- 1Nursing Care Health Facility Asahina, Medical Corporation Nakamurakai, Kanagawa, Japan
- 2School of Industrial Technology, Advanced Institute of Industrial Technology, Tokyo Metropolitan Public University Corporation, Tokyo, Japan
- 3Department of Neurology, Mie University, Tsu, Japan
- 4Department of Electrical and Electronic Engineering, Setsunan University, Osaka, Japan
- 5Advanced Applied Music Institute, Social Welfare Organization Kibounoie, Hyogo, Japan
Despite the fact that accessible digital musical instruments can take into account the level of cognitive demands, previous studies have been conducted with patients with mild cognitive impairment (MCI), and it is not known whether they can be used by people with moderate to severe dementia or dementia with worsening behavioral and psychological symptoms of dementia (BPSD). The participant was an 88-year-old woman with vascular dementia (VaD) (Mini-Mental State Examination [MMSE] and Neuropsychiatric Inventory [NPI] scores: 8 and 20, respectively). Music therapy (MT) was provided twice a week for 15 min, and MT sessions spanned over 18 months. For the MT, we used the cyber musical instrument with score (Cymis), an accessible digital musical instrument; it could be played using a touch panel and switches. The cognitive function of the participant declined further, with MMSE scores of 4 after 1 year and 0 after 1.5 years. BPSD peaked with the NPI score of 54 at 1 year and declined thereafter, although only apathy remained. Despite these changes, during MT, she was able to play the accessible digital musical instrument and focus on the performance. These results suggest that even patients with severe VaD can play an accessible digital instrument and continue active music therapy even if their BPSD progress with cognitive decline.
Introduction
To date, no fundamental cure has been developed for many forms of dementia (1). In addition to pharmacological treatment with anti-dementia drugs that slow down the progression of symptoms, music therapy (MT) is widely used in the treatment of dementia (2–6). Musical instrument playing involves motor and cognitive functions simultaneously (7). Because of this multimodal intervention, musical instruments are often used in MT for dementia (8–15).
In healthy elderly people and people with mild cognitive impairment (MCI), most interventions use pianos (16, 17), although in dementia, percussion is the main musical instrument type (12, 18). In addition to rhythm, music has elements of melody and harmony. It is very disadvantageous to be unable to play melodic and harmonic elements as cognitive function declines. Accessible digital musical instruments compensate for this disadvantage. Current advances in music technology have enabled the creation of customized accessible digital musical instruments, and in recent years, the use of music technology in music therapy has been gaining attention (19). Han et al. (20) aimed to evaluate the effect of a cognitive intervention with an accessible digital musical instrument on MCI. In this prospective study, 24 patients with MCI (intervention group, 12; and control group, 12) were enrolled. An electronic device with musical instruments and a song-based cognitive stimulation therapy protocol was developed for the intervention group. In the intervention group, the Mini-Mental State Examination (MMSE) and Montreal Cognitive Assessment scores improved significantly after the 10-week intervention.
Despite the fact that accessible digital musical instruments can take into account the level of cognitive demands, previous studies have been conducted with patients with MCI, and it is not known whether such methods can be used by people with moderate to severe dementia or dementia with worsening behavioral and psychological symptoms of dementia (BPSD). We asked patients with severe dementia to use the accessible digital musical instrument Cymis (cyber musical instrument with score) (21), which has already been used in MT for patients with cerebral palsy, to assess whether they could play it when their cognitive function declined or when their BPSD worsened.
We report a case study of a patient with severe vascular dementia (VaD) who was able to play an accessible digital instrument and to continue active MT even as her cognitive function declined and her BPSD progressed over an 18-month period.
