
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Neurol. , 13 September 2022
Sec. Neurorehabilitation
Volume 13 - 2022 | https://doi.org/10.3389/fneur.2022.933679
Background: Urinary incontinence (UI) is a common disease in the middle-aged and elderly women, and physical therapy has gradually become the mainstream treatment of UI. We conducted a meta-analysis to evaluate the efficacy of intravaginal electrical stimulation (IVES) in the treatment of UI.
Methods: From January 2006 to December 2021, we finally selected nine randomized controlled trials (RCTs) including 657 participants from PubMed, EMBASE, and Cochrane databases to evaluate the efficacy of IVES in the treatment of female UI. Continuous data were represented by mean difference and 95% CI, while dichotomous data were represented by odds ratio and 95% CI. All the data were analyzed by the Review Manager Version 5.4.
Results: Compared with the control group, there were significant improvements in urine pad test (P = 0.01), urinary incontinence frequency (P = 0.04), some indicators in the incontinence quality of life questionnaire and King's health questionnaires, and subjective feeling of cure (P = 0.009) in the IVES group. However, in other indicators reflecting UI, there was no significant difference between the IVES group and the control group. In addition, subgroup analysis showed that IVES and IVES combined with training could significantly reduce the weight of the urine pad, which reflected the improvement of urine leakage.
Conclusion: This meta-analysis proved that IVES can partially improve the symptoms of female patients with UI compared with the control group. However, it still needs to be further evaluated through more high-quality research in the future.
Urinary incontinence (UI) is a common disease, which is defined as the phenomenon of transurethral urine leakage that is not controlled by will by the International Conference Society (ICS) (1). Women are more likely to suffer from UI than men due to age growth, improper postpartum care, congenital urogenital abnormalities, and previous gynecological surgery (2–5). Although UI will not endanger the life of patients, long-term suffering from UI will seriously affect the physical and mental health, and the quality of life of patients. Patients will deliberately avoid going out, reduce social activities, and gradually become disconnected from society. Therefore, urinary incontinence is also known as “social cancer” (6–8).
Physical therapy is usually used as the first-line therapy of UI treatment, including pelvic floor muscle training, bladder training, intravaginal electrical stimulation (IVES), and other methods (9, 10). Intravaginal electrical stimulation (IVES) can inhibit the activity of the reflex parasympathetic nerve and reduce the involuntary contraction of the bladder detrusor (11, 12). Other studies have also shown that IVES stimulate pelvic floor muscle contraction and relaxation directly through the sensors in the vagina, increasing pelvic floor muscle strength, and effectively improving UI symptoms (13). However, due to embarrassment, discomfort, and other shortcomings, its clinical use rate is not high now (14).
We conducted a meta-analysis of the retrieved randomized controlled trials (RCTs) to evaluate the efficacy of IVES in the treatment of female urinary incontinence.
We searched related literature from PubMed, Embase, and Cochrane databases according to the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) (15), and the retrieval time was limited from January 2006 to December 2021. We formulated the retrieval strategy according to the PICOS (populations, interventions, comparators, outcomes, and study designs) principle. The keywords searched are as follows: electrical stimulation, intravaginal electrical stimulation, female, women, incontinence, urinary incontinence, RCT, and randomized controlled trials. There were no restrictions on the language of the article when searching the literature. The two authors searched according to the search strategy, then compared the search results, respectively. All the articles retrieved were read independently by two researchers. In case of dispute, a third researcher would be invited to read and provide suggestions to reach an agreement. In addition, we would also download and read some references to related articles if necessary.
All the articles included are supposed to meet the criteria as follows: (1) the articles describing IVES in treating women's urinary incontinence; (2) every article's content should be obtained and all the data are true and effective; (3) the experimental method is a randomized controlled trial. If the same research is published repeatedly in different journals or at different times, we would select the latest research literature for this meta-analysis. In addition, if an article type is a case report, review article, meeting report, or abstract, this article would be excluded. The relevant details of inclusion criteria and exclusion criteria are shown in Table 1.
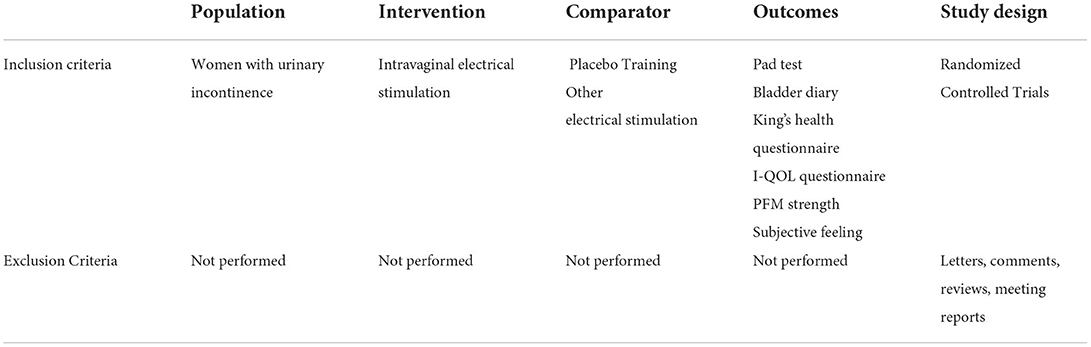
Table 1. Search strategy according to populations, interventions, comparators, outcomes, and study designs (PICOS).
