
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
STUDY PROTOCOL article
Front. Neurol. , 08 July 2022
Sec. Sleep Disorders
Volume 13 - 2022 | https://doi.org/10.3389/fneur.2022.911668
This article is part of the Research Topic Interaction Between Neuropsychiatry and Sleep Disorders: from Mechanism to Clinical Practice View all 19 articles
Background: Acute sleep deprivation (ASD) can effect mood, attention, memory, alertness and metabolism. Especially, it is often accompanied by cognitive impairment of the brain. Acupuncture is safe and effective for improving cognitive function, but its underlying mechanism is not fully understood. In this study, an event-related potential (ERP) technique will be employed to measure the behavioral, cognitive, and physiological changes produced by electroacupuncture intervention after ASD.
Methods: We will recruit 60 healthy subjects. The participants will be randomly divided into a treatment group, a control group, a sham electroacupuncture group and a blank group, at a 1:1:1:1 ratio. The primary outcome will be determined by the change from baseline to 36 h in the MoCA score. The secondary results include the amplitude and latency of ERP N2 and P3, Go-hit rates, Go-RTs, No-Go-FA rates, the WCST, the Digit Span Subtest of the WAIS, the ESS score and FS-14. The 15 healthy subjects will not receive acupuncture treatment and ASD, but will receive EEG records and cognition functions test at the beginning and end of the experiment. Electroacupuncture intervention will be performed for 30 min once every 12 h, a total of three times. ERP measurements and other tests will be performed after baseline and ASD, and the statistician and outcome evaluator will be blinded to treatment allocation.
Discussion: This study is expected to investigate the effectiveness of electroacupuncture in improving cognition for ASD.
Trial Registration: ChiCTR2200055999.
Acute sleep deprivation (ASD) is the elimination of sleep for a period of time (at least 24 h) to significantly prolong wakefulness (1). Inadequate sleep and sleep disorders have become an important public health problem. ASD can effect mood, attention, memory, alertness, cognitive performance and metabolism (2, 3). With the increasing pace of life, the incidence of sleep deprivation has increased significantly, which has attracted attention in the military field and many social sectors (such as aviation, navigation, medical treatment, and transportation). The common negative effects of sleep deprivation include feeling too sleepy during the day, accidents from lack of attention, mood changes, and changes in appetite (4). Insufficient sleep increases the risk of human error-related accidents (5). ASD affects cognition in many ways and can negatively impact alertness, learning, memory, and executive function (6–12). Since ASD has serious effects on human cognitive brain function, safety intervention studies on the effects of ASD, such as acupuncture, are increasingly popular in this field (13, 14).
Studies show that administration of caffeine may improve vigilance, alertness, mood and cognitive processes and enhance cognitive processing related to response selection and inhibition (15, 16). Compared with the central nervous system stimulant caffeine, acupuncture is a safe alternative therapy with minimal side effects (17). A Delphi expert consensus survey (18) shows that more than 80% of experts agree that acupuncture can be used to improve cognitive function, which has been underpinned by the results of previous studies (19, 20). Although acupuncture has been studied for a long time, there is still a lack of knowledge of the effects of acupuncture on the human brain. More research is necessary to better understand how brain activity is affected by acupuncture.
Executive function (also called executive control or cognitive control) is fundamental to human cognition (21). It is a top-down mental process needed when one has to concentrate and pay attention, when going on automatic or relying on instinct would be insufficient (22–24). There are three core executive functions: inhibition, working memory (WM), and cognitive flexibility (25, 26). The Go/No-go paradigm has been used to study the executive function (27). Event-related potential (ERP) has often been used to investigate the effects of sleep deprivation on neurocognitive functioning. It is non-invasive and simple to perform, and it does not entail discomfort for participants. Certain components of ERP have been found to reflect specific forms of information processing related to sensory, motor and/or cognitive functions (28). The visual Go/No-go task is often used to study response inhibition (29). There have been several reports supporting the hypothesis that the visual N2 reflects a frontal inhibition mechanism (30, 31), including cognitive control and response inhibition (32, 33). Furthermore, recent studies suggest that P3 may play an important role in the post-response stage, reflecting processes of cognitive processing, such as stimulus identification and evaluation (34, 35) or monitoring of inhibition (36, 37).
This high-quality randomized controlled trial (RCT) was designed via a pragmatic trial approach to objectively assess the efficacy of electroacupuncture for brain cognition using ERP. By comparing ERP related to response inhibition tasks before and after ASD, we can understand the effect of ASD on the brain's inhibition control and the effect of electroacupuncture on brain cognition function after ASD.