Patient Information
Clinical Findings, Timeline, and Diagnostic Assessment
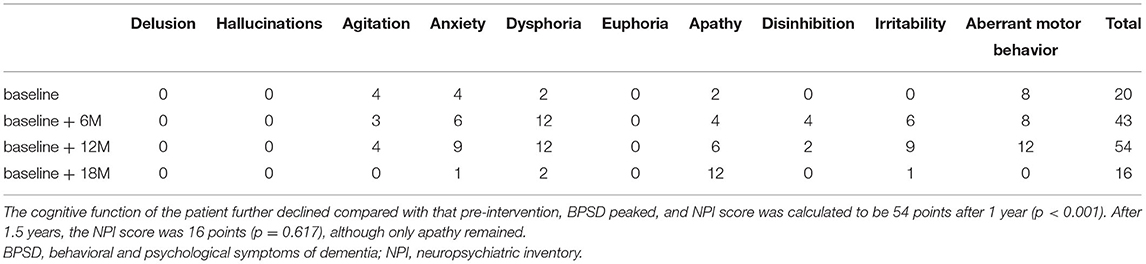
Ms. A, an 88-year-old right-handed Japanese woman was born in North Korea. After World War II, she moved to Japan. She worked as an office worker at a clothing company and learned calligraphy and the koto (Japanese harp) as a child. Ms. A has a son and a daughter from her marriage. She underwent surgery for colon and uterine cancer in X and had a stroke in X + 9. After losing her husband in X + 11, she lived alone. After being diagnosed with cerebrovascular dementia in X + 16, her eldest son stayed with her on weekends to take care of her. Ms. A used day care five times a week and nursing helpers five times a week in the mornings and evenings. In October, X + 18, she was admitted to the hospital with suspected pneumonia; this, along with her diagnosis of heart failure, made it difficult for her to live alone, and in November of the same year, she was admitted to our geriatric health care facility. At the time of admission to the facility, she had heart disease and was given medication for her hypertension. She received a score of 7 on the revised Hasegawa's dementia scale (22), with point scores of 0 for time disorientation, 1 for place disorientation, 3 for word recognition, and 3 for object recognition. She was originally mild-mannered but had a strong desire to return to her home and exhibited disruptive behavior on admission; after September, X + 19, her anxiety, restlessness, insomnia, agitation, desire to go home, and refusal of care became stronger. She participated in group MT several times but was not actively involved. During the day, Ms. A spent most of her time asleep and did not interact with others. In the afternoons, she exhibited stronger BPSD; she would cry from anxiety and clap her hands for attention. This study started in January, X + 20 and continued until July, X + 21. It was approved by the Research Safety and Ethics Committee of AIIT. Informed consent was given by the music therapist and by Ms. A and her care staff at the health care facility. On admission, Ms. A's score for the MMSE was 8 and that for the Neuropsychiatric Inventory (NPI) was 20. The caregiver completed an assessment of Ms. A's BPSD status. All tests were performed at the geriatric health care facility where Ms. A was admitted (Figure 1).
Therapeutic Intervention
Neuropsychological Tests
Evaluation was conducted using the MMSE (23) and NPI (24). The MMSE was used to quantify intellectual function, and the NPI was used to assess the 10 behavioral disturbances that occur in patients with dementia: delusions, hallucinations, dysphoria, anxiety, agitation/aggression, euphoria, disinhibition, irritability/lability, apathy, and aberrant motor activity. The NPI uses a screening strategy to minimize administration time by examining and scoring only those behavioral domains with responses to screening questions. The frequency and severity of each behavior were determined. Information for the NPI was obtained from a caregiver familiar with the patient's behavior. Neuropsychological tests were conducted before the intervention, and at 6, 12, and 18 months after the intervention to compare the results. Each value was statistically processed using a chi-squared test.