We evaluated all included randomized controlled trials studies according to the guideline of the Cochrane Handbook for Systematic Reviews of Interventions v5.10. At the same time, each article was classified according to the following three quality evaluation criteria: (+) low risk of bias, (?) moderate risk of bias or insufficient evidence to judge the degree of bias, and (–) high risk of bias. All the authors participated independently in the risk assessment of each RCT. After the evaluation was completed, everyone summarized and discussed until all the evaluation results were consistent.
Two authors independently collected data from the included articles and tabulated them. The extracted data include (a) first author's name, (b) published year, (c) country, (d) sample size of experimental group and control group, (e) setup of experimental group and control group, (f) methodology, and (g) outcome indicators. This study did not need ethical approval since it was a retrospective analysis of published research.
The data in this study were analyzed by Review Manager Version 5.4.0 (Cochrane Collaboration, Oxford, UK). We used fixed or random effect models to evaluate the indicators. The continuous data type was expressed by mean difference (MD) and 95% confidence interval (CI), while the dichotomous data type was expressed by odds ratio (OR) and 95% CI. In addition, we tested the heterogeneity by Q-value test or I2 test. If the P < 0.05 in the Q-value statistic test or I2 was greater than 50% in the I2 test, the study was considered to be heterogeneous and would be analyzed by the random effect model. Otherwise, the study would be analyzed by a fixed effect model because of homogeneity. In the results section, the data with P-value < 0.05 were considered statistically significant.
We searched and finally found 70 articles according to the aforementioned search strategy and another 49 articles were deleted when we first screened the titles and abstracts. An additional seven articles, of the remaining 21 articles were excluded because they lacked relevant data. Five duplicate articles were excluded from the remaining 14 articles, and at last, nine randomized controlled trials were included in our study to evaluate the efficacy of IVES in improving UI symptoms (16–24). The process of study selection is presented in Figure 1, and the characteristics of these studies are shown in Table 2.
All included studies in this meta-analysis were randomized controlled trials. The summary and graph of bias risk are shown in Figures 2, 3.
The urine pad test of seven randomized controlled trials involving 491 patients (266 in the vaginal electrical stimulation group and 225 in the control group) showed that the weight (unit: g) of the urine pad in the vaginal electrical stimulation group decreased significantly (MD = −6.34; 95% CI = [−11.24, −1.45]; P = 0.01) compared with the control group and the difference was statistically significant (Figure 4). The data involved in the analysis adopts the change value or final value before and after processing.
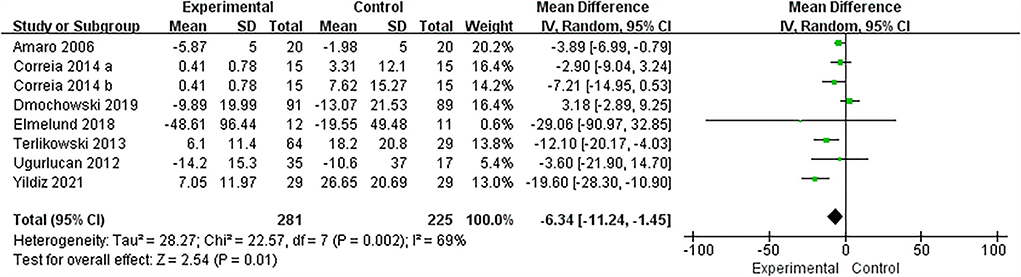
Figure 4. Forest plots showing the improvement of pad test by IVES treatment. SD, standard deviation; IV, inverse variance; CI, confidence interval; df, degrees of freedom.
Overall, six of the nine articles provided data on changes in the average number of episodes of urinary incontinence per 24 h, and the meta-analysis used a random effect model. The results showed that compared with the control group, the average number of episodes of urinary incontinence in the vaginal electrical stimulation group was significantly reduced (MD = −1.01, 95% CI = [−1.99, −0.03], P = 0.04; Figure 5A).

Figure 5. Forest plots showing the changes in bladder diary after IVES treatment. (A) Incontinence episodes; (B) Nocturia; (C) Daytime micturition; (D) Number of urine pads. SD, standard deviation; IV, inverse variance; CI, confidence interval; df, degrees of freedom.
Nocturia episodes refer to the number of times a person gets up and urinates at night after falling asleep. Four RCTs comprising 245 patients (148 and 97 in the experimental and control groups, respectively) described the change in the number of nocturia episodes per night. The results reported that there was no significant difference in the efficacy of IVES on nocturia episodes compared with the control group (MD = −0.68, 95% CI = [−1.49, 0.12], P = 0.10; Figure 5B).
