- 1Neurology, Saarland University, Homburg, Germany
- 2East of England Ambulance Service NHS Trust, Melbourn, United Kingdom
- 3Institute of Clinical Chemistry, Laboratory Medicine and Transfusion Medicine, Nuremberg General Hospital, Paracelsus Medical University, Nuremberg, Germany
- 4Division of Imaging Science and Technology, School of Medicine, University of Dundee, Dundee, United Kingdom
Although prehospital stroke management is challenging, it is a crucial part of the acute stroke chain to enable equal access to highly specialised stroke care. It involves a critical understanding of players usually not specialized in acute stroke treatments. There is contradictory information about gender inequity in prehospital stroke detection, dispatch, and delivery to hospital stroke centers. The aim of this narrative review is to summarize the knowledge of gender differences in the first three stages of acute stroke management. Information on the detection of acute stroke symptoms by patients, their relatives, and bystanders is discussed. Women seem to have a better overall knowledge about stroke, although general understanding needs to be improved. However, older age and different social situations of women could be identified as reasons for reduced and delayed help-seeking. Dispatch and delivery lie within the responsibility of the emergency medical service. Differences in clinical presentation with symptoms mainly affecting general conditions could be identified as a crucial challenge leading to gender inequity in these stages. Improvement of stroke education has to be applied to tackle this inequal management. However, specifically designed projects and analyses are needed to understand more details of sex differences in prehospital stroke management, which is a necessary first step for the potential development of substantially improving strategies.
Introduction
Acute stroke care and access to timely treatment strongly depend on efficiently organized prehospital management. The stroke chain of survival with its first 3 “Ds”, detection, dispatch, and delivery, based in the prehospital setting emphasizes the importance of optimal pathways before the patients arrive at the hospital (1). There is contradictory information about gender inequity in acute stroke treatment. A German nationwide cohort analysis with >1 million patients identified a higher probability of men receiving stroke unit treatment (OR, 1.11; 95% CI, 1.09–1.12) with a lower in-hospital mortality (OR, 0.91; 95% CI, 0.89–0.93) compared to women (2). However, intravenous thrombolysis (IVT) treatment numbers were similar in this study and more women received endovascular treatment (EVT). A Swedish analysis confirmed significantly lower numbers of women receiving stroke unit care in their cohort (3). In contrast, a retrospective analysis of patients with acute ischemic stroke (AIS) arriving at hospital within 2 h after symptom onset from the American Get-With-The-Guidelines-Stroke registry identified female sex as a risk factor for not receiving IVT (4). It is unclear whether these differences are caused by an already existing gender inequity in the very first prehospital stages of acute stroke care in different regions. This review gives insights into available knowledge on gender differences from symptom onset until arrival at the hospital emergency department and discusses available information on detection, dispatch, and delivery of the acute stroke management cascade.
Detection of Acute Stroke Symptoms
Identification of acute symptoms of stroke can be challenging even for specialists. However, this is the first crucial step in gaining access to modern stroke treatment, especially to recanalizing therapies with a time-limited treatment window for the best outcome. Most of the current literature describes a better recognition and identification of acute stroke symptoms by women, but there are also publications emphasizing their lack of stroke understanding.
Differences in Stroke Knowledge
A meta-analysis of 22 studies, of which 20 were cross-sectional and 2 pretest–posttest design surveys, mainly conducted in the USA and Canada, identified a greater knowledge of stroke symptoms and related risk factors in women compared to men (5). In a Spanish randomized study, in which knowledge about stroke symptoms and risk factors was collected with structured face-to-face questionnaires, no sex difference could be detected in general knowledge about stroke, but women showed a higher understanding of risk factors. However, they were less likely to call an ambulance (6). In contrast, in a cross-sectional Chinese study, in which men and women with stroke and hypertension were questioned regarding their stroke knowledge and behavior, men demonstrated a better knowledge about stroke but had a worse pre-stroke health behavior than women (7). An American stroke survey performed with a limited number of stroke survivors detected women as significantly more likely compared to men to identify all the five traditional warning signs of stroke and subsequently take the correct action by calling the Emergency Medical Service [EMS; (8)]. In 4 Canadian cross-sectional surveys, in which public awareness campaigns including information about stroke preceded a stroke-knowledge questionnaire about face, arm, speech symptoms, a clear association of limited knowledge with male sex was found [Odds ratio 0.68; 95% CI: 0.53, 0.86; (9)].
In addition, the overall perception of stroke knowledge in women is poor. A survey of 1,024 women contacted by randomly selected telephone numbers in the USA in 2003 identified that only one-fourth of all women felt well informed about stroke and stroke risk and just below a quarter reported to be very concerned about the disease. Standing out was that younger women aged 25–34 years had the highest rate of nescience (37%). Hispanic or Black ethnicity was associated with less knowledge, but correct identification of acute stroke symptoms was low for all age groups and independent of racial backgrounds (10).