Playing an Accessible Digital Musical Instrument
Individual sessions for MT were held twice a week, for 15 min per session in the evening, over 18 months. For the musical instrumental performance, we used an accessible digital musical instrument called the Cymis (21), which has a built-in programmed score and is played using touch panels and switches (Figure 2). The technical novelty of the Cymis lies in its human interface devices that emphasize the sensory experience and is characterized by its built-in score information and program. This computerized musical instrument system comprises a monitor display, a personal computer, a sound source, a speaker, and human interface devices (image sensor for finger movement detection, touch panel, and others). The system is an electronic musical instrument that is barrier-free, allows for the understanding of music notation, and allows beginners of any age to easily play music comprising melody, rhythm, and harmony. As Ms. A was often in an anxious state of mind, we used “Kojo no Tsuki,” which is a song in the minor key, to calm her anxiety. The melody of “Kojo no Tsuki” was familiar to Ms. A; it comprises a series of quarter notes every beat, and the rhythm is consistent, making it easy to play on the Cymis by using the image sensor for finger movement detection and touch panel. There was no change in this procedure or the music chosen for the session.
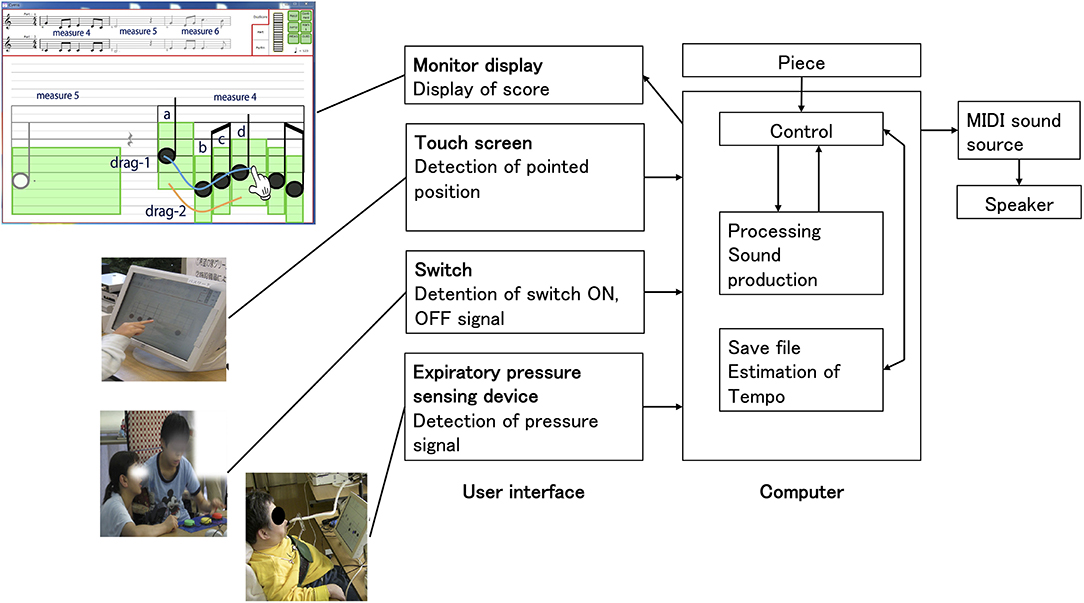
Figure 2. For the musical instrumental performance, we used an accessible digital musical instrument called the Cymis (cyber musical instrument with score) [Akazawa et al. (21)], which has a built-in programmed score and is played using touch panels and switches. The technical novelty of the Cymis lies in its human interface devices that emphasize the sensory experience and is characterized by its built-in score information and program. This computerized musical instrument system comprises a monitor display, a personal computer, a sound source, a speaker, and human interface devices (image sensor for finger movement detection, touch panel, and others). The system is an electronic musical instrument that is barrier-free, allows understanding of music notation, and allows beginners of any age to easily play music comprising melody, rhythm, and harmony.
Follow-Up Period and Outcomes
The cognitive function of the participant declined further compared with that pre-intervention, with an MMSE score of 4 after 1 year (p = 0.388), and BPSD peaked with an NPI score of 54 after 1 year (p < 0.001). After a year and half, Ms. A's MMSE score was 0 (p < 0.001) and her NPI score was 16 (p = 0.617), although only apathy remained (Figure 3, Table 1).