The aim of this study is to assess the effect of electroacupuncture on brain inhibition control function.
This study is a participant-, statistician-, and assessor-blinded parallel randomized control clinical trial. The study will follow the principles of the Consolidated Standards of Reporting Trials (CONSORT) as well as the Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA) statement for acupuncture. Sixty healthy college students will be randomly assigned to a treatment group, a sham electroacupuncture group and a blank group, at a 1:1:1:1 ratio. The control group will be set to evaluate the efficacy of electroacupuncture. The sham electroacupuncture group be set to rule out placebo effects. The study will be conducted at the Third Affiliated Hospital of Henan University of Traditional Chinese Medicine, Department of Acupuncture, Henan, China, following the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT). For the participant timeline, see Table 1.
According to the pre-test study, the average MoCA scores in the treatment group, control group, and blank group are 26.70, 25.72, and 27.32, respectively, and the standard deviations are 1.03, 1.59, and 1.37, respectively. Using the sample size calculation method of multi-group mean, the sample size estimation [one-way analysis of variance (ANOVA)] F-test] method will use the test level α = 0.05 (bilateral) and test efficiency 1 – β = 0.90. The bilateral test will be used. The total sample size of 45 cases was estimated using PASS 15.0 software.
All participants will be recruited through advertisements on websites and posters at colleges and universities near Henan University of Traditional Chinese Medicine. Treatment and measurements will be performed in quiet rooms. Participants will contact the recruitment staff by telephone or WeChat. Recruitment staff will be responsible for the enrollment of participants. If they meet the study criteria, they will be invited to the study. Eligible candidates will be asked to sign an informed consent form before the experiment begins. We will provide accommodation and meals during the experiment, and provide the participants a certain reward at the end of the experiment.
Recruitment conditions are as follows: (1) male college student in good health after physical examination; (2) 18–24 years of age and right-hand according to the modified Edinburgh Handedness Questionnaire; (3) normal or corrected-to-normal visual acuity; (4) normal state of sleep awakening, with no unusual sleep schedule–that is, waking up unusually early or late–and no history of shift; the self-made “sleep log” table and interview show that the subjects have good sleep habits; (5) on Symptom Checklist 90 (Symptom List-90 SCL Mel 90), the total average score is <1, and the score of each factor is <1; (6) the score of the Pittsburgh Sleep Quality Index (PSQI) is <5; (7) no habit of drinking coffee, tea, or alcohol or smoking; (8) voluntarily signing an informed consent form. The participants will be contacted a few days later to determine whether they are interested in participating, and, if so, an appointment will be made for them to physical examination package at the Third Affiliated Hospital of Henan University of Traditional Chinese Medicine.
Participants with any of the following conditions will be excluded: (1) having taken sedative or sleep-aiding drugs, such as estazolam or alprazolam, in the past month; (2) having received acupuncture or moxibustion treatment in the past month; (3) severe heart, liver, or kidney disease, mental illness, or coagulation dysfunction; (4) family history of mental illness or history of infectious diseases; (5) allergies, especially to needles; (6) implantation of a cardiac pacemaker or implantable electronic equipment.
(1) Those who do not fill in the cases in a timely and accurate manner or those who do not fill in the cases properly; (2) those who fail to follow the plan for treatment in the course of the trial; (3) subjects who automatically asked to withdraw.
Unrestricted (simple) randomization will be used to allocate participants to either the treatment group, control group, blank group. Participants will be randomized using sequentially numbered, opaque sealed envelopes (SNOSE) to maintain allocation concealment (38). Different personnel will carry out tasks such as assigning a sequence, recruiting subjects, or intervention.
In this trial, outcome assessors, and data analysts will be blinded to the treatment allocation to minimize potential sources of bias and the clinical researcher, assessor, and statistician will not share study information with each other. After the end of the experiment, we will use a questionnaire to ask the participants if they know whether they received real acupuncture or sham acupuncture.
All practitioners in this trial are licensed TCM acupuncture therapists with at least 5 years of clinical experience, and they will be trained to master the study protocol. The acupuncturist will be asked to administer the standard manipulation.