Daytime micturition episodes refer to the number times a person urinates during the daytime, and the normal range is usually from four to six times. Among the nine included studies, six articles provided the mean number of daytime micturition data. The results identified that there was no significant difference in reducing the number of nocturnal urination in the treatment group compared with the control group (MD = −0.84, 95% CI = [−1.92, 0.24], P = 0.13; Figure 5C).
Changes in the number of urine pads used per day were also reported in randomized controlled trials. Four randomized controlled trials involving 373 patients (204 in the experimental group and 169 in the control group) described that compared with the control group, the results of the experimental group were not statistically significant (MD = −0.89, 95% CI = [−2.10, 0.31], P = 0.15; Figure 5D).
The King's health questionnaire is usually used as a quality-of-life evaluation index for female patients with urinary incontinence because it is easy to manage and increases the objectivity of patients' descriptions of subjective symptoms. Each item of this questionnaire is rated from 0 (best) to 100 (worst) (25). We found that a total of two RCTs mentioned the relevant indicators in the King's health questionnaire and the forest plot results are shown as follows. In the part of General health perception, the scores of the experimental group were significantly decreased compared with the control group, and the difference was statistically significant (MD = −9.45, 95% CI = [−18.14, −0.77], P = 0.03). There was no significant difference between the experimental group and the control group in the effects of incontinence impact, role limitations and physical limitations (Incontinence impact: MD = −23.03, 95% CI = [−55.55, 9.48], P = 0.17; role limitations: MD = −10.34, 95% CI = [−33.72, 13.04], P = 0.39; physical limitations: MD = −15.21, 95% CI = [−42.04, 11.61], P = 0.27). Besides, in the social limitations, personal relationship and emotions part, two RCTs identified that the improvement of the experimental group was significantly better than that of the control group (social limitations: MD = −13.91, 95% CI = [−26.16, −1.66], P = 0.03; personal relationship: MD = −11.69, 95% CI = [−20.41, −2.97], P = 0.009; emotions: MD = −29.03, 95% CI = [−52.16, −5.90], P = 0.01). In two studies comprising 97 participants (50 and 47 in the treatment and control group, respectively) reported sleep/energy and severity of urinary symptoms with an outcome respectively of MD = 0.68, 95% CI = [−17.42, 18.78], P = 0.94, and MD = −24.77, 95% CI = [−57.09, 7.55], P = 0.13. Unfortunately, the difference in these two results was not statistically significant. The forest plots of all relevant King's health questionnaire results are shown in Figure 6.

Figure 6. Forest plots showing the changes of various indexes in King's health questionnaire after IVES treatment. SD, standard deviation; IV, inverse variance; CI, confidence interval; df, degrees of freedom.
Incontinence quality of life (I-QOL) questionnaire score is another quality-of-life assessment questionnaire for patients with urinary incontinence. Each question in the questionnaire reflects whether urinary incontinence is causing trouble, and the quantitative score ranges from one (completely) to five (never) (26). This questionnaire was mentioned in three studies and the result identified that the changes in the experimental group were not statistically significant compared with the control group (MD = 10.70, 95% CI = [−10.30, 31.70], P = 0.32, Figure 7).
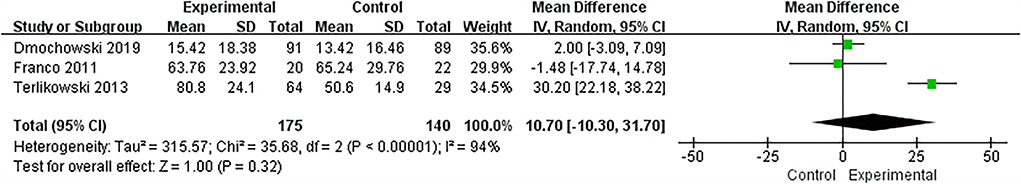
Figure 7. Forest plots showing the changes in I-QOL questionnaire scores after IVES treatment. SD, standard deviation; IV, inverse variance; CI, confidence interval; df, degrees of freedom.
Pelvic floor muscle (PFM) strength measurement is another index to evaluate the outcome of urinary incontinence and a total of two studies mentioned this indicator. The results showed that compared with the control group, the IVES treatment could not significantly improve the pelvic floor muscle strength of participants, and the difference was not statistically significant (MD = 0.4, 95% CI = [−0.04, 0.84], P = 0.08, Figure 8).