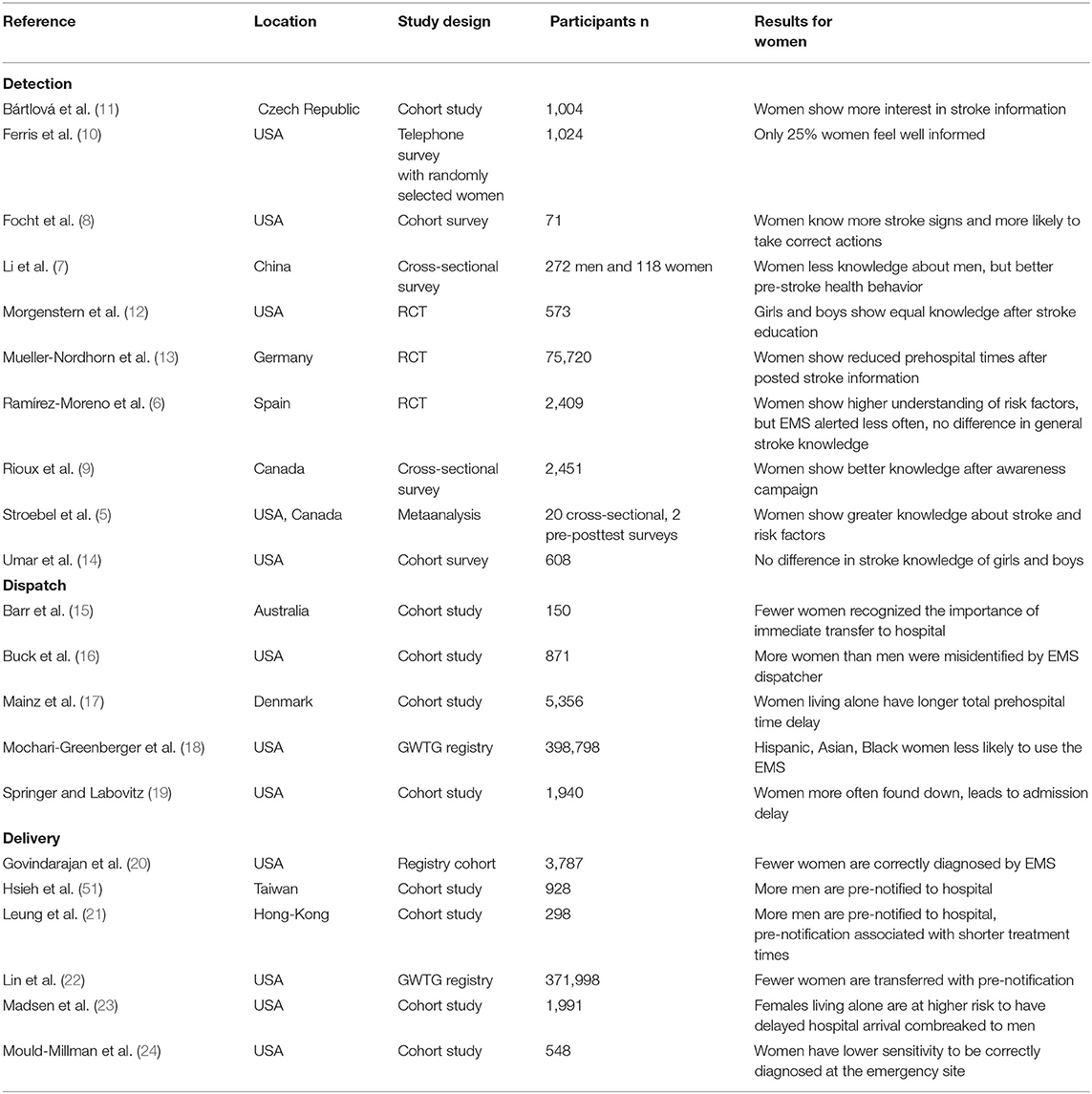
The above examples of available evidence (summarized in Table 1) emphasize that in many countries women are not generally underprivileged in their knowledge about stroke and understanding of the necessary actions to take. But, knowledge in general still needs improvement and differs not only between the countries but also between different ethnic groups. Both latter stress the need for tailored regional educational programmes involving women of all ethnic groups. A one-fit-all approach will not reach the aim.
Another possibility to increase stroke knowledge is to address pupils rather than only adults and to integrate medical education into school programmes. There is only limited information about the potential benefits of an early school education about stroke and stroke symptoms. However, there seems to be no gender difference. In an 11-question multiple-choice stroke awareness survey with >600 American High school pupils, no difference in stroke symptom knowledge between girls and boys was detected (14). A randomized controlled, multiethnic school-based intervention study called “Kids Identifying and Defeating Stroke” (KIDS), which was started in middle schools enrolling 8,827 pupils in Texas, USA investigated whether a structured stroke education campaign for their year 6 to year 8 pupils could improve stroke knowledge and necessary emergency actions. The programme was performed as four 1-h classes each year, taught by health teachers and neurologists, and included a homework assignment involving parents. A significant increase in stroke knowledge and correct reaction to witnessed symptoms of students' in the KIDS group compared with controls could be observed. The result did not show any gender differences (12). No information could be found from other countries. Also, it stays unclear whether school educational programmes can lead to a longer-lasting increase in the overall understanding of stroke symptoms, and emergency actions needed. This requires further investigation.
Educational Effect of Public Awareness Campaigns
Public awareness campaigns, comparable to advertisements promoting products or services, are general means that use mass media and new media to transfer information.
