- 1Bloorview Research Institute, Holland Bloorview Kids Rehabilitation Hospital, Toronto, ON, Canada
- 2Rehabilitation Sciences Institute, University of Toronto, Toronto, ON, Canada
- 3Centre for Addiction and Mental Health, Toronto, ON, Canada
- 4Department of Pharmacology and Toxicology, University of Toronto, Toronto, ON, Canada
- 5Department of Psychiatry, University of Toronto, Toronto, ON, Canada
- 6Neuroscience and Mental Health Program, Hospital for Sick Children, Toronto, ON, Canada
- 7Department of Physiology, University of Toronto, Toronto, ON, Canada
- 8Sunnybrook Research Institute, Sunnybrook Health Sciences Centre, Toronto, ON, Canada
- 9Institute of Medical Sciences, University of Toronto, Toronto, ON, Canada
- 10Department of Paediatrics, University of Toronto, Toronto, ON, Canada
Objective: Concussion is a common yet heterogenous injury. Approximately 15–30% of cases present with persistent post-concussion symptoms (PPCS), continuing 4 weeks or more post-injury in children, youth, and adolescents, and 3 months or more in adults. There are known bidirectional links between PPCS and mental health outcomes. The focus of this scoping review is to explore the literature on mental health outcomes in individuals experiencing PPCS. Research objectives were to explore: (1) the mental health outcomes of individuals with PPCS and types of assessments used to identify mental health outcomes this group, and (2) how mental health outcomes compare in terms of similarities and differences among pediatric and adult populations with PPCS.
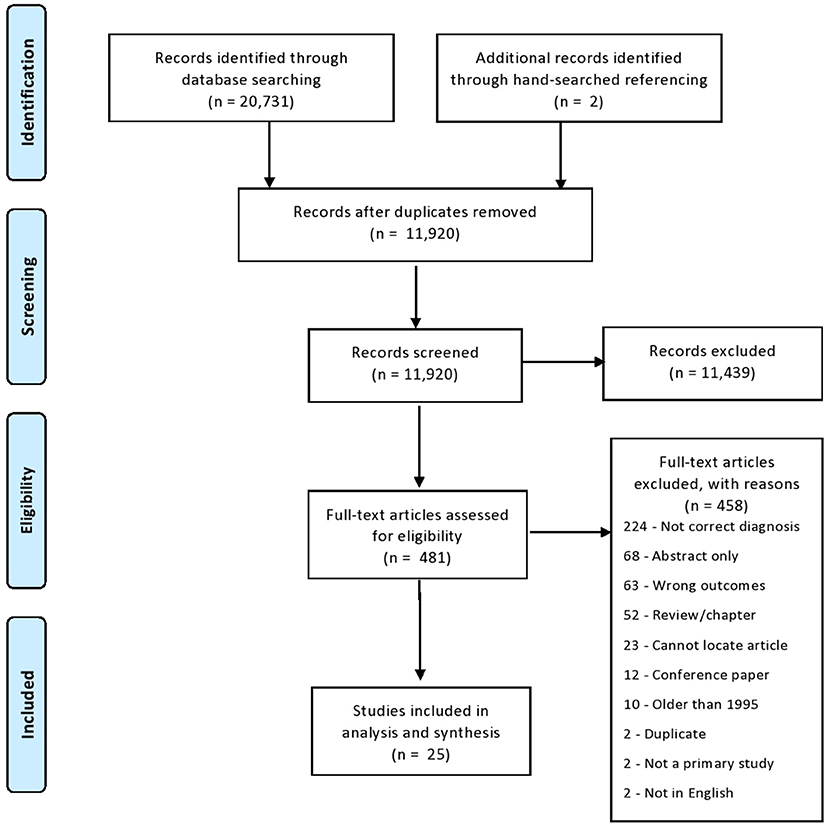
Method: Ovid MEDLINE; EMBASE; CINAHL, and PsycInfo databases were searched. After title and abstract screening of 11,920 studies, 481 articles were reviewed. Twenty-five papers met inclusion criteria. Results were organized by mental health outcomes of pediatric and adult populations, separately.
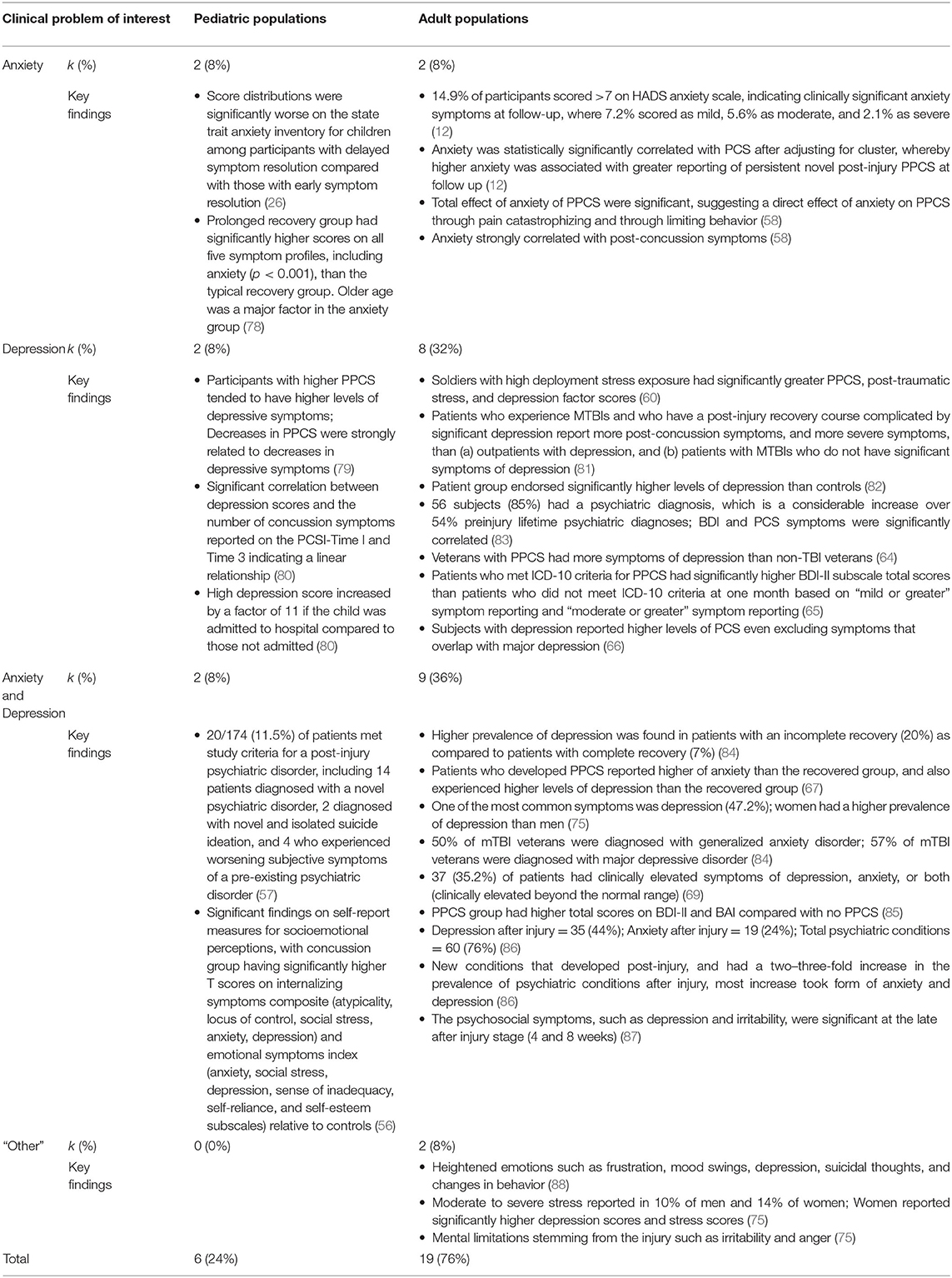
Results: There was a significantly higher number of studies devoted to adult populations. Of the 25 studies, 19 (76%) focused on adults, while six (24%) focused on adolescents. In adult populations, studies focused on symptoms of: anxiety (n = 2), depression (n = 8), and anxiety and depression (n = 9). Two studies assessed other emotional outcomes (10.5%). Within pediatric populations, an equal number of studies explored symptoms of: anxiety (n = 2), depression (n = 2), and anxiety and depression (n = 2). No studies focused on other emotional outcomes. Studies ranged greatly in methods, design, and control group. Most studies reported higher psychiatric symptoms of anxiety and/or depression in those with PPCS compared to individuals with recovered concussion or healthy controls.
Discussion: This review contributes to the understanding of mental health outcomes in those experiencing PPCS. Mental health and PPCS requires greater attention in pediatric populations, and consider strategies for those experiencing PPCS and mental health impacts. Future studies should consider including a wider range of emotional outcomes in their design, not limited to anxiety and depression. Study results may lead to improvements and research in the identification, assessment, and management of PPCS and mental health.
Introduction
Mild traumatic brain injury (mTBI), or concussion, is an international public health concern (1–5). Concussion is an injury induced by biomechanical forces, such as a blow to the head or body causing the brain to move rapidly inside the skull (6). Clinical presentation of symptoms following concussion are variable, and can manifest as a combination of cognitive, physical, affective, or sleep-related outcomes (7–9). Although most individuals who sustain a concussion recover without complications, studies show that symptoms can persist beyond 3 months post-concussion for 15–25% of adults (10–12) and beyond 4 weeks post-injury in ~30% of children (13). Hence, after sustaining a concussion, a sub-set of individuals may experience persistent post-concussion symptoms (PPCS). Common PPCS symptoms include headaches, dizziness, sleep disturbance, and psychological symptoms such as irritability, anxiety, and depression (14).
One challenge within this field is that there are several definitions of PPCS that differ within the adult and pediatric literatures and limited understanding for exactly which individuals will fall into the PPCS sub-set (15, 16). One definition requires adults (18+ years) to have a history of concussion, display cognitive impairments, and showcase at least three of the following symptoms for a minimum 3-month duration: fatigue, headache, dizziness, sleep disruption, irritability, apathy, or changes in personality (17). The Berlin Consensus Statement on Concussion in Sport defined a prolonged time frame to be more than 2 weeks in adults and more than 4 weeks in children (6). The specific symptoms or symptom profiles are not explicitly outlined within this definition. An expert consensus-based definition for persistent post-concussion diagnosis in those 16 years or older states that concussion symptoms must be present every day for 3 months after the trauma, and have an impact on at least one sphere of a person's life (18). Despite these differing definitions, there seems to be consensus that PPCS may have serious consequences for psychosocial-behavioral development (19, 20) and quality of life (21).
