30 ms; flip angle, 90°; FOV, 240 × 240 mm2; data matrix, 64 × 64; total volumes, 205).
To detect any white matter abnormalities, diffusion tensor imaging (DTI) will be performed with the following parameters: TR, 8500 ms; TE, 84 ms; data matrix, 128 × 128; FOV, 256 × 256 mm2; slice thickness, 2 mm; and 78 continuous axial slices with no gap. Two diffusion-weighted sequences will be acquired using gradient values b = 0 s/mm2 and 1,000 s/mm2 with diffusion-sensitizing gradients applied along with 64 non-linear directions.
Data analysis
Collected data will be managed with printed case report forms (CRFs) and only outcome assessors will have access to these data. The research team will be responsible for data organization. Two data entry checks will be performed. The Ethics Committee of the First Affiliated Hospital of Chengdu University of Traditional Chinese Medicine will be supervising this study with a check-in every 3 months and will make the final decision on whether or when to terminate the trial.
Clinical data analysis
Clinical outcomes will be analyzed using SPSS v22.0 statistical software (IBM, Armonk, NY, USA). The level of statistical significance (two sided) will be set as 0.05 in all analyses. The per-protocol set was the primary population for efficacy analyses.
All continuous variables will be expressed as means with standard deviations. Categorical variables will be described as numbers and percentages. The Kolmogorov–Smirnov test will first be used to test the distribution of continuous variables. For normally distributed data, the paired-sample t-test will be used to evaluate differences within groups; when the data follow a skewed distribution, a non-parametric test will be used.
MRI data preprocessing
BOLD functional MRI data will be preprocessed (i.e., slice timing, motion correction, spatial normalization, detrending, and bandwidth filtering) using MATLAB R2018a (Mathworks, Natick, MA, USA) and SPM12 (SPM12; Wellcome Department of Imaging Neuroscience, London, UK; http://www.fil.ion.ucl.ac.uk/spm/) software. After preprocessing, the amplitude of low-frequency fluctuation (ALFF), fractional ALFF (fALFF), regional homogeneity (ReHo), functional connectivity (FC), and other possible brain functional parameters will be analyzed. The 3D-T1 data will be analyzed by voxel-based morphometry using SPM12 and the CAT12 toolbox in MATLAB (33). DTI data will be preprocessed and analyzed using Functional Software Library v4.1.9 (http://fsl.fmrib.ox.ac.uk/fsl/fslwiki/TBSS/). Fractional anisotropy (FA) index and mean diffusivity (MD) maps will be obtained after head action correction, eddy current correction of DTI images, and tensor model fitting.
Classification and prediction using machine learning methods
Multivariate pattern analysis (34) will be carried out to classify migraineurs and HCs; this will include feature selection, model construction, and performance evaluation. Principal component analysis (35) will be performed and the searchlight algorithm (36) will be used to select features from multimodal parameters of brain regions, such as gray matter volume (GMV), ReHo, ALFF, fALFF, FA, and MD. The linear kernel support vector classification will be used to construct the classification model (37), which will be assessed by leave-one-out cross-validation (LOOCV). Clusters with a minimum accuracy of 70% will be identified as meaningful classifying features.
Patients with MwoA will be divided into the response and non-response groups (defined as ≥50% and <50% reduction, respectively, in the number of migraine days end of treatment compared with baseline). Support vector regression will be performed to discriminate between the response and non-response groups using the abovementioned classifying features of brain regions (ie, GMV, ReHo, ALFF, fALFF, FC, FA, and MD) (38). In addition to neuroimaging features, we may combine multidimensional features such as clinical data to build the model. After constructing the prediction model for patients with MwoA, LOOCV will be performed to evaluate the robustness of the model. A receiver operating characteristic (ROC) curve will be generated, and the area under the curve (AUC, 0–1) will be calculated to assess the power of the model. The performance of the SVR model will be quantified by calculating sensitivity and specificity based on the number of true positives and true negatives.
Patient safety
Routine examination of blood, urine, and stools; blood biochemical testing (including liver and kidney function); and electrocardiography will be performed for each participant before trial enrollment. Adverse events caused by acupuncture, such as bleeding, hematoma, pain, and needle-related fainting, will be recorded in detail in the CRF. Severe adverse events such as death, life-threatening disability, or the need for hospitalization will be reported to the project leader, the research institute, and the ethics committee within 24 h and will be documented in the CRF.
Quality control
Diagnostic, inclusion and exclusion criteria will be strictly applied to screen participants. Patients with MwoA and HCs will be matched in age and education, and patients with average headache VAS scores at baseline >3 will be included. Before the study, the acupuncturists will undergo standardized training and will be required to strictly control the manipulation of the acupuncture needle to minimize interindividual differences. MRI data collection will be carried out according to the operating procedures and experimental design. Communication with patients will be controlled to minimize the influence of the environment and other factors.