It is very well described that most public awareness campaigns can improve stroke knowledge only for a short amount of time, usually lasting between 3 and 6 months (25). Interestingly, it seems that there is a gender difference in susceptibility to such campaigns. A randomized study analyzing the effect of a posted information letter about stroke symptoms showed that the outcome of reduction of prehospital times was only significant for women (13). This could be explained by the finding from a cohort analysis in the Czech Republic, where a sample of 1,004 people were interrogated about their stroke knowledge. Women showed significantly higher interest in the information than men (11). Nevertheless, it stays unclear whether permanently repeated public awareness campaigns in the spirit of “Groundhog Day” could lead to a more solid understanding of stroke of all genders and ethnicities.
Dispatch: Involvement of EMS
Early activation and dispatch of EMS is a vital element in the acute stroke chain of survival (26). The use of EMS is associated with shorter times to treatment (27); however the existing literature evidences a large degree of variation in how quickly patients alert the EMS and the subsequent dispatch of a medical resource. Prehospital delays can range from 20 min to >150 h based on a number of factors, including the patient's awareness of the severity of their symptoms with data suggesting that female patients with stroke experience an increased delay time in calling for help (15).
There is a paucity of contemporary evidence surrounding sex differences in activation and dispatch of EMS; however there is a recognized inequity in emergency care access in women with stroke, which may be a result of delay in EMS dispatch (28). In a study of 5,515 patients with stroke in the Netherlands, symptom onset to door time was found to be on average 27 min longer in women than in men (29). This finding can be caused by multiple different underlying reasons, of which some are discussed below and are summarized in Table 1.
Willingness to Call
Existing literature presents an inconsistent picture of sex differences in the activation of EMS. Ramirez-Moreno et al. (6) studied responses from 2,409 participants aged 18 and over, who were surveyed through face-to-face interviews consisting of open-ended questions about the respondent's hypothetical answer to presenting or witnessing signs of a stroke and upon suspecting stroke or transient ischemic attack (TIA) in a family member or themselves. An appropriate response to a suspected stroke was indicated by 83.4% of men compared to only 77.5% of women. These findings are corroborated by further research which suggest that women are more likely to delay accessing emergency care than men, with some literature suggesting that the odds of being admitted to hospital within 3 h of symptom onset was 10% lower for women than men (30). Possible reasons for the disparity in the response to stroke symptoms between men and women may include a difference in perceived severity of the symptoms with women underestimating the urgency of the situation (6). But there are also intrasexual differences. Data analyzed from 398,798 American Get-with-the-guideline stroke registry patients, identified Hispanic or Asian or Black women compared to White women as less likely to use the EMS when stroke symptoms occurred [aOR, 95%CI: Black: 0.87, 0.84–0.91; Hispanic: 0.71, 0.67–0.74; Asian: 0.71, 0.67–0.76; (18)].
Reasons for Delayed Calling
Delayed calling for help might have multiple underlying causes. An American questionnaire study assessing attitudes toward response to stroke onset found that women, who arrived at hospital over 3 h after symptom onset, cited reasons such as not wanting to trouble others, opting to see if their symptoms might resolve, hiding their symptoms from others, and trying to continue with their normal actives for a delay in seeking emergency care (31). This finding demonstrates some plausible reasons for the delay in EMS dispatch, and therefore hospital arrival, that impacts the eligibility for recanalizing treatments due to arriving outside the treatment window (17).
Whilst the study did not include men and therefore provides no opportunity for comparison with regard to responses, it is recognized that there are sex-specific differences in the way in which medical assistance is summoned following the onset of stroke symptoms, which can result in a delay in dispatch for women (32). In a study of 150 patients with stroke in Australia, it was found that women experienced a delay in symptom onset to presentation to ED that was a mean average of 1.4 h longer than men, with knowledge and recognition of stroke symptoms and not recognizing the importance of their symptoms significantly impacting this delay (15).
Impact of Difference in Social Situations
If a stroke is witnessed, the activation of EMS is substantially shorter than if symptom onset was unwitnessed (33). It is, therefore, reasonable to suggest that living alone may result in a higher incidence of stroke with an unwitnessed symptom onset and therefore delayed EMS dispatch. Mainz and collaborators published in 2020 (17) the higher proportion of women living alone at the time of their stroke as a likely cause for a longer delay in symptom onset to EMS call. Their study found that this “patient-dependent delay” for women was 19.8 min longer than for men, with living alone being associated with a longer total prehospital time delay. About 50.4% of women lived alone compared to only 31.7% of men.
A retrospective cohort analysis of 1,904 hospital patients with stroke in New York, USA identified that women are significantly more often found with severe stroke symptoms unable to seek help on their own (“found down”) and that this led to all of them arriving 3 h or later after onset (19).
If the onset of stroke symptoms is witnessed, it is most commonly by the patient's partner (34); however more women than men are widowed at the time of stroke and therefore live alone, with a delay in EMS dispatch a plausible consequence of this (35). The caller was the patient themselves in only 3% of cases based on a study of 198 patients transported to the emergency department (ED) by EMS in Melbourne (34), further supporting the hypothesis that women are susceptible to delays in EMS dispatch.