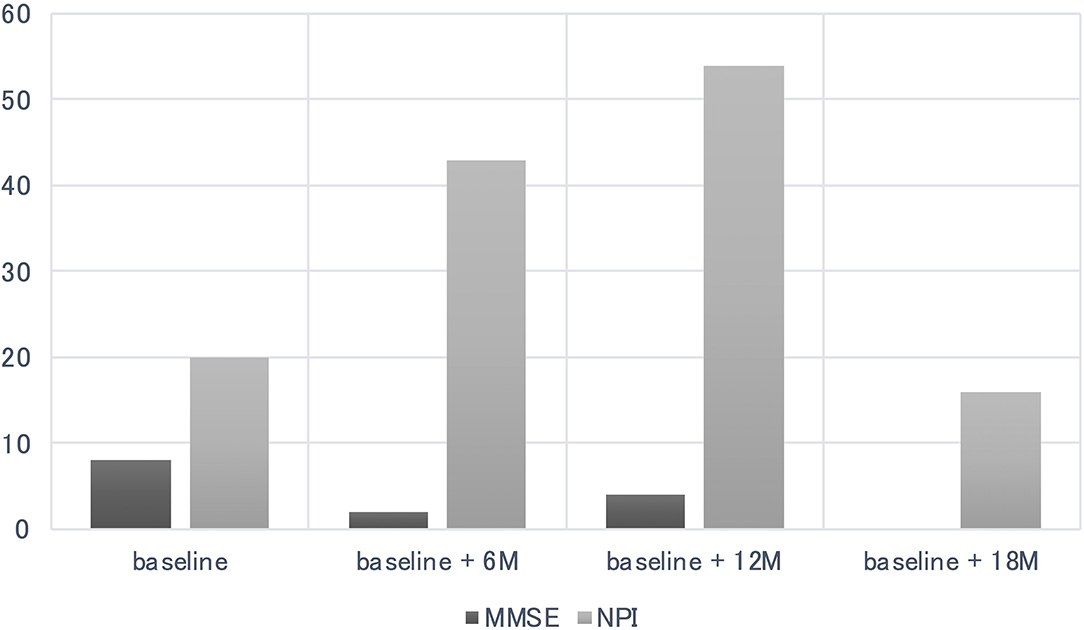
Figure 3. Cognitive function of the participant declined further compared to pre-intervention, with a Mini-Mental State Examination (MMSE) scores of 4 after 1 year (p = 0.388), behavioral and psychological symptoms of dementia (BPSD) peaked with the NPI score of 54 after 1 year (p < 0.001). After a year and half, Ms. A's MMSE score was 0 (p < 0.001) and Neuropsychiatric Inventory (NPI) was 16 (p = 0.617), but only apathy remained.
Despite her cognitive and behavioral abnormalities, the patient continued to play the Cymis twice a week for 15 min per session over an 18-month period. During the MT, Ms. A was able to play the Cymis and focused on the performance even when she was restless. After playing, Ms. A showed a sense of accomplishment and familiarity with the musical instrument. Her music therapist considered her an excellent player with advanced skills in accuracy, rhythm, and tempo.
Sessions (S) S1 to S17 dealt with using the touch panel (playing notes), and S18 onward dealt with using one switch (playing beats), and subsequently, the touch panel (playing notes or beats). In S24, although the patient was very unsettled, she understood that she could play notes by touching the rectangular part of the musical instrument and played it with her thumb; however, she subsequently returned to playing the musical instrument with her index finger to make it easier for her to play. In S4, Ms. A remembered having played the musical instrument previously. From S15 onward, the Ms. A's cognitive and verbal functions gradually declined, and she had difficulty recalling words and repeated a single word. Ms. A's mental decline progressed, and she had difficulty in writing her name and letters. Ms. A would cry due to restlessness and anxiety. However, Ms. A was able to turn her attention to her performance while playing the Cymis. It was observed that Ms. A would hit the touch panel and switches to play the musical instrument when she was restless. She would also repeatedly press the switch when the sound did not play due to an operational error. After the performance, a sense of accomplishment, positive feedback, and a sense of familiarity were observed in the patient: she would say “It felt good,” “It was easy,” and “I've done it before.” In the self-evaluation, although Ms. A was unable to write, she welcomed the opportunity to self-evaluate, and although she was unable to say words due to the decline in her language function around S74, she expressed her anxiety and smiled when we listened to her. After S74, her language function declined and she could not speak, although when we talked to her, she expressed her anxiety and smiled. After S84, her activities of daily living (ADL) decreased and she was confined to a wheelchair, and her hand movements and upper arm range of motion also decreased. However, she was able to operate switches and touch panels with only simple support for the MT. After S90, neuropsychological tests were not performed. After S120, the patient's ADL decreased further, and she became unsteady in a seated position and was sometimes unresponsive. She became unable to understand the operation of the switches and could not operate them, saying “I don't know.” At present, the MT supports Ms. A's hand to operate the touch panel, and she is able to grasp the rectangle and follow the order of the notes with her fingers and press them to play. After the performance, she smiles and applauds.