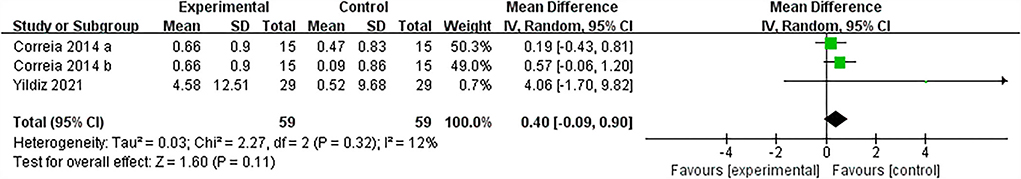
Figure 8. Forest plots showing the changes in PFM strength after IVES treatment. SD, standard deviation; IV, inverse variance; CI, confidence interval; df, degrees of freedom.
The subjective feeling after treatment is usually used as a parameter to evaluate the effect of IVES. A total of three studies involving 230 participants (104 and 126 in the IVES and control groups, respectively) reported this data. The heterogeneity was high in the two parts of data in which the participants' responses were cure or no change. However, after deleting one of the studies (20), the heterogeneity was significantly reduced, so only the remaining two RCTs were analyzed. The results identified that the “cure” response rate of the IVES group was higher than the control group and the results were statistically significant (OR = 3.90, 95% CI = [1.41, 10.79], P = 0.009), while the “better than before” or “no change” response rate of the experimental group was not statistically significant compared with the control group (Better than before: OR = 1.19, 95% CI = [0.40, 3.55], P = 0.75; No change: OR = 0.25, 95% CI = [0.04, 1.53], P = 0.13; Figure 9).
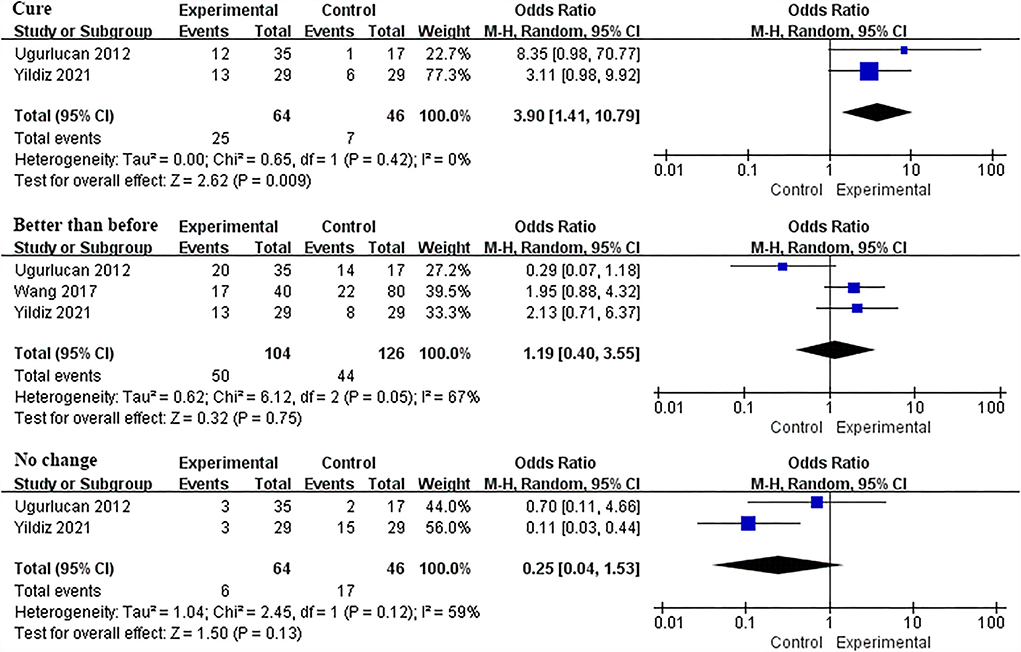
Figure 9. Forest plots showing the changes in patients' subjective feelings after IVES treatment. M–H, Mantel–Haenszel; CI, confidence interval; df, degrees of freedom.
According to different experimental designs, we divided the included RCTs into three categories: IVES vs. sham group, IVES united training vs. training, and IVES vs. other electrical stimulation. At the same time, we performed a subgroup analysis of pad test, frequency of urinary incontinence, and the number of daily micturition. Through data analysis, it was found that IVES and the IVES united training can significantly reduce the weight of urine pad compared with the sham group and simple training group (IVES VS sham group: MD = −6.58, 95% CI = [−11.34, −1.83], P = 0.007; IVES united training vs. training: MD = −19.78, 95% CI = [−28.40, −11.17], P < 0.00001) while there was no significant difference between the IVES and other electrical stimulation groups (IVES vs. sham group: MD = −0.04, 95% CI = [−4.34, 4.27], P = 0.99; Figure 10). In the subgroup analysis of the urinary incontinence frequency, compared with the sham group, IVES can reduce the frequency of urinary incontinence, while IVES is not significantly improved compared with other electrical stimulation group or bladder training group. In addition, there was also no statistically significant difference among the three subgroups in the subgroup analysis of the number of daily micturition. The detailed results are shown in the Supplementary Figures S1, S2.