The treatment group will receive electroacupuncture and 36-h ASD. The choice of acupuncture points is based on a previous study (18). The acupoints will be Baihui (GV20), Sishencong (EX-HN1), and Shenting (GV24). Acupuncture at these acupoints mentioned above can regulate Qi of Governor Vessel, clear the mind, lift the spirits, nourish Yang based on Chinese acupuncture theory (39). Modern research shows that Baihui, Shenting and sishencong acupuncture can alleviates cognitive impairment (40–42).We will use sterile, disposable stainless-steel needles of the Hwato brand measuring 0.30 × 25 mm, with horizontal needling of 12–20 mm following an angle of 0–15°. After eliciting the Deqi response, the researcher will apply electroacupuncture by connecting an acupoint nerve stimulator (G6805-2A) to Baihui (GV20) and Shenting (GV24). The stimulation parameters are dense wave, frequency of 5 Hz, current of 1–5 mA, and needle retention for 30 min, with intervention performed every 12 h.
Placebo group is intervened with sham electroacupuncture. The sham GV20 point is 0.5 cun (≈12.5 mm) lateral to GV20, the sham EX-HN1 point is 0.5 cun (≈12.5 mm) horizontal to EX-HN1 and the sham GV24 point is 0.5 cun (≈12.5 mm) horizontal to GV24, pierce of 3–5 mm following an angle of 0–15°. Procedures, electrode placements, and other treatment settings are the same as in the treatment group but with no electricity output and needle manipulation for de qi.
Participants in the control group will receive only 36-h ASD but will not receive electroacupuncture treatment.
The healthy control group will not receive any intervention. They will keep normal work and rest time.
At the beginning of the visual Go/No-Go task, a small white cross (+) on a black background appears at the center of the screen for 100 ms before each trial, followed by the stimulus. Each stimulus is presented for a duration of 100 ms, with an inter-stimulus interval of 800 ms. The task has two blocks with 150 trials in each block. In one block, the subjects are asked to respond to the left arrow [target stimulus (Go)] and withhold responding to the right arrow [non-target stimulus (No-Go)], while in the other block, the response pattern is reversed. The Go stimuli occur with a one-third probability, and the sequence of Go/No-Go stimuli is pseudorandom to ensure that the No-Go stimuli do not appear in a continuous sequence. The participants will undergo a training session to ensure that they understand the Go/No-Go task and that their performance is above 90%.
The participants will arrive at the lab at 20:00 p.m. and perform a Go/No-Go task as a baseline. They will be asked to ensure that they get a full night's sleep (by wearing a wrist-operated sleep monitor and “sleep log” to ensure that they get at least 8 h of sleep), and the experiment will begin at 8:00 a.m. the next morning, taking the Go/No-Go task as 0 h. The participants will not be allowed to sleep for the next 36 h, during which time they will receive acupuncture every 11 h. After 36 h, the participants will be asked to complete the Go/No-Go task again. They will be accompanied and supervised by 10 staff members, and there will be two emergency doctors and nurses in the laboratory at all times. The participants will be asked to stay in the laboratory and will be allowed to talk, read, play computer games, and engage in other non-strenuous activities. They will not be allowed to smoke or drink coffee, tea, hot chocolate, wine, or other bladder-irritating drinks (Figure 1).
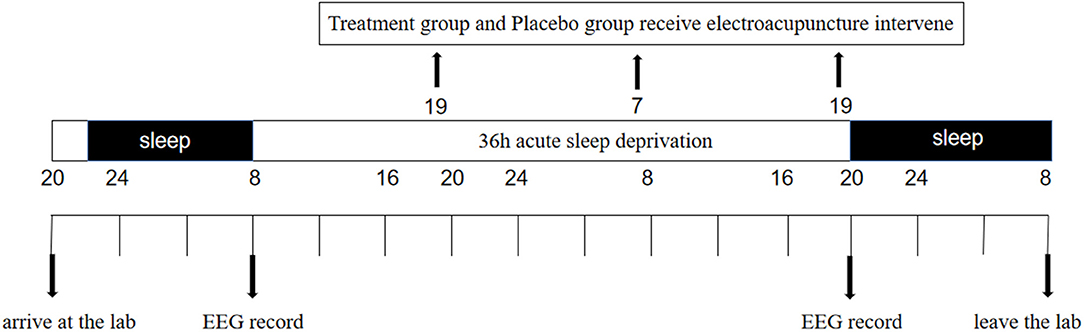
Figure 1. Study protocol. In the study protocol, subjects will undergo 36 h periods of acute sleep deprivation (ASD). The black arrows indicate the time points of Electro- encephalogram (EEG) recordings and treatment group receive electroacupuncture treatment.