Discussion
Despite the fact that accessible digital musical instruments can take into account the level of cognitive demands, previous studies (20) have been conducted with MCI, and it is not known whether these instuments can be used by people with moderate to severe dementia or dementia with worsening BPSD. In our case, the patient with VaD was able to play the Cymis throughout the 18 months of MT. The patient's cognitive function of the participant declined further, and BPSD peaked, until only apathy remained. Despite these changes, during MT, the patient was able to play the accessible digital musical instrument and to focus on the performance. These results suggest that patients with severe VaD can play an accessible digital instrument and continue active MT even if their BPSD progress with cognitive decline.
The relationship between the exacerbation of BPSD with cognitive decline and ability to play musical instruments, which plays an important role in active MT, remains unknown. Herein, we report a case of long-term individual MT using an accessible digital musical instrument, which resulted in the person being able to play the musical instrument and to focus on the performance even when she was restless. The Cymis, which has a built-in programmed score, is played using a touch panel and switches. MT gave the patient a sense of accomplishment and familiarity.
The patient in this study learned to play an accessible digital musical instrument for the first time in the late stage of VaD and continued to play it despite progressive BPSD with cognitive decline. These findings suggest that it is possible to learn to play a new accessible digital musical instrument even in the late stage of VaD. Previous case reports have described several patients with dementia who continued to skillfully play musical instruments; however, these patients were professional musicians premorbidly and had a preserved musical ability even after the diagnosis of dementia (25–27). In contrast, Ms. A. had never played a musical instrument other than the koto before her diagnosis of VaD. To the best of our knowledge, this is the first reported case of a person who was able to play a new accessible digital musical instrument in the late stage of VaD, despite no prior professional musical training. There may be several reasons for this. First, playing a musical instrument requires different circuits from those essential to BPSD. Up to 23 brain structures were associated with an increased risk of developing BPSD (28), for which the frontal volume was the most powerful predictor of the frontal gyri, anterior cingulate cortex, and orbital gyri being involved (28). Even if BPSD worsens due to frontal lobe damage, it may be possible to play musical instruments if motor and visuospatial functions are relatively preserved, as described below. Second, learning how to play a new accessible digital musical instrument may require motor skills, which can be attributed to the procedural, non-declarative forms of memory (29, 30). Non-declarative memory includes different forms of learning and memory abilities, including perceptual and motor skills involved in musical performance. The basal ganglia, cerebellum, and supplementary motor regions play a collective role in procedural memory (31, 32). As these areas are generally not affected by VaD, Ms. A. may have acquired and maintained the procedural memory skills required for playing a musical instrument. Third, visuoperceptual skills are required to read musical scores (26). Patients with VaD often have preserved visuo-constructive abilities because the posterior parietal regions are not significantly affected (33); this may have allowed Ms. A. to read the score and to play music on Cymis. VaD is associated with aphasia along with visuospatial and motor impairments, depending on the location of the affected area of the cerebrum, and symptoms tend to fluctuate everyday due to inadequate cerebral blood flow (33). However, in some cases, as in the patient in this study, it is possible for the person to play a musical instrument. Therefore, the preserved functions should be assessed before intervention, which should be tailored to the person's preserved functions (34).