Discussion
Previous studies have demonstrated the feasibility and validity of predicting acupuncture treatment outcomes in patients with migraine using machine learning technology based on Fisher's z transformation ALFF (27) and fALFF maps (26). However, multimodal brain imaging features have higher prediction accuracy than any single modal feature (39). Machine learning technologies are useful for extracting key features from large complex data obtained by multimodal neuroimaging. Machine learning approaches such as support vector machines, artificial neural networks, decision trees, and Bayesian networks have been widely used to develop predictive models with effective and accurate decision-making capabilities (26, 27, 34).
Using machine learning methods to screen positive responders to acupuncture treatment for migraine is a novel approach for improving clinical outcomes and identifying specific patients who would most benefit. This study can help to better understand the brain structural and functional features in patients with MwoA that are critical for the analgesic effect of acupuncture treatment.
Limitation
Acupuncture is an effective evidence-based treatment for migraine. The main strength of this study is identifying patients with migraine who will respond positively to acupuncture treatment based on objective multimodal MRI data. However, there is no sham acupuncture group in this trial because constructing prediction models of sham treatment is of limited value for improving the clinical efficacy of acupuncture.
Trial status
This trial was registered with the Chinese Clinical Trial Registry (http://www.chictr.org.cn) on January 31, 2021 (registration no. ChiCTR2100042915; protocol version no. 2.0). Patient recruitment began on March 1, 2021, and 15 patients with MwoA have been recruited to date.
Ethics statement
The studies involving human participants were reviewed and approved by Institutional Review Boards and Ethics Committees of the Hospital of Chengdu University of Traditional Chinese Medicine. The participants provided their written informed consent to participate in this study.
Author contributions
ZL and FZ conceived the study. ZL, FL, SC, and XZ initiated the study design. SC, XZ, and NJ helped with its implementation. SC, XZ, and HZ drafted the manuscript. JZ, XL, YF, and XH revised the manuscript. All authors contributed to the refinement of the study protocol and approved the final manuscript.
Funding
This trial was financially supported by the National Natural Science Foundation of China (nos. 81973958, 82225050, and 82205288), Innovation Team and Talents Cultivation Program of National Administration of Traditional Chinese Medicine (no. ZYYCXTD-D-202003), and China Postdoctoral Science Foundation (nos. 2017M610593, 2018T110954, and 20190037). The sponsor plays no part in study design, collection, or management and will not participate in analysis, interpretation of data, writing of reports, and the decision to submit reports for publication.
Acknowledgments
The authors thank Zhaoxuan He, Yuke Teng, Xiaohui Dong, Lei Lan, and Jianfu Li for their help in the consultation of this neuroimaging trial protocol.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition. Cephalalgia. (2018) 38:1–211. doi: 10.1177/0333102417738202
2. GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. (2016) 388:1545–602. doi: 10.1016/S0140-6736(16)31678-6
3. GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national burden of migraine and tension-type headache, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. (2018) 17:954–76. doi: 10.1016/S1474-4422(18)30322-3
5. Tfelt-Hansen P, Pascual J, Ramadan N, Dahlöf C, D'Amico D, Diener HC, et al. Guidelines for controlled trials of drugs in migraine: third edition. Cephalalgia. (2012) 32:6–38. doi: 10.1177/0333102411417901
6. Silberstein SD, Holland S, Freitag F, Dodick DW, Argoff C, Ashman E. Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. (2012) 78:1337–45. doi: 10.1212/WNL.0b013e3182535d20
7. Zhao L, Chen J, Li Y, Sun X, Chang X, Zheng H, et al. The long-term effect of acupuncture for migraine prophylaxis: a randomized clinical trial. JAMA Intern Med. (2017) 177:508–15. doi: 10.1001/jamainternmed.2016.9378
8. Xu S, Yu L, Luo X, Wang M, Chen G, Zhang Q, et al. Manual acupuncture versus sham acupuncture and usual care for prophylaxis of episodic migraine without aura: multicentre, randomised clinical trial. BMJ. (2020) 368:m697. doi: 10.1136/bmj.m697