The subjects will sit comfortably in a quiet room. Continuous EEG recordings will be obtained using Brain Vision recorder software. The sampling frequency will be 1,000 Hz, and the electrode impedances will be maintained below 5 kΩ. The electrodes will be placed according to the international 10–20 system; a total of 32 electrodes will be recorded in this study. ERP component analysis will be performed using Matlab 2018b and will include amplitudes and latencies. EEG data will be analyzed and collected by people who have received professional training.
The primary outcome is the MoCA score. The cognitive areas assessed include attention and concentration, executive function, memory, language, visual structure skills, abstract thinking, calculation and orientation, with a total score of 30. The lower the score, the more severe the cognitive impairment.
The behavioral data and latency and amplitude of N2 and P3 amplitude will be used to evaluate the effect of sleep deprivation and the intervention effect of acupuncture. ERP component detection, such as N2 and P3, has been used for the measurement of brain activity (13) and as a reflection of brain executive function (30–37). The behavioral outcome variables include the mean RT for correct hits, hit rates (correct button presses for Go stimuli), and the percentage of false alarms (FAs, incorrect button presses in response to No-Go stimuli), which are used as indices of individual behavior performance. Executive function and working memory will be assessed with the Wisconsin Card Sorting Test (WCST). Working memory and the Digit Span (DS) of the Wechsler Adult Intelligence Scale (43). The Epworth Sleepiness Scale (ESS), also known as the Epworth Daytime Sleepiness Scale, developed by Johns (44), will be used to evaluate excessive drowsiness during the day. The maximum score on the scale is 24 points, with >6 points indicating drowsiness, >11 points indicating excessive drowsiness, and >16 points indicating dangerous drowsiness. The FS-14 was jointly compiled by a number of experts, including Chalder and Berelowitz, in the United Kingdom (45). The physical fatigue score is obtained by adding the scores of eight items (1–8), the mental fatigue score is obtained by adding the scores of six items (9–14), and the total fatigue score is the sum of physical and mental fatigue scores. The highest score of physical fatigue is 8, the highest score of mental fatigue is 6, and the highest total score is 14. The higher the score, the more serious the fatigue.
Participant characteristics such as age, weight, body mass index, blood pressure, heart rate, pulse, liver function, renal function, electrocardiogram, and back pain history will be collected using electronic case report forms.
Any adverse event resulting from electroacupuncture in participants, such as headache, nausea, dizziness, localized infections, bleeding, or local subcutaneous hematoma, will be recorded, assessed, and reported. The occurrence time, cessation time duration, correlation with acupuncture, measures taken, and outcomes of adverse events will also be recorded. If serious adverse events occur, the Institutional Ethics Committee of the Third Affiliated Hospital of Henan University of Traditional Chinese Medicine will be informed, and the committee will decide whether to unblind and withdraw from the study.
Twelve hours after the completion of the trial, a follow-up health checkup will be performed, and the participants will be asked if they are experiencing any physical discomfort. The trial work plan is summarized in Figure 2.
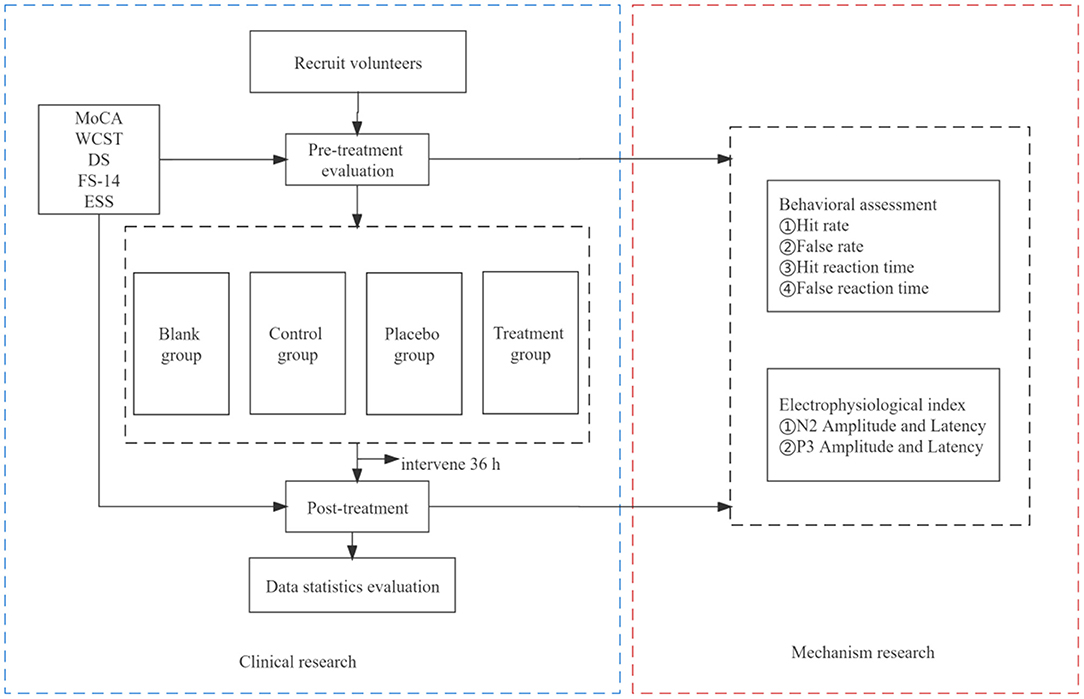
Figure 2. Trial work plan. The primary outcome measure will be MoCA. The remaining outcome measures will be for secondary outcomes.
Both paper files and electronic documents will be preserved for at least 5 years after publication. If readers have any questions, they can contact the corresponding author for access to the original data. Patient information will remain anonymous, including name, ID number, and telephone number. The protocol will be reviewed and revised by experts in acupuncture, emergency, methodology, and statistics. We will perform a pre-specified standard operating procedure, which includes screening patients, improving relevant inspection, acupuncture, filling out the CRF, assessing outcomes, and data management. Outcome assessments, completion of case report forms and data management will be closely supervised. We will be monitored by the IEC of the Third Affiliated Hospital of Henan University of Chinese Medicine, and it is independent from the investigators and sponsor which will audit trial conduct every 12 months. Any modifications and corrections to operation procedures will be fully documented using a breach report form, monitored, and submitted to the directors of the ethics committee and China Clinical Trial Registration.
We will use SPSS software version 21.0 (IBM Corp, Armonk, New York, US) to perform data analysis. Demographic and baseline data will be analyzed with standard descriptive statistics. Data will be presented as the mean ± standard deviation (SD). A repeated measure ANOVA is employed to analyze the electroacupuncture effects and the time effects on the behavioral data. The repeated measure ANOVA is also used for the analysis of ERP indices. ANOVAs are performed on the N2 and P3 components of the scalp electrodes in the Go/No-Go task. The accepted level of significance for all analyses will be P < 0.05.
All candidates who agree to participate and who meet all of the inclusion criteria and none of the exclusion criteria will be provided an informed consent form to provide them with full understanding of what the study participation will entail and the potential risks. Participants have the right to discontinue participation at any time. Data will be used in the aggregate only, and no identifying characteristics of individuals will be published or presented. In the consent form, the participants will be asked if they agree to the use of their data, should they choose to withdraw from the trial. The participants will also be asked for permission for the research team to share relevant data with people from the regulatory authorities, where relevant. This trial does not involve collecting biological specimens for storage. The study conforms to the principles of the Declaration of Helsinki. Ethical approval has been obtained from the IEC of the Third Affiliated Hospital of Henan University of Chinese Medicine. The trial protocol has been registered at the Chinese Clinical Trial Registry. The results will be disseminated through journal articles, a master's thesis, or conference presentations.
The purpose of this trial is to assess the impact of acupuncture on the management of brain cognition control. It is obvious that cognitive function is impaired after sleep deprivation. We intend to compare the effects of time (baseline and 36-h ASD) and intervention (electroacupuncture, sham electroacupuncture and non-electroacupuncture treatment) on executive brain function using a visual Go/No-Go task with simultaneous EEG recordings. Acupuncture is a non-toxic, economical intervention with minimal adverse effects (32) that has been shown to be effective after the therapy (11).
There are several methodological limitations to this study: (1) Due to the characteristics of acupuncture is the non-blinding of the acupuncturist. (2) Only young male subjects will be included; so, the findings may not be generalizable to women and older people. (3) The sample size is small. Despite these limitations, we will use rigorous methodology in this study, and we hope that the trial will help provide new insights into the value of acupuncture and evidence of ERP in executive brain function.
Recruiting will start in February 2022. The current protocol is version 1 of 27-12-2021. Patient recruitment is estimated to be completed around June 2022.
The studies involving human participants were reviewed and approved by The Third Affiliated Hospital of Henan University of Traditional Chinese Medicine. The patients/participants provided their written informed consent to participate in this study.
XC is the principal investigator, conceived the study and led the proposal, protocol development, study design, and methodology. HL and MW drafted the manuscript and performed the trial registration. YW will perform electroacupuncture operation and provided critical revision of the manuscript. CX designed the statistical analysis. PL, RZ, and ZL participated in the data collection. All authors have read and approved the final manuscript.
This trial was funded by National Natural Science Foundation of China Funded project plan (No. 81704183), the Traditional Chinese Medicine Administration of Henan Province (Nos. 2022ZYZD12 and 2018ZY2009), and the Construction Project of Chinese Medicine in Henan Province (STG-ZYX02-202111). The sponsor and funder have not participated in the study design, data collection and management, analysis, or interpretation of the data, the writing of the report, the decision to publish the report, or the preparation of the manuscript. The funder does not have ultimate authority over any of these activities.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We thank all students, school authorities, and staff for their contributions to this project. We thank LetPub (www.letpub.com) for its linguistic assistance during the preparation of this manuscript.
ASD, acute sleep deprivation; ERPs, event-related potentials; EHQ, Edinburgh Handedness Questionnaire; SCL-90, Symptom Checklist-90; PSQI, Pittsburgh Sleep Quality Index; MoCA, Montreal Cognitive Assessment; WCST, Wisconsin Card Sorting Test; DS, Digit Span of the Wechsler Adult Intelligence Scale; WAIS, Wechsler Adult Intelligence Scale; ESS, Epworth Sleepiness Scale; FS-14, Fatigue Scale-14; ANOVA, analysis of variance; IEC, Institutional Ethics Committee; EEG, electroencephalogram.
1. Reynolds AC, Banks S. Total sleep deprivation, chronic sleep restriction and sleep disruption. Prog Brain Res. (2010) 185:91–103. doi: 10.1016/B978-0-444-53702-7.00006-3
2. Banks S, Dinges DF. Behavioural and physiological consequences of sleep restriction. J Clin Sleep Med. (2007) 25:519–28. doi: 10.5664/jcsm.26918
3. Philip P, Akerstedt T. Transport and industrial safety, how are they affected by sleepiness and sleep restriction? Sleep Med Rev. (2006) 5:347–56. doi: 10.1016/j.smrv.2006.04.002
4. Bandyopadhyay A, Sigua NL. What is sleep deprivation? Am J Respir Crit Care Med. (2019) 199:11–2. doi: 10.1164/rccm.1996P11
5. Dinges DF. An overview of sleepiness and accidents. J Sleep Res. (1995) 4:4–14. doi: 10.1111/j.1365-2869.1995.tb00220.x
6. Doran SM, Van Dongen HP, Dinges DF. Sustained attention performance during sleep deprivation: evidence of state instability. Arch Ital Biol. (2001) 139:253–67. doi: 10.4449/aib.v139i3.503
7. Van Dongen HP, Baynard MD, Maislin G, Dinges DF. Systematic interindividual differences in neurobehavioral impairment from sleep loss: evidence of trait-like differential vulnerability. Sleep. (2004) 27:423–33. doi: 10.1093/sleep/27.3.42
8. Heuer H, Kohlisch O, Klein W. The effects of totalsleep deprivation on the generation of random sequences of key-presses, numbers and nouns. Q J Exp Psychol A. (2005) 58:275–307. doi: 10.1080/02724980343000855
9. Killgore WD. Effects of sleep deprivation on cognition. Prog Brain Res. (2010) 185:105–29. doi: 10.1016/B978-0-444-53702-7.00007-5
10. Jackson ML, Gunzelmann G, Whitney P, Hinson JM, Belenky G, Rabat A, et al. Deconstructing and reconstructing cognitive performance in sleep deprivation. Sleep Med Rev. (2013) 17:215–25. doi: 10.1016/j.smrv.2012.06.007
11. Krause AJ, Simon EB, Mander BA, Greer SM, Saletin JM, Goldstein-Piekarski AN, et al. The sleep-deprived human brain. Nat Rev Neurosci. (2017) 18:404–18. doi: 10.1038/nrn.2017.55
12. Chen J, Liang J, Lin X, Zhang Y, Zhang Y, Lu L, et al. Sleep deprivation promotes habitual control over goal-directed control: behavioral and neuroimaging evidence. J Neurosci. (2017) 37:11979–92. doi: 10.1523/JNEUROSCI.1612-17.2017
13. Gao L, Zhang M, Gong H, Bai L, Dai X-J, Min Y, et al. Differential activation patterns of FMRI in sleep-deprived brain: restoring effects of acupuncture. Evid Based Complement Alternat Med. (2014) 2014:465760. doi: 10.1155/2014/465760
14. Li J, Ran X, Cui C, Xiang C, Zhang A, Shen F. Instant sedative effect of acupuncture at GV20 on the frequency of electroencephalogram α and β waves in a model of sleep deprivation. Exp Ther Med. (2018) 15:5353–8. doi: 10.3892/etm.2018.6123
15. Chen X, Zhang L, Yang D, Li C, An G, Wang J, et al. Effects of caffeine on event-related potentials and neuropsychological indices after sleep deprivation. Front Behav Neurosci. (2020) 22:14:108. doi: 10.3389/fnbeh.2020.00108
16. Spriet LL. Exercise and sport performance with low doses of caffeine. Sports Med. (2014) 44:S175–84. doi: 10.1007/s40279-014-0257-8
17. Zulli A, Smith RM, Kubatka P, Novak J, Uehara Y, Loftus H, et al. Caffeine and cardiovascular diseases: critical review of current research. Eur J Nutr. (2016) 55:1331–43. doi: 10.1007/s00394-016-1179-z
18. Su XT, Wang LQ, Li JL, Zhang N, Wang L, Shi GX, et al. Acupuncture therapy for cognitive impairment: a Delphi expert consensus survey. Front Aging Neurosci. (2020) 12:596081. doi: 10.3389/fnagi.2020.596081
19. Liu F, Li ZM, Jiang YJ, Chen LD. A meta-analysis of acupuncture use in the treatment of cognitive impairment after stroke. J Altern Complement Med. (2014) 20:535–44. doi: 10.1089/acm.2013.0364
20. Wang YY, Yu SF, Xue HY, Li Y, Zhao C, Jin YH. Effectiveness and safety of acupuncture for the treatment of Alzheimer's disease: a systematic review and meta-analysis. Front Aging Neurosci. (2020) 12:98. doi: 10.3389/fnagi.2020.00098
21. Doebel S. Rethinking executive function and its development. Perspect Psychol Sci. (2020) 15:942–56. doi: 10.1177/1745691620904771
22. Espy KA. Using developmental, cognitive, and neuroscience approaches to understand executive control in young children. Dev Neuropsychol. (2004) 26:379–84. doi: 10.1207/s15326942dn2601_1
23. Miller EK, Cohen JD. An integrative theory of prefrontal cortex function. Annu Rev Neurosci. (2001) 24:167–202. doi: 10.1146/annurev.neuro.24.1.167
24. Diamond A. Executive functions. Annu Rev Psychol. (2013) 64:135–68. doi: 10.1146/annurev-psych-113011-143750
25. Miyake A, Friedman NP, Emerson MJ, Witzki AH, Howerter A, Wager TD. The unity and diversity of executive functions and their contributions to complex “frontal lobe” tasks: a latent variable analysis. Cogn Psychol. (2000) 41:49–100. doi: 10.1006/cogp.1999.0734
26. Lehto JE, Juujärvi P, Kooistra L, Pulkkinen L. Dimensions of executive functioning: evidence from children. Br J Dev Psychol. (2003) 21:59–80. doi: 10.1348/026151003321164627
27. Kropotov JD, Ponomarev VA, Hollup S, Mueller A. Dissociating action inhibition, conflict monitoring and sensory mismatch into independent components of event related potentials in GO/NOGO task. Neuroimage. (2011) 57:565–75. doi: 10.1016/j.neuroimage.2011.04.060
28. Ford JM, Pfefferbaum A. Event-related potentials and eyeblink responses in automatic and controlled process sing: effects of age. Electroencephalogr Clin Neurophysiol. (1991) 78:361–77. doi: 10.1016/0013-4694(91)90098-O
29. Cid-Fernández S, Lindín M, Díaz F. Effects of amnestic mild cognitive impairment on N2 and P3 Go/NoGo ERP components. J Alzheimers Dis. (2014) 38:295–306. doi: 10.3233/JAD-130677
30. Geczy I, Czigler I, Balazs L. Effects of cue information on response production and inhibition measured by event-related potentials. Acta Physiol Hung. (1999) 86:37–44.
31. Bokura H, Yamaguchi S, Kobayashi S. Electrophysiological correlates for response inhibition in a Go/NoGo task. Clin Neurophysiol. (2001) 112:2224–32. doi: 10.1016/S1388-2457(01)00691-5
32. Magnuson JR, Peatfield NA, Fickling SD, Nunes AS, Christie G, Vakorin V, et al. Electrophysiology of inhibitory control in the context of emotion processing in children with autism spectrum disorder. Front Hum Neurosci. (2019) 13:78. doi: 10.3389/fnhum.2019.00078
33. Quaglia JT, Zeidan F, Grossenbacher PG, Freeman SP, Braun SE, Martelli A, et al. Brief mindfulness training enhances cognitive control in socioemotional contexts: behavioral and neural evidence. PLoS ONE. (2019) 14:e0219862. doi: 10.1371/journal.pone.0219862
34. Feng X, Huang L, Wang Z, Wang L, Du X, Wang Q, et al. Efficacy of remote limb ischemic conditioning on poststroke cognitive impairment. J Integr Neurosci. (2019) 18:377–85. doi: 10.31083/j.jin.2019.04.1192
35. Khedr EM, El Fetoh NA, Gamal RM, Elzohri MH, Azoz NMA, Furst DE. Evaluation of cognitive function in systemic sclerosis patients: a pilot study. Clin Rheumatol. (2020) 39:1551–9. doi: 10.1007/s10067-019-04884-9
36. Beste C, Willemssen R, Saft C, Falkenstein M. Response inhibition subprocesses and dopaminergic pathways: basal ganglia disease effects. Neuropsychologia. (2010) 48:366–73. doi: 10.1016/j.neuropsychologia.2009.09.023
37. Schmiedt-Fehr C, Basar-Eroglu C. Event-related delta and theta brain oscillations reflect age-related changes in both a general and a specific neuronal inhibitory mechanism. Clinical Neurophysiol. (2011) 122:1156–67. doi: 10.1016/j.clinph.2010.10.045
38. Doig GS, Simpson F. Randomization and allocation concealment: a practical guide for researchers. J Crit Care. (2005) 20:187–91. doi: 10.1016/j.jcrc.2005.04.005
39. Yu C, Wang L, Kong L, Fenga S, Chaoyang M, Yanjun D, et al. Acupoint combinations used for treatment of Alzheimer's disease: a data mining analysis. J Tradit Chin Med. (2018) 38:943–52. doi: 10.1016/S0254-6272(18)30995-6
40. Jittiwat J. Baihui point laser acupuncture ameliorates cognitive impairment, motor deficit, and neuronal loss partly via antioxidant and anti-inflammatory effects in an animal model of focal ischemic stroke. Evid Based Complement Alternat Med. (2019) 2019:1204709. doi: 10.1155/2019/1204709
41. Li F, Wang Y, Jiang T-X, Zhu M-J, Ji J-J, Wu W-W, et al. Acupuncture and moxibustion for vascular dementia and its effect on serum VEGF and AChE. Zhongguo Zhen Jiu. (2021) 41:851–4. doi: 10.13703/j.0255-2930.20200816-0001
42. Han H, Xin L, Jiang H-N, Xu K, Wang Y. Effect of early acupuncture on cognitive function in patients with vasculai dementia after cerebral infarction. Zhongguo Zhen Jiu. (2021) 41:979–83.
43. Maltese F, Adda M, Bablon A, Hraeich S, Guervilly C, Lehingue S, et al. Night shift decreases cognitive performance of ICU physicians. Intensive Care Med. (2016) 42:393–400. doi: 10.1007/s00134-015-4115-4
44. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. (1991) 14:540–5. doi: 10.1093/sleep/14.6.540
Keywords: electroacupuncture, cognition, acute sleep deprived, Go/No-Go, ERP
Citation: Li H, Wang M, Wu Y, Chen X, Xue C, Liu P, Zhang R and Liao Z (2022) Clinical Effect of Electroacupuncture on Acute Sleep Deprivation and Event-Related Potential Affecting the Inhibition Control of the Brain: Study Protocol for a Randomized Controlled Trial. Front. Neurol. 13:911668. doi: 10.3389/fneur.2022.911668
Received: 03 April 2022; Accepted: 17 June 2022;
Published: 08 July 2022.
Edited by:
Huajun Liang, University of Maryland, United StatesReviewed by:
Yang Hu, Xidian University, ChinaCopyright © 2022 Li, Wang, Wu, Chen, Xue, Liu, Zhang and Liao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xinwang Chen, Y3h3MjMxNjFAMTI2LmNvbQ==
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.