Another reason adding to the gender difference in EMS activation might be that women are older than men at the time of stroke, particularly in Europe, Australia, and South America (36). This results in a higher level of functional limitation prior to their stroke (35, 37), which may impact their physical ability to summon help.
Role of the Emergency Medical Service Dispatch Center
The identification of stroke symptoms at the point of EMS dispatch is key in optimizing the chain of survival in acute stroke and this remains one of the least investigated elements of the chain (38). It is critical that dispatch centers accurately identify stroke to avoid the assignment of an incorrect “code” and cause subsequent delays in EMS dispatch (39). There are many differences in the organization of EMS worldwide (40); however findings show a stark variation in the proportion of strokes correctly identified at the point of dispatch with successful identification ranging from 45 to 83% (16, 41).
In some countries, the Medical Priority Dispatch System (MPDS) is used for EMS dispatch. This system is based on a structured caller interrogation with additional instructions on what to do until EMS arrival. In a Los Angeles study of 871 patients, 58 were assigned the stroke MPDS code by the dispatcher, but only 45% received a confirmed in-hospital stroke diagnosis (16). A total of 56.2% of female patients with stroke were misidentified in this study. In a review of existing literature, Oostema and collaborators (42) found that despite the use of a stroke screening tool, the recognition of stroke by the dispatch center was inadequate and it is suggested that many subtle stroke presentations may be misidentified (39). A barrier to the identification of stroke symptoms at the point of dispatch is the variety of presenting symptoms that may fall outside of the screening system adopted by the communication center. With women more likely to experience non-traditional stroke symptoms, an inherent risk not only of incorrect call coding at the point of dispatch with subsequent delays in timely EMS care but also of EMS identification of a woman with stroke, decelerating the delivery to the stroke center, has to be considered.
Delivery to Hospital
There are many reports on differences in clinical presentation between men and women [Table 1; (43)]. This likely not only affects stroke patient's identification at the dispatch center level but also at the scene, influencing the delivery step of the acute stroke chain of survival. Delivery comprises of rapid EMS identification of stroke symptoms, management of the patient on the scene, and timely transportation and prenotification to the hospital, as defined by the American Heart Association (44).
Gender Differences in Stroke Presentation and EMS Recognition
Women are reported to often present with unusual stroke symptoms such as generalized weakness, fatigue, and mental status change. In an analysis of 461 patients, 52% of women compared to 44% of men presented with a non-traditional stroke symptom (43). This result was primarily driven by the number of women with mental status changes, a symptom caused by many other differential diagnoses (45). Further studies confirmed that non-traditional stroke symptoms were present in 51.8% of women compared to 43.9% of men (46). In addition, disorientation, visual disturbance, dizziness headache, general pain, urinary incontinence, or changes in consciousness are specifically described to be shown in female stroke (47, 48).
These reported differences in the clinical presentation of stroke between genders can therefore be of challenge for the EMS when diagnosing stroke in the prehospital environment with only limited diagnostic tools available. This is supported by multiple studies (49). A recent systematic meta-analysis of 21 observational studies with 6,934 stroke and transient ischemic attack patients identified that 26% of all patients with stroke, who were missed by the EMS, presented with non-FAST symptoms like speech abnormalities, nausea/vomiting, dizziness, changes in mental status, and visual disturbance (41). A study with 3,787 patients transported by EMS found that only 30% of women compared to 35% of men received a correct diagnosis of stroke, with these findings perceived to be based on the non-traditional stroke symptoms displayed more frequently by women (20).
Various measures have been previously discussed to enhance prehospital stroke recognition, including the use of validated stroke scales (50). A retrospective analysis of 548 emergency patients in Atlanta, USA evaluated that paramedics were more likely to positively identify stroke when the Cincinnati Prehospital Stroke Scale (CPSS) was positive. However, sensitivity to be diagnosed at the scene was lower for women than men [odds ratio 0.53, 95%CI 0.17–1.63; (24)].
It is likely that different presentations of women with acute stroke lead to a wrong working diagnosis by the EMS in the prehospital phase, which could impact further stroke management. However, more prospective studies are needed to understand the real impact.
Gender Differences in EMS On-Scene Time Metrics and Prenotification to Hospital
A large study of nearly 2,000 patients presenting with AIS found that before adjustment, the time of symptom onset to arrival at the hospital via the EMS was slightly longer in women (mean 337 min vs. 297 min in men); however, they subsequently found that gender was not associated with a delayed time to arrival when considering age and National Institute Of Health Stroke Severity (NIHSS) score. It was demonstrated that 30% of women in the study (324/1097) lived alone compared to 22% of men (200/894), and that this was a factor in delayed arrival at the hospital, potentially due to the lack of self-recognition of symptoms (23). A study of 5,356 patients identified that 40.5% of women and 44.4% of men arrived at the stroke unit within 3 h of symptom onset, and similarly living alone was deemed to be a contributory factor involved in this finding. About 54.4% (1,256) of women were documented as living alone, leading to an average delay of 20 min longer than their male counterparts (17).