9. Linde K, Allais G, Brinkhaus B, Fei Y, Mehring M, Vertosick EA, et al. Acupuncture for the prevention of episodic migraine. Cochrane Database Syst Rev. (2016) 2016:Cd001218. doi: 10.1002/14651858.CD001218.pub3
10. Sun XL, Sun SB, Chen SF, Gao YB. Observation on the effect difference in migraine treated with the combination of acupuncture and blood-letting therapy and medication with carbamazepine. World J Acupunct Moxibustion. (2021) 31:16–21. Available online at: https://kns.cnki.net/kcms/detail/11.2892.R.20201029.0939.002.html
11. Sherman KJ, Cherkin DC, Ichikawa L, Avins AL, Delaney K, Barlow WE, et al. Treatment expectations and preferences as predictors of outcome of acupuncture for chronic back pain. Spine. (2010) 35:1471–7. doi: 10.1097/BRS.0b013e3181c2a8d3
12. Witt CM, Schützler L, Lüdtke R, Wegscheider K, Willich SN. Patient characteristics and variation in treatment outcomes: which patients benefit most from acupuncture for chronic pain? Clin J Pain. (2011) 27:550–5. doi: 10.1097/AJP.0b013e31820dfbf5
13. Martins F, Kaster T, Schützler L, Witt CM. Factors influencing further acupuncture usage and a more positive outcome in patients with osteoarthritis of the knee and the hip: a 3-year follow-up of a randomized pragmatic trial. Clin J Pain. (2014) 30:953–9. doi: 10.1097/AJP.0000000000000062
14. Linde K, Witt CM, Streng A, Weidenhammer W, Wagenpfeil S, Brinkhaus B, et al. The impact of patient expectations on outcomes in four randomized controlled trials of acupuncture in patients with chronic pain. Pain. (2007) 128:264–71. doi: 10.1016/j.pain.2006.12.006
15. Fu CH, Steiner H, Costafreda SG. Predictive neural biomarkers of clinical response in depression: a meta-analysis of functional and structural neuroimaging studies of pharmacological and psychological therapies. Neurobiol Dis. (2013) 52:75–83. doi: 10.1016/j.nbd.2012.05.008
16. Ichesco E, Peltier SJ, Mawla I, Harper DE, Pauer L, Harte SE, et al. Prediction of differential pharmacologic response in chronic pain using functional neuroimaging biomarkers and support vector machine algorithm - An exploratory study. Arthritis Rheumatol. (2021) 73:2127–37 doi: 10.1002/art.41781
17. Wang ZL, Potenza MN, Song KR, Fang XY, Liu L, Ma SS, et al. Neural classification of internet gaming disorder and prediction of treatment response using a cue-reactivity fMRI task in young men. J Psychiatr Res. (2020) 145:309–16. doi: 10.1016/j.jpsychires.2020.11.014
18. Liu J, Mu J, Chen T, Zhang M, Tian J. White matter tract microstructure of the mPFC-amygdala predicts interindividual differences in placebo response related to treatment in migraine patients. Hum Brain Mapp. (2019) 40:284–92. doi: 10.1002/hbm.24372
19. Li Z, Zhou J, Lan L, Cheng S, Sun R, Gong Q, et al. Concurrent brain structural and functional alterations in patients with migraine without aura: an fMRI study. J Headache Pain. (2020) 21:141. doi: 10.1186/s10194-020-01203-5
20. Tu Y, Fu Z, Zeng F, Maleki N, Lan L, Li Z, et al. Abnormal thalamocortical network dynamics in migraine. Neurology. (2019) 92:e2706–e16. doi: 10.1212/WNL.0000000000007607
21. Li Z, Liu M, Lan L, Zeng F, Makris N, Liang Y, et al. Altered periaqueductal gray resting state functional connectivity in migraine and the modulation effect of treatment. Sci Rep. (2016) 6:20298. doi: 10.1038/srep20298
22. Li Z, Lan L, Zeng F, Makris N, Hwang J, Guo T, et al. The altered right frontoparietal network functional connectivity in migraine and the modulation effect of treatment. Cephalalgia. (2017) 37:161–76. doi: 10.1177/0333102416641665
23. Li Z, Zeng F, Yin T, Lan L, Makris N, Jorgenson K, et al. Acupuncture modulates the abnormal brainstem activity in migraine without aura patients. NeuroImage Clin. (2017) 15:367–75. doi: 10.1016/j.nicl.2017.05.013
24. Xu ST, Zhao JJ, Zhong YB, Shan CL. Status quo of brain mechanism research of acupuncture in rehabilitation of chronic pain. World J Acupunct Moxibustion. (2020) 30:65–68. Available online at: https://kns.cnki.net/kcms/detail/detail.aspx?FileName=SJJA202001013&DbName=CJFQ2020
25. Liu J, Mu J, Liu Q, Dun W, Zhang M, Tian J. Brain structural properties predict psychologically mediated hypoalgesia in an 8-week sham acupuncture treatment for migraine. Hum Brain Mapp. (2017) 38:4386–97. doi: 10.1002/hbm.23667
26. Li Z, Zhou J, Cheng S, Lan L, Sun R, Liu M, et al. Cerebral fractional amplitude of low-frequency fluctuations may predict headache intensity improvement following acupuncture treatment in migraine patients. J Tradit Chin Med. (2020) 40:1041–51.