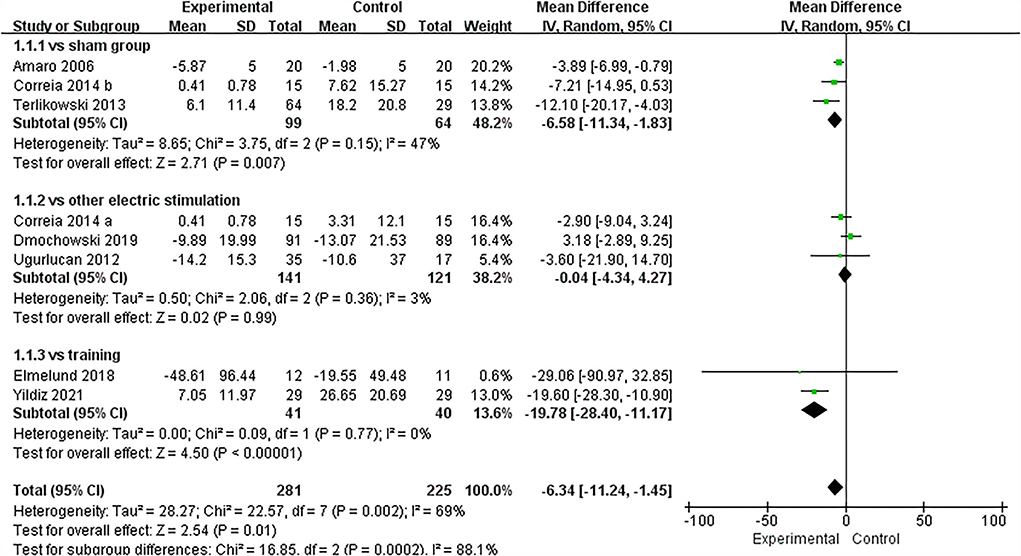
Figure 10. Forest plots showing the improvement of pad test in each subgroup. SD, standard deviation; IV, inverse variance; CI, confidence interval; df, degrees of freedom.
We conducted a systematic review and meta-analysis of nine RCT studies, including 657 participants, to evaluate the efficacy of IVES in the treatment of female urinary incontinence. The results identified that after treatment with IVES, the urine pad test and urinary incontinence frequency of patients were improved to a certain extent. In addition, the ratio of cure in the subjective feeling of patients in the experimental group was also better than that in the control group. Some indicators in the King's health questionnaire and I-QOL questionnaire had also improved, but there were still some other indicators' changes in the questionnaire that had no statistical significance. Besides, the improvement of PFM strength after the IVES treatment was also not satisfactory. The above results suggested that IVES may partially improve the symptoms of patients with urinary incontinence.
The clinical treatment methods for female urinary incontinence mainly include drug therapy, physical therapy, and surgical treatment (27–30). Among them, physical therapy has become the preferred treatment for many patients with urinary incontinence because of its relatively simple treatment, low medical cost, and almost no side effects and adverse reactions (31). Physical therapy mainly includes pelvic floor muscle training, bladder training, and nerve regulation (32–34). Electrical stimulation is a way of nerve regulation and it is to stimulate the afferent nerve, efferent nerve, or effector innervating the bladder by outputting appropriate current through the electrical stimulation device, so as to reduce the sensitivity of the bladder in patients and improve the state of overactive bladder (35, 36). At present, the common clinical electrical stimulation methods are to stimulate the common peroneal nerve, sacral nerve, and posterior tibial nerve in vitro, but there are few reports on the treatment of urinary incontinence by transvaginal electrical stimulation of the pudendal nerve.
Urgent urinary incontinence (UUI) and stress urinary incontinence (SUI) are two common types of UI. UUI refers to the behavior of bladder urinating without conscious control, which is usually secondary to cystitis, neurogenic bladder, and severe bladder outlet obstruction. SUI refers to the involuntary outflow of urine when the intra-abdominal pressure increases suddenly (cough, sneeze, laugh, exercise, etc.). SUI is common in women with multiple deliveries or postmenopausal women, which is caused by the weakening or loss of tension in the anterior vaginal wall and pelvic floor supporting tissue. Among the nine included studies, three studies mentioned the impact of IVES on UUI (Ugurlucan, Yildiz, Wang), and another three articles mentioned the impact of IVES on SUI (Correia, Terlikowski, Dmochowski). Ugurlucan's and Yildiz's research showed that IVES can significantly reduce the frequency of urinary incontinence and urine pad weight in UUI patients, and the subjective cure rate and satisfaction were also significantly improved. The research results of Correia, Terlikowski, and Dmochowski showed that in addition to improving the symptoms of urinary incontinence and subjective cure rate of patients, the improvement of IVES in patients with SUI was also reflected in PFM contraction intensity and pressure.