A study from 2016 demonstrated an association not only between pre-notification and faster door to computed tomography (CT) scan in patients presenting within 3 h of symptom onset but also a shorter door-to-needle (DTN) time. This study comprised of 928 patients, of whom 727 received pre-notification to the hospital. There was a significantly higher number of men who were transported with pre-notification (64.5%), and more pre-notified patients had a DTN of <60 min (45.1 vs. 28%) compared to those not pre-notified (51). A similar pattern was shown in a study from Hong Kong, which found that the ratio of men to women receiving pre-notification to hospital for stroke was 1.22:1. Pre-notification was also demonstrated to improve door-to-CT and DTN time (21).
An analysis of the American Get-with-the-Guideline stroke registry of 371,998 enrolled patients with stroke in 1,585 hospitals over 8 years showed a pre-notification rate of 67%. Patients with EMS pre-notification to the hospital were more likely to be younger, white, and male. In the 122,791 patients eligible for pre-notification where none was given, 54.3% were women (22).
These differences in prehospital management of women with acute stroke might be caused by a higher number of misdiagnoses, subsequently leading to lower numbers with accurately initiated stroke alert to the hospital. But clearly, further research is required to understand unbiased differences in prehospital treatment and outcomes.
Discussion
This review addresses gender differences in the very first stages of acute stroke management, the detection of disease symptoms to the delivery of the suspected stroke patient to the specialized center. It highlights some of the available evidence with the aim to raise awareness and identify a pattern, hinting toward areas of necessary improvement to guarantee gender equity in prehospital acute stroke treatment.
Detection of acute stroke and initiation of the necessary steps, which enable health care specialists to administer up-to-date and high-quality stroke care, is incumbent to the patient and or relatives or bystanders. There is a lot of evidence coming from different countries that women have a better knowledge about acute stroke symptoms, risk factors, and the necessary actions to take than men. However, the overall public level of knowledge about stroke, the number three disease cause for disability is still poor (52, 53). Gender inequity in the detection of stroke seems to show geographical differences, but further systematic evaluations are needed to understand where and what differences exist.
Despite often having a higher and better knowledge about stroke, women seem to feel uncertain about many aspects of the disease. Women's confidence in their own knowledge differs from that of men (54), which needs to be considered and addressed in educational programmes.
The idea to implement health education in standard school programmes would be one possibility to establish gender-independent knowledge transfer in the future. But, to reach girls and young women in countries with relevant sex inequity would need strong collaboration between health services and educational sectors with strong political and governmental support.
It is well described that public campaigns do not lead to a sustainable solution to improve health awareness (1); however it seems that women are more likely and willing to pick up information provided by mass media campaigns (55).
However, equal knowledge and awareness alone do not lead to equal acute stroke care. The available evidence suggests that women arrive at the hospital later than men, indicating an inequity in dispatch and delivery of acute stroke care. Relevant confounders like social disparity with more women living alone at an older age, when the risk of stroke increases, have to be considered. Management of women seeking help at an emergency medical dispatch center does not seem to show any gender-based differences. But many countries use systematized interrogation programmes, like the Medical Priority Dispatch System to identify stroke suspects, which could be prone to errors and disadvantageous to women with stroke, who often present with non-traditional symptoms (43).
There is no information available on whether a criteria-based dispatch, used in many Nordic and European countries (56), which relies on the experience of the telecommunicator, is less prone to misidentify women with suspected strokes. More studies comparing both modes of emergency service dispatch are needed to identify gender-related challenges of different dispatch systems.
The differences in the clinical presentation of women compared to men can make it difficult for paramedics to quickly conclude a stroke working diagnosis at the emergency site. This likely presents the biggest challenge in the delivery of equal care. There is evidence for an inequity in pre-notification of cases to the receiving hospital. To tackle this, paramedic and EMS stroke-specific training have to be considered and addressed. A correlation between high-quality medical education and patient outcome has been demonstrated for nurse care (57, 58), but data for the EMS or, more important, training programme adjustment for prehospital staff is lacking.
To conclude, more structured data and results from specifically designed clinical trials are needed to understand gender inequity in the first stages of acute stroke care and to develop solutions to overcome potential gender disbalances. Identified gender inequity is mostly caused by unawareness of gender-specific aspects of stroke, which are not considered in acute prehospital pathways.