Individuals who have experienced a concussion may be at risk for poor mental health outcomes (22–24). A population-based study by Yang et al. (25) found that adolescents who experience a concussion are at an increased risk for higher depressive symptoms and self-injurious behaviors. Additionally, delayed symptom resolution has been associated with increased anxiety compared to children with early symptom resolution (26). Amongst adults, a study by Whelan-Goodinson et al. (27) found that >65% of those with concussion experienced symptoms of depression and anxiety after injury and showed poor recovery rates. For those with PPCS, new diagnoses of psychiatric symptoms have been reported in 36% of adolescents (28). In addition, pre-injury psychological and psychiatric history have shown to be predictors of PPCS (12, 29). Therefore, a link between concussion and poor mental health outcomes such as depression and anxiety (30) in both pediatric and adult populations has been established in the literature. There are three possibilities that may explain this link. First, concussion directly results in mood dysregulation and symptoms that impact mental health. The Concussion in Sport Group Consensus Statement highlights the importance of post-concussion mental health as mood problems like depression can develop after injury (6). Another possibility is that reduced activities associated with the post-concussive state have psychosocial implications that could lead to poor mental health outcomes. A third possibility is the link between pre-injury family and personal psychiatric history that can increase susceptibility to future mental health conditions post-injury (31). PPCS can make daily functioning significantly harder, thereby lowering quality of life in social, academic, and professional sectors (21). In addition, symptom overlap may partially explain this link, as irritability, anxiety, and difficulty concentrating, are a few of the symptoms found in those with PPCS and other psychiatric disorders (32). Thus, it is important to explore the relationship between mental health outcomes and PPCS for the early identification of mental health difficulties in individuals with PPCS.
Recent reviews have focused on the association between post-injury mental health and prolonged recovery in athletes (33, 34), and the most popular topics in concussion focus on the relationship between acute concussion and mental health outcomes rather than PPCS (35, 36). While studies are emerging that focus on PPCS, they predominantly report on interventions, treatments, and management (37–39). Therefore, the focus of this scoping review is to explore: (1) the mental health outcomes of individuals with PPCS and the types of assessments used to identify mental health outcomes this group, and (2) how mental health outcomes compare in terms of similarities and differences among pediatric and adult populations with PPCS. Specifically, we wanted to answer the question: What are the associations of mental health outcomes and PPCS post-injury and types of assessments used that examine mental health outcomes across the lifespan in individuals with PPCS?
Methods
A scoping review was used to address study objectives. The purpose of a scoping review is to establish and survey the current field of literature on a given topic, identify common and key characteristics of studies or related concepts, and divulge existing gaps (40, 41), rather than comment on the quality of studies or confirm current practices and/or interventions (41), as a systematic review would do. A scoping review is preferential to a systematic review for this topic, as studies on mental health outcomes across the lifespan in individuals with PPCS has yet to be synthesized. Thus, a broad scope of the literature is warranted prior to a systematic review. Scoping review guidelines and frameworks were adopted in line with Arksey and O'Malley (42), with considerations from Levac et al. (40), as well as adhering to the PRISMA-ScR checklist (43).
Stage 1: Identify the Research Question
Our goal was to explore the mental health outcomes that occur across the lifespan in those with PPCS. As PPCS has various terminology, definitions were set in order to thoroughly capture all studies that may mention any synonym of PPCS. PPCS was defined as any concussion disorder lasting longer than 4 weeks, and could be addressed as “PPCS,” “persistent concussion symptom (PCS),” or “chronic,” “long-term,” “persistent,” or “prolonged” followed by “mTBI,” “concussion,” “minor TBI,” or “mild/minor head injury.” As there is ambiguity in specific diagnostic criteria of PPCS, a minimum of 4 weeks was the chosen symptom duration. This criterion is also consistent with what is found in more recent literature (44, 45). There was no upper limit set on duration, to try and capture as many studies with persistent symptoms as possible.
For the purpose of our study, the term “adolescents” is defined as individuals aged 10–18 years old, according to the World Health Organization (46); and those aged younger than 10 years are described as “children.” For this review, the age range for pediatrics was operationalized to include children and adolescents aged 0–18 years old, but could be in their 19th year (e.g., 18 years, 11 months). To note, anyone in the children or adolescent range will be referred to hereinafter under the umbrella term “pediatric” to encompass this age span. Adults are defined as individuals aged 19 years and above. Any studies including “university-aged” participants with no stated age range, fell under the adult definition, as most university students are 19 years or older. Furthermore, mental health outcomes were defined as mood disorders or emotional outcomes that could be measured and assessed by standardized psychological tests or psychological screening measures, that have been reported as symptoms of PPCS. Mental health outcomes did not need to be clinically diagnosed, and terminology included but was not limited to “depression,” “anxiety,” “worry,” “sadness,” “aggression,” and “irritability.” Inclusion and exclusion of particular mental health outcomes will be addressed in the eligibility criteria. Moving forward for simplicity, all mTBI terminology will be referred to as “concussion,” and PPCS terminology referred to as “PPCS.”
Stage 2: Identifying Relevant Studies
Eligibility Criteria
To be considered an eligible study, the participants in the study must have experienced a concussion, as classified by diagnostic measures, such as: ICD-10 criteria, Glasgow Coma Scale score between 13 and 15, loss of consciousness <30 min, and/or post-traumatic amnesia lasting <24 h (47). In addition, participants needed to experience at least one concussion symptom, classified by a concussion assessment measure such as the Post-Concussion Symptom Inventory (48), Post-Concussion Symptom Scale (49), or the Sport Concussion Assessment Tool (50), lasting for at least 4 weeks in duration. Concussions determined by self-report and healthcare professional were both included if definition criteria were met. All age groups were considered eligible, including infants and older adults. Injuries categorized as an acute concussion (<4 weeks post-injury), or moderate or severe TBI were excluded. Participants could have multiple previous concussions documented, but the primary focus of the study had to center on PPCS. Additionally, head injuries (including moderate and severe TBI) that were not related to their concussion (e.g., contusion, edema, hematoma, hemorrhages, fractures, or chronic traumatic brain injury) were also not included in the review. Studies with mental health outcomes including psychiatric/psychological disorders of anxiety (including generalized anxiety disorder, social anxiety, and phobias) and depression (major depressive disorder, and persistent depressive disorder) were eligible. Studies were not excluded if they did not include data on pre-injury personal or family psychiatric history, as post-injury data was the primary focus. Literature suggests that emotional and behavioral challenges are part of PPCS sequelae (51–53). Hence, we included studies that address commonly reported emotional symptoms that do not require a formal diagnosis. This includes sadness, worry, anger, irritability, and low mood. Of note, attention was excluded if it was classified as a cognitive domain. Quality of life studies were included, but had to explicitly measure an emotional outcome stated from this study (e.g., sadness, worry, etc.).
Studies were excluded if they were published prior to 1995, as this was the point at which PPCS emerged as accepted terminology, and extending the timeline prior to 1995 would make it difficult to distinguish what was captured as PPCS (54). Of note, the earliest study extracted from the search results was published in 2003. Studies could not be written in anything other than the English language. Further, only peer-reviewed primary studies were accepted, of both qualitative and quantitative nature. Study designs were limited to human subjects only. Studies could include a neuroimaging component, but they also required mental health outcome measures, rather than solely neuroimaging.
Database Search
Identifying studies relevant to the question of interest was achieved using four databases: Ovid MEDLINE, PsycInfo, CINAHL, and EMBASE. A hand-search of all reference lists from included studies was conducted to ensure relevant papers were captured in the search.
Search Strategy
Search queries and strategies used followed the population, concept, context framework (see Supplementary Tables 1–4 for database search strategies) (41). Each search was guided using Boolean operators “AND” and “OR” to create a relevant search queue. The appropriate truncations and adjacencies associated with each database were used, as well as MeSH terms and keywords, where applicable.
Stage 3: Study Selection
In total, 20,731 studies were extracted from the four databases. Upon retrieval of all relevant papers from each database, EndNote X9®, a reference management software, was used to compile all papers, and remove duplicates. Once duplicates were removed, all papers were transferred to Covidence®, an online tool designed to streamline review processes, to begin screening the papers. A final number of 11,920 papers advanced to screening following de-duplication. Of note, an original database search was conducted in July 2020. A second, updated search was run from July 2020 to February 2021 due to the advancing literature in this subject area. All statistics and results have been updated to reflect the most recent search date.
Two screening processes were completed to ensure a detailed and thorough review of all relevant papers was practiced: (1) title and abstract screening, and (2) full text screening. Two independent reviewers completed title and abstract screening [ES, HA], with the same inclusion and exclusion criteria. The reviewers met prior to screening to discuss their strategy and ensure they were following the same criteria. A third, independent reviewer [BL] assisted with all stages of screening, charting, and analysis, as well as resolution of screening conflicts between the first and second reviewers.
After title and abstract screening, 481 papers advanced to full text screening, also completed in Covidence®. Once included papers were finalized, papers were transferred to Mendeley®, another reference management tool, to house the full-text, and subsequently back to Covidence® to read the full text and screen. From full-text screening, 23 papers successfully met inclusion criteria. Additionally, two papers met inclusion criteria from hand-searched referencing, which arose from manually checking the reference lists of each included paper. Thus, a total of 25 papers were included in the scoping review. Four hundred and fifty-eight papers were excluded from review after full-text screening (see Figure 1 for full PRISMA diagram and exclusion justification).
Stage 4: Charting the Data
Once all included studies were established, data was documented using Microsoft Excel® charting via spreadsheet program. The chart was co-created by all three reviewers and discussed thoroughly to ensure that all relevant and important details from each study were documented. Prior to charting all data, 10 studies were selected, reviewed and charted by all reviewers to serve as a pilot run. This ensured that reviewers were consistent in their documentation processes. The three reviewers met after pilot charting to review the process and study eligibility criteria.