Our meta-analysis results found that IVES could improve a portion of symptoms of UI patients, which is consistent with the results of Correia et al. (16) and Franco et al. (17). Amaro et al. (18) and Elmelund et al. (24) found through their research that the control group and the experimental group achieved the same treatment effect, so they questioned the effectiveness of IVES, which may be caused by too few follow-up people (Amaro: 40; Elmelund: 27). Dmochowski et al. (21) and Wang (20) believed that the effect of the control group was better than that of the IVES group, which may be due to the fact that the control group was not treated with sham therapy but with other electrical stimulation methods. In addition, the research of Yildiz, Terlikowski, and Ugurlucan believed that although IVES had brought a certain degree of improvement and relief to patients' quality-of-life and symptoms, more research and longer follow-up time were still needed to evaluate the effect of IVES.
As a matter of interest, the subgroup analysis results showed that IVES and IVES united training could significantly reduce the weight of urine pads compared with the sham group and the simple training group. While compared with other electrical stimulation methods, the improvement of IVES was not obvious, and the difference was not statistically significant. These results suggested that we can consider using IVES combined training to treat female urinary incontinence. In addition, we also performed a subgroup analysis on the frequency of urinary incontinence and daily micturition, but we did not get statistically significant results.
In the process of data analysis, we found that some studies only provide sample median and interquartile range (IQR). Therefore, we, at last, used the formula to convert them into mean data and standard deviation to facilitate our statistics and comparison (37, 38).
This is the first meta-analysis to study the efficacy of IVES in the treatment of female urinary incontinence. Although the intention is novel and the included studies are high-quality randomized controlled trials, there are still some limitations. First, there are too many indicators to evaluate urinary incontinence, and the indicators used by different RCTs are not unified, so some indicators lack sufficient experimental data to support our analysis. Second, the application of IVES is not popular, so there are few relevant studies, which is not conducive to our subgroup analysis. Third, some indicators in the research are displayed through the median and interquartile spacing, and we must use the formula to convert the original data into mean and standard deviation to facilitate our final statistical analysis. This conversion process may bring some errors, which affect the final result. At last, our study did not report other indicators to evaluate urinary incontinence, such as urethral pressure, maximum bladder volume, and other questionnaires reflecting the quality of life of urinary incontinence, because only one randomized controlled trial reported these indicators, which is not conducive to our analysis of the data. In conclusion, we may need more unified indicators, more studies and results to help us evaluate the effect of IVES in the treatment of female urinary incontinence.
This meta-analysis of nine randomized controlled trials showed that IVES could partially improve some indicators reflecting UI, such as lightening the quality of urinary pad in urinary pad test, reducing the frequency of urinary incontinence, increasing the proportion of cure in subjective evaluation, etc. However, there were still some indicators that did not improve significantly. In general, IVES is gradually becoming a popular choice for the treatment of female UI because of its effectiveness and convenience, but more experimental data are still needed to support our conclusion.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
HY, XZ, FS, GT, JW, and ZZ study concept and design. HY, XZ, FS, JW, and ZZ analysis and interpretation of data and preparation of the manuscript. JW and ZZ critical revision of the manuscript. All authors contributed to the article and approved the submitted version.
This work was supported by grants from the National Nature Science Foundation of China (Nos. 81870525 and 81572835) and Taishan Scholars Program of Shandong Province (No. tsqn201909199).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2022.933679/full#supplementary-material
Supplementary Figure S1. Forest plots showing the improvement of urinary incontinence frequency in each subgroup. SD, standard deviation; IV, inverse variance; CI, confidence interval; df, degrees of freedom.
Supplementary Figure S2. Forest plots showing the improvement of the number of daily micturition in each subgroup. SD, standard deviation; IV, inverse variance; CI, confidence interval; df, degrees of freedom.