Author Contributions
SW, BW, RM, and KF contributed to the conception and design of the review. SW, BW, and RM wrote the first draft of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Fassbender K, Walter S, Grunwald IQ, Merzou F, Mathur S, Lesmeister M, et al. Prehospital stroke management in the thrombectomy era. Lancet Neurol. (2020) 19:601–10. doi: 10.1016/S1474-4422(20)30102-2
2. Weber R, Krogias C, Eyding J, Bartig D, Meves SH, Katsanos AH, et al. Age and sex differences in ischemic stroke treatment in a nationwide analysis of 111 million hospitalized cases. Stroke. (2019) 50:3494–502. doi: 10.1161/STROKEAHA.119.026723
3. Dahl S, Hjalmarsson C, Andersson B. Sex differences in risk factors, treatment, and prognosis in acute stroke. Womens Health. (2020) 16:1745506520952039. doi: 10.1177/1745506520952039
4. Messé SR, Khatri P, Reeves MJ, Smith EE, Saver JL, Bhatt DL, et al. Why are acute ischemic stroke patients not receiving IV tPA? Results from a national registry. Neurology. (2016) 87:1565–74. doi: 10.1212/WNL.0000000000003198
5. Stroebele N, Müller-Riemenschneider F, Nolte CH, Müller-Nordhorn J, Bockelbrink A, Willich SN. Knowledge of risk factors, and warning signs of stroke: a systematic review from a gender perspective. Int J Stroke. (2011) 6:60–6. doi: 10.1111/j.1747-4949.2010.00540.x
6. Ramírez-Moreno JM, Alonso-González R, Peral-Pacheco D, Millán-Núñez MV, Aguirre-Sánchez JJ. Knowledge of stroke a study from a sex perspective. BMC Res Notes. (2015) 8:604. doi: 10.1186/s13104-015-1582-1
7. Li ZR, Ruan HF, Shen LP, Zhang XP, Wan LH. Gender difference in the association between stroke knowledge and health behavior before the onset of stroke among Chinese hypertensive patients. J Neurosci Nurs. (2021) 53:160–5. doi: 10.1097/JNN.0000000000000599
8. Focht KL, Gogue AM, White BM, Ellis C. Gender differences in stroke recognition among stroke survivors. J Neurosci Nurs. (2014) 46:18–22. doi: 10.1097/JNN.0000000000000026
9. Rioux B, Brissette V, Marin FF, Lindsay P, Keezer MR, Poppe AY. The Impact of Stroke Public Awareness Campaigns Differs Between Sociodemographic Groups. Can J Neurol Sci. (2021) 20:1–8. doi: 10.1017/cjn.2021.76
10. Ferris A, Robertson RM, Fabunmi R, Mosca L, American Heart Association, American Stroke Association. American Heart Association and American Stroke Association national survey of stroke risk awareness among women. Circulation. (2005) 111:1321–6. doi: 10.1161/01.CIR.0000157745.46344.A1
11. Bártlová S, Šedová L, Rolantová L, Hudáčková A, Dolák F, Sadílek P. General awareness of stroke in the Czech Republic. Cent Eur J Public Health. (2021) 29:230–5. doi: 10.21101/cejph.a6212
12. Morgenstern LB, Gonzales NR, Maddox KE, Brown DL, Karim AP, Espinosa N, et al. randomized, controlled trial to teach middle school children to recognize stroke and call 911: the kids identifying and defeating stroke project. Stroke. (2007) 38:2972–8. doi: 10.1161/STROKEAHA.107.490078
13. Müller-Nordhorn J, Wegscheider K, Nolte CH, Jungehülsing GJ, Rossnagel K, Reich A, et al. Population-based intervention to reduce prehospital delays in patients with cerebrovascular events. Arch Intern Med. (2009) 169:1484–90. doi: 10.1001/archinternmed.2009.232
14. Umar AB, Koehler TJ, Zhang R, Gilbert V, Farooq MU, Davis AT, et al. Stroke knowledge among middle and high school students. J Int Med Res. (2019) 47:4230–41. doi: 10.1177/0300060519858887
15. Barr J, McKinley S, O'Brien E, Herkes G. Patient recognition of and response to symptoms of TIA or stroke. Neuroepidemiology. (2006) 26:168–75. doi: 10.1159/000091659
16. Buck BH, Starkman S, Eckstein M, Kidwell CS, Haines J, Huang R, et al. Dispatcher recognition of stroke using the National Academy Medical Priority Dispatch System. Stroke. (2009) 40:2027–30. doi: 10.1161/STROKEAHA.108.545574
17. Mainz J, Andersen G, Valentin JB, Gude MF, Johnsen SP. Disentangling sex differences in use of reperfusion therapy in patients with acute ischemic stroke. Stroke. (2020) 51:2332–8. doi: 10.1161/STROKEAHA.119.028589
18. Mochari-Greenberger H, Xian Y, Hellkamp AS, Schulte PJ, Bhatt DL, Fonarow GC, et al. Racial/ethnic and sex differences in emergency medical services transport among hospitalized us stroke patients: analysis of the national get with the guidelines-stroke registry. J Am Heart Assoc. (2015) 4:e002099. doi: 10.1161/JAHA.115.002099
19. Springer MV, Labovitz DL. The effect of being found with stroke symptoms on predictors of hospital arrival. J Stroke Cerebrovasc Dis. (2018) 27:1363–7. doi: 10.1016/j.jstrokecerebrovasdis.2017.12.024
20. Govindarajan P, Friedman BT, Delgadillo JQ, Ghilarducci D, Cook LJ, Grimes B, et al. Race and sex disparities in prehospital recognition of acute stroke. Acad Emerg Med. (2015) 22:264–72. doi: 10.1111/acem.12595
21. Leung WCY, Teo KC, Kwok WM, Lam LHC, Choi OMY, Tse MMY, et al. Pre-hospital stroke screening and notification of patients with reperfusion-eligible acute ischaemic stroke using modified Face Arm Speech Time test. Hong Kong Med J. (2020) 26:479–85. doi: 10.12809/hkmj208552
22. Lin CB, Peterson ED, Smith EE, Saver JL, Liang L, Xian Y, et al. Emergency medical service hospital prenotification is associated with improved evaluation and treatment of acute ischemic stroke. Circ Cardiovasc Qual Outcomes. (2012) 5:514–22. doi: 10.1161/CIRCOUTCOMES.112.965210