General study characteristics (title, author, year, design, and objectives) were charted to archive traditional study qualities. Furthermore, following the “population, concept, and context framework” (40), population (participant group, gender, age, and sample number), concept (mental health outcome, assessment measurement, symptom severity, and key findings), and context (PPCS injury mechanism and history, terminology, outcome measurement, diagnosis information, and key findings) information were documented to chronicle important features, and draw comparisons and generate themes later during analyses (see Supplementary Table 5 for extraction chart template).
Stage 5: Collating, Summarizing, and Analyzing Results
Following charting of all relevant data, Microsoft Excel® spreadsheets were used to collate results, resulting in summary tables, organized, and separated by pediatric and adult study findings. Each pediatric and adult summary table consisted of the following headings: author, year, study purpose, population (sample size and mean age), study design, mental health outcome and measurement, and key findings. Numerical analyses were used to understand the extent, breadth, nature, and distribution of included studies by evaluating the general study characteristics across papers (41). Furthermore, a smaller table was created to document the general mental health outcome findings within and between pediatric and adult studies, in order to better conceptualize the distribution of outcomes across groups.
Results
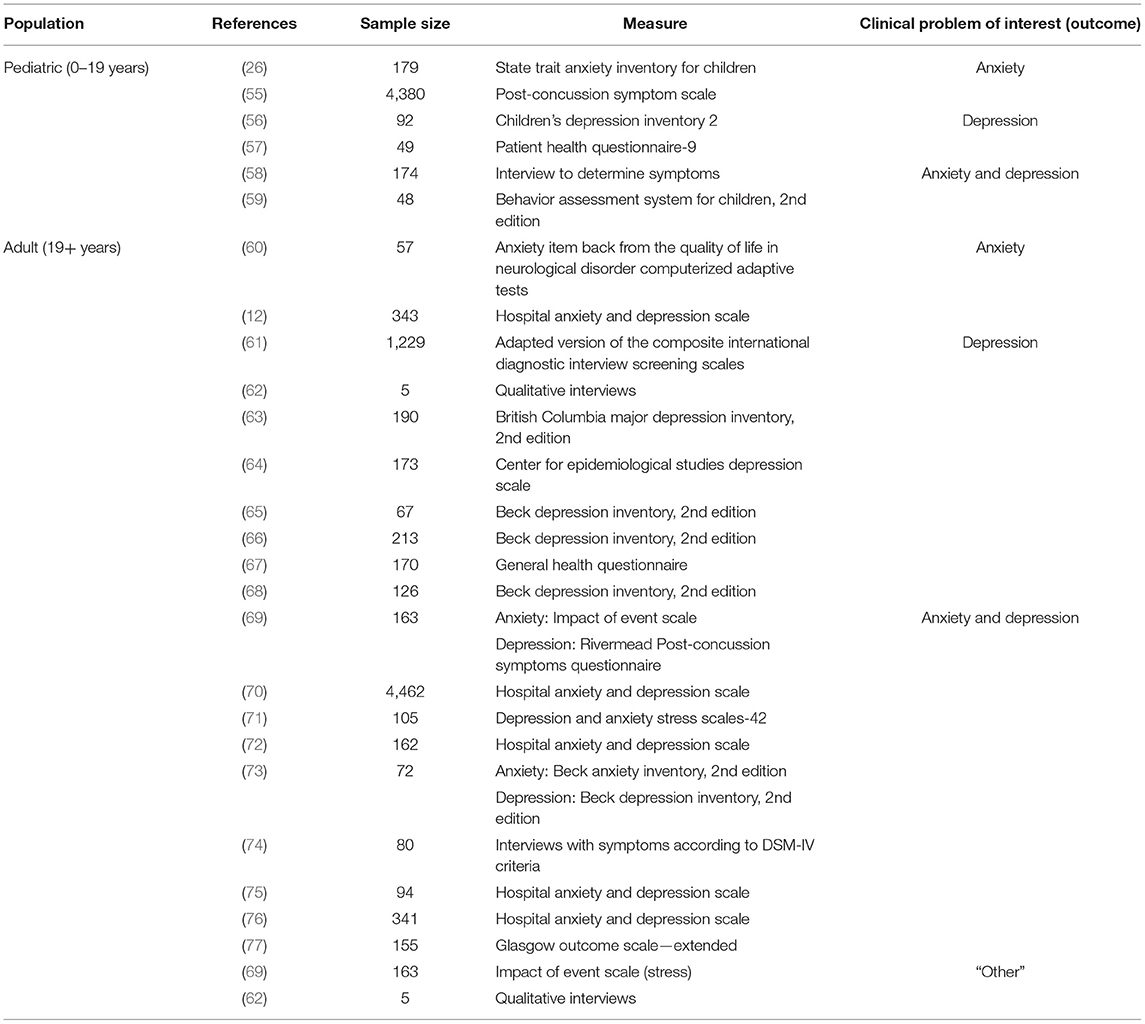
Results are organized first according to general participant and study characteristics, followed by outcome measures (see Supplementary Table 5). Thereafter, mental health outcome results are summarized, and organized according to anxiety, depression, anxiety and depression, and “other” mental health outcomes, and further sub-categorized into pediatric and adult findings, to allow for comparisons between groups (see Table 1 for summary of outcome and assessments and Table 2 for summary of key findings across populations, and Supplementary Tables 6, 7 for detailed results of the studies).
General Participant and Study Characteristics
Of the 25 studies published from 2003 to 2021, six studies focused on children and adolescents, and the remaining 19 focused on adults. The primary location of studies was within North America, originating in the United States (n = 11) or Canada (n = 7), followed by a small number in Europe, including Sweden (n = 2), Finland (n = 1), and The Netherlands (n = 1). The remaining studies were in New Zealand (n = 1), Australia (n = 1), and China (n = 1). Sample size was broad amongst studies, with as small as five participants, to as large as 4,462 participants. The varied distribution of sample sizes is displayed in Table 1. There was heterogeneity in the distribution of male and female representation across studies; the majority had a relatively equal proportion, where the male-female ratio fell between 40 and 50% (n = 13); however, when comparing unequal distributions, there was much greater number of studies with male majority (n = 9) than female majority (n = 3). Age of participants ranged from 8 to 19 years in pediatric studies, and 19–91 years in adult groups. The primary participant group featured outpatients from past hospital visit (e.g., emergency department) or TBI clinics (n = 13). Other studies included pediatrics with past unspecified or sports-related concussion (n = 4), army or combat veterans (n = 3), community-dwelling participants (n = 3), university students (n = 1) or older adult populations (n =1). Nineteen studies required a formal diagnosis of concussion (e.g., by physician or nurse practitioner) and five relied on self-report. One study did not specify how they were diagnosed. Furthermore, while seven studies included pre-injury personal and/or family mental health history in their data but was not the main outcome of the study, and many studies did not document or assess pre-injury mental health personal or family history (n = 14).
Most studies were quantitative in nature, using a cohort (n = 10), cross-sectional (n = 4), or case-control/case-series (n = 4) design. Other quantitative studies included descriptive analysis (n = 2), retrospective chart review (n = 1), a clustered randomized trial (n = 1), and a randomized controlled trial (n = 1). There was also one qualitative, interpretative phenomenological study, and one mixed-methods study. While we were not interested in intervention studies, the designs utilizing a trial method included follow-up data from an intervention study, rather than the trial itself (12, 54). Cohort designs typically compared participants with PPCS to healthy controls, or to participants with resolved or acute concussion. Some studies also compared PPCS participants who also had a mental health outcome, such as symptoms of depression, to PPCS participants without psychiatric symptoms or diagnoses. Terminology related to PPCS fell under a large umbrella of terms but were based on length of symptom duration criteria; almost all studies referred to PPCS as persistent or long-term post-concussion or post-concussive symptoms or syndrome, in conjunction with concussion; other less common terms were prolonged, protracted, or persistent concussion, as well as persistent symptoms after a concussion.
Outcome Measures
Due to the variety of outcome measures used across studies, between different mental health outcomes, and varying assessments based on age range, the measures used are important to present. Across the six pediatric studies, six different measures were utilized to assess the clinical problem of interest. Anxiety measures included the State-Trait Anxiety Inventory for Children (26, 78), and the Post-Concussion Symptom Scale (55, 79, 89). Depressive symptom measures consisted of the Children's Depression Inventory (57, 80) and the Patient Health Questionnaire-9 (56, 90). Combined symptoms of anxiety and depression studies utilized a semi-structured interview (58) or the Behavior Assessment System for Children, 2nd Edition (59, 91).
Outcome measures utilized for adults were also quite varied across studies. The two anxiety studies utilized two different measures; the anxiety item bank from the Quality of Life in Neurological Disorder Computerized Adaptive Tests (60, 92), and the Hospital and Anxiety Depression Scale (12, 93). The eight adult studies that centered on symptoms of depression utilized the adapted version of the Composite International Diagnostic Interview Screening Scales (61, 88), qualitative interviews (62, 81), the British Columbia Major Depression Inventory, 2nd Edition (63, 82), the Center for Epidemiological Studies Depression Scale (64, 83), the Beck Depression Inventory (65, 66, 68, 94), or the General Health Questionnaire (67, 84). Between the nine adult studies on combined symptoms of anxiety and depression, four used the Hospital Anxiety and Depression Scale (70, 72, 75, 76, 93), while others used the Impact of Event Scale (69, 95), the Rivermead Post-Concussion Symptoms Questionnaire (69, 96), Depression and Anxiety Stress Scales-42 (71, 85), the Beck Anxiety Inventory (73, 86) and Beck Depression Inventory (73, 94), interviews with symptoms according to DSM-IV criteria (74, 87), and the Glasgow Outcome Scale -Extended (77, 97). Finally, the two adult studies that included “other” mental health outcomes, included the Impact of Event Scale (69, 95) and qualitative interviews (62, 81).
Anxiety
Pediatric
Two studies measured anxiety outcomes among children and adolescents with PPCS (26, 55). The first study characterized the psychological factors associated with persistent symptoms following a concussion in pediatric participants (aged 8–18 years old). The second study examined the difference of symptom burden between pediatric participants (aged 10–18 years) with prolonged recovery to those with typical recovery (55). Both studies demonstrated anxiety symptoms were significantly worse among participants with delayed symptom resolution compared to those with early symptom resolution (26, 55). In particular, Schilling et al. (55) demonstrated there was a higher score on the anxiety profile in the prolonged recovery group than the typical recovery group, indicating higher severity and symptom burden.