1. Rogers RG, Pauls RN, Thakar R, Morin M, Kuhn A, Petri E, et al. An international Urogynecological association (IUGA)/international continence society (ICS) joint report on the terminology for the assessment of sexual health of women with pelvic floor dysfunction. Int Urogynecol J. (2018) 29:647–66. doi: 10.1007/s00192-018-3603-9
2. Baek JM, Song JY, Lee SJ, Park EK, Jeung IC, Kim CJ, et al. Caffeine Intake Is Associated with Urinary Incontinence in Korean Postmenopausal Women: Results from the Korean National Health and Nutrition Examination Survey. PLoS One. (2016) 11:e0149311. doi: 10.1371/journal.pone.0149311
3. Brown JS, Sawaya G, Thom DH, Grady D. Hysterectomy and urinary incontinence: a systematic review. Lancet. (2000) 356:535–9. doi: 10.1016/S0140-6736(00)02577-0
4. Choi JB, Yoon BI, Han KD, Hong SH, Ha US. Urinary incontinence is associated with the development of peptic ulcers in adult women: Data from the KNHANES IV. Medicine. (2017) 96:e8266. doi: 10.1097/MD.0000000000008266
5. Minassian VA, Drutz HP, Al-Badr A. Urinary incontinence as a worldwide problem. Int J Gynaecol Obstet. (2003) 82:327–38. doi: 10.1016/S0020-7292(03)00220-0
6. Sims J, Browning C, Lundgren-Lindquist B, Kendig H. Urinary incontinence in a community sample of older adults: prevalence and impact on quality of life. Disabil Rehabil. (2011) 33:1389–98. doi: 10.3109/09638288.2010.532284
7. Langemo D, Hanson D, Hunter S, Thompson P, Oh IE. Incontinence and incontinence-associated dermatitis. Adv Skin Wound Care. (2011) 24:126–40. doi: 10.1097/01.ASW.0000395037.28398.6c
8. Oh SJ, Ku JH, Choo MS, Yun JM, Kim DY, Park WH. Health-related quality of life and sexual function in women with stress urinary incontinence and overactive bladder. Int J Urol. (2008) 15:62–7. doi: 10.1111/j.1442-2042.2007.01905.x
9. Imamura M, Abrams P, Bain C, Buckley B, Cardozo L, Cody J, et al. Systematic review and economic modelling of the effectiveness and cost-effectiveness of non-surgical treatments for women with stress urinary incontinence. Health Technol Assess. (2010) 14:1–188. doi: 10.3310/hta14400
10. Caldwell KP. The electrical control of sphincter incompetence. Lancet. (1963) 2:174–5. doi: 10.1016/S0140-6736(63)92807-1
11. Messelink EJ. The overactive bladder and the role of the pelvic floor muscles. BJU Int. (1999) 83:31–5. doi: 10.1046/j.1464-410X.83.s2.7.x
12. Brubaker L. Electrical stimulation in overactive bladder. Urology. (2000) 55:17–23. doi: 10.1016/S0090-4295(99)00488-4
13. Fall M, Lindström S. Electrical stimulation. A physiologic approach to the treatment of urinary incontinence. Urol Clin North Am. (1991) 18:393–407. doi: 10.1016/S0094-0143(21)01005-3
14. Schreiner L, Santos TG, dos Souza ABA de, Nygaard CC, Silva Filho IG da. Electrical stimulation for urinary incontinence in women: a systematic review. Int Braz J Urol. (2013) 39:454–64. doi: 10.1590/S1677-5538.IBJU.2013.04.02
15. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. (2009) 339:b2535. doi: 10.1136/bmj.b2535
16. Correia GN, Pereira VS, Hirakawa HS, Driusso P. Effects of surface and intravaginal electrical stimulation in the treatment of women with stress urinary incontinence: randomized controlled trial. Eur J Obstet Gynecol Reprod Biol. (2014) 173:113–8. doi: 10.1016/j.ejogrb.2013.11.023
17. Franco M de M, Souza F de O, Vasconcelos ECLM de, Freitas MMS de, Ferreira CHJ. Avaliação da qualidade de vida e da perda urinária de mulheres com bexiga hiperativa tratadas com eletroestimulação transvaginal ou do nervo tibial. Fisioter Pesqui. (2011) 18:145–50. doi: 10.1590/S1809-29502011000200008
18. Amaro JL, Gameiro MO, Kawano PR, Padovani CR. Intravaginal electrical stimulation: a randomized, double-blind study on the treatment of mixed urinary incontinence. Acta Obstet Gynecol Scand. (2006) 85:619–22. doi: 10.1080/00016340500495058
19. Gungor Ugurlucan F, Onal M, Aslan E, Ayyildiz Erkan H, Kizilkaya Beji N, Yalcin O. Comparison of the effects of electrical stimulation and posterior tibial nerve stimulation in the treatment of overactive bladder syndrome. Gynecol Obstet Invest. (2013) 75:46–52. doi: 10.1159/000343756
20. Wang S, Lv J, Feng X, Lv T. Efficacy of electrical pudendal nerve stimulation versus transvaginal electrical stimulation in treating female idiopathic urgency urinary incontinence. J Urol. (2017) 197:1496–501. doi: 10.1016/j.juro.2017.01.065
21. Dmochowski R, Lynch CM, Efros M, Cardozo L. External electrical stimulation compared with intravaginal electrical stimulation for the treatment of stress urinary incontinence in women: A randomized controlled noninferiority trial. Neurourol Urodyn. (2019) 38:1834–43. doi: 10.1002/nau.24066