23. Madsen TE, Sucharew H, Katz B, Alwell KA, Moomaw CJ, Kissela BM, et al. Gender and time to arrival among ischemic stroke patients in the greater cincinnati/Northern Kentucky Stroke Study. J Stroke Cerebrovasc Dis. (2016) 25:504–10. doi: 10.1016/j.jstrokecerebrovasdis.2015.10.026
24. Mould-Millman NK, Meese H, Alattas I, Ido M, Yi I, Oyewumi T, et al. Accuracy of prehospital identification of stroke in a large stroke belt municipality. Prehosp Emerg Care. (2018) 22:734–42. doi: 10.1080/10903127.2018.1447620
25. Fassbender K, Grotta JC, Walter S, Grunwald IQ, Ragoschke-Schumm A, Saver JL. Mobile stroke units for prehospital thrombolysis, triage, and beyond: benefits and challenges. Lancet Neurol. (2017) 16:227–37. doi: 10.1016/S1474-4422(17)30008-X
26. Ashcraft S, Wilson SE, Nyström KV, Dusenbury W, Wira CR, Burrus TM, et al. Care of the patient with acute ischemic stroke (prehospital and acute phase of care): update to the 2009 comprehensive nursing care scientific statement: a scientific statement from the American Heart Association. Stroke. (2021) 52:e164–78. doi: 10.1161/STR.0000000000000356
27. Bray JE, Mosley I, Bailey M, Barger B, Bladin C. Stroke public awareness campaigns have increased ambulance dispatches for stroke in Melbourne, Australia. Stroke. (2011) 42:2154–7. doi: 10.1161/STROKEAHA.110.612036
28. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. (2019) 50:e344–418. doi: 10.1161/STR.0000000000000211
29. de Ridder I, Dirks M, Niessen L, Dippel D, PRACTISE Investigators. Unequal access to treatment with intravenous alteplase for women with acute ischemic stroke. Stroke. (2013) 44:2610–2. doi: 10.1161/STROKEAHA.113.002263
30. Foerch C, Misselwitz B, Humpich M, Steinmetz H, Neumann-Haefelin T, Sitzer M. Arbeitsgruppe Schlaganfall Hessen. Sex disparity in the access of elderly patients to acute stroke care. Stroke. (2007) 38:2123–6. doi: 10.1161/STROKEAHA.106.478495
31. Beal CC. Women's interpretation of and cognitive and behavioral responses to the symptoms of acute ischemic stroke. J Neurosci Nurs. (2014) 46:256–66. doi: 10.1097/JNN.0000000000000083
32. Mandelzweig L, Goldbourt U, Boyko V, Tanne D. Perceptual, social, and behavioral factors associated with delays in seeking medical care in patients with symptoms of acute stroke. Stroke. (2006) 37:1248–53. doi: 10.1161/01.STR.0000217200.61167.39
33. Rosamond WD, Gorton RA, Hinn AR, Hohenhaus SM, Morris DL. Rapid response to stroke symptoms: the Delay in Accessing Stroke Healthcare (DASH) study. Acad Emerg Med. (1998) 5:45–51. doi: 10.1111/j.1553-2712.1998.tb02574.x
34. Mosley I, Nicol M, Donnan G, Patrick I, Dewey H. Stroke symptoms and the decision to call for an ambulance. Stroke. (2007) 38:361–6. doi: 10.1161/01.STR.0000254528.17405.cc
35. Willers C, Lekander I, Ekstrand E, Lilja M, Pessah-Rasmussen H, Sunnerhagen KS, et al. Sex as predictor for achieved health outcomes and received care in ischemic stroke and intracerebral hemorrhage: a register-based study. Biol Sex Differ. (2018) 9:11. doi: 10.1186/s13293-018-0170-1
36. Carcel C, Wang X, Sandset EC, Delcourt C, Arima H, Lindley R, et al. Sex differences in treatment and outcome after stroke: Pooled analysis including 19,000 participants. Neurology. (2019) 93:e2170–80. doi: 10.1212/WNL.0000000000008615
37. Phan HT, Blizzard CL, Reeves MJ, Thrift AG, Cadilhac DA, Sturm J, et al. Factors contributing to sex differences in functional outcomes and participation after stroke. Neurology. (2018) 90:e1945–53. doi: 10.1212/WNL.0000000000005602
38. Puolakka T, Strbian D, Harve H, Kuisma M, Lindsberg PJ. Prehospital phase of the stroke chain of survival: a prospective observational study. J Am Heart Assoc. (2016) 5:e002808. doi: 10.1161/JAHA.115.002808
39. Ramanujam P, Guluma KZ, Castillo EM, Chacon M, Jensen MB, Patel E, et al. Accuracy of stroke recognition by emergency medical dispatchers and paramedics–San Diego experience. Prehosp Emerg Care. (2008) 12:307–13. doi: 10.1080/10903120802099526
40. Sikka N, Margolis G. Understanding diversity among prehospital care delivery systems around the world. Emerg Med Clin North Am. (2005) 23:99–114. doi: 10.1016/j.emc.2004.09.007
41. Jones SP, Bray JE, Gibson JM, McClelland G, Miller C, Price CI, et al. Characteristics of patients who had a stroke not initially identified during emergency prehospital assessment: a systematic review. Emerg Med J. (2021) 38:387–93. doi: 10.1136/emermed-2020-209607
42. Oostema JA, Carle T, Talia N, Reeves M. Dispatcher Stroke Recognition Using a Stroke Screening Tool: A Systematic Review. Cerebrovasc Dis. (2016) 42:370–7. doi: 10.1159/000447459
43. Bushnell C, Howard VJ, Lisabeth L, Caso V, Gall S, Kleindorfer D, et al. Sex differences in the evaluation and treatment of acute ischaemic stroke. Lancet Neurol. (2018) 17:641–50. doi: 10.1016/S1474-4422(18)30201-1
44. Jauch EC, Cucchiara B, Adeoye O, Meurer W, Brice J, Chan YY, et al. Part 11: adult stroke: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. (2010) 122:S818–28. doi: 10.1161/CIRCULATIONAHA.110.971044
45. Patti L, Gupta M. Change In Mental Status. 2021 Aug 11. In: StatPearls. Treasure Island (FL): StatPearls Publishing (2021).