Adults
Two studies measured anxiety outcomes among adults with PPCS (12, 60). One study (60) tested the strength of the cognitive and behavioral pathways that mediate the relationship between anxiety and post-concussion symptoms among patients with concussion. The other study (12) examined PPCS and anxiety in patients with concussion. Results demonstrate that anxiety could be correlated with PPCS, and in particular, clinically significant anxiety (HADS-anxiety score > 7) was reported by 12.8% and significantly associated with symptom reporting in patients (12).
Depression
Pediatric
Of the six studies that centered around pediatric populations with PPCS, only two studies measured symptoms of depression (56, 57). Overall, both studies reported that increased PPCS symptoms were correlated with increased symptoms of depression, especially closer to the time of the injury. The first study (57) followed pediatric participants (11–17-years-old) with prolonged recovery following sports-related concussion and found that participants with higher symptom severity of PPCS also reported higher symptoms of depression. As well, participants who had higher initial symptoms of depression and PPCS (onset of or increased intensity in three or more post-concussive symptoms for at least 1 month duration following injury) significantly predicted a larger decline in symptoms over time, indicating an improvement in symptoms of depression for these subgroups. The second study (56) measured symptoms of depression in pediatric participants (8–18 years-old) to investigate predictors of developing depression in individuals with persistent concussion symptoms. This study found symptoms of depression in 22% of participants and noted that this group had significantly higher PPCS symptom severity scores than non-depressed participants. Interestingly, the adolescent depression scores increased by a factor of 11 if they also had a hospital admission as a result of concussion.
Adults
Of the 19 studies that centered around adults with PPCS, eight studies measured symptoms of depression (61–68). Like in the pediatric population, most studies found that participants reporting higher PPCS symptoms also reported higher severity of depression symptoms (64, 65, 67, 68, 82). For example, 61% of participants with PPCS reported presence of a depressive disorder, endorsing elevated symptoms using self-reported measures (65). Also noted in two studies, symptoms of depression was present in participants with PPCS, even without including overlapping symptoms between PPCS, PTSD, and depression, such as depressed mood, insomnia, fatigue, irritability, restlessness (65, 67). In a study with a participant group of veterans, it was reported that deployment stress was related to an increase in both PPCS scores and depression scores (61). Furthermore, in a qualitative study conducted with university students, all five participants reported symptoms of depression following PPCS, and one participant described a previous suicide attempt following concussion (62).
Anxiety and Depression
Pediatric
There were two studies that looked at anxiety and depression (58, 59) in the pediatric population. Both studies reported increased symptoms of depression in individuals with PPCS. The first study by Ellis et al. (58) looked at psychiatric diagnoses following a sports-related concussion. Of the pediatric participants (19-years-old or younger), 14 (8.0%) were diagnosed with a novel psychiatric disorder. Two (1.1%) participants reported suicidal ideation and 4 (2.3%) experienced worsening symptoms of a pre-existing psychiatric disorder. Moreover, 10 (52.6%) individuals with novel psychiatric disorder were diagnosed with a depressive disorder, 4 (21.1%) with a new-onset anxiety disorder, and 1 (5.3%) with major depressive disorder and an anxiety disorder. The second study (59) measured the severity of anxiety and depression symptoms in 48 pediatric participants (13–17-years-old), in which those with a history of concussion reported significantly higher anxiety and depression symptoms.
Adults
There were nine included studies that analyzed both anxiety and depression on in an adult sample (69–77). For each of these studies, the severity of both depression and anxiety was measured. There were five studies that reported a higher prevalence of anxiety and depression symptoms in patients who develop PPCS (69, 71, 72, 74, 75). Four studies did not find a significant difference in both outcomes (69, 73, 77, 98). Two studies reported higher depression scores in those with PPCS, however had no significant differences in anxiety scores when compared with the general population (74, 77). Moreover, one study found the prevalence of anxiety and depression symptoms to be comparable to the general population (76). Although Doroszkiewicz et al. (71) found no statistical significance between any variables (i.e., sex, gender, age, and number of concussion) and PPCS, they found that individuals with PPCS reporting higher anxiety and depression symptoms had lower quality of life scores, as measured by the World Health Organization Quality of Life Assessment-BREF (99).
“Other” Mental Health Outcomes
Pediatrics
No studies that met our inclusion criteria examined psychological outcomes beyond symptoms of anxiety and depression in pediatric populations.
Adults
There were two studies that measured other emotional or behavioral outcomes among adults (62, 69). The first study (62) looked at mood swings, heightened emotions, and suicide ideation as mental health outcomes. This study used interpretative phenomenological analysis (81) to explore the experiences of five female university athlete's post-concussion. In several participants, there were more feelings of frustration and changes in mood 1-month post-concussion. One participant reported a suicide attempt and extreme emotional distress (62). The second study (69) characterized the long-term consequences of concussion and post-concussion symptoms in men and women. One of the outcomes included stress reactions, which found that women reported higher scores compared to men. Moderate to severe stress was reported by 10% of men and 14% of women with PPCS.
Discussion
This scoping review reported a total of 25 papers relevant to our question: What are the associations of mental health outcomes and PPCS post-injury and types of assessments used that examine mental health outcomes across the lifespan in individuals with PPCS? Furthermore, we investigated the differences between the six pediatric studies, in comparison to the 19 adult studies. In general, these studies largely focused on symptoms of anxiety and depression with minimal coverage on other emotional outcomes common to PPCS such as stress, irritability, aggression, or frustration. The common trend shown amongst studies was a higher association of symptoms of anxiety, symptoms of depression, or “other” mood disorders in those with higher PPCS scores. While this was not representative of all studies, most studies reported statistical significance of higher psychiatric symptoms correlated with PPCS groups. This was compared to normative data in most studies, but six did include typically developing (n = 5) or orthopedic injury (n = 1) control groups. In pediatric settings, two of the six studies found significantly increased mood symptoms (depression: n = 1, anxiety and depression: n = 1), as compared to normative data or a typically developing control group. This ranged from 22% for depression studies (57) and 11.5% for anxiety and depression studies (58). The remaining four of the six studies did not include results related to prevalence, instead commenting on the significance of relationship between PPCS and mental health outcomes (anxiety: n = 2, depression: n = 1, anxiety and depression: n = 1).
In adult populations, all but one study (n = 18) reported that increased PPCS symptoms related to increased mood symptoms (anxiety: n = 2, depression: n = 8, anxiety and depression: n = 8, “other”: n = 2). Prevalence ranged from as high as 44% of PPCS participants with increased depression symptoms (77), as compared to as high as 24% of PPCS participants with increased anxiety (74). In studies that combined symptoms of anxiety and depression, results were staggering, reporting a prevalence as high as 76% in individuals with PPCS (74). The remaining study (76) concluded no differences between those with PPCS and the general population.
In general, the findings also suggest that research specific to certain PPCS age groups is lacking, noted in both young pediatric and older adult settings. While eligibility criteria were inclusive of all ages, no pediatric participants were younger than 8 years old. Concussions in infants and young children are widely underreported and understudied, even though they are a high-risk incident group (98, 100, 101). Furthermore, only six of the 25 studies focused on children and adolescents. This is of concern as incidence rates of pediatric concussion are increasing, and likely at a higher rate than reported due to under-reporting of concussion by adolescents, parents, and coaches (102, 103). This leads to apprehension about whether these studies are truly representative samples that reflect prevalence in the population. Children and youth are at a critical period where mental health is impressionable and malleable, justifying the need for more pediatric studies. In addition, only one study focused on geriatric populations (72), even though falls are a primary cause of concussion, and common in older adults (104, 105). Furthermore, older adults report more pre-existing cognitive impairments that make it difficult to treat and manage concussion (106), as well literature suggests older adults can experience poor quality of life post-concussion, due to factors such as reduced independence and difficulty in recovery due to comorbidities or frailty (107). As most studies (17/25) focused exclusively on individuals aged 19–60 years old, there is a need to conduct more studies that target pediatric and older adult populations in these critical life stages.
Furthermore, most papers measured symptoms of depression (10/25), or symptoms of anxiety and depression together (10/25). Upon analysis of findings, there was a clear distinction between symptoms of anxiety, symptoms of depression, and what we categorized as “other” mental health outcomes. Results demonstrate fewer papers on anxiety and PPCS. Hence, future research should focus on anxiety-based outcomes since it is highly reported in adolescents and adults with PPCS (104). As there is ambiguity among distinguishable features of PPCS and mental health disorders such as symptoms of anxiety and depression, further interest on anxiety onset post-concussion is also necessary to help identify mental health outcomes as potential diagnostic symptoms of PPCS. Additionally, almost no studies investigated mental health outcomes or symptoms other than depression and anxiety. Emotional symptoms such as stress, irritability, and aggression were reported in adolescents and adults with PPCS (108). The Rivermead Post-Concussion Symptoms Questionnaire, a commonly used diagnostic assessment for PPCS, includes mood disturbances such as irritability and frustration, despite minimal literature and investigation on these symptoms in adolescents and adults (97, 109). Thus, more research is needed in this area to understand the impact of mood disturbances beyond depression and anxiety following PPCS. Related, the reporting of PPCS itself may include symptom overlap with mental health outcomes like depression, such as fatigue, low mood, and irritability (110). Few studies made distinctions between defining features of depression that overlap less with PPCS, and is important to consider in future studies moving forward.
In addition, only a small number of studies included prior mental health diagnosis and/or family history in their demographic information and/or analyses. Causal associations of mental health in those with concussion and PPCS, including symptoms of anxiety and depression, remain arguable and inconclusive. Many studies show evidence of an increase in the severity of mental health symptoms in those with PPCS, emphasized and exacerbated if those individuals had pre-existing psychiatric symptoms prior to injury (68, 111). Family and personal psychiatric history are of notable causal interest of PPCS symptoms as a retrospective cohort study of concussed high school athletes were 5 times more likely to develop PPCS with family or personal pre-existing psychiatric symptoms (31). Strikingly, a study by Iverson (110) found that ~9 out of 10 individuals diagnosed with depression met self-report criteria for PPCS, without concussion history. Not only do studies suggest mental health history may play a contributing role in severity of PPCS, but multiple conditions could be a factor, including chronic pain (112) and cerebrovascular injuries (113). Contrastingly, other studies support findings of presence of mental health symptoms post-concussion, in those without any prior history of mental health (68, 77, 83, 114). While documentation of prior mental health history was not a requirement for study inclusion, it does provide insightful knowledge on the question of causality of prolonged emotional and behavioral symptoms of PPCS for future studies.