27. Yin T, Sun G, Tian Z, Liu M, Gao Y, Dong M, et al. The spontaneous activity pattern of the middle occipital gyrus predicts the clinical efficacy of acupuncture treatment for migraine without aura. Front Neurol. (2020) 11:588207. doi: 10.3389/fneur.2020.588207
28. Yang XY, Shi GX Li QQ, Zhang ZH, Xu Q, Liu CZ. Characterization of deqi sensation and acupuncture effect. Evid Based Complement Alternat Med. (2013) 2013:319734. doi: 10.1155/2013/319734
29. Linde K, Streng A, Jürgens S, Hoppe A, Brinkhaus B, Witt C, et al. Acupuncture for patients with migraine: a randomized controlled trial. Jama. (2005) 293:2118–25. doi: 10.1001/jama.293.17.2118
30. Chen J, Zhao L, Zheng H, Li Y, Yang M, Chang X, et al. Evaluating the prophylaxis and long-term effectiveness of acupuncture for migraine without aura: study protocol for a randomized controlled trial. Trials. (2013) 14:361. doi: 10.1186/1745-6215-14-361
31. Diener HC, Kronfeld K, Boewing G, Lungenhausen M, Maier C, Molsberger A, et al. Efficacy of acupuncture for the prophylaxis of migraine: a multicentre randomised controlled clinical trial. Lancet Neurol. (2006) 5:310–6. doi: 10.1016/S1474-4422(06)70382-9
32. Fillingim RB, Loeser JD, Baron R, Edwards RR. Assessment of chronic pain: domains, methods, and mechanisms. J Pain. (2016) 17:T10–20. doi: 10.1016/j.jpain.2015.08.010
33. Ashburner J, Friston KJ. Voxel-based morphometry–the methods. Neuroimage. (2000) 11:805–21. doi: 10.1006/nimg.2000.0582
34. Haxby JV. Multivariate pattern analysis of fMRI: the early beginnings. Neuroimage. (2012) 62:852–5. doi: 10.1016/j.neuroimage.2012.03.016
35. Zeng P, Huang J, Wu S, Qian C, Chen F, Sun W, et al. Characterizing the structural pattern predicting medication response in herpes zoster patients using multivoxel pattern analysis. Front Neurosci. (2019) 13:534. doi: 10.3389/fnins.2019.00534
36. Kriegeskorte N, Goebel R, Bandettini P. Information-based functional brain mapping. Proc Natl Acad Sci U S A. (2006) 103:3863–8. doi: 10.1073/pnas.0600244103
37. Chang CC, Lin CJ. LIBSVM: a library for support vector machines. ACM Trans Intell Syst Technol. (2011) 2:1-27. doi: 10.1145/1961189.1961199
38. Huppertz HJ, Möller L, Südmeyer M, Hilker R, Hattingen E, Egger K, et al. Differentiation of neurodegenerative parkinsonian syndromes by volumetric magnetic resonance imaging analysis and support vector machine classification. J Mov Disord. (2016) 31:1506–17. doi: 10.1002/mds.26715
Keywords: acupuncture, migraine without aura, efficacy prediction, magnetic resonance imaging, resting state
Citation: Cheng S, Zhang X, Zheng H, Jiang N, Zhou J, Li X, Fang Y, Huang X, Liang J, Yin T, Liang F, Zeng F and Li Z (2022) Efficacy prediction of acupuncture treatment for migraine without aura based on multimodal MRI: A study protocol. Front. Neurol. 13:953921. doi: 10.3389/fneur.2022.953921
Received: 26 May 2022; Accepted: 14 September 2022;
Published: 10 October 2022.
Edited by:
Raquel Gil-Gouveia, Hospital da Luz Lisboa, PortugalReviewed by:
Yi Zhang, Xidian University, ChinaTiansong Yang, Heilongjiang University of Chinese Medicine, China
Jia Liu, China Academy of Chinese Medical Sciences, China
Copyright © 2022 Cheng, Zhang, Zheng, Jiang, Zhou, Li, Fang, Huang, Liang, Yin, Liang, Zeng and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fang Zeng, emVuZ19mYW5nQDEyNi5jb20=; Zhengjie Li, bHpqYmVuamFtaW5AMTYzLmNvbQ==
†These authors have contributed equally to this work
 Shirui Cheng
Shirui Cheng Xinyue Zhang
Xinyue Zhang Huabin Zheng
Huabin Zheng Nannan Jiang
Nannan Jiang Jun Zhou
Jun Zhou Xinling Li1,2
Xinling Li1,2 Jingtao Liang
Jingtao Liang Tao Yin
Tao Yin Fanrong Liang
Fanrong Liang Fang Zeng
Fang Zeng Zhengjie Li
Zhengjie Li