46. Branyan TE, Sohrabji F. Sex differences in stroke co-morbidities. Exp Neurol. (2020) 332:113384. doi: 10.1016/j.expneurol.2020.113384
47. Lisabeth LD, Brown DL, Hughes R, Majersik JJ, Morgenstern LB. Acute stroke symptoms: comparing women and men. Stroke. (2009) 40:2031–6. doi: 10.1161/STROKEAHA.109.546812
48. Girijala RL, Sohrabji F, Bush RL. Sex differences in stroke: review of current knowledge and evidence. Vasc Med. (2017) 22:135–45. doi: 10.1177/1358863X16668263
49. Brandler ES, Sharma M, McCullough F, Ben-Eli D, Kaufman B, Khandelwal P, et al. Prehospital stroke identification: factors associated with diagnostic accuracy. J Stroke Cerebrovasc Dis. (2015) 24:2161–6. doi: 10.1016/j.jstrokecerebrovasdis.2015.06.004
50. Fassbender K, Balucani C, Walter S, Levine SR, Haass A, Grotta J. Streamlining of prehospital stroke management: the golden hour. Lancet Neurol. (2013) 12:585–96. doi: 10.1016/S1474-4422(13)70100-5
51. Hsieh MJ, Tang SC, Chiang WC, Tsai LK, Jeng JS, Ma MH, et al. Effect of prehospital notification on acute stroke care: a multicenter study. Scand J Trauma Resusc Emerg Med. (2016) 24:57. doi: 10.1186/s13049-016-0251-2
52. GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. (2021) 20:795–820. doi: 10.1016/S1474-4422(21)00252-0
53. Melak AD, Wondimsigegn D, Kifle ZD. Knowledge, prevention practice and associated factors of stroke among hypertensive and diabetic patients - a systematic review. Risk Manag Healthc Policy. (2021) 14:3295–310. doi: 10.2147/RMHP.S324960
54. Bleidorn W, Arslan RC, Denissen JJ, Rentfrow PJ, Gebauer JE, Potter J, et al. Age and gender differences in self-esteem-A cross-cultural window. J Pers Soc Psychol. (2016) 111:396–410. doi: 10.1037/pspp0000078
55. Hodgson C, Lindsay P, Rubini F. Can mass media influence emergency department visits for stroke? Stroke. (2007) 38:2115–22. doi: 10.1161/STROKEAHA.107.484071
56. Bohm K, Kurland L. The accuracy of medical dispatch-a systematic review. Scand J Trauma Resusc Emerg Med. (2018) 26:94. doi: 10.1186/s13049-018-0528-8
57. Aiken LH, Sloane DM, Bruyneel L, Van den Heede K, Griffiths P, Busse R, et al. Nurse staffing and education and hospital mortality in nine European countries: a retrospective observational study. Lancet. (2014) 3830:1824–30. doi: 10.1016/S0140-6736(13)62631-8
Keywords: prehospital, acute stroke, management, women, gender inequity
Citation: Walter S, Phillips D, Wells B, Moon R, Bertsch T, Grunwald IQ and Fassbender K (2022) Detection to Hospital Door: Gender Differences of Patients With Acute Stroke Symptoms. Front. Neurol. 13:833933. doi: 10.3389/fneur.2022.833933
Received: 12 December 2021; Accepted: 09 March 2022;
Published: 07 April 2022.
Edited by:
Christina Kruuse, Copenhagen University Hospital-Herlev Gentofte, DenmarkReviewed by:
Serefnur Ozturk, Selcuk University, TurkeyKrystyna Jaracz, Poznan University of Medical Sciences, Poland
Copyright © 2022 Walter, Phillips, Wells, Moon, Bertsch, Grunwald and Fassbender. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Silke Walter, c2lsa2Uud2FsdGVyQHVrcy5ldQ==
 Silke Walter
Silke Walter Daniel Phillips2
Daniel Phillips2 Brittany Wells
Brittany Wells Thomas Bertsch
Thomas Bertsch Klaus Fassbender
Klaus Fassbender