The number of methods, measures, control groups, and samples sizes used to assess both mental health outcomes and PPCS criteria in individuals was extremely diverse. In fact, there were four pediatric-specific measures and twenty measures inclusive of adult and/or pediatric populations used to capture mood throughout the reviewed studies. The impact of method heterogeneity is two-fold: diversity can create more avenues to explore factors related to mental health outcomes that may otherwise be overlooked but can also create a lack of consistency in assessments, leading to inconclusiveness and skepticism of study quality. Additionally, broad differences amongst study designs, control groups, and sample sizes augment the conversation regarding variables that can create discrepant results amongst studies and impact subsequent findings. These findings of heterogeneity supports the call for common data elements in TBI research, such as those outlined by the National Institute of Neurological Disorders and Stroke, which aims to standardize and unify data collection studies related to TBI to increase efficiency and efficacy (115, 116).
Almost all studies used quantitative designs such as observational cohort, case-control studies, or randomized trials. Only one included study used a qualitative design to document the thoughts and feelings of university-aged students suffering from PPCS (81). Using in-depth semi-structured interviews, findings reported on extremely personal details, such as suicidal ideation and attempts post-injury. Incorporating qualitative and mixed methods for data collection could offer in-depth narratives and complex emotions that quantitative studies fail to capture. Qualitative studies on lived experiences following PPCS exist to broadly magnify quality of life rather than emotional and social domains (117, 118), and literature on emotional and social aspects of PPCS are beginning to emerge slowly. For example, a study by Davies et al. (51) was published recently on the emotional and social burden of persistent concussion. To note, while this study reported looking at persistent concussion, they did not specify the duration of symptoms. Thus, it did not fit eligibility criteria.
Finally, our definition of PPCS was created based on the current literature. However, there are varying definitions of PPCS, and ambiguity of criteria exists around included symptoms and severity, duration of symptoms, and diagnostic tools. Current definitions of PPCS are not specific to concussion (119). There are several explanations for the heterogeneity in PPCS definitions, one of which was most recently applied to the predisposing, precipitating, and perpetuating (PPP) model. The PPP model proposes that factors contributing to the course and development of PPCS are individualistic, and must consider personal attributions (120). While it is understandable that PPCS duration and symptoms are variable due to individual and personal factors, it does not make it easier to form a consensus on definitions and criteria, or to gather all pertinent literature on the subject matter. The most recent uniform definition for PPCS emerged from experts using the Delphi Method, which was created on the basis of three criteria: (1) symptoms must occur within hours of concussion, and continue for a minimum of 3 months consistently; (2) must not be symptoms present from a pre-existing condition, and (3) impacts at least one domain of everyday life (15). This Delphi study could suggest that a central body should try to create unity on this matter. Reference to these new studies is important as it speaks to the rapidly evolving nature of the concussion literature and interest in persistent presentations more broadly.
The natural progression of this review prompts a systematic review, to assess the diversity of study methods and designs, and to provide an overview of study quality and critical appraisal. Study evaluation will lead to greater understanding about what kinds of methods produce reliable and rigorous results, while also addressing designs that have the potential to produce meaningful results and could be employed further. Future meta-analysis is warranted to rigorously examine the strength of evidence provided in these studies, to comment on value, purpose, and effectiveness of the outcome assessments, study designs and methodologies.
Strengths and Limitations
There are both strengths and limitations to the study processes that should be reflected on to improve future review processes. Chosen exclusion criteria may have limited relevant studies included in this review, as we chose to narrow our search to the English language (and translations), as well as limit the time frame to studies occurring in or after 1995. Furthermore, our choice of definition for PPCS may not have truly captured the varying terminology used across previously published literature, due to the inconclusiveness of the definition itself. Therefore, it is possible there are important studies missing. In addition, restricting the terms for mental health outcomes could have also decreased results, as we chose to focus on mood disturbances related to mental health disorders and PPCS, but did not specifically include many disorders themselves.
One strength of this study was having three reviewers engaged in all stages of the review process and having weekly meetings for transparency and constant communication. This added to the reliability of study results, as three people completed screening (title and abstract, and full text), charting the data, and analysis of findings. While this lengthened the duration of each step of the review, it strengthened the integrity of the studies chosen and reviewed. Furthermore, our study included literature from four established databases that created a broad and diverse landscape for possible studies included, from medical, psychological, and international sources.
Implications
The findings of this study highlight the importance of interdisciplinary care for individuals with PPCS. Along with the cognitive and somatic symptoms that individuals may experience, symptoms such as anxiety and depression can be common. Moreover, the prevalence of anxiety and depression symptoms suggests that access to mental health interventions are important for individuals experiencing PPCS (58, 65, 70, 74). Thus, a biopsychosocial and holistic approach that addresses both physical and mental health needs should be emphasized in clinic and research settings (121). The complexities of PPCS warrant multiple healthcare professionals to provide specialized care that can encompass the range of symptoms they can experience—physically, mentally, and emotionally. The emotional burden associated with PPCS may also come with economic consequences. For example, the additional healthcare costs from mental health interventions may be a financial burden at the individual and population levels (122, 123).
This scoping review describes the various mental health outcomes that may emerge in those with PPCS. However, individuals with PPCS form a diverse group with different demographic characteristics (124) and mental health outcomes may differ based on these variables. For example, female sex is associated with greater frequency of PPCS (125). Further exploration of differences based on sex may serve as a prognostic indicator of poor mental health in this group. Future studies should also look at other socio-demographic variables that may predict mental health outcomes in this population. Psycho-social factors such as social support and family dynamics have been associated with PPCS frequency (126, 127), however, their contribution to mental health should be more closely examined. In addition, demographics of pre-existing personal and family mental health history should be carefully considered when designing, conducting, and analyzing studies. Given the diverse findings regarding PPCS and mental health outcomes, with both pre-existing mental health history and lack thereof reporting increase in psychiatric symptoms, there is a need to conduct further research exploration in this evolving area. This study included a review of the associations of mental health outcomes in individuals with PPCS and types of assessments used to capture these outcomes. This allowed us to survey different ways that mental health was assessed.
For many studies in this scoping review, PPCS is associated with an increased incidence of symptoms anxiety, symptoms of depression, and related mental health problems. However, the magnitude of this association is unknown. Since there appears to be a risk for mental health concerns after concussion, future research should quantify the strength of this relationship in those with PPCS. Obtaining prevalence estimates of anxiety and depressive disorders in those with PPCS may inform healthcare providers on the extent of this problem (24) and can support the development of optimal care strategies and pathways.
Conclusion
Mental health outcomes are a primary concern following concussion especially in individuals experiencing persistent symptoms post-injury. Of particular interest, pediatric (or adolescent) and adult populations with PPCS exhibit symptoms of depression and anxiety. Furthermore, there is evidence to suggest that mood difficulties such as frustration, irritability, stress, attention, and worry can arise as a result of PPCS. However, minimal research has focused on this area. Both adolescents and adults suffer from PPCS, but literature on adolescents appears to be lacking compared to adults.
This scoping review highlights the existence of mental health outcomes following PPCS. It also outlines the need for further research in this area. For example, greater clarity and advancements should be made to reach a universal definition of PPCS. Also, it is important to investigate prevalence estimates in emotional and behavioral symptomatology among adolescents and adults with PPCS, with the lack of findings present. Emphasis should be directed toward studies involving children and adolescents, who are at a vulnerable age for cognitive, behavioral, and emotional development. As concussion becomes increasingly more common, it is important to advance clarity and insight for those experiencing prolonged and challenging symptoms.
Author Contributions
ES and SS conceived the main idea and objectives of the review. ES, HA-H, and BL carried out all review steps, including search query, screening, analysis, charting of the data, and wrote the manuscript, with support from BG, AW, MB, BD, NR, and SS. NR and SS supervised the project. All authors provided critical feedback of drafts and contributed to the final version of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
This work was supported by The Azrieli Foundation and The Holland Family Professorship in Acquired Brain Injury, held by SS, which is a joint Hospital-University Named Chair between the University of Toronto, Holland Bloorview Rehabilitation Hospital, and Holland Bloorview Rehabilitation Hospital Foundation. We would like to acknowledge the efforts of the members of the NOvEL Lab Team (Bloorview Research Institute), specifically Andrea Hicking. This scoping review would not have been possible without the expansive knowledge of database search queries, of Erica Nekolaichuk, the Faculty Liaison and Instruction Librarian at Gerstein Library at the University of Toronto. Her dedicated help, care, patience, and thoughtfulness were greatly appreciated, and the authors were extremely grateful for the time and expertise she invested.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2022.850590/full#supplementary-material
References
1. Beidler E, Wallace J, Alghwiri AA, O'Connor S. Collegiate Athletes' concussion awareness, understanding, and reporting behaviors in different countries with varying concussion publicity. J Athl Train. (2021) 56:77–84. doi: 10.4085/1062-6050-0575.19
2. Comper P, Hutchison M, Richards D, Mainwaring L. A model of current best practice for managing concussion in University Athletes: the University of Toronto approach. J Clin Sport Psychol. (2012) 6:231–46. doi: 10.1123/jcsp.6.3.231
3. Laker SR. Epidemiology of concussion and mild traumatic brain injury. Am Acad Phys Med Rehab. (2011) 3:S354–S8. doi: 10.1016/j.pmrj.2011.07.017
4. Macpherson A, Fridman L, Scolnik M, Corallo A, Guttmann A. A population-based study of Paediatric Emergency Department and Office Visits for Concussions from 2003 to 2010. Pediatr Child Health. (2014) 19:543–6. doi: 10.1093/pch/19.10.543
5. Vos PE, Alekseenko Y, Battistin L, Ehler E, Gerstenbrand F, Muresanu D, et al. Mild traumatic brain injury. Euro J Neurol. (2012) 19:191–8. doi: 10.1111/j.1468-1331.2011.03581.x
6. McCrory P, Meeuwisse W, Dvorak J, Aubry M, Bailes J, Broglio S, et al. Consensus statement on concussion in sport-the 5th International Conference on Concussion in Sport Held in Berlin, October 2016. Br J Sports Med. (2017) 51:838–47. doi: 10.1136/bjsports-2017-097699
7. Kay T, Newman B, Cavallo M, Ezrachi O, Resnick M. Toward a neuropsychological model of functional disability after mild traumatic brain injury. Neuropsychology. (1992) 6:371–84. doi: 10.1037/0894-4105.6.4.371
8. Bernstein DM. Recovery from mild head injury. Brain Inj. (1999) 13:151–72. doi: 10.1080/026990599121683
9. Howell D, Osternig L, Van Donkelaar P, Mayr U, Chou LS. Effects of concussion on attention and executive function in adolescents. Med Sci Sports Exerc. (2013) 45:1030–7. doi: 10.1249/MSS.0b013e3182814595
10. Emanuelson I, Andersson Holmkvist E, Björklund R, Stålhammar D. Quality of life and post-concussion symptoms in adults after mild traumatic brain injury: a population-based study in Western Sweden. Acta Neurol Scand. (2003) 108:332–8. doi: 10.1034/j.1600-0404.2003.00155.x
11. Mercier LJ, Fung TS, Harris AD, Dukelow SP, Debert CT. Improving symptom burden in adults with persistent post-concussive symptoms: a randomized aerobic exercise trial protocol. BMC Neurol. (2020) 20:46. doi: 10.1186/s12883-020-1622-x
12. Ponsford J, Nguyen S, Downing M, Bosch M, McKenzie JE, Turner S, et al. Factors associated with persistent post-concussion symptoms following mild traumatic brain injury in adults. J Rehabil Med. (2019) 51:32–9. doi: 10.2340/16501977-2492
13. Zemek RL, Grool AM, Rodriguez DD, DeMatteo C, Rothman L, Benchimol B, et al. Annual and seasonal trends in ambulatory visits for pediatric concussion in ontario between 2003 and 2013. J Pediatr. (2017) 181:222–8. doi: 10.1016/j.jpeds.2016.10.067
14. Ponsford J, Willmott C, Rothwell A, Cameron P, Kelly AM, Nelms R, et al. Factors influencing outcome following mild traumatic brain injury in adults. J Int Neuropsychol Soc. (2000) 6:568–79. doi: 10.1017/S1355617700655066
15. Carroll L, Cassidy JD, Peloso P, Borg J, von Holst H, Holm L, et al. Prognosis for mild traumatic brain injury: results of the WHO collaborating centre task force on mild traumatic brain injury. J Rehabil Med. (2004) 36:84–105. doi: 10.1080/16501960410023859
16. Marshall S, Bayley M, McCullagh S, Velikonja D, Berrigan L. Clinical practice guidelines for mild traumatic brain injury and persistent symptoms. Can Fam Physician. (2012) 58:257–67, e128–e40.
17. Barlow KM. Postconcussion syndrome: a review. J Child Neurol. (2016) 31:57–67. doi: 10.1177/0883073814543305
18. Lagacé-Legendre C, Boucher V, Robert S, Tardif P-A, Ouellet M-C, de Guise E, et al. Persistent postconcussion symptoms: an expert consensus-based definition using the delphi method. J Head Trauma Rehabil. (2020) 36:96–102. doi: 10.1097/HTR.0000000000000613
19. Daneshvar DH, Riley DO, Nowinski CJ, Mckee AC, Stern RA, Cantu RC. Long-term consequences: effects on normal development profile after concussion. Phys Med Rehabil Clin N Am. (2011) 22:683–700. doi: 10.1016/j.pmr.2011.08.009
20. Halstead ME Walter KD The The council on sports medicine and fitness. Sport-related concussion in children and adolescents. Am Acad Pediatr. (2010) 126:597–615. doi: 10.1542/peds.2010-2005
21. Novak Z, Aglipay M, Barrowman N, Yeates KO, Beauchamp MH, Gravel J, et al. Association of persistent post-concussion symptoms with pediatric quality of life. JAMA Pediatr. (2016) 170:e162900. doi: 10.1001/jamapediatrics.2016.2900
22. Fralick M, Sy E, Hassan A, Burke MJ, Mostofksy E, Karsies T. Association of concussion with the risk of suicide: a systematic review and meta-analysis. JAMA Neurol. (2019) 76:144–51. doi: 10.1001/jamaneurol.2018.3487
23. Hellewell SC, Beaton CS, Welton T, Grieve SM. Characterizing the risk of depression following mild traumatic brain injury: a meta-analysis of the literature comparing chronic mTBI to non-mTBI populations. Front Neurol. (2020) 11:350. doi: 10.3389/fneur.2020.00350
24. Scholten AC, Haagsma JA, Cnossen MC, Olff M, van Beeck EF, Polinder S. Prevalence of and risk factors for anxiety and depressive disorders after traumatic brain injury: a systematic review. J Neurotrauma. (2016) 33:1969–94. doi: 10.1089/neu.2015.4252
25. Yang MN, Clements-Nolle K, Parrish B, Yang W. Adolescent concussion and mental health outcomes: a population-based study. Am J Health Behav. (2019) 43:258–65. doi: 10.5993/AJHB.43.2.3
26. Grubenhoff JA, Currie D, Comstock RD, Juarez-Colunga E, Bajaj L, Kirkwood MW. Psychological factors associated with delayed symptom resolution in children with concussion. J Pediatr. (2016) 174:27–32. doi: 10.1016/j.jpeds.2016.03.027
27. Whelan-Goodinson R, Ponsford J, Johnston L, Grant F. Psychiatric disorders following traumatic brain injury: their nature and frequency. J Head Trauma Rehabil. (2009) 24:324–32. doi: 10.1097/HTR.0b013e3181a712aa
28. Max JE, Smith WL, Sato Y, Mattheis PJ, Castillo CS, Lindgren SD, et al. Traumatic brain injury in children and adolescents: psychiatric disorders in the first three months. J Am Acad Child Adolesc Psychiatry. (1997) 36:94–102. doi: 10.1097/00004583-199701000-00022
29. Polinder S, Cnossen MC, Real RGL, Covic A, Gorbunova A, Voormolen DC, et al. A multidimensional approach to post-concussion symptoms in mild traumatic brain injury. Front Neurol. (2018) 9:1113. doi: 10.3389/fneur.2018.01113
30. Auclair-Pilote J, Lalande D, Tinawi S, Feyz M, de Guise E. Satisfaction of basic psychological needs following a mild traumatic brain injury and relationships with post-concussion symptoms, anxiety, and depression. Disabil Rehabil. (2021) 43:507–15. doi: 10.1080/09638288.2019.1630858
31. Legarreta AD, Brett BA, Solomon GS, Zuckerman SL. The role of family and personal psychiatric history in postconcussion syndrome following sport-related concussion: a story of compounding risk. J Neurosurg Pediatr. (2018) 22:238–43. doi: 10.3171/2018.3.PEDS1850
32. Silver JM. Neuropsychiatry of persistent symptoms after concussion. Psychiatr Clin N Am. (2014) 37:91–102. doi: 10.1016/j.psc.2013.11.001
33. Rice SM, Parker AG, Rosenbaum S, Bailey A, Mawren D, Purcell R. Sport-related concussion and mental health outcomes in elite athletes: a systematic review. Sports Med. (2018) 48:447–65. doi: 10.1007/s40279-017-0810-3
34. Finkbeiner NW, Max JE, Longman S, Debert C. Knowing what we don't know: long-term psychiatric outcomes following adult concussion in sports. Can J Psychiatry. (2016) 61:270–6. doi: 10.1177/0706743716644953
35. Gouttebarge V, Kerkhoffs GMMJ. Sports career-related concussion and mental health symptoms in former elite athletes. Neurochirurgie. (2021) 67:280–2. doi: 10.1016/j.neuchi.2020.01.001
36. Reardon CL. Psychiatric manifestations of sport-related concussion. Curr Psychiatry. (2020) 19:23–8. doi: 10.12788/cp.0010
37. Hunt AW, Agnihotri S, Sack L, Tint A, Greenspoon D, Gauvin-Lepage J, et al. Mood-related changes in children and adolescents with persistent concussion symptoms following a six-week active rehabilitation program. Brain Inj. (2020) 34:1068–73. doi: 10.1080/02699052.2020.1776396
38. Stilling J, Paxman E, Mercier L, Gan LS, Wang M, Amoozegar F, et al. Treatment of persistent post-traumatic headache and post-concussion symptoms using repetitive transcranial magnetic stimulation: a pilot, double-blind, randomized controlled trial. J Neurotrauma. (2020) 37:312–23. doi: 10.1089/neu.2019.6692
39. Tomfohr-Madsen L, Madsen J, Bonneville D, Virani S, Plourde V, Barlow KM, et al. A pilot randomized controlled trial of cognitive-behavioural therapy for insomnia in adolescents with persistent post-concussion symptoms. J Head Trauma Rehabil. (2020) 35:e103–e12. doi: 10.1097/HTR.0000000000000504
40. Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci. (2010) 5:1–9. doi: 10.1186/1748-5908-5-69
41. Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. (2018) 18:143. doi: 10.1186/s12874-018-0611-x
42. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8:19–32. doi: 10.1080/1364557032000119616
43. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169:467–73. doi: 10.7326/M18-0850
44. Eisenberg MA, Meehan WP, Mannix R. Duration and course of post-concussive symptoms. Pediatrics. (2014) 133:999–1006. doi: 10.1542/peds.2014-0158
45. Rose SC, Fischer AN, Heyer GL. How long is too long? The lack of consensus regarding the post-concussion syndrome diagnosis. Brain Inj. (2015) 29:798–803. doi: 10.3109/02699052.2015.1004756
46. World Health Organization. Adolescent Health. Available online at: https://www.who.int/southeastasia/health-topics/adolescent-health (accessed February 21, 2021).