The results of this study showed that even if BPSD continues to worsen, if the ability to play musical instruments is relatively preserved, it is possible to play accessible digital musical instruments in MT and to continue MT even in the later stages of dementia.
Our study had some limitations. We did not use the severe impairment battery (35) ideal test and did not examine the performedADLs (36) on a regular basis, similar to other neuropsychological tests. Moreover, we could not establish a pathological diagnosis for the patient. Finally, this was a case study; thus, the findings cannot be generalized.
In conclusion, this study showed that it is possible for people with late-stage VaD to learn to play a new accessible digital musical instrument and to continue to play it despite progressive BPSD with cognitive decline, which may have implications for the use of MT and music-based cognitive rehabilitation in persons with VaD.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by the Research Safety and Ethics Committee of the Advanced Institute of Industrial Technology (AIIT). Written informed consent to participate in this study was provided by the patient's legal guardian/next of kin. Written informed consent was obtained from the patient's legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
Author Contributions
KT: conceived and designed the experiments and analyzed the data. EK: conducted the experiments. KT, EK, and KA: wrote the paper. RO and KA: contributed materials. KA: supervised and interpreted the data. All authors read and approved the final version of the article.
Funding
This study was supported by JSPS KAKENHI (Grant Numbers: 17K17811, 20H04303, and 21K12194).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Mecocci P, Boccardi V. The impact of aging in dementia: It is time to refocus attention on the main risk factor of dementia. Ageing Res Rev. (2021) 65:101210. doi: 10.1016/j.arr.2020.101210
2. Zhang Y, Cai J, An L, Hui F, Ren T, Ma H, et al. Does music therapy enhance behavioral and cognitive function in elderly dementia patients? A systematic review and meta-analysis. Ageing Res Rev. (2017) 35:1–11. doi: 10.1016/j.arr.2016.12.003
3. Dorris JL, Neely S, Terhorst L, VonVille HM, Rodakowski J. Effects of music participation for mild cognitive impairment and dementia: a systematic review and meta-analysis. J Am Geriatr Soc. (2021) 69:2659–67. doi: 10.1111/jgs.17208
4. Moreno-Morales C, Calero R, Moreno-Morales P, Pintado C. Music therapy in the treatment of dementia: a systematic review and meta-analysis. Front Med (Lausanne). (2020) 7:160. doi: 10.3389/fmed.2020.00160
5. van der Steen JT, Smaling HJ, van der Wouden JC, Bruinsma MS, Scholten RJ, Vink AC. Music-based therapeutic interventions for people with dementia. Cochrane Database Syst Rev. (2018) 7:CD003477. doi: 10.1002/14651858.CD003477.pub4
6. Tsoi KKF, Chan JYC, Ng YM, Lee MMY, Kwok TCY, Wong SYS. Receptive music therapy is more effective than interactive music therapy to relieve behavioral and psychological symptoms of dementia: a systematic review and meta-analysis. J Am Med Dir Assoc. (2018) 19:568–76 e3. doi: 10.1016/j.jamda.2017.12.009
7. Kim SJ, Yoo GE. Instrument playing as a cognitive intervention task for older adults: a systematic review and meta-analysis. Front Psychol. (2019) 10:151. doi: 10.3389/fpsyg.2019.00151