22. Terlikowski R, Dobrzycka B, Kinalski M, Kuryliszyn-Moskal A, Terlikowski SJ. Transvaginal electrical stimulation with surface-EMG biofeedback in managing stress urinary incontinence in women of premenopausal age: a double-blind, placebo-controlled, randomized clinical trial. Int Urogynecol J. (2013) 24:1631–8. doi: 10.1007/s00192-013-2071-5
23. Yildiz N, Alkan H, Sarsan A. Efficacy of intravaginal electrical stimulation added to bladder training in women with idiopathic overactive bladder: A prospective randomized controlled trial. Int braz j urol. (2021) 47:1150–9. doi: 10.1590/s1677-5538.ibju.2021.0161
24. Elmelund M, Biering-Sørensen F, Due U, Klarskov N. The effect of pelvic floor muscle training and intravaginal electrical stimulation on urinary incontinence in women with incomplete spinal cord injury: an investigator-blinded parallel randomized clinical trial. Int Urogynecol J. (2018) 29:1597–606. doi: 10.1007/s00192-018-3630-6
25. Hebbar S, Pandey H, Chawla A. Understanding King's Health Questionnaire (KHQ) in assessment of female urinary incontinence. Int J Res Med Sci. (2015) 3:531. doi: 10.5455/2320-6012.ijrms20150301
26. Nojomi M, Baharvand P, Moradi lakeh M, Patrick DL. Incontinence quality of life questionnaire (I-QOL): translation and validation study of the Iranian version. Int Urogynecol J. (2009) 20:575–9. doi: 10.1007/s00192-009-0808-y
27. Zhang HL, Huang ZG, Qiu Y, Cheng X, Zou XQ, Liu TT. Tamsulosin for treatment of lower urinary tract symptoms in women: a systematic review and meta-analysis. Int J Impot Res. (2017) 29:148–56. doi: 10.1038/ijir.2017.12
28. Bai SW, Sohn WH, Chung DJ, Park JH, Kim SK. Comparison of the efficacy of Burch colposuspension, pubovaginal sling, and tension-free vaginal tape for stress urinary incontinence. Int J Gynaecol Obstet. (2005) 91:246–51. doi: 10.1016/j.ijgo.2005.08.023
29. El-Barky E, El-Shazly A, El-Wahab OA, Kehinde EO, Al-Hunayan A, Al-Awadi KA. Tension free vaginal tape versus Burch colposuspension for treatment of female stress urinary incontinence. Int Urol Nephrol. (2005) 37:277–81. doi: 10.1007/s11255-004-6101-6
30. Goldman HB, Amundsen CL, Mangel J, Grill J, Bennett M, Gustafson KJ, et al. Dorsal genital nerve stimulation for the treatment of overactive bladder symptoms. Neurourol Urodyn. (2008) 27:499–503. doi: 10.1002/nau.20544
31. Bø K. Physiotherapy management of urinary incontinence in females. J Physiother. (2020) 66:147–54. doi: 10.1016/j.jphys.2020.06.011
32. Wallace SL, Miller LD, Mishra K. Pelvic floor physical therapy in the treatment of pelvic floor dysfunction in women. Curr Opin Obstet Gynecol. (2019) 31:485–93. doi: 10.1097/GCO.0000000000000584
33. Ptak M, Ciećwiez S, Brodowska A, Starczewski A, Nawrocka-Rutkowska J, Diaz-Mohedo E, et al. The effect of pelvic floor muscles exercise on quality of life in women with stress urinary incontinence and its relationship with vaginal deliveries: a randomized trial. Biomed Res Int. (2019) 2019:5321864. doi: 10.1155/2019/5321864
34. Hersh L, Salzman B. Clinical management of urinary incontinence in women. Am Fam Physician. (2013) 87:634–40.
35. Scaldazza CV, Morosetti C, Giampieretti R, Lorenzetti R, Baroni M. Percutaneous tibial nerve stimulation versus electrical stimulation with pelvic floor muscle training for overactive bladder syndrome in women: results of a randomized controlled study. Int Braz J Urol. (2017) 43:121–6. doi: 10.1590/s1677-5538.ibju.2015.0719
36. Iyer S, Laus K, Rugino A, Botros C, Lozo S, Botros SM, et al. Subjective and objective responses to PTNS and predictors for success: a retrospective cohort study of percutaneous tibial nerve stimulation for overactive bladder. Int Urogynecol J. (2019) 30:1253–9. doi: 10.1007/s00192-018-3822-0
37. Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. (2018) 27:1785–805. doi: 10.1177/0962280216669183
Keywords: intravaginal electrical stimulation, women, urinary incontinence, randomized controlled trials, meta-analysis
Citation: Yao H, Zhang X, Sun F, Tang G, Wu J and Zhou Z (2022) The efficacy of intravaginal electrical stimulation (IVES) in treating female with urinary incontinence symptom from meta-analysis of nine randomized controlled trials. Front. Neurol. 13:933679. doi: 10.3389/fneur.2022.933679
Received: 01 May 2022; Accepted: 26 July 2022;
Published: 13 September 2022.
Edited by:
Paul Yoo, University of Toronto, CanadaReviewed by:
Bowen Chang, The First Affiliated Hospital of University of Science and Technology of China Anhui Provincial Hospital, ChinaCopyright © 2022 Yao, Zhang, Sun, Tang, Wu and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhongbao Zhou, MzQ2ODk0MzgzQHFxLmNvbQ==; Jitao Wu, d2p0dXJvbG9neUAxNjMuY29t
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.