47. Rose SC, Weber KD, Collen JB, Heyer GL. The diagnosis and management of concussion in children and adolescents. Ped Neurol. (2015) 53:108–18. doi: 10.1016/j.pediatrneurol.2015.04.003
48. Sady MD, Vaughan CG J, Gioia GA. Psychometric characteristics of the postconcussion symptom inventory in children and adolescents. Arch Clin Neuropsychol. (2014) 29:348–63. doi: 10.1093/arclin/acu014
49. Kontos AP, Elbin RJ, Schatz P, Covassin T, Henry L, Pardini J, et al. A revised factor structure for the post-concussion symptom scale: baseline and postconcussion factors. Am J Sports Med. (2012) 40:2375–84. doi: 10.1177/0363546512455400
50. The Concussion in Sport Group. Sport concussion assessment tool. Br J Sports Med. (2017) 51:851–8.
51. Davies SC, Bernstein ER, Daprano CM. A qualitative inquiry of social and emotional support for students with persistent concussion symptoms. J Ed Psychol Consult. (2020) 30:156–82. doi: 10.1080/10474412.2019.1649598
52. McKinlay A, Grace RC, Horwood LJ, Fergusson DM, MacFarlane MR. Long-term behavioural outcomes of pre-school mild traumatic brain injury. Child Care Health Dev. (2009) 36:22–30. doi: 10.1111/j.1365-2214.2009.00947.x
53. Taylor HG, Orchinik LJ, Minich N, Dietrich A, Nuss K, Wright M, et al. Symptoms of persistent behaviour problems in children with mild traumatic brain injury. J Head Trauma Rehabil. (2015) 30:302–10. doi: 10.1097/HTR.0000000000000106
54. Alexander MP. Mild traumatic brain injury: pathophysiology, natural history, and clinical management. Neurology. (1995) 45:1253–60. doi: 10.1212/WNL.45.7.1253
55. Schilling S, Mansour A, Sullivan L, Ding K, Pommering T, Yang J. Symptom burden and profiles in concussed children with and without prolonged recovery. Int J Env Res Public Health. (2020) 17:351. doi: 10.3390/ijerph17010351
56. Stazyk K, DeMatteo C, Moll S, Missiuna C. Depression in youth recovering from concussion: correlates and predictors. Brain Inj. (2017) 31:631–8. doi: 10.1080/02699052.2017.1283533
57. Stein E, Howard W, Rowhani-Rowbar A, Rivara FP, Zatzick D, McCarty CA. Longitudinal trajectories of post-concussive and depressive symptoms in adolescents with prolonged recovery from concussion. Brain Inj. (2017) 31:1736–44. doi: 10.1080/02699052.2017.1380843
58. Ellis MJ, Ritchie LJ, Koltek M, Hosain S, Cordingley D, Chu S, et al. Psychiatric outcomes after pediatric sports-related concussion. J Neurosurg Pediatr. (2015) 16:709–18. doi: 10.3171/2015.5.PEDS15220
59. Rieger B, Lewandowski L, Potts H, Shea N. Effects of concussion in adolescent students: perceptions and performance. J Int Neuropsychol Soc. (2019) 25:777–86. doi: 10.1017/S1355617719000468
60. Greenburg J, Mace RA, Funes CJ, Silverberg ND, Iverson GL, Caplan DN, et al. Pain catastrophizing and limiting behavior mediate the association between anxiety and postconcussion symptoms. Psychosomatics. (2020) 61:49–55. doi: 10.1016/j.psym.2019.09.004
61. Agtarap S, Campbell-Sills L, Thomas ML, Kessler RC, Ursano RJ, Stein MB. Postconcussive, posttraumatic stress and depressive symptoms in recently deployed U.S. Army Soldiers with traumatic brain injury. Psychol Assess. (2019) 31:1340–56. doi: 10.1037/pas0000756
62. Andr-Morin D, Caron JG, Bloom GA. Exploring the unique challenges faced by female university athletes experiencing prolonged concussion symptoms. Sport Exerc Perform Psychol. (2017) 6:289–303. doi: 10.1037/spy0000106
63. Lange RT, Iverson G, Rose A. Depression strongly influences postconcussion symptom reporting following mild traumatic brain injury. J Head Trauma Rehabil. (2011) 26:127–37. doi: 10.1097/HTR.0b013e3181e4622a
64. Maruta J, Spielman LA, Yarusi BB, Wang Y, Silver JM, Ghajar J. Chronic post-concussion neurocognitive deficits. II. Relationship with persistent symptoms. Front Hum Neurosci. (2016) 10:45. doi: 10.3389/fnhum.2016.00045
65. Mooney G, Speed J, Sheppard S. Factors related to recovery after mild traumatic brain injury. Brain Inj. (2005) 19:975–87. doi: 10.1080/02699050500110264
66. Morissette SB, Woodward M, Kimbrel NA, Meyer EC, Kruse MI, Dolan S, et al. Deployment-related TBI, persistent postconcussive symptoms, PTSD, and depression in OEF/OIF veterans. Rehabil Psychol. (2011) 6:340–50. doi: 10.1037/a0025462
67. Rapoport MJ, McCullagh S, Streiner D, Feinstein A. The clinical significance of major depression following mild traumatic brain injury. Psychosomatics. (2003) 44:31–7. doi: 10.1176/appi.psy.44.1.31
68. Waljas M, Iverson GL, Lange RT, Hakulinen U, Dastidar P, Huhtala H, et al. A prospective biopsychosocial study of the persistent post-concussion symptoms following mild traumatic brain injury. J Neurotrauma. (2015) 32:534–47. doi: 10.1089/neu.2014.3339
69. Ahman S, Saveman B-I, Skyrke J, Bjornstig U, Stalnacke B-M. Long-term follow-up of patients with mild traumatic brain injury: a mixed methods study. J Rehabil Med. (2013) 45:758–64. doi: 10.2340/16501977-1182
70. Donnell AJ, Kim MS, Silva MA, Vanderploeg RD. Incidence of postconcussion symptoms in psychiatric diagnostic groups, mild traumatic brain injury, and comorbid conditions. Clin Neuropsychol. (2012) 26:1092–101. doi: 10.1080/13854046.2012.713984
71. Doroszkiewicz C, Gold D, Green R, Tartaglia RC, Ma J, Tator CH. Anxiety, depression, and quality of life: a long-term follow-up study of patients with persisting concussion symptoms. J Neurotrauma. (2021) 38:493–505. doi: 10.1089/neu.2020.7313
72. Eman Abdulle A, van der Naalt J. The role of mood, post-traumatic stress, post-concussive symptoms and coping on outcome after MTBI in elderly patients. Int Rev Psychiatry. (2020) 32:3–11. doi: 10.1080/09540261.2019.1664421
73. Lange RT, Panenka WJ, Shewchuk JR, Heran MKS, Brubacher JR, et al. Diffusion tensor imaging findings and postconcussion symptom reporting six weeks following mild traumatic brain injury. Arch Clin Neuropsychol. (2015) 30:7–25. doi: 10.1093/arclin/acu060
74. Mooney G, Speed J. The association between mild traumatic brain injury and psychiatric conditions. Brain Inj. (2001) 15:865–77. doi: 10.1080/02699050110065286
75. Oldenburg C, Lundin A, Edman G, Deboussard CN, Bartfai A. Emotional reserve and prolonged post-concussive symptoms and disability: a Swedish prospective 1-year mild traumatic brain injury cohort study. BMJ Open. (2018) 8:e020884. doi: 10.1136/bmjopen-2017-020884
76. Theadom A, Parag V, Dowel T, McPherson K, Starkey N, Barker-Collo S, et al. Persistent problems one year after mild traumatic brain injury: a longitudinal population study in New Zealand. Br J Gen Pract. (2016) 66:16–23. doi: 10.3399/bjgp16X683161
77. Yang C-C, Tu Y-K, Hua M-S, Huang S-J. The association between the postconcussion symptoms and clinical outcomes for patients with mild traumatic brain injury. J Trauma. (2007) 62:657–63. doi: 10.1097/01.ta.0000203577.68764.b8
78. Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory (Form Y). Palo Alto, CA: Consulting Psychologists Press (1983).
79. Kontos AP, Sufrinko A, Sandel N, Emami K, Collins MW. Sport-related concussion clinical profiles: clinical characteristics, targeted treatments, and preliminary evidence. Curr Sports Med Rep. (2019) 18:82–92. doi: 10.1249/JSR.0000000000000573
80. Kovacs M. Children's depression inventory (CDI and CDI 2). In: Cautin RL, Lilienfeld SO, editors. The Encyclopedia of Clinical Psychology. Hoboken, NJ: Wiley & Sons (2014).
81. Smith JA, Flowers P, Larkin M. Interpretative Phenomenological Analysis: Theory, Method, and Research. Thousand Oaks, CA: Sage (2009).
82. Iverson GL, Remick R. Diagnostic accuracy of the British Columbia major depression inventory. Psychol Rep. (2004) 95:1241–7. doi: 10.2466/pr0.95.3f.1241-1247
83. Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. (1977) 1:385–401. doi: 10.1177/014662167700100306
84. Goldberg D, Hillier VF. A scaled version of the general health questionnaire. Psychol Med. (1979) 9:139–45. doi: 10.1017/S0033291700021644
85. Lovibond SH, Lobvibond PF. Manual for the Depression and Anxiety Stress Scales, 2nd Edn. Sydney: Psychology Foundation (1995).
86. Beck AT, Epstein N, Brown GK, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psych. (1988) 56:893–7. doi: 10.1037/0022-006X.56.6.893
87. First MB. Structured Clinical Interview for the DSM-IV Axis I Disorders: SCID-I/P, Version 2.0. New York, NY: Biometrics Research Department, New York State Psychiatric Institute (1997).
88. Kessler RC, Calabrese JR, Farley P, Gruber MJ, Jewell MA, Katon W, et al. Composite international diagnostic interview screening scales for DSM-IV anxiety and mood disorders. Psychol Med. (2013) 43:1625–37. doi: 10.1017/S0033291712002334
89. Lovell MR, Iverson GL, Collins MW, Podell K, Johnston KM, Pardini D, et al. Measurement of symptoms following sports-related concussion: reliablility and normative data for the post-concussion scale. Appl Neuropsychol. (2006) 13:166–74. doi: 10.1207/s15324826an1303_4
90. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Internal Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
91. Reynolds CR, Kamphaus RW, Vannest KJ. Behavior assessment system for children (BASC). In: Kreutzer JS, DeLuca J, Caplan B, editors. Encyclopedia of Clinical Neuropsychology. New York, NY: Springer, (2011). p. 366–371.
92. Gershon RC, Lai JS, Bode R, Choi S, Moy C, Bleck T, et al. Neuro-QoL: quality of life item banks for adults with neurological disorders: item development and calibrations based upon clinical and general population testing. Qual Life Res. (2012) 21:475–86. doi: 10.1007/s11136-011-9958-8
93. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. (1983) 67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x
94. Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation (1996).
95. Weiss DS, Marmar CR. The impact of event scale - revised. In: Wilson J, Keane TM, editors. Assessing Psychological Trauma PTSD. New York, NY: Guilford (1996). p. 399–411.
96. King NS, Crawford S, Wenden FJ, Moss NEG, Wade DT. The rivermead post concussion symptoms questionnaire: a measure of symptoms commonly experienced after head injury and its reliability. J Neurol. (1995) 242:587–92. doi: 10.1007/BF00868811
97. Pettigrew LE, Teasdale GM, Wilson JT. Assessing disability after head injury: improved use of the Glasgow Outcome Scale. J Neurosurg. (1998) 89:939–43. doi: 10.3171/jns.1998.89.6.0939
98. Bodin D, Yeates KO, Klamar K. Definition and classification of concussion. In: Niskala Apps J, Walter KD, editors. Pediatric and Adolescent Concussion: Diagnosis, Management, and Outcomes. New York, NY: SpringerLink (2012). p. 9–20.
99. World Health Organization Division Division of Mental Health. WHOQOL-BREF: Introduction, Administration, Scoring, and Generic Version of the Assessment: Field Trial Version. (1996). Available online at: https://www.apps.who.int/iris/handle/10665/63529 (accessed December 29, 2020).
100. McKinlay A, Grace RC, Horwood LJ, Fergusson DM, Ridder EM, MacFarlane MR. Prevalence of traumatic brain injury among children, adolescents and young adults: evidence from a birth cohort. Brain Inj. (2008) 22:175–81. doi: 10.1080/02699050801888824
101. Myhre MC, Grogaard JB, Dyb GA, Sandvik L, Nordhov M. Traumatic head injury in infants and toddlers. Acta Paediatr. (2007) 96:1159–63. doi: 10.1111/j.1651-2227.2007.00356.x
102. Manzanero S, Elkington LJ, Praet SF, Lovell G, Waddington G, Hughes DC. Post-concussion recovery in children and adolescents: a narrative review. J Concussion. (2017) 1:1–8. doi: 10.1177/2059700217726874
103. Zhang AL, Sing DC, Rugg CM, Feeley BT, Senter C. The rise of concussions in the adolescent population. Orthop J Sports Med. (2016) 4:1–7. doi: 10.1177/2325967116S00200
104. Papa L, Mendes ME, Braga CF. Mild traumatic brain injury among the geriatric population. Curr Trans Geriatr Experl Gerontol Rep. (2012) 1:135–42. doi: 10.1007/s13670-012-0019-0
105. Thompson HJ, McCormick WC, Kagan SH. Traumatic brain injury in older adults: epidemiology, outcomes, and future implications. J Am Geriatr Soc. (2006) 54:1590–5. doi: 10.1111/j.1532-5415.2006.00894.x
106. Mercier E, Mitra B. Challenges in assessment of the mild traumatic brain injured geriatric patient. Int J Care Injured. (2016) 47:985–7. doi: 10.1016/j.injury.2016.04.001
107. McCulloch KL, Osborne MA, Ramsey CR. Geriatric mild traumatic brain injury (mTBI). Curr Geriatr Rep. (2020) 9:142–53. doi: 10.1007/s13670-020-00329-3
108. Han DY, Combs HL, Koehl L, Camargo FC, Mattacola CG. Irritability and aggression in persistent youth concussions. Br J Sports Med. (2017) 5:e1.
109. McLean SA, Kirsch NL, Tan-Schriner CU, Sen A, Frederiksen S, Harris RE, et al. Health status, not head injury, predicts concussion symptoms after minor injury. Am J Emerg Med. (2009) 27:182–90. doi: 10.1016/j.ajem.2008.01.054
110. Iverson G. Misdiagnosis of the persistent postconcussion syndrome in patients with depression. Arch Clin Neuropsychol. (2006) 21:303–10. doi: 10.1016/j.acn.2005.12.008
111. Booker J, Sinha S, Choudhari K, Dawson J, Singh R. Description of the predictors of persistent post-concussion symptoms and disability after mild traumatic brain injury: the SHEFBIT cohort. Br J Neurosurg. (2019) 33:367–75. doi: 10.1080/02688697.2019.1598542
112. Snell DL, Martin R, Macleod AD, Surgenor LJ, Siegert RJ, Hay-Smith EJC, et al. Untangling chronic pain and post-concussion symptoms: the significance of depression. Brain Inj. (2018) 32:583–92. doi: 10.1080/02699052.2018.1432894
113. Leddy JJ, Baker JG, Merchant A, Picano J, Gaile D, Matusak J, et al. Brain or strain? Symptoms alone do not distinguish physiologic concussion from cervical/vestibular injury. Clin J Sports Med. (2015) 25:237–42. doi: 10.1097/JSM.0000000000000128
114. Mehrolhassani N, Movahedi M, Nazemi-Rafi M, Mirafzal A. Persistence of post-concussion symptoms in patients with mild traumatic brain injury and no psychiatric history in the Emergency Department. Brain Inj. (2020) 34:1350–7. doi: 10.1080/02699052.2020.1802659
115. Broglio SP, Kontos AP, Levin H, Schnieder K, Wilde EA, Cantu RC, et al. National Institute of Neurological Disorders and Stroke and Department of Defense sport-related concussion common data elements Version 1.0 Recommendations. J Neurotrauma. (2018) 35:2776–83. doi: 10.1089/neu.2018.5643
116. Meeuws S, Yuke JK, Hujben JA, Nair N, Lingsma HF, Bell MJ, et al. Common data elements: critical assessment of harmonization between current multi-center traumatic brain injury studies. J Neurotrauma. (2020) 37:1283–90. doi: 10.1089/neu.2019.6867
117. Iadevaia C, Roiger T, Zwart MB. Qualitative examination of adolescent health-related quality of life at 1 year postconcussion. J Athl Train. (2015) 50:1182–9. doi: 10.4085/1062-6050-50.11.02
118. McLeod TC, Wagner AJ, Bacon CE. Lived experiences of adolescent athletes following sport-related concussion. Orthop J Sports Med. (2017) 5:1–10. doi: 10.1177/2325967117745033
119. Dean PJA, O'Neill D, Sterr A. Post-concussion syndrome: prevalence after mild traumatic brain injury in comparison with a sample without head injury. Brain Inj. (2012) 26:14–26. doi: 10.3109/02699052.2011.635354
120. Rickards TA, Cranston CC, McWhorter J. Persistent post-concussive symptoms: a model of predisposing, precipitating, and perpetuating factors. Appl Neuropsychol Adult. (2020) 29:284–94. doi: 10.1080/23279095.2020.1748032
121. Scratch SE, Stevens SA, King G, Schwellnus H, Searl N, McPherson AC. Mental health care in pediatric rehabilitation hospitals: a biopsychosocial, collaborative, and agency-based service integration approach. Dev Neurorehabil. (2020) 23:359–67. doi: 10.1080/17518423.2019.1687600
122. Corwin DJ, Master CL, Grady MF, Zonfrillo MR. The economic burden of pediatric postconcussive syndrome. Clin J Sport Med. (2020) 30:154–5. doi: 10.1097/JSM.0000000000000732
123. Fallesen P, Campos B. Effect of concussion on salary and employment: a population-based event time study using a quasi-experimental design. BMJ Open. (2020) 10:38161. doi: 10.1136/bmjopen-2020-038161
124. Tator CH, Davis HS, Dufort PA, Tartaglia MC, Davis KD, Ebraheem A, et al. Postconcussion syndrome: demographics and predictors in 221 patients. J Neurosurg. (2016) 125:1206–16. doi: 10.3171/2015.6.JNS15664
125. Silverberg ND, Gardner AJ, Brubacher JR, Panenka WJ, Li JJ, et al. Systematic review of multivariable prognostic models for mild traumatic brain injury. J Neurotrauma. (2015) 32:517–26. doi: 10.1089/neu.2014.3600
126. Silverberg ND, Iverson GL. Etiology of the post-concussion syndrome: physiogenesis and psychogenesis revisited. NeuroRehabilitation. (2011) 29:317–29. doi: 10.3233/NRE-2011-0708
Keywords: concussion, persistent, children, adults, mental health, prevalence
Citation: Sheldrake E, Al-Hakeem H, Lam B, Goldstein BI, Wheeler AL, Burke M, Dunkley BT, Reed N and Scratch SE (2022) Mental Health Outcomes Across the Lifespan in Individuals With Persistent Post-Concussion Symptoms: A Scoping Review. Front. Neurol. 13:850590. doi: 10.3389/fneur.2022.850590
Received: 07 January 2022; Accepted: 18 March 2022;
Published: 11 April 2022.
Edited by:
Andrea Martinuzzi, Eugenio Medea (IRCCS), ItalyReviewed by:
Nathan E. Cook, Massachusetts General Hospital and Harvard Medical School, United StatesChristianne Laliberte Durish, University of Calgary, Canada
Alec Vestri, Eugenio Medea (IRCCS), Italy
Copyright © 2022 Sheldrake, Al-Hakeem, Lam, Goldstein, Wheeler, Burke, Dunkley, Reed and Scratch. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elena Sheldrake, ZWxlbmEuc2hlbGRyYWtlQG1haWwudXRvcm9udG8uY2E=
 Elena Sheldrake
Elena Sheldrake Hiba Al-Hakeem
Hiba Al-Hakeem Brendan Lam1
Brendan Lam1 Benjamin I. Goldstein
Benjamin I. Goldstein Anne L. Wheeler
Anne L. Wheeler Matthew Burke
Matthew Burke Benjamin T. Dunkley
Benjamin T. Dunkley Nick Reed
Nick Reed