8. Liu MN, Liou YJ, Wang WC, Su KC, Yeh HL, Lau CI, et al. Group Music Intervention Using Percussion Instruments to Reduce Anxiety Among Elderly Male Veterans with Alzheimer Disease. Med Sci Monit. (2021) 27:e928714. doi: 10.12659/MSM.928714
9. Kim SJ, Cho SR, Yoo GE. Age-related changes in bimanual instrument playing with rhythmic cueing. Front Psychol. (2017) 8:1569. doi: 10.3389/fpsyg.2017.01569
10. Doi T, Verghese J, Makizako H, Tsutsumimoto K, Hotta R, Nakakubo S, et al. Effects of Cognitive Leisure Activity on Cognition in Mild Cognitive Impairment: Results of a Randomized Controlled Trial. J Am Med Dir Assoc. (2017) 18:686–91. doi: 10.1016/j.jamda.2017.02.013
11. Sung HC, Lee WL, Li TL, Watson R. A group music intervention using percussion instruments with familiar music to reduce anxiety and agitation of institutionalized older adults with dementia. Int J Geriatr Psychiatry. (2012) 27:621–7. doi: 10.1002/gps.2761
12. Chen YL, Pei YC. Musical dual-task training in patients with mild-to-moderate dementia: a randomized controlled trial. Neuropsychiatr Dis Treat. (2018) 14:1381–93. doi: 10.2147/NDT.S159174
13. Chu H, Yang CY, Lin Y, Ou KL, Lee TY, O'Brien AP, et al. The impact of group music therapy on depression and cognition in elderly persons with dementia: a randomized controlled study. Biol Res Nurs. (2014) 16:209–17. doi: 10.1177/1099800413485410
14. Shimizu N, Umemura T, Matsunaga M, Hirai T. Effects of movement music therapy with a percussion instrument on physical and frontal lobe function in older adults with mild cognitive impairment: a randomized controlled trial. Aging Ment Health. (2018) 22:1614–26. doi: 10.1080/13607863.2017.1379048
15. Magee WL, Clark I, Tamplin J, Bradt J. Music interventions for acquired brain injury. Cochrane Database Syst Rev. (2017) 1:CD006787. doi: 10.1002/14651858.CD006787.pub3
16. Seinfeld S, Figueroa H, Ortiz-Gil J, Sanchez-Vives MV. Effects of music learning and piano practice on cognitive function, mood and quality of life in older adults. Front Psychol. (2013) 4:810. doi: 10.3389/fpsyg.2013.00810
17. Bugos JA, Perlstein WM, McCrae CS, Brophy TS, Bedenbaugh PH. Individualized piano instruction enhances executive functioning and working memory in older adults. Aging Ment Health. (2007) 11:464–71. doi: 10.1080/13607860601086504
18. Cho H, Chin J, Suh MK, Kim HJ, Kim YJ, Ye BS, et al. Postmorbid learning of saxophone playing in a patient with frontotemporal dementia. Neurocase. (2015) 21:767–72. doi: 10.1080/13554794.2014.992915
19. Frid E. Accessible Digital Musical Instruments—A Review of Musical Interfaces in Inclusive Music Practice. Multimodal Technol Interact. (2019) 4:34. doi: 10.3390/mti3030057
20. Han E, Park J, Kim H, Jo G, Do HK, Lee BI. Cognitive intervention with musical stimuli using digital devices on mild cognitive impairment: a pilot study. Healthcare (Basel). (2020) 8:45. doi: 10.3390/healthcare8010045
21. Akazawa K, Ichinose T, Matsumoto K, Ichie M, Masuko T, Okuno R. Novel electronic musical instrument with pre-programmed score for the disabled to enjoy playing music. Adv Biomed Eng. (2017) 6:1–7. doi: 10.14326/abe.6.1
22. Katoh S. Development of the revised version of Hasegawa's Dementia Scale (HDS-R). Jpn J Ger Psychiat. (1991) 2:1339–47.
23. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. (1975) 12:189–98. doi: 10.1016/0022-3956(75)90026-6
24. Cummings JL, Mega M, Gray K, Rosenberg-Thompson S, Carusi DA, Gornbein J. The Neuropsychiatric Inventory: comprehensive assessment of psychopathology in dementia. Neurology. (1994) 44:2308–14. doi: 10.1212/WNL.44.12.2308
25. Hailstone JC, Omar R, Warren JD. Relatively preserved knowledge of music in semantic dementia. J Neurol Neurosurg Psychiatry. (2009) 80:808–9. doi: 10.1136/jnnp.2008.153130
26. Miller BL, Boone K, Cummings JL, Read SL, Mishkin F. Functional correlates of musical and visual ability in frontotemporal dementia. Br J Psychiatry. (2000) 176:458–63. doi: 10.1192/bjp.176.5.458
27. Weinstein J, Koenig P, Gunawardena D, McMillan C, Bonner M, Grossman M. Preserved musical semantic memory in semantic dementia. Arch Neurol. (2011) 68:248–50. doi: 10.1001/archneurol.2010.364
28. Boublay N, Bouet R, Dorey JM, Padovan C, Makaroff Z, Federico D, et al. Brain Volume Predicts Behavioral and Psychological Symptoms in Alzheimer's Disease. J Alzheimers Dis. (2020) 73:1343–53. doi: 10.3233/JAD-190612
29. Crystal HA, Grober E, Masur D. Preservation of musical memory in Alzheimer's disease. J Neurol Neurosurg Psychiatry. (1989) 52:1415–6. doi: 10.1136/jnnp.52.12.1415
30. Polk M, Kertesz A. Music and language in degenerative disease of the brain. Brain Cogn. (1993) 22:98–117. doi: 10.1006/brcg.1993.1027
31. Daselaar SM, Rombouts SA, Veltman DJ, Raaijmakers JG, Jonker C. Similar network activated by young and old adults during the acquisition of a motor sequence. Neurobiol Aging. (2003) 24:1013–9. doi: 10.1016/S0197-4580(03)00030-7
32. Exner C, Koschack J, Irle E. The differential role of premotor frontal cortex and basal ganglia in motor sequence learning: evidence from focal basal ganglia lesions. Learn Mem. (2002) 9:376–86. doi: 10.1101/lm.48402
33. O'Brien JT, Thomas A. Vascular dementia. Lancet. (2015) 386:1698–706. doi: 10.1016/S0140-6736(15)00463-8
34. Tabei KI, Satoh M, Ogawa JI, Tokita T, Nakaguchi N, Nakao K, et al. Cognitive Function and Brain Atrophy Predict Non-pharmacological Efficacy in Dementia: The Mihama-Kiho Scan Project2. Front Aging Neurosci. (2018) 10:87. doi: 10.3389/fnagi.2018.00087
35. Panisset M, Roudier M, Saxton J, Boller F. Severe impairment battery. A neuropsychological test for severely demented patients. Arch Neurol. (1994) 51:41–5. doi: 10.1001/archneur.1994.00540130067012
36. Galasko D, Bennett D, Sano M, Ernesto C, Thomas R, Grundman M, et al. An inventory to assess activities of daily living for clinical trials in Alzheimer's disease. The Alzheimer's Disease Cooperative Study. Alzheimer Dis Assoc Disord. (1997) 11 Suppl 2:S33–9. doi: 10.1097/00002093-199700112-00005
Keywords: dementia, accessible digital musical instrument, cyber musical instrument with score, neuropsychological test, behavioral and psychological symptoms of dementia
Citation: Kondo E, Tabei K, Okuno R and Akazawa K (2022) Case Report: Accessible Digital Musical Instrument Can Be Used for Active Music Therapy in a Person With Severe Dementia and Worsening Behavioral and Psychological Symptoms: A Case Study Over a Year and a Half. Front. Neurol. 13:831523. doi: 10.3389/fneur.2022.831523
Received: 08 December 2021; Accepted: 17 February 2022;
Published: 06 April 2022.
Edited by:
Bruce Miller, University of California, San Francisco, United StatesReviewed by:
Nilton Custodio, Peruvian Institute of Neurosciences (IPN), PeruChan-Young Kwon, Dong-eui University, South Korea
Copyright © 2022 Kondo, Tabei, Okuno and Akazawa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ken-ichi Tabei, a2VuaWNoaS50YWJlaUBnbWFpbC5jb20=
 Eisuke Kondo
Eisuke Kondo Ken-ichi Tabei
Ken-ichi Tabei Ryuhei Okuno4
Ryuhei Okuno4 Kenzo Akazawa
Kenzo